Published online Dec 20, 2025. doi: 10.5662/wjm.v15.i4.104655
Revised: March 5, 2025
Accepted: March 20, 2025
Published online: December 20, 2025
Processing time: 220 Days and 22.5 Hours
Advanced materials and techniques are used to successfully manage the apexi
Apexification is a regenerative endodontic procedure that involves creating a calcified barrier at the apex of a nonvital tooth with an open apex. This technique is commonly used in immature teeth with necrotic pulps to ensure proper root canal sealing. Traditionally, calcium hydroxide was the preferred material, but advances have introduced bioceramic cements like MTA or Biodentine, which provide superior results with less treatment time. Apexification not only helps to maintain the tooth's structural integrity but also prevents further complications, making it an important procedure in such cases.
This case demonstrates the effectiveness of integrating advanced materials, precise irrigation protocols, and magnification tools in the apexification of immature teeth with open apices. The use of MTA created a stable apical barrier, while bioceramic sealers enhanced the seal and promoted long-term healing. NaOCl with internal heating, ultrasonic activation, and double-sided vented needles ensured thorough irrigation and disinfection, especially in complex canal anatomy.
Core Tip: Advanced materials and techniques are used to successfully manage the apexification of immature teeth with open apices. The use of mineral trioxide aggregate (MTA), bioceramic sealers, and sodium hypochlorite, combined with internal heating activation, ensures that canals are cleaned, disinfected, and sealed properly. Magnification devices, such as dental operating microscopes, provide precise visualization for accurate material placement, while the micro apical placement system ensures void-free MTA delivery. This modern approach improves procedural outcomes, lowers iatrogenic errors, and increases long-term success in apexification, making it a dependable and predictable treatment option for immature teeth.
- Citation: Chauhan R, Chauhan S, Bhasin P, Sood A, Kumar H, Gupta A, Bhasin M. Precision at the apex: Apexification under magnification: A case report. World J Methodol 2025; 15(4): 104655
- URL: https://www.wjgnet.com/2222-0682/full/v15/i4/104655.htm
- DOI: https://dx.doi.org/10.5662/wjm.v15.i4.104655
Apexification is a specialized pediatric procedure aimed at managing immature teeth with necrotic pulp and open apices, often caused by trauma, caries, or pulp pathosis. The procedure focuses on inducing the formation of a calcified apical barrier, enabling proper sealing and long-term retention of the affected tooth[1]. Historically, calcium hydroxide was the material of choice for apexification due to its ability to stimulate the formation of hard tissue barriers[2]. However, its use necessitated a longer treatment period and multiple visits, increasing the risk of root fractures and patient noncompliance. These limitations paved the way for the adoption of bioactive materials like mineral trioxide aggregate (MTA), biodentine (Septodont, Saint-Maur-des-Fosses, France), and bioceramic putty as a superior alternative[3].
MTA has revolutionized apexification due to its exceptional biocompatibility, sealing ability, and capacity to promote cementogenesis and osteogenesis. Unlike calcium hydroxide, MTA provides predictable results in a much shorter amount of time and improves the long-term prognosis of immature teeth[4]. It creates a strong apical barrier that effectively seals the root canal system and prevents bacterial infiltration. Furthermore, its ability to promote periapical healing and stimulate hard tissue deposition has made it the preferred material for apexification procedures[5].
The use of advanced magnification devices, such as dental operating microscopes (DOMs), has increased the precision and efficacy of apexification. Magnification is essential for identifying the complex anatomy of immature teeth with open apices, which frequently exhibit irregularities or resorption[6]. The use of DOMs provides clinicians with unparalleled visualization, allowing for meticulous canal debridement, accurate apical defect assessment, and precise MTA placement. This level of precision minimizes procedural errors like overfilling and void formation, both of which can jeopardize the outcome[7].
In the context of apexification, the combination of MTA and magnification results in superior clinical outcomes. MTA's regenerative properties, combined with the increased accuracy provided by DOMs, allow for optimal apical barrier formation even in difficult cases[8]. This combination has significantly improved the predictability and success rate of apexification procedures, allowing teeth to be saved that would otherwise be extracted[9]. This case report demonstrates the successful management of an open apex with MTA under magnification, highlighting the importance of these advancements in modern pediatric and endodontic practice.
A 13-year-old female patient presented with severe pain and discomfort in her upper front tooth, which had persisted for the previous 2 months following trauma 2 years prior.
The pain was described as spontaneous, intermittent, and aggravated by biting and thermal stimuli. The patient's discomfort had progressively worsened, limiting her ability to eat and speak comfortably.
Upon further investigation, the patient stated that he had noticed occasional swelling and the presence of a sinus tract near the affected teeth in the previous few weeks. There was no history of fever or underlying illness. The patient had not taken any pain relievers before coming to the clinic.
