©The Author(s) 2025.
World J Nephrol. Jun 25, 2025; 14(2): 103027
Published online Jun 25, 2025. doi: 10.5527/wjn.v14.i2.103027
Published online Jun 25, 2025. doi: 10.5527/wjn.v14.i2.103027
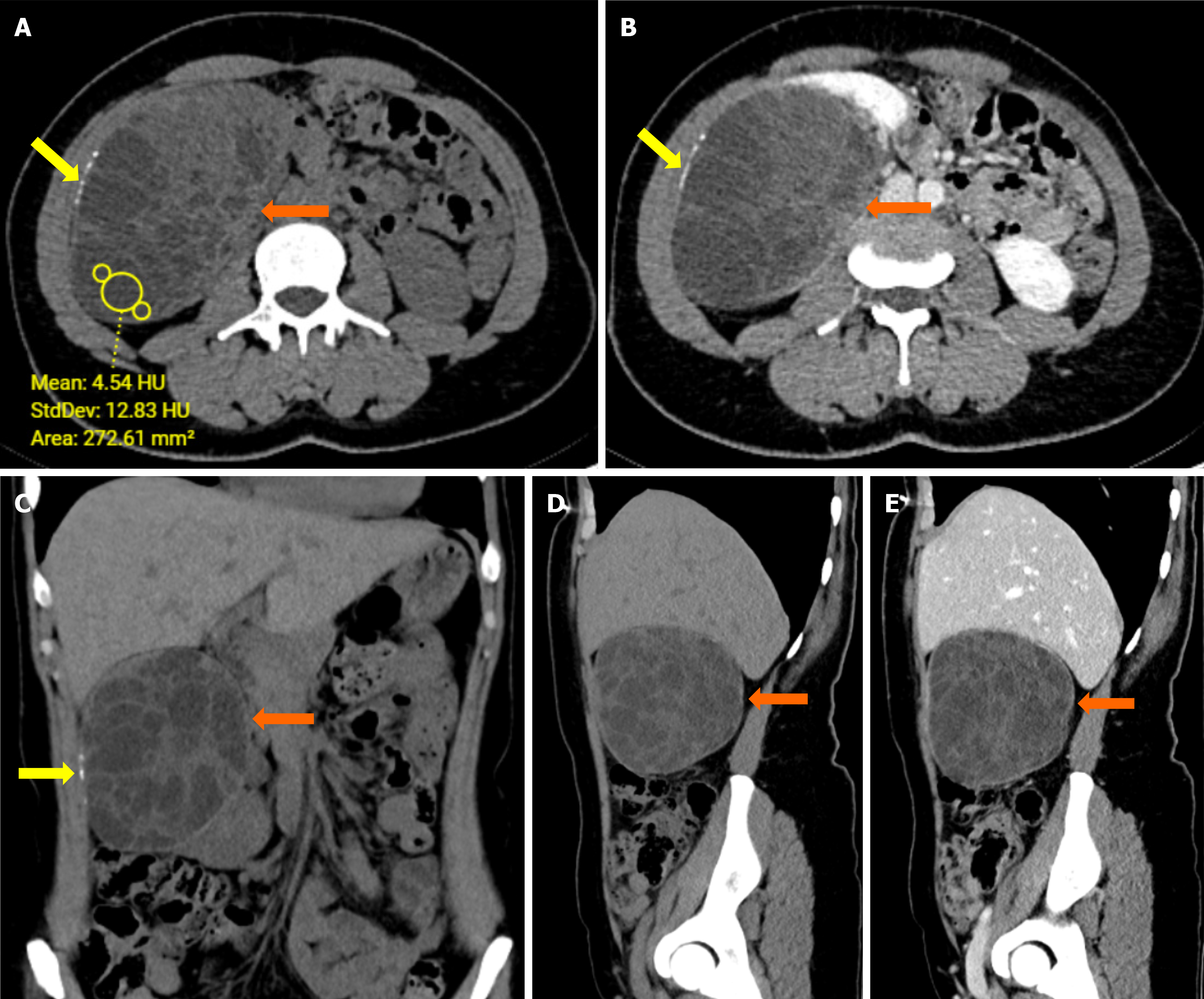
Figure 1 Axial and coronal abdominal computed tomography images of a complex cystic lesion in the right kidney.
