Published online Jul 20, 2022. doi: 10.5662/wjm.v12.i4.293
Peer-review started: February 16, 2022
First decision: April 12, 2022
Revised: April 19, 2022
Accepted: July 8, 2022
Article in press: July 8, 2022
Published online: July 20, 2022
Processing time: 154 Days and 1.7 Hours
Smoking and chewing tobacco are associated with numerous oral mucosal lesions and conditions, often leading to cancer progression.
To investigate the prevalence of precancerous lesions and conditions among the Indian population.
Systematic search was conducted for population or community-based observational epidemiological studies in PubMed, EMBASE, Web of Science, IndMED, Google Scholar, reports of the WHO South-East Asia Region, MOHFW India reports, Science Citation Index, WHO Index Medicus of the South-East Asian Region, Reference Citation Analysis (https://www.referencecitationanalysis.com/) and Open Grey from the earliest available up to 31st January 2022. The effect size was calculated for the prevalence of precancerous lesions and conditions.
One hundred sixty-two estimates from 130 studies yielded 52 high, 71 moderate, and seven low-quality studies from 823845. Point estimate based on cross-sectional studies for leukoplakia was 4.3% (95%CI: 4.0-4.6), oral submucous fibrosis was 2.7% (95%CI: 2.5-3.0), palatal lesions in reverse smokers and nicotine palatine were 5.8% (95%CI: 4.4-7.2), and Erythroplakia was 1.2% (95%CI: 0.7-1.7), and lichen planus was 1.1% (95%CI: 0.9-1.2). Amongst hospital-based studies, the pooled prevalence for Leukoplakia was 6.7% (95%CI: 6.0-7.3), oral submucous fibrosis was 4.5% (95%CI: 4.2-4.9), lichen planus was 7.5% (95%CI: 5.3-9.6), and erythroplakia was 2.5% (95%CI: 0.4-4.5), and palatal lesions in reverse smokers and nicotine palatini were 11.5% (95%CI: 8.0-15.0).
Precancerous lesions and conditions are prevailing problems among the Indian population. It is mainly due to tobacco use, the smokeless form of tobacco. The meta-analysis indicates that hospital-based studies have a higher effect size of 6.7% than community-based studies. Patients who have already developed this condition may be advised to reduce their exposure to the risk factor to prevent the condition from progressing further.
Core Tip: World Health Organization assessment estimated that by 2020 tobacco-related death may exceed 1.5 million annually or 13% of all deaths in India. Tobacco consumption and smoking are seen in different socioeconomic groups, and this adverse habit is spread over urban and rural areas, giving rise to precancerous lesions and conditions. Prevalence of various oral lesions and conditions in India are varying in different studies. Numerous studies have been conducted throughout India to determine the prevalence of precancerous lesions and conditions.
- Citation: Kumbhalwar A, Shetiya SH, Kakodkar P, Mehta V, Mathur A, Porwal P. Prevalence of precancerous lesions and conditions in India: A systematic review and meta-analysis. World J Methodol 2022; 12(4): 293-304
- URL: https://www.wjgnet.com/2222-0682/full/v12/i4/293.htm
- DOI: https://dx.doi.org/10.5662/wjm.v12.i4.293
World Health Organization (WHO) assessment estimated that by 2020 tobacco-related death may exceed 1.5 million annually, or 13% of all deaths in India[1]. Most smokers living in middle-income countries are the most giant smokers globally, amounting to 68% of all smokers[2]. South-East Asia Region (SEAR) is home to over 80% of global smokeless tobacco (SLT) users, higher than smoking[3]. Prevalence of tobacco use has decreased by 6%, points from 34.6% in GATS-1 in 2009-2010 to 28.6% in GATS-2 in 2016-2017 in India[4].
In the community-based study by Kvv et al[5] in 2004, 46579 were examined, and the prevalence of Lichen planus was 2.02%, and Leukoplakia was 1.73%. A study done by Mehrotra et al[6] in 2017 amongst 453823 people showed a prevalence of 1.29% for OSMF, 1% for Leukoplakia, and 0.47% for palatal lesions. In a hospital-based study done by Hazarey et al[7] in 2007, amongst 266418 patients prevalence of OSMF was 0.37%, and lichen planus was 0.7%. Erythroplakia 0.2% and Leukoplakia 4.8%. In a study done by Pratik et al[8] in 2015, amongst 10000 patients, the prevalence of Palatal lesions was 1.96%.
Tobacco consumption and smoking are seen in different socioeconomic groups, and this adverse habit is spread over urban and rural areas, giving rise to precancerous lesions and conditions. WHO has defined precancerous lesions as “a morphologically altered tissue in which oral cancer is more likely to occur than its normal counterpart”; a precancerous condition is ‘a generalized state associated with a significantly increased cancer risk[9]. Leukoplakia associated with chewing habits may possess a greater chance of malignant transformation[10]. Different studies vary the prevalence of various oral lesions and conditions in India[11,12]. Numerous studies have been conducted throughout India to determine the prevalence of precancerous lesions and diseases. Hence, a pooled estimate was synthesized, which gave the prevalence of precancerous lesions and conditions among tobacco users.
The title and details of this selected topic have been registered in PROSPERO (Reg. No. CRD42017062434). This systematic review was conducted according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement[13].
What is the prevalence of precancerous lesions and conditions among the Indian population?
