Published online Aug 26, 2014. doi: 10.13105/wjma.v2.i3.127
Revised: May 17, 2014
Accepted: July 18, 2014
Published online: August 26, 2014
Processing time: 212 Days and 1.2 Hours
AIM: To analyze the cost-effectiveness of the diagnosis of solitary pulmonary nodule (SPN) in China.
METHODS: Decision analysis models were constructed to assess the cost-effectiveness of four strategies for the management of SPN: computed tomography (CT) alone, CT plus CT-guided automated cutting needle biopsy (ACNB), CT plus positron emission tomography/computed tomography (PET/CT), CT plus diffusion-weighted magnetic resonance imaging (DWI) plus PET/CT.
RESULTS: The prevalence of lung cancer among SPN discovered in the clinical setting was approximately 50%. The CT plus ACNB strategy had higher diagnostic accuracies (87% vs 81%), with a cost saving of ¥1945 RMB per patient, and reducing unnecessary thoracotomy by 16.5%; this was associated with a 4.5% missed diagnosis rate. CT plus DWI plus PET/CT strategy also had higher accuracies (95% vs 81%), with a cost saving of ¥590 RMB per patient, and reducing unnecessary thoracotomy by 13.5%; this was accompanied by 0.3% missed diagnosis rate. CT plus PET strategy is cost effective at a prevalence rate of 0-34%, but there was a larger prevalence range of lung cancer for CT plus ACNB strategy (from 0 to 0.6) and CT plus DWI plus PET/CT strategy(from 0 to 0.64).
CONCLUSION: CT plus DWI plus PET/CT strategy was cost-effective, and had a higher accuracy accompanied by a lower missed diagnosis rate than CT plus ACNB strategy.
Core tip: It has become a major concern how to manage solitary pulmonary nodule (SPN) discovered in the clinical setting with low cost and high accuracy and reduce the morbidity and mortality associated with radiation, biopsy, and surgical procedures. However, up to now there has not been an analysis of cost-effectiveness of various strategies for the diagnosis and management of SPN in China. Recent studies in other countries may not hold true in a Chinese hospital because of differences in health-care systems and diagnostic strategy. We are the first to perform such an analysis for the cost-effective management of solitary pulmonary nodules in China.
- Citation: Lu B, Sun LX, Yan X, Ai ZZ, Xu JZ. Decision-tree analysis for cost-effective management of solitary pulmonary nodules in China. World J Meta-Anal 2014; 2(3): 127-134
- URL: https://www.wjgnet.com/2308-3840/full/v2/i3/127.htm
- DOI: https://dx.doi.org/10.13105/wjma.v2.i3.127
Lung cancer has become the leading cause of cancer deaths in China because the incidence and mortality are rapidly increasing. Although earlier detection of peripheral lung cancer may reduce the mortality rate, population-based screening using plain chest radiography has been not carried out in China. Therefore, most solitary pulmonary nodules (SPN), which are usually discovered in the clinical setting on hospital in China, have a higher malignant prevalence[1,2]. It has become a major concern how to manage SPN discovered in the clinical setting with low cost and high accuracy and reduce the morbidity and mortality associated with radiation, biopsy, and surgical procedures.
However, up to now there has not been an analysis of cost-effectiveness of various strategies for the diagnosis and management of SPN in China. Recent studies in other countries may not hold true in a Chinese hospital because of differences in health-care systems and diagnostic strategy[3-7]. The cost of surgery is not obviously higher than that of automated cutting needle biopsy (ACNB, six times) and positron emission tomography/computed tomography (PET/CT, three times) in China. But in the United States, Japan and European countries the cost of surgery was twenty times as much as that of biopsy and PET/CT. Because of high cost, PET/CT has not gained widespread popularity in most areas of China. A recent study showed that diffusion-weighted magnetic resonance imaging (DWI) may be able to be used in place of PET/CT for discriminating malignant from benign pulmonary nodules and is associated with significantly less false positives and lower costs than PET/CT[8]. Furthermore, in general, physicians in Chinese hospitals do not perform thoracoscopy with local anesthesia in patients who have or are suspected of having lung cancer.
According to the upper analysis, it is necessary to borrow previous study methods to evaluate the role of CT, ACNB, DWI, and PET/CT in the investigation of SPN which are discovered in the clinical setting in hospital in China. We used decision-tree analysis models and compared four strategies to understand under what conditions various strategies should be cost-effective and have high diagnostic accuracy.
