Published online Jun 20, 2024. doi: 10.5662/wjm.v14.i2.89809
Peer-review started: November 13, 2023
First decision: January 25, 2024
Revised: January 31, 2024
Accepted: March 19, 2024
Article in press: March 19, 2024
Published online: June 20, 2024
Processing time: 213 Days and 16.9 Hours
Total patellectomy is currently reserved for exceptional cases, such as recalcitrant patellofemoral instability and comminuted fractures, due to its demonstrated negative impact on knee biomechanics. Therefore, managing patellectomy is crucial to mitigate its inherent deleterious effects. Various techniques have been described, including autologous or allogeneic bone grafts for reconstruction and soft tissue realignment to enhance the extensor mechanism.
A 73-year-old male underwent a patellectomy due to a comminuted fracture, subsequently developing osteoarthritis and experiencing a decline in functional status. Concurrent with total knee replacement, we conducted a patellar reconstruction, incorporating routine bone cuts and utilizing bone chips to fashion a new patella. This intervention resulted in the restoration of full extension and improvement of knee function.
Patellar reconstruction demonstrates benefits on knee mechanics and stabilization, contributing to enhanced outcomes and satisfaction following knee replacement. We present an affordable technique for managing patellectomized patients undergoing total knee replacement.
Core Tip: Patients who have undergone patellectomy tend to experience worse outcomes following total knee arthroplasty than those with an intact patella. We present a 73-year-old male who, after a left patellectomy due to a comminuted fracture, developed osteoarthritis leading to detriment knee function. We reconstructed the patella using bone chips from routine bone cuts during the total knee arthroplasty. Post-surgery, the patient reported improved knee function and satisfaction. The key takeaway is that patellar reconstruction enhances knee function mainly due to its mechanical advantages, leading to better outcomes. The technique performed is safe and feasible.
- Citation: Perez-Abdala JI, De Cicco FL, Nicolino T, Astoul J. Patellar reconstruction in primary total knee arthroplasty using bone chips from routine cuts: A case report and review of literature. World J Methodol 2024; 14(2): 89809
- URL: https://www.wjgnet.com/2222-0682/full/v14/i2/89809.htm
- DOI: https://dx.doi.org/10.5662/wjm.v14.i2.89809
Total patellectomy was a prevalent procedure in past decades, primarily employed to address conditions such as chondromalacia, patellofemoral arthritis, patellofemoral dislocation, and comminuted fractures[1-5]. In contemporary times, an enhanced understanding of the patella's role in biomechanical knee function, coupled with advancements in surgical techniques, has relegated this radical surgery to a salvage option[6]. Nonetheless, patients with patellectomy sequelae persist or when there is no alternative to avoid patellectomy, as is the case with malignant tumors. Concerning the mechanical properties of the patella, numerous studies have demonstrated that its absence can lead to a decrease in tibial torque force by up to 30%, resulting in a reduction of the lever arm between the quadriceps tendon and the center of rotation, causing an extension deficit[1,7,8]. Additionally, the femorotibial reaction force amplifies the tangential force, potentially contributing to osteoarthritis development[9]. Other adverse effects include quadriceps muscle wasting, loss of joint protection, an unfavorable aesthetic appearance, and instability of the remaining tendon, which may lead to degeneration and, ultimately, rupture[2,10-13]. Decades ago, the theory of the four-bar linkage system was introduced, depicting the patella as a stabilizer in the sagittal plane, limiting anterior femoral displacement during knee flexion. However, contemporary perspectives cast doubt on the full acceptance of this role of the patella[10-15].
The literature supports that patients without patella requiring total knee arthroplasty (TKA) report poorer overall outcomes compared to those with an intact patella, encompassing factors such as range of motion, knee function, patient satisfaction, and complication rates[14-20]. Given these considerations, surgeons must evaluate how to reconstruct the patella, considering the need to preserve biomechanical properties. Patellar reconstruction might be performed using various methods, including autologous bone grafts, allogeneic extensor or bone grafts, and, less commonly, metal augmentations[6,10,21-29]. Additionally, alternative techniques involving soft tissue have been described[30]. However, the existing literature is characterized by scarce evidence and heterogeneous samples, preventing the establishment of reliable recommendations regarding the optimal approach. In this context, our goal is to introduce an alternative technique for patellar reconstruction in patellectomized patients while simultaneously performing a TKA.
A 73-year-old male patient presented at the hospital with severe knee pain and difficulty ambulating.
