Published online Jun 25, 2025. doi: 10.5527/wjn.v14.i2.100092
Revised: January 15, 2025
Accepted: January 23, 2025
Published online: June 25, 2025
Processing time: 245 Days and 11.2 Hours
Surgically created arterio-venous fistulas (AVFs) are the gold standard for haemodialysis access for patients with end-stage renal disease. Standard practice of AVF creation involves selecting the non-dominant upper limb and starting with most distally with radio-cephalic arterio-venous fistula. The primary patency rate of radio-cephalic arterio-venous fistula varies from 20%-25%. It has been suggested the neointimal hyperplasia at the mobilized venous segment causes stenosis of the anastomosis. Therefore, the radial artery deviation and reim
To compare the RADAR technique with classical technique in creation of AVF including: (1) Success rate; (2) Time to maturation; (3) Duration of surgery; and (4) Complication rate.
In our study we recruited 94 patients in two randomized groups and performed the AVF by the classical method or the RADAR method.
The RADAR group had higher primary success rate (P = 0.007), less rate of complications (P = 0.04), shorter duration of surgery (P = 0.00) and early time to maturation (0.001) when compared with the classical group. The RADAR proce
The RADAR procedure is a safe and more efficient alternative to the current classical method of AVF creation. Longer duration of follow-up is required to assess the long-term outcomes in the future.
Core Tip: Creating an arterio-venous fistula is a complex surgical procedure that often faces high failure rates. Ensuring appropriate patient selection and thorough preoperative optimization are crucial for successful outcomes. The radial artery deviation and reimplantation procedure offers a safer and more efficient alternative to the traditional method of arterio-venous fistula creation. However, extended follow-up is necessary to evaluate its long-term effectiveness.
- Citation: Sarangi SS, Kumar S, Bhirud DP, Singh M, Navriya SC, Choudhary GR, Sandhu AS. Radial artery deviation and reimplantation technique vs classical technique in arterio-venous fistula: A randomised control trial. World J Nephrol 2025; 14(2): 100092
- URL: https://www.wjgnet.com/2220-6124/full/v14/i2/100092.htm
- DOI: https://dx.doi.org/10.5527/wjn.v14.i2.100092
Chronic kidney disease (CKD) is a burden of enormous proportion on the global health infrastructure. There are about upwards of 70 lakh patients living in CKD and with a dearth of organ donors, most of these patients remain on haemodialysis (HD). Such patients require a reliable repeatable vascular access for HD. Surgically created arterio-venous fistula (AVF) is the gold standard for HD access. Although the AVF can be created relatively quickly and under local anaesthesia, the surgery is technically demanding. Standard practice of AVF creation involves selecting the non-dominant upper limb for radio-cephalic arterio-venous fistula (RC-AVF) and selecting sites that are more proximal if it fails. The major drawback of the procedure is the poor early patency rate. Neointimal hyperplasia near the anastomotic site has been observed by a landmark paper by Sadaghianloo et al[1], in the mobilized segment (e.g., the proximal vein mobilized to form the end-to-side anastomosis). This surgically mobilized segment coincides with turbulent flow as well as with devascularisation of the vasa vasorum; leading to intimal hyperplasia and stenosis. Therefore, a surgical technique, that minimizes venous dissection may improve rate of fistula maturation and access patency. In our study, we randomized the patients undergoing AVF creation in our institute into two groups and compared the outcomes of radial artery deviation and reimplantation (RADAR) technique vs the classical technique.
The study was conducted at Department of Urology, All India Institute of Medical Sciences Jodhpur from March 2021 to September 2022. All the patients, undergoing AVF creation and considering the inclusion and exclusion criteria; were recruited in the study. The inclusion criteria were; age > 18 years, patients needing AVF for HD. The exclusion criteria were; incomplete palmar arch, previously failed AVF at wrist, severe calcification or atherosclerosis in artery, un-correctable coagulopathy, unwilling to participate, radial artery diameter < 2 mm, cephalic vein diameter of < 2 mm and/or presence of thrombosis. Sample size was calculated using the following formula for randomized control trial for statistical superiority design with dichotomous variable.