A: Axial pre-contrast computed tomography (CT) image shows a complex cystic lesion with several septations in the right kidney (orange arrows); B: Axial post-contrast CT image demonstrates enhancement of the lesion, with noticeable septations (orange arrows) and linear calcifications along its wall (yellow arrows); C: Coronal pre-contrast CT image highlights the extent of the cystic lesion and linear calcifications (yellow arrows); D: Sagittal pre-contrast CT image presents the multiloculated nature of the lesion; E: Sagittal post-contrast CT image further delineates the lesion’s characteristics with contrast enhancement of the septations.
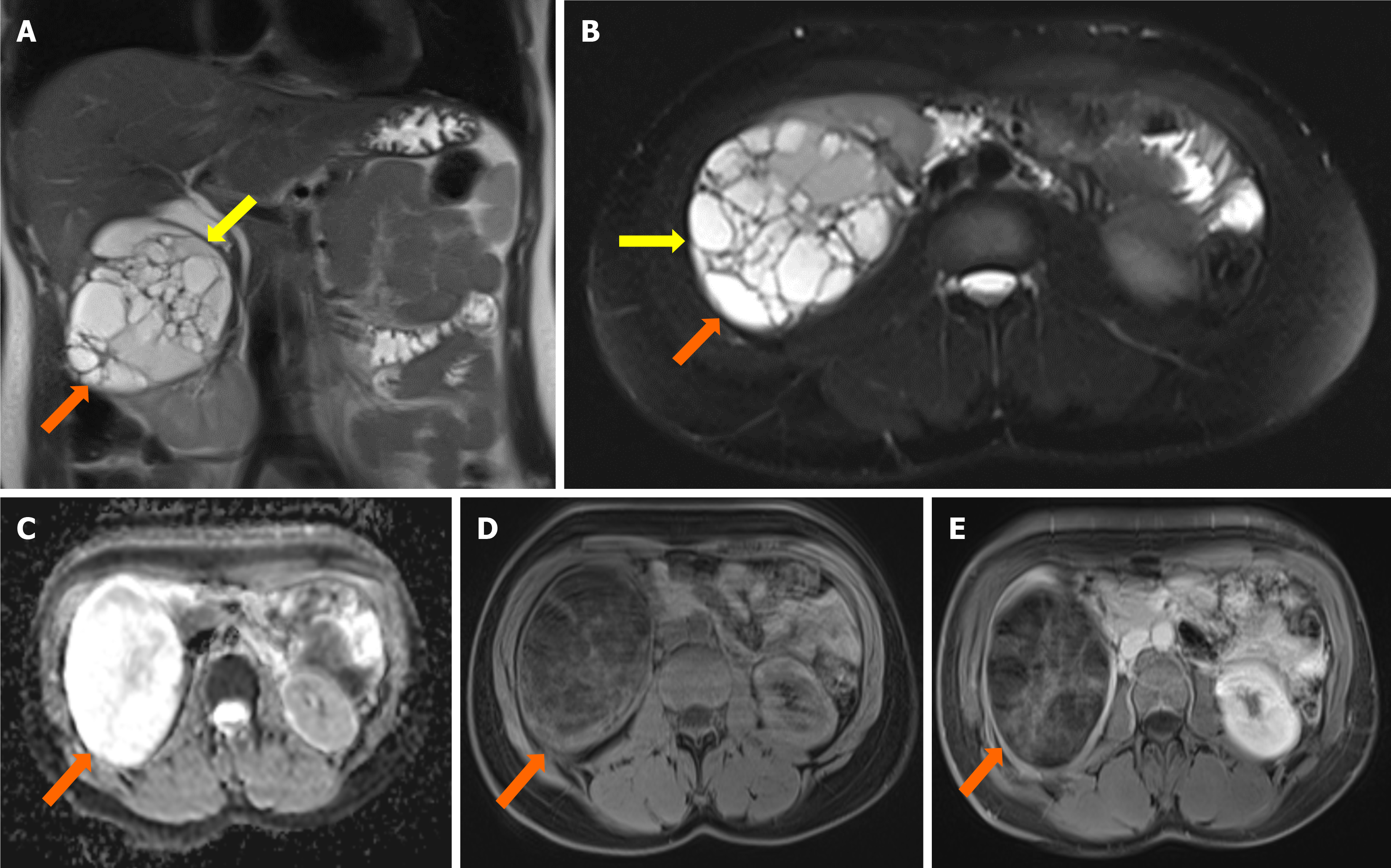
Figure 2 Coronal and axial abdominal magnetic resonance imaging of a multiloculated cystic lesion in the right kidney.