The patient underwent a total patellectomy of his left knee for a comminuted fracture sixty years ago, which led to the development of osteoarthritis with valgus deformity. The patient required a walker to ambulate and experienced high levels of pain, rated at 9/10 on the visual analogue scale (VAS) in activity, which resulted in daily opioid consumption.
The patient underwent a total patellectomy of his left knee for a comminuted fracture sixty years ago. Moreover, he was developing pain, subjective knee instability, and lesser strength than another knee.
He denies any personal or family disease that could be significant for the pathology and outcomes.
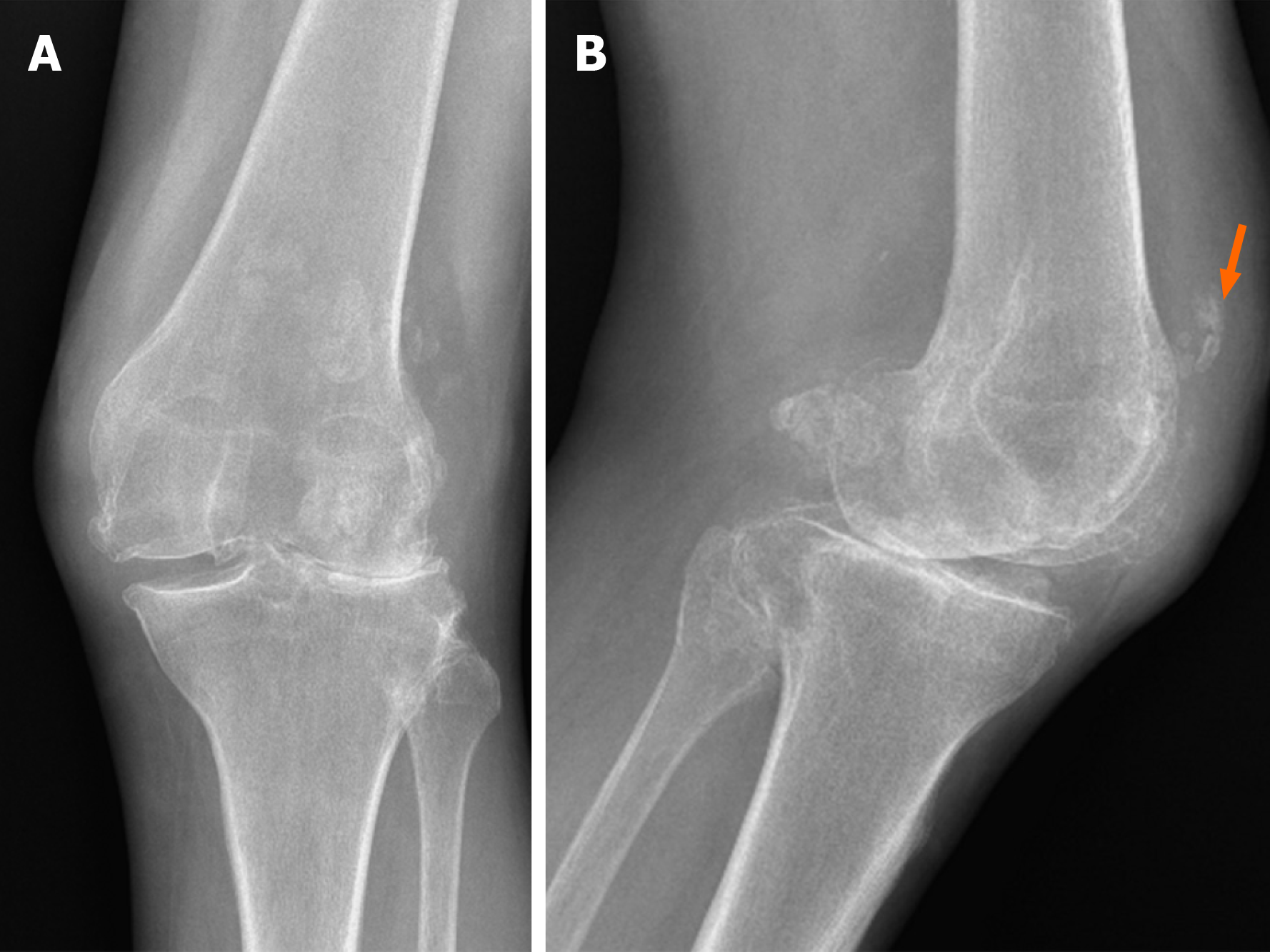
On physical examination, the patient had 10° of deficit active extension and flexion greater than 120°. Despite coronal misalignment, as shown in Figure 1, the medial collateral ligament was competent in varus-valgus stress examination with a firm endpoint. The Knee Society Score (KSS) was 29 points for the knee and 45 points for function, and the strength was 3/5 according to the Medical Research Council (MRC) scale[31].
