Published online Jun 25, 2025. doi: 10.5527/wjn.v14.i2.104207
Revised: March 14, 2025
Accepted: March 25, 2025
Published online: June 25, 2025
Processing time: 117 Days and 14.2 Hours
Urologists are commonly consulted regarding difficult and traumatic urethral catheterizations. Complications surrounding Foley catheterizations represent a significant burden to the healthcare system.
To assess the demographic and patient characteristics surrounding urological consultation for difficult and traumatic Foley catheterizations at our institution across multiple hospitals.
This is a single-institution, multi-hospital, 263 patient, retrospective chart review from Jan 2020–December 2023.
The majority of consultations (80.2%) did not require heroic measures by the urology service. A Foley catheter placement was determined not difficult in the majority 191 (72.6%) of patients. Sub-group analysis of “difficult by urology” vs “not difficult by urology”, showed a significant difference between those with zero attempts, one attempt, and greater than one attempts (P = 0.004). Those patients specifically with greater than one attempts were more likely to be seen as a difficult insertion by urology assessment (60.6%) compared to not difficult (38.6%). Likewise, those patients with a history of difficult urethral catheter (DUC)/traumatic urethral catheterization (TUC) (25.8%) were more likely to be difficult compared to those without a history of DUC/TUC (14.2%) (P = 0.038).
The study found that majority of consultations received did not require heroic measures by the urology service to place a catheter. Patients who had a history of DUC/TUC and those who had greater than one catheter attempts were statistically more likely to be a DUC based on urology assessment. At our institution we hope to propose a protocol in which nursing staff and non-urologic clinicians will utilize a troubleshooting checklist and an algorithm when difficult or traumatic urethral catheters are encountered in order to improve patient care and decrease healthcare costs. For example, this protocol would ideally address complications of multiple catheter attempts such as urethral trauma, development of urethral strictures, and infection risk. Additionally, future trainings and availability of additional resources will be provided and assessed with a goal of reducing healthcare cost surrounding these complications.
Core Tip: We performed a single institution, retrospective review of 263 consultations for “difficult urethral catheter” or “traumatic urethral catheter”. The study found that of total consultations, 80.2% did not require heroic measures. A Foley catheter placement was determined not difficult in 73% of patients. Patients who had a history of difficult or traumatic catheter and those who had greater than one catheter attempts were statistically more likely to be a difficult urethral catheter. At our institution we hope to propose a protocol in which nursing staff will utilize a troubleshooting checklist and an algorithm when difficult urinary catheter or traumatic catheters are encountered to promote improved patient care.
- Citation: Sarver J, Farley R, Daugherty S, Bilbrew J, Palka J. Improving outcomes in foley catheterization: A retrospective review with a proposed protocol. World J Nephrol 2025; 14(2): 104207
- URL: https://www.wjgnet.com/2220-6124/full/v14/i2/104207.htm
- DOI: https://dx.doi.org/10.5527/wjn.v14.i2.104207
Urologists are commonly consulted regarding difficult and traumatic urethral catheterizations (TUC). An anatomic or structural abnormality is usually the culprit when placing a catheter into the bladder causing a difficult urethral catheter (DUC). Bleeding and/or injury to the urethra from TUC due to multiple failed catheter attempts can follow. Approximately 10%-25% of hospitalized patients undergo urethral catheterization[1]. A DUC may be due to anatomic challenges in male patients including: Urethral strictures, phimosis, or false passages[2]. In females, challenges exist in the post-menopausal setting due to intravaginal retraction of the urethral meatus[2]. Traumatic insertions occur after repeated failed attempts to cannulate the urethra and may lead to acute urinary retention, urosepsis, bleeding, acute kidney injury, and urethral strictures[3]. The incidence of TUC in hospitalized patient is approximately 13.4 per 1000 catheter attempts[3]. Complications of traumatic catheter insertion can include the development of urethral strictures. Prior studies quote a majority (78%) of patients developing urethral strictures after being seen for a TUC[3]. The associated healthcare costs of managing iatrogenic urethral injuries may translate to $371790 per patient[4]. These findings emphasize the need for developing solutions to decrease the complications surrounding catheterizations.
Prior to urology consultation, studies report an average of 1.6 catheter attempts by previous providers[5]. DUC is treated and managed based on the anatomic etiology. Most catheters can be successfully inserted using the appropriate exposure or with the use of different tip catheters (e.g. Coude catheter)[6]. In rare cases, the need of surgical placement of a urethral catheter via cystoscopy or insertion of a suprapubic tube can be completed by a trained urologist[6]. Approximately 41% of consultations received for difficult Foley placement do not require special interventions or maneuvers[7]. Protocols exist that can help health care professionals in different settings such as the emergency room or medical floor to improve success in catheter placement and better techniques in complex patients[8]. However, there is a lack of data surrounding the study of difficult and TUC and the requirement of consultation. Implementation of nursing protocols surrounding traumatic catheters may lead to decreased incidence of urethral injury[4]. Traumatic catheterization and inability to place a urethral catheter among nursing staff is common, with a need and desire for a protocol and education regarding catheterizations[9]. Prior studies highlight the success of designed protocols that combine an education program, catheter algorithm, and skilled nursing catheter nursing team and showed a reduction the frequency of catheter-associated trauma and procedures[10]. Although, there still remains a need in the literature for further studies regarding prevention, education, and awareness surrounding catheter management[7].
