Published online Sep 25, 2021. doi: 10.5527/wjn.v10.i5.101
Peer-review started: April 24, 2021
First decision: June 6, 2021
Revised: June 19, 2021
Accepted: July 30, 2021
Article in press: July 30, 2021
Published online: September 25, 2021
Processing time: 154 Days and 11 Hours
Lemierre's syndrome is a disease that causes anaerobic sepsis, internal jugular vein thrombosis, and septic embolism in the lungs and other organs after acute oropharyngeal infection. It was named after André-Alfred Lemierre in 1936.
Here, we have reported a case of Lemierre’s syndrome in a 56-year-old female patient who presented with a sore throat. The patient had septic shock, had not voided, and had severe hyperglycemia at the time of her visit. Imaging tests revealed bilateral pneumonia, pleural effusion, pulmonary embolism, and renal vein thrombosis. The patient was admitted to the intensive care unit and placed on mechanical ventilation due to acute respiratory distress syndrome. Continuous renal replacement therapy was administered to treat renal failure with anuria. Klebsiella pneumoniae was cultured from blood and sputum samples. After reviewing various results, the patient was ultimately diagnosed with Lemierre’s syndrome. The patient was treated with appropriate antibiotics and thrombolytic agents. She was discharged from the hospital after recovery.
Lemierre’s syndrome is associated with a high mortality rate. Therefore, clinicians should be familiar with the signs and symptoms of this disease as well as the preemptive examinations, procedures, and treatments.
Core Tip: Lemierre’s syndrome is mostly caused by Fusobacterium. However, we present a rare case of Lemierre’s syndrome caused by Klebsiella pneumoniae in a patient with poor glycemic control. Uncommon in Lemierre’s syndrome, renal vein thrombosis and acute kidney injury occurred, continuous renal replacement therapy was performed, and mechanical ventilation was performed for serious pulmonary complications. The incidence of Lemierre's syndrome decreased after antibiotics were developed. However, when Lemierre’s syndrome occurs, the mortality rate from its complications is high, so we want to emphasize that patients with systemic symptoms accompanied by fever and sore throat should be suspicious of Lemierre's syndrome.
- Citation: Hwang SY, Shin SJ, Yoon HE. Lemierre's syndrome caused by Klebsiella pneumoniae: A case report. World J Nephrol 2021; 10(5): 101-108
- URL: https://www.wjgnet.com/2220-6124/full/v10/i5/101.htm
- DOI: https://dx.doi.org/10.5527/wjn.v10.i5.101
Lemierre’ syndrome, also known as postanginal sepsis, was first named in 1936 after the French microbiologist André-Alfred Lemierre. This syndrome is characterized by anaerobic sepsis and blood clots in the internal jugular vein (IJV) after acute oropharyngeal infection. It also causes septic embolism in the lungs and other organs[1].
Lemierre’s syndrome is typically caused by Fusobacterium necrophorum, which is a part of the normal flora of the oropharynx. However, the recent development of various antibiotics and advancements in medical care have led to diversified and antibiotic-resistant strains.
Therefore, after referring to the current literature, we have reported a single case of Lemierre’s syndrome caused by Klebsiella pneumoniae (K. pneumoniae). In accordance with the course of this disease, pulmonary embolism, occurring after oropharyngeal infection, developed into acute respiratory distress syndrome.
A 56-year-old female patient presented to the emergency department of our institution with sore throat, dyspnea, abdominal pain, and diarrhea.
The patient was unable to eat due to a sore throat and had been unable to take her diabetes medication for 5 d prior to the visit.
Subsequently, the patient visited the hospital with abdominal pain, diarrhea, and shortness of breath.
The patient had been prescribed medication for diabetes and hypertension 2 years previously. She also had a history of a canceled surgery for chronic right-sided otitis media.
The patient had diabetes, hypertension, and chronic otitis media.