His laboratory testing was within normal parameters.
X-rays showed severe femorotibial osteoarthritis, valgus misalignment, absence of the patella, and areas of tendon calcification (Figure 2). Following a thorough discussion of potential treatment options with the patient, we proposed a TKA with patellar reconstruction, to which the patient willingly consented.
Left knee osteoarthritis with sequelae of patellectomy.
We performed a standard medial para-patellar approach, exposing the femur and tibia and making cuts using intra and extra-medullary jigs, respectively. Subsequently, achieving balance in all ranges of motion and successfully restoring the mechanical axis. A cemented semi-constrained implant with a long tibial stem was then used.
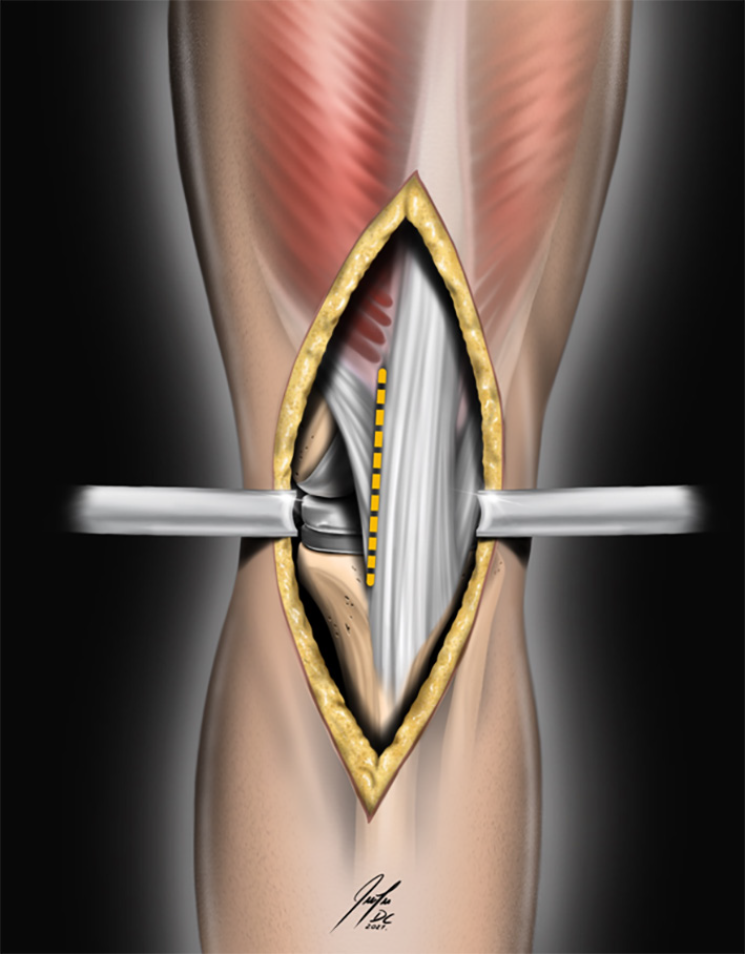
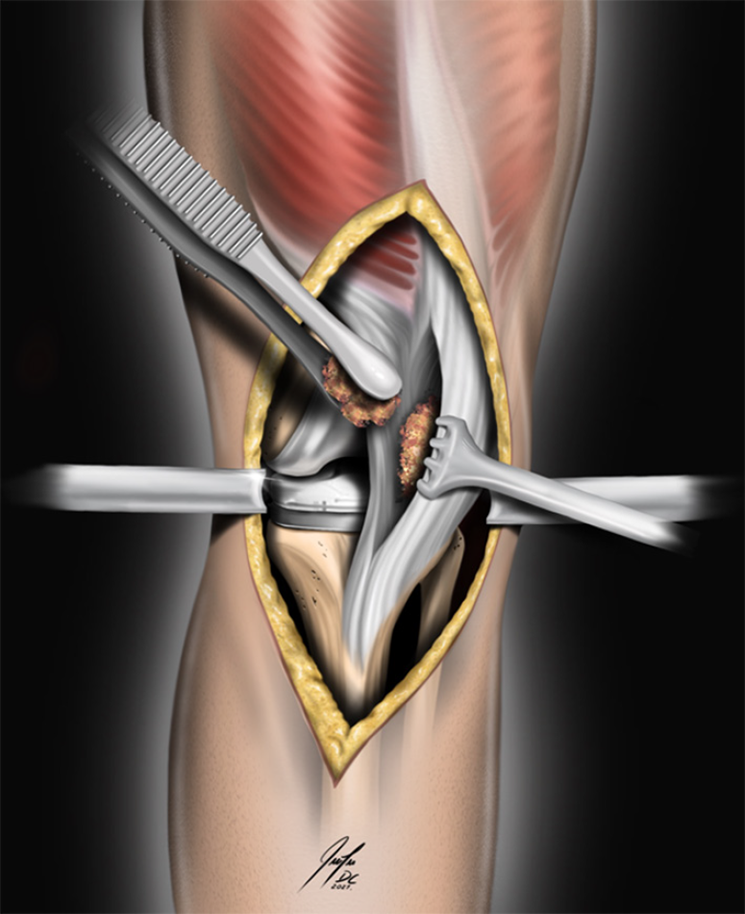
Proceeding to the patellar reconstruction, we morselized the remaining bone from the tibia and femur cuttings with a rongeur, obtaining cortico-cancellous chips. To determine the accurate positioning and size of the neo-patella, we measured the dimensions of the contralateral patella beforehand, trying to replicate the Insall-Salvati ratio[32]. Notably, the patellar tendon was hypertrophy, measuring approximately 2 cm in thickness. Addressing this, we made a 5 cm longitudinal incision on the medial aspect of the tendon, creating an intra-tendon pocket while leaving a 7 cm remnant of the patellar tendon (Figure 3). The amount of bone chips used varied; however, the objective was to reconstruct a neo-patella that would reposition the extensor apparatus away from the knee's center of rotation, mirroring a healthy knee. The pocket was filled with bone chips using a press-fit technique. Before closing the tendon pocket, we conducted tests to ensure correct patellar tracking and to verify