In the current study, we have defined SPN as spherical intrapulmonary x-ray densities less than 4.0 cm in diameter with no calcium visible on a standard chest X-ray. There is no associated atelectasis, hilar enlargement, or pleural effusion. We do not include patients with any evidence of metastasis or a recent primary malignancy outside of the chest. We also exclude cases that have previous radiographs that have already established the stability of the rate of growth of the nodule. Multiple nodules are also not considered in the current analysis.
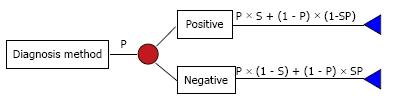
The analysis for cost-effectiveness was performed using quantitative methods of decision analysis. Decision-tree models were constructed with multiple competing strategies, and reported values of prior probability of cancer, and sensitivity and specificity of each diagnostic modality were applied to them using Chinese health care costs. The average cost per patient for each strategy, including all diagnostic tests and surgery when undertaken, was calculated. The medical literature was surveyed to obtain the performance of each diagnostic test. For the calculations, Decision Analysis Add-In for Microsoft Excel (Version1.0.6, Palisade Corporation) was used. The decision tree was constructed using the choices and potential outcomes of the choices. All conditional probabilities of each outcome in the tree were calculated and obtained as a function of the variables listed in Tables 1 and 2 by using Bayesian analysis, Calculation Methods:
Math 6
| Sensitivity | Specificity | Ref. | |
| Chest CT | 0.99 | 0.63 | [5] |
| PET-CT | 0.97 | 0.85 | [5] |
| ACNB | 0.769 | 0.936 | [5] |
| CT-Follow | 0.56 | 0.95 | [3] |
| DWI | 0.7 | 0.97 | [3] |
| Cost (RMB) | |
| Chest CT without contrast enhancement | ¥360 |
| PET-CT | ¥6500 |
| ACNB1 | ¥3000 |
| CT-Follow: continuous three Chest CT | ¥1080 |
| DWI | ¥585 |
| Surgical resection of SPN | ¥20000 |
Where P = prevalence, S = sensitivity, and Sp = specificity.
Calculations of overall cost of competing strategies were calculated by summing the products of the probabilities and values of the outcome of each strategy. Overall costs per patient in each strategy can be calculated automatically by the software and listed under “chance” in Figure 1. Accuracies (A) of each diagnosis method in each strategy were calculated by formula:
A = (S - Sp)P + Sp
False positive (FP), false negatives (FN), true positive (TP) and true negatives (TN) of each diagnosis method in each strategy were calculated by the formula:
FP = 1/{[(Sp-A)S/(1-Sp)(A-S)]+1}
FP = 1/{[(S-A)Sp/(1-S)(A-Sp)]+1}
Overall accuracies of each strategy were calculated by summing the products of the probabilities of the outcome of each strategy and TP plus TN in each strategy; The overall misdiagnosis rate of each strategy was calculated by summing the products of the probabilities of the outcome of each strategy and FP in each strategy; the overall missed diagnosis rate of each strategy was calculated by summing the products of the probabilities of the outcome of each strategy and FN in each strategy.
Cost-effectiveness was expressed as the incremental cost-accuracy ratio (ICAR) where:
ICAR = (Coststrat-Costbl/(Accuracystrat-Accuracybl) (RMB/%)[9].
Coststrat and Accuracystrat are the average cost per patient and accuracy of the strategy being compared, and Costbl and Accuracybl are the cost per patient and accuracy of a baseline strategy, which was the CT alone strategy in this study. A negative ICAR resulting from a negative numerator and positive denominator indicates that the strategy being compared is clearly preferred. In the case of a positive ICAR, a criterion must be chosen that gives the acceptable cost to get a higher accuracy.