At the time of admission, the patient’s blood pressure, pulse rate, respiratory rate, body temperature, and oxygen saturation level were 11.3/7.8 kPa, 104, 22, 36 °C, and 90%, respectively. The patient was conscious. Swelling and redness were observed in the left neck and both tonsils. Rales were auscultated throughout the chest. Auscultation of the abdomen revealed a normoactive bowel sound with no tenderness.
No urine was produced after catheter insertion.
Blood tests revealed an evaluated white blood cell count (16.47 × 103/µL), anemia (hemoglobin level, 7.2 g/dL; hematocrit level, 24.4%), renal failure (blood urea nitrogen, 78.8 mg/dL; creatinine level, 4.22 mg/dL). The patient was hyperglycemic, with a glucose level of 32.6 mmol/L. The patient had uncontrolled diabetes, with a glycated hemoglobin level of 11%. The C-reactive protein level was also elevated at 207.58 mg/dL. An arterial blood gas test revealed acidosis of pH 7.27. Additionally, a pCO2 level of 25 mmHg, a pO2 level of 83 mmHg, and a bicarbonate level of 11.5 mEq/L indicated metabolic acidosis.
The anion gap was 21.5 mEq/L, and the serum lactate level was 1.8 mmol/L. Therefore, a provisional diagnosis of lactic acidosis was established. Urine ketone was present in trace amounts. Spot urine microalbumin/creatinine ratio was 123.6 mg/gCr.
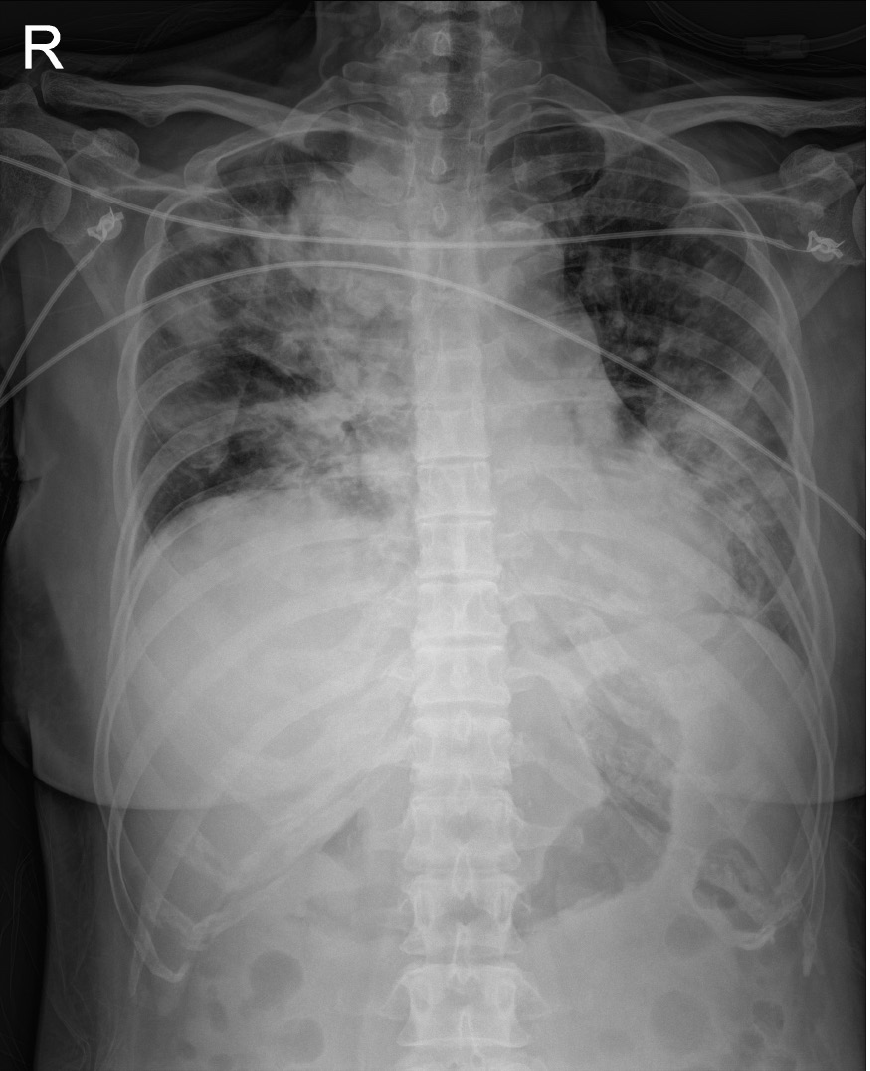
Chest radiography showed multiple patchy infiltrations in both lungs (Figure 1).
