INTRODUCTION
Point of care ultrasonography (POCUS) is a focused ultrasound examination performed by the treating clinician at the bedside to address specific questions that aid in guiding patient management[1]. Ultrasonography itself has been a trusted imaging modality for several decades. During the 1980s, the development of real-time ultrasound revolutionized the way sonographic images were viewed, eliminating any lag between signal generation and image display. This breakthrough created new opportunities for physicians to perform bedside ultrasound evaluations of trauma patients in emergency settings, leading to the evolution of the POCUS we recognize today[2]. With ongoing technological advancements and the miniaturization of ultrasound devices, POCUS has gained significant momentum in the recent past emerging as the fifth pillar of physical examination alongside traditional four pillars, namely inspection, palpation, percussion, and auscultation. As such, it is being incorporated into medical school curricula. According to a 2019 survey, over 70% of the responding medical schools in the United States reported having a formal POCUS curriculum. Interestingly, 73.8% of these schools have integrated POCUS into basic science courses, highlighting its role in establishing a strong foundation in anatomy and physiology before entering the clinical years[3]. Despite growing interest, the adoption of diagnostic POCUS in nephrology remains sparse and comprehensive training beyond kidney ultrasound is only offered by a few select fellowship programs[4]. This has two significant implications for the near future. Firstly, prospective nephrology fellows who already received basic POCUS training and anticipate learning specialty-specific POCUS applications during their fellowship are left disappointed. This negatively impacts the already dwindling interest in nephrology as a career choice. Secondly, when fellows with some POCUS training use it during rounds, it can create confusion in the clinical decision-making process if the supervising physicians are unfamiliar with the findings. In addition to the lack of trained faculty, several misconceptions surrounding the use of POCUS hinder its widespread adoption. In this minireview, we aim to dispel common myths associated with integrating POCUS into day-to-day nephrology practice.
Myth: Pocus is the same as a comprehensive ultrasound study performed by the radiology department
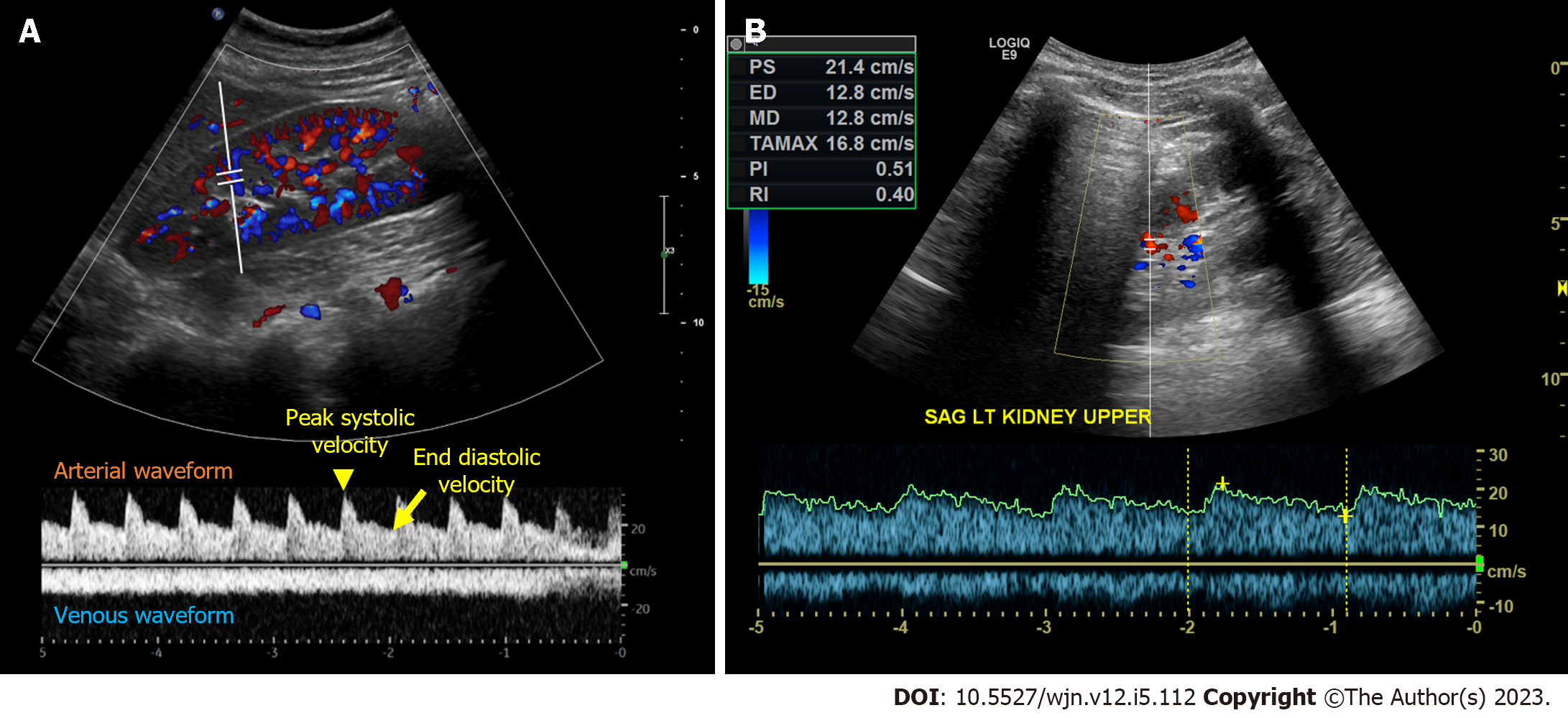
