Published online Jan 20, 2022. doi: 10.5662/wjm.v12.i1.54
Peer-review started: June 10, 2021
First decision: July 31, 2021
Revised: August 5, 2021
Accepted: December 2, 2021
Article in press: December 2, 2021
Published online: January 20, 2022
Processing time: 220 Days and 14.5 Hours
Obsessive-compulsive disorder (OCD) is a heterogeneous disease in many respects and exhibits this diversity in terms of phenomenology. It also displays several different characteristics in children compared to adults.
To describe the socio-demographic and phenomenological features of children with OCD and to investigate the impact of these features on response to pharmacotherapy.
This retrospective study was carried out with 150 children and adolescents who had been diagnosed with OCD between 2014 and 2018. Data was collected by examining the files of the patients with diagnosis of OCD and similar disorders from the hospital database. Yale-Brown Obsessive-Compulsive Scale for Children was used for the assessment of obsession-compulsion subtypes. The Clinical Global Impression (CGI) scale was used to evaluate the severity of the disease (CGI-S) and global improvement (CGI-I). The predictors of treatment response were evaluated using linear regression analysis. The level of significance for all statistic tests was set as P < 0.05.
The sample was divided into prepubertal (44%) and adolescent (56%) age groups. The most prevalent obsessions were contamination and aggression obsessions, and the most frequent compulsions were washing and checking. While contamination was observed more commonly in the prepubertal age group, the religious obsession was seen more frequently in adolescents. Patients with aggression obsession presented a higher frequency of comorbid anxiety (P = 0.022) and mood (P = 0.047) disorder. CGI-I scores did not differ according to phenomenological subgroups (P > 0.05). A lower CGI-I score was linked to a lower CGI-S score (95% confidence interval 0.21-0.39, P < 0.001) and the prepubertal age of admission (95% confidence interval 0.03-0.87, P = 0.020).
The phenomenology of OCD shows differences depending on the age group and the comorbid psychiatric disorders. Earlier identification and treatment of OCD may help to prevent the impairment of the mental health of children and adolescents.
Core Tip: We aimed to analyze the socio-demographic and phenomenological features of children and adolescents with obsessive-compulsive disorder and to investigate the impact of these features on the pharmacotherapy response. Contamination was the commonest obsession, and washing-cleaning was the most common compulsion. The type of obsession varied with the age group: Contamination was seen more frequent in prepubertal age group, whereas the religious obsessions in adolescents. Aggression obsession was associated with the comorbid anxiety disorders and depression. The treatment response deteriorated with the increase in severity of disease and the age of admission. No difference was observed between the phenomenological subgroups in case of treatment response.
- Citation: Cifter A, Erdogdu AB. Phenomenology of obsessive-compulsive disorder in children and adolescents: Sample from a tertiary care center in Istanbul, Turkey. World J Methodol 2022; 12(1): 54-63
- URL: https://www.wjgnet.com/2222-0682/full/v12/i1/54.htm
- DOI: https://dx.doi.org/10.5662/wjm.v12.i1.54
Obsessive-compulsive disorder (OCD) is a neuropsychiatric disorder characterized by recurrent, unwanted thoughts (obsessions) and rituals to reduce anxiety (com
In contemporary psychiatric terminology, the term phenomenology is used to describe the symptoms and signs of diseases[3]. As a disorder with heterogeneous features in many respects, OCD also shows its variability and diversity in terms of phenomenological features, which are affected by many structural and environmental factors, and shows several different characteristics in children compared to adults. Rosario-Campos et al[4] stated that aggression, sexual and religious obsessions are more common in adults, whereas symmetry-ordering obsession/compulsions are more common in the pediatric age group. In addition, comorbid psychiatric disorders have been associated with some phenomenological subgroups. While mood and anxiety disorders accompany aggression obsession more frequently, it is reported that symmetry-ordering obsession and compulsions are more common in patients with tic disorders[5].
Whilst phenomenology is affected by multifactorial components, it also plays an essential role in the treatment response of OCD. However, there are contradictory results in the literature about which subgroup responds better to treatment[6]. In clinical practice, some subgroups benefit from selective serotonin reuptake inhibitors (SSRI) and clomipramine, whereas some groups need an antipsychotic augmentation in treatment[7].
In this study, we aimed to analyze the socio-demographic and phenomenological features of children and adolescents with OCD and to investigate the influence of these features on the pharmacotherapy response.