Two authors (Kumbhalwar A and Shetiya SH) independently carried out the literature search. Disagreements on study inclusion, quality assessment, and data extraction were resolved by deliberation or by the third author (Kakodkar P). We searched databases such as PubMed, EMBASE, Web of Science, IndMED, Google Scholar, reports of the WHO South-East Asia Region, CDC tobacco reports, MOHFW India reports, Science Citation Index, WHO Index Medicus of the South-East Asian Region, Reference Citation Analysis (https://www.referencecitationanalysis.com/) and Open Grey. The following keywords were utilized to search PubMed: “a precancerous lesion”, “precancerous condition”, “prevalence”, and “India”, various combinations of the keywords were used for each precancerous lesion and condition to search Google Scholar, and the first 50 pages were screened for relevant and non-duplicated articles.
Similarly, various combinations of the keywords were used in each of the databases, and the same process was repeated. A set of journals was identified based on their propensity to publish articles on this topic. Each journal issue’s table of contents was then screened from the journal's inception till 31st January 2022 for relevant and non-duplicated articles. The cross-references of all selected papers were scanned for additional studies. Attempts were made to retrieve grey literature such as unpublished data, dissertations, and conference proceedings. To obtain publicly inaccessible data, a minimum of two email requests were sent to the corresponding author. If more than one article was published in a study, the article that provided the most updated data was selected.
Population or community-based observational epidemiological studies were included. Hospital-based studies assessed oral health, precancerous lesions, and conditions due to risk factors like tobacco and alcohol. Epidemiological studies that provided inadequate information for calculating prevalence, prevalence mentioned in letters to the editor, short communication, and reviews were excluded. Studies that gave prevalence separately for smokers, chewers, and those with mixed habits were not included. Classification of precancerous lesions and conditions by WHO (1978)[14] was used for classifying lesions as leukoplakia, erythroplakia, palatal lesions in reverse smokers, and conditions as oral submucous fibrosis actinic keratosis, lichen planus, and discoid lupus erythematosus.
Data were extracted and calculated concerning the prevalence of the precancerous lesions and conditions from the various studies that met the inclusion criteria. Studies that gave a prevalence of white lesions were considered leukoplakia. Combined prevalence was taken for studies recording oral health status and treatment needs. The highest prevalence was considered for tobacco and alcohol users. The review’s objective was to report the point estimate and pooled estimate of lesions and conditions. We carried out a qualitative and quantitative analysis of the observations.
A total of 5 domains were assessed mainly, study characteristics (author, year of publication, study design) were collected, as well as population variables (sample size, gender, age, and related etiological factors), OPMD features (clinical diagnosis), and outcome measures (prevalence of OPMD). The maximum possible score was 8, and studies scoring 6-8 were classified as high quality, 3-5 as moderate, and less than or equal to 2 were categorized as low-quality studies. Two reviewers (Kumbhalwar A and Shetiya SH) independently conducted quality assessments with any disagreement resolved by consensus (Table 1).
| Domain | Criteria |
| Examination | 0-Not mentioned |
| 1-Others (Nurse, ENT doctor, Medical officer, Health worker etc.) | |
| 2-by dentist | |
| Study settings | Community setting (field); Hospital setting. |
| Clinical examination | 0-Not mentioned |
| 1-Visual screening (Tongue blade, Illumination) | |
| 2-Mouth mirror | |
| Sampling technique | Detailed description of the sampling strategy used, type of sampling (random or non-random) was determined. |
| 0-Not mentioned | |
| 1-Non-random | |
| 2-Random sampling | |
| Sample size adequacy | If description of sample size calculations was not done, the relative precision was calculated (assuming simple random sampling) from the study sample size and estimated proportion. |
| Relative precision was ≤ 20% of the point estimate | |
| 0-Relative precision > 20% of the point estimate | |
| (e.g., If the precision of a study varied from 8%-28% for different lesions and conditions in the mouth, prevalence of more than 20% was considered and score 0 was given) |
The meta-analysis was performed using Open_Meta_Analyst software using the random effect method. We assumed that the estimates from various reviewed studies arose from different populations. The effect size of interest was the prevalence of the respective lesion and condition which developed. A given lesion/condition meta-analysis was conducted separately for community-based and hospital-based studies, and the pooled effect size was obtained. Sub-group analysis was performed to know the prevalence of lesion/condition before and after the Cigarette, and another Tobacco Product Act was implemented across various country regions (North, South, East, and West). Sixty-seven estimates were included from the North region, from South 170 estimates, from East 13 estimates, whereas 102 estimates were included in the review from the West region. Sensitivity analysis was also performed to know the prevalence amongst high, moderate, and low-quality studies. The community and hospital-based studies were pooled for the subgroup and sensitivity analysis. Heterogeneity was checked, and an I2 value of > 50% was considered evidence of heterogeneity. Statistical significance was set at a P value < 0.05.