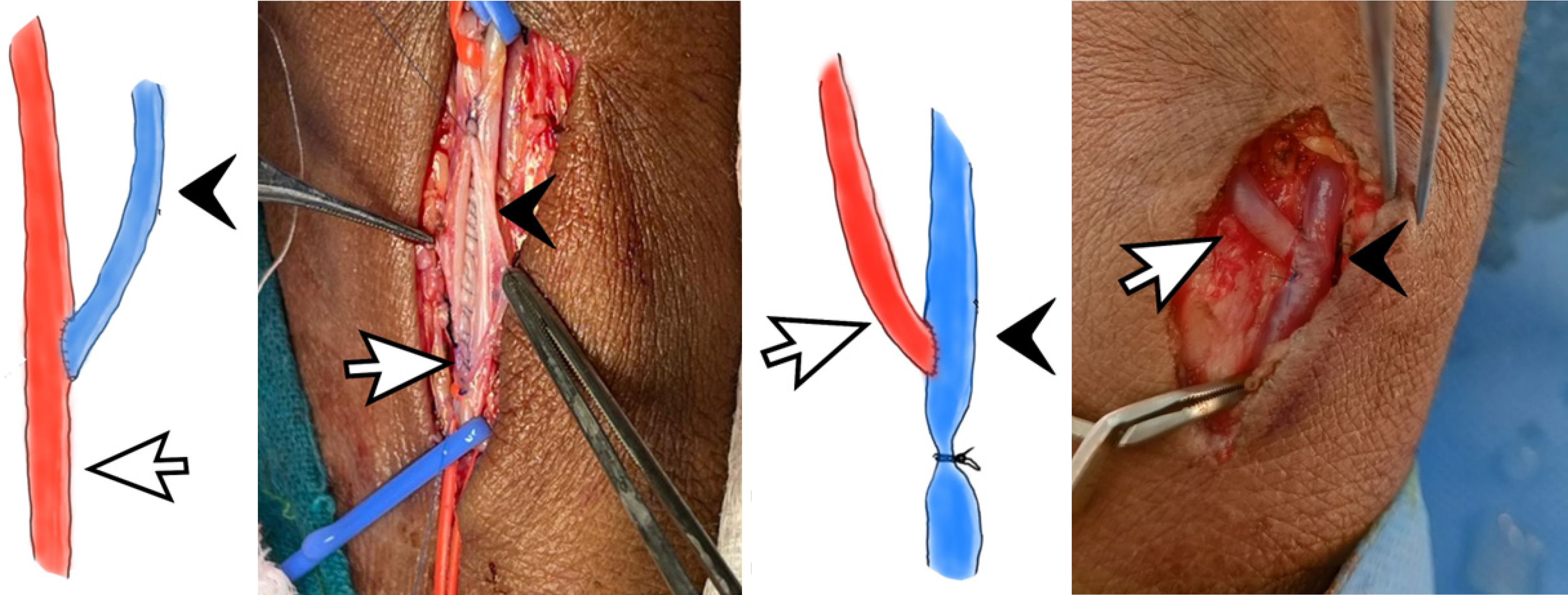
N = size per group; p = the response rate of standard treatment group (classical AVF; 60%[2,3]); p0 = the response rate of new treatment group (RADAR AVF; 85%[3]); zx = the standard normal deviate for a one- or two-sided x. Where α = 0.05, β = 0.20 and keeping in mind the fact that power of study being 80%. Minimum sample size calculated from above formula comes out to be 47 in each group. Randomization was done by computer generated random numbers. Patients’ baseline assessment including the demographic characteristics, medical history, physical examination, ultrasound guidance (USG) doppler of both limbs or non-dominant limb where AVF is planned to characterises status of vessels along with routine investigations for AVF surgery. Institutional ethics and review committee, approval No. AIIM/IEC/2021/3324 was obtained to conduct the study in our institute, and informed consent for the surgery was taken during the treatment. The procedures adhered to the ethical guidelines of Declaration of Helsinki and its amendments. We confirm the availability of, and access to, all original data reported in this study. Team of urologist who were experienced in AVF surgery performed all the procedures. All AVFs creation were performed by surgeons with substantial experience in both RADAR and conventional classic technique, ensuring proficiency in both approaches. The procedures were performed under local anesthesia. The patients undergoing the standard technique, the AVF was created with end vein anastomosed to the artery in end to side manner. The patients undergoing the RADAR technique, the radial artery was mobilized and anastomosed to the side of cephalic vein and the distal end of the cephalic vein was ligated making it a functional end to end anastomosis (Figure 1). Assessment of the following aspects were done between these two groups for comparison; time taken for completion of procedure, immediate complications in terms of bleeding, hematoma, thrombosis, gangrene, pulmonary edema, delayed postoperative complications like - steal phenomenon, venous hypertension, time to maturation of fistulas (post-operative day of starting of dialysis), primary failure rate and any re-exploration.
