Published online Jun 25, 2025. doi: 10.5527/wjn.v14.i2.103035
Revised: February 21, 2025
Accepted: March 4, 2025
Published online: June 25, 2025
Processing time: 154 Days and 20.7 Hours
Emphysematous pyelonephritis (EPN) is a life-threatening necrotizing renal parenchyma infection characterized by gas formation due to severe bacterial infection, predominantly affecting diabetic and immunocompromised patients. It carries high morbidity and mortality, requiring early diagnosis and timely intervention. Various prognostic scoring systems help in triaging critically ill patients. The National Early Warning Score 2 (NEWS 2) scoring system is a widely used physiological assessment tool that evaluates clinical deterioration based on vital parameters, but its standard form lacks specificity for risk stratification in EPN, necessitating modifications to improve treatment decision-making and prognostic accuracy in this critical condition.
To highlight the need to modify the NEWS 2 score to enable more intense moni
This prospective study was done on all EPN patients admitted to our hospital over the past 12 years. A weighted average risk-stratification index was calculated for each of the three groups, mortality risk was calculated for each of the NEWS 2 scores, and the need for intervention for each of the three groups was calculated. The NEWS 2 score was subsequently modified with 0-6, 7-14 and 15-20 scores included in groups 1, 2 and 3, respectively.
A total of 171 patients with EPN were included in the study, with a predominant association with diabetes (90.6%) and a female-to-male ratio of 1.5:1. The combined prognostic scoring of the three groups was 10.7, 13.0, and 21.9, respectively (P < 0.01). All patients managed conservatively belonged to group 1 (P < 0.01). Eight patients underwent early nephrectomy, with six from group 3 (P < 0.01). Overall mortality was 8 (4.7%), with seven from group 3 (87.5%). The cutoff NEWS 2 score for mortality was identified to be 15, with a sensitivity of 87.5%, specificity of 96.9%, and an overall accuracy rate of 96.5%. The area under the curve to predict mortality based on the NEWS 2 score was 0.98, with a confidence interval of (0.97, 1.0) and P < 0.001.
Modified NEWS 2 (mNEWS 2) score dramatically aids in the appropriate assessment of treatment-related outcomes. MNEWS 2 scores should become the practice standard to reduce the morbidity and mortality associated with this dreaded illness.
Core Tip: We present the most extensive single-centre study on patients diagnosed with emphysematous pyelonephritis (EPN), comprehensively evaluating risk stratification, disease severity, and treatment outcomes. While the traditional National Early Warning Score 2 (NEWS 2) score is a well-established tool for triaging critically ill patients in emergency settings, its ability to predict long-term treatment outcomes in EPN remains limited. The modified NEWS 2 score proposed in this study enhances risk differentiation, allowing for more accurate prognostication and timely clinical decision-making. This refined scoring system enables optimized resource allocation, early intensive care unit admission, and tailored treatment approaches, ultimately improving patient survival and reducing morbidity in EPN.
- Citation: Krishnamoorthy S, Thiruvengadam G, Sekar H, Palaniyandi V, Ramadurai S, Narayanasamy S. Modified National Early Warning Score 2, a reliable early warning system for predicting treatment outcomes in patients with emphysematous pyelonephritis. World J Nephrol 2025; 14(2): 103035
- URL: https://www.wjgnet.com/2220-6124/full/v14/i2/103035.htm
- DOI: https://dx.doi.org/10.5527/wjn.v14.i2.103035
Emphysematous pyelonephritis (EPN) is a commonly encountered urological emergency. The presence of gas in the renal parenchyma, collecting system, and peri/para nephric spaces causes a necrotizing infection that leads to severe sepsis-related complications. Historically, the mortality rate for EPN reached 78% in medically treated patients, with an overall mortality of 54%[1]. Recent studies, however, indicate a significant decline to approximately 20%–40%[2]. Standardized staging and prognostic scoring systems have facilitated early diagnosis, effective triage, and appropriate treatment, reducing morbidity and mortality[3-5].
With improved diagnostics and an ever-increasing awareness about this lethal disease, various authors looked at the next steps to improve the prognosis and further reduce the morbidity associated with EPN. Various inflammatory markers and scoring systems were looked into, and visible changes were observed in the management of EPN[6]. Focus has now shifted towards renal conservation therapy, with emphasis on early detection, internal (double J stenting) or external diversion [percutaneous nephrostomy (PCN) or drainage of peri-nephric collection][7-9].
Triaging such patients in the Emergency room is an essential pre-requisite. Emphasis should be placed on identifying those critically ill and those who need intensive care and early intervention. Urosepsis, gram-negative septicemia, Systemic inflammatory response syndrome (SIRS) and Multi-organ dysfunction syndrome are the dangerous sequelae of this dreaded condition. Once high-risk patients are identified, treating physicians must prioritize the treatment plans. Various scoring systems have helped identify and triage those high-risk individuals. Modified Early Warning score (MEWS), Pediatric Early Warning Score, National Early Warning Score (NEWS), and Sequential Organ Failure Assess
The Royal College of Surgeons of London introduced the original NEWS score in 2012[17,18]. The primary purpose was to detect and prioritize those who need acute emergency intensive care, as early detection, timely response and competent clinical responses are the three parameters that objectively define ultimate patient outcomes. The Royal College redefined this scoring system in 2017 to enhance the precision of diagnosis and treatment. The NEWS 2 score is critical in identifying patients susceptible to clinical deterioration, prompting expedited care and medical/surgical intervention[19].
The NEWS 2 scoring system takes into consideration six physiological parameters. The readily available measures, ease of usability, lack of inter-observer variability, and higher degree of validity of the score have made it a popular triaging score in the emergency rooms of the United Kingdom and many other countries. Each has a score ranging from 0 to 3, with zero being the least severe and 3 being the most severe form. The NEWS 2 scoring system offers a tracking aid in assessing the patient's condition in an emergency setting and triaging geriatric patients in crowded emergency rooms[20-22].
The NEWS 2 score ranges from 0 to 20. A score of below 4 indicates a lower risk of clinical deterioration. Scores of 5 and 6 suggest a moderate risk of worsening, warranting an "urgent response threshold". The National Health Service of the United Kingdom, in association with The Royal College of Physicians, proposed a score of 7 as an "emergency response threshold" for triaging patients needing higher dependency unit or intensive care unit (ICU) monitoring[23]. While the NEWS 2 scoring system has been instrumental in the early detection of clinical deterioration and prioritizing emergency responses, its ability to predict treatment outcomes in severe infections like EPN remains suboptimal. A significant limitation lies in the broad risk stratification at higher scores—patients with a NEWS 2 score of 7 and those with a score of 20 are categorized similarly despite likely having vastly different prognoses and treatment responses. This lack of granularity in risk differentiation may lead to delayed or inappropriate allocation of critical care resources. Recognizing this limitation, we propose modifying the NEWS 2 system modified NEWS 2 (mNEWS 2) to enhance its predictive power by refining risk stratification, allowing for more precise triaging and early intervention. By tailoring the score to reflect clinical severity and response to treatment better, mNEWS 2 aims to bridge the gap between early warning and outcome prediction, ultimately improving decision-making and patient survival in EPN.
Though the NEWS 2 scoring system effectively detects clinical deterioration, its broad risk stratification at higher scores limits its ability to predict treatment outcomes in severe infections like EPN. Patients with scores of 7 and 20 are categorized similarly despite significant differences in clinical severity, which may lead to delayed or inappropriate critical care interventions. This study addresses this gap in knowledge by proposing a mNEWS 2 score that enhances risk differentiation, enables more precise triaging, prioritizes intensive monitoring and facilitates timely interventions in EPN cases.
This study was conducted on all patients with EPNs admitted to our tertiary care referral teaching institution in South India between July 2012 and June 2024. Our study primarily evaluated clinical parameters and prognostic scoring in patients with EPN. Demographic attributes such as origin, ethnicity, and language were not specifically analyzed, as the objective was to assess risk stratification and treatment outcomes based on physiological and biochemical markers rather than population-based variations.
A list of all prognostic variables was tabulated from our institution's prospective database containing all those pre-defined prognostic variables. Prognostic scoring and risk stratification were done based on the author's previous published literature[4].
The prognostic scores were listed based on specific premeditated parameters. A total of 18 parameters found to be significant from the author's previously published literature were short-listed. Each parameter was given a score ranging from 0 to 2, with a minimum total score of 1 and a maximum total score of 26. Risk stratification of EPN was done based on a combined prognostic score. Those with a score of 1–8 were grouped under the very low-risk category. The low-risk group scored 9–15, the intermediate-risk group scored 16–20, and those with a score of > 20 (high-risk group) carried a much higher risk of succumbing to the disease. The maximum score that could be obtained was 26 (read authors' earlier publication for reference)[4].