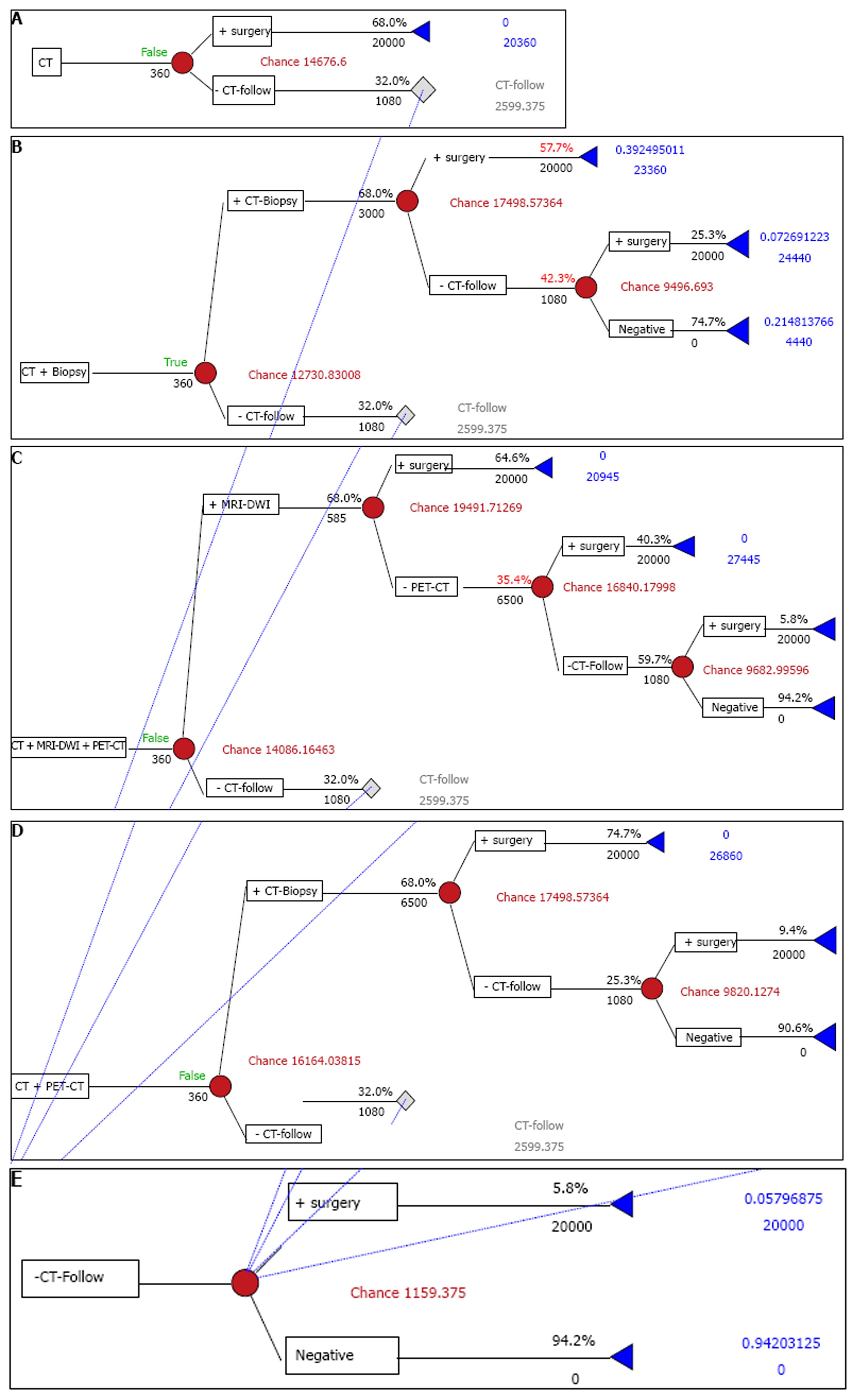
We compared four strategies for the management of SPN (Figure 1): (1) CT alone strategy (baseline), (2) CT plus PET/CT strategy, (3) CT plus ACNB strategy, and (4) a CT-plus-DWI plus PET/CT strategy.
In these strategies, all patients initially undergo a chest CT examination without contrast enhancement. If an initial CT diagnosis of benign pulmonary nodule is made or no SPN is demonstrated on CT, the patients are followed up using an unenhanced chest CT. When follow-up CT shows the growth of the SPN, the diagnosis of lung cancer is made: (1) CT alone strategy: The CT alone strategy simulates a simple diagnostic approach to the management of patients with SPN. In this strategy, all patients, in whom SPN is diagnosed as lung cancer on the initial chest CT, proceed to surgical resection without pathological confirmation; (2) CT plus PET strategy: In this strategy, all patients who are CT positive (i.e., an SPN is diagnosed as lung cancer) undergo chest PET-CT. If the PET/CT is then also positive, the patients proceed to surgical resection. If a chest PET/CT examination is negative after a positive CT examination, the patients are followed up by an unenhanced chest CT; (3) CT plus ACNB strategy: If the initial CT is positive, it is followed directly by ACNB. If the biopsy is then also positive, patient undergo surgical resection. If ACNB is negative, the patients are followed up by an unenhanced chest CT; (4) CT plus DWI plus PET/CT strategy: In this strategy, all patients who are CT positive undergo a chest CT plus DWI strategy. If the CT plus DWI strategy is then also positive, the patients proceed to surgical resection. If a chest a CT plus DWI strategy examination is negative after a positive CT examination, the patients are given an extra CT-plus-PET strategy above-mentioned.