The patient described a dental trauma that occurred approximately two years ago, resulting in an injury to the maxillary central incisors (teeth #11 and #21). There was no immediate treatment sought, and the teeth remained asymptomatic until two months ago, when pain began.
No family history.
Clinical examination revealed an Ellis class IV fracture of the permanent maxillary right and left central incisor, i.e., 11, 21, which was accompanied by a sinus tract near the root apex. The teeth did not respond to electric or thermal pulp sensibility tests.
None.
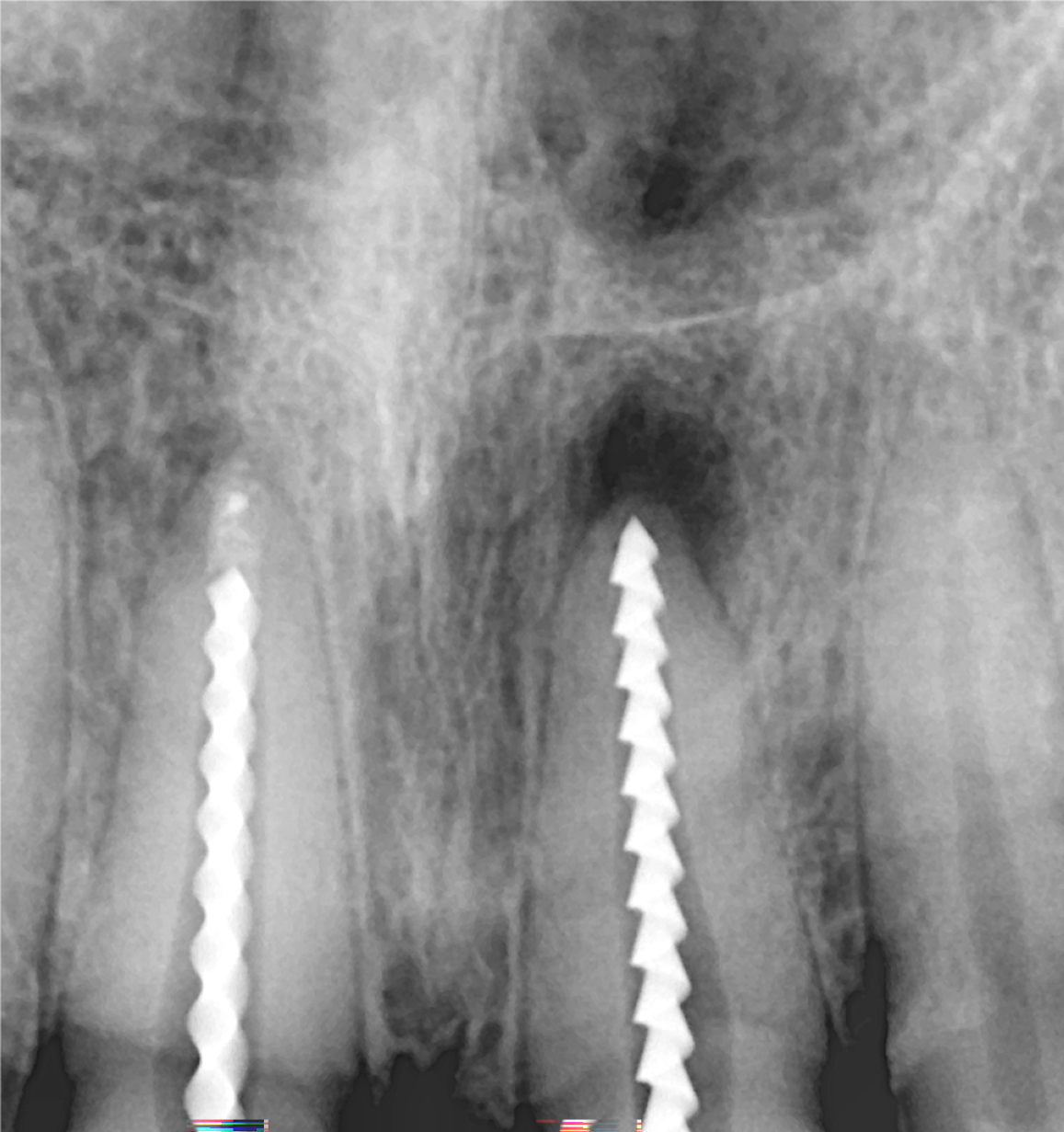
A radiographic examination revealed a blunderbuss canal and a periapical lesion for both teeth.
Based on these findings, a periapical abscess wrt 11 and 21 was diagnosed.