The data so collected was entered into an excel sheet and analysis was done using SPSS 25 (SPSS Inc, Chicago, Il, United States) software. Appropriate statistical tests were applied and P value of < 0.05 was regarded as significant.
Total of 107 cases were operated for RC-AVF during the study period. Of these, 94 patients were enrolled in our study and 13 patients were excluded. The excluded cases had vascular characteristics pertaining to the exclusion criteria (8 patients had vessel diameter less than that mentioned in exclusion criteria and 5 patients had incomplete palmar arch). The remaining 94 cases enrolled in our study, were divided into two groups by computer generated randomization of 47 in each. While our study includes 94 patients, which may indeed limit the generalizability of our findings, we believe it provides valuable initial insights into the comparative outcomes of RADAR vs conventional classic technique of AV fistula creation. The single-center nature of this study allowed us to maintain consistency in surgical protocols and data collection.
We fully agree that larger, multicenter studies are essential to validate and generalize these findings across diverse patient populations and clinical settings. This study serves as a foundation for such future research endeavors. Both the groups had similar demographic profiles and it is summarized in the following table (Table 1). When comparing the vessel diameters with maturation period, a linear correlation emerged. All the intrinsic patient specific factors which could lead to a change in outcome and can introduce a bias like, the arterial diameter, the diameter of vein, duration of CKD and duration of HD prior to surgery were evaluated for their effect on success of the surgery individually. All the patients included in the study were diagnosed with CKD stage 5 and had hypertension as the only comorbidity. Vein quality was clinically assessed and determined to have good caliber and patency, while the arterial condition in all patients was deemed to be in an apparently satisfactory state based on clinical evaluation. We acknowledge, however, that a more extensive analysis of these patient-specific variables could provide deeper insights into their potential impact on outcomes. Future studies with larger cohorts and detailed assessments of these factors will help to better delineate their influence and further refine patient selection and management strategies. The individual parameters were analyzed with t-test and 95% confidence interval (CI) was calculated. The intraoperative findings were also noted and compared among both the groups. The time duration taken for completion of a procedure was measured. The average duration to complete a procedure for the RADAR group was 1 hour 40 minutes, while for the classical group it was 1 hour 55 minutes. The time duration was split into 4 categories, i.e. < 1:30 hours, 1:31-1:45 hours, 1:46-2:00 hours, > 2:00 hours and was analyzed for statistically significance difference if any. It was noted that, in the RADAR group; the procedure could be completed relatively quickly which was statistically significant (P value = 0.001).