Although there were no large sample statistics for epidemiology, some small sample studies and our experience indicated the prevalence of lung cancer among SPN was approximately 50% in China[1,2]. Therefore, we applied this value (50%) to the decision-tree analyses.
The diagnostic performance (sensitivity and specificity) of each diagnostic test are gleaned from the literature and entered into the models (Table 1). Although multi-slice spiral CT is taking the place of conventional thin slice CT gradually, the diagnostic performance of multi-slice spiral CT on SPN still lack of large sample statistics. Tsubamoto et al[10] reported that accuracy of the final diagnosis based on coronal multi-planar reconstruction of with a multi-detector-row CT scanner (74%) was almost equal to that based on transverse thin-section CT (71%) (P = 0.3) for the evaluation of solitary pulmonary nodules. As a result, we still used CT sensitivity of 99% and specificity of 63% in the largest series published by Siegelman et al[11], their study included 634 nodules, using conventional thin slice CT. From many published reports of PET/CT imaging of SPN, we adopted the results of Yi et al[12] and Kim et al[13]. We applied PET/CT sensitivity of 97% and specificity of 85% to the decision-tree analyses. The diagnostic accuracy of CT-guided transthoracic ACNB has been reported based on comparisons with fine-needle aspiration biopsy. In China, ACNB has been often used by physicians, usually without combining the use of a long-throw biopsy needle, higher mean number of needle passes, and tandem system like Satoh et al[14]; as a result we selected ACNB sensitivity of 76.9% and specificity of 93.6% by Tsukada et al[15]. Although serial CT is probably the most common follow-up methodology to be adopted in the practice, there is little data on the utility of follow-up chest CT for the diagnosis of SPN. Takashima et al[16] reported the sensitivity of 0.56 and specificity of 0.95, when the nodule showing an increase of 0.5 mm or more in the maximum or perpendicular diameter or both on high-resolution CT images was diagnosed as a lung cancer. We applied these values to our analysis. There is a few data on the utility of DWI for the diagnosis of SPN. The study by Mori et al[8] reported the sensitivity of 0.70 and specificity of 0.97, which is similar to our unpublished results, we applied these values to our analysis.
The mean costs of diagnostic tests and thoracotomy in China are shown in Table 2. The cost of thoracotomy in RMB was based on the bills in our hospital during 2009 (n = 20). The costs of diagnostic examinations include the costs of diagnostic procedure and radiological or/and pathological interpretations based on the data of the Harbin Price Bureau (These costs are uniform in China according to the Ministry of Public Health of the People’s Republic of China). In China, patients undergoing ACNB do not stay overnight in a hospital. Although major complications are rare, pneumothorax is the most common complication after ACNB with a reported rate of 22%-54%[14,17,18]. According to our study, chest tube placement was not necessary for the incidence of pneumothorax. A central venous catheter attached to a negative pressure aspirator was used for the treatment of pneumothorax in our hospital. The costs of possible treatment of pneumothorax were included in the cost of CT-guided needle biopsy.
The decision tree methodology can be extended by performing sensitivity analysis to determine the conditions under which the new test remains cost-effective. This was achieved by entering different values for the disease prevalence (0-100%) into the decision-tree models. Although the costs of medical procedures will clearly vary among countries, within China these costs are fixed and therefore need not constitute a variable in the sensitivity analysis.