the absence of excessive pressure or instability in the extensor mechanism. Finally, we closed the pocket using strong non-absorbable sutures, specifically Ti-Cron™ #0 (Figure 4). Immediate postoperative x-rays, primarily in the lateral view, revealed the neo-patella positioned slightly high, measuring 5 cm in length and 1.5 cm in thickness (Figure 5).
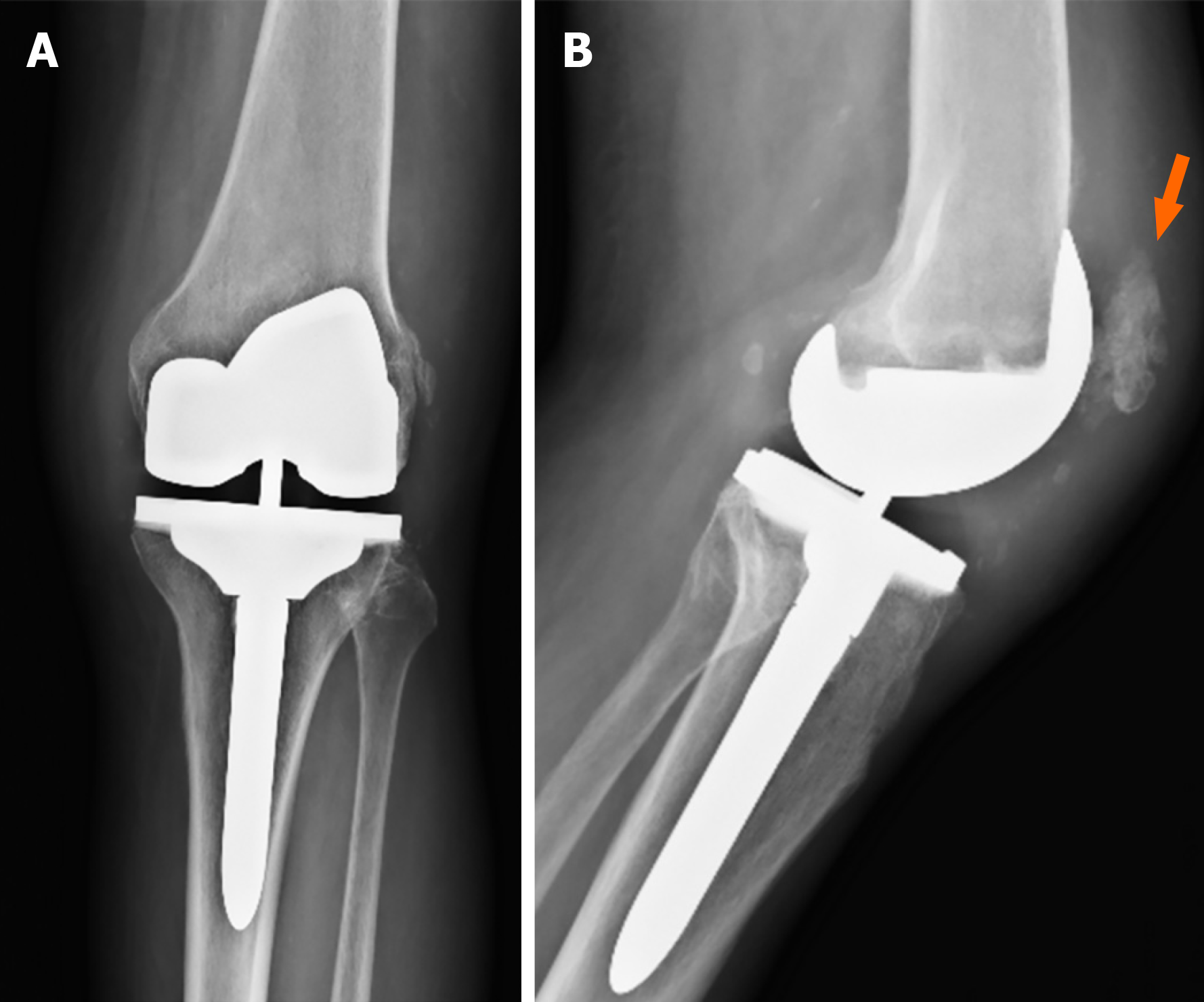
The standardized rehabilitation protocol was initiated on the first day postoperative, incorporating passive and active mobility exercises, quadriceps isometric exercises, and progressive weight-bearing using a walker, as tolerated by the patient. He used a walker for the initial fifteen days, then a cane until definitively discontinuing walker support at the two-month postoperative mark, achieving a stable and pain-free gait. By five months postoperative, he reached full active extension (0° to 115°) and 5/5 muscle strength according to the MRC scale. At the last follow-up, two years after the surgery, he preserved full extension and quadriceps strength (Figure 6). The KSS improved to 68 points for knee and 80 points for function, and the VAS decreased to 2/10. Also, the patient reported complete satisfaction with the procedure. Upon the two-year follow-up, radiographs demonstrated an improved shape of the neo-patella, with no signs of bone resorption. The lateral image revealed a persistent increased Insall-Salvati ratio of 1.6, although the patient denied any symptoms related to patellar stability (Figure 7).
We are presenting a case involving patellar reconstruction in a patient with a history of patellectomy who developed knee osteoarthritis and experienced impaired knee function. Although the specific contribution of a missing patella to the development of osteoarthritis may be a subject of debate, it is