Published online Nov 20, 2022. doi: 10.5662/wjm.v12.i6.476
Peer-review started: April 15, 2022
First decision: August 1, 2022
Revised: September 1, 2022
Accepted: November 4, 2022
Article in press: November 4, 2022
Published online: November 20, 2022
Processing time: 215 Days and 3.9 Hours
Several unique clinical features of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the cause of coronavirus disease 2019 (COVID-19) infection, have been identified and characterized. One such feature, mostly among patients with severe COVID-19 infection, has become known as COVID-19-induced coagu
To perform a systematic review and meta-analysis of the literature on COVID-19 infections that led to thrombotic complications necessitating surgical intervention.
The current systematic review implemented an algorithmic approach to review all the currently available English medical literature on surgical interventions necessitated by COVID-19 thrombotic complications using the preferred reporting items for systematic reviews and meta-analysis principles. A comprehensive search of the medical literature in the “PubMed”, “Scopus”, “Google Scholar” top 100 results, and archives of Plastic and Reconstructive Surgery was performed using the key words “COVID-19” AND “surgery” AND “thromboembolism” AND “compli
The database search resulted in the final inclusion of 22 retrospective studies, after application of the inclusion/exclusion criteria. Of the included studies, 17 were single case reports, 3 were case series and 2 were cross sectional cohort studies. All studies were retrospective in nature. Twelve of the reported studies were conducted in the United States of America, with the remaining studies originating from Italy, Turkey, Pakistan, France, Serbia, and Germany. All cases reported in our study were laboratory confirmed SARS-CoV-2 positive. A total of 70 cases involving surgical intervention were isolated from the 22 studies included in this review.
There is paucity of data describing the relationship between COVID-19 infection and thrombotic complications necessitating the need for surgical intervention. Intestinal ischemia and acute limb ischemia are amongst the most common thrombotic events due to COVID-19 that required operative management. An overall postoperative mortality of 30% was found in those who underwent operative procedures for thrombotic complications, with most deaths occurring in those with bowel ischemia. Physicians should be aware that despite thromboprophylaxis, severe thrombotic complications can still occur in this patient population, however, surgical intervention results in relatively low mortality apart from cases of ischemic bowel resection.
Core Tip: Surgical patient with a history of or current active infection with severe acute respiratory syndrome coronavirus 2 bear a significantly high risk for postoperative thrombotic complications. These patients may require surgical intervention to treat severe thrombotic complications. In total, 70 cases of thromboembolic complications necessitating surgical intervention have been documented. These patients have an overall mortality rate of 30%. Intestinal ischemia and acute limb ischemia are the most common thrombotic complications that required operative management. Physicians should be aware that severe thrombotic complications can occur in this patient population, however, surgical intervention results in relatively low mortality apart from cases of ischemic bowel resection.
- Citation: Ferraro JJ, Reynolds A, Edoigiawerie S, Seu MY, Horen SR, Aminzada A, Hamidian Jahromi A. Associations between SARS-CoV-2 infections and thrombotic complications necessitating surgical intervention: A systematic review. World J Methodol 2022; 12(6): 476-487
- URL: https://www.wjgnet.com/2222-0682/full/v12/i6/476.htm
- DOI: https://dx.doi.org/10.5662/wjm.v12.i6.476
Coronavirus disease 2019 (COVID-19) is a pandemic infection caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)[1]. Since December 2019, COVID-19 has spread throughout the world and changed the landscape of biomedical research and healthcare in a myriad of ways. Several unique clinical features of the virus have been identified and extensively characterized. One such feature, mostly among patients with severe COVID-19 infection and to some extent in less severe cases, is known as COVID-19-induced coagulopathy (CIC), which manifests as considerable elevation in D-dimer and fibrin split products, with little to no associated change in activated partial thromboplastin time and prothrombin time[2].
A large proportion of patients with CIC have been reported to develop venous and arterial thromboembolic complications[3]. Critically ill patients and patients undergoing surgeries are generally predisposed to thromboembolism due to a combined immobility, systemic inflammation, endothelial dysfunction, and circulatory stasis[4,5]. The progression of CIC can be insidious, with some cases of pulmonary embolism (PE) identified as the first sign of SARS-CoV-2 infection in patients with no early evidence of virus upon testing with nasopharyngeal swab[6]. Thrombotic risks posed by CIC cannot be underestimated, as it is not limited to patients within intensive care or other high-dependency settings[7].
Postoperative thrombotic complications such as venous thromboembolism (VTE) and PE are responsible for significant morbidity and mortality among patients undergoing invasive procedures and surgeries[8,9]. Approximately 50% of all reported VTEs are provoked by prolonged immobilization, trauma, surgery, or hospitalization within the last 3 mo[10,11]. Therefore, a surgical patient with a history of or active COVID-19 infection would be at a significantly higher risk for postoperative thrombotic complications than the general population[12,13]. Traditionally cases of VTE are treated with systemic anticoagulation (i.e., heparin, low molecular weight heparins, direct oral anticoagulants, and vitamin-K antagonists) following a careful evaluation of the risks and benefits. The thrombolysis is reserved for clinically serious and massive PE conditions in an attempt to dissolve the clot more rapidly than with anticoagulation options and reduce the mortality[14]. Severe cases of thromboembolic complications may require surgical intervention (i.e., mechanical thrombectomy, catheter direct thrombolysis) to reduce the risk of post thrombotic syndrome and venous insufficiencies [in case of deep venous thrombosis (DVT)][15] or the risk of pulmonary insufficiencies, hemodynamic instability and or death (in cases of PE)[14]. Therefore, a patient with previous or active COVID-19 infection may require surgical intervention to treat severe thrombotic complications. Few studies have characterized this association. The purpose of this study was to perform a systematic review and meta-analysis of the literature on COVID-19 infections that led to thrombotic complications necessitating surgical intervention.