A: Coronal T2-weighted (T2W) image shows a 10 cm-sized multiloculated cystic lesion in the upper part of the right kidney (orange arrows), with a hypointense rim (yellow arrows); B: Axial fat-saturated T2W image highlights the multiloculated cystic lesion (orange arrows) with a hypointense rim (yellow arrows); C: Apparent diffusion coefficient map reveals restricted diffusion within the lesion; D: Axial fat-saturated pre-contrast T1-weighted (T1W) image shows the lesion without significant enhancement; E: Axial fat-saturated post-contrast T1W image demonstrates slight contrast enhancement in the septa of the cystic lesion (orange arrows).
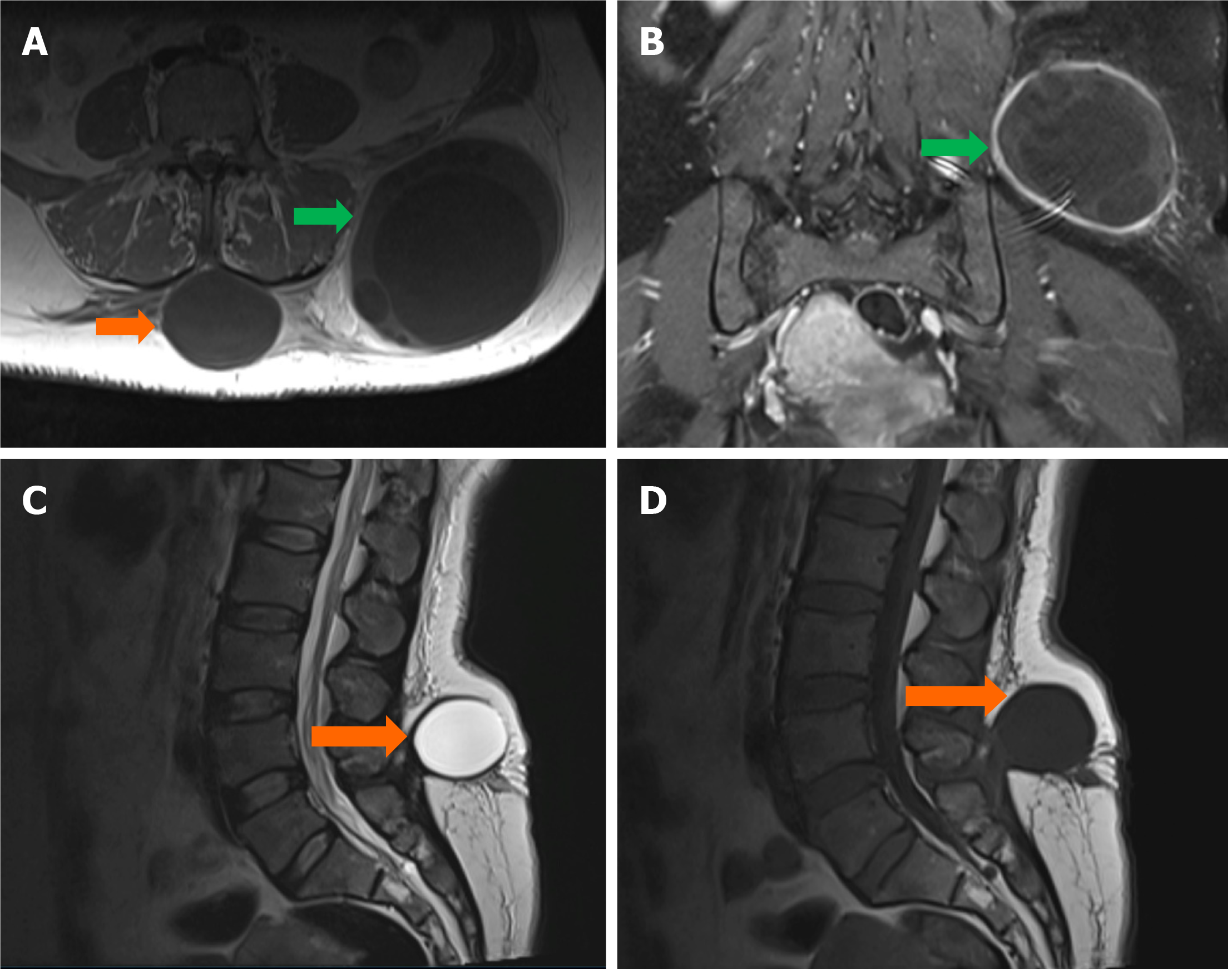
Figure 3 Lumbar region magnetic resonance imaging of multiloculated cystic lesions in the subcutaneous fat tissue.