well-documented that its absence can substantially affect the function of the extensor mechanism[7-13]. Following the simultaneous performance of total knee arthroplasty and patellar reconstruction, the patient exhibited enhanced knee function, particularly emphasizing the restoration of the extensor mechanism[1,2,11,33].
Several studies have consistently demonstrated that, in patellectomized patients, the clinical and functional outcomes after TKA are lower than those in patients with an intact patella[14,16-19]. In a study by Haque et al[20] two groups were followed for an average of 9.5 years: one comprised patellectomized patients, and the other had patients with an intact patella. Most cases were managed with TKA, utilizing either posterior-stabilized (PS) or cruciate-retaining (CR) designs based on the surgeon's discretion[20]. The study demonstrated lower survivorship free from revision in the group without a patella (82%) compared to the group with an intact patella (94%). Additionally, the patellectomized group had a higher rate of complications, mainly attributed to infections and instability. The increased instability in the patellectomized group was attributed to quadriceps weakness due to the absence of the patella. The concept of four-bar linkage system can explain this fact, where the patella could serve as a stabilizer in the sagittal plane, limiting anterior femoral displacement during knee flexion. Moreover, the absence of patellar bone anteriorly, coupled with soft tissue laxity or instability, may lead to significant soft tissue effusions. In turn, this can contribute to challenges in wound healing and an increased risk of infection[20]. Considering these outcomes, the authors suggest patellar reconstruction procedures as a viable alternative for patients with a history of patellectomy.