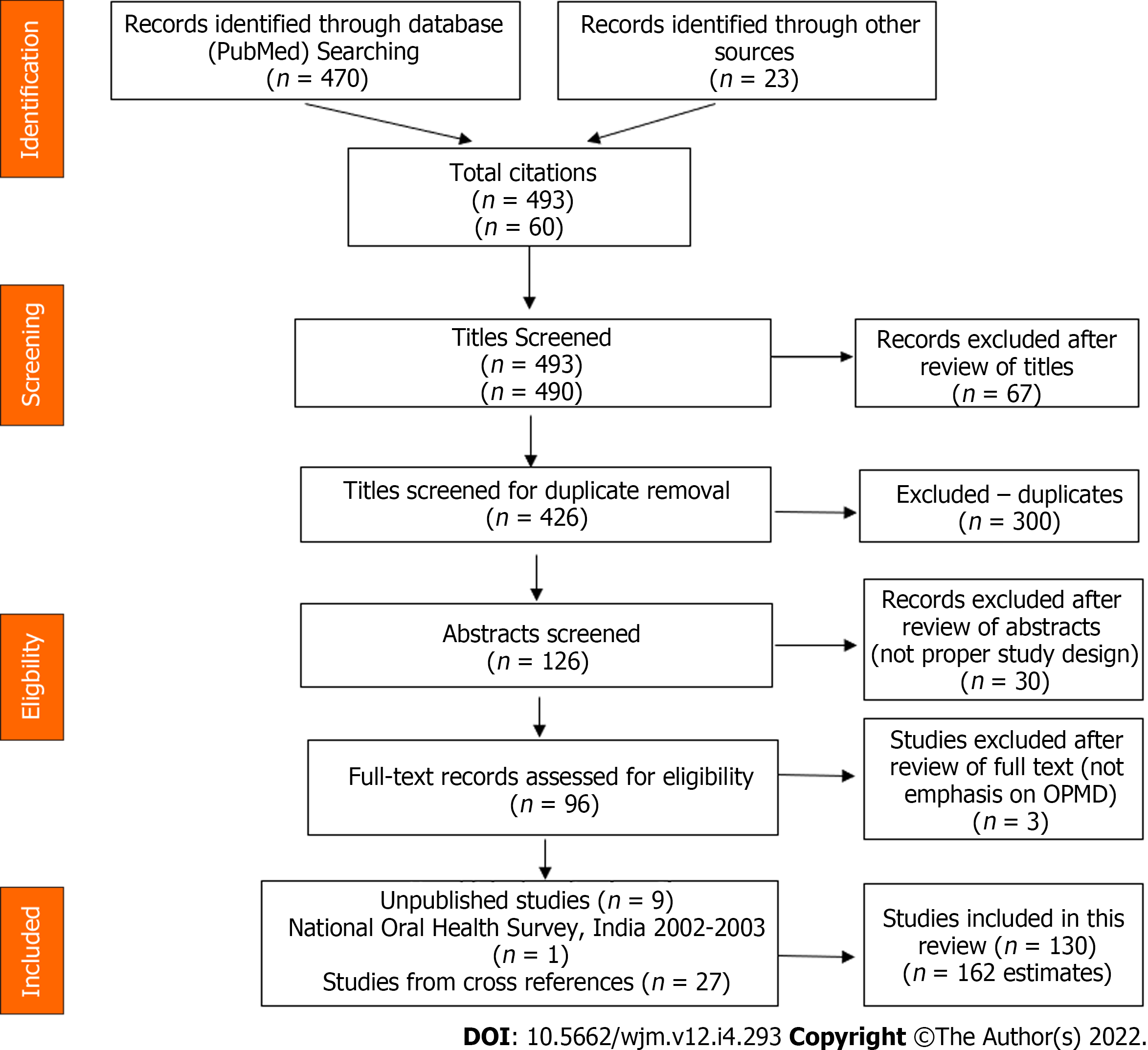
A total of 493 unique records were screened by title and abstracts (Figure 1). After full-text reading, three papers were excluded. This exclusion resulted in 130 full-text studies (162 estimates) plus nine unpublished records, one record from National Oral Health Survey, India (2002-2003), and 27 studies from cross-references were included. Few studies were split into a, b, c, etc., indicating the prevalence of lesion/condition within a study. For example, a. psychiatric and b. non-psychiatric inmates, a. fishermen, and b. non-fishermen etc. Actinic Keratosis and Discoid Lupus erythematosus considered in the review were not reported in any studies.
Age ranged from childhood to adulthood, and either gender and various states of India were considered. The prevalence of the precancerous lesions varied from 0.44%-73.8%, and the combined prevalence of oral precancerous lesions and conditions ranged from 2.79%-51.21%. One hundred sixty-two estimates from 130 community and hospital-based studies yielded 52 high, 71 moderate, and seven low-quality studies. Prevalence of lesions and conditions was estimated for various country regions, classified as North, South, East, and West.
A random-effect model was used for meta-analysis as the population from different states, age groups, and gender consuming varied types of smokeless tobacco and smoking were included. The point estimate for various lesions and conditions are given in Table 2.
| Precancerous lesions and conditions (Event/n) | No of estimates included | Point prevalence (95%CI) | I2(%) |
| LKP1 (16828/901715) | 92 | 4.3 (4.0-4.6) | 99.47 |
| LKP2 (23090/653349) | 46 | 6.7 (6.0-7.3) | 99.74 |
| LKP3 (39918/1555064) | 138 | 4.9 (4.7-5.2) | 99.65 |
| ERP1 (223/20,164) | 12 | 1.2 (0.7-1.7) | 94.97 |
| ERP2 (1112/275674) | 6 | 2.5 (0.4-4.5) | 99.15 |
| ERP3 (1335/295838) | 18 | 1.4 (1.0-1.7) | 97.91 |
| PL1 (4353/488610) | 16 | 5.8 (4.4-7.2) | 99.49 |
| PL2 (8148/57951) | 19 | 11.5 (8.0-15.0) | 99.81 |
| PL3 (12501/546561) | 35 | 8.9 (7.4-10.3) | 99.77 |
| OSMF1 (9229/749768) | 50 | 2.7 (2.5-3.0) | 99.18 |
| OSMF2 (8160/487272) | 38 | 4.5 (4.2-4.9) | 99.58 |
| OSMF3 (17389/1237040) | 88 | 3.4 (3.2-3.6) | 99.43 |
| LP1 (2759/233782) | 48 | 1.1 (0.9-1.2) | 97.59 |
| LP2 (3811/50300) | 25 | 7.5 (5.3-9.6) | 99.92 |
| LP3 (6570/627947) | 73 | 1.2 (1.1-1.3) | 98.14 |
Heterogeneity was high. Sub-group analysis provided effect size for multiple lesions and conditions before and after COTPA (2003) was enacted and different Indian regions. The studies published before 2003 showed a lower prevalence of the lesions and diseases than those carried out after 2003 (Table 3).