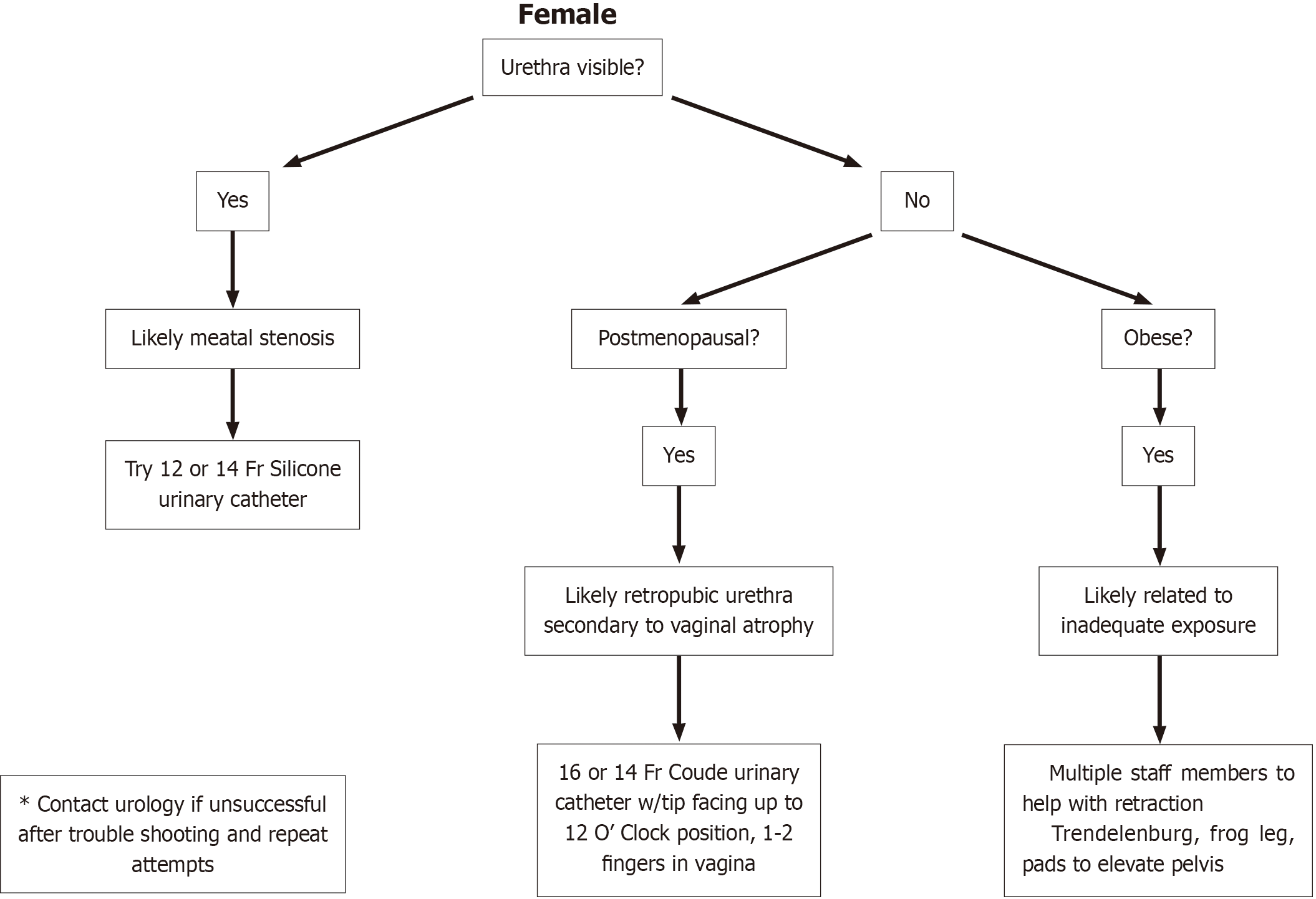
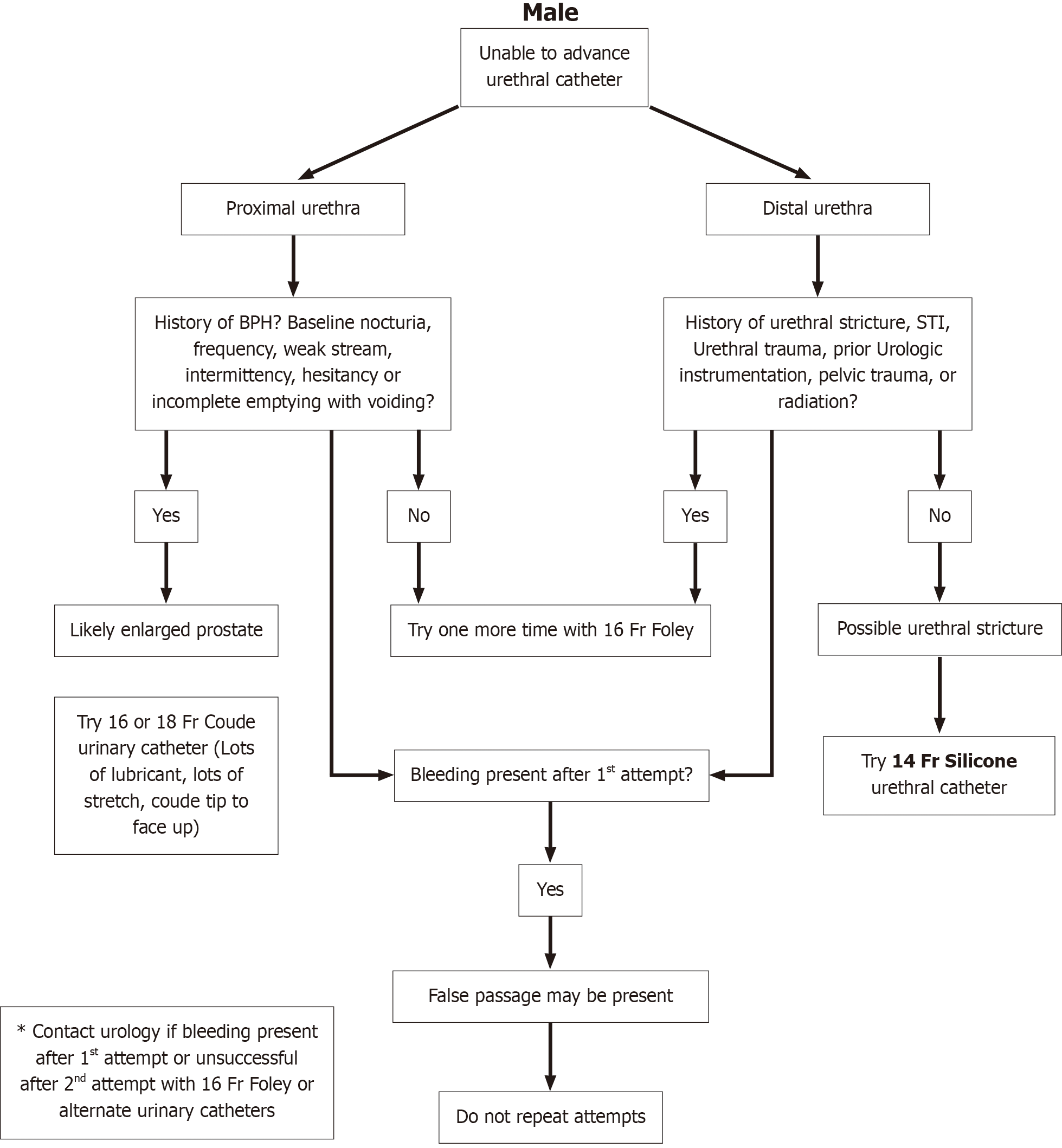
This study aimed to assess the demographic and patient characteristics surrounding urological consultation for difficult and traumatic Foley catheterizations at our institution across multiple hospitals. Future trainings and availability of additional resources at our institution will be added and assessed with a goal of reducing and preventing complications associated with these consultations. This will be accomplished by providing examples of algorithms for female (Figure 1) and male (Figure 2) difficult catheter insertions to the nursing staff at our institutions across different departments.
After institutional review board approval was given, retrospective chart review was performed over a three years period including 263 patients. Inclusion variables including either “difficult urethral catheter” or “traumatic urethral catheter” were queried. Patients that were included are those who were seen and consulted at our institutions during the data collection period for either difficult or traumatic catheterization as the consulting diagnosis. Included patients had a completed consultation note documenting the nature of the consult and the interventions or steps completed by the on call urologist. Additional information was obtained from the general information of each patient’s medical record. Descriptive variables of the patients were collected including age, biological sex, body mass index (BMI), and race by review of background information for those meeting inclusion criteria. Reason for consultation was collected and reported as either DUC, TUC, or both, based on the consultation diagnosis or order. DUC was defined as a consultation to the urology service for placement of Foley catheter where a nursing or physician noted difficulty on catheter insertion. TUC was defined as either gross hematuria or a malpositioned catheter. This information was detailed in the “history” portion of the consultation note during the history taking by the urologist. Data was collected including whether the urology team considered the foley catheter insertion difficult or if procedural techniques were needed. Difficulty was overall defined and determined by the need of bedside or operating room procedures for catheter insertion, or other means requiring urology assessment that a nursing staff or non-urological physician alike could not otherwise accomplish to insert the catheter. Information regarding operating or procedural intervention was collected from the “impression” and “plan” sections of the consultation note. Insertion of routine Coude catheter or 3-way port catheters were not considered difficult unless the consulting urologist required additional materials or procedural techniques. The type of catheter inserted by urology was also reported. The type of catheter was reported in either the “physical exam” or the “plan” portion of the consultation note.