| Variable | RADAR (n = 47) | Classical (n = 47) | P value |
| Average age (year), mean ± SD | 44.36 ± 15.85317 | 47.42 ± 15.85317 | 0.856 |
| Sex | |||
| Male | 37 (78.7) | 33 (70.2) | 0.344 |
| Female | 10 (21.3) | 14 (29.8) | - |
| Comorbidities | |||
| HTN | 44 (93.6) | 42 (89.36) | 0.24 |
| DM | 8 (17.02) | 12 (25.53) | 0.17 |
| CAD | 4 (8.51) | 2 (4.25) | 0.20 |
| Others | 1 (2.12) | 2 (4.25) | 0.28 |
| Diameter (mm), mean ± SD | |||
| Artery | 2.18 ± 0.20358 | 2.18 ± 0.22824 | 0.159 |
| Vein | 2.29 ± 0.24181 | 2.36 ± 0.38086 | 0.200 |
| CKD diagnosis (months), mean ± SD | 2.7553 ± 2.16412 | 3.13 ± 2.795 | 0.472 |
| HD duration (months), mean ± SD | 1.64 ± 0.814 | 1.91 ± 1.943 | 0.390 |
| BMI, mean ± SD | 23.4043 ± 1.34342 | 22.8745 ± 1.77415 | 0.472 |
There were no cases of any death, ischemia or surgical site infection noted in either group. Two patients, one from each group had minor complications in the form of edema over the dorsum of hand and surrounding the surgical site which resolved on conservative management (limb elevation). Two patients in the RADAR group had acute onset breathlessness and pulmonary edema just after completion of the procedure. These two patients needed immediate HD for stabilization. One patient from each group underwent re-exploration for thrombosis on post-operative day 1. Comparing the complication rates in both the groups did produce a statistically significant result (P value = 0.044) in favor of the RADAR group.
Comparing the failure rates, 11 patients in the classical group had failure while only 2 patients in the RADAR group had failure (P value = 0.007). Two patients in the classical group had low flow across the AVF. Although these patients did not technically had failure, but HD could not be started during the 3 months follow-up period and they were analyzed as failure. Out of the two patients who underwent re-exploration for thrombosis in the post-operative period, one from the classical group later went on to have functional AVF, however he was evaluated as a failure in the analysis. There were no instances of abandoned AVF or secondary failures. None of the patients underwent any endovascular procedure. When comparing the all-cause complication rates for both the groups, the result came out to be statistically significant (P value = 0.049).
While our study focuses on short- to mid-term outcomes, we acknowledge that long-term follow-up is crucial to fully evaluate the durability and patency of AVF. The current study was limited by the follow-up period of 3 months due to resource and time constraints. However, we believe it provides important preliminary data on early outcomes and complications, which are critical in the initial stages of AVF care. We agree that future studies with extended follow-up periods are necessary to assess long-term durability and patency comprehensively. This will be a priority in our subsequent research efforts.
The average time to maturation of fistula was measured as when the fistula was ready to support HD. The duration of maturation period was divided into two categories for analysis, that is less than 4 weeks and more than 4 weeks. Analyzing the data, the RADAR group had statistically significant result (P value = 0.001).
Once HD was started for a patient, the patient was evaluated at the end of 3 months follow-up period to assess whether HD was being continued or not. This was the patency rates of each group. All the patients after initiation of HD had continued HD at the end of 3 months. All the patient specific factors, that can affect the surgical outcome, were analyzed to test the individual factor’s influence and the results were noted (Table 2). The P value in the duration of maturation category came to be 0.001 which was suggestive of clinically significant outcome.
| Variable | Classical | RADAR | P value |
| Duration of CKD (months) | 3.13 ± 2.795 | 2.76 ± 2.164 | 0.472 |
| Duration of hemodialysis (months) | 1.91 ± 1.943 | 1.65 ± .814 | 0.389 |
| Radial artery diameter (mm) | 2.1630 ± 2.0616 | 2.1872 ± 1.4237 | 0.509 |
| Cephalic vein diameter (mm) | 2.2277 ± 3.6576 | 2.3021 ± 2.3636 | 0.244 |
| Time for maturation (in days) | 37.78 ± 5.683 | 28.33 ± 5.437 | 0.001 |
All the outcome factors, i.e.; success rate, complication rate, time to maturation and continuation of dialysis, were evaluated with univariate analysis to calculate the odds ratio (OR) with respect to procedure (Table 3). The RADAR group was taken as reference for calculation. The unadjusted OR for the success rate was 0.145 and the P value was calculated to be 0.016. The unadjusted OR for the complication rate was 2.899 and the P value was calculated to be 0.049. The unadjusted OR for the maturation time was 18.874 with 95%CI being 15.136 the upper and 22.613 the lower limit. The P value was calculated to be 0.001. The unadjusted OR for the continuation of dialysis was 0.252 with 95%CI being 0.065 the upper and 0.985 the lower limit. The P value was calculated to be 0.048.