POCUS constitutes limited ultrasound examinations performed by the clinician at the patient’s bedside, with the specific purpose of answering “focused questions” to confirm a suspected diagnosis or narrow down the differential. Examples of such questions include, “Does this patient with acute kidney injury (AKI) have hydronephrosis?”, “Does this patient with intra-dialytic hypotension have pericardial effusion?”, or “Is this location of arteriovenous fistula suitable for cannulation?”. On the other hand, comprehensive referral ultrasound studies performed by the radiology or cardiology departments involve a thorough assessment of an anatomical region, documenting predefined parameters and measurements. In addition, POCUS reduces fragmentation of care by allowing multiple evaluations performed during the same study. For example, a nephrologist evaluating a patient with suspected congestive nephropathy can assess cardiac function, right atrial pressure, presence or absence of venous congestion, pleural effusion, and ascites in a few minutes at bedside[5,6]. In contrast, without POCUS, obtaining answers to the same questions would require ordering a multitude of studies, including an echocardiogram, a chest radiograph, an abdominal sonogram, and a duplex study of the right upper quadrant and kidney. This process would consume significant time and resources, more so when repeating an entire study to follow one or two imaging parameters (e.g., improvement in Doppler stigmata of venous congestion). With that being said, POCUS users need to use their clinical judgement in order to decide when a focused examination would suffice and when a more extensive assessment may be necessary to make accurate and informed clinical decisions. For instance, while a nephrologist using POCUS might be able to detect mitral regurgitation as a potential cause for unilateral pulmonary edema, accurately grading the lesion and providing detailed information related to mitral valve surgery would be beyond their expertise. Likewise, while a POCUS user may suspect renal artery stenosis based on the intrarenal Doppler waveform, performing a comprehensive evaluation would be time-consuming and necessitates skill levels beyond typical POCUS training (Figure 1).
Figure 1 Intrarenal Doppler.
A and B: Intrarenal Doppler demonstrated normal waveforms (A), tardus parvus (B) waveform in a case of suspected renal artery stenosis that should warrant further investigations such as radiology-performed Doppler ultrasonography and/or magnetic resonance angiography. A and B: Citation: Batool A, Chaudhry S, Koratala A. Transcending boundaries: Unleashing the potential of multi-organ point-of-care ultrasound in acute kidney injury. World J Nephrol 2023; 12: 93-103. Copyright© The Authors 2023. Published by Baishideng Publishing Group Inc (corresponding author’s prior open access publication).