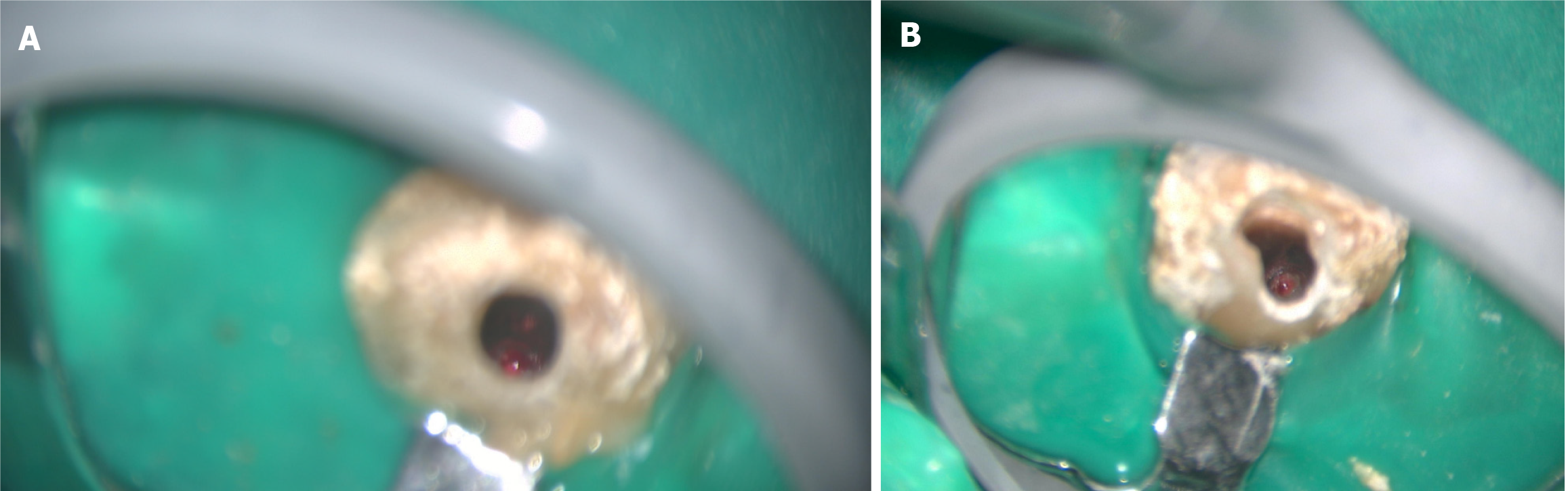
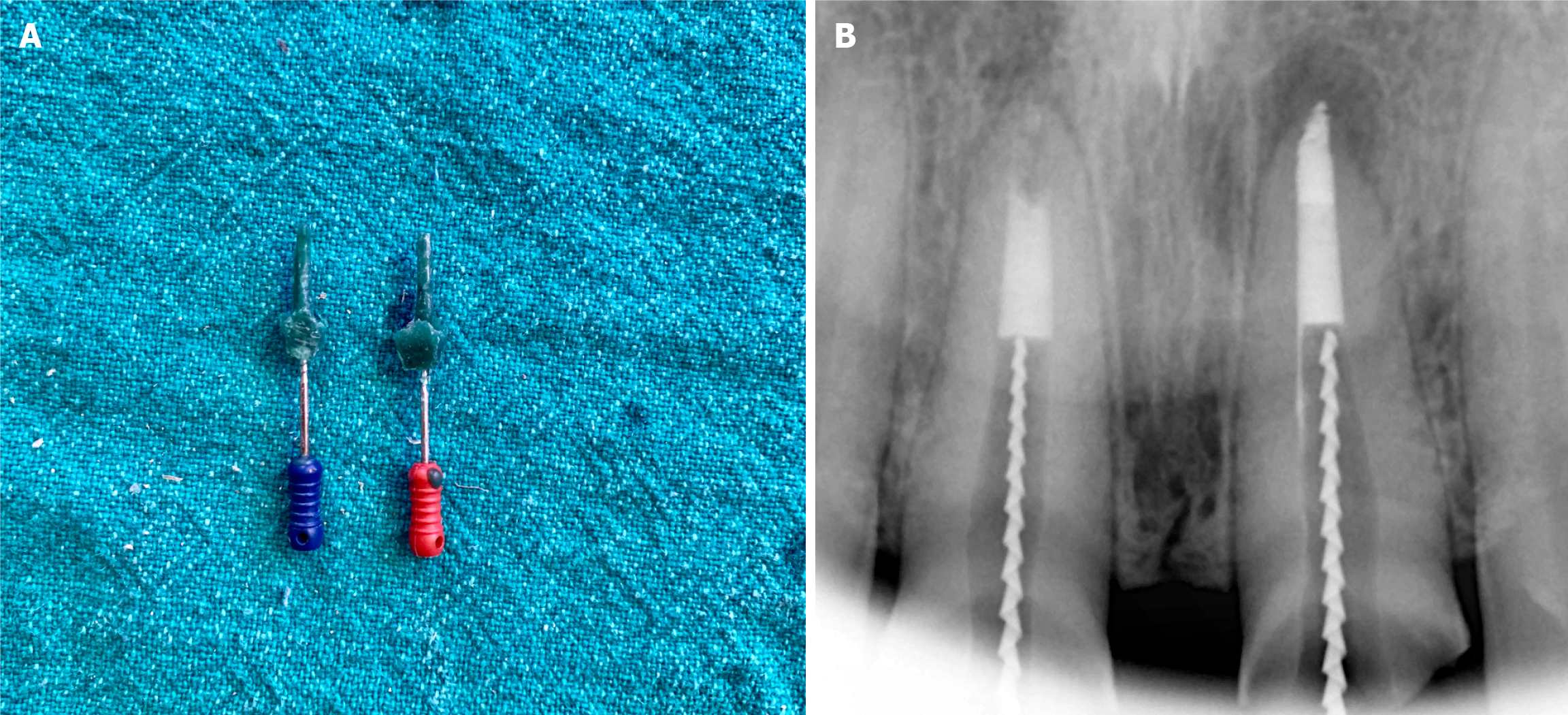
Following a discussion of various treatment options, it was decided to proceed with apexification using MTA wrt 11 and 21 under magnification, followed by cast post and zirconia crowns wrt 11 and 21. Rubber dam isolation was done on 11 and 21, and an access cavity was created on both teeth (Figure 1). A #80H file (Mani, Prime Dental Product Pvt. Ltd., India) (Figure 2) was used to determine the working length, while JIZAI (Mani, Prime Dental Product Pvt. Ltd., India) rotary files were used for canal instrumentation. The canal was then thoroughly cleaned with mechanical instruments and extensively irrigated with 2.5% sodium hypochlorite (NaOCl) (Bharat Chemical, India) administered through a 30 G double-sided vented needle (Master Clean, Amplemeds, India). Internal heating at 180 degrees Celsius for 5 seconds and ultrasonic activation was done to improve canal disinfection.
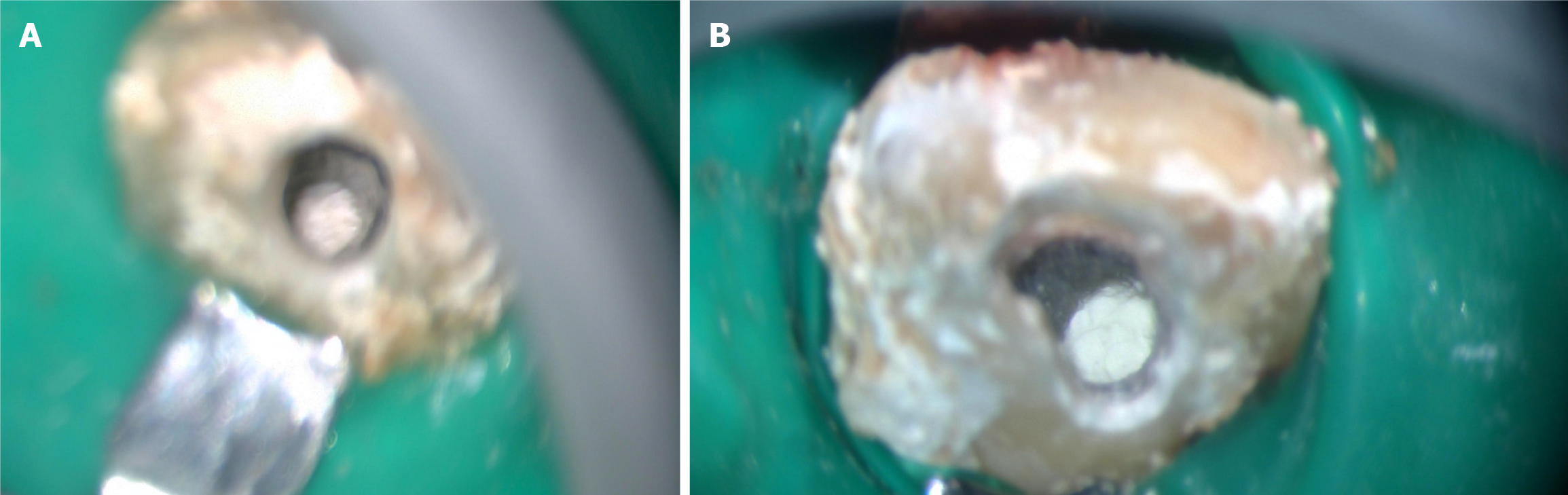
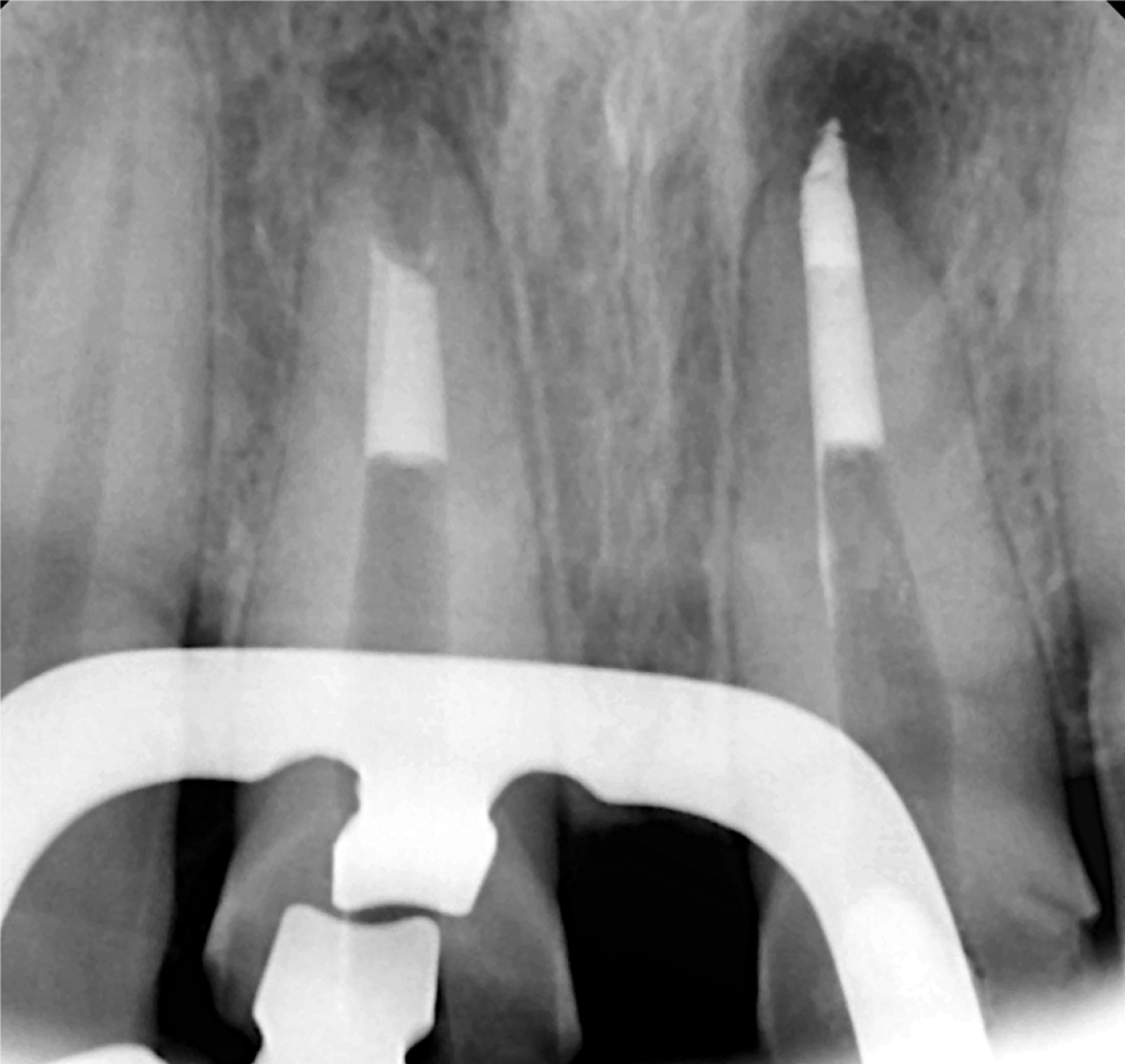
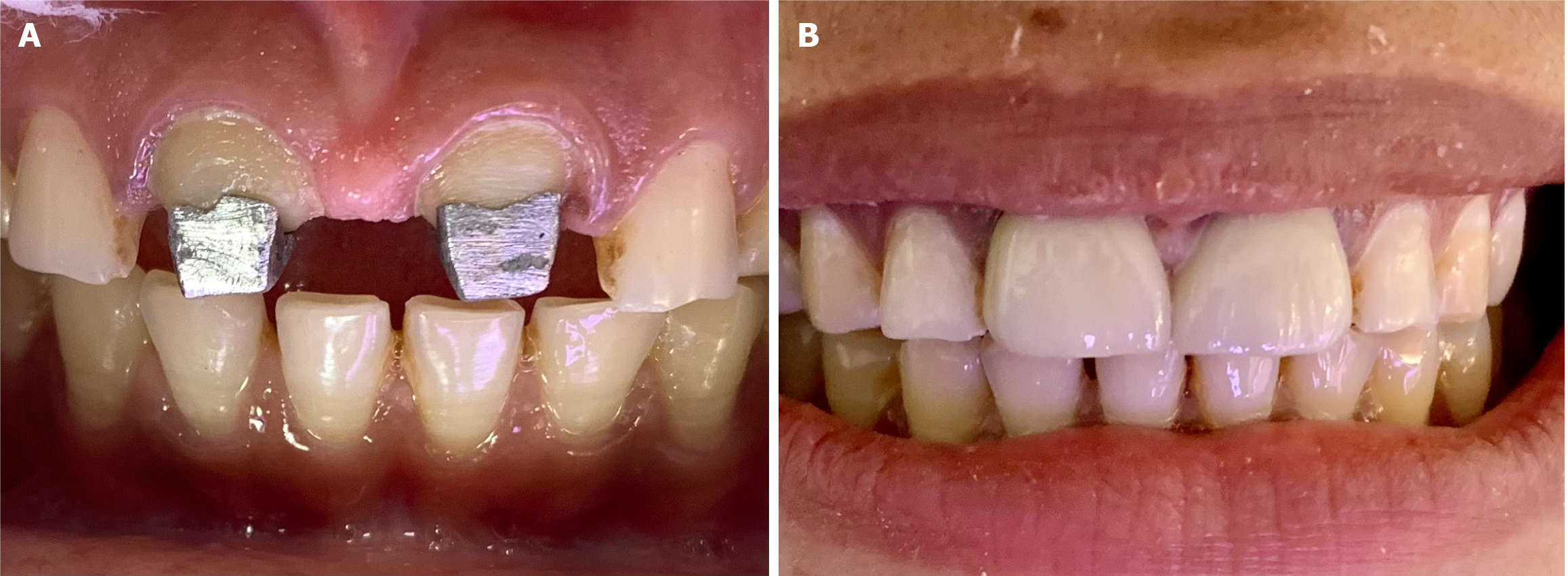
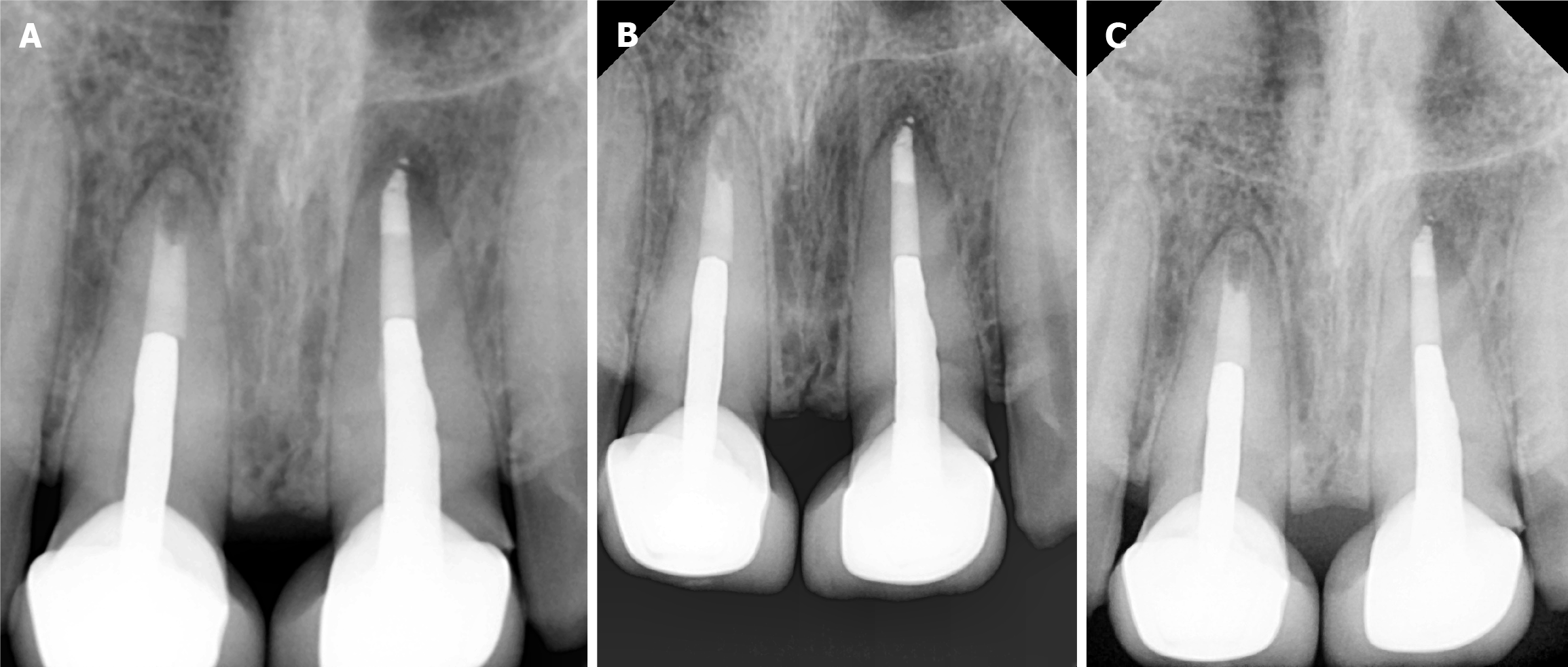