This research was conducted in the Marmara University School of Medicine, which houses the largest child and adolescent psychiatry clinic on the Asian side of Istanbul, Turkey. The study was carried out retrospectively by examining the files of the emergency and outpatient clinics of the Child and Adolescent Psychiatry Department.
For our research, files of patients with International Classification of Diseases-10 diagnostic code F42 and refractions (OCD and similar disorders) were collected from the hospital database from a total of 88710 outpatient and 3896 emergency /consultation admissions between 2014 and 2018. There was totally 1516 applications belonging to 642 patients, and the patient files were overviewed systematically according to date of admission to the clinic. Out of the files overviewed, 153 could not be accessed due to problems in file archiving, and 101 patients were excluded since the diagnostic criteria of Diagnostic and Statistical Manual of Mental Disorders, 5th Edition for OCD were not fully met[1]. Also, the information in another 238 patient files was not taken into consideration due to lack of data. Finally, a total of 150 children and adolescents fully meeting the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition criteria were included in the study.
At least one drug treatment (SSRI, clomipramine, second generation antipsychotics) had been given to 118 (78.7%) children who had applied for at least two follow-up interviews, and seven of the children who started drug treatment discontinued the follow-up. One hundred and eleven children under medication continued their follow-up for an average of 5.5 mo. Children who had not used any psychotropic drugs received supportive psychotherapy.
The data were collected through Patient Follow-Up Form from patient records. Obsession and compulsion subgroups were established based on the Yale-Brown Obsessive-Compulsive Scale for Children[8]. Obsessions such as the need to know or remember, fear of saying certain things, fear of not saying just the right thing, intrusive images and sounds were evaluated under the heading of “miscellaneous obsessions” in Yale-Brown Obsessive-Compulsive Scale for Children. Also, compulsions such as mental rituals, the need to tell, ask or confess, the need to take precautions to prevent damage to himself/herself and others, and the need to touch, tap or rub were evaluated as “miscellaneous compulsions.”
Clinical Global Impression (CGI), one of the most commonly used clinician rated tools in psychiatry, measures the severity of the disease with CGI-S and the global improvement with CGI-I. The CGI-S score ranges from 1 (normal, not at all ill) to 7 (among the most extremely ill patients), and the CGI-I assesses the improvement from 1 (much improved) to 7 (much worse), which was recorded at the last interview following the treatment[9].
SPSS 20.0 for Windows (IBM, 2011, Armonk, NY, United States) was used during the statistical analyses. The Shapiro-Wilk test was used to evaluate the normality of data distribution. Parametric variables were analyzed with Pearson’s χ2 or Fisher’s exact test, independent samples t test, one-way analysis of variance, and for the non-parametric variables Kruskal-Wallis and Mann-Whitney U tests were used. The predictors of treatment response were evaluated using linear regression analysis. The level of all significance for all statistical tests was set as P < 0.05.
The study protocol was conducted in keeping with the code of ethics of the Declaration of Helsinki and was approved by the Marmara University School of Medicine Clinical Research Ethics Committee (Protocol No: 09.2019.360, date: April 5, 2019). Written informed consent was obtained from parents or legal guardians of the patients.
A total of 150 children, with a mean age of admission to the clinic of 11.90 ± 3.02 (min: 4, max: 17) and a mean age of onset of symptoms of 11.01 ± 3.36 (min: 3, max: 17), participated in our study. As the age of onset of the symptoms was in congruence with the age of admission and was prone to recall bias, we divided the study group into prepubertal/childhood (44.0%) and postpubertal/adolescent (56.0%) age groups based on the age at admission and accepted the onset of puberty as 12 years of age. The socio-demographic and clinical characteristics of the children are shown in Table 1. The socio-demographic features such as parental educational and employment status were similar in terms of sex (P > 0.05).