Myth: Pocus is unnecessary if we improve training in conventional physical examination skills
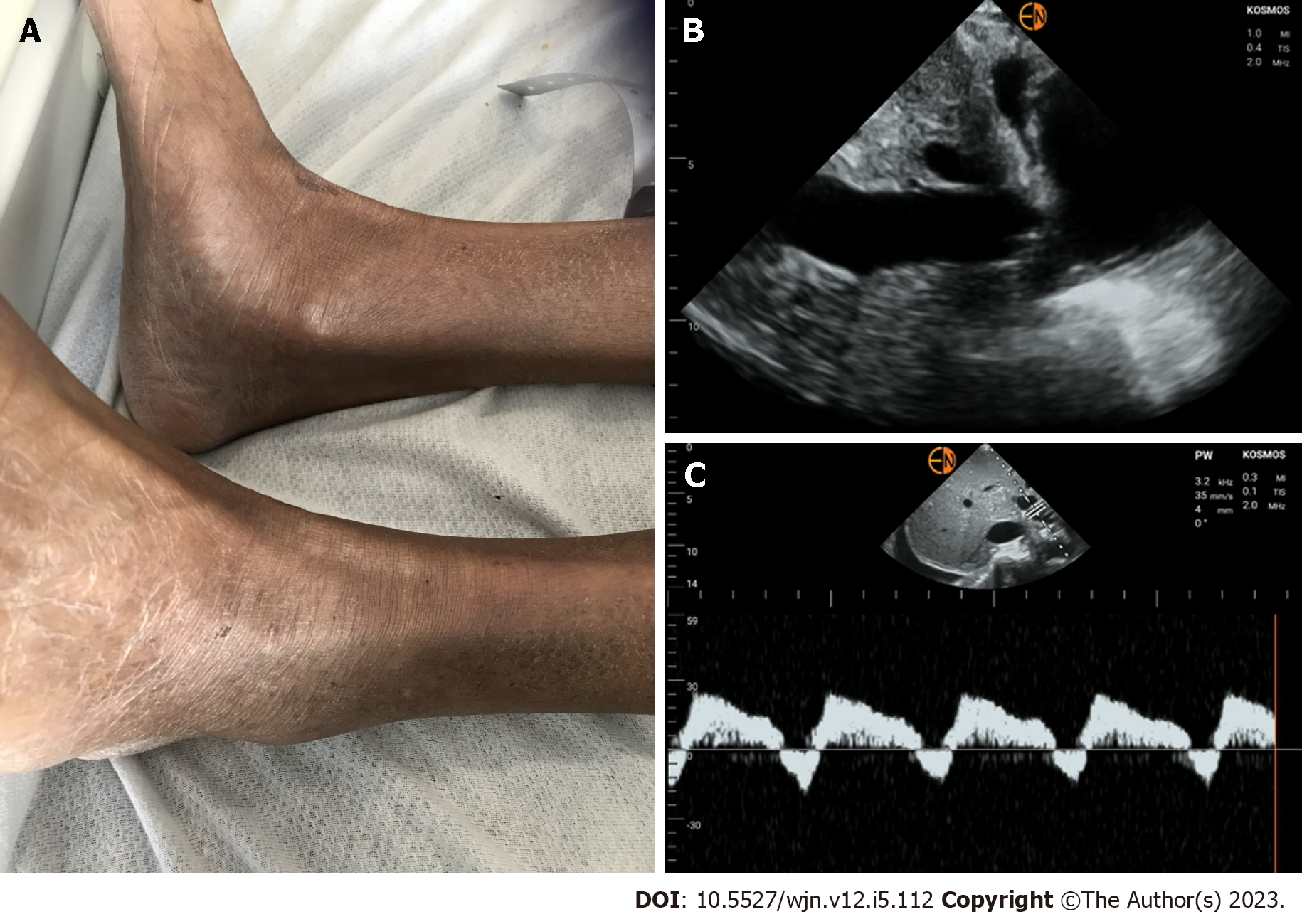
It is true that physical examination skills are declining among physicians[7,8]. However, a less acknowledged aspect is that the diagnostic accuracy of physical examination is limited[9-12]. The so-called ‘classic’ signs and symptoms were described in an era when late-stage presentations were common, often occurring after the onset of significant symptoms. As a result, there is a need for a more sensitive bedside tool to detect pathology earlier, before substantial organ damage has occurred, and to provide timely guidance for patient management. Therefore, it is essential not only to enhance the instruction of physical examination skills but also to augment them by incorporating POCUS. It is now well-established that POCUS significantly improves the sensitivity of physical examination. For instance, in a study including 32 patients with acute respiratory distress syndrome, lung ultrasound demonstrated a diagnostic accuracy of 93% for pleural effusion, 97% for alveolar consolidation, and 95% for alveolar-interstitial syndrome. In comparison, the accuracy of auscultation in detecting these abnormalities was much lower, at 61%, 36%, and 55%, respectively[13]. Similarly, in a study involving 926 critically ill patients admitted to the intensive care unit, it was observed that 51% of those with pulmonary edema on lung POCUS showed normal findings on auscultation[14]. Moreover, the incorporation of POCUS has demonstrated significant improvements in diagnostic capabilities for common cardiac conditions[15-17]. These observations are very much relevant to nephrologists who frequently rely on physical examination to assess volume status and adjust ultrafiltration goals or diuretic therapy. Furthermore, certain