An area of debate for individuals who have undergone patellectomy revolves around the choice of implant. We opt for a semi-constrained design due to the perceived intra-operative stability, evident in both sagittal and coronal planes, surpassing that of the PS design. Some authors, like Paletta et al[15], advocate for PS designs, reporting improved functional and clinical scores with this choice[15,34]. These findings align with the earlier-discussed four-bar linkage system. However, Haque et al[20] observed similar complication and revision risks with both CR and PS designs, acknowledging a potential bias in design selection, particularly in cases with preoperative quadriceps weakness and consistent instability where PS was preferred for added sagittal stability. Other reports, such as the meta-analysis by Asadollahi et al[19], have indicated similar outcomes between these designs[17-19]. Nonetheless, the latter study suggests that PS designs may provide enhanced sagittal stability for patellectomized patients lacking a competent posterior cruciate ligament. Additionally, unicompartmental replacements, though limited to case reports, have shown favorable short-term functional and clinical scores[35,36]. However, we assert that the choice of implant design should primarily be guided by stability testing in both the preoperative and intraoperative phases, with particular attention to cases involving patellar reconstruction, as it can contribute to increased stability. Several techniques for patellar reconstruction have been described, encompassing autograft bone, allograft extensor mechanisms, prosthetic augments, and soft tissue reconstruction (Table 1).
| Ref. | Type of patellar reconstruction | Number of patients | Follow-up | Outcomes | Complications |
| Buechel[26], 1991 | Bone auto and allograft - iliac crest, femoral resection and bone bank | 6 (7 knees) | 24 to 125 months | Full ROM, strengthening, pain free gait and no signs of graft resorption | 1 CRPS |
| Kulkarni et al[28], 1999 | Extensor mechanism allograft | 1 | 3 yr | Improve ROM, strength, level of pain and no signs of graft resorption | None |
| Tirveilliot et al[25], 2003 | Bone auto and allograft - 6 tibial plateau / 1 fragment of femoral head | 7 | 1.5 months to 6 yr | IKS pre/postoperative; Knee: 41/78; Function: 35/72 | 4 were removed for migration |
| Lakshmanan and Wilson[10], 2004 | Bone autograft - entire tibial plateau | 1 | 9 months | KSS postoperative; Knee: 90; Function: 92 | None |
| Busfield and Ries[27], 2006 | Extensor mechanism allograft | 7 (9 knees) | 39 to 48 months | KSS pre/postoperative; Knee: 59/85; Function: 63/67 | 2 infections 1 patellar resorption |
| Kwong and Desai[29], 2008 | Prosthetic augment | 7 | 6 to 21 months | Initial recovery was good, complications emerged over time | 3 loosening 2 continuing pain |
| Pang and Sathappan[23], 2008 | Bone autograft - distal medial femoral condyle | 1 | 2 yr | Full ROM, strengthening, pain free gait and no signs of graft resorption | None |
| Jabbar and Ruiz[22], 2009 | Bone autograft - posterior lateral femoral condyle | 1 | 4 yr | Full ROM, strengthening, pain free gait and no signs of graft resorption | None |
| Daentzer et al[24], 2012 | Bone autograft - iliac crest | 13 | 3 to 92 months | KSS postoperative; Knee 67.3; Function 57.5 | 3 infections (one removed patella); 1 patellar instability; 1 fracture of ASISe |
| George et al[21], 2017 | Bone autograft - medial femoral condyle | 2 | 1.5 to 4 yr | Full ROM, strengthening, pain free gait and no signs of graft resorption | None |
| Giessler and Hendrich[37], 2016 | Hybrid - vascularized bone graft with metal augmentation | 1 | 6 months | Full ROM, strengthening, pain free gait and no signs of graft resorption | None |
| Gómez-Palomo et al[6], 2019 | Extensor mechanism allograft | 1 | 5 yr | Full ROM, strengthening and pain free gait | None |
Autograft bone can be harvested from the medial femoral condyle or tibial plateau through distal cutting[21,23-25]. While both techniques are generally reliable, our case presented challenges due to the size due to the size of the medial femoral condyle, particularly in cases of severe valgus knee osteoarthritis. It's worth noting that reinforcing sutures is crucial to prevent neo-patella migration, as emphasized by the authors. Alternatively, the iliac crest bone can be utilized, yielding satisfactory results in select patients[24,26]. However, it is being acknowledged that morbidity at the harvest site and complications are not uncommon[24]. Additionally, immediate aggressive rehabilitation is strongly recommended for achieving optimal outcomes[23-26].
Allogeneic extensor grafts remain an irreplaceable option in patients with tumor pathology[6]. Nonetheless, there is a growing concern regarding the heightened risk of infection, prompting surgeons to approach this technique with extreme care[27,28]. More recently, tantalum augmentation has been proposed as an alternative for these patients, yet its inferior outcomes and high revision rates dissuade its widespread adoption[29]. Moreover, a patellar reconstruction employing a hybrid technique has been described, integrating prosthetic augmentation with a vascularized bone graft harvested from the scapula, resulting in successful outcomes[37]. Soft tissue reconstruction emerges as a viable option, aiming to restore patellar function, with most reconstructions focusing on advancing the vastus medialis oblique[12,30].