| Socio-demographic characteristics | Prepubertal | Postpubertal | Overall | Statistical analysis |
| n (%) | n (%) | n (%) | ||
| Sex (male) | 40 (60.6) | 43 (51.2) | 83 (55.3) | χ2 = 1.326, P = 0.250 |
| Educational level of mother | ||||
| Secondary school and lower | 24 (32.9) | 40 (54.1) | 73 (49.7) | χ2 = 6.704, P = 0.0101 |
| High school and above | 49 (67.1) | 34 (45.9) | 74 (50.3) | |
| Employment status of mother | 16 (24,6) | 13 (15.5) | 29 (19.5) | χ2 = 1.953, P = 0.162 |
| Educational level of father | ||||
| Secondary school and lower | 20 (35.1) | 44 (51.2) | 57 (39.9) | χ2 = 3.583, P = 0.058 |
| High school and above | 37 (64.9) | 42 (48.8) | 86 (60.1) | |
| Employment status of father | 63 (96.9) | 67 (82.7) | 130 (89.0) | χ2 = 7.459, P = 0.0061 |
| Parents live together | 62 (93.9) | 73 (86.9) | 135 (90.0) | χ2 = 2.032, P = 0.154 |
| Consanguinity | 13 (19.7) | 21 (25.0) | 34 (22.7) | χ2 = 0.593, P = 0.441 |
| Mental disorder in 1st degree relatives | 24 (36.4) | 29 (34.5) | 53 (35.3) | χ2 = 0.055, P = 0.815 |
| Comorbid psychopathology | 48 (72.7) | 53 (63.1) | 101 (63.3) | χ2 = 1.559, P = 0.212 |
| Anxiety disordersa | 22 (33.3) | 29 (34.5) | 51 (34.0) | χ2 = 0.023, P = 0.879 |
| Disruptive behavioral disordersb | 23 (34.8) | 18 (21.4) | 41 (27.3) | χ2 = 3.351, P = 0.067 |
| Neurodevelopmental disordersc | 20 (30.3) | 16 (19.0) | 36 (24.0) | χ2 = 2.567, P = 0.109 |
| Mood disorders (major depressive disorder) | 1 (1.5) | 6 (7.1) | 7 (4.7) | χ2 = 2.631, P = 0.105 |
| mean ± SD | ||||
| Age gap between mother and father | 3.34 ± 2.75 | 4.54 ± 4.18 | 4.00 ± 3.26 | t = -1.736, P = 0.085 |
| Birth order | 1.69 ± 0.86 | 2.17 ± 1.37 | 1.95 ± 1.19 | t = -2.444, P = 0.0161 |
In the year prior to the admission, 35.3% of the children had experienced a stressful life event, which included the death of one of the nuclear or extended family members (10.7%), material loss (8.0%), serious illness of themselves or family members (8.0%), moving to another place (7.3%), an accident (3.3%) and parental divorce (0.7%). Before admission to our clinic, 22.0% of the children had been admitted to a mental health professional due to OCD, and 20.0% had shown psychiatric symptoms other than OCD. Out of all participants, 35.3% of the first-degree relatives had a history of psychiatric disorder, the most prominent of these being major depressive disorder (19.3%), which was followed by OCD and panic disorder (both 7.5%).