| Variable | n | Unadjusted OR | 95%CI | P value |
| Success | ||||
| RADAR (Ref) | 45 (95.74) | - | - | - |
| Classical | 36 (76.59) | 0.145 | 0.030-0.699 | 0.016 |
| Complication | ||||
| RADAR (Ref) | 6 (12.8) | - | - | - |
| Classical | 14 (29.8) | 2.899 | 1.004-8.372 | 0.049 |
| Maturation time | ||||
| RADAR (Ref) | 28.33 | - | - | - |
| Classical | 37.78 | 18.874 | 15.136-22.613 | 0.001 |
The various factors which are supposed to affect the success rate were evaluated with univariate regression analysis and the unadjusted OR and 95%CI was calculated (Table 4). Out of which, the cephalic vein diameter came out to be statistically significant with P value being 0.003. The RADAR procedure was associated with higher success rate with P value being 0.016. Rest of the parameters came out to be statistically insignificant. The statistically significant factors were then analyzed for significance with multivariate analysis. The P value for the RADAR procedure came out to be 0.018. The P value for cephalic vein diameter came out to be 0.002 (Table 4).
| Univariate regression analysis | |||
| Variable | Unadjusted OR | 95%CI | P value |
| Age (years) | |||
| 18-40 (Ref) | - | - | 0.360 |
| 40-55 | 0.628 | 0.180-2.194 | 0.466 |
| > 55 | 2.879 | 0.313-26.506 | 0.351 |
| Sex | |||
| Male | 0.333 | 0.099-1.118 | 0.075 |
| Female (Ref) | |||
| CKD duration | 0.909 | 0.742-1.114 | 0.358 |
| Hemodialysis duration | 1.376 | 0.657-2.880 | 0.397 |
| BMI | 1.144 | 0.793-1.651 | 0.472 |
| Radial artery diam | 3.961 | 0.088-178.903 | 0.479 |
| Cephalic vein diam | 15.969 | 14.160-25.856 | 0.003 |
| Procedure | |||
| Radar (Ref) | 0.145 | 0.030-0.699 | 0.016 |
| Classical | |||
| Maturation time | 0.744 | 0.540-1.025 | 0.070 |
| Complication | 0.000 | 0.000 | 0.996 |
| Multivariate regression analysis | |||
| RADAR (Ref) | 0.091 | 0.013-0.663 | 0.018 |
| Cephalic vein diameter | 3.907 | 2.397-31.3 | 0.002 |
The AVF for HD has been through many iterations over the period of years. All the forms are associated with failure rates which are quite high and the search for an ideal method is still on going. One study by Wolowczyk et al[4] published in January 2000 retrospectively analyzed the patency rate of RC-AVF done in the snuff box4. There were 11% occurrence of thrombosis within the first 24 hours. The maturation rate was 80% at six weeks. The patency rate was 65% at 1 year. This approach could provide with a long segment arterialization of vein with preservation of more proximal veins for further intervention if required. However, this method had higher failure rates when compared with the classical method which had failure rates around 20%-25% (Our study 23.4%). Hence this method could not gain popularity and was abandoned in favor of the classical method.
Similar results were noted by Sadaghianloo et al[1]. They noted that the RADAR group had excellent primary patency rates, secondary patency rates and maturation rates. There were also significantly less intervention rates. In our study, the RADAR group had similar or low complication rates when compared with the classical method and it was statistically significant (P value = 0.44). Two patients in the RADAR group had pulmonary edema in the immediate post-operative period needing HD. While these can be an isolated event, due to pre-existing undiagnosed cardiac condition or it might be due to the immediate high flow rates across the AVF following the RADAR procedure. In a meta-analysis conducted by Al-Jaishi et al[5] showed a cumulative primary failure rate of 23%. In our study, the classical group had primary failure rate of (23.4%), which is similar to previously reported studies. However, the RADAR group had significantly lower rates of primary failure rates at only 4.2%. The reason for this result may be dependent on the physics of the procedure itself.