Chest computed tomography (CT) revealed peribronchial consolidation and ground-glass opacity with cavitary nodules in both lungs. Pulmonary thromboembolism (PTE) in the segmental and subsegmental pulmonary arteries of the right lower lobe was suspected (Figure 2).
Abdominal computed tomography showed extensive thrombosis in the left renal vein, extending to partial thrombosis in the suprarenal inferior vena cava (IVC).
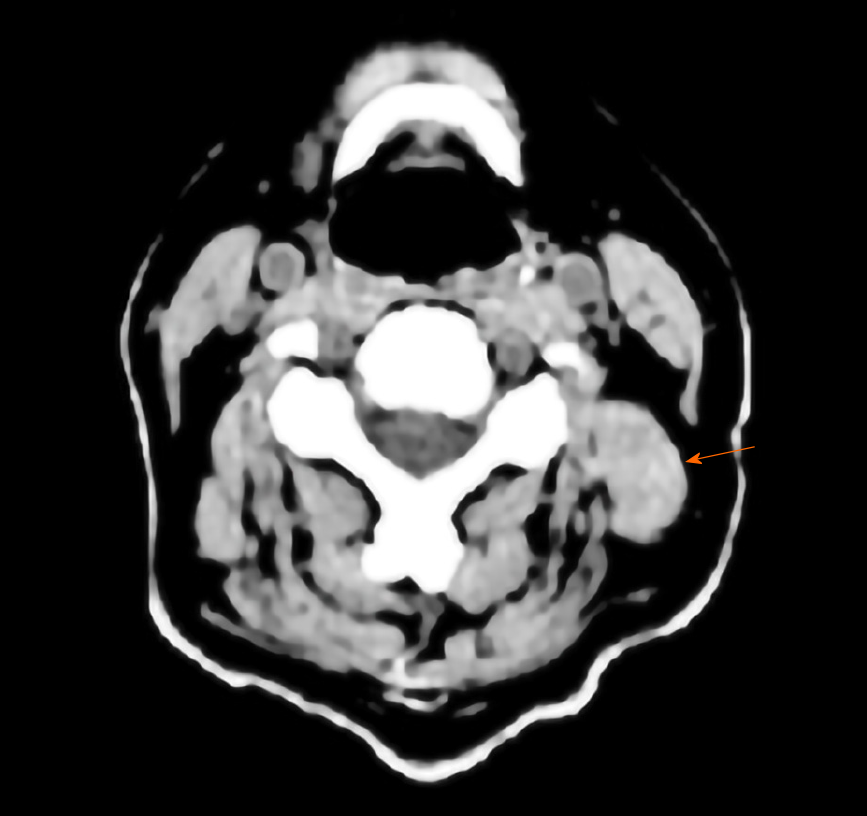
A neck angio CT was performed on the third day to assess left neck swelling. A 13 mm × 10 mm nodular lesion was observed on the left parotid gland (Figure 3).
For further evaluation, blood, sputum, and urine cultures, hypercoagulability test were performed.
The hypercoagulability test showed decreased protein S activity and less free protein S antigen but normal total protein S antigen, protein C activity, and protein C antigen. The von Willebrand factor and factor V Leiden were normal, and lupus anti-coagulant level was elevated. However, anticardiolipin and anti-β2 glycoprotein-1 antibodies were absent.