The canal was irrigated again with NaOCl (Bharat Chemical, India), followed by 17% EDTA to remove the smear layer. To control bleeding, a collagen sponge (Hemospon; Technew, Rio de Janeiro, Brazil) was placed in the apical third of the canal, and MTA (BioStructure, SafeEndo, India) was placed (Figure 3) incrementally using the micro-apical placement (MAP) system (Produits Dentaires SA, Vevey, Switzerland) under magnification. Each increment of MTA was condensed using a paper point (Diadent, Chungju, Korea) and a pre-fitted plugger (Meta Biomed, Chungcheongbuk-do, Korea) to form a 5 mm apical plug. Radiographs were taken to confirm MTA's precise placement at the apex (Figure 4)
After the initial set, moist cotton was placed over the MTA plug, and the patient was recalled after 24 hours. The cast post impressions were made (Figure 5) with the help of wax wrt 11 and 21. Then, after 1 week, the cast posts were cemented, a radiograph was taken (Figure 6), and crown preparations were done wrt 11 and 21, followed by crown cementation after 1 week (Figure 7).
At follow-up visits, the patient remained asymptomatic, and radiographs at 3, 6, and 12 months (Figure 8) revealed significant healing of the periapical lesion.
Apexification in immature teeth with open apices is a technically challenging procedure due to the lack of a natural apical barrier, irregular root canal anatomy, and high risk of microbial invasion[10]. This case demonstrates the use of advanced materials, precise irrigation protocols, magnification, and delivery systems, such as the MAP system, to achieve a predictable and successful clinical result[11].
MTA remains the primary apexification material, providing biocompatibility, superior sealing properties, and the ability to induce hard tissue formation. Its application in this case resulted in a strong apical barrier, which prevented reinfection and promoted periapical healing[12]. In addition to MTA, the use of a bioceramic sealer improved the seal and ensured the canal system's hermetic seal. Bioceramic sealers are well-known for their excellent adhesion, dentin bonding ability, and bioactivity, all of which contribute to long-term success by preventing microleakage and encouraging tissue regeneration[13].