Quality metrics were collected and reported as length of stay, development of catheter-associated urinary tract infection (CAUTI), and amount of prior nursing or non-urological physician attempts at catheter insertion prior to consultation. The length of stay was recorded by reviewing the current admission and discharge date of the patient based on when the consult was placed. CAUTI was recorded by reviewing the presence of positive urine cultures obtained from the patient during the hospitalization after the catheter was placed by the consulting urologist. Amount of catheter attempts by nursing were collected using the “history” portion of the consultation note. We collected patient data on history of prior difficult or traumatic catheter insertions that required a urology consult previously by reviewing the “history” portion of the consultation note or by reviewing prior consultation notes for the same patient by the urology service on a previous admission.
The responses were collected and reported using mean, medians, and standard deviations, where applicable. Statistical analyses were reported using SPSS software including Student’s t test, Fisher exact probability test, and χ² analyses.
A total of 263 consultations were reviewed during the study period of three years across six hospitals at a single institution. The average age of the patient population was 65.6 years, ranging from 18-99 years of age. The mean BMI of the patients is 27.9, ranging from 13-78. On average, 237 (90.1%) consultations were male and 26 (9.9%) were female patients. The background race of consultations was, on average, 147 (55.9%) African American, with an additional 75 (28.5%) being white, 9 (3.4%) being multiple races, 3 (1.1%) Cuban, 1 (0.4%) Hispanic, and 28 (10.6%) without documenta