| Period of study | LKP (95%CI) (Estimates) | ERP (95%CI) (Estimates) | PL (95%CI) (Estimates) | OSMF (95%CI) (Estimates) | LP (95%CI) (Estimates) |
| ≤ 2003 | 3.2 (2.5-4.0) (15) | No study; (0) | 5.2 (-3.2-13.6); (2) | 0.6 (0.4-0.7); (13) | 0.6 (0.2-1.0); (4) |
| > 2003 | 5.5 (5.2-5.9); (123) | 1.4 (1.0-1.7); (18) | 9.2 (7.5-10.8); (33) | 4.7 (4.4-5.0); (75) | 1.3 (1.1-1.4); (69) |
Prevalence of Lichen Planus was highest in the North region, whereas Leukoplakia, Erythroplakia, Palatal lesion, and Oral submucous fibrosis in the Western part of India (Table 4).
| Regions | East (95%CI) (Estimates) | West (95%CI) (Estimates) | North (95%CI) (Estimates) | South (95%CI) (Estimates) |
| LKP | 4.4 (1.9-6.9) (7) | 8.4 (7.7-9.1) (44) | 5.2 (4.6-5.8) (24) | 3.4 (3.0-3.8) (63) |
| ERP | One study (1) | 3.5 (2.1-5.0) (4) | 2.9 (-1.5-7.2) (3) | 1.0 (0.5-1.5) (10) |
| PL | No study (0) | 16.9 (5.0-28.7) (5) | 6.2 (2.4-10.0) (10) | 8.1 (6.4-9.8) (20) |
| OSMF | 3.4 (2.1-4.6) (2) | 5.1 (4.7-5.4) (34) | 1.4 (1.0-1.8) (15) | 4.7 (4.2-5.3) (37) |
| LP | 5.0 (1.2-8.7) (3) | 1.2 (1.0-1.5) (15) | 1.7 (1.2-2.3) (15) | 1.0 (0.7-1.2) (40) |