applications such as ruling out obstructive uropathy or evaluating venous blood flow patterns to guide decongestive therapy, cannot be achieved through conventional examination methods regardless of clinicians’ skill level. Figure 2 depicts a scenario in which a patient with heart failure and AKI received intravenous fluids under the assumption of overdiuresis, given the absence of pedal edema or shortness of breath. Nevertheless, POCUS revealed a dilated inferior vena cava and significantly pulsatile portal vein, indicating severe venous congestion. In response to these findings, intravenous diuretics were administered, leading to an improvement in serum creatinine levels.
Figure 2 A case of discrepant clinical and point of care ultrasonography findings.
A: Absent pedal edema; B: Plethoric inferior vena cava suggestive of elevated right atrial pressure; C: Pulsatile portal vein Doppler with flow reversal indicative of severe venous congestion.
Myth: The scope of nephrologist-performed pocus is confined to kidney ultrasound
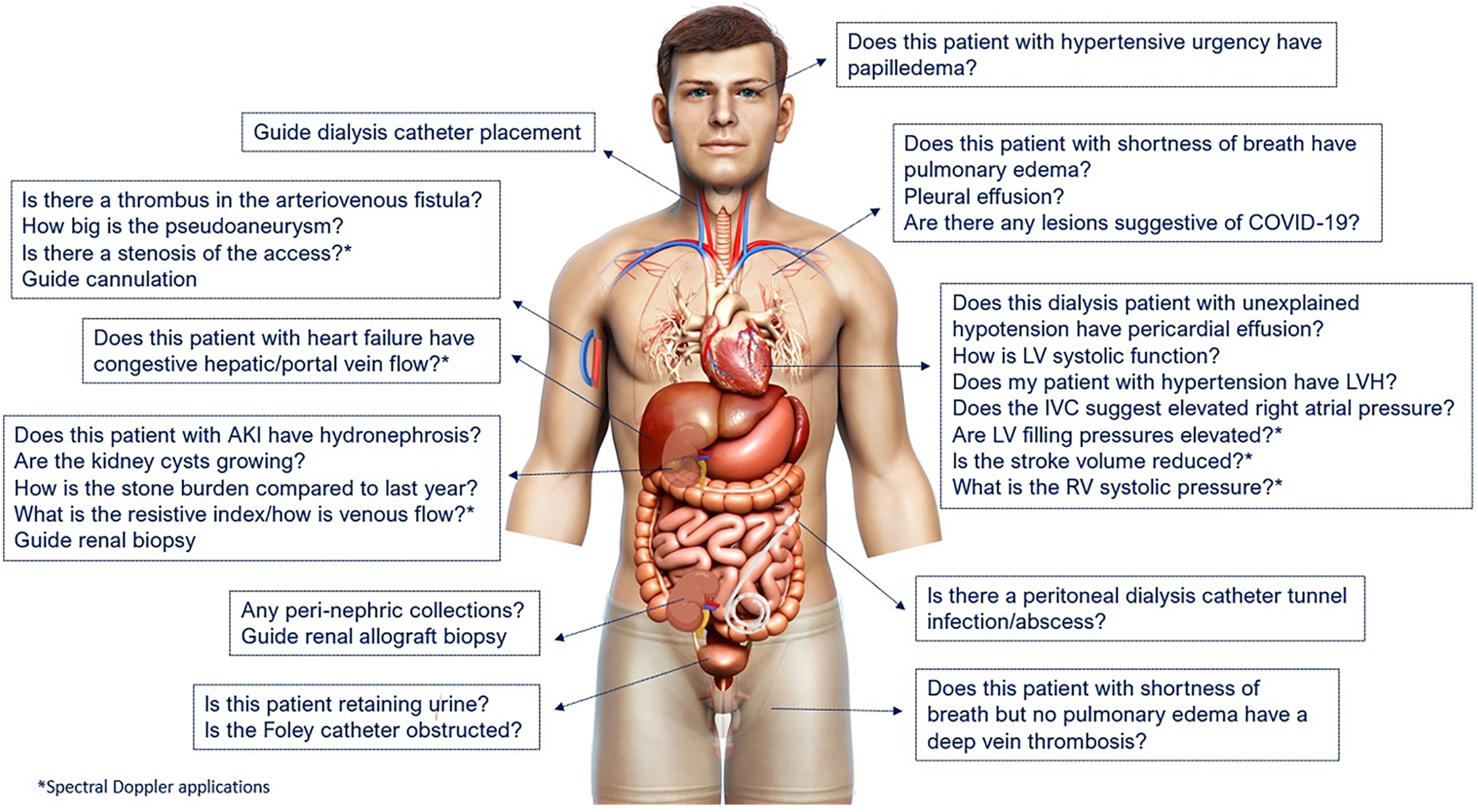
The scope of POCUS depends on two main factors: Physician’s competency and the relevance of a specific sonographic application to the physician’s specialty. There is little debate about the relevance of kidney and urinary bladder ultrasound for nephrologists, as they are expected to diagnose structural abnormalities of the kidneys and integrate this information into clinical decision-making[18]. However, in real-life situations, consulting teams often order a formal renal sonogram before seeking nephrology input in cases of AKI. Therefore, while nephrologist-performed urinary tract POCUS can be beneficial, its utility is limited to specific scenarios, such as avoiding patients’ referral to radiology to get an ultrasound in the outpatient setting or diagnosing Foley