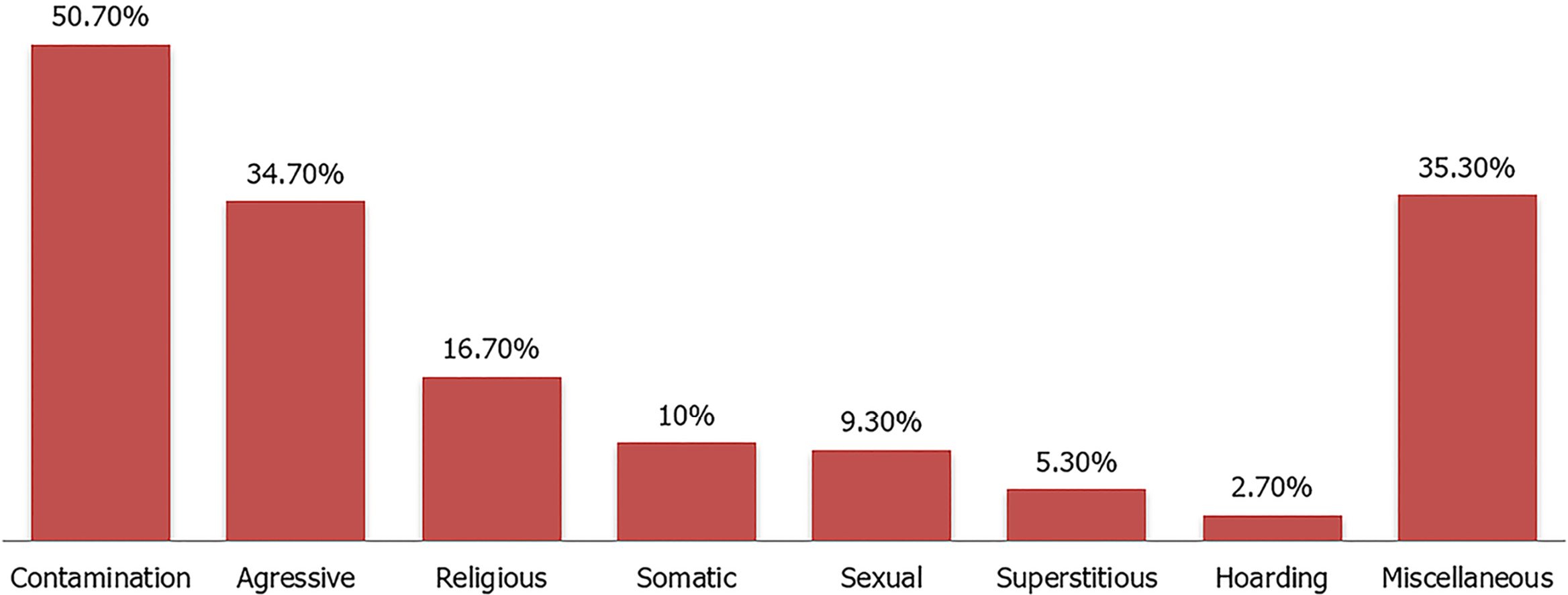
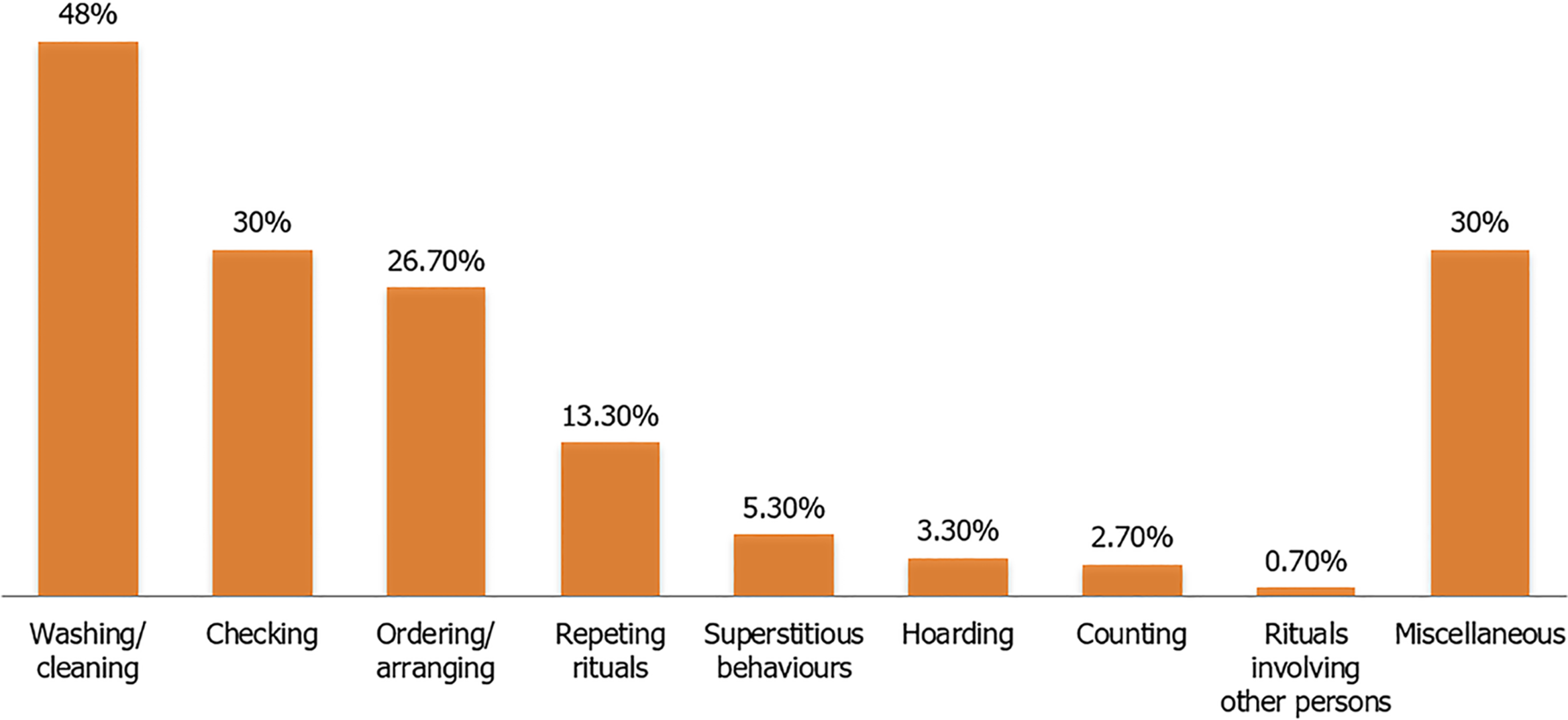
While 96.6% of the children had an obsession and 88.0% had a compulsion, 55.3% had more than one obsession, and 47.3% had more than one compulsion. The patterns of obsessions are shown in Figure 1 and compulsions are shown in Figure 2. There was no difference in the phenomenological subgroups between females and males (P > 0.05). Contamination obsessions were observed more commonly in the prepubertal age group (χ2 = 4.658, P = 0.031), whereas religious obsessions were more common in adolescents (χ2 = 7.013, P = 0.008). There was no variance in compulsions and other obsessions according to age group (P > 0.05). In terms of stressful life events, aggression obsession was observed more frequently in children who had recently lost one of their family members (χ2 = 3.684, P = 0.05), and superstitious obsession was more common in children who had recently been in or witnessed an accident (χ2 = 12.312, P = 0.023). Ordering-arranging compulsion was found to be more common in children who had moved in the last year (χ2 = 4.718, P = 0.03).
In respect of comorbid psychiatric disorders, patients with aggression obsession presented a higher frequency of comorbid anxiety disorders (χ2 = 5.239, P = 0.022) and major depressive disorder (P = 0.047, Fisher’s exact test). Ordering-arranging compulsion was seen less frequently in children with comorbid disruptive behavior disorders (χ2 = 6.042, P = 0.014).
The baseline CGI-S and post-treatment CGI-I scores are shown in Table 2. A positive, moderately strong and statistically significant correlation was found between CGI-S and CGI-I scores (r = 0.443, P < 0.001). The CGI-I scores of the adolescents were higher than children (t = -2.231, P = 0.027), but there was no significant difference between CGI-S scores of age groups (t = -0.894 P = 0.373). While CGI-S scores were higher (t = 2.342, P = 0.021) in children with superstitious behaviors (mean: 4.42 ± 0.53) compared to those without (mean: 3.20 ± 1.37), CGI-I scores did not differ according to phenomenological subgroups (P > 0.05).