High-quality studies showed a higher prevalence of Erythroplakia, Palatal lesion in reverse smokers. OSMF except for Leukoplakia and lichen planus, seen in moderate quality studies (Table 5).
| Study quality (Studies) | LKP (95%CI) | ERP (95%CI) | PL (95%CI) | OSMF (95%CI) | LP (95%CI) |
| High (52) | 4.6 (4.2-5.0) | 1.6 (0.9-2.3) | 11.0 (8.2-13.8) | 4.0 (3.6-4.4) | 1.1 (0.9-1.3) |
| Moderate (71) | 6.6 (5.9-7.2) | 1.6 (0.5-2.7) | 8.2 (5.2-11.2) | 3.3 (3.0-3.5) | 1.3 (1.1-1.5) |
| Low (7) | 1.4 (0.9-1.8) | One study | One study | 2.8 (1.3-4.3) | No study |
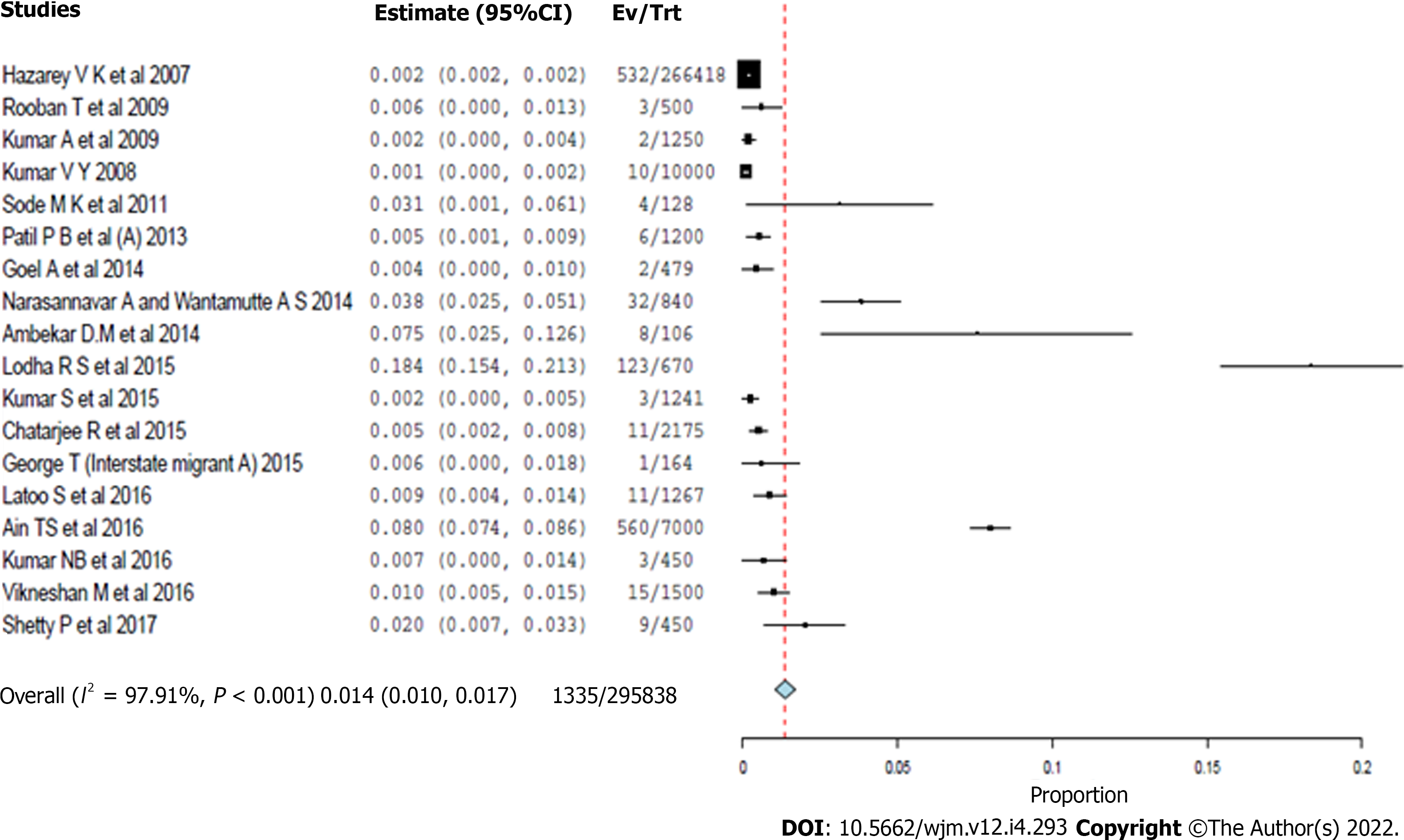
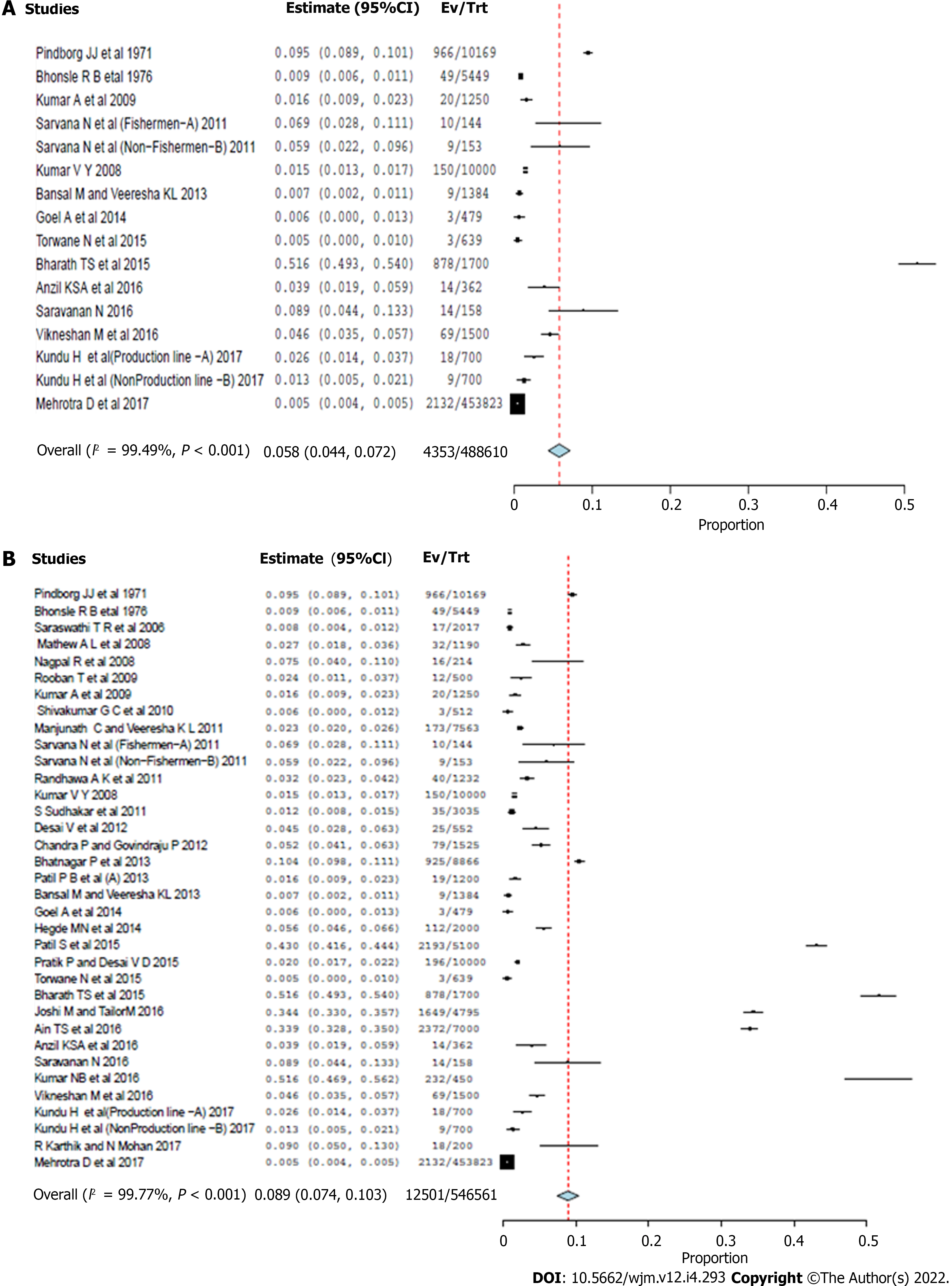
Pooled community and hospital-based studies, studies with high and moderate quality, and studies undertaken after COTPA was enacted showed similar effect sizes around 1.4%-1.6% (Figure 2). Meta-analysis showed an effect size between 8.1-9.2% amongst the moderate quality studies in the southern region, pooled studies, and after COTPA enactment (Figure 3A). Hospital-based studies, high-quality studies, and sand studies reflections from the western and northern parts showed larger effect sizes with wide confidence intervals (Figure 3B).