catheter obstruction in a patient with sudden decrease in urine output, among others. A significant portion of a nephrologist’s time on a consultation service is devoted to managing patients with complex fluid and electrolyte disorders. Therefore, it is conceivable that the assessment of volume status using POCUS is vital in nephrology practice. As outlined in prior publications, incorporating multi-organ POCUS, which includes focused cardiac ultrasound, lung ultrasound, and Doppler assessment of systemic veins, greatly assists in evaluating cases of hemodynamic AKI[5,19,20]. This is especially valuable in addressing common diagnostic challenges such as hepatorenal dysfunction[21]. In addition, POCUS facilitates assessment of acute abnormalities of arteriovenous access in the dialysis unit and thereby guides appropriate management. Figure 3 outlines the sonographic applications commonly used in nephrology practice. The next question is whether nephrologists are permitted to perform multi-organ POCUS. The answer is yes. In 1999, the American Medical Association House of Delegates passed a resolution (H-230.960; reaffirmed 2020) stating that “ultrasound imaging is within the scope of practice of appropriately trained physicians”[22]. Additionally, each hospital’s medical staff should review and approve criteria for granting ultrasound privileges, taking into account physicians’ background and training in accordance with recommendations developed by their respective specialty societies. Hence it is clear that the ability to perform POCUS is not determined by the physician’s specialty but rather by their training and competency. Currently, nephrologists have access to multiple certification opportunities tailored to their skill levels though development of specialty-specific universal competency standards remains a work in progress[23].