| Total (n = 263) | Average | Range |
| Age (years) | 65.6 | 18-99 |
| BMI | 27.9 | 13-78 |
| Race | ||
| AA | 147 (55.9) | |
| Cuban | 3 (1.1) | |
| Hispanic | 1 (0.4) | |
| White | 75 (28.5) | |
| Multiple | 9 (3.4) | |
| Unknown | 28 (10.6) | |
| Sex | ||
| Male | 237 (90.1) | |
| Female | 26 (9.9) |
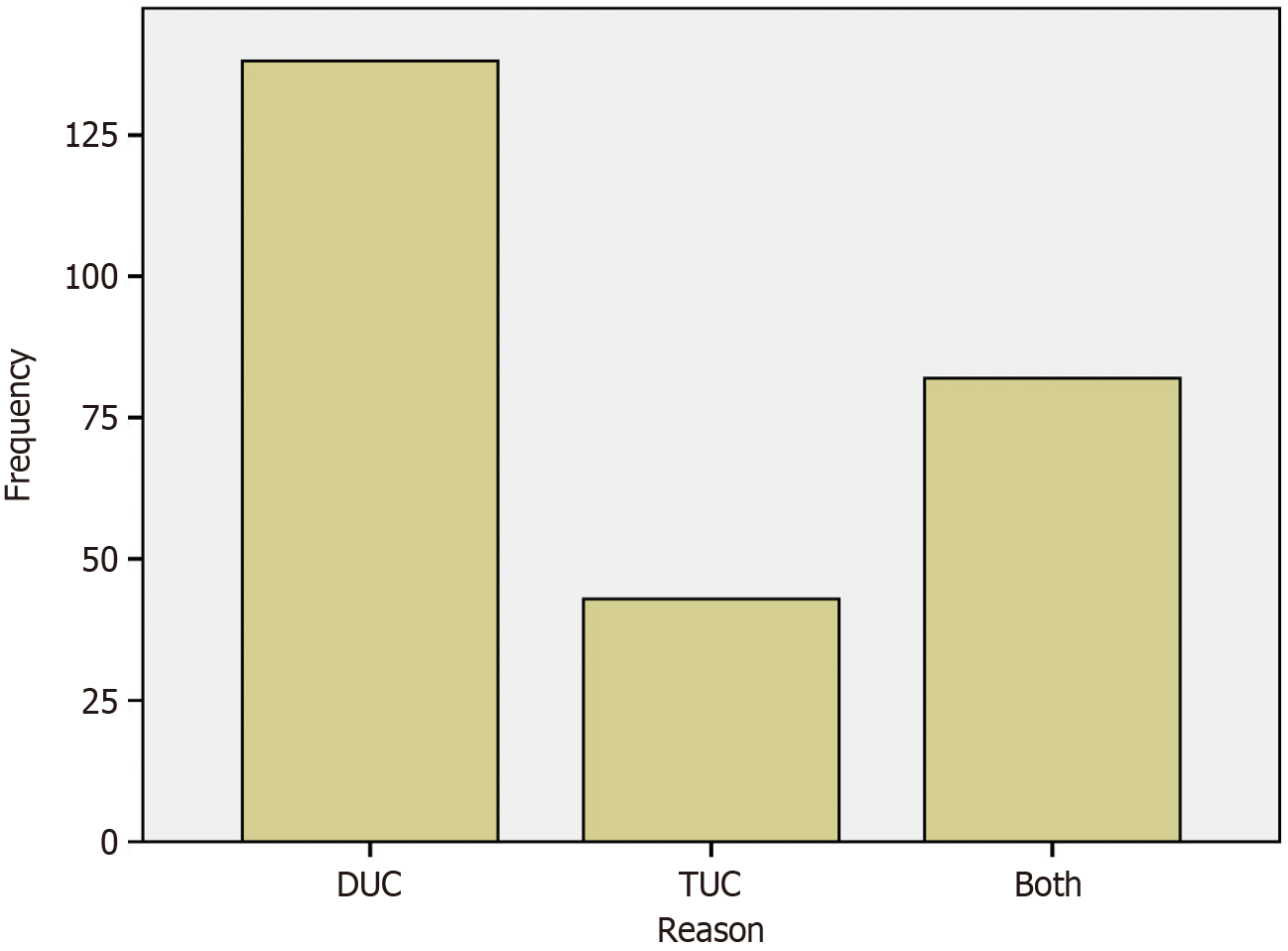
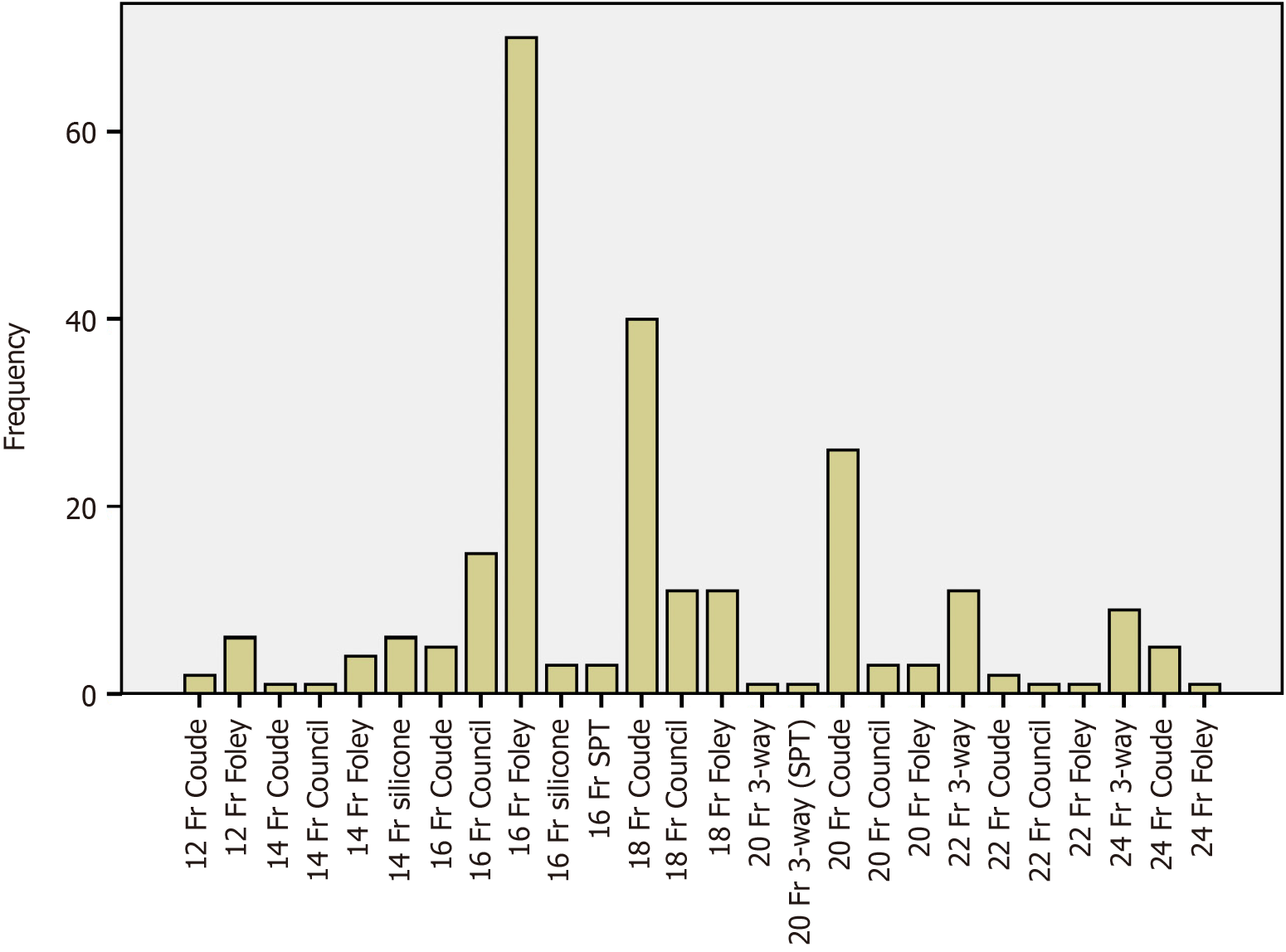
Overall, 138 (52.2%) consultations were for DUC, 43 (16.3%) for TUC, and 82 (31.2%) had both components of DUC and TUC (Figure 3). Of the total consultations, 211 (80.2%) did not require surgical intervention by the urology service with 50 (19.2%) requiring urologic intervention. A Foley catheter placement was determined difficult by the urology service in 66 (25.1%) of consultations and not difficult in the majority, 191 (72.6%) of patients, with 6 (2.3%) consultations not having proper documentation or assessment of catheter difficulty by urology. The type of Foley used most commonly by the treating urologist was 16 French (Fr) straight Foley (26.6%), followed by a 18 Fr Coude (15.2%), 20 Fr Coude (9.9%), 16 Fr Council tip (5.7%), 18 Fr Council (4.2%), 18 Fr straight Foley (4.2%), and 22 Fr 3-way catheter (4.2%), with 8.0% of catheter type not documented (Figure 4). A CAUTI was reported in 35 (13.3%) of patients and no evidence of CAUTI in 228 (86.7%) of patients.