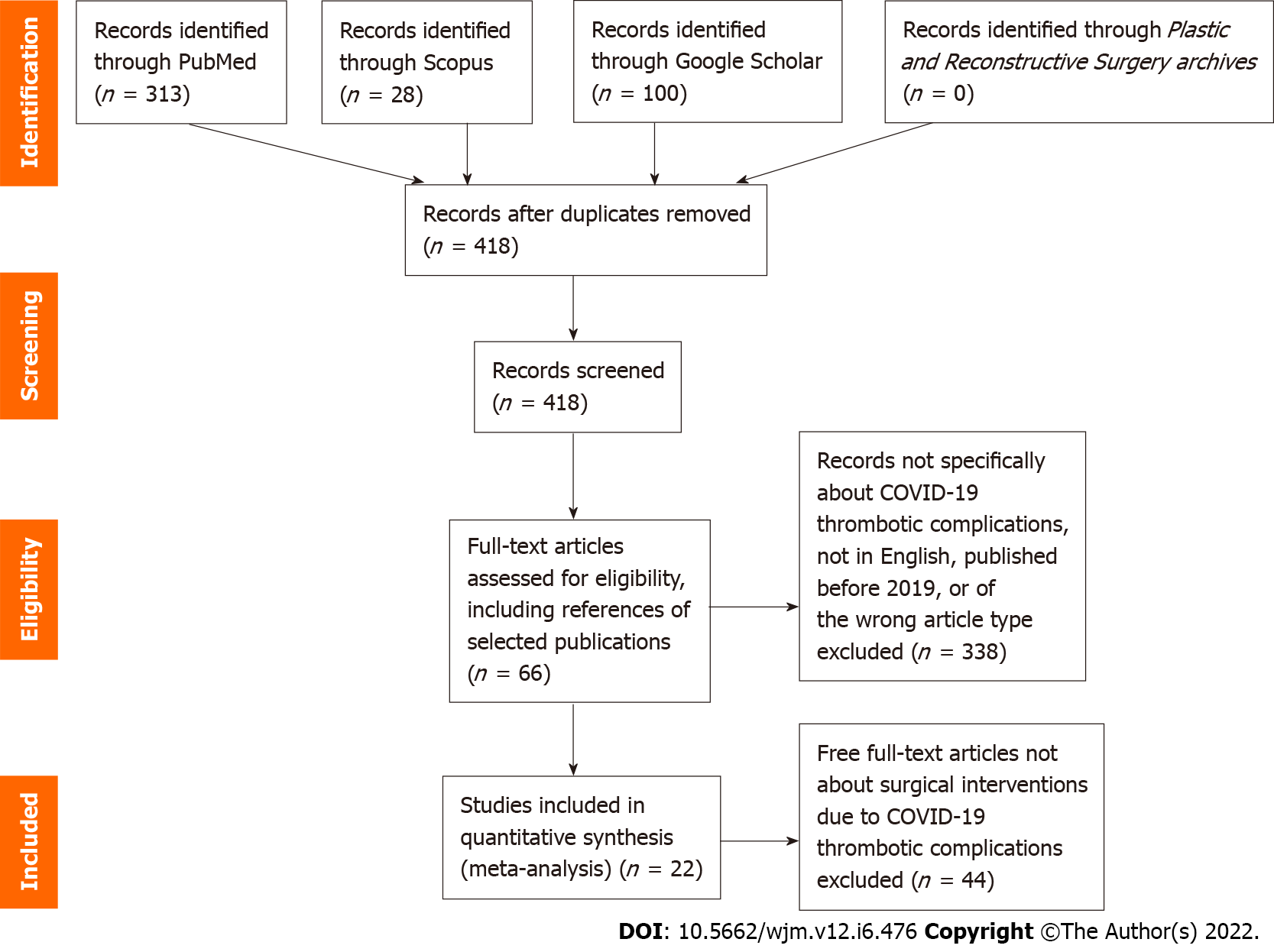
The current systematic review implemented an algorithmic approach to review all the currently available English medical literature on surgical interventions necessitated by COVID-19 thrombotic complications using the preferred reporting items for systematic reviews and meta-analysis principles (Figure 1). A comprehensive search of the medical literature in the “PubMed”, “Scopus”, “Google Scholar” top 100 results, and archives of Plastic and Reconstructive Surgery was performed by two authors (Reynolds A and Edoigiawerie S) on January 4, 2022, using the key words “COVID-19” AND “surgery” AND “thromboembolism” AND “complication” as well as associated terms.
The search string was generated and the records which were not specific about surgical interventions or thrombotic complications due to COVID-19 infection were excluded. Foreign language articles were not eligible for inclusion. Articles published prior to 2019 were excluded as being prior to the COVID-19 pandemic and therefore not relevant to complications associated with COVID-19 infection. Titles and abstracts were screened by two authors (Reynolds A and Edoigiawerie S) after which full-text articles were assessed for eligibility and inclusion. On initial and secondary search, papers in review, commentary, or letter format or those without accessible full-text articles were excluded.
Finally, results were further refined to focus on articles that featured surgical interventions that were necessitated by COVID-19 thrombotic complications. For completion of the search, the references of the selected publications were additionally screened with the priorly mentioned inclusion criteria. We also cited high-quality articles in Reference Citation Analysis (https://www.referencecitationanalysis.com).