Figure 3 Scope of nephrology-related point of care ultrasonography: Organ-specific focused questions that can be answered by bedside ultrasonography.
Those marked with asterisk (*) indicate advanced sonographic applications requiring a higher operator skill level/additional training. COVID-19: Coronavirus disease 2019; LV: Left ventricle; LVH: Left ventricular hypertrophy; IVC: Inferior vena cava; RV: Right ventricle. Citation: Koratala A, Reisinger N. POCUS for Nephrologists: Basic Principles and a General Approach. Kidney360 2021; 2: 1660-1668. Copyright © 2021 by the American Society of Nephrology. The authors have obtained the permission for figure using from the Wolters Kluwer Health, Inc (Supplementary material).
Myth: Pocus should be incorporated only if it enhances patient survival
POCUS is often criticized for the lack of robust data demonstrating its direct impact on mortality. However, it is essential to remember that POCUS is a diagnostic aid. For a meaningful effect on mortality, it needs to be combined with treatments that have the ability to improve patient survival. As a diagnostic test, POCUS is expected to have better diagnostic accuracy compared to conventional methods, which it does as discussed above. Nevertheless, POCUS findings do have a significant impact on several clinically relevant and measurable outcomes such as time to diagnosis, need for imaging studies, healthcare cost burden, and patient satisfaction. For instance, in a systematic review and meta-analysis including 5393 patients with dyspnea, the time to correct diagnosis and treatment were significantly shorter in the POCUS group compared to those receiving conventional care (mean difference -63 min and -27 min respectively). Interestingly, patients in the POCUS group had significantly higher odds of receiving appropriate therapy vs controls (odds ratio = 2.31; 95% confidence interval: 1.61-3.32). Further, the length of stay in the intensive care unit was significantly shorter in the group managed using POCUS (mean difference -1.27 d)[24]. This clinical scenario is pertinent to nephrologists as they are often responsible for managing patients with dyspnea related to fluid overload. The ability to quickly differentiate between dyspnea caused by fluid accumulation and other potential causes is crucial in guiding appropriate interventions. Similarly, POCUS-guided management has shown to reduce the number of subsequent imaging studies including chest radiographs, echocardiograms and computed tomography scans thereby having a favorable impact on the healthcare costs[25,26]. Likewise, in hemodialysis patients, POCUS-guided titration of ultrafiltration has demonstrated more significant reductions in left ventricular filling pressures, cardiac chamber dimensions and ambulatory blood pressure readings, indicating an effective treatment approach[27,28]. With respect to patient-reported outcomes, there is increasing evidence that POCUS enhances patient satisfaction and facilitates better understanding of their diagnosis[29,30]. This is of particular interest to nephrologists, as they must adeptly communicate dietary restrictions and medication adherence to asymptomatic patients. In this context, discussing and presenting POCUS images to patients could prove effective[31]. The fundamental responsibility of a physician is to make accurate diagnoses through thoughtful integration of history and physical examination findings. It is illogical to forgo the use of improved bedside diagnostic tools merely because there may not be a treatment that directly impacts mortality.