Apexification relies heavily on apical seal and efficient irrigation systems. NaOCl, the gold standard irrigant, was used because of its ability to dissolve necrotic tissue while also eliminating microbial biofilms[14]. In this case, activation and internal heating of NaOCl at 180 degrees Celsius for 5 seconds under magnification increased its efficacy, allowing for thorough disinfection of the canal system, especially in the intricate apical anatomy[15]. The use of double-sided vented irrigation needles improved irrigant distribution and penetration, resulting in thorough cleaning while lowering the risk of extrusion. The combination of NaOCl, advanced irrigation techniques, and magnification ensured that all inaccessible areas were adequately debrided, resulting in an ideal environment for healing[16].
Magnification was essential throughout the procedure, allowing the clinician to see the intricate details of the canal system and apical defect. The DOM enabled the precise removal of necrotic tissue, accurate assessment of the defect, and meticulous placement of MTA[17]. The MAP system helped to deliver MTA incrementally and without voids, ensuring precise adaptation to the desired area. This method reduced procedural errors and improved the stability of the apical barrier[18].
The use of advanced materials and technologies (MTA, bioceramic sealer, NaOCl with internal heating activation, double-sided vented needles, magnification, and the MAP system) demonstrates a modern, comprehensive approach to apexification. This case demonstrates how these innovations address the challenges of managing open apices while also improving procedural efficiency and clinical outcomes, paving the way for predictable and patient-centered endodontic care[19].
This case demonstrates the effectiveness of integrating advanced materials, precise irrigation protocols, and magnification in the apexification of immature teeth with open apices. The use of MTA created a stable apical barrier, while bioceramic sealers enhanced the seal and promoted long-term healing. NaOCl with internal heating, ultrasonic activation, and double-sided vented needles ensured thorough irrigation and disinfection, especially in complex canal anatomy. Magnification tools, particularly the DOM, allowed for precise visualization, careful tissue removal, and accurate placement of MTA. The MAP system facilitated void-free delivery of MTA, optimizing treatment outcomes.