The NEWS 2 is a scoring system based on a simple aggregate of six physiological parameters routinely measured and monitored in emergency rooms. The parameters studied are respiration rate, oxygen saturation, systolic blood pressure, pulse rate, level of Consciousness and body temperature. Each of the six parameters is assigned a score that reflects the extremes of variability from the standard set norm. The higher the score, the greater the variability from the standard norms. The maximum cumulative score is 20. The NEWS 2 score was then calculated for each admitted patient and classified into three groups. Traditionally, the aggregate score of 5 and above is a critical threshold value that triggers the need for an urgent clinical assessment and review. A score of 7 and above triggers the need for an elevated clinical response, necessitating an emergency clinical review.
While the NEWS 2 score perfectly holds good for the initial triaging, an initial pilot study on treatment outcomes revealed considerable overlap between the scores. Treatment outcomes in patients with scores of 5 and 6 behaved almost the same as those between 0 and 4. Similarly, patients with scores between 7 and 14 behaved very differently from those with a score of 15 and above. This prompted us to revisit the NEWS 2 score and see if this score can be modified only regarding treatment outcomes.
A weighted average risk stratification index was calculated for the three groups. The weighted average is the average of a data set that ensures similar data points are equal in the proportion represented. The weighted average is calculated by multiplying each value in the set by its weight, then adding up the products and calculating its average. The weighted average risk stratification index was calculated as follows: For example, 20 patients in group 1, with 2 patients, 4 patients, 6 patients and 8 patients having a risk stratification index of 1, 2, 3 and 4, respectively. In that case, the weighted average is calculated as follows: (2 × 1) + (4 × 2) + (6 × 3) + (8 × 4) divided by 20, 2 + 8 + 18 + 32 divided by 20, which means 60 ÷ 20 = 3. This group's Weighted average Risk stratification index would be measured as 3. This formed the basis for modifying the NEWS 2 scoring system.
The scores of 5 and 6 were combined with 0 to 4 and were included in group 1. Scores of 7 to 20 were divided into two groups. Group 2 included patients with scores of 7 to 14. Patients with scores of 15 and above were included in group 3. All the qualitative and quantitative variables between the revised three groups were analyzed and compared with treatment outcomes. All patients were divided into three broad groups: (1) Group 1; (2) Group 2; and (3) Group 3.
A preliminary calculation was done based on the original NEWS 2 score (Table 1). We observed that the weighted average risk stratification index between the three groups was significant, but when rounded off to the nearest whole number, it was the same for all three groups. Table 1 was formulated by dividing group 3 into two groups (7-14 and 15-20). In Table 1, the group 3 was subdivided into three subgroups (7-10, 11-14 and 15-20). In Table 1, groups 1 and 2 behaved alike. Table 1 combined groups 1 and 2 and subdivided group 3 into two subgroups (7-14 and 15-20). Though the need for intervention was almost the same in groups 1 and 2, mortality was noted only in group 2. Table 1 was finally considered to be the mNEWS 2 score.
| Original NEWS 2 score | |||||||
| Weighted average risk stratification index | Group 1: Score 0-4 (n = 48) | Group 2: Score 5 and 6 (n = 35) | Group 3: Scores 7-20 (n = 88) | P value | |||
| 1.875 | 1.857 | 2.44 | 0.02 | ||||
| Risk stratification index (rounded off) | 2 | 2 | 2 | ||||
| Need for intervention | 33 (68.75) | 27 (77.14) | 71 (80.68) | < 0.01 | |||
| Mortality | 0 | 0 | 8 | < 0.01 | |||
| Group 3, subdivided into two | |||||||
| Weighted average risk stratification index | Group 1: Score 0-4 (n = 48) | Group 2: Score 5 and 6 (n = 35) | Group 3: Scores 7-20 (n = 88) | P value | |||
| Scores 7-14 (n = 76) | Scores 15-20 (n = 12) | ||||||
| 1.875 | 1.857 | 2.319 | 3.75 | < 0.01 | |||
| Risk stratification index (rounded off) | 2 | 2 | 2 | 3 | |||
| Need for intervention | 40 (83.33) | 27 (77.14) | 61 (80.26) | 12 (100) | < 0.01 | ||
| Mortality | 0 | 0 | 1 | 7 | < 0.01 | ||
| Group 3, subdivided into three | |||||||
| Risk stratification | Group 1: Score 0-4 (n = 48) | Group 2: Score 5 and 6 (n = 35) | Group 3: Scores 7-10 (n = 55) | Group 4: Scores 11-14 (n = 21) | Group 5: Scores 15-20 (n = 12) | P value | |
| Weighted average risk stratification index | 1.875 | 1.857 | 1.982 | 2.762 | 3.75 | < 0.01 | |
| Weighted average risk stratification index (rounded off) | 2 | 2 | 2 | 3 | 4 | ||
| Need for intervention | 40 (83.33) | 27 (77.14) | 44 (80) | 17 (80.95) | 12 (100) | < 0.01 | |
| mortality | 0 | 0 | 0 | 1 | 7 | < 0.01 | |
| Modified NEWS 2 scoring system | |||||||
| Parameters | Group 1: Score 0-6 (n = 83) | Group 2: Score 7-14: n = 76 | Group 3: Score 15-20 (n = 12) | P value | |||
| Weighted average Risk stratification index | 1.867 | 2.039 | 3.75 | < 0.01 | |||
| Risk stratification index (rounded off) | 2 | 2 | 4 | ||||
| Need for intervention | 67 (80.72) | 60 (78.95) | 12 (100) | < 0.01 | |||
| mortality | 0 | 1 (1.32) | 7 (58.33) | < 0.01 | |||
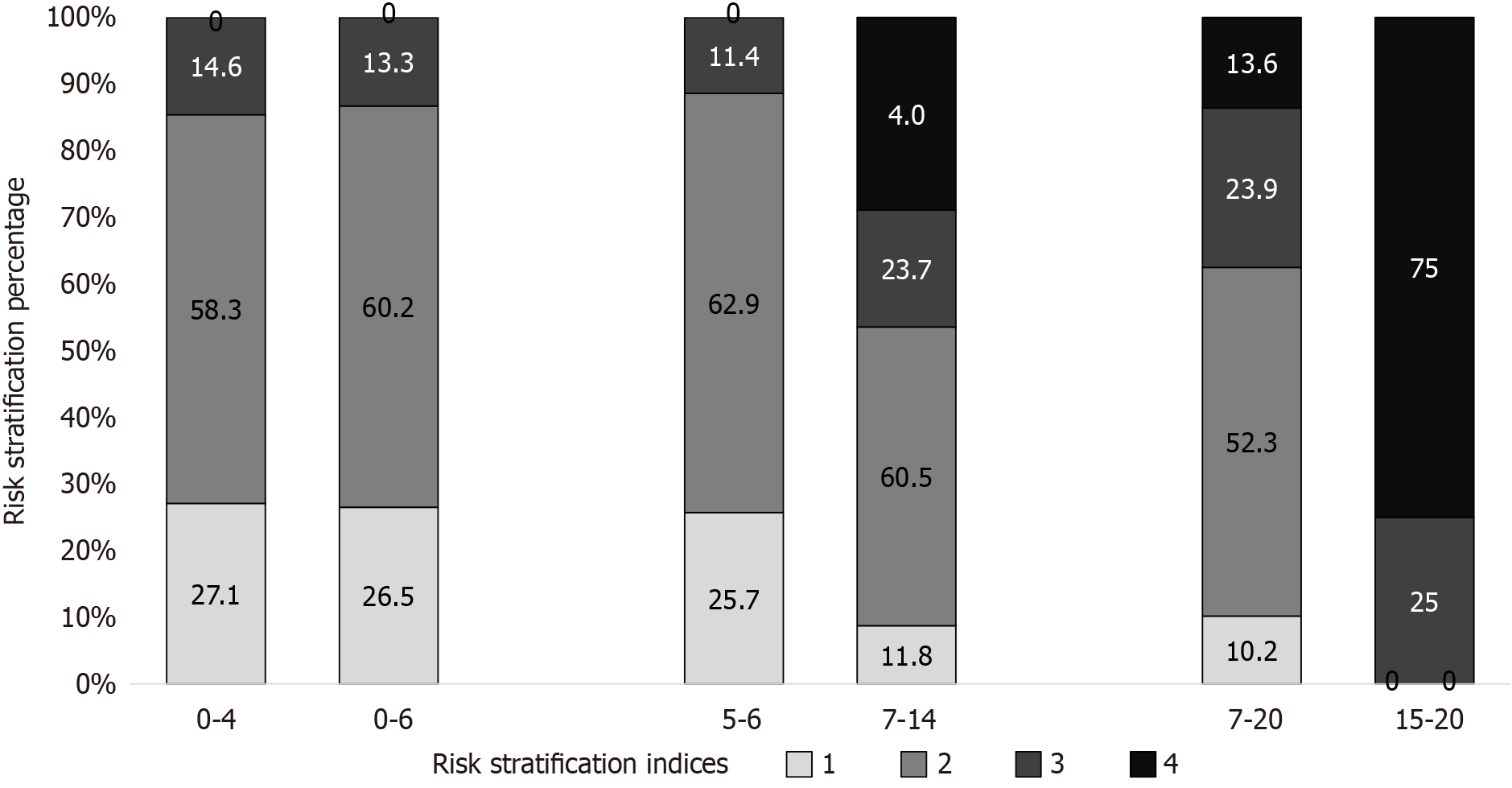
Figure 1 gives a graphic representation of the distribution of the risk stratification indices across various NEWS 2 groups. The standard NEWS 2 groups (0-4, 5-6 and 7-20) matched the mNEWS 2 scores of 0-6, 7-14 and 15-20. The groups 0-4 and 0-6 almost behaved the same. Groups 5-6 and 7-14 behaved virtually the same, except that significant numbers with higher risk stratification would have missed out if the original scoring was considered. Similarly, the modified group 3 includes only patients with a higher risk index, so focused treatment could be offered to the smaller group of patients who deserve it more.