A: Axial T1W image reveals two distinct multiloculated cystic lesions in the lumbar subcutaneous fat tissue, one located in the midline (orange arrows) and the other on the left lateral side (green arrows); B: Coronal post-contrast fat-saturated T1W image shows contrast enhancement in both the septal and mural components of the lesions; C: Sagittal T2W image demonstrates the cystic nature of the lesions; D: Sagittal T1W image further characterizes the lesions with visible enhancement in their septal and mural components.
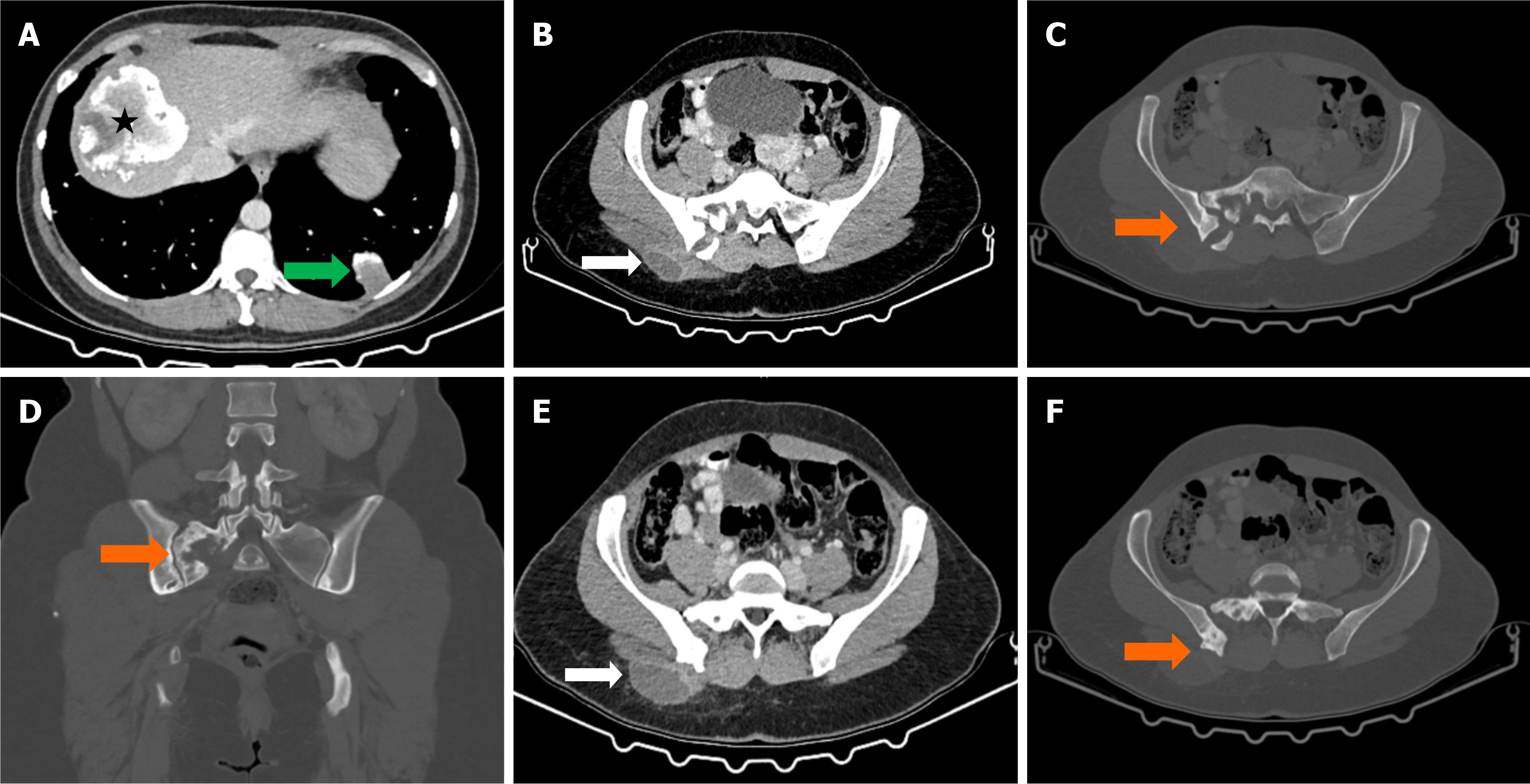
Figure 4 Abdominal computed tomography images showing inactive hydatid cysts and associated bone lesions.
A: Axial abdominal computed tomography (CT) image demonstrates an inactive hydatid cyst in the right lobe of the liver (black asterisk) and another inactive hydatid cyst in the lower lobe of the left lung (green arrow); B: Axial post-contrast abdominal CT image reveals a rim-enhancing cystic lesion in the subcutaneous adipose tissue of the right gluteal region (white arrows); C: Axial bone window CT image displays erosive lesions in the right half of the sacrum (orange arrows); D: Coronal bone window CT image highlights erosive lesions in the posterior part of the right iliac wing (orange arrows); E: Axial post-contrast abdominal CT image confirms rim enhancement in the gluteal cystic lesion; F: Axial bone window CT image further depicts bone erosions in the sacrum and iliac wing (orange arrows).