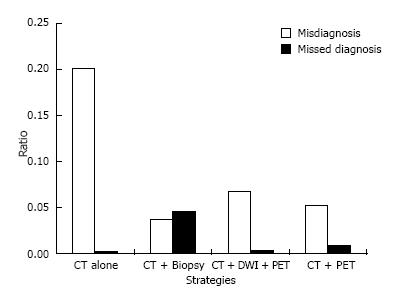
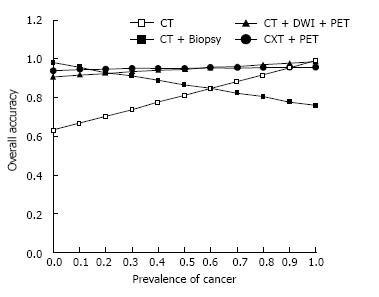
The prevalence of lung cancer among SPN discovered in hospital in the clinical setting was approximately 50%. In this prevalence, the strategies using CT plus ACNB and CT plus DWI plus PET/CT were the cost-effective alternatives to the CT alone strategy. The CT plus ACNB strategy had higher accuracies (87% vs 81%), with a cost saving of ¥1945 RMB per patient, and reduced the number of candidates who underwent unnecessary thoracotomy for a benign SPN by 16.5%; this was accompanied by a rate of missed diagnosis of 4.5%. The strategies using CT plus DWI plus PET/CT had also higher accuracies (95% vs 81%), with a cost saving of ¥590 RMB per patient, and reduced unnecessary thoracotomy by 13.5%; this was accompanied by a rate of missed diagnosis of 0.3% (Table 3, Figure 2).
| Strategy | Accuracy | Cost per patient | ICAR (RMB/%) |
| CT alone | 0.81 | 14676 | Baseline |
| CT + PET-CT | 0.952 | 16164 | 8196 |
| CT + ACNB | 0.867 | 12731 | -17583 |
| CT + DWI + PET-CT | 0.949 | 14086 | -4247 |
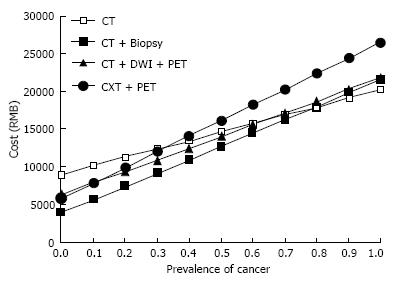
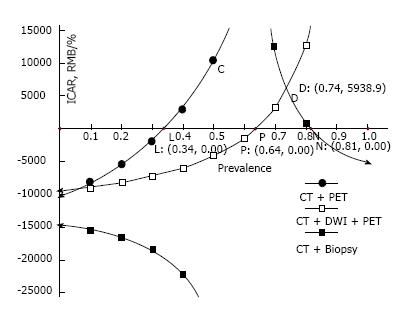
At a prevalence of cancer up to 34%, CT plus PET strategy is cost effective with a higher accuracy than CT alone strategy. But CT plus ACNB strategy and CT plus DWI plus PET/CT strategy had a better cost-effectiveness over a larger prevalence of lung cancer, ranging from 0 to 0.60 (CT plus ACNB) and from 0 to 0.63 (CT plus DWI plus PET/CT).
The total costs per patient were increased regardless of the strategies, and the difference among the strategies became small (Figure 3). By reducing the number of the candidates who undergo unnecessary thoracotomy for a benign SPN (Figure 2), CT plus ACNB strategy and CT plus DWI plus PET/CT strategy decreased the total costs per patients. The total costs per patient of CT plus DWI plus PET/CT strategy were reduced not only by reducing unnecessary thoracotomy by 13.5%, but also by giving 44% of the candidates a chance to avoid undergoing expensive PET/CT, meanwhile, the overall accuracy of the CT plus DWI plus PET/CT strategy was not lower than that of CT plus PET strategy (Figure 4).
ICAR of the strategies using CT plus ACNB and CT plus DWI plus PET/CT were negative values with higher accuracies, clearly representing cost-effectiveness compared to the CT alone strategy (Figure 5). Although CT plus ACNB strategy is more cost saving, CT plus DWI plus PET/CT strategy has a lower rate of missed diagnosis (Figure 2) and a higher overall accuracy (Figure 4).
Figure 5 plots the prevalence of cancer versus ICAR. Since the CT alone strategy had a higher cost at the prevalence of cancer between 0 and 64% (Figure 3), in our analysis, a negative ICAR means that CT plus ACNB strategy and CT plus DWI plus PET/CT strategy have lower costs with higher accuracies. At the prevalence of cancer up to 34%, all strategies were cost-effective.
From the analyses performed here, adding ACNB, DWI, or PET/CT is advantageous in terms of greater accuracy and cost-effectiveness. The results of our sensitivity analyses showed that CT plus ACNB strategy and CT plus DWI plus PET/CT strategy have a wide range of prevalence of cancer, and CT alone strategy becomes more cost-effective only when the prevalence of cancer exceeds approximately 65%.