The database search resulted in the final inclusion of 22 retrospective studies, after application of the inclusion/exclusion criteria. Of the included studies, 17 were single case reports, 3 were case series and 2 were cross sectional cohort studies. All studies were retrospective in nature. Twelve of the reported studies were conducted in the United States of America, with the remaining studies originating from Italy, Turkey, Pakistan, France, Serbia, and Germany. All cases reported in our study were laboratory confirmed SARS-CoV-2 positive. A total of 70 cases involving surgical intervention were isolated from the 22 studies included in this review. The 22 studies which were included in the review are listed in detail in (Table 1).
| Ref. | Location | Study design | No. of patients | Age (yr) | Sex: Males, females (%) | Comorbidities | Thromboprophylaxis | Thromboembolic complication(s) | Surgical intervention(s) | Outcome |
| Adekiigbe et al[43], 2020 | NY, United States | Case report | 1 | 47 | Male | DM | Yes | Cutaneous vasculitic lesions and gangrene of all toes, bilateral DVT | Bilateral transmetatarsal amputations of all 10 toes | Discharged home |
| Ali Nasir et al[20], 2021 | Pakistan | Case report | 1 | 64 | Male | T2DM, HTN | No | Acute LLI | Above knee amputation | Discharged home |
| Balanescu et al[33], 2021 | MI, United States | Case series | 4 | 20-77 (median 52) | Male (50) | Obesity (50%) | Unknown | PE | Mechanical thrombectomy (100%) | Discharged home (100%) |
| Bilge et al[21], 2021 | Turkey | Case report | 1 | 73 | Male | HTN | No | Upper extremity arterial thromboembolism | Left upper extremity arteriotomy and arterial thrombectomy. Repeat thrombectomy 12 h later. Amputation at the level of the forearm 13 d later. Stump revision with amputation 22 d later | Discharged home |
| Bozzani et al[22], 2020 | Italy | Case series | 6 | 71 (49-83) | 4 males (66) | 3 PAD, other unknown | Unknown | Acute LLI | Urgent revascularization procedures (embolectomy in 3 cases, and hybrid open/endo procedures in other 3) | 1 rethrombosed day 5, died 30 d later of MOF. 1 rethrombosed day 5, repeat embolectomy, above knee amputation. 4 discharged home. 23 discharged home in good condition |
| Cheung et al[55], 2020 | NY, United States | Case report | 1 | 55 | Male | HTN | No | SMA thrombosis, bowel ischemia | Emergency exploratory laparotomy and SMA thrombectomy, necrotic small bowel resection | Discharged home |
| Dao et al[56], 2021 | CA, United States | Case report | 1 | 61 | Male | HTN | Yes | Free floating descending aortic thrombus | Percutaneous vacuum assisted aortic thrombectomy | Discharged home |
| Dinoto et al[23], 2021 | Italy | Case report | 1 | 78 | Male | DM, obesity, prior remote endovascular surgery for large popliteal aneurysm | No | Acute LLI. Thrombosis of left femoral-popliteal stent | Mechanical thrombectomy | Discharged home |
| Galastri et al[34], 2020 | Brazil | Case report | 1 | 57 | Male | DM, obesity, HTN | Yes | Massive PE | Catheter directed thrombolysis | Discharged home |
| Gutierrez et al[39], 2022 | NY, United States | Case report | 1 | 53 | Male | HTN, remote smoking, DM | Yes | Due to phlegmasia cerulean dolens | Fasciotomy and mechanical thrombectomy | Discharged PAD 70 |
| Hwabejire et al[19], 2021 | MA, United States | Case series | 20 | 58 ± 7 | 13 males (65) | Obesity (60%) | 85% (17) received preoperative anticoagulation | Acute bowel ischemia | Laparotomy with resection of bowel | 50% overall mortality rate: (1) 100% mortality in patients ≥ 65 yr; (2) 33% mortality < 65 yr; and (3) 40% (8) developed |
| Jamshidi et al[40], 2021 | CA, United States | Case report | 1 | 51 | Male | Tricuspid atresia status post Fontan and extracardiac Shunt | Yes | Bilateral lower extremity DVT, phlegmasia cerulea dolens of the left lower extremity | Catheter directed mechanical thrombectomy (PAD 13), left below knee amputation (PAD 41) | Discharged to rehabilitation facility PAD 50 |
| Khanna et al[32], 2021 | PA, United States | Case report | 1 | 67 | Female | HTN | No | Acute stroke from bilateral anterior circulation large vessel occlusion | Bilateral simultaneous mechanical thrombectomy | Full neurologic recovery |
| Nascimbene et al[35], 2021 | TX, United States | Case report | 1 | 44 | Male | Patent foramen ovale, T2DM, HTN, dyslipidemia, obesity | No | Massive PE with a large right atrial thrombus | Percutaneous right and left atrium embolectomy | Discharged home |
| Naudin et al[24], 2021 | France | Case report | 1 | 56 | Male | T2DM, HTN, obesity | No | Acute aortoiliac thrombus and LLI | Aortoiliac and lower limb artery mechanical thrombectomy and left lower limb fasciotomies, subsequent left below knee amputation | Extubated but still in ICU 6 wk post operatively |
| Szeles et al[25], 2021 | NY, United States | Case report | 1 | 67 | Male | DM, hyperlipidemia, HTN | No | Acute LLI and aortic mural thrombosis | Emergency bilateral aortoliliac and distal embelectomies, followed by transmetatarsal amputation of the right foot and below knee amputation of the left limb | |
| Topcu et al[26], 2021 | Turkey | Single center cross sectional study | 3 | 62 (58-70) | 3 (100) | 1 ex-smoker | Yes (100%) | Acute LLI | 3 emergency surgical thrombectomy | 1 minor amputation (33.3%); 1 death (33.3%); 1 bilateral major amputation (33.3%) |
| Traina et al[18], 2021 | Italy | Case report | 1 | 80 | Male | CVD, prior endovascular aortic repair in 2019 for abdominal aneurysm repair, and dyslipidemia | No | Bowel ischemia with aorto-enteric fistula formation | Laparotomy with resection of necrotic small bowel (occult COVID-19, diagnosed on histologic examination of resected small bowel) | Discharged home |
| Vyas et al[36], 2020 | NY, United States | Case report | 1 | 32 | Male | None | No | Large saddle pulmonary embolus | Bilateral percutaneous pulmonary artery mechanical thrombectomy | Discharged home 3 d post procedure |
| Yang et al[17], 2021 | Germany | Cohort study | 20 | 69 (62-72) | 15 males (75) | 65% (13) obese | 25% (5) | Colonic ischemia | 12 (60%) underwent (sub)total colectomy, 7 (35%) right hemicolectomy, 1 (5%) ileocecal resection | 9 (45%) surgical complications, 10 (50%) required revision surgery, 9 (45%) mortality |
| Zivkovic et al[57], 2021 | Serbia | Case report | 1 | 44 | Female | None | No | Ascending aorta floating thrombus with acute right arm ischemia | Surgical thrombus extraction through open sternotomy and bypass surgery | Discharged POD 6 |
| Madani et al[27], 2021 | CA, United States | Cases report | 1 | 40 | Male | HTN, T2DM | Yes | Acute LLI | Right lower extremity above knee amputation | Discharged 41 d after admission |
Thromboembolic complications are a well-known sequela of COVID-19 infection, and their incidence has been the subject of many recent studies. The predisposition to the development of both venous and arterial thromboembolic complications by COVID-19 has also been well established, with incidences of thromboembolic complications in COVID-19 patients ranging from 7.2% to 40.8%[16]. The high complication rate poses a public health concern due to the increased morbidity, mortality and high costs associated with their development[16]. Such complications also pose a significant challenge to physicians treating them, as the need for a surgical intervention must be weighed against the risk of operation in an unstable and high-risk individual while the patient is in an already prothrombotic state. There is a significant gap in the literature describing the relationship between COVID-19 infections and thrombotic events requiring surgical intervention.