Most of the studies in the review were carried out in the Southern states of India. For those studies where oral health assessment was the primary objective, the authors used WHO-Oral Health Assessment Proforma 1986, 1997, or 2013. Eighty-one field surveys were assessed, and 49 studies were exclusively done in the hospital setting, while most community and hospital-based studies were undertaken after 2003. Since there was no uniformity in the definition and classification of lesions and conditions, the chance of bias in determining the prevalence could be prevailing in the considered observational studies.
More than 50% prevalence of all precancerous lesions and disorders was reported in specific population groups like fishermen and urban/rural populations who are tobacco consumers or slum dwellers or patients reporting to a dental college general population.
It was observed that the prevalence was higher amongst mine laborers, industrial workers, institutionalized elderly, chewers, jail inmates, fishermen, sex workers, tribes, and laborers in community-based studies. Most of the included studies have reported the prevalence of leukoplakia, unlike the other lesions and conditions.
Hospital-based studies, moderate quality records, and studies undertaken after COTPA was enacted showed a similar effect size of around 6%. Available estimates on the affordability of SLT products have indicated that they have become more affordable in India from 2001-to 2007[3]. However, the pooled estimate and the high-quality studies and those studies done in the northern region show an effect size of around 5%. This indicates that the prevalence of leukoplakia is around 5%-6%, and the effect sizes show a narrow confidence interval.
Hospital-based studies by Hazarey et al[7] and Kumar et al[15] conducted amongst 266418 and 25400 patients indicated a 4.8% and 6.16% prevalence for leukoplakia which is in concordance with this meta-analysis effect size. The risk factors that may cause oral leukoplakia include tobacco smoking (especially for localized leukoplakia), heavy alcohol consumption, and areca nut use. SLT lesions are caused by contact with tobacco-containing caustic agents. Early lesions are reversible and are usually resolved when the habit is discontinued. True leukoplakia has substantial potential to develop into cancer. It should be biopsied to rule out dysplasia[16]. Retail prices are generally lower for SLT products in low-income and low-middle-income countries and higher in high-income countries[3].
It was observed in the review that the prevalence of erythroplakia is higher in slum dwellers and prisoners. Erythroplakia showed an effect size of 1.2% for the community-based studies, which is lower than hospital-based studies. Pooled community and hospital-based studies, studies with high and moderate quality, and studies undertaken after COTPA was enacted showed similar effect sizes around 1.4%-1.6%. However, the western region’s hospital-based studies estimates and analyses show an effect size of around 2.5%-3.4%. The prevalence of erythroplakia was about 1.4%-1.6%, as indicated by the narrow confidence interval. Studies carried out by Hazarey et al[7] and Kumar et al[15] amongst 266418 and 10000 study populations showed the prevalence of erythroplakia to be 0.2%-0.1% in concordance with the present meta-analysis effect size. Erythroplakia offers dysplastic features and often presents as “carcinoma in situ” at the time of biopsy. Heavy alcohol consumption and tobacco use are known to be important etiological factors[17,18]. Implementation of the ban on SLT Advertisement, Promotion, and Sponsorship status over high SLT burden Parties such as in India, is poor and exposure to SLT advertisements and promotion among adults is more elevated than smoked products[3], which is a deterrent to the cause of lesion and condition.
The probable cause of lichen planus from the growing database of information about this disorder suggests specific immune responses, stress, and viral infection[19]. Though tobacco is not an etiological factor, it was part of the WHO classification and considered here. It was observed in the review that the prevalence is higher in the geriatric population. High and moderate-quality community-based studies in India's southern and western regions and those conducted after 2003 showed similar effect sizes with narrow confidence intervals. The prevalence of Lichen planus could be around 1%. Community-based studies done by Smith et al[20] and Kvv et al[5] amongst 57518 and 46579 people showed a prevalence of 0.63%-2.02%, which is in concordance with the present meta-analysis, which has indicated an effect size of 1.1 %.
The review suggests that the prevalence is higher in jail inmates. Hospital-based studies, studies with high quality, those done in India's southern and western region, and those undertaken after COTPA was enacted showed a similar effect size, around 4-5%, with a narrow confidence interval. Community-based studies, pooled studies, and studies with moderate quality showed a similar effect size of 3%. Studies were done by Kumar et al[15], and Mehrotra et al[6] amongst 25400 and 453823 study populations showed a prevalence of 1.29%, which is not in concordance with the present meta-analysis result, whereas 3.96%, which is in concordance with the current meta-analysis effect size. In southeast Asia, SLT is often mixed with areca nut, betel leaf, slaked lime, and spices, and these preparations are strongly associated with SMF, a fibrotic precancerous condition[21].
In India, some states and union territories have been relatively successful in enforcing the ban on gutkha. However, the tobacco industry is circumventing these bans by selling pan masala and tobacco in separate pouches. Successive GATS surveys in India in 2010 and 2017 revealed a significant reduction in the prevalence of SLT use in the general adult population[3]. As of 2016-2017, there has been a 1% reduction in the percentage of the adult population using Gutkha in India[4].
This disorder is specific to populations who smoke with the lighted end of the cigarette inside the mouth, resulting in red, white, or mixed palate lesions[14]. Few studies reported palatal lesions in reverse smokers, showing a wide variation of prevalence from 0.9%[22]. 51.77%[23] from Goa and Andhra Pradesh amongst community-based studies. Fishers of Andhra Pradesh showed a higher prevalence. Meta-analysis showed an effect size between 8.1-9.2% amongst the moderate quality studies in the southern region, pooled studies, and after COTPA enactment. However, hospital-based studies, high-quality studies, and sand studies reflections from the western and northern parts showed larger effect sizes with wide confidence intervals. Studies were done by Mehrotra et al[6] and Pindborg et al[24] amongst 453823, and 10169 study populations showed a prevalence of 0.47%, which is not by the present meta-analysis result and 9.5%, which is in concordance with the current meta-analysis effect size.