Allon et al[6] evaluated the effect of preoperative mapping of vessels with USG for planning of surgery. They noted that with USG mapping and better planning, the fistulas could be made with higher success rate. The rate of adequacy increased from 46% to 54%. Marked improvement was noted among diabetic (21% to 50%) and female patients (7% to 36%). Such cases are supposedly have compromised vascular status in terms of atherosclerosis and small diameter of vessels. The initial pre-operative work-up included the USG doppler study of vessels. Our study showed that the initial diameter the veins can significantly affect the outcomes of the procedure. Irrespective of the procedure, the vein diameters were independent predictors of a successful AVF creation. A study conducted by Khavanin Zadeh et al[7] also found a similar relation between the preoperative vein diameter and time to maturation with a larger vein diameter resulting in a favorable outcome. This finding further solidifies the role of clinical examination before a patient is undertaken for AVF creation.
It has been known historically that, hypertension (HTN) favors AVF patency. The higher blood pressure maintains adequate flow across the newly created AVF and helps preventing thrombus formation. This observation was initially made by Feldman et al[8]. We had 86 (91.48%) patients with HTN which might be a leading cause of higher success rate in our study when compared with other similar studies. The duration since diagnosis of CKD to AVF creation and the period of maintenance HD have also been implicated as significant predictors of outcome. It has been observed since long that advanced uremic condition (longer duration since diagnosis of CKD to AVF creation) can lead to higher failure rates. Smith et al[9] in their study noted that patients undergoing AVF creation preemptively had a higher success rate. Similarly, patient who were on HD for a longer period of time had poorer outcome after AVF creation[8]. When compared for success rates of AVF creation in our study, both the CKD duration and HD duration the outcome was statistically insignificant. This is contrary to some of the previously done studies[9]. This discrepancy can be due to the fact that the time period from diagnosing CKD to performing AVF and duration of HD was relatively short.
In our study, we measured the time duration for each procedure as an indicator for ease of doing the procedure. As per our knowledge, ours is the only randomized control trial comparing the RADAR method with the classical method. Both the procedures were compared and the time duration to perform a procedure came out to be significant (P value = 0.001) in favor of the RADAR group. Such finding can be attributed to relative simplification of steps of doing the procedure in the RADAR group. Unlike other procedures, the AVF after its creation is subjected to adverse conditions continuously in the form of turbulent blood flow, pricks for HD and also the CKD status of the patient itself. Moreover, the surgical procedure itself has some inherent factors for failure. One of such factors is the angle between the two vessels being anastomosed. If the angle is too acute, then the blood flows with excessive turbulence and may lead to stenosis later. Likewise, overzealous dissection of the vein can lead to damage to the vasa vasorum of the vein. These factors lead to a cascade of abnormal wound healing and result in neointimal hyperplasia in the venous channel of the AVF. The RADAR technique addresses both these issues and this might be the cause behind the higher success rate in the RADAR group. In the RADAR technique the artery is mobilized in a gentle curve so as to make a favorable angle for anastomosis. Not disturbing the venous channel helps in preserving the vasa vasorum and possibly contributes the higher success rate in this group.
While analyzing the various patient factors in success or failure of AVF, one of the crucial factors that sometimes is overlooked, i.e., the surgeon. The surgeon plays crucial role in performing any surgery and the role of the surgeon is indispensable in high stake surgeries like AVF creation. One study by Prischl et al[10] addresses this issue. They analyzed the outcome of AVF from various parameters including the operating surgeons. They concluded that, when the groups are matched demographically; the surgeon is the most important factor determining the outcome of the procedure. Similarly in our study, only the same group of experienced surgeons performed all the cases. The performing surgeons had more than 50 cases experience in doing the classical AVF and also performed 10 RADAR procedures each before the study was initiated. This led to standardization of surgical steps and overcame the learning curve and associated failure rates.