Also, the sensitivity, specificity, positive and negative predictive value (NPV) and accuracy of the testing were calcu
| Cutoff National Early Warning Score 2 for mortality | Sensitivity % (95%CI) | Specificity % (95%CI) | Positive predictive value % (95%CI) | Negative predictive value % (95%CI) | Accuracy % (95%CI) |
| ≥ 7 | 100 (63.06-100) | 50.92 (42.98-58.82) | 9.09 (7.88-10.47) | 100 (95.65-100) | 53.22 (45.45-60.87) |
| ≥ 8 | 100 (63.06-100) | 58.90 (50.93-66.53) | 10.67 (9.04-12.55) | 100 (96.23-100) | 60.82 (53.07-68.18) |
| ≥ 9 | 100 (63.06-100) | 69.94 (62.27-76.86) | 14 (11.44-17.10) | 100 (96.82-100) | 71.35 (63.94-77.99) |
| ≥ 10 | 100 (63.06-100) | 80.98 (74.10-86.7) | 20.51 (15.82-26.16) | 100 (97.24-100) | 81.87 (75.27-87.34) |
| ≥ 11 | 100 (63.06-100) | 84.66 (78.20-89.82) | 25.24 (18.24-31.46) | 100 (97.36-100) | 85.38 (79.18-90.31) |
| ≥ 12 | 100 (63.06-100) | 86.50 (80.28-91.34) | 26.67 (19.78-34.91) | 100 (97.42-100) | 87.13 (81.17-91.76) |
| ≥ 13 | 100 (63.06-100) | 89.57 (83.83-93.81) | 32 (23.08-42.46) | 100 (97.51-100) | 90.06 (84.56-94.10) |
| ≥ 14 | 100 (63.06-100) | 91.41 (86.01-95.22) | 36.36 (25.72-48.53) | 100 (97.55-100) | 91.81 (86.64-95.45) |
| ≥ 15 | 87.50 (47.35-99.68) | 96.93 (92.99-99) | 58.33 (36.23-77.53) | 99.37 (96.19-99.9) | 96.49 (92.52-98.70) |
| ≥ 16 | 75 (34.91-96.81) | 98.16 (94.72-99.62) | 66.67 (37.82-86.8) | 98.77 (96.01-99.63) | 97.08 (93.31-99.04) |
| ≥ 17 | 50 (15.7-84.3) | 98.77 (95.64-99.85) | 66.67 (29.97-90.34) | 97.58 (95.27-98.77) | 96.49 (92.52-98.7) |
| ≥ 18 | 25 (3.19-65.09) | 100 (97.76-100) | 100 (15.81-100) | 96.45 (94.79-97.59) | 96.49 (92.52-98.7) |
| ≥ 19 | 12.50 (0.32-52.65) | 100 (97.76-100) | 100 (2.50-100) | 95.88 (94.71-96.8) | 95.91 (91.75-98.34) |
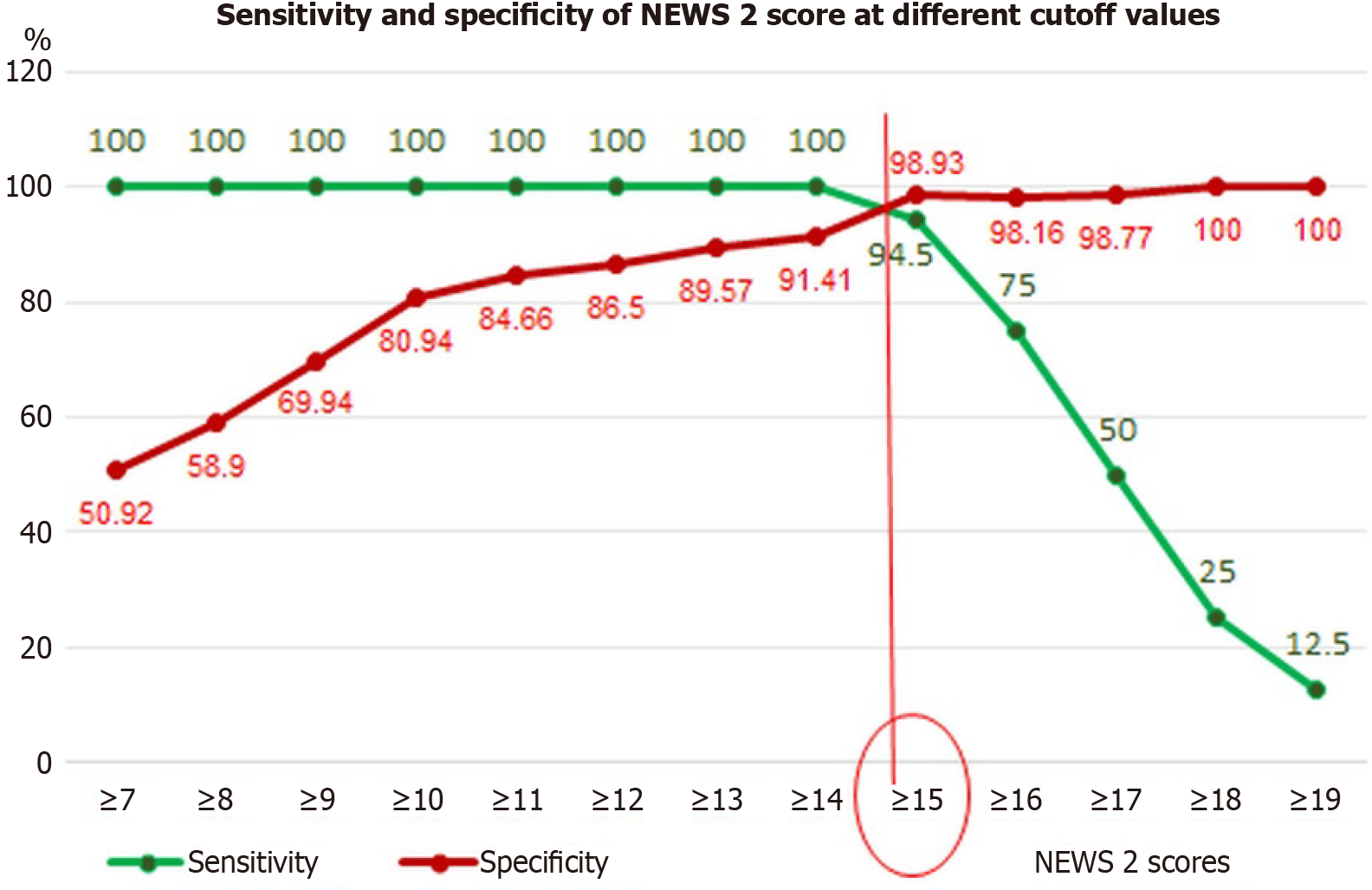
Figure 2 shows the NEWs 2 scores on the X axis and the percentage of sensitivity (green line) and specificity (red line) on the Y axis. The sensitivity and specificity are maximal for a score of 15 and above. Hence, the cutoff value of 15 and above is chosen to include patients in group 3.
The selection of specific cutoff values for the mNEWS 2 score was based on clinical observations, statistical modelling, and predictive performance analysis. An initial pilot study revealed overlapping treatment outcomes in specific score ranges, particularly between scores 5–6 and 0–4, and among patients scoring 7–14 compared to those scoring ≥ 15. We employed weighted average risk stratification indices to refine risk stratification, ensuring that each group had distinct clinical outcomes.