In the linear regression analysis, the CGI-S score and the age of admission were found to be the parameters that predicted the CGI-I score (Table 3).
| Independent variables | Non-standardized coefficients | Standardized coefficients | P | Confidence interval 95% | t | |
| β | Standard error | β | ||||
| CGI-S | 0.259 | 0.070 | 0.289 | < 0.001 | (0.121)-(0.397) | 3.719 |
| Age of admission1 | 0.507 | 0.238 | 0.165 | 0.035 | (0.036)-(0.878) | 2.127 |
| R = 0.336; F = 9.347; P < 0.001; Durbin-Watson = 1.925 | ||||||
To the best of our knowledge, this study is the largest from Turkey concerning the phenomenology of pediatric OCD. Also, the study data was derived from a child and adolescent psychiatry clinic in a tertiary university hospital rather than a specialized clinic for OCD and therefore should be more representative of all pediatric OCD patients. So, ranging from mild to moderate, all severity levels of OCD, including treatment-resistant patients, were represented in the sample, suggesting that the findings could be broadly applied to OCD.
In the present study, the most common obsession was contamination, followed by miscellaneous, aggression and religious obsessions, and the most common compulsions were washing/cleaning, control, the miscellaneous category and ordering-arranging. Many studies worldwide also indicated contamination as the commonest obsession and cleaning as the commonest compulsion[10-12]. However, some researchers revealed symmetry-ordering as the most prevalent phenomenological subgroup[4,13], whereas Bryńska and Wolańczyk[14] described aggression as the most frequent obsession in adolescents. There was no sex difference between phenomenological subgroups in our study. Despite that, Tanidir et al[15] reported more contamination and somatic obsessions in males by using another diagnostic tool (K-SADS-PL) on 110 children and adolescents in Istanbul. Mataix-Cols et al[16] found in their study in the United States that hoarding was common in girls, while sexual obsessions were more common in boys. The variance in results of such studies may be due to the wide range of age and methodologies and the cultural differences.