Additionally, the following findings were noted: prothrombin time, 14.5 s; antithrombin III, 72.1; D-dimer, 2.01; and fibrinogen, 926.1. These results did not meet the diagnostic criteria for disseminated intravascular coagulation.
On the fourth day of hospitalization, as pneumonia was worsening, sputum analysis was performed using bronchoalveolar lavage.
A fine-needle aspiration biopsy of the nodule on the left parotid gland was performed on day 14. The nodule was found on neck angio CT. Biopsy results indicated that the nodule consisted of inflammatory cells. Although there was a possibility of cervical lymphadenopathy, the mass was not removed and was closely observed.
The patient had a history of discontinued treatment for chronic right-sided otitis media. Therefore, she underwent otoscopy after being transferred to a general hospital unit. Chronic otitis media with cholesteatoma was suspected. An additional temporal bone was identified on CT. The focal bone defect was suspected to be the right tegmen mastoideum. Therefore, surgical therapy was considered after the acute inflammation was controlled.
Follow-up chest CT was performed as there was no further clinical improvement in pneumonia. Progression of invasive aspergillosis was observed.
K. pneumoniae was identified on culture of blood samples taken immediately after admission and on culture of sputum samples extracted via bronchoscopy. Except for piperacillin and ampicillin, the bacteria were susceptible to other antibiotics.
Aspergillus niger (A. niger) was identified on a follow-up sputum culture. The (1-3)-β-D-glucan assay confirmed the presence of invasive Aspergillus.
The final diagnosis was Lemierre’s syndrome due to K. pneumoniae.
After admission, the patient was transferred to the intensive care unit to undergo treatment for anuria and metabolic acidosis. After continuous renal replacement therapy and administration of a large amount of fluid, the patient started to urinate on the first day of hospitalization. Acute renal failure improved on the second day. However, oxygen demand gradually increased, and pneumonia was aggravated in both lungs on chest radiographs. Therefore, mechanical ventilation was initiated.
Piperacillin-tazobactam and levofloxacin were used as empirical antibiotics. They were used to simultaneously manage Streptococcus pneumoniae and Pseudomonas spp., the causative agents of severe community-acquired pneumonia. These antibiotics were selected based on previous reports of fluoroquinolone combination therapy leading to a better prognosis than β-lactam alone in severe cases[2].
Enoxaparin, a low-molecular-weight heparin, was initiated on the second day to treat the pulmonary thromboembolism.
However, the patient’s clinical condition further deteriorated due to pneumonia. Therefore, on the fourth day, the initial antibiotics were replaced with vancomycin and meropenem.
As there was no improvement in pneumonia after the antibiotics were changed, mechanical ventilation was continued. On the ninth day, vancomycin was discontinued due to a lack of evidence of a gram-positive bacterial infection. Amikacin was added to meropenem. On day 13, improvement was seen in pneumonia. The patient’s oxygen demand decreased, and therefore, she was weaned from mechanical respiratory support. She was subsequently transferred to a general hospital unit.
Moreover, A. niger was isolated in a follow-up sputum culture. Therefore, we started administering amphotericin following consultation with the infectious disease medical staff.
Subsequently, the patient recovered gradually, amphotericin was switched to itraconazole and low-molecular-weight heparin was switched to apixaban. She was ultimately discharged from the hospital.
Leukocytosis occurred on the 12th day after discharge; therefore, the patient was re-hospitalized. There was suspicion of an abscess in the right lung field. An air-fluid level was identified (Figure 4).
A. niger was not identified in the follow-up culture performed after hospitalization. K. pneumoniae susceptible to third-generation cephalosporins was identified, consistent with the initial culture result. Therefore, during hospitalization, piperacillin-tazobactam was administered. The patient was discharged with a prescription of cefditoren and itraconazole.