Myth: Acquiring competency in pocus is a fast and simple process
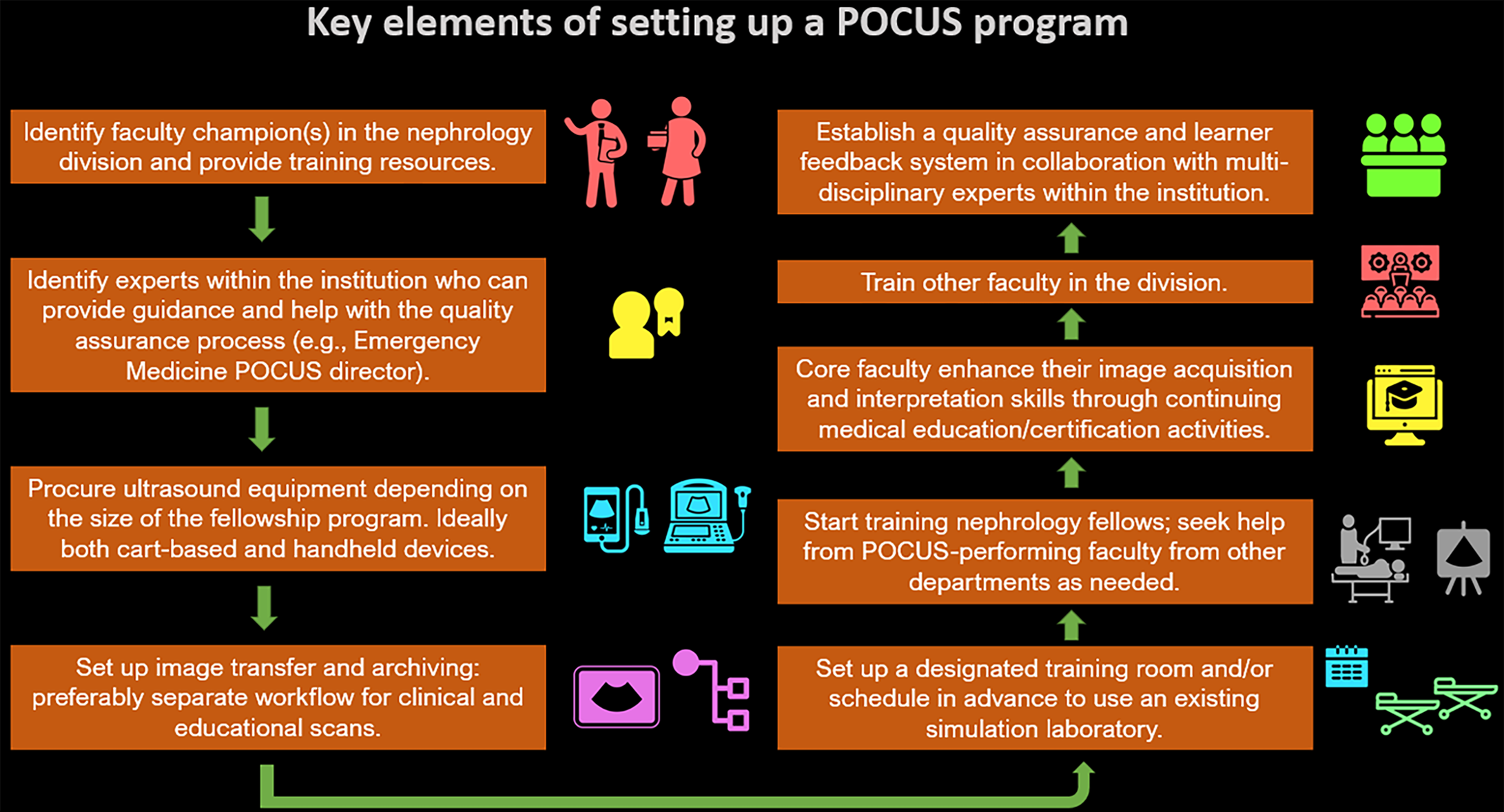
POCUS comprises three essential components: Image acquisition, interpretation, and clinical integration. Competency in POCUS means being proficient in all these aspects. In medical school, students typically receive longitudinal instruction in physical examination, starting from the first year, progressing from normal findings to abnormal findings, and finally, correlating these findings clinically to arrive at a diagnosis and develop a management plan. As such, it is logical to assume that achieving competency in POCUS cannot be accomplished just by attending a short course. It requires persistent practice under the guidance of experts, if possible, or at the very least, cross-checking findings with the reports of formal imaging studies till the learner is consistently able to obtain images of acceptable quality and independently interpret them. The duration of training can vary significantly based on the specific sonographic applications and the level of expertise needed. For instance, mastering Doppler echocardiography takes considerably more time compared to learning how to obtain basic cardiac views. As expected, the literature documents highly variable training durations, ranging from 4-320 h according to a systematic review[32]. Merely attending training sessions does not ensure competence. It must be assessed through various methods, such as knowledge checks, objective structured clinical examinations, standardized direct observation tools and periodic quality assessments. In addition, a benchmark of a minimum number of scans to be performed is commonly used when determining certification criteria or granting hospital privileges for POCUS. For example, the American College of Emergency Physicians policy statement on emergency ultrasound recommends that a trainee should perform a minimum of 25-50 quality-reviewed ultrasounds per core application and a total of 150-300 scans as part of POCUS training[33]. These recommendations are widely adopted by hospital credentialing committees and other POCUS-performing specialties albeit with necessary modifications depending on the scope of practice. In nephrology, current expert recommendation includes a minimum of 25 quality-reviewed scans per basic application (e.g., kidney, focused cardiac, lung, vascular access) and 50 per advanced application (e.g., Doppler cardiac, systemic venous Doppler, arteriovenous fistula flow assessment)[34]. To summarize, mastering POCUS is a gradual and long-term process, and physicians should plan for a stepwise learning approach. Additionally, it is crucial to be aware of both personal limitations and the limitations of the equipment being used (e.g., handheld ultrasound device vs a traditional portable