Regarding age group, contamination obsessions were related to prepubertal age group, whereas religious obsessions to adolescent age group. Consistent with our findings, studies conducted with children and adults asserted that contamination obsessions were seen in earlier ages[17], and religious obsessions were more apparent in older ages[15,18-19]. Exceptionally, Albert et al[20] related religious obsessions in adult OCD patients with the disease onset before the age of ten. Considering that the concepts of abstract thought and religion in children become more elaborated during adolescence, it is expected that religious obsessions would be seen more frequently in this period.
During our follow-up, approximately two-thirds of the children were diagnosed with a psychiatric disorder other than OCD, and the most common comorbid disorder was anxiety disorders (34.0%). Similar pediatric OCD studies also reported high rates of comorbidity, and the commonest comorbid mental disorders were defined as anxiety disorders, attention deficit/hyperactivity disorder, and tic disorder[14,16,21]. Among the phenomenological subgroups, variations in terms of comorbidities were observed, and the aggressive obsession was more frequently seen in children with anxiety and mood disorders. Studies conducted in Western and Asian countries have related anxiety disorder with aggressive symptomatology of OCD[5,22-23]. Also, Storch et al[24] observed daily functional impairment in the presence of either comorbid anxiety disorder or aggressive obsessions in children with OCD. Additionally, we observed nearly one-third of the children had a history of psychiatric disorder in their first-degree relatives. In other studies, the rate of psychiatric family history in childhood-onset OCD cases varied from 35%-45%[13,25], and the earlier age of onset of symptoms has been strongly associated with the familiality of the disorder[26].
In the light of our results, the treatment response deteriorated with the increase in severity of disease and the age of admission. Congruent with our results, Masi et al[27] highlighted that a better response to SSRIs is related to less severe illness in pediatric OCD. In a systematic review, early pharmacotherapeutic intervention was found to be the most remarkable indicator of treatment response in pediatric OCD[28]. Notwithstanding, some researchers did not find a significant relationship between age of onset/admission and response to pharmacotherapy in children with OCD[29,30]. Furthermore, in our study group maternal educational level and paternal employment level were found significantly higher in the prepubertal age group, which are supposed to be critical protective factors for a child’s mental health and might be associated with better therapy outcomes.
Between the phenomenological subgroups, no difference was observed in case of treatment response. Results of the studies concerning which single subgroup responds better to SSRIs are controversial[29,31], and this may be due to the heterogeneous nature of the disorder. Therefore, in future studies, response to pharmacotherapy of OCD symptoms in children and adolescents should be examined in homogeneous subgroups with a dimensional approach rather than in single phenomenological groups.
There are also some limitations to the study. First, some of the children were excluded from the study due to lack of data, failure to meet the diagnostic criteria and problems in file archiving, all of which limited the number of participants. Second, retrospective data collection from the files might cause reporting bias. Third, due to its nature, the sample might have some ascertainment biases such as medication discontinuation due to fear of stigmatization, type of responders to SSRIs in terms of OCD phenomenology, family characteristics, and underlying neuropathology, etc. Lastly, data concerning the children who dropped-out would provide a comparison of the results with the follow-up group and could strengthen our results.
In the present study, it has been shown that obsessive-compulsive disorder in children and adolescents show their heterogeneity in terms of phenomenology. There are variations in the phenomenology of obsessions depending on the age group and comorbid mental disorders. During the follow-up of pediatric OCD patients, comorbid psychiatric disorders associated with certain phenomenological subgroups should be considered. The response to pharmacotherapy was associated with a younger age of admission and lower severity of disorder, which emphasizes the value of therapeutic interventions in the early stages of the disease in order to limit the impairment of social functioning and prevent the development of secondary mental disorders in adulthood.
As a disease with heterogeneous features in many respects, obsessive-compulsive disorder (OCD) shows variability in terms of phenomenology.
Phenomenology of obsessions and compulsions are affected by many structural and environmental factors and shows several different characteristics in children compared to adults.
To identify the most common phenomenological subgroups of pediatric OCD and to determine the relationship of these subgroups with familial and clinical characteristics of children and the treatment response.
Data of 150 children and adolescents, who had been diagnosed with OCD between 2014 and 2018, were examined retrospectively.
Contamination obsession was observed more frequently in the prepubertal age group, whereas religious obsessions were more frequent in adolescents. The treatment response deteriorated with the increase in severity of disease and the age of admission.
Variations in phenomenology of obsessions are found in terms of age groups. The response to pharmacotherapy was found to be better in patients in the prepubertal age group and with lower severity of disease.