Total catheter attempts before urology evaluation were documented as greater than one attempt in 114 (43.3%), one attempt in 113 (43.0%), and zero attempts in 33 (12.5%) patients, with three (1.1%) without documentation of catheter attempt number. The average length of stay for patients consulted was 15.6 days, median length of stay being 11.0 days, and ranged from 0-123 days. Prior history of DUC or TUC was documented for 45 (17.1%) of patients consulted and no prior history in 217 (82.5%) of patients, and one (0.4%) patient without documentation provided.
A sub-group analysis was obtained comparing demographic and clinical differences between the cohort of patients deemed “difficult by urology” vs “not difficult by urology” after catheter insertion and evaluation. There were no statistically significant differences between race, sex, and CAUTI between the two groups. When comparing the two groups with regards to catheter attempts, there was a significant difference between those with zero attempts, one attempt, and greater than one attempts (P = 0.004). Those patients specifically with greater than one attempts were more likely to be seen as a difficult insertion by urology assessment (60.6%) compared to not difficult (38.6%) across the other groups (Table 2). This translates to the cohort of patients who had greater than one catheter attempts were statistically more likely to be a DUC on urology assessment. This may be due to trauma to the urethra from multiple failed attempts that require better visualization via cystoscopy or from a prior urological history of the patient that requires urological assistance to place the catheter. In this study we did not consider prior urological history as a factor to study among patients included, which would be an additional interesting variable to consider in a future study. Likewise, those patients with a history of DUC/TUC (25.8%) were more likely to be difficult compared to those without a history of DUC/TUC (14.2%) after urology assessment (P = 0.038) (Table 2). Therefore, patients who had a history of DUC/TUC were more likely to be report as a DUC by the consulted urologist based on this sub-group analysis and statistically analysis. This is likely due to an underlying urological history requiring urological assistance to place the catheter however this is a factor that was not evaluated at this time.
| Difficult by urology | Not difficult by urology | Unknown | P value | |
| Total | 66 (25.1) | 191 (72.6) | 6 (2.3) | |
| Race | 33 (12.5) | 0.506 | ||
| AA | 34 (58.6) | 108 (62.8) | ||
| Cuban | 1 (1.7) | 2 (1.2) | ||
| Hispanic | 1 (1.7) | 0 (0) | ||
| White | 20 (34.5) | 55 (32) | ||
| Multiple | 2 (3.4) | 7 (4.1) | ||
| Sex | 6 (2.3) | 0.806 | ||
| Female | 5 (7.6) | 19 (9.9) | ||
| Male | 61 (92.4) | 172 (90.1) | ||
| CAUTI | 0.836 | |||
| Yes | 8 (12.1) | 27 (14.1) | 6 (2.3) | |
| No | 58 (87.9) | 164 (85.9) | ||
| Catheter attempt | 9 (3.4) | 0.004 | ||
| > 1 | 40 (60.6) | 72 (38.6) | ||
| 1 | 18 (27.3) | 92 (48.9) | ||
| 0 | 8 (12.1) | 24 (12.8) | ||
| History of DUC/TUC | 7 (2.7) | 0.038 | ||
| Yes | 17 (25.8) | 27 (14.2) | ||
| No | 49 (74.2) | 163 (85.8) |
This study was a single institution, retrospective review of 263 consultations placed to the urology service across several hospitals for either “difficult urethral catheter” or “traumatic urethral catheter.” The study found the patient population had an average age of 65, mostly male (90%), African American (55.9%), and an average BMI of 27.9. Of the total consultations, 211 (80.2%) did not require surgical intervention by the urology service. A Foley catheter placement was determined not difficult in the majority 191 (72.6%) of patients. Total catheter attempts before urology evaluation were documented as greater than one attempt in 114 (43.3%), one attempt in 113 (43.0%), and zero attempts in 33 (12.5%) patients. Prior history of DUC or TUC was documented for 45 (17.1%) of patients consulted and no prior history in 217 (82.5%) of patients. Those patients specifically with greater than one attempt were more likely to be seen as a difficult insertion compared to not difficult across the other groups (P = 0.004). Likewise, those patients with a history of DUC/TUC were more likely than those without a history of DUC/TUC to be assessed by the urology team as difficult (P = 0.038). We found that traumatic catheterization and inability to place a urethral catheter among nursing staff is common, with a need and desire for a protocol and education regarding catheterizations[9].