In the study, we assumed that SPN evaluated were discovered in the clinical setting in hospital. In our daily clinical setting, the prevalence of lung cancer among SPN was approximately 50%, far higher than those detected on lung cancer screening. For SPN discovered in the lung cancer screening, for a lower prevalence (approximately 10%), reducing false-positives to avoid more morbidity, mortality and increased costs for unnecessary thoracotomy is of importance; but for SPN discovered in the clinical setting in hospital, with a very high pretest probability, avoiding a missed diagnosis for false-negatives is as important as decreasing the misdiagnosis rate and reducing the cost. In the current study, CT plus ACNB strategy had a more cost saving and lower misdiagnosis rate, but also accompanied by higher rate of missed diagnosis up to 4.5%. The strategies using CT plus DWI plus PET/CT had higher accuracies (95% vs 81%), accompanied by a lower rate of missed diagnosis of 0.3%. This means there is an increase in life expectancy for decreasing rate of missed diagnosis.
The current analysis implies that the use of CT plus ACNB strategy or CT plus DWI plus PET/CT strategy can provide an advantage of a lower cost with higher accuracy. In the prevalence of cancer of 50%, the CT plus DWI plus PET/CT strategy is the optimal choice. In the United States, Japan and European countries the cost of surgery was twenty times as much as that of PET/CT. But in China the cost of surgery is only three times as much as that of PET/CT. Therefore, by reducing the number of the candidates who undergo unnecessary thoracotomy for a benign SPN, CT plus PET/CT strategy only decreased limited total costs per patients, which was hard to compensate for expensive cost of PET/CT, especially when the prevalence of lung cancer was up to 34%. A recent study showed that DWI may be able to be used in place of PET/CT for discriminating malignant from benign pulmonary nodules and is associated with significantly less false positive and lower cost than PET/CT[8]. In our unpublished study, a false-positive of DWI for SPN was only 3.5%. We assumed that most malignant SPN first could be identified by undergoing DWI previous to PET/CT, then negative nodules were added to PET/CT examination at a relatively low prevalence of lung cancer. The current study showed that the CT plus DWI plus PET/CT strategy decreased the total costs per patients not only by reducing unnecessary thoracotomy by 13.5%, but also by giving 44% of the candidates a chance to avoid undergoing expensive PET/CT; meanwhile, overall accuracies of CT plus DWI plus PET/CT strategy was not significantly lower than that of CT plus PET strategy.
ICAR of CT plus ACNB strategy are lower than that of the CT plus DWI plus PET/CT strategy, suggesting better cost-effectiveness of ACNB for SPN diagnosis, but we considered CT plus ACNB strategy is not an optimal option for the evaluation of SPN according to the analysis of current results. Most importantly, overall accuracies of CT plus ACNB strategy decreased gradually with the prevalence of lung cancer increasing, and was similar to that of CT alone strategy at a prevalence of lung cancer up to 50%. With the accompaniment of this, CT plus ACNB strategy had a rate of missed diagnosis of 4.5% for the evaluation of SPN, which was significantly higher than 0.3% of CT plus DWI plus PET/CT strategy. The high rate of missed diagnosis will inevitably reduce life expectancy. Secondly, unlike those discovered by screening chest radiography, most SPN discovered in the clinical setting in hospital are usually larger than 1 cm in diameter and with a high pretest probability. For such a large SPN, PET/CT has a higher negative predictive value and a lower rate of missed diagnosis; if this is accompanied with DWI with a higher positive predictive value and lower misdiagnosis rate, there will be an increase in cost-effectiveness. Our results underscored the point. In addition, although major complications are rare, pneumothorax is the most common complication with a reported rate of 22%-54% with ACNB[14,17,18]. A central venous catheter attached to negative pressure aspirator was used for the treatment of pneumothorax in our hospital. These invasions not only increased medical costs, but also caused some physical or mental injuries.
The current study is entirely a statistical simulation, and individual variation should and will inevitably occur in real medical practice. Therefore, the utility of a decision tree analysis must always be limited. Patient preferences and concerns must be considered when determining how to manage an individual patient. Although, according to this analysis, the CT plus DWI plus PET strategy was the optimal choice, the selection of strategy depends not only on the cost-effectiveness, but also on variable patient factors and accessibility to the modalities. Risk-taking attitudes of the patient and physician will also influence the choice of testing strategies. Because PET/CT is not yet widely available in China, with a difficulty in accessing it for many patients, CT alone strategy often is used for discrimination between malignant and benign SPN. Because of a high prevalence of lung cancer among SPN discovered in hospital in China, especially with a pretest probability up to 64%, in terms of ICAR in Figure 5 CT alone strategy is cost-effective. Between a prevalence of 80%-100%, CT plus ACNB is also cost-effective (Figure 5), but is often not used because of a rather low accuracy (Figure 4).