Itraconazole was discontinued after 3 mo. The lung lesion with bilateral ground-glass opacity on radiography did not improve. Therefore, the patient continued taking cefditoren and received continuous respiratory rehabilitation treatment. To reduce the risk of PTE recurrence, apixaban was administered for ≥ 6 mo.
In 1989, Sinave et al[3] summarized the key symptoms of Lemierre’s syndrome and suggested the following diagnostic criteria: (1) Primary infection of the oropharynx; (2) Sepsis with at least one bacteria identified on a blood culture; (3) Clinical or imaging findings of IJV thrombosis; and (4) At least one metastasis.
Lemierre’s syndrome was a common disease until the development of antibiotics. However, recently it has become a rare disease and has been called the “forgotten disease”[1].
This disease occurs mainly in adolescents and young adults. However, its cause has not been clearly established.
In young adults, pharyngitis symptoms are observed during the initial stages of the disease. In contrast, elderly individuals manifest early metastatic complications, such as pneumonia and brain abscesses. This suggests that infection of the IJV causes complications in other organs through blood circulation. In recent studies, 7% cases of Lemierre’s syndrome progressed to septic shock[4]. Pulmonary impairment was the most common metastatic complication, leading to pneumonia, pulmonary embolism, pleural effusion, pneumothorax, and thoracic empyema. A total of 10% cases required mechanical respiratory assistance for acute respiratory distress syndrome. This was the case in our study.
Less than 5% patients receive renal replacement therapy for acute renal failure[4]. However, for 2 d, our patient underwent continuous renal replacement therapy for acute kidney injury caused by septic shock and renal vein thrombosis.
Lemierre’s syndrome is primarily caused by Fusobacteria, which are a part of the normal flora in the oropharynx, genitourinary tract, and gastrointestinal tract. Among the 13 species of Fusobacterium, F. necrophrum is the most common pathogen[5]. In other case reports, Bacteroides spp., Streptococcus spp., Enterococcus spp., Peptostre
In the present case, K. pneumoniae was the causative pathogen. However, K. pneumoniae has rarely been reported as a cause of Lemierre’s syndrome in previous case reports. Based on some retrospective studies, only 2.5% cases have been reported to be caused by K. pneumoniae[6].
In a study published in 2015, eight of nine patients with Lemierre’s syndrome associated with K. pneumoniae had poorly controlled diabetes[7].
Similarly, our patient had poor blood glucose control with a glycated hemoglobin level of 11% and a serum glucose level of 32.6 mmol/L at the time of admission.
Patients with type 2 diabetes mellitus are vulnerable to infection because of the decreased activity of neutrophils[8]. The underlying mechanism of the increased susceptibility of patients with type 2 diabetes mellitus to K. pneumoniae is as follows. The hypermucoviscosity phenotype of K. pneumoniae, especially K1/K2 isolates, is resistant to phagocytosis[9]. Poor glycemic control significantly reduces phagocytosis of virulent K1/K2 K. pneumoniae. Additionally, Lin et al[10] showed that older patients with poor glycemic control had decreased phagocytosis activity.
Beta-lactamase-resistant beta-lactam antibiotics are recommended for typical Lemierre’s syndrome. Beta-lactamase produced by F. necrophorum may lead to therapy failure[7].
Therefore, treatment should be changed from empirical antibiotics to targeted antibiotics based on the results of the blood culture and antibiotic susceptibility analysis.
If K. pneumoniae is the likely cause of Lemierre’s syndrome, drugs that can also treat gram-negative aerobic rods should be used until the causative pathogen is identified. Additionally, the appropriate drug must be selected based on the susceptibility data of K. pneumoniae in the region and the risk of an Extended-spectrum beta-lactamases-producing strain[11,12].
In our patient, IJV thrombosis was not observed. Instead, pulmonary thromboembolism, partial thrombosis of the suprarenal IVC, and extensive thrombosis of the left renal vein were observed.