Earlier diagnosis and therapeutic interventions in OCD may limit the impairment of mental health of children and adolescents.
The authors would like to thank all the children and their families whose participation made this study possible.
| 1. | American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Publishing, 2013. [RCA] [DOI] [Full Text] [Cited by in Crossref: 66101] [Cited by in RCA: 61331] [Article Influence: 3607.7] [Reference Citation Analysis (5)] |
| 2. | Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11472] [Cited by in RCA: 12117] [Article Influence: 577.0] [Reference Citation Analysis (1)] |
| 3. | Beşiroğlu L. Obsesif kompulsif bozuklukta fenomenoloji: tedavi yanıtı için önemli mi? Psikiyatr Güncel. 2014;4:221-229. |
| 4. | Rosario-Campos MC, Miguel EC, Quatrano S, Chacon P, Ferrao Y, Findley D, Katsovich L, Scahill L, King RA, Woody SR, Tolin D, Hollander E, Kano Y, Leckman JF. The Dimensional Yale-Brown Obsessive-Compulsive Scale (DY-BOCS): an instrument for assessing obsessive-compulsive symptom dimensions. Mol Psychiatry. 2006;11:495-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 321] [Cited by in RCA: 320] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 5. | Hasler G, LaSalle-Ricci VH, Ronquillo JG, Crawley SA, Cochran LW, Kazuba D, Greenberg BD, Murphy DL. Obsessive-compulsive disorder symptom dimensions show specific relationships to psychiatric comorbidity. Psychiatry Res. 2005;135:121-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 181] [Article Influence: 8.6] [Reference Citation Analysis (1)] |
| 6. | Beşiroğlu L. Understanding treatment response and resistance in obsessive compulsive disorder in the context of cognitive neuropsychological model. Turk Psikiyatri Derg. 2016;27:204-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Nazeer A, Latif F, Mondal A, Azeem MW, Greydanus DE. Obsessive-compulsive disorder in children and adolescents: epidemiology, diagnosis and management. Transl Pediatr. 2020;9:76-93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 8. | Yucelen AG, Rodopman-Arman A, Topcuoglu V, Yazgan MY, Fisek G. Interrater reliability and clinical efficacy of Children’s Yale-Brown Obsessive-Compulsive Scale in an outpatient setting. Compr Psychiatry. 2006;47:48-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 61] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 9. | Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry (Edgmont). 2007;4:28-37. [PubMed] |
| 10. | Deepthi K, Sagar Kommu JV, Smitha M, Reddy YCJ. Clinical profile and outcome in a large sample of children and adolescents with obsessive-compulsive disorder: A chart review from a tertiary care center in India. Indian J Psychiatry. 2018;60:205-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Diler RS, Avci A. Sociodemographic and clinical characteristics of Turkish children and adolescents with obsessive-compulsive disorder. Croat Med J. 2002;43:324-329. [PubMed] |
| 12. | Garcia AM, Freeman JB, Himle MB, Berman NC, Ogata AK, Ng J, Choate-Summers ML, Leonard H. Phenomenology of Early Childhood Onset Obsessive Compulsive Disorder. J Psychopathol Behav Assess. 2009;31:104-111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 47] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Güler AS, do Rosário MC, Ayaz AB, Gökçe S, Yulaf Y, Başgül S, Özcan Ö, Karabekiroğlu K, Munir K, Beşiroğlu L, Yazgan Y. Psychometric properties of the DY-BOCS in a Turkish sample of children and adolescents. Compr Psychiatry. 2016;65:15-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 14. | Bryńska A, Wolańczyk T. Epidemiology and phenomenology of obsessive-compulsive disorder in non-referred young adolescents: a Polish perspective. Eur Child Adolesc Psychiatry. 2005;14:319-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (1)] |
| 15. | Tanidir C, Adaletli H, Gunes H, Kilicoglu AG, Mutlu C, Bahali MK, Aytemiz T, Uneri OS. Impact of gender, age at onset, and lifetime tic disorders on the clinical presentation and comorbidity pattern of obsessive-compulsive disorder in children and adolescents. J Child Adolesc Psychopharmacol. 2015;25:425-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Mataix-Cols D, Nakatani E, Micali N, Heyman I. Structure of obsessive-compulsive symptoms in pediatric OCD. J Am Acad Child Adolesc Psychiatry. 2008;47:773-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 98] [Article Influence: 5.4] [Reference Citation Analysis (1)] |
| 17. | Hunt C. Differences in OCD symptom presentations across age, culture, and gender: A quantitative review of studies using the Y-BOCS symptom checklist. J Obsessive Compuls Relat Disord. 2020;26:100533. [DOI] [Full Text] |