Bacsu et al[7] reported on a cohort of 81 patients assessed for DUC requiring urological consultation. Forty-one percent of consultations were classified as inappropriate based on successful placement of standard or Coude catheter by a urologist. In our study, 80.2% of DUC or TUC consultations did not require heroic measures by the urology service. Likewise, 73% of consultations for DUC or TUC were not difficult by the urology service assessment. At our institution we found that most catheter insertions could be performed without urological assistance. This may be due to a lack of education or improper technique with catheter placement in the consulting nurses or physicians, placing a need for further educational sessions surrounding routine catheter placement. If catheters can be successfully placed by the appropriate nurse or provider prior to urology consult this would save the patient multiple catheter attempts as well as decrease in healthcare costs as a result of trauma or potential complications[11]. Similar findings were addressed by Liu et al[12], who studied 81 consults at their tertiary care center. In 70% of cases, successful placement was achieved by the urology resident. However, 20% of patients required cystoscopy manipulation and 9% required suprapubic tube placement. Catheterization was achieved without adjunct procedures in the majority of consults[12]. These results support a treatment strategy in which all patients without a prior history of lower urinary tract pathology should undergo an initial placement attempt by the primary team or nurses prior to urology consult and encourage continued education by the nursing staff[12].
Additional findings of Bacsu et al[7] showed 17% of patients had a history of previous DUC and 65% had a previous urologic history. In our study, a prior history of DUC or TUC was documented for 17% of patients consulted. This value is similar between our studies however we did not consider prior urological history, which would be an additional interesting variable to consider in the future. Patients who had a history of DUC/TUC were more likely to be a DUC based on our sub-group analysis. This is likely due to underlying urological history requiring urological assistance to place the catheter. Additionally, a consultation to urology would be more likely in those with a prior urological history.
Prior studies quote that a majority (90%) of cases have an initial attempt at catheter placement prior to urology consult, with nurses being the most common health care workers to attempt insertion of the catheter[7]. In this study, greater than one catheter attempts were seen in 43% of patients and one attempt in 43% of patients, prior to urology assessment. Prior to urology consultation, studies report an average of 1.6 catheter attempts by previous providers.5 Interestingly, the zero attempts category in this study yielded a larger number of cases than expected. Prior studies show 6% of consultations are made in which not a single healthcare provider even attempted catheter placement[7]. Approximately 12.5% of patients were noted to have no attempt of catheter placement prior to urology consultation, in this study. This may be due to providers noticing a history of urological consultation and placing a consult proactively, which may be warranted. However, urological consultations may be placed without proper need or before attempts were made. Patients who had greater than one catheter attempts were statistically more likely to be a DUC on urology assessment, based on our sub-group analysis. As previously mentioned, this may be due to trauma to the urethra from multiple failed attempts that require better visualization via cystoscopy due to bleeding or from a prior urological history of the patient that requires urological assistance to place the catheter. Placement of a Foley catheter is a common procedure perform by nursing staff and physicians. Nurses and providers should be educated and equipped enough to otherwise place a non-difficult catheter. The increase in healthcare cost and consultation burden would likely increase if urology consults are placed out of ease without the need of a urologic practitioner[4,13].
Patient morbidity and healthcare costs regarding traumatic and difficult catheterization is significant. The nursing staff are usually the first to evaluate and attempt placement of the urethral catheters, making discussion regarding education and protocols important, especially among nursing staff. Prior studies by Laborde et al[14] have examined nurse driven Foley catheter protocols and have shown a decrease in catheter-associated trauma after implementation. Likewise, other studies report the need for further improvements in catheter training protocols to avoid iatrogenic complications due to the burden of patient morbidity and health care costs associated with urethral catheter injuries[15]. Some solutions exist and are currently being studied in the literature, such as those proposed by Hackett et al[16], suggesting implementation of a rapid response nurse driven training and proficiency programs to assist with decreasing Foley catheter complications. At our institution we hope to propose a protocol in which nursing staff and non-urologic clinicians will utilize a troubleshooting checklist when difficult urinary catheter or traumatic catheters are encountered. Prospectively, traumatic or DUC consults will be tracked at our hospitals before initiating protocol. A newly designed protocol will then be implemented at these hospitals to evaluate for reduction in DUC.
A limitation to this study is the retrospective nature of the data collection. Consultation documentation and assessment of difficulty differed on the chart reviewed depending on which resident or attending received the consultation, potentially leading to an observer bias. In future studies this could be more generalizable if all consultations were assessed by the same provider to help with similar assessments of difficulty, however this may limit patient case and consultation volume. Likewise, we would have preferred to have additional information on catheter trouble shooting during urological consultation. For example, we were not able to accurately assess the stepwise attempts of the difficult catheter insertion by the urologist consulted (i.e. if multiple catheters were tried before successful insertion) based on documentation limitations. Inclusion of the reason or indication for catheter insertion was not included in this study but would be an interesting topic to include in future projects. Lack of adjusting for confounding variables is an additional concern with the retrospective nature of the study. As this study did not include the topics of prior history, patient comorbidities, prior urological surgery, and other factors alike, the generalizability of the study is limited. Likewise, we would have, in hindsight, tried to limit confounding factors by assessing more of the patient’s prior urological history and compared this across the subgroups that were difficult vs not difficult based on urological assessment. These factors should be studied in future projects as prior urological history is an important factor in troubleshooting difficult Foley insertion when patients present to the hospital. Another limitation that may limit generalizability is the definition of a difficult Foley catheter. For this study, the insertion of a Coude catheter was not defined as difficult. Unless the assessment by urology specified the need for cystoscope or guidewire use for insertion, it was our decision and practice that nursing or non-urology staff can and should learn to place a Coude catheter without the need for consultation. Likewise, the emergency room staff at our institution routinely places 3-way hematuria catheters before consultation to urology therefore those consultations may be deemed not difficult if the catheter placement was without further need for surgical assistance. Our study did include a large volume of patients and provides statistically and clinically significant findings that are novel to medical practice and literature. A future prospective study surrounding difficult and traumatic catheters at our institution after implementation of protocol and trainings would help with generalizing these findings.