Overall, combining these technologies has revolutionized apexification, improving procedural efficiency and clinical success. The use of these advanced techniques reduces the risk of iatrogenic errors, enhances material adaptation, and ensures long-term tooth preservation. This case emphasizes the importance of a modern, comprehensive approach to apexification in achieving predictable and successful results.
| 1. | Chotvorrarak K, Danwittayakorn S, Banomyong D, Suksaphar W. Intraradicular reinforcement of traumatized immature anterior teeth after MTA apexification. Dent Traumatol. 2024;40:389-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 5.5] [Reference Citation Analysis (1)] |
| 2. | Kasimoglu Y, Koyuncuoglu G, Bayrak S, Ugur-Aydin Z, Aren G. Evaluation of the Effects of MTA Apexification and Regenerative Endodontic Therapy on Lesion Healing using Fractal Analysis: A Retrospective Study. Eur J Paediatr Dent. 2024;1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (1)] |
| 3. | Wikström A, Brundin M, Mohmud A, Anderson M, Tsilingaridis G. Outcomes of apexification in immature traumatised necrotic teeth and risk factors for premature tooth loss: A 20-year longitudinal study. Dent Traumatol. 2024;40:658-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Naved N, Umer F, Khowaja AR. Cost-Effectiveness Analysis of Regenerative Endodontics versus MTA Apexification. JDR Clin Trans Res. 2024;9:231-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Bhasin P, Saraf BG, Chauhan S, Kumar H, Wahi P, Vats V. The Successful Interdisciplinary Outcome of Blunderbuss Canal with an Open Apex Using MTA under Magnification: A Case Report. Int J Clin Pediatr Dent. 2024;17:97-101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (2)] |
| 6. | Anjum FS, Brusevold IJ, Wigen TI. Prognosis of non-vital incisors after apexification using bioceramics: a retrospective study. Eur Arch Paediatr Dent. 2024;25:637-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 7. | Wigler R, Kaufman AY, Lin S, Steinbock N, Hazan-Molina H, Torneck CD. Revascularization: a treatment for permanent teeth with necrotic pulp and incomplete root development. J Endod. 2013;39:319-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 166] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 8. | Sharma V, Sharma S, Dudeja P, Grover S. Endodontic management of nonvital permanent teeth having immature roots with one step apexification, using mineral trioxide aggregate apical plug and autogenous platelet-rich fibrin membrane as an internal matrix: Case series. Contemp Clin Dent. 2016;7:67-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Bhasin P, Vats V, Chauhan S, Tandon M, Kumar H, Chugh R. Magnifiers, ultrasound, and bioceramics-an ideal trio for archival retrieval: a case report. J Bull Stomatol Мaxillofac Surg. 2023;19:9-13. [RCA] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 10. | Fathima A, Ravindran V, Jeevanandan G, Mohanraj KG, Eswaramoorthy R, Arthanari A. Histologic Assessment of a Fast-Set Mineral Trioxide Aggregate (MTA) and Two Novel Antibacterial-Enhanced Fast-Set MTAs for Apexification and Periapical Healing of Teeth With Incomplete Root Formation in a Rat Model: An In Vivo Animal Study. Cureus. 2024;16:e59064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 11. | Acharya S, Sahoo D, Singh B, Gurunathan D. Revascularization Revisited with Modified Triple Antibiotic Paste and NeoPutty MTA®. J Pharm Bioallied Sci. 2024;16:S1871-S1874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 12. | Sinha Y, Agarwal T, Chatterjee I, Pradhan P. Revitalizing the Smile: A Case Report on the Modified Apexification Procedure for Discolored Non-Vital Immature Teeth With Periapical Lesions. Cureus. 2024;16:e71140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 13. | Chauhan S, Chauhan R, Bhasin P, Sharaf BG. Present status and future directions: Apexification. World J Methodol. 2025;15:96923. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (10)] |
| 14. | Chauhan S, Chauhan R, Bhasin P, Bhasin M. Magnification: The game changer in dentistry. World J Methodol. 2025;15:100937. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (37)] |
| 15. | Kaur M, Singh H, Dhillon JS, Batra M, Saini M. MTA versus Biodentine: Review of Literature with a Comparative Analysis. J Clin Diagn Res. 2017;11:ZG01-ZG05. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 92] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 16. | Yalin FA, Tabibi M, Majidi A, Kabiri F, Rasouli A, Aghaali M. Evaluation and comparison of four types of bio-ceramic materials AGM MTA, Ortho MTA, pro root MTA and Cem cement in oral and dental health. BMC Oral Health. 2024;24:1052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 17. | Camilleri J, Pitt Ford TR. Mineral trioxide aggregate: a review of the constituents and biological properties of the material. Int Endod J. 2006;39:747-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 259] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 18. | Simon S, Rilliard F, Berdal A, Machtou P. The use of mineral trioxide aggregate in one-visit apexification treatment: a prospective study. Int Endod J. 2007;40:186-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 149] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 19. | Rafter M, Baker M, Alves M, Daniel J, Remeikis N. Evaluation of healing with use of an internal matrix to repair furcation perforations. Int Endod J. 2002;35:775-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/