Further justification for these cutoffs comes from sensitivity, specificity, and accuracy calculations, which identified a threshold at a NEWS 2 score of 15, where predictive performance was maximized. This was validated through receiver operating characteristic (ROC) curve analysis, confirming that the new stratification better aligns with intervention needs and mortality risk. While this modification improves outcome differentiation within our cohort, we acknowledge the need for external validation in diverse clinical settings to confirm its broader applicability.
The mNEWS 2 score was designed to retain the simplicity and ease of application of the original NEWS 2 system. The reclassification groups align with clinically relevant risk stratification while maintaining an intuitive scoring structure that can be seamlessly used in emergency settings without additional complexity.
The collected data were entered into Microsoft Excel 2016 and analyzed using Statistical Package for the Social Sciences, version 19. Descriptive statistics were used to summarize the characteristics of the sample: Continuous variables were presented as mean and SD, while categorical variables were reported as frequencies and percentages. For inferential analysis, analysis of variance with post hoc multiple comparisons was used to compare continuous variables across more than two groups. The χ2 test was applied to analyze categorical variables. An independent sample t-test assessed significant differences between the two groups. To determine the optimal cutoff score, ROC curve analysis was performed, and sensitivity, specificity, positive predictive value, and NPV were calculated. A significance level of 5% (P < 0.05) was considered statistically significant.
A total of 171 patients with EPN were included in our study. Table 3 illustrates the demographic data of patients in our study. Females were more commonly involved in all three groups. While fever was common in all three groups, temperature extremes were observed more commonly in groups 2 and 3. Most patients in groups 1 and 2 were alert, conscious, and oriented to time, place, and person. Only one-third in group 3 were alert.
| Pt characteristics | Group 1: Score 0-6 (n = 83) | Group 2: Score 7-14 (n = 76) | Group 3: Score 15-20 (n = 12) | P value |
| Mean age in years (SD) | 52.639 (10.55) | 55.553 (11.95) | 60.083 (3.45) | 0.046 |
| Age > 50 years | 0.053 | |||
| Yes | 56 (67.47) | 57 (75) | 12 (100) | |
| No | 27 (32.53) | 19 (25) | 0 | |
| Sex | ||||
| Male | 39 (46.99) | 25 (32.90) | 5 (41.67) | 0.194 |
| Female | 44 (53.01) | 51 (67.10) | 7 (58.33) | |
| Sex (female:male) | 1.1:1 | 2.1:1 | 1.4:1 | |
| Laterality | 0.162 | |||
| Unilateral | 68 (81.93) | 70 (92.10) | 10 (83.33) | |
| Bilateral | 15 (18.07) | 6 (7.90) | 2 (16.67) | |
| Body temp | < 0.01 | |||
| No fever | 29 (34.94) | 11 (14.47) | 0 (0) | |
| Temp between 37-40 °C | 54 (65.06) | 58 (76.31) | 5 (41.67) | |
| Temp < 36.8 °C, > 40 °C | 0 | 7 (9.21) | 7 (58.33) | |
| Level of consciousness | < 0.01 | |||
| Alert | 82 (98.8) | 51 (67.10) | 4 (33.33) | |
| Disoriented/unconscious | 1 (1.2) | 25 (32.90) | 8 (66.67) | |
| Other parameters | ||||
| Palpable tender kidney | 7 (8.43) | 48 (63.16) | 12 (100) | < 0.01 |
| Shock at presentation | 1 (1.21) | 20 (2.63) | 11 (91.67) | < 0.01 |
| Need for intensive care unit care | 9 (10.84) | 43 (56.58) | 12 (100) | < 0.01 |
| Need for hemodialysis | 5 (5.95) | 15 (19.74) | 11 (91.67) | < 0.01 |
| Presence of diabetes mellitus | 71 (85.6) | 73 (96.1) | 12 (100) | 0.035 |
| Early nephrectomy | 0 (0) | 2 (2.63) | 6 (50) | < 0.01 |
| Mean combined prognostic scoring (SD) | 10.74 (3.81) | 12.95 (3.90) | 21.92 (2.61) | < 0.01 |
| Risk stratification index | < 0.01 | |||
| 1 | 22 (26.5) | 9 (11.84) | 0 | |
| 2 | 50 (60.24) | 46 (60.52) | 0 | |
| 3 | 11 (13.25) | 18 (23.68) | 3 (25) | |
| 4 | 0 (0) | 3 (3.95) | 9 (75) | |
Diabetes mellitus was a common occurrence in all three groups. A palpable tender kidney was seen in all patients with a NEWS 2 score of above 15 and nearly two-thirds with a score of 7 to 14. Similarly, hemodynamic instability, shock at initial Presentation, and the need for intensive monitoring and Hemodialysis were observed in high numbers in patients with a score of 15 and above. The mean combined prognostic scoring was found to correlate directly with the NEWS 2 score. A higher prognostic score was observed in patients with higher NEWS 2 scores (P < 0.01). Similarly, most patients in groups 1 and 2 had a lower while three-fourths of patients in group 3 had a higher risk stratification index of 4 (P < 0.01).
The demographic variables like patient age, sex, laterality, body mass index, the six parameters of NEWS 2 score, hemodynamic stability, comorbidities and need for intensive care monitoring were tabulated for each of the three groups (Table 3).
Across all groups, females were more commonly affected, with a higher female-to-male ratio observed in groups 2 and 3. Advanced age correlated with increasing severity, as all patients in group 3 were above 50 (P = 0.046). Fever was a common presenting symptom in all groups, but extreme temperature variations (< 36.8 °C or > 40 °C) were significantly more frequent in group 3 (58.3%) compared to groups 1 and 2 (P < 0.01). Similarly, altered mental status was more prevalent in patients with higher NEWS 2 scores, with only one-third of group 3 remaining alert at Presentation (P < 0.01).
Hemodynamic instability was a key distinguishing factor among the groups. While nearly all patients in group 1 were stable at presentation, 91.67% of group 3 presented with shock (P < 0.01). A palpable, tender kidney was universally noted in group 3, correlating with increased disease severity (P < 0.01). The need for intensive care monitoring and hemodialysis was also significantly greater in group 3, highlighting the critical condition of this subset.
Table 4 illustrates the details of various biochemical parameters and radiological variables in three groups. The mean blood sugar and hemoglobin A1c (HbA1c) levels were significantly higher in group 3. All other blood biochemistry (except leukocyte count) showed a significant difference between group 3 and other groups. The computed tomography (CT) scan of all patients in group 3 had a class 3 or 4 EPN, while most in groups 1 and 2 had class 1 and 2 EPN.
| Biochemical variables | Group 1: Score 0-6 (n = 83) | Group 2: Score 7-14 (n = 76) | Group 3: Score 15-20 (n = 12) | P value |
| Absolute leukocyte count (SD) | 15394.2 (6895.11) | 16489.3 (7478.58) | 20778.3 (7875.63) | 0.152 |
| Heart rate (per minute) (SD) | 86.711 (12.58) | 90.026 (17.79) | 110.750 (21.16) | < 0.01 |
| Blood sugar on admission (mg/dL) (SD) | 245.578 (100.78) | 323.21 (129.33) | 346.167 (59.12) | < 0.01 |
| Hemoglobin A1c (SD) | 8.712 (2.55) | 9.375 (1.7) | 10.07 (2.59) | 0.023 |
| S creatinine on admission (mg/dL) (SD) | 3.187 (2.21) | 3.928 (2.54) | 5.14 (1.45) | 0.003 |
| International normalized ratio test (SD) | 1.18 (0.18) | 1.27 (0.31) | 1.86 (0.61) | < 0.01 |
| Serum sodium level (mEq/L) (SD) | 131.94 (6.03) | 131.90 (5.76) | 123.58 (4.89) | < 0.01 |
| Serum albumin (grams/dL) (SD) | 3.14 (0.65) | 3.08 (0.73) | 2.392 (0.45) | 0.004 |
| Platelet count (SD) | 220695.181 (128292.52) | 124053.947 (87178.32) | 54575.000 (25853.30) | < 0.01 |
| Mean hospital stay (days) (SD) | 5.7 (2.99) | 7.6 (3.72) | 8.3 (4.72) | < 0.01 |
| Computed tomography classification | < 0.01 | |||
| Class 1 | 32 (38.55) | 11 (14.47) | 0 (0) | |
| Class 2 | 25 (30.12) | 33 (43.42) | 0 (0) | |
| Class 3A | 9 (10.84) | 9 (11.82) | 1 (8.33) | |
| Class 3B | 2 (2.41) | 15 (19.74) | 2 (2.63) | |
| Class 4 | 15 (18.07) | 8 (10.53) | 9 (11.84) |
Biochemical parameters further supported the stratification of disease severity. Group 3 had markedly elevated blood glucose levels (mean 346.16 mg/dL) and HbA1c levels (10.07%), reinforcing the strong association between diabetes and severe EPN (P = 0.023). Similarly, renal function markers such as serum creatinine were significantly elevated in group 3 (mean 5.14 mg/dL, P = 0.003), suggesting a higher likelihood of acute kidney injury in this cohort. Hypoalbuminemia and hyponatremia were also pronounced in group 3, further emphasizing the impact of systemic inflammation and metabolic derangements in disease progression.