The hypercoagulability test results led to the suspicion of protein S deficiency. However, protein S deficiency is difficult to diagnose solely based on the results obtained once in the acute phase[13].
We have scheduled another test for the protein S deficiency diagnosis 3 mo later. Since prolonged prothrombin time and decreased antithrombin III levels are common in sepsis, the result was considered to be non-specific.
We compared the hypercoagulability properties of F. necrophorum and K. pneumoniae because they are related to the pathogenesis of Lemierre’s syndrome.
F. necrophorum produces a component of the cell surface called hemagglutinin, which forms thrombi[4]. Russo et al[14] have suggested that this is because K. pneumoniae causes more frequent metastatic spread in the K1/K2 group. Another possibility is increased capsule production in the hypervirulent type.
Although the hypothesis has not been tested, it appears that the mucoviscosity of the strain’s thick capsules persists in the bloodstream and causes greater aggregation of bacterial cells to form thrombi[14].
The role of anticoagulation for IJV thrombosis is controversial. As Lemierre’s syndrome has a low incidence rate, there is a lack of controlled investigations for anticoagulation treatment.
Also, anticoagulation medication was introduced to prevent respiratory failure and propagation of the septic thrombus to the intracranial sinuses.
There is no clear evidence to outline the appropriate duration of anticoagulation treatment. Previously reported findings suggest a duration of 4 wk to 6 mo[15]. Schubert et al[16] analyzed 23 patients diagnosed with septic thrombosis of the IJV from 1998 to 2010. The primary infection site in 11 patients was the middle ear[16]. Otitis is a common disease. However, it can progress to systematic infection by forming septic thromboses in the IJV. Therefore, source control is fundamental even if it is a local infection.
In addition, the incidence rate of Lemierre’s syndrome is increasing again in recent years. The development of various antibiotics and advancements in medical care have led to the emergence of various new pathogenic strains and multidrug-resistant strains. The syndrome may be fatal as it is accompanied by numerous systemic complications. Therefore, Lemierre’s syndrome must be suspected in cases of fever or throat pain associated with infections of the oropharynx and middle ear. Preemptive examinations, consultation with other specialists, appropriate procedures, and targeted treatments are essential.
The primary site of infection in Lemierre’s syndrome is the oropharynx. Oropharyngeal infections cause IJV thrombosis and anaerobic sepsis. The disease typically manifests as sore throat, a symptom of oropharyngeal infection. This can lead to metastatic complications and death. Lemierre’s syndrome is a rare disease[17]. Therefore, it is difficult for doctors with no experience with this syndrome to suspect it[5]. In addition, symptoms of oropharyngeal infection are often resolved when the patient visits the hospital. This disease should be considered in the differential diagnosis when systemic complications caused by upper respiratory tract infection are suspected.
Atypical Lemierre’s syndrome should be suspected in cases in which a typical causative strain is not identified or cases of thromboembolism at a site other than the IJV thrombosis. After diagnosis, it is essential to assess whether surgery or intervention is necessary through active consultation with other specialists. Appropriate antibiotic treatment according to the causative strain must be initiated.