While the precise contribution of patellar reconstruction to enhanced knee function remains elusive, the literature cited indirectly supports our favorable clinical and functional outcomes following its implementation. We attribute our success to the meticulous placement of the fragmented autograft bone in a press-fit manner within the intra-tendon pocket, facilitating optimal patellar tracking, and securing closure with strong sutures to prevent graft migration. Despite the potentially compromised vascularity of the extensor mechanism due to prior surgeries, our patellar reconstructions have maintained bone integrity on radiographs two years post-operation, showing no signs of resorption[21,37]. Though the long-term viability of the bone graft remains uncertain, our hypothesis asserts that maintaining the occupied space through patella reconstruction, whether by original bone or fibrous tissue replacement, may suffice to preserve the mechanical integrity of the patella and yield satisfactory outcomes. Additionally, rigorous postoperative rehabilitation under the guidance of an experienced physiotherapist is imperative. This technique offers several advantages, including a low complication rate, cost-effectiveness, technical reproducibility, and adherence to biomechanical principles. However, limitations may arise from the thin and poor-quality tendon of the extensor mechanism, posing a rupture risk if a pocket is attempted. Therefore, despite encouraging outcomes observed in just one case, further research is imperative to ascertain the efficacy and safety of this technique in a larger prospective cohort.
A patellar reconstruction is a viable option for patellectomized patients with clinical impairment. It restores the knee biomechanics and enhances outcomes for patients undergoing primary or revision total knee arthroplasty TKA. Our technique is novel and reproducible without adding morbidity and cost to surgery; therefore, it would be a therapeutic alternative for patellectomized patients.
| 1. | Steurer PA Jr, Gradisar IA Jr, Hoyt WA Jr, Chu M. Patellectomy: a clinical study and biomechanical evaluation. Clin Orthop Relat Res. 1979;84-90. [PubMed] |
| 2. | Günal I, Karatosun V. Patellectomy: an overview with reconstructive procedures. Clin Orthop Relat Res. 2001:74-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Belal MA, Ochsner PE. [Indications and contraindications for patellectomy]. Z Orthop Ihre Grenzgeb. 1986;124:266-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Kelly MA, Brittis DA. Patellectomy. Orthop Clin North Am. 1992;23:657-663. [PubMed] |
| 5. | Asopa V, Willis-Owen C, Keene G. Patellectomy for osteoarthritis: a new tension preserving surgical technique to reconstruct the extensor mechanism with retrospective review of long-term follow-up. J Orthop Surg Res. 2015;10:107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Gómez-Palomo JM, Jiménez-Garrido C, Martínez-Crespo A, García-Vera JJ, Pérez-Cardeña J, Montañez-Heredia E. Extensor Mechanism Allograft in Osteosarcoma of the Patella: A Case Report. JBJS Case Connect. 2019;9:e0277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 7. | Peeples RE, Margo MK. Function after patellectomy. Clin Orthop Relat Res. 1978;180-186. [PubMed] |
| 8. | Kaufer H. Mechanical function of the patella. J Bone Joint Surg Am. 1971;53:1551-1560. [PubMed] |
| 9. | Denham RA, Bishop RE. Mechanics of the knee and problems in reconstructive surgery. J Bone Joint Surg Br. 1978;60-B:345-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 41] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Lakshmanan P, Wilson C. Total knee arthroplasty in a patellectomised posterior cruciate ligament-deficient knee: a new technique of patellar tendon bone grafting. Knee. 2004;11:481-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Lennox IA, Cobb AG, Knowles J, Bentley G. Knee function after patellectomy. A 12- to 48-year follow-up. J Bone Joint Surg Br. 1994;76:485-487. [PubMed] |
| 12. | Günal I, Taymaz A, Köse N, Göktürk E, Seber S. Patellectomy with vastus medialis obliquus advancement for comminuted patellar fractures: a prospective randomised trial. J Bone Joint Surg Br. 1997;79:13-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Sutton FS Jr, Thompson CH, Lipke J, Kettelkamp DB. The effect of patellectomy on knee function. J Bone Joint Surg Am. 1976;58:537-540. [PubMed] |
| 14. | Joshi AB, Lee CM, Markovic L, Murphy JC, Hardinge K. Total knee arthroplasty after patellectomy. J Bone Joint Surg Br. 1994;76:926-929. [PubMed] |
| 15. | Paletta GA Jr, Laskin RS. Total knee arthroplasty after a previous patellectomy. J Bone Joint Surg Am. 1995;77:1708-1712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 43] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Kang JD, Papas SN, Rubash HE, McClain EJ Jr. Total knee arthroplasty in patellectomized patients. J Arthroplasty. 1993;8:489-501. [PubMed] |