We performed a single institution, retrospective review of 263 consultations placed to the urology service for either “difficult urethral catheter” or “traumatic urethral catheter”. The study found that of the total consultations, 80.2% did not require heroic measures by the urology service. A Foley catheter placement was determined not difficult in 73% of patients. Patients who had a history of DUC/TUC and those who had greater than one catheter attempts were statistically more likely to be a DUC based on urology assessment. At our institution we hope to propose a protocol in which nursing staff and non-urologic clinicians will utilize a troubleshooting checklist and an algorithm when difficult urinary catheter or traumatic catheters are encountered in order to promote improved patient care. Our goal in this strategy would be to provide better nursing education through urology lead seminars on catheter placement and provide resources when troubleshooting difficult catheter insertions. We would ideally see improvement in healthcare costs by having less traumatic catheter insertions and the complications that result. Prospectively, traumatic or DUC consults will be tracked at our hospitals before initiating the protocol.
| 1. | Bhatt NR, Davis NF, Addie D, Flynn R, McDermott TED, Manecksha RP, Thornhill JA. Evaluating the cost of iatrogenic urethral catheterisation injuries. Ir J Med Sci. 2017;186:1051-1055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 2. | Ghaffary C, Yohannes A, Villanueva C, Leslie SW. A practical approach to difficult urinary catheterizations. Curr Urol Rep. 2013;14:565-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Davis NF, Bhatt NR, MacCraith E, Flood HD, Mooney R, Leonard G, Walsh MT. Long-term outcomes of urethral catheterisation injuries: a prospective multi-institutional study. World J Urol. 2020;38:473-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (1)] |
| 4. | Davis NF, Quinlan MR, Bhatt NR, Browne C, MacCraith E, Manecksha R, Walsh MT, Thornhill JA, Mulvin D. Incidence, Cost, Complications and Clinical Outcomes of Iatrogenic Urethral Catheterization Injuries: A Prospective Multi-Institutional Study. J Urol. 2016;196:1473-1477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 79] [Article Influence: 7.9] [Reference Citation Analysis (1)] |
| 5. | Villanueva C, Hemstreet GI. Difficult catheterization: tricks of the trade. AUA Update Ser. 2011;30 Lesson 5:41-48. |
| 6. | Beller HL, Greene KL. Difficult Foleys and Foley Difficulties. AUA Update Ser. 2023;42 Lesson 4:1-8. |
| 7. | Bacsu C, Van Zyl S, Rourke KF. A prospective analysis of consultation for difficult urinary catheter insertion at tertiary care centres in Northern Alberta. Can Urol Assoc J. 2013;7:343-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Willette PA, Coffield S. Current trends in the management of difficult urinary catheterizations. West J Emerg Med. 2012;13:472-478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Sarver J, Farley R, Daugherty S, Bilbrew J, Palka J. Proposal to decrease incidence, morbidity, and associated healthcare costs regarding difficult and traumatic urethral catheterization - a protocol for DMC hospitals: A pilot study. Can J Urol. 2023;30:11624-11628. [PubMed] |
| 10. | Dave C, Faraj K, Vakharia P, Boura J, Hollander J. Quality Improvement Foley Project to Reduce Catheter-Related Trauma in a Large Community Hospital. J Healthc Qual. 2018;40:51-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Kashefi C, Messer K, Barden R, Sexton C, Parsons JK. Incidence and prevention of iatrogenic urethral injuries. J Urol. 2008;179:2254-7; discussion 2257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 105] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 12. | Liu JJ, Guo DP, Gill H. Patterns of urinary catheter consults in a tertiary care hospital. Can J Urol. 2013;20:7046-7049. [PubMed] |
| 13. | Lawton JD, Ortiz N, Henry A, Smith C, Smith R, Rapp DE. Characterization and Outcomes of Iatrogenic Urethral Catheterization Injuries. Urol Pract. 2024;11:385-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 14. | Laborde E, Hill H, Dukovac TE, Carriere SP, Lata-Arias K, Hebert K, Patel R, Gills J. A Nurse-Driven Protocol for Foley Catheter Utilization Decreases the Incidence of Traumatic Foley Catheterization. Ochsner J. 2021;21:41-62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 15. | Bhatt NR, Davis NF, Quinlan MR, Flynn RJ, McDermott TED, Manecksha RP, Thornhill JA. A prospective audit on the effect of training and educational workshops on the incidence of urethral catheterization injuries. Can Urol Assoc J. 2017;11:E302-E306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Hackett A, Wells C, Drew L, Curto J, Ennis-Welch P, Zafra K, Bass K, Rosen D, Gupta R, Kohli-Seth R. Expanding access to difficult urinary catheter insertion services through a novel nurse practitioner-led team. J Am Assoc Nurse Pract. 2023;35:392-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/