| 18. | Geller DA, Biederman J, Faraone S, Agranat A, Cradock K, Hagermoser L, Kim G, Frazier J, Coffey BJ. Developmental aspects of obsessive compulsive disorder: findings in children, adolescents, and adults. J Nerv Ment Dis. 2001;189:471-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 190] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 19. | Tek C, Ulug B. Religiosity and religious obsessions in obsessive-compulsive disorder. Psychiatry Res. 2001;104:99-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 62] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Albert U, Manchia M, Tortorella A, Volpe U, Rosso G, Carpiniello B, Maina G. Admixture analysis of age at symptom onset and age at disorder onset in a large sample of patients with obsessive-compulsive disorder. J Affect Disord. 2015;187:188-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Ivarsson T, Melin K, Wallin L. Categorical and dimensional aspects of co-morbidity in obsessive-compulsive disorder (OCD). Eur Child Adolesc Psychiatry. 2008;17:20-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 85] [Article Influence: 4.7] [Reference Citation Analysis (1)] |
| 22. | Gallant J, Storch EA, Merlo LJ, Ricketts ED, Geffken GR, Goodman WK, Murphy TK. Convergent and discriminant validity of the Children’s Yale-Brown Obsessive Compulsive Scale-Symptom Checklist. J Anxiety Disord. 2008;22:1369-1376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 42] [Article Influence: 2.3] [Reference Citation Analysis (1)] |
| 23. | Viswanath B, Narayanaswamy JC, Rajkumar RP, Cherian AV, Kandavel T, Math SB, Reddy YC. Impact of depressive and anxiety disorder comorbidity on the clinical expression of obsessive-compulsive disorder. Compr Psychiatry. 2012;53:775-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (1)] |
| 24. | Storch EA, Larson MJ, Muroff J, Caporino N, Geller D, Reid JM, Morgan J, Jordan P, Murphy TK. Predictors of functional impairment in pediatric obsessive-compulsive disorder. J Anxiety Disord. 2010;24:275-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 119] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 25. | Mancebo MC, Garcia AM, Pinto A, Freeman JB, Przeworski A, Stout R, Kane JS, Eisen JL, Rasmussen SA. Juvenile-onset OCD: clinical features in children, adolescents and adults. Acta Psychiatr Scand. 2008;118:149-159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 67] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 26. | Nestadt G, Samuels J, Riddle M, Bienvenu OJ 3rd, Liang KY, LaBuda M, Walkup J, Grados M, Hoehn-Saric R. A family study of obsessive-compulsive disorder. Arch Gen Psychiatry. 2000;57:358-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 436] [Cited by in RCA: 387] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 27. | Masi G, Millepiedi S, Perugi G, Pfanner C, Berloffa S, Pari C, Mucci M. Pharmacotherapy in paediatric obsessive-compulsive disorder: a naturalistic, retrospective study. CNS Drugs. 2009;23:241-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 28. | Varigonda AL, Jakubovski E, Bloch MH. Systematic Review and Meta-Analysis: Early Treatment Responses of Selective Serotonin Reuptake Inhibitors and Clomipramine in Pediatric Obsessive-Compulsive Disorder. J Am Acad Child Adolesc Psychiatry. 2016;55:851-859.e2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 56] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 29. | Ginsburg GS, Kingery JN, Drake KL, Grados MA. Predictors of treatment response in pediatric obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry. 2008;47:868-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 85] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 30. | Nakatani E, Krebs G, Micali N, Turner C, Heyman I, Mataix-Cols D. Children with very early onset obsessive-compulsive disorder: clinical features and treatment outcome. J Child Psychol Psychiatry. 2011;52:1261-1268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 58] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 31. | Landeros-Weisenberger A, Bloch MH, Kelmendi B, Wegner R, Nudel J, Dombrowski P, Pittenger C, Krystal JH, Goodman WK, Leckman JF, Coric V. Dimensional predictors of response to SRI pharmacotherapy in obsessive-compulsive disorder. J Affect Disord. 2010;121:175-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 66] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Pasquini M S-Editor: Wu YXJ L-Editor: Filipodia P-Editor: Wu YXJ