| 17. | Reinhardt KR, Huffaker SJ, Thornhill TS, Scott RD. Cruciate-retaining TKA is an option in patients with prior patellectomy. Clin Orthop Relat Res. 2015;473:111-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Martin SD, Haas SB, Insall JN. Primary total knee arthroplasty after patellectomy. J Bone Joint Surg Am. 1995;77:1323-1330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 31] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Asadollahi S, Sorial R, Coffey S, Gupta M, Eslick GD. Total knee arthroplasty after patellectomy: A meta-analysis of case-control studies. Knee. 2017;24:191-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Haque OJ, Maradit Kremers H, Kremers WK, Berry DJ, Lewallen DG, Trousdale RT, Sierra RJ. Increased Risk of Postoperative Complications After Total Knee Arthroplasty in Patients With Previous Patellectomy. J Arthroplasty. 2016;31:2278-2281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | George DA, Dosani A, Morgan-Jones R. Patellar reconstruction following previous patellectomy: a review of the literature and a case series using distal femoral autograft during total knee arthroplasty. Ann R Coll Surg Engl. 2017;99:e97-e101. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Jabbar Y, Ruiz A. Patellar reconstruction using posterior femoral condyle: a 5-year follow-up. Ann R Coll Surg Engl. 2009;91:W7-W8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Pang HN, Sathappan SS. Patellar reconstruction using distal femoral autograft in a patellectomized patient undergoing total knee arthroplasty. J Arthroplasty. 2008;23:939.e1-939.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Daentzer D, Rudert M, Wirth CJ, Stukenborg-Colsman C. Reconstruction of the patella with an autogenous iliac graft: clinical and radiologic results in thirteen patients. Int Orthop. 2012;36:545-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Tirveilliot F, Migaud H, Tillie B, Vielpeau C, Flautre B, Gougeon F. [Patellar reconstruction during total knee arthroplasty after previous patellectomy]. Rev Chir Orthop Reparatrice Appar Mot. 2003;89:613-620. [PubMed] |
| 26. | Buechel FF. Patellar tendon bone grafting for patellectomized patients having total knee arthroplasty. Clin Orthop Relat Res. 1991;72-78. [PubMed] |
| 27. | Busfield BT, Ries MD. Whole patellar allograft for total knee arthroplasty after previous patellectomy. Clin Orthop Relat Res. 2006;450:145-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 28. | Kulkarni S, Sawant M, Ireland J. Allograft reconstruction of the extensor mechanism for progressive extensor lag after total knee arthroplasty and previous patellectomy: a 3-year follow-up. J Arthroplasty. 1999;14:892-894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 29. | Kwong Y, Desai VV. The use of a tantalum-based Augmentation Patella in patients with a previous patellectomy. Knee. 2008;15:91-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 30. | Matar HE, Bawale R, Gollish JD. Extensor mechanism reconstruction "Tubeplasty" in total knee arthroplasty with previous patellectomy: Surgical technique and clinical outcomes. J Orthop. 2020;21:14-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 31. | Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;13-14. [PubMed] |
| 32. | Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1105] [Cited by in RCA: 1026] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 33. | Wendt PP, Johnson RP. A study of quadriceps excursion, torque, and the effect of patellectomy on cadaver knees. J Bone Joint Surg Am. 1985;67:726-732. [PubMed] |
| 34. | Dodds A, Crowley R, Menz T, Spriggins T, Keene G, Bauze A. Outcome following total knee replacement in patients with a previous patellectomy. Acta Orthop Belg. 2018;84:251-256. [PubMed] |
| 35. | Brauns J, Feyen H. Unicondylar knee arthroplasty following a patellectomy. Arthroplast Today. 2020;6:48-51. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 36. | Kouk S, Kalbian I, Wolfe E, Strickland SM. Robot-Assisted Medial Compartment Arthroplasty Following Remote Patellectomy: A Case Report. J Orthop Case Rep. 2018;8:11-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 37. | Giessler GA, Hendrich C. De Novo Reconstruction of a Hybrid Patella by Staged Fabrication of a Microvascular Bone Transplant with an Osteointegrated Prosthetic Socket. Plast Reconstr Surg Glob Open. 2016;4:e1159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Argentina
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Hosseinzadeh N, Iran; Jennane R, France; Oommen AT, India S-Editor: Gong ZM L-Editor: A P-Editor: Yu HG