| 1. | Johannesen KM, Bodtger U. Lemierre's syndrome: current perspectives on diagnosis and management. Infect Drug Resist. 2016;9:221-227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 127] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 2. | Martínez JA, Horcajada JP, Almela M, Marco F, Soriano A, García E, Marco MA, Torres A, Mensa J. Addition of a macrolide to a beta-lactam-based empirical antibiotic regimen is associated with lower in-hospital mortality for patients with bacteremic pneumococcal pneumonia. Clin Infect Dis. 2003;36:389-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 259] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 3. | Sinave CP, Hardy GJ, Fardy PW. The Lemierre syndrome: suppurative thrombophlebitis of the internal jugular vein secondary to oropharyngeal infection. Medicine. 68:85-94. [PubMed] |
| 4. | Riordan T. Human infection with Fusobacterium necrophorum (Necrobacillosis), with a focus on Lemierre's syndrome. Clin Microbiol Rev. 2007;20:622-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 427] [Cited by in RCA: 402] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 5. | Kuppalli K, Livorsi D, Talati NJ, Osborn M. Lemierre's syndrome due to Fusobacterium necrophorum. Lancet Infect Dis. 2012;12:808-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 199] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 6. | Garbati MA, Ahsan AM, Hakawi AM. Lemierre's syndrome due to Klebsiella pneumoniae in a 63-year-old man with diabetes: a case report. J Med Case Rep. 2012;6:97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Chuncharunee A, Khawcharoenporn T. Lemierre's Syndrome Caused by Klebsiella pneumoniae in a Diabetic Patient: A Case Report and Review of the Literature. Hawaii J Med Public Health. 2015;74:260-266. [PubMed] |
| 8. | Delamaire M, Maugendre D, Moreno M, Le Goff MC, Allannic H, Genetet B. Impaired leucocyte functions in diabetic patients. Diabet Med. 1997;14:29-34. [PubMed] [DOI] [Full Text] |
| 9. | Lin JC, Chang FY, Fung CP, Xu JZ, Cheng HP, Wang JJ, Huang LY, Siu LK. High prevalence of phagocytic-resistant capsular serotypes of Klebsiella pneumoniae in liver abscess. Microbes Infect. 2004;6:1191-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 145] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 10. | Lin JC, Siu LK, Fung CP, Tsou HH, Wang JJ, Chen CT, Wang SC, Chang FY. Impaired phagocytosis of capsular serotypes K1 or K2 Klebsiella pneumoniae in type 2 diabetes mellitus patients with poor glycemic control. J Clin Endocrinol Metab. 2006;91:3084-3087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 162] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 11. | Paterson DL, Ko WC, Von Gottberg A, Mohapatra S, Casellas JM, Goossens H, Mulazimoglu L, Trenholme G, Klugman KP, Bonomo RA, Rice LB, Wagener MM, McCormack JG, Yu VL. Antibiotic therapy for Klebsiella pneumoniae bacteremia: implications of production of extended-spectrum beta-lactamases. Clin Infect Dis. 2004;39:31-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 401] [Cited by in RCA: 407] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 12. | Sabaka P, Kachlíková M, Bendžala M, Káčerová H. Lemierre syndrome caused by Klebsiella pneumoniae complicated by epidural abscess - Case report. IDCases. 2020;19:e00664. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Campello E, Spiezia L, Simion C, Tormene D, Camporese G, Dalla Valle F, Poretto A, Bulato C, Gavasso S, Radu CM, Simioni P. Direct Oral Anticoagulants in Patients With Inherited Thrombophilia and Venous Thromboembolism: A Prospective Cohort Study. J Am Heart Assoc. 2020;9:e018917. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 14. | Russo TA, Marr CM. Hypervirulent Klebsiella pneumoniae. Clin Microbiol Rev. 2019;32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 438] [Cited by in RCA: 844] [Article Influence: 120.6] [Reference Citation Analysis (0)] |
| 15. | Phua CK, Chadachan VM, Acharya R. Lemierre syndrome-should we anticoagulate? Int J Angiol. 2013;22:137-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 66] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 16. | Schubert AD, Hotz MA, Caversaccio MD, Arnold A. Septic thrombosis of the internal jugular vein: Lemierre's syndrome revisited. Laryngoscope. 2015;125:863-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Hagelskjaer Kristensen L, Prag J. Lemierre's syndrome and other disseminated Fusobacterium necrophorum infections in Denmark: a prospective epidemiological and clinical survey. Eur J Clin Microbiol Infect Dis. 2008;27:779-789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 162] [Cited by in RCA: 191] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, general and internal
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dumic I, Shelat VG S-Editor: Gong ZM L-Editor: A P-Editor: Ma YJ