Radiologically, CT findings correlated well with clinical severity. Patients in groups 1 and 2 predominantly had class 1 and 2 EPN, whereas all patients in group 3 exhibited class 3 or 4 disease, indicating widespread parenchymal involve
Table 5 gives details of the treatment given to our patients. All 32 patients (100%) who were medically treated and conservatively managed were from group 1. Six patients in group 3 had a double J stenting done. The remaining six (in group 3) either had an early nephrectomy (n = 4) or succumbed to the illness (n = 2). Early nephrectomy was performed in 8 patients, of which two patients died after surgery. However, all four patients in group 3, who had an early nephrectomy done, recovered well after surgery. Ten patients in group 3 had either PCN or percutaneous catheter drainage (PCD) placed or both. Seven out of 8 mortality (87.5%) were observed in group 3 patients.
| Treatment given | Group 1: Score 0-6 (n = 83) | Group 2: Score 7-14 (n = 76) | Group 3: Score 15-20 (n = 12) | P value |
| Non-surgical treatment (n = 32) | 32 (100) | 0 (0) | 0 (0) | < 0.01 |
| DJ stenting (n = 127) | 49 (59) | 72 (94.7) | 6 (50) | < 0.01 |
| Percutaneous nephrostomy (n = 26) | 4 (4.8) | 14 (18.4) | 8 (66.7) | < 0.01 |
| Percutaneous catheter drainage (n = 28) | 5 (6) | 16 (21.1) | 7 (58.3) | < 0.01 |
| Need for hemodialysis (n = 31) | 5 (6) | 15 (19.7) | 11 (91.7) | < 0.01 |
| Early nephrectomy (n = 8) | 0 (0) | 2 (2.6) | 6 (50) | < 0.01 |
| Mortality (n = 8) | 0 (0) | 1 (1.3) | 7 (58.3) | < 0.01 |
Treatment strategies and outcomes varied significantly between groups. Non-surgical management was effective in all 32 patients from group 1, while interventional procedures such as PCD and PCN were increasingly required in groups 2 and 3. Notably, 50% of patients in group 3 underwent early nephrectomy, reflecting the aggressive nature of the disease in this subset (P < 0.01).
The mortality rate was disproportionately high in group 3, with 7 out of 12 patients (58.3%) succumbing to the illness, compared to just one patient (1.3%) in group 2 and none in group 1 (P < 0.01). The NEWS 2 score was found to be a strong predictor of mortality, with a cutoff of ≥ 15 demonstrating the highest predictive accuracy (96.49%), emphasizing its utility as a clinical decision-making tool.
Table 2 summarizes the sensitivity and specificity for mortality at various cutoff NEWS 2 scores from 7 to 18. The cutoff score of ≥ 15 showed the highest accuracy report of 96.49. The specificity, positive and negative predictive values were also maximum at this cutoff value of ≥ 15. This formed the basis for redefining the NEWS 2 scores regarding treatment-related outcomes.
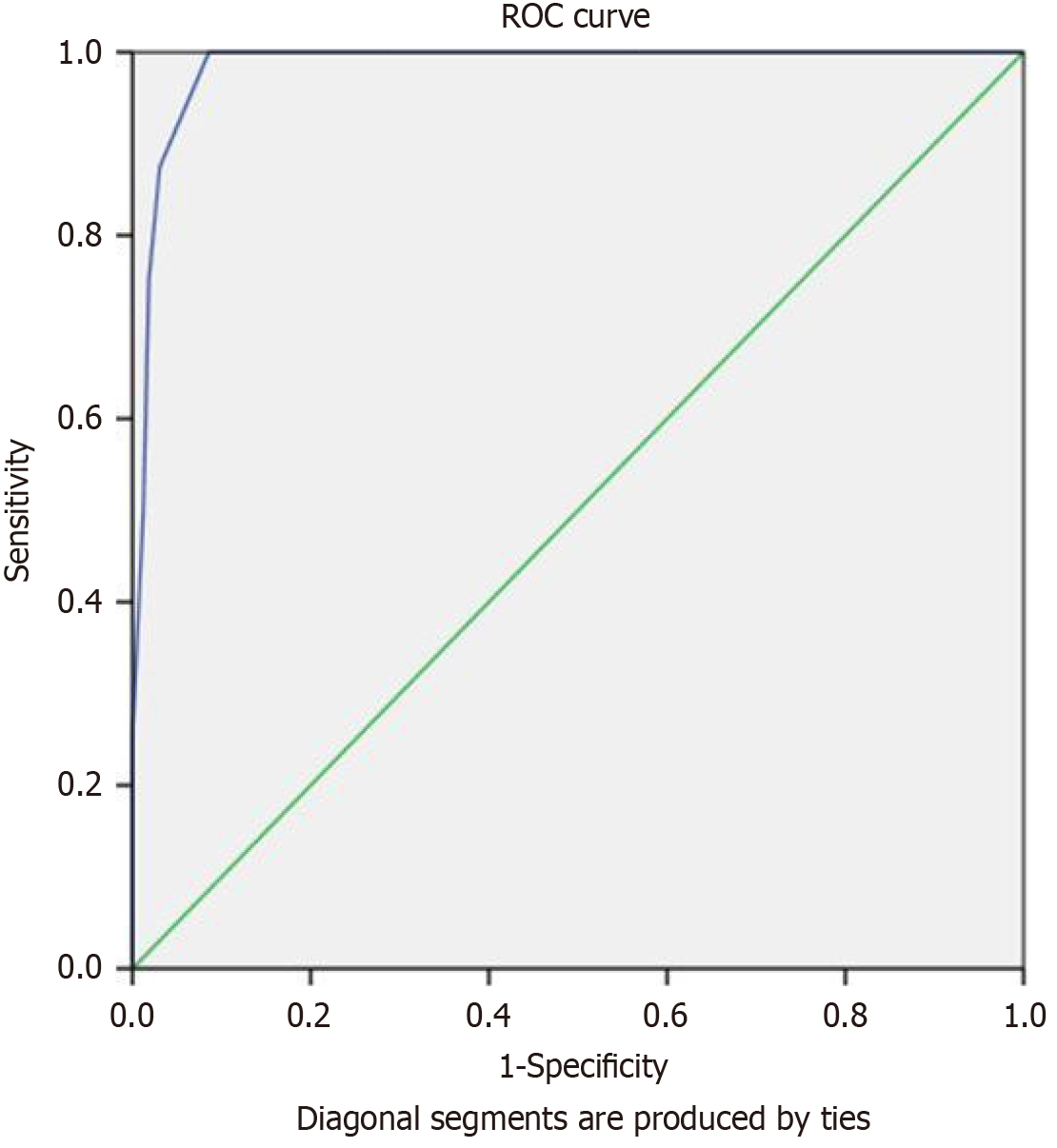
The ROC curve gives us a visual and graphic illustration of the study's performance across various thresholds. In this graph, we plotted the false positive rates on the X-axis and true positive values on the Y-axis. The area under the curve (AUC) measures the performance of the model under study.