There were some limits to our study. First, SPN which are diagnosed as lung cancer were assumed to require surgery regardless of cancer staging. However, many factors interact to determine the needs of further examinations of the lung lesions and its resectability, including not only tumor staging, but also performance status and cardiopulmonary status. These factors were not traced in the models. Secondly, because of the lack of large sample study in China, the diagnostic performance (sensitivity and specificity) of each diagnostic test was gleaned from the literature which were published in the United States, Japan and European countries. We used those that were similar to results of a small sample study in China.
In conclusion, the introduction of CT plus DWI plus PET/CT strategy for the evaluation of SPN, which are discovered on chest radiography in the clinical setting, is potentially cost-effective in China with higher accuracy, over a large prevalence of cancer. When the prevalence of cancer rises up to 65%, the introduction of CT alone strategy for the evaluation of SPN is potentially cost-effective.
It has become a major concern about how to reduce the mortality rate of lung cancer, for it has become the leading cause of cancer deaths in China because the incidence and mortality are rapidly increasing. Although the authors have noted earlier detection of peripheral lung cancer, population-based screening using plain chest radiograph has been not carried out in China. Therefore, most solitary pulmonary nodules, which are usually discovered in the clinical setting in hospital in China, have a higher malignant prevalence.
Recent studies in other countries may not work for the Chinese hospital setting because of differences in health-care systems and diagnostic strategy. The cost of surgery is not obviously higher than that of automated cutting needle biopsy (ACNB, six times) and positron emission tomography/computed tomography (PET/CT, three times) in China. But in the United States, Japan and European countries the cost of surgery was twenty times as much as that of biopsy and PET/CT. Because of expensive cost, PET/CT has not gained widespread popularity in most areas of China. A recent study showed that diffusion-weighted magnetic resonance imaging (DWI) may be able to be used in place of PET/CT for discriminating malignant from benign pulmonary nodules and is associated with significantly less false positives and lower cost than PET/CT.
Up to now there has not been an analysis of cost-effectiveness of various strategies for the diagnosis of solitary pulmonary nodule (SPN) in China. Through the four strategies for the management of SPN: CT alone, CT plus CT-guided ACNB, CT plus PET/CT, CT plus DWI plus PET/CT, we analyzed the cost-effectiveness and chose CT plus DWI plus PET/CT strategy as an optimal option for the evaluation of SPN in China, because this strategy was not only cost-effective, but also had a higher accuracy accompanied by a lower missed diagnosis rate than CT plus ACNB strategy.
According to this analysis, the CT plus DWI plus PET strategy was the optimal choice, which can be applied on chest radiograph in the clinical setting, having potential cost-effectiveness in China with higher accuracy, over a large prevalence of cancer.
SPN is the round or oval opaque areas of solitary pulmonary with the diameter < 3 cm performed on the X-line. The standards of the diagnosis of lung cancer by CT: there is a blood supply in the malignant tumor, while the benign tumor has lower or no blood supply; the malignant tumor has an irregular shape and sublobe with burrs on the edge.
In the manuscript Lu et al present the results of an analysis of cost-effectiveness of various strategies for the diagnosis of SPN in China. They have assessed the cost-effectiveness of four strategies for the management of SPN: CT alone, CT plus CT-guided ACNB, CT plus PET/CT, CT plus DWI plus PET/CT. The English of the text is of high quality, clear and easy to follow. The tables and the figures are clear and self explanatory. The statistical approach meets the current standards.