The timing of creating AVF is also of paramount importance. In a study published in 1998 by Hakim et al[11], discusses this point in detail. They noted that, early placement of a vascular access improves the survival of the access. In our study, the average duration from starting of HD to AVF creation was within 2 months, while 3 cases underwent pre-emptive AVF creation. This might be a reason behind the better outcome in our study population. This study further acknowledges the many nuances of AVF and recommends to perform vascular access surgery as early as possible for better patient outcome and AVF survival too. We found that clinical examination of veins closely corelates with outcome and also predicts a shorter duration of maturation. Malovrh et al[12], also found similar findings in his study. He found that proper clinical examination is as good as or even better than doppler USG in predicting the outcome. There has been only one more study comparing the classical group and RADAR group by Sadaghianloo et al[1]. This comparison shows that, our study is comparable to previous studies as far as the classical group is considered. The RADAR group performed better than many previous study cohorts.
The AVF creation is a technically demanding surgery with high failure rates. Proper patient selection and preoperative optimization is of paramount importance in success of the procedure. The RADAR procedure is a safe and more efficient alternative to the current classical method of AVF creation. Longer duration of follow-up is required to assess the long-term outcomes in the future.
| 1. | Sadaghianloo N, Declemy S, Jean-Baptiste E, Haudebourg P, Robino C, Islam MS, Hassen-Khodja R, Dardik A. Radial artery deviation and reimplantation inhibits venous juxta-anastomotic stenosis and increases primary patency of radial-cephalic fistulas for hemodialysis. J Vasc Surg. 2016;64:698-706.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (1)] |
| 2. | Allon M, Robbin ML. Increasing arteriovenous fistulas in hemodialysis patients: Problems and solutions. Kidney Int. 2002;62:1109-1124. [PubMed] [DOI] [Full Text] |
| 3. | Patel ST, Hughes J, Mills JL Sr. Failure of arteriovenous fistula maturation: an unintended consequence of exceeding dialysis outcome quality Initiative guidelines for hemodialysis access. J Vasc Surg. 2003;38:439-45; discussion 445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 192] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 4. | Wolowczyk L, Williams AJ, Donovan KL, Gibbons CP. The snuffbox arteriovenous fistula for vascular access. Eur J Vasc Endovasc Surg. 2000;19:70-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 61] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Al-Jaishi AA, Oliver MJ, Thomas SM, Lok CE, Zhang JC, Garg AX, Kosa SD, Quinn RR, Moist LM. Patency rates of the arteriovenous fistula for hemodialysis: a systematic review and meta-analysis. Am J Kidney Dis. 2014;63:464-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 399] [Cited by in RCA: 499] [Article Influence: 41.6] [Reference Citation Analysis (0)] |
| 6. | Allon M, Lockhart ME, Lilly RZ, Gallichio MH, Young CJ, Barker J, Deierhoi MH, Robbin ML. Effect of preoperative sonographic mapping on vascular access outcomes in hemodialysis patients. Kidney Int. 2001;60:2013-2020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 333] [Cited by in RCA: 324] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 7. | Khavanin Zadeh M, Gholipour F, Naderpour Z, Porfakharan M. Relationship between Vessel Diameter and Time to Maturation of Arteriovenous Fistula for Hemodialysis Access. Int J Nephrol. 2012;2012:942950. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 8. | Feldman HI, Joffe M, Rosas SE, Burns JE, Knauss J, Brayman K. Predictors of successful arteriovenous fistula maturation. Am J Kidney Dis. 2003;42:1000-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 180] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 9. | Smith GE, Gohil R, Chetter IC. Factors affecting the patency of arteriovenous fistulas for dialysis access. J Vasc Surg. 2012;55:849-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 182] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 10. | Prischl FC, Kirchgatterer A, Brandstätter E, Wallner M, Baldinger C, Roithinger FX, Kramar R. Parameters of prognostic relevance to the patency of vascular access in hemodialysis patients. J Am Soc Nephrol. 1995;6:1613-1618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 107] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | Hakim R, Himmelfarb J. Hemodialysis access failure: a call to action. Kidney Int. 1998;54:1029-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 186] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 12. | Malovrh M. Native arteriovenous fistula: preoperative evaluation. Am J Kidney Dis. 2002;39:1218-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 208] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/