Although this table reiterates data from Tables 2, 3, 4, and 5, it highlights the most clinically relevant differences across groups. Group 3 (mNEWS 2: 15-20) consists entirely of patients over 50 years, compared to 67.5% in group 1 (mNEWS 2: 0-6). Body temperature extremes, shock at presentation, and altered consciousness increased significantly across the groups, with shock affecting 91.7% and altered consciousness in 66.7% of group 3 patients. A palpable tender kidney, present in 100% of group 3 patients, is a key distinguishing clinical feature (Table 6).
| Clinical parameter | Group 1 (NEWS 2: 0-6, n = 83) | Group 2 (NEWS 2: 7-14, n = 76) | Group 3 (NEWS 2: 15-20, n = 12) | P value |
| Percentage (95%CI)/mean ± SD (95%CI) | ||||
| Age > 50 years (%) | 67.50 (58.9-75.4) | 75 (65.4-82.8) | 100 (73.5-100) | 0.046 |
| Body temperature extremes (%) | 0 (0-4.4) | 9.21 (4.5-17.8) | 58.30 (34.8-78.4) | < 0.01 |
| Shock at presentation (%) | 1.20 (0.2-6.5) | 26.30 (18.2-36.1) | 91.70 (65.3-98.8) | < 0.01 |
| Altered consciousness (%) | 1.20 (0.2-6.5) | 32.90 (24.2-42.9) | 66.70 (41.0-85.6) | < 0.01 |
| Palpable tender kidney (%) | 8.40 (4.1-16.3) | 63.20 (52.4-72.9) | 100 (73.5-100) | < 0.01 |
| Presence of diabetes mellitus (%) | 85.6 (76.1-92) | 96.1 (88.9-99.18) | 100 (73.5-100) | 0.035 |
| Need for intensive care unit care (%) | 10.80 (6.0-18.6) | 56.60% (45.7-66.9) | 100 (73.5-100) | < 0.01 |
| Need for hemodialysis (%) | 6.00 (2.7-12.7) | 19.70% (12.7-29.2) | 91.70 (65.3-98.8) | < 0.01 |
| Early nephrectomy (%) | 0 (0-4.4) | 2.60 (0.7-9.0) | 50 (26.9-73.1) | < 0.01 |
| Mortality (%) | 0 (0-4.4) | 1.30 (0.2-6.9) | 58.30 (34.8-78.4) | < 0.01 |
| Heart rate (per minute) | 86.71 ± 12.58 (84.004- 89.416) | 90.03 ± 17.79 (86.03-94.03) | 110.75 ± 21.16 (98.78-122.72) | < 0.01 |
| Mean blood sugar (mg/dL) | 245.6 ± 100.8 (225.4-265.8) | 323.2 ± 129.3 (298.5-347.9) | 346.2 ± 59.1 (325.4-367.0) | < 0.01 |
| Serum creatinine (mg/dL) | 3.18 ± 2.21 (2.7-3.6) | 3.92 ± 2.54 (3.3-4.5) | 5.14 ± 1.45 (4.6-5.7) | 0.003 |
| Serum albumin (g/dL) | 3.14 ± 0.65 (2.9-3.3) | 3.08 ± 0.73 (2.9-3.3) | 2.39 ± 0.45 (2.2-2.6) | 0.004 |
| Hemoglobin A1c | 8.712 ± 2.55 (8.16- 9.26) | 9.375 ± 1.7 (8.99-9.76) | 10.07 ± 2.59 (8.665-11.53) | 0.023 |
| Sodium (mEq/L) | 131.94 ± 6.03 (130.3-133.6) | 131.90 ± 5.76 (130.3-133.4) | 123.58 ± 4.89 (121.4-125.8) | < 0.01 |
| International normalized ratio test | 1.18 ± 0.18 (1.14- 1.22) | 1.27 ± 0.31 (1.2- 1.34) | 1.86 ± 0.61 (1.515-2.205) | < 0.01 |
| Platelet count | 220695 ± 128292 (189345-252045) | 124053 ± 87178 (101345-146761) | 54575 ± 25853 (45676-63474) | < 0.01 |
| Computed tomography class 3/4 (%) | 20.50 (13.6-29.6) | 30.30 (21.5-40.4) | 100% (73.5-100) | < 0.01 |
| Risk stratification index (mean ± SD) | 1.867 ± 0.35 (1.8-2.0) | 2.039 ± 0.45 (1.9-2.2) | 3.75 ± 0.50 (3.5-4.0) | < 0.01 |
| Combined prognostic scoring index (mean ± SD) | 10.74 ± 3.81 (9.8-11.7) | 12.95 ± 3.90 (11.9-14.0) | 21.92 ± 2.61 (20.9-23.0) | < 0.01 |
The need for ICU care, haemodialysis, and early nephrectomy rises sharply, with ICU admission required for all group 3 patients and 50% undergoing nephrectomy. Absent in group 1, mortality reaches 58.3% in group 3, emphasizing the prognostic significance of disease severity.
Laboratory markers reflect worsening systemic dysfunction. Heart rate, mean blood sugar, and serum creatinine increase significantly while serum albumin and platelet count decline, suggesting progressive metabolic and hematologic deterioration. International normalized ratio test rises in group 3, indicating a higher bleeding risk. CT class 3/4 findings, seen in all group 3 patients, confirm the radiologic progression of the disease. Statistically significant differences (P < 0.01 for most parameters) underscore the mNEWS 2 score's predictive value in identifying critically ill patients, guiding clinical decision-making, and stratifying risk effectively.
It summarizes the progressive worsening of clinical parameters with increasing mNEWS 2 scores, highlighting significant differences in disease severity, organ dysfunction, and mortality.
Figure 3 illustrates our study's ROC curve. The true positive rates and false positive values for the NEWS 2 scores ranging from 1 to 20 were plotted in the Y and X axes, respectively. The AUC was then measured. The AUC to predict the mortality based on the News 2 score is 0.984 with a confidence interval of (0.966, 1) (P value < 0.001). This suggests that the cutoff value of 15 and above most specifically correlates with the degree of mortality.
The findings of this study underscore the prognostic significance of the NEWS 2 score in EPN patients. Higher scores correlate with increased mortality, greater need for intensive care, and more invasive interventions. The strong asso
The last two decades have witnessed a paradigm shift in evaluating and managing urological emergencies. With abundant e-resources available and the curiosity and keenness to know about their problems increasing many folds amongst the patients seeking treatment, predicting risk has become an essential and integral component of medical/surgical care. Prognostic scoring systems are formulated, risk stratification indices are developed, and nomograms and guidelines are established for each urological condition to facilitate the prognostication and treatment of various urological diseases and emergencies.
Various authors have studied the role of such predictive scores in the management of renal stone diseases, planning partial nephrectomy in solid renal masses and nomograms for prostate cancer[24-27]. Machine learning methods are being used these days to assess the predictability of the success of a surgical procedure[28]. Integrating machine learning techniques could further enhance the predictive accuracy and clinical applicability of the mNEWS 2 score. Machine learning models, such as logistic regression, random forests, or neural networks, could analyze large datasets to refine risk stratification by identifying complex interactions between clinical parameters. Such an approach may enable dynamic score adjustments, improving early detection of high-risk patients and optimizing triage decisions. Future research should focus on developing and validating machine learning-driven models that complement the mNEWS 2 score while ensuring interpretability and ease of integration into clinical workflows.
NEWS 2 scoring system is one such standardized and systematized early warning system that has been validated and extensively used in the United Kingdom and the rest of European countries. It greatly aids the activation of the hospital's rapid response teams on time[29]. The main application of this scoring system has been in the emergency room, where triaging of patients who need more intensive monitoring/stabilization is done based on various physiological para
Multiple studies have looked into the various predictive scores for EPN. Chawla et al[30] compared various predictive scores that facilitated expedited care in EPN patients. Kim et al[31] studied the role of blood culture and axial imaging in assessing the clinical utility for diagnosing pyelonephritis and predicting hospital mortality. Elbaset et al[32] studied the role of platelet-to-leukocyte ratio as a marker of sepsis in EPN patients. Bedoui et al[33] identified absolute leukocytic and lymphocytic counts at admission as independent predictors of urosepsis in EPN patients. MEWS 2, quick SOFA, SOFA and SIRS score have been extensively studied. The NEWS 2 score is the best predictor of the need for expedited ICU care[34]. However, when we correlated risk stratification with the NEWS 2 score, we observed that the rounded-off risk score was the same across all three NEWS 2 groups. Group 3 patients, with a score of 7 to 20, had a considerable overlap with patients in group 2 (score of 5 and 6). Similarly, scores 5 and 6 overlapped considerably with scores 0-4. The cutoff score for mortality with the highest degree of accuracy and sensitivity, specificity, and predictive values was 15. Hence, the mNEWS 2 score (0-6, 7-14 and 15-20) was used to assess the various treatment outcomes. This is the first-ever study on urological emergencies using the mNEWS 2 scoring system.
Our study had a female preponderance, with most patients aged 50 years and above. Diabetes mellitus is the most commonly associated comorbidity in such patients. Yap et al[35] observed diabetes in 90% of their EPN patients. Our study highlights a significant association between diabetes mellitus and EPN severity, with its prevalence increasing across severity groups (P = 0.035) (Table 3). Additionally, higher blood sugar and HbA1c levels were observed in patients with worse clinical outcomes (P < 0.01 and P = 0.023, respectively) (Table 4). Diabetes is known to impair immune function through mechanisms such as reduced neutrophil activity, microvascular dysfunction, and hyperglycemia-induced bacterial proliferation, all of which may contribute to more severe disease progression. While our results emphasize the role of diabetes, other comorbidities, such as chronic kidney disease and hypertension, may also influence outcomes. Further studies with multivariate analysis could help delineate the independent impact of diabetes on disease severity. These findings have important clinical implications, suggesting that glycemic control may play a role in risk stratification and treatment planning for EPN patients. Integrating diabetes status with prognostic scoring systems like NEWS 2 could enhance the early identification of high-risk individuals and guide more aggressive management strategies. While our study provides substantial evidence of an association, future prospective studies should evaluate whether targeted glycemic control can improve outcomes in this patient population.