Of the 70 COVID-19 patients with thromboembolic complications necessitating surgical intervention found in our study, 85% (n = 60) had thrombotic complications considered to be arterial in origin. The most common complication reported was intestinal ischemia at 60% (n = 42)[17-19]. The second most common complication was acute limb ischemia (ALI) at 23% (n = 16), which included 14 cases of lower limb ischemia and 2 cases of upper limb ischemia[20-27]. ALI is defined as a sudden decrease in arterial perfusion of an extremity that compromises the viability of a limb[28]. Prior to the COVID-19 pandemic, the incidence of ALI in the general population was found to be 10 to 15 per 100000 cases each year (0.0001%-0.00015%)[20]. However, one study performed in a New York City hospital found the rate of ALI in the COVID-19 population to be as high as 0.38%[29]. Treatment of ALI includes endovascular or open surgical revascularization, however 10% to 15% of patients end up undergoing amputation during their hospitalization[30,31]. Of the 16 cases of ALI in the population being investigated, 8 (50%) of these patients eventually underwent some form of amputation of the affected extremity. In addition to the above cases, our cohort had 1 case of stroke due to bilateral arterial thrombosis of the anterior circulating vessels, which was treated with bilateral simultaneous mechanical thrombectomy[32].
In contrast to arterial thrombotic events, venous thrombotic events are a more common sequela of COVID-19, with the PE and DVT at an estimated incidence of 13.5% and 11.8% respectively[16].In our study, PE accounted for 10% (n = 7) of thrombotic events necessitating surgical intervention[33-36], notably higher than both the reported incidence of PE amongst non-intensive care unit (ICU) hospitalized patients and ICU patients with COVID-19 (1.3% and 6.2%, respectively)[37,38]. Interestingly, our study included two cases of phlegmasia cerulean dolens (PCD)[39,40], a rare and life-threatening form of DVT that results in arterial occlusion secondary to compartment syndrome caused by total venous occlusion[41]. PCD has been reported to have an amputation rate close to 50%, as well as a mortality of up to 40%[42]. Of the two patients in our study with PCD, only one required amputation. Also included in our cohort was one patient who required bilateral transmetatarsal amputations due to the development of “COVID toes”, thought to be due to either microvascular thrombosis or related to a rare complication of venous thrombosis manifesting as venous gangrene[43].
Several studies have attempted to quantify mortality related to thromboembolic events in COVID-19 patients. One study found that COVID-19 patients with a thromboembolic event had a 40% mortality rate, over twice that of COVID patients without a thrombotic event[44]. Another study, a meta-analysis of 8271 patients, found that patients with COVID-19 who had thromboembolic events had a pooled mortality rate of 23%, with thromboembolism significantly increasing the odds of mortality by as high as 74%[45]. Similarly, Gonzalez-Fajardo et al[46] found a mortality rate of 23.58% in their retrospective review of COVID-19 patients with thrombotic events, with a higher mortality seen in patients with peripheral arterial thrombosis and ischemic stroke compared to those with DVT and PE. Our study of COVID-19 patients with thrombotic events needing surgical intervention produced an overall mortality rate of 30% (n = 21). Notably, the highest mortality rate was seen in patients with acute intestinal ischemia who underwent bowel resection (45%, n = 19 of 42), followed by patients treated for ALI (13%, n = 2 of 15). It is unclear at this time if COVID-19 infection significantly complicated the cases of bowel resection, as acute intestinal ischemia has been noted to have a mortality rate as high as 80%, even without the added complexity of COVID-19 infection[47]. This is partly due to difficulty in diagnosis, importance of early diagnosis, and the rapid deteriorating nature of ischemic intestinal tissue and the patient’s condition. It is possible that severe COVID-19 infection delayed the diagnosis of intestinal ischemia in several of the patients included in this study, leading to higher mortality rates. Difficulties in accessing medical and surgical care due the widespread impact of the current COVID-19 pandemic in every aspect of the health care could also be influential although the true nature and depth of such an impact is a matter of speculation.