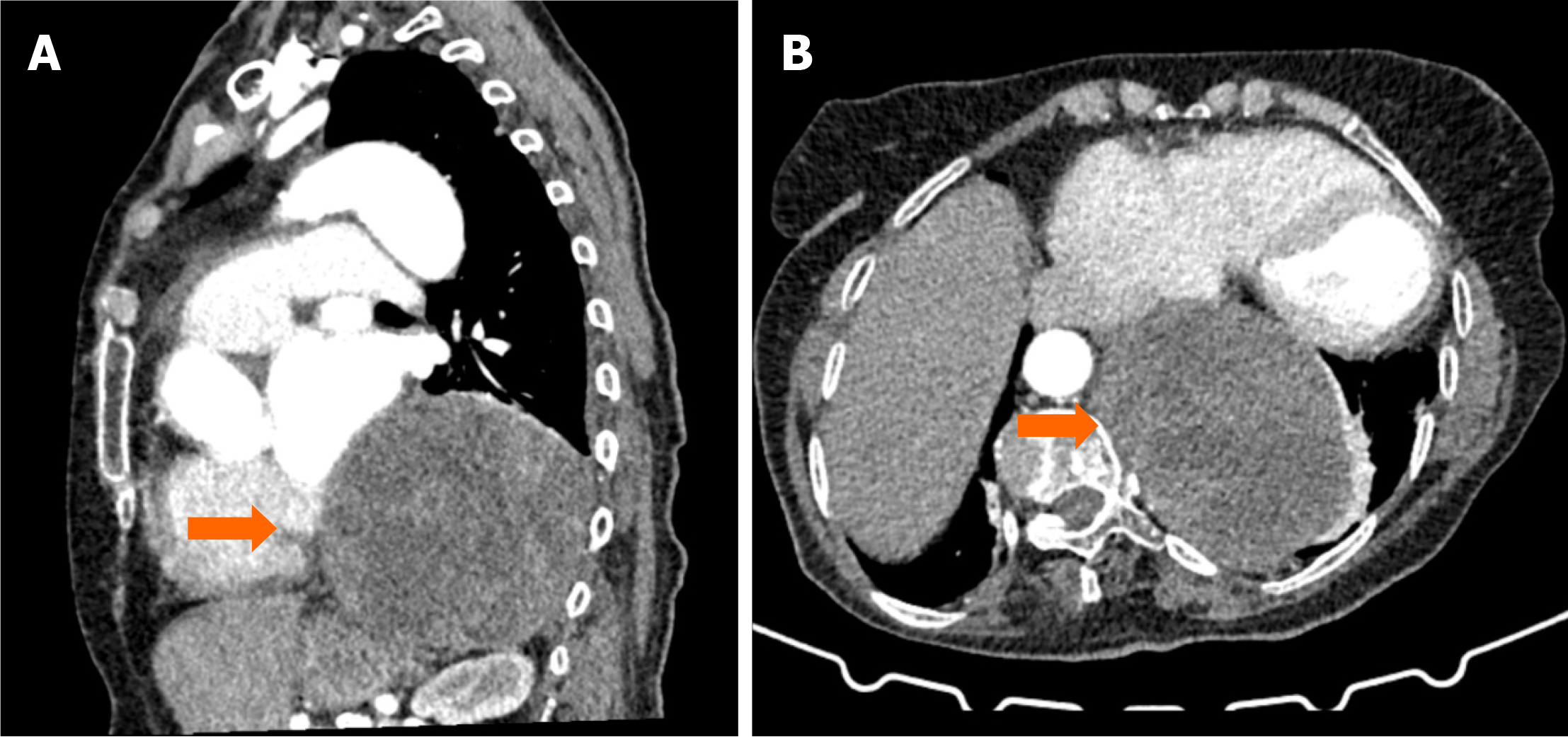
Figure 5 Thorax computed tomography images showing a cystic lesion in the left paravertebral area.
A: Sagittal contrast-enhanced thorax computed tomography (CT) scan demonstrates a cystic lesion with multiple enhancing septa and smooth contours, located extrapulmonary in the left paravertebral area (orange arrows); B: Axial contrast-enhanced thorax CT image further illustrates the extrapulmonary cystic lesion with well-defined septations (orange arrows).