A palpable tender kidney is one of the sure clinical signs associated with a higher mNEWS 2 score. All patients in group 3 and two-thirds in group 2 had a palpable tender kidney. Also, all eight early nephrectomies had a palpable tender kidney, while all eight who succumbed to this illness also had a palpable tender kidney. No other authors have correlated the significance of palpable kidneys to the ultimate treatment outcomes.
Trujillo et al[36] proposed a risk assessment score that predicted treatment outcomes in patients with EPN. In the largest-ever multi-centric study on EPN involving 570 patients from 15 centres, they proposed an 8-point scoring system to predict mortality in EPN[36]. They predicted a 100% mortality for a score of 7. In our study, two-thirds of our patients (66.67%) with a prognostic score of 22 and above succumbed to the illness.
Thrombocytopenia, chronic kidney disease, and hyponatremia at presentation were found to be associated with high mortality[37,38]. Our study also observed these biochemical parameters were significantly associated with higher mortality. Falagas et al[39], in their meta-analysis of 175 patients from 7 published studies, observed an overall mortality of 25%. They observed that mortality was associated with thrombocytopenia, conservative treatment, and bilaterality. Our study also noted these parameters closely correlating with higher mNEWS 2 scores.
To our knowledge, this is the first-ever and the largest single-centre study that compared the subgroups of group 3 of the NEWS 2 score. Our study stresses the need to implement mNEWS 2 scores in managing EPN patients. While the NEWS 2 score is a standardized system for triaging patients who need intensive monitoring, the conventional scoring exhibits a considerable overlap between the three groups. This necessitates and reinforces the growing need to modify the NEWS 2 score, which would greatly help the urologists prognosticate the treatment outcomes.
The revised scoring system can be easily incorporated into existing electronic medical record (EMR) systems, automated triage software, or bedside calculation tools, ensuring its practical implementation in emergency care. By improving the accuracy of risk stratification, mNEWS 2 enhances clinical decision-making without disrupting workflow efficiency. The mNEWS 2 score maintains the same core physiological parameters as the NEWS 2 system to ensure real-time usability. The reclassification does not require additional measurements or manual recalculations, allowing for rapid risk assessment at the point of care.
Our study provides valuable insights into the prognostic significance of NEWS 2 scores in EPN; however, certain limitations must be acknowledged.
The 12-year data collection period includes cases before the introduction of NEWS 2 in 2017, which may introduce inconsistencies, though standardized medical records ensured uniform data collection.
Variability in clinical management among multiple urologists could have influenced outcomes, but this reflects real-world practice, enhancing generalizability.
Demographic attributes such as origin, ethnicity, or language were not analyzed, as the focus was on clinical parameters and prognostic scoring in EPN. Future research incorporating demographic variations may provide further insights into population-specific disease patterns and management.
The small sample size of group 3 (n = 12) may limit subgroup analysis, though it aligns with the natural incidence of severe cases.
The study's single-centre design restricts external validity and ensures consistent data collection and standardized protocols. The lack of external validation is another limitation, emphasizing the need for a prospective multi-centre study to further substantiate findings, compare mNEWS 2 scores with other scoring systems, and assess the clinical applicability of mNEWS 2 in diverse populations.
Information bias from over-reliance on medical records and potential confounding factors such as prior treatments and pre-existing conditions may have influenced outcomes.
Lack of prospective validation is another limitation. It restricts the ability to fully assess the mNEWS 2 score's predictive accuracy compared to other established scoring systems. Future studies would focus on validating the score in larger, independent cohorts to strengthen its prognostic reliability.
To further improve global patient care for EPN, we propose integrating mNEWS 2 into EMR and clinical decision support systems for real-time triage and early intervention. Multi-centre validation studies and a global EPN registry could enhance risk prediction and treatment protocols. Machine learning models could further refine risk stratification, enabling personalized treatment pathways. Expanding telemedicine and remote monitoring can improve post-discharge follow-ups and early detection of complications. Finally, developing internationally standardized EPN management guidelines will ensure consistent, evidence-based treatment worldwide. These advancements will help reduce morbidity and mortality and optimize critical care decisions globally.
While the NEWS 2 score is an established scoring system for the initial triaging of patients with EPN, our study reiterates the need for a mNEWS 2 scoring to facilitate an appropriate assessment of treatment-related outcomes. A prompt diagnosis, early risk assessment, and proper treatment strategies based on the mNEWS 2 score would further reduce morbidity and mortality in patients with EPN. Our study introduces the mNEWS 2 score, a refined risk stratification tool for EPN, improving the predictive accuracy of the original NEWS 2 system. By reassessing cutoff thresholds, mNEWS 2 better correlates with disease severity, treatment outcomes, and mortality risk, enhancing clinical decision-making in urological emergencies. The mNEWS 2 scores should be seamlessly implemented into EMR, aiding real-time triage and patient management.
| 1. | Michaeli J, Mogle P, Perlberg S, Heiman S, Caine M. Emphysematous pyelonephritis. J Urol. 1984;131:203-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 209] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 2. | Chen CC, Hsieh MS, Hu SY, Huang SC, Tsai CA, Tsai YC. Performance of Scoring Systems in Predicting Clinical Outcomes of Patients with Emphysematous Pyelonephritis: A 14-Year Hospital-Based Study. J Clin Med. 2022;11:7299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (1)] |
| 3. | Jain A, Manikandan R, Dorairajan LN, Sreenivasan SK, Bokka S. Emphysematous pyelonephritis: Does a standard management algorithm and a prognostic scoring model optimize patient outcomes? Urol Ann. 2019;11:414-420. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 4. | Krishnamoorthy S, Zumla A, Sekar H, Muneer A, Thiruvengadam G, Kumaresan N. Prognostic scoring system and risk stratification in patients with emphysematous pyelonephritis: an 11-year prospective study at a tertiary referral centre. BJU Int. 2021;127:418-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Huang JJ, Tseng CC. Emphysematous pyelonephritis: clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern Med. 2000;160:797-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 437] [Cited by in RCA: 465] [Article Influence: 17.9] [Reference Citation Analysis (1)] |
| 6. | Ngo XT, Nguyen TT, Dobbs RW, Thai MS, Vu DH, Dinh LQV, Quy K, Le HT, Hoang TD, Ngo HTT, Van TNK, Tiong HY, Vuong HG. Prevalence and Risk Factors of Mortality in Emphysematous Pyelonephritis Patients: A Meta-Analysis. World J Surg. 2022;46:2377-2388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 7. | Desai R, Batura D. A systematic review and meta-analysis of risk factors and treatment choices in emphysematous pyelonephritis. Int Urol Nephrol. 2022;54:717-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 8. | Wu SY, Yang SS, Chang SJ, Hsu CK. Emphysematous pyelonephritis: classification, management, and prognosis. Tzu Chi Med J. 2022;34:297-302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 28] [Reference Citation Analysis (0)] |
| 9. | Rahoui M, Ouanes Y, Chaker K, Bibi M, Mourad Dali K, Sellami A, Ben Rhouma S, Nouira Y. Predictive factors for failure of conservative management in patients with emphysematous pyelonephritis. Ann Med Surg (Lond). 2022;78:103930. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 10. | Usman OA, Usman AA, Ward MA. Comparison of SIRS, qSOFA, and NEWS for the early identification of sepsis in the Emergency Department. Am J Emerg Med. 2019;37:1490-1497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 179] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 11. | Guan G, Lee CMY, Begg S, Crombie A, Mnatzaganian G. The use of early warning system scores in prehospital and emergency department settings to predict clinical deterioration: A systematic review and meta-analysis. PLoS One. 2022;17:e0265559. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 64] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 12. | Brink A, Alsma J, Verdonschot RJCG, Rood PPM, Zietse R, Lingsma HF, Schuit SCE. Predicting mortality in patients with suspected sepsis at the Emergency Department; A retrospective cohort study comparing qSOFA, SIRS and National Early Warning Score. PLoS One. 2019;14:e0211133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 119] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 13. | Churpek MM, Snyder A, Han X, Sokol S, Pettit N, Howell MD, Edelson DP. Quick Sepsis-related Organ Failure Assessment, Systemic Inflammatory Response Syndrome, and Early Warning Scores for Detecting Clinical Deterioration in Infected Patients outside the Intensive Care Unit. Am J Respir Crit Care Med. 2017;195:906-911. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 468] [Article Influence: 52.0] [Reference Citation Analysis (0)] |