In total, 17 of the 70 patients in this review had specific comorbidity data readily available. The most common comorbidities amongst our cohort of patients were hypertension (64%, n = 11), diabetes mellitus (53%, n = 9), and obesity (35%, n = 6), all of which have previously been associated with a prothrombotic state[48,49]. Hypertension has been noted to be an independent risk factor for the development of deep vein thrombosis in a large study of over 18000 patients[50], so it is not surprising that patients with hypertension and COVID-19 infection were at an increased risk of thrombotic complications necessitating surgical intervention. However, a recent study by Xiong et al[51] demonstrated no increase in thrombotic events among COVID-19 patients who were obese or had hypertension. Interestingly, their meta-analysis also found a previous diagnosis of diabetes mellitus to have a protective rather than potentiating effect on thrombotic events in this population. These results have been attributed to the use of medications such as statins and metformin, which have some degree of anti-inflammatory effects. While concomitant medication use was not a variable under investigation in our study, future studies may look at the relationship between medications with anti-inflammatory effects and reduced thrombotic complications of COVID-19.
Since it became apparent that COVID-19 produces a prothrombotic state, much of the focus on thrombotic complication management has been shifted towards prevention. In May of 2020, the International Society on Thrombosis and Hemostasis published a statement regarding hospitalized COVID-19 patients in the ICU, recommending routine thromboprophylaxis with standard-dose low molecular-weight heparin or unfractionated heparin, unless contraindicated[52]. Yet our study found that 44%(n = 31) of patients who developed thrombotic complications requiring surgical intervention received some type of prophylactic anticoagulant therapy. This finding is consistent with the current literature, as studies have shown a high rate of thromboembolic complications in COVID-19 patients despite the use of prophylactic anticoagulation[53], with one study estimating this phenomenon to occur in almost one-third of all critically ill COVID-19 patients[54]. As previously stated, CIC has been reported to be the presenting symptom of some severe COVID-19 infections, making it possible for some patients in our study to have had thrombotic events prior to their presentation or COVID-19 diagnosis. Additionally, in several of the studies analyzed by this systematic review, dosage information and duration of thromboprophylaxis was not described, therefore it is unclear if some patients were subtherapeutic with their thromboprophylaxis regimen. Further studies to look at the dose and choice of anticoagulant in relation to severe thromboembolic events in the setting of COVID-19 infection is warranted.
Our study is one of the first to analyze the relationship between COVID-19 infection and thrombotic complications that required surgical intervention, but there were several limitations. As all the included studies in this review were retrospective in nature, bias cannot be eliminated. Additionally, differences between the studies included in this review may lead to an additional bias, including the reporting of and variation of type and dosage of thromboprophylaxis. The reporting of outcomes and mortality, location of thrombotic events, and the method of surgical management also varied between many of the studies. Finally, our review drew a relatively small sample size, and our search criteria included only those studies in which patients were reported to have surgical intervention for their thrombotic events, and therefore incidence data could not be calculated.
There is paucity of data describing the relationship between COVID-19 infection and thrombotic complications necessitating the need for surgical intervention. Intestinal ischemia and ALI are amongst the most common thrombotic events due to COVID-19 that required operative management. An overall postoperative mortality of 30% was found in those who underwent operative procedures for thrombotic complications, with most deaths occurring in those with bowel ischemia. Physicians should be aware that despite thromboprophylaxis, severe thrombotic complications can still occur in this patient population, however, surgical intervention results in relatively low mortality apart from cases of ischemic bowel resection.
It is well-known that coronavirus disease 2019 (COVID-19) infection is associated with hypercoagulability among affected patients. This has become known as COVID-19 induced coagulopathy (CIC). This study investigated CIC-related thrombotic complications through a systematic review and meta-analysis of the existing literature.
There is paucity of data describing the relationship between COVID-19 infection and thrombotic complications necessitating the need for surgical intervention. Intestinal ischemia and acute limb ischemia (ALI) are amongst the most common thrombotic events due to COVID-19 that required operative management. An overall postoperative mortality of 30% was found in those who underwent operative procedures for thrombotic complications, with most deaths occurring in those with bowel ischemia. Physicians should be aware that despite thromboprophylaxis, severe thrombotic complications can still occur in this patient population, however, surgical intervention results in relatively low mortality apart from cases of ischemic bowel resection.
Main, overarching objective was to conduct a systematic review to find the currently published medical literature describing surgical interventions necessitated by COVID-19 thrombotic complications. We achieved this objective and identified intestinal ischemia and ALI as the most common thrombotic events necessitating surgical intervention.
The current systematic review was performed using an algorithmic approach to review all the currently available articles in the English medical literature on surgical interventions necessitated by COVID-19 thrombotic complications using the preferred reporting items for systematic reviews and meta-analysis principles. A comprehensive literature search in the “PubMed”, “Scopus”, “Google Scholar” top 100 results, and archives of Plastic and Reconstructive Surgery was performed by two authors (Reynolds A and Edoigiawerie S) on January 4, 2022, using the key words “COVID-19” AND “surgery” AND “thromboembolism” AND “complication” as well as associated terms. The search string was generated and the records which were not relevant were excluded. Articles published prior to 2019 were excluded as being prior to the COVID-19 pandemic and therefore not relevant to complications associated with COVID-19 infection. Titles, abstracts, and full-text articles were assessed for eligibility and inclusion. On initial and secondary search, papers in review, commentary, or letter format or those without accessible full-text articles were excluded. Finally, results were further reviewed and refined to focus on articles that featured surgical interventions that were necessitated by COVID-19 thrombotic complications. For completion of the search, the references of the selected publications were additionally screened with the previously mentioned inclusion criteria.
The database search resulted in the final inclusion of 22 retrospective studies, after application of the inclusion/exclusion criteria. Of the included studies, 17 were single case reports, 3 were case series and 2 were cross sectional cohort studies. All studies were retrospective in nature. Twelve of the reported studies were conducted in the United States of America, with the remaining studies originating from Italy, Turkey, Pakistan, France, Serbia, and Germany. All cases reported in our study were laboratory confirmed severe acute respiratory syndrome coronavirus 2 positive. A total of 70 cases involving surgical intervention were isolated from the 22 studies included in this review.
Physicians should be aware that despite thromboprophylaxis, severe thrombotic complications can still occur in this patient population, however, surgical intervention results in relatively low mortality apart from cases of ischemic bowel resection.