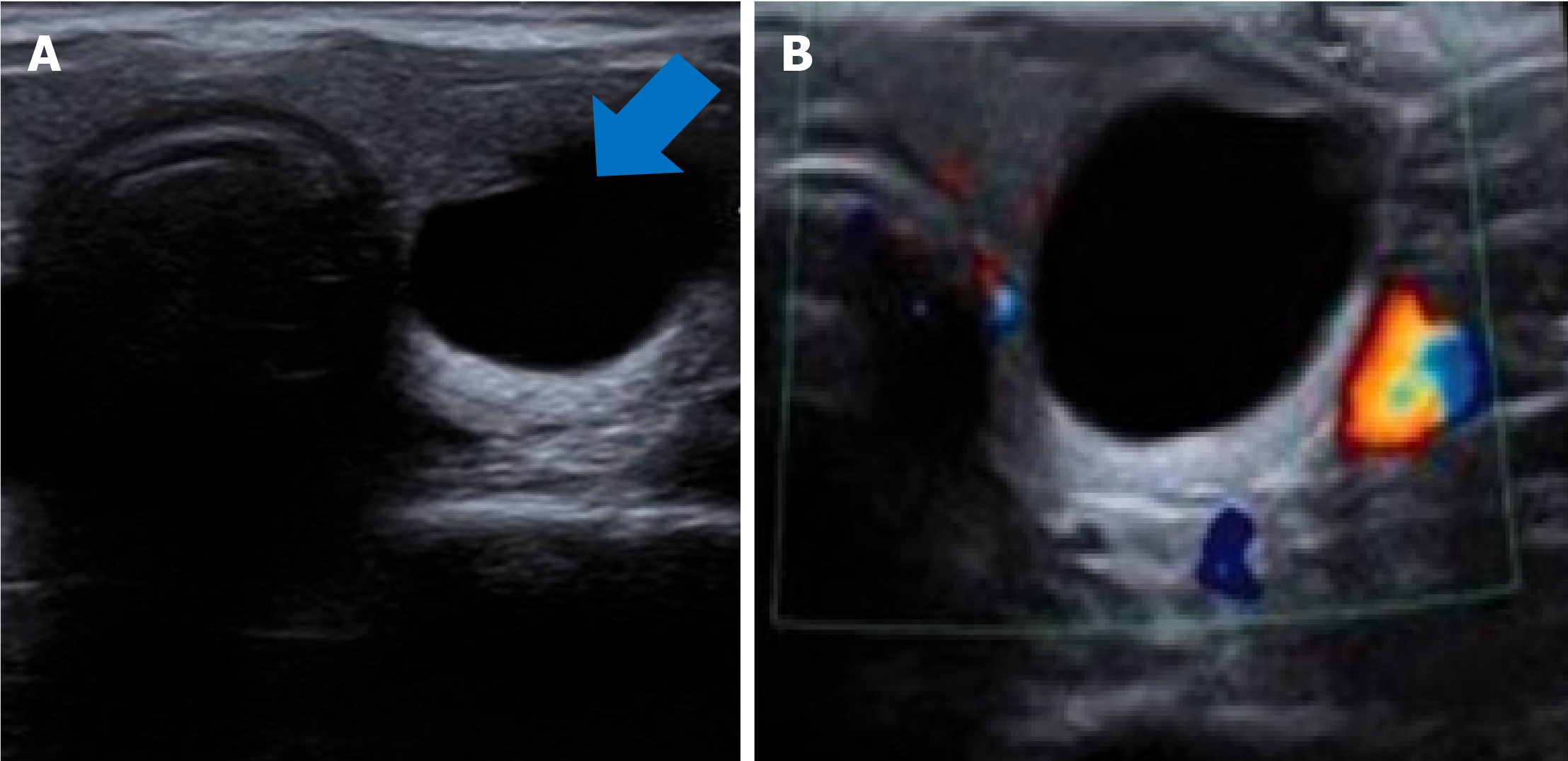
Figure 6 Ultrasound images of an anechoic cystic lesion in the left lobe of the thyroid gland.
A: Anechoic cystic lesion in the left lobe of the thyroid gland (blue arrow); B: No blood flow signal was observed with ultrasound.
- Citation: Celik AS, Yosunkaya H, Yayilkan Ozyilmaz A, Memis KB, Aydin S. Echinococcus granulosus in atypical localizations: Five case reports. World J Nephrol 2025; 14(2): 103027
- URL: https://www.wjgnet.com/2220-6124/full/v14/i2/103027.htm
- DOI: https://dx.doi.org/10.5527/wjn.v14.i2.103027