machine) when interpreting the scans to avoid misdiagnosis or missing significant findings. All these factors must be taken into consideration when nephrology faculty are considering starting a POCUS training program at their institutions. Division leadership should acknowledge the significant time commitment involved and allocate the necessary resources to support the initiative. Figure 4 depicts essential elements for implementing a robust POCUS program within an institution.
Figure 4 Flow chart depicting the key elements of establishing a point of care ultrasonography program at the institutional level.
POCUS: Point of care ultrasonography. Citation: Koratala A, Reisinger N. POCUS for Nephrologists: Basic Principles and a General Approach. Kidney360 2021; 2: 1660-1668. Copyright © 2021 by the American Society of Nephrology. The authors have obtained the permission for figure using from the Wolters Kluwer Health, Inc (Supplementary material).
Myth: Pocus has limited utility because of its operator-dependent nature
POCUS is frequently criticized for its operator-dependent nature, but this limitation is intrinsic to ultrasonography as an imaging method in general irrespective of who performs it (e.g., a nephrologist or a professional sonographer or a radiologist). In contrast to other imaging modalities such as CT or magnetic resonance imaging with standardized image acquisition, obtaining optimal images relies on the expertise of the person performing ultrasound. Therefore, it is not a POCUS-specific (clinician-performed ultrasound) limitation. In reality, nearly every aspect of physician-patient interaction, such as history-taking, physical examination, and interpreting laboratory data, is operator-dependent. The emphasis should be on providing proper training to the operator rather than blaming the modality itself.
Myth: Incorporating pocus makes physicians more susceptible to lawsuits
The fear of misinterpreting findings or overlooking incidental findings, which could lead to adverse legal actions, is frequently seen as a hindrance to the adoption of POCUS in nephrology practice[35]. Several studies have examined lawsuits involving POCUS performed by various specialties. However, to date, no study has indicated that missed findings on focused or limited ultrasound scans resulted in adverse legal action against physicians. Instead, the research suggests that adverse legal action is more commonly associated with failure to perform POCUS in a timely manner when required[36-40]. In this context, implementing a hospital wide system for archiving POCUS images and standardizing the reporting of findings can be beneficial. Such a system streamlines the process of providing timely feedback to trainees, facilitates billing procedures, and allows for seeking expert opinion when uncertainty arises.