Future directions could focus on how to prevent thrombotic complications and mitigate mortality among patients at risk for ALI and bowel ischemia in particular.
| 1. | Khan M, Adil SF, Alkhathlan HZ, Tahir MN, Saif S, Khan M, Khan ST. COVID-19: A Global Challenge with Old History, Epidemiology and Progress So Far. Molecules. 2020;26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 247] [Cited by in RCA: 249] [Article Influence: 41.5] [Reference Citation Analysis (0)] |
| 2. | Hadid T, Kafri Z, Al-Katib A. Coagulation and anticoagulation in COVID-19. Blood Rev. 2021;47:100761. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 108] [Cited by in RCA: 130] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 3. | Levi M, Thachil J, Iba T, Levy JH. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020;7:e438-e440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 878] [Cited by in RCA: 1085] [Article Influence: 180.8] [Reference Citation Analysis (0)] |
| 4. | The Lancet Haematology. COVID-19 coagulopathy: an evolving story. Lancet Haematol. 2020;7:e425. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 90] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 5. | Stoneham SM, Milne KM, Nuttall E, Frew GH, Sturrock BR, Sivaloganathan H, Ladikou EE, Drage S, Phillips B, Chevassut TJ, Eziefula AC. Thrombotic risk in COVID-19: a case series and case-control study. Clin Med (Lond). 2020;20:e76-e81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 67] [Article Influence: 11.2] [Reference Citation Analysis (1)] |
| 6. | Carbone F, Montecucco F, Twickler M. SARS-CoV-2: What is known and what there is to know-Focus on coagulation and lipids. Eur J Clin Invest. 2020;50:e13311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Pooni RS. Research in brief: Coagulopathy in COVID-19: Determining and managing thrombotic risk in COVID-19 infection. Clin Med (Lond). 2020;20:e59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Edmonds MJ, Crichton TJ, Runciman WB, Pradhan M. Evidence-based risk factors for postoperative deep vein thrombosis. ANZ J Surg. 2004;74:1082-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 89] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Hanh BM, Cuong LQ, Son NT, Duc DT, Hung TT, Hung DD, Giang TB, Hiep NH, Xuyen HTH, Nga NT, Chu DT. Determination of Risk Factors for Venous Thromboembolism by an Adapted Caprini Scoring System in Surgical Patients. J Pers Med. 2019;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Shen C, Ge B, Liu X, Chen H, Qin Y, Shen H. Predicting the occurrence of venous thromboembolism: construction and verification of risk warning model. BMC Cardiovasc Disord. 2020;20:249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Hereford T, Thrush C, Kimbrough MK. Using Injury Severity Score and Abbreviated Injury Score to Determine Venous Thromboembolism Risk. Cureus. 2019;11:e5977. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Di Minno A, Ambrosino P, Calcaterra I, Di Minno MND. COVID-19 and Venous Thromboembolism: A Meta-analysis of Literature Studies. Semin Thromb Hemost. 2020;46:763-771. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 129] [Cited by in RCA: 202] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 13. | COVIDSurg Collaborative; GlobalSurg Collaborative. SARS-CoV-2 infection and venous thromboembolism after surgery: an international prospective cohort study. Anaesthesia. 2022;77:28-39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 97] [Cited by in RCA: 90] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 14. | Hao Q, Dong BR, Yue J, Wu T, Liu GJ. Thrombolytic therapy for pulmonary embolism. Cochrane Database Syst Rev. 2018;12:CD004437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Notten P, Ten Cate-Hoek AJ, Arnoldussen CWKP, Strijkers RHW, de Smet AAEA, Tick LW, van de Poel MHW, Wikkeling ORM, Vleming LJ, Koster A, Jie KG, Jacobs EMG, Ebben HP, Coppens M, Toonder I, Ten Cate H, Wittens CHA. Ultrasound-accelerated catheter-directed thrombolysis vs anticoagulation for the prevention of post-thrombotic syndrome (CAVA): a single-blind, multicentre, randomised trial. Lancet Haematol. 2020;7:e40-e49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 140] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 16. | Kunutsor SK, Laukkanen JA. Incidence of venous and arterial thromboembolic complications in COVID-19: A systematic review and meta-analysis. Thromb Res. 2020;196:27-30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 68] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 17. | Yang C, Hakenberg P, Weiß C, Herrle F, Rahbari N, Reißfelder C, Hardt J. Colon ischemia in patients with severe COVID-19: a single-center retrospective cohort study of 20 patients. Int J Colorectal Dis. 2021;36:2769-2773. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Traina L, Mucignat M, Rizzo R, Gafà R, Bortolotti D, Passaro A, Zamboni P. COVID-19 induced aorto duodenal fistula following evar in the so called "negative" patient. Vascular. 2021;17085381211053695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Hwabejire JO, Kaafarani HMA, Mashbari H, Misdraji J, Fagenholz PJ, Gartland RM, Abraczinskas DR, Mehta RS, Paranjape CN, Eng G, Saillant NN, Parks J, Fawley JA, Lee J, King DR, Mendoza AE, Velmahos GC. Bowel Ischemia in COVID-19 Infection: One-Year Surgical Experience. Am Surg. 2021;87:1893-1900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Ali Nasir S, Arif A, Shahid M, Ahmed Y, Riaz B, Sherwani NZF. Acute Limb Ischemia in a Patient With COVID-19 Pneumonia. Cureus. 2021;13:e18574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 21. | Bilge A, Karasoy İ, Neziroğlu E, Güner Y. Upper extremity arterial thromboembolism in a patient with severe COVID-19 pneumonia: A case report. Jt Dis Relat Surg. 2021;32:551-555. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Bozzani A, Arici V, Tavazzi G, Franciscone MM, Danesino V, Rota M, Rossini R, Sterpetti AV, Ticozzelli G, Rumi E, Mojoli F, Bruno R, Ragni F. Acute arterial and deep venous thromboembolism in COVID-19 patients: Risk factors and personalized therapy. Surgery. 2020;168:987-992. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 23. | Dinoto E, Ferlito F, Urso F, Pakeliani D, Bajardi G, Pecoraro F. Mechanical rotational thrombectomy in long femoropopliteal artery and stent occlusion in COVID-19 patient: Case report. Int J Surg Case Rep. 2021;84:106133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Naudin I, Long A, Michel C, Devigne B, Millon A, Della-Schiava N. Acute aortoiliac occlusion in a patient with novel coronavirus disease-2019. J Vasc Surg. 2021;73:18-21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 25. | Szeles A, El-Daher NT, Lachant N, Rizk TA. Acute limb ischemia and aortic mural thrombosis as primary manifestations of severe acute respiratory syndrome coronavirus 2. J Vasc Surg Cases Innov Tech. 2021;7:605-609. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Topcu AC, Ozturk-Altunyurt G, Akman D, Batirel A, Demirhan R. Acute Limb Ischemia in Hospitalized COVID-19 Patients. Ann Vasc Surg. 2021;74:88-94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 27. | Madani MH, Leung ANC, Becker HC, Chan FP, Fleischmann D. Aorto-iliac/right leg arterial thrombosis necessitating limb amputation, pulmonary arterial, intracardiac, and ilio-caval venous thrombosis in a 40-year-old with COVID-19. Clin Imaging. 2021;75:1-4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Björck M, Earnshaw JJ, Acosta S, Bastos Gonçalves F, Cochennec F, Debus ES, Hinchliffe R, Jongkind V, Koelemay MJW, Menyhei G, Svetlikov AV, Tshomba Y, Van Den Berg JC; Esvs Guidelines Committee; de Borst GJ, Chakfé N, Kakkos SK, Koncar I, Lindholt JS, Tulamo R, Vega de Ceniga M, Vermassen F, Document Reviewers, Boyle JR, Mani K, Azuma N, Choke ETC, Cohnert TU, Fitridge RA, Forbes TL, Hamady MS, Munoz A, Müller-Hülsbeck S, Rai K. Editor's Choice - European Society for Vascular Surgery (ESVS) 2020 Clinical Practice Guidelines on the Management of Acute Limb Ischaemia. Eur J Vasc Endovasc Surg. 2020;59:173-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 330] [Article Influence: 47.1] [Reference Citation Analysis (0)] |
| 29. | Etkin Y, Conway AM, Silpe J, Qato K, Carroccio A, Manvar-Singh P, Giangola G, Deitch JS, Davila-Santini L, Schor JA, Singh K, Mussa FF, Landis GS. Acute Arterial Thromboembolism in Patients with COVID-19 in the New York City Area. Ann Vasc Surg. 2021;70:290-294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 74] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 30. | Eliason JL, Wainess RM, Proctor MC, Dimick JB, Cowan JA Jr, Upchurch GR Jr, Stanley JC, Henke PK. A national and single institutional experience in the contemporary treatment of acute lower extremity ischemia. Ann Surg. 2003;238:382-9; discussion 389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 128] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 31. | Earnshaw JJ, Whitman B, Foy C. National Audit of Thrombolysis for Acute Leg Ischemia (NATALI): clinical factors associated with early outcome. J Vasc Surg. 2004;39:1018-1025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 106] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 32. | Khanna O, Hafazalla K, Saiegh FA, Tahir R, Schunemann V, Theofanis TN, Mouchtouris N, Gooch MR, Tjoumakaris S, Rosenwasser RH, Jabbour PM. Simultaneous bilateral mechanical thrombectomy in a patient with COVID-19. Clin Neurol Neurosurg. 2021;206:106677. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 33. | Balanescu DV, Kado HS, Mertens A, Chand R, Savin M, McNally V, Bowers TR. Mechanical Thrombectomy in Pulmonary Embolism Associated with COVID-19: A "Clotography" Gallery. Vasc Endovascular Surg. 2021;55:903-906. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 34. | Galastri FL, Valle LGM, Affonso BB, Silva MJ, Garcia RG, Junior MR, Ferraz LJR, de Matos GFJ, de la Cruz Scarin FC, Nasser F. COVID-19 complicated by pulmonary embolism treated with catheter directed thrombectomy. Vasa. 2020;49:333-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 35. | Nascimbene A, Basra SS, Dinh K, Patel JA, Gregoric ID, Kar B. Percutaneous Thrombus Removal in COVID-19-Infected Patient with Pulmonary Embolism. Methodist Debakey Cardiovasc J. 2021;17:e33-e36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 36. | Vyas V, Kanagalingam G, Yadava S, Gambhir HS, Costanza M, Chaudhuri D. Bilateral pulmonary artery thrombectomy with saddle embolism and COVID-19 infection. Proc (Bayl Univ Med Cent). 2020;33:666-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 37. | Hill JB, Garcia D, Crowther M, Savage B, Peress S, Chang K, Deitelzweig S. Frequency of venous thromboembolism in 6513 patients with COVID-19: a retrospective study. Blood Adv. 2020;4:5373-5377. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 64] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 38. | Bilaloglu S, Aphinyanaphongs Y, Jones S, Iturrate E, Hochman J, Berger JS. Thrombosis in Hospitalized Patients With COVID-19 in a New York City Health System. JAMA. 2020;324:799-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 527] [Cited by in RCA: 598] [Article Influence: 99.7] [Reference Citation Analysis (0)] |