| 1. | Zhang L, Wang M, Wang Y, Li L. [Clinico-pathological study of 98 patients with pulmonary solitary nodule]. Zhonghua Zhong Liu Za Zhi. 2002;24:491-493. [PubMed] |
| 2. | Chen W, Liu J, Chen Q, Li W, Xiong Z, Long X. [Bayes analysis in clinical decision-making for solitary pulmonary nodules]. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2009;34:401-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Tsushima Y, Endo K. Analysis models to assess cost effectiveness of the four strategies for the work-up of solitary pulmonary nodules. Med Sci Monit. 2004;10:MT65-MT72. [PubMed] |
| 4. | Keith CJ, Miles KA, Griffiths MR, Wong D, Pitman AG, Hicks RJ. Solitary pulmonary nodules: accuracy and cost-effectiveness of sodium iodide FDG-PET using Australian data. Eur J Nucl Med Mol Imaging. 2002;29:1016-1023. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Gambhir SS, Shepherd JE, Shah BD, Hart E, Hoh CK, Valk PE, Emi T, Phelps ME. Analytical decision model for the cost-effective management of solitary pulmonary nodules. J Clin Oncol. 1998;16:2113-2125. [PubMed] |
| 6. | Kosuda S, Ichihara K, Watanabe M, Kobayashi H, Kusano S. Decision-tree sensitivity analysis for cost-effectiveness of chest 2-fluoro-2-D-[(18)F]fluorodeoxyglucose positron emission tomography in patients with pulmonary nodules (non-small cell lung carcinoma) in Japan. Chest. 2000;117:346-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Gould MK, Sanders GD, Barnett PG, Rydzak CE, Maclean CC, McClellan MB, Owens DK. Cost-effectiveness of alternative management strategies for patients with solitary pulmonary nodules. Ann Intern Med. 2003;138:724-735. [PubMed] |
| 8. | Mori T, Nomori H, Ikeda K, Kawanaka K, Shiraishi S, Katahira K, Yamashita Y. Diffusion-weighted magnetic resonance imaging for diagnosing malignant pulmonary nodules/masses: comparison with positron emission tomography. J Thorac Oncol. 2008;3:358-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 153] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 9. | Dietlein M, Weber K, Gandjour A, Moka D, Theissen P, Lauterbach KW, Schicha H. Cost-effectiveness of FDG-PET for the management of solitary pulmonary nodules: a decision analysis based on cost reimbursement in Germany. Eur J Nucl Med. 2000;27:1441-1456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 38] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Tsubamoto M, Johkoh T, Kozuka T, Honda O, Koyama M, Murai S, Inoue A, Sumikawa H, Tomiyama N, Hamada S. Coronal multiplanar reconstruction view from whole lung thin-section CT by multidetector-row CT: determination of malignant or benign lesions and differential diagnosis in 68 cases of solitary pulmonary nodule. Radiat Med. 2003;21:267-271. [PubMed] |
| 11. | Siegelman SS, Khouri NF, Leo FP, Fishman EK, Braverman RM, Zerhouni EA. Solitary pulmonary nodules: CT assessment. Radiology. 1986;160:307-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 194] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 12. | Yi CA, Lee KS, Kim BT, Choi JY, Kwon OJ, Kim H, Shim YM, Chung MJ. Tissue characterization of solitary pulmonary nodule: comparative study between helical dynamic CT and integrated PET/CT. J Nucl Med. 2006;47:443-450. [PubMed] |
| 13. | Kim SK, Allen-Auerbach M, Goldin J, Fueger BJ, Dahlbom M, Brown M, Czernin J, Schiepers C. Accuracy of PET/CT in characterization of solitary pulmonary lesions. J Nucl Med. 2007;48:214-220. [PubMed] |
| 14. | Satoh S, Ohdama S, Matsubara O, Okochi Y, Tanaka R, Kimula Y. CT-guided automated cutting needle biopsy by a combined method for accurate specific diagnosis of focal lung lesions. Radiat Med. 2005;23:30-36. [PubMed] |
| 15. | Tsukada H, Satou T, Iwashima A, Souma T. Diagnostic accuracy of CT-guided automated needle biopsy of lung nodules. AJR Am J Roentgenol. 2000;175:239-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 211] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 16. | Takashima S, Sone S, Li F, Maruyama Y, Hasegawa M, Kadoya M. Indeterminate solitary pulmonary nodules revealed at population-based CT screening of the lung: using first follow-up diagnostic CT to differentiate benign and malignant lesions. AJR Am J Roentgenol. 2003;180:1255-1263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 100] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 17. | Klein JS, Salomon G, Stewart EA. Transthoracic needle biopsy with a coaxially placed 20-gauge automated cutting needle: results in 122 patients. Radiology. 1996;198:715-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 218] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 18. | Li H, Boiselle PM, Shepard JO, Trotman-Dickenson B, McLoud TC. Diagnostic accuracy and safety of CT-guided percutaneous needle aspiration biopsy of the lung: comparison of small and large pulmonary nodules. AJR Am J Roentgenol. 1996;167:105-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 259] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
P- Reviewer: Komócsi A S- Editor: Song XX L- Editor: O’Neill M E- Editor: Lu YJ