Smoking prevalence in low and middle-income countries is projected to decline slower than in high-income countries[2]. There is a possibility of worldwide tuberculosis rates falling as much as 20% if smoking is eliminated[25]. 68% and 17% of cigarette and bidi smokers purchased loose cigarettes and bidis. On average, the expenditure incurred during the last purchase was Rs 30 and Rs 12.5, respectively, making the purchase easy for a commoner[4].
Precancerous lesions and conditions are prevailing problems among the Indian population. It is mainly due to tobacco use, the smokeless form of tobacco. The meta-analysis indicates that hospital-based studies have a higher effect size of 6.7% than community-based studies, which show an effect size of 4.3%. Based on the present meta-analysis, the prevalence of leukoplakia is around 5%-6%. The majority of erythroplakia in community-based studies is lower (1.2%) than in hospital-based studies. The prevalence of erythroplakia in the current meta-analysis is 1.4-1.6%, as indicated by the narrow confidence interval. The prevalence of lichen planus seems to be higher (7.5%) for hospital-based studies than for community-based studies. The prevalence of Lichen planus is around 1%. The prevalence of oral submucous fibrosis seems higher (4.5%) for hospital-based studies than for community-based studies. The prevalence of oral submucous fibrosis was around 4%-5%. Compared to hospital-based studies, most Palatal lesions in community-based studies are lower (5.8%). Meta-analysis showed an effect size between 8.1%-9.2% amongst the moderate quality studies. Knowing these risk factors paved the way for more effective prevention of these pre-cancerous conditions. Patients who have already developed this condition may be advised to reduce their exposure to this risk factor to prevent the disorder from progressing further. Early intervention is essential to effective prevention. Thus, necessary efforts should be implemented.
World Health Organization (WHO) assessment estimated that by 2020 tobacco-related death may exceed 1.5 million annually or 13% of all deaths in India. Tobacco consumption and smoking are seen in different socioeconomic groups, and this adverse habit is spread over urban and rural areas, giving rise to precancerous lesions and conditions. Prevalence of various oral lesions and conditions in India are varying in different studies. Numerous studies have been conducted throughout India to determine the prevalence of precancerous lesions and conditions.
Tobacco consumption and smoking are seen in different socioeconomic groups, and this adverse habit is spread over urban and rural areas, giving rise to precancerous lesions and conditions. Different studies vary the prevalence of various oral lesions and conditions in India. So we were interested in compiling the data of precancerous lesions and conditions.
The objective of the present systematic literature review was to investigate a pooled estimate, which gave the prevalence of precancerous lesions and conditions among tobacco users in India population.
Systematic search was conducted for population or community-based observational epidemiological studies in PubMed, EMBASE, Web of Science, IndMED, Google Scholar, reports of the WHO South-East Asia Region, MOHFW India reports, Science Citation Index, WHO Index Medicus of the South-East Asian Region, Reference Citation Analysis (https://www.referencecitationanalysis.com/) and Open Grey from the earliest available up to 31st January 2022. The effect size was calculated for the prevalence of precancerous lesions and conditions.
One hundred sixty-two estimates from 130 studies yielded 52 high, 71 moderate, and seven low-quality studies from 823845. Point estimate based on cross-sectional studies for leukoplakia was 4.3% (95%CI: 4.0-4.6), oral submucous fibrosis was 2.7% (95%CI: 2.5-3.0), palatal lesions in reverse smokers and nicotine palatine were 5.8% (95%CI: 4.4-7.2), and Erythroplakia was 1.2% (95%CI: 0.7-1.7), and lichen planus was 1.1% (95%CI: 0.9-1.2). Amongst hospital-based studies, the pooled prevalence for Leukoplakia was 6.7% (95%CI: 6.0-7.3), oral submucous fibrosis was 4.5% (95%CI: 4.2-4.9), lichen planus was 7.5% (95%CI: 5.3-9.6), and erythroplakia was 2.5% (95%CI: 0.4-4.5), and palatal lesions in reverse smokers and nicotine palatini were 11.5% (95%CI: 8.0-15.0). The meta-analysis indicates that hospital-based studies have a higher effect size of 6.7% than community-based studies, which show an effect size of 4.3%. Based on the present meta-analysis, the prevalence of leukoplakia is around 5%-6%. The prevalence of erythroplakia in community-based studies is lower (1.2%) than in hospital-based studies.
Precancerous lesions and conditions are prevailing problems among the Indian population. It is mainly due to tobacco use, the smokeless form of tobacco. The meta-analysis indicates that hospital-based studies have a higher effect size of 6.7% than community-based studies. Patients who have already developed this condition may be advised to reduce their exposure to the risk factor to prevent the condition from progressing further.