| 39. | Gutierrez JR, Volteas P, Skripochnik E, Tassiopoulos AK, Bannazadeh M. A Case of Phlegmasia Cerulea Dolens in a Patient With COVID-19, Effectively Ttreated With Fasciotomy and Mechanical Thrombectomy. Ann Vasc Surg. 2022;79:122-126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 40. | Jamshidi N, Tan W, Foote D, Reardon L, Lluri G, Aboulhosn J, Moriarty J, Lin J. Mechanical thrombectomy of COVID-19 DVT with congenital heart disease leading to phlegmasia cerulea dolens: a case report. BMC Cardiovasc Disord. 2021;21:592. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 41. | ELsaid AS, AlQattan AS, Elashaal E, AlSadery H, AlGhanmi I, Aldhafery BF. The ugly face of deep vein thrombosis: Phlegmasia Cerulea Dolens-Case report. Int J Surg Case Rep. 2019;59:107-110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 42. | Oguzkurt L, Ozkan U, Demirturk OS, Gur S. Endovascular treatment of phlegmasia cerulea dolens with impending venous gangrene: manual aspiration thrombectomy as the first-line thrombus removal method. Cardiovasc Intervent Radiol. 2011;34:1214-1221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 43. | Adekiigbe R, Ugbode F, Seoparson S, Katriyar N, Fetterman A. A 47-Year-Old Hispanic Man Who Developed Cutaneous Vasculitic Lesions and Gangrene of the Toes Following Admission to Hospital with COVID-19 Pneumonia. Am J Case Rep. 2020;21:e926886. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 44. | Cohen KR, Anderson D, Ren S, Cook DJ. Contribution of the elevated thrombosis risk of males to the excess male mortality observed in COVID-19: an observational study. BMJ Open. 2022;12:e051624. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 45. | Malas MB, Naazie IN, Elsayed N, Mathlouthi A, Marmor R, Clary B. Thromboembolism risk of COVID-19 is high and associated with a higher risk of mortality: A systematic review and meta-analysis. EClinicalMedicine. 2020;29:100639. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 424] [Cited by in RCA: 422] [Article Influence: 70.3] [Reference Citation Analysis (0)] |
| 46. | Gonzalez-Fajardo JA, Ansuategui M, Romero C, Comanges A, Gómez-Arbeláez D, Ibarra G, Garcia-Gutierrez A. Mortality of COVID-19 patients with vascular thrombotic complications. Med Clin (Engl Ed). 2021;156:112-117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 47. | Debus ES, Müller-Hülsbeck S, Kölbel T, Larena-Avellaneda A. Intestinal ischemia. Int J Colorectal Dis. 2011;26:1087-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 48. | Goldhaber SZ, Savage DD, Garrison RJ, Castelli WP, Kannel WB, McNamara PM, Gherardi G, Feinleib M. Risk factors for pulmonary embolism. The Framingham Study. Am J Med. 1983;74:1023-1028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 158] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 49. | Vazzana N, Ranalli P, Cuccurullo C, Davì G. Diabetes mellitus and thrombosis. Thromb Res. 2012;129:371-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 185] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 50. | Holst AG, Jensen G, Prescott E. Risk factors for venous thromboembolism: results from the Copenhagen City Heart Study. Circulation. 2010;121:1896-1903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 284] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 51. | Xiong X, Chi J, Gao Q. Prevalence and risk factors of thrombotic events on patients with COVID-19: a systematic review and meta-analysis. Thromb J. 2021;19:32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 56] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 52. | Spyropoulos AC, Levy JH, Ageno W, Connors JM, Hunt BJ, Iba T, Levi M, Samama CM, Thachil J, Giannis D, Douketis JD; Subcommittee on Perioperative, Critical Care Thrombosis, Haemostasis of the Scientific, Standardization Committee of the International Society on Thrombosis and Haemostasis. Scientific and Standardization Committee communication: Clinical guidance on the diagnosis, prevention, and treatment of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020;18:1859-1865. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 492] [Cited by in RCA: 558] [Article Influence: 93.0] [Reference Citation Analysis (0)] |
| 53. | Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, Nigoghossian C, Ageno W, Madjid M, Guo Y, Tang LV, Hu Y, Giri J, Cushman M, Quéré I, Dimakakos EP, Gibson CM, Lippi G, Favaloro EJ, Fareed J, Caprini JA, Tafur AJ, Burton JR, Francese DP, Wang EY, Falanga A, McLintock C, Hunt BJ, Spyropoulos AC, Barnes GD, Eikelboom JW, Weinberg I, Schulman S, Carrier M, Piazza G, Beckman JA, Steg PG, Stone GW, Rosenkranz S, Goldhaber SZ, Parikh SA, Monreal M, Krumholz HM, Konstantinides SV, Weitz JI, Lip GYH; Global COVID-19 Thrombosis Collaborative Group, Endorsed by the ISTH, NATF, ESVM, and the IUA, Supported by the ESC Working Group on Pulmonary Circulation and Right Ventricular Function. COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;75:2950-2973. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2178] [Cited by in RCA: 2216] [Article Influence: 369.3] [Reference Citation Analysis (0)] |
| 54. | Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers D, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, Endeman H. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb Res. 2020;191:148-150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1017] [Cited by in RCA: 1198] [Article Influence: 199.7] [Reference Citation Analysis (0)] |
| 55. | Cheung S, Quiwa JC, Pillai A, Onwu C, Tharayil ZJ, Gupta R. Superior Mesenteric Artery Thrombosis and Acute Intestinal Ischemia as a Consequence of COVID-19 Infection. Am J Case Rep. 2020;21:e925753. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 65] [Article Influence: 10.8] [Reference Citation Analysis (2)] |
| 56. | Dao L, Lund A, Schibler CD, Yoshioka CA, Barsky M. A Case of COVID-19-Associated Free-Floating Aortic Thrombus Successfully Treated with Thrombectomy. Am J Case Rep. 2021;22:e933225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 57. | Zivkovic I, Milacic P, Mihajlovic V, Krasic S, Lesanovic J, Peric M, Zdravkovic D. Surgical treatment of ascending aorta floating thrombus in a patient with recent SARS-CoV-2 infection. Cardiovasc Diagn Ther. 2021;11:467-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medical laboratory technology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Al-Ani RM, Iraq; Du BB, China S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