| 14. | Roney JK, Whitley BE, Maples JC, Futrell LS, Stunkard KA, Long JD. Modified early warning scoring (MEWS): evaluating the evidence for tool inclusion of sepsis screening criteria and impact on mortality and failure to rescue. J Clin Nurs. 2015;24:3343-3354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 15. | Thorén A, Joelsson-Alm E, Spångfors M, Rawshani A, Kahan T, Engdahl J, Jonsson M, Djärv T. The predictive power of the National Early Warning Score (NEWS) 2, as compared to NEWS, among patients assessed by a Rapid response team: A prospective multi-centre trial. Resusc Plus. 2022;9:100191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 16. | Chen L, Zheng H, Chen L, Wu S, Wang S. National Early Warning Score in Predicting Severe Adverse Outcomes of Emergency Medicine Patients: A Retrospective Cohort Study. J Multidiscip Healthc. 2021;14:2067-2078. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 17. | McGinley A, Pearse RM. A national early warning score for acutely ill patients. BMJ. 2012;345:e5310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 106] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 18. | Jones M. NEWSDIG: The National Early Warning Score Development and Implementation Group. Clin Med (Lond). 2012;12:501-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 86] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 19. | Williams B. The National Early Warning Score: from concept to NHS implementation. Clin Med (Lond). 2022;22:499-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 83] [Reference Citation Analysis (0)] |
| 20. | Küçükceran K, Ayrancı MK, Koçak S, Girişgin AS, Dündar ZD, Ataman S, Bayındır E, Karaçadır O, Tatar İ, Doğru M. An Evaluation of the National Early Warning Score 2 and the Laboratory Data Decision Tree Early Warning Score in Predicting Mortality in Geriatric Patients. J Emerg Med. 2024;66:e284-e292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 21. | Pimentel MAF, Redfern OC, Gerry S, Collins GS, Malycha J, Prytherch D, Schmidt PE, Smith GB, Watkinson PJ. A comparison of the ability of the National Early Warning Score and the National Early Warning Score 2 to identify patients at risk of in-hospital mortality: A multi-centre database study. Resuscitation. 2019;134:147-156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 111] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 22. | Durantez-Fernández C, Martín-Conty JL, Polonio-López B, Castro Villamor MÁ, Maestre-Miquel C, Viñuela A, López-Izquierdo R, Mordillo-Mateos L, Fernández Méndez F, Jorge Soto C, Martín-Rodríguez F. Lactate improves the predictive ability of the National Early Warning Score 2 in the emergency department. Aust Crit Care. 2022;35:677-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 23. | Pullyblank A, Tavaré A, Little H, Redfern E, le Roux H, Inada-Kim M, Cheema K, Cook A; West of England Patient Safety Collaborative. Implementation of the National Early Warning Score in patients with suspicion of sepsis: evaluation of a system-wide quality improvement project. Br J Gen Pract. 2020;70:e381-e388. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 24. | Kırlı EA, Erdal FS, Özman O, Özalp AU, Selçuk B, Önal B. The Efficacy of Guy's Stone Score for Predicting the Stone-Free and Complication Rates in Children Treated by Percutaneous Nephrolithotomy. J Endourol. 2020;34:128-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 25. | Kumar U, Tomar V, Yadav SS, Priyadarshi S, Vyas N, Agarwal N, Dayal R. STONE score versus Guy's Stone Score - prospective comparative evaluation for success rate and complications in percutaneous nephrolithotomy. Urol Ann. 2018;10:76-81. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 26. | Khan N, Nazim SM, Farhan M, Salam B, Ather MH. Validation of S.T.O.N.E nephrolithometry and Guy's stone score for predicting surgical outcome after percutaneous nephrolithotomy. Urol Ann. 2020;12:324-330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 27. | Epstein M, Syed K, Danella J, Ginzburg S, Belkoff L, Tomaszewski J, Trabulsi E, Singer EA, Jacobs BL, Raman JD, Guzzo TJ, Uzzo R, Reese AC. Model risk scores may underestimate rate of biochemical recurrence in African American men with localized prostate cancer: a cohort analysis of over 3000 men. Prostate Cancer Prostatic Dis. 2024;27:257-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 28. | Zhao H, Li W, Li J, Li L, Wang H, Guo J. Predicting the Stone-Free Status of Percutaneous Nephrolithotomy With the Machine Learning System: Comparative Analysis With Guy's Stone Score and the S.T.O.N.E Score System. Front Mol Biosci. 2022;9:880291. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 29. | Tirkkonen J, Karlsson S, Skrifvars MB. National early warning score (NEWS) and the new alternative SpO(2) scale during rapid response team reviews: a prospective observational study. Scand J Trauma Resusc Emerg Med. 2019;27:111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 30. | Chawla A, Bhaskara SP, Taori R, de la Rosette JJMCH, Laguna P, Pandey A, Mummalaneni S, Hegde P, Rao S, K P. Evaluation of early scoring predictors for expedited care in patients with emphysematous pyelonephritis. Ther Adv Urol. 2022;14:17562872221078773. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 31. | Kim Y, Seo MR, Kim SJ, Kim J, Wie SH, Cho YK, Lim SK, Lee JS, Kwon KT, Lee H, Cheong HJ, Park DW, Ryu SY, Chung MH, Pai H. Usefulness of Blood Cultures and Radiologic Imaging Studies in the Management of Patients with Community-Acquired Acute Pyelonephritis. Infect Chemother. 2017;49:22-30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 32. | Elbaset MA, Zahran MH, Hashem A, Ghobrial FK, Elrefaie E, Badawy M, Shokeir AA, Ibrahim MA. Could platelet to leucocytic count ratio (PLR) predict sepsis and clinical outcomes in patients with emphysematous pyelonephritis? J Infect Chemother. 2019;25:791-796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 33. | Bedoui MA, Saadi A, Zaghbib S, Mokadem S, Boussaffa H, Hermi A, Ayed H, Bouzouita A, Chakroun M, Ben Slama R. Risk factors for sepsis and mortality in patients with emphysematous pyelonephritis : a series of 68 cases (case series). Ann Med Surg (Lond). 2024;86:240-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 34. | Bibi M, Chaker K, Ouanes Y, Baccouch R, Madani MA, Mediouni H, Mosbahi B, Mourad Dali K, Rahoui M, Nouira Y. Comparison of prognosis of five scoring systems in emphysematous pyelonephritis patients requiring intensive care. Int Urol Nephrol. 2023;55:3045-3050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 35. | Yap XH, Ng CJ, Hsu KH, Chien CY, Goh ZNL, Li CH, Weng YM, Hsieh MS, Chen HY, Chen-Yeen Seak J, Seak CK, Seak CJ. Predicting need for intensive care unit admission in adult emphysematous pyelonephritis patients at emergency departments: comparison of five scoring systems. Sci Rep. 2019;9:16618. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 36. | Trujillo-Santamaría H, Robles-Torres JI, Teoh JY, Tanidir Y, Campos-Salcedo JG, Bravo-Castro EI, Wroclawski ML, Yeoh WS, Kumar S, Sanchez-Nuñez JE, Espinoza-Aznar JE, Ragoori D, Hamri SB, Aik OT, Tarot-Chocooj CP, Shrestha A, Lakmichi MA, Cosentino-Bellote M, Vázquez-Lavista LG, Kabre B, Tiong HY, Arrambide-Herrera JG, Gómez-Guerra LS, Kutukoglu U, Alves-Barbosa JAB, Jaspersen J, Acevedo C, Virgen-Gutiérrez F, Agrawal S, Duarte-Santos HO, Ann CC, Castellani D, Gahuar V. A novel mortality risk score for emphysematous pyelonephritis: A multicenter study of the Global Research in the Emphysematous Pyelonephritis group. Curr Urol. 2024;18:55-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 37. | Kapoor R, Muruganandham K, Gulia AK, Singla M, Agrawal S, Mandhani A, Ansari MS, Srivastava A. Predictive factors for mortality and need for nephrectomy in patients with emphysematous pyelonephritis. BJU Int. 2010;105:986-989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 80] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 38. | Aswathaman K, Gopalakrishnan G, Gnanaraj L, Chacko NK, Kekre NS, Devasia A. Emphysematous pyelonephritis: outcome of conservative management. Urology. 2008;71:1007-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 70] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 39. | Falagas ME, Alexiou VG, Giannopoulou KP, Siempos II. Risk factors for mortality in patients with emphysematous pyelonephritis: a meta-analysis. J Urol. 2007;178:880-5; quiz 1129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 122] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/