Knowing these risk factors paved the way for more effective prevention of these pre-cancerous conditions. Patients who have already developed this condition may be advised to reduce their exposure to this risk factor to prevent the disorder from progressing further. Early intervention is essential to effective prevention. Thus, necessary efforts should be implemented.
| 1. | Murray CJ, Lopez AD, eds. The global burden of disease is a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and 2020. Cambridge, Massachusetts: Harvard School of Public Health, 1996. |
| 2. | World Health Organisation. WHO report on the global tobacco epidemic, 2017: monitoring tobacco use and prevention policies. Available from: https://www.who.int/publications/i/item/9789241512824. |
| 3. | Mehrotra R, Sinha DN, Szilagyi T. Global smokeless tobacco control policies and their implementation. 2018. Available from: https://www.researchgate.net/publication/324825055_GLOBAL_SMOKELESS_TOBACCO_CONTROL_POLICIES_AND_THEIR_IMPLEMENTATION. |
| 4. | GATS-2 Global Adult Tobacco Survey FACT SHEET | INDIA 2016-17. https://ntcp.nhp.gov.in/assets/document/surveys-reports-publications/GATS-2-FactSheet.pdf. |
| 5. | Kvv P, Javali SB, Rajesh G, Ariga J. An Epidemiological Study of Oral Mucosal Lesions in Karnataka State, India. J Indian Acad Oral Med Radiol. 2004;1:9-18. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (3)] |
| 6. | Mehrotra D, Kumar S, Mishra S, Mathur P, Pandey CM, Pandey A, Chaudhry K. Pan masala habits and risk of oral precancer: A cross-sectional survey in 0.45 million people of North India. J Oral Biol Craniofac Res. 2017;7:13-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Hazarey VK, Erlewad DM, Mundhe KA, Ughade SN. Oral submucous fibrosis: study of 1000 cases from central India. J Oral Pathol Med. 2007;36:12-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 111] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 8. | Pratik P, Desai VD. Prevalence of habits and oral mucosal lesions in Jaipur, Rajasthan. Indian J Dent Res. 2015;26:196-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 9. | World Health Organization. Report of a meeting of investigators on the histological definition of precancerous lesions. Geneva: World Health Organization, 1973, Can ⁄731. |
| 10. | Gangadharan P, Paymaster JC. Leukoplakia--an epidemiologic study of 1504 cases observed at the Tata Memorial Hospital, Bombay, India. Br J Cancer. 1971;25:657-668. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 34] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Mehta FS, Gupta PC, Daftary DK, Pindborg JJ, Choksi SK. An epidemiologic study of oral cancer and precancerous conditions among 101,761 villagers in Maharashtra, India. Int J Cancer. 1972;10:134-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 76] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Saravanan N, Reddy CVK, Veeresh DJ. A study to assess the oral health status and treatment needs of fishermen population in coastal region of Tamil Nadu. J Indian Association Public Health Dent. 2011;9:266-277. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15040] [Cited by in RCA: 16732] [Article Influence: 1521.1] [Reference Citation Analysis (1)] |
| 14. | Kramer IR, Lucas RB, Pindborg JJ, Sobin LH. Definition of leukoplakia and related lesions: an aid to studies on oral precancer. Oral Surg Oral Med Oral Pathol. 1978;46:518-539. [PubMed] |
| 15. | Kumar S, Debnath N, Ismail MB, Kumar A, Badiyani BK, Dubey PK, Sukhtankar LV. Prevalence and Risk Factors for Oral Potentially Malignant Disorders in Indian Population. Adv Prev Med. 2015;2015:208519. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 16. | Srivastava R, Jyoti B, Pradhan D, Siddiqui Z. Prevalence of oral submucous fibrosis in patients visiting dental OPD of a dental college in Kanpur: A demographic study. J Family Med Prim Care. 2019;8:2612-2617. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 17. | Sciubba JJ. Oral cancer. The importance of early diagnosis and treatment. Am J Clin Dermatol. 2001;2:239-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 150] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 18. | Duvvi SK, Thomas L, Vijayanand S, Reddy KT. Two-week rule for suspected head and neck cancer. A study of compliance and effectiveness. J Eval Clin Pract. 2006;12:591-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Kurago ZB. Etiology and pathogenesis of oral lichen planus: an overview. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122:72-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 140] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 20. | Smith LW, Bhargava K, Mani NJ, Malaowalla AM, Silverman S Jr. Oral cancer and precancerous lesions in 57,518 industrial workers of Gujarat, India. Indian J Cancer. 1975;12:118-123. [PubMed] |
| 21. | Nair U, Bartsch H, Nair J. Alert for an epidemic of oral cancer due to use of the betel quid substitutes gutkha and pan masala: a review of agents and causative mechanisms. Mutagenesis. 2004;19:251-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 256] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 22. | Bhonsle RB, Murti PR, Gupta PC, Mehta FS. Reverse dhumti smoking in Goa: an epidemiologic study of 5449 villagers for oral precancerous lesions. Indian J Cancer. 1976;13:301-305. [PubMed] |
| 23. | Naveen-Kumar B, Tatapudi R, Sudhakara-Reddy R, Alapati S, Pavani K, Sai-Praveen KN. Various forms of tobacco usage and its associated oral mucosal lesions. J Clin Exp Dent. 2016;8:e172-e177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Pindborg JJ, Mehta FS, Gupta PC, Daftary DK, Smith CJ. Reverse smoking in Andhra Pradesh, India: a study of palatal lesions among 10,169 villagers. Br J Cancer. 1971;25:10-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 49] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Drope J, Schluger N, Cahn Z, Drope J, Hamill S, Islami F, Liber A, Nargis N, Stoklosa M. The Tobacco Atlas. Atlanta: American Cancer Society, and vital strategies (6th ed.), 2018. |
| 26. | Pindborg JJ, Reichart PA, Smith CJ, Van der Waal I. World Health Organization International Histological Classification of Tumours. Histological typing of cancer and precancer of the oral mucosa. Berlin: Springer, 1997. |
| 27. | Warnakulasuriya S, Johnson NW, van der Waal I. Nomenclature and classification of potentially malignant disorders of the oral mucosa. J Oral Pathol Med. 2007;36:575-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 858] [Cited by in RCA: 983] [Article Influence: 51.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Batyrbekov K, Kazakhstan; Haile D, Ethiopia S-Editor: Ma Y L-Editor: A P-Editor: Cai YX