Published online Dec 24, 2016. doi: 10.5500/wjt.v6.i4.743
Peer-review started: June 28, 2016
First decision: August 5, 2016
Revised: October 8, 2016
Accepted: November 1, 2016
Article in press: November 3, 2016
Published online: December 24, 2016
Processing time: 172 Days and 5 Hours
To explore the effect of primary liver disease and comorbidities on transplant length of stay (TLOS) and LOS in later admissions in the first two years after liver transplantation (LLOS).
A linked United Kingdom Liver Transplant Audit - Hospital Episode Statistics database of patients who received a first adult liver transplant between 1997 and 2010 in England was analysed. Patients who died within the first two years were excluded from the primary analysis, but a sensitivity analysis was also performed including all patients. Multivariable linear regression was used to evaluate the impact of primary liver disease and comorbidities on TLOS and LLOS.
In 3772 patients, the mean (95%CI) TLOS was 24.8 (24.2 to 25.5) d, and the mean LLOS was 24.2 (22.9 to 25.5) d. Compared to patients with cancer, we found that the largest difference in TLOS was seen for acute hepatic failure group (6.1 d; 2.8 to 9.4) and the largest increase in LLOS was seen for other liver disease group (14.8 d; 8.1 to 21.5). Patients with cardiovascular disease had 8.5 d (5.7 to 11.3) longer TLOS and 6.0 d (0.2 to 11.9) longer LLOS, compare to those without. Patients with congestive cardiac failure had 7.6 d longer TLOS than those without. Other comorbidities did not significantly increase TLOS nor LLOS.
The time patients spent in hospital varied according to their primary liver disease and some comorbidities. Time spent in hospital of patients with cancer was relatively short compared to most other indications. Cardiovascular disease and congestive cardiac failure were the comorbidities with a strong impact on increased LOS.
Core tip: Time patients spent in hospital in transplant admission and in later admissions after liver transplantation may reflect the success of liver transplantation. By analysing a linked United Kingdom Liver Transplant Audit - Hospital Episode Statistics database between 1997 and 2010, we found that average transplant length of stay (LOS) was 24.8 d, and mean LOS of all admissions in the first two years after transplantation was 24.2 d. Primary liver disease and comorbidities had a significant impact on LOS. Patients transplanted for cancer has shorter LOS compared to other indications. Cardiovascular disease and congestive cardiac failure were associated with increased LOS.
- Citation: Tovikkai C, Charman SC, Praseedom RK, Gimson AE, van der Meulen J. Time spent in hospital after liver transplantation: Effects of primary liver disease and comorbidity. World J Transplant 2016; 6(4): 743-750
- URL: https://www.wjgnet.com/2220-3230/full/v6/i4/743.htm
- DOI: https://dx.doi.org/10.5500/wjt.v6.i4.743
The short-term and long-term survival after liver transplantation has been improving over the last few decades. However, length of stay (LOS) is another outcome that reflects the success of liver transplantation. Transplant LOS (TLOS) has also been one of the main outcomes in investigating health care resource use in organ transplantation. Identifying variables predicting longer LOS will help clinicians plan hospital resources in advance, and maximise the resource utilisation. LOS in transplant admission can also reliably reflect the cost of liver transplant admission[1].
There are several studies report risk factors predicting longer transplant LOS[2-9]. Recipient factors (e.g., age, sex, liver disease severity, retransplantation, pre-transplant nutritional status, pre-transplant renal support), donor factors (e.g., age, weight, non-local donor centre) and early post-transplant complications and graft dysfunction have been shown to be associated with prolonged transplant LOS. LOS also varies between liver transplant centres[4,5]. Nevertheless, primary liver disease and comorbidities have rarely been investigated in terms of their effects on LOS. Moreover, the previous studies were based on only single or few centres, and the cohort sizes were often limited. In this study, we used a national clinical database linked to an administrative hospital database in England to investigate LOS in a larger national cohort of liver transplant patients.
LOS in later admissions after liver transplantation may reflect quality of life after liver transplantation and represent the success of liver transplantation. Moreover, it can reflect the healthcare resource use in the maintenance period after liver transplantation. To the best of our knowledge, there has not been any study in this topic.
In this study, we aim to investigate the effect of primary liver disease and pre-transplant comorbidities on TLOS as these two important factors have rarely been studied. The secondary aim is the effect of these factors on LOS in later admissions (LLOS) in the first two years after liver transplantation.
Records from the United Kingdom Liver Transplant Audit (UKLTA) database linked at a patient level to Hospital Episode Statistics (HES) records were used in this study. The UKLTA database prospectively collects liver transplant-specific data for all patients undergoing liver transplantation in the United Kingdom for audit purposes[10]. The HES database is an administrative hospital database of all admissions to National Health Service (NHS) hospitals in England[11]. A HES record contains the tenth revision of the International Classification of Diseases (ICD-10) diagnosis codes[12], procedure codes, admission method as well as length of hospital stay based on date of admission and date of discharge. The linkage process was based on hierarchical deterministic linkage criteria, including NHS number, sex, date of birth, postcode, date of transplant and a procedure code for liver transplantation or a diagnosis code relevant to liver disease. A detailed description of the linkage process has been published elsewhere[13].
This linked database contained records of patients receiving a first liver transplant in England between 1st April 1997 and 31st March 2010. We excluded linked records of paediatric liver transplantation (younger than 17 years), multi-organ transplantation, living-donor liver transplantation and domino liver transplantation. To avoid the interference from the short LOS in patients who died early after transplantation, the patients who died within the first two years after liver transplantation (718 patients) were also excluded from the primary analysis. However, a sensitivity analysis for the whole cohort was also performed. At least two years follow-up was available for all included patients.
LOS information was obtained from the HES database. TLOS was calculated from date of transplant to date of discharge, while LOS of a later admission was calculated from date of admission to date of discharge. LOS of all later admissions in the first two years after transplantation (LLOS) was defined as a sum of LOS of every admission in any NHS hospital in England that had an admission date within the first two years from the date of transplant.
Unadjusted TLOS and LLOS of patients in each primary liver disease group and of patients with each comorbidity were compared using unpaired two-tailed Student’s t-test and analysis of variance (ANOVA) as appropriate. Primary liver diseases were categorised into ten indication groups according to Roberts et al[14], including one group with less common indications grouped together as the other liver diseases group. Eight comorbidities were identified from ICD-10 diagnosis codes in HES based on the adaptation of the Royal College of Surgeons Charlson Score for liver transplantation[15]. Cardiovascular comorbidity comprises of a history of myocardial infarction, peripheral vascular disease and cerebrovascular disease.
Multivariable linear regression analysis was performed to determine the effects of the individual variables on TLOS and LLOS, taking into account other baseline characteristics, severity of liver disease and transplant centres. Variables included in the model were 10-group primary liver disease, all eight comorbidities, recipient age, sex, serum bilirubin, creatinine, sodium and international normalised ratio (INR) of prothrombin time (factors reflecting the severity of liver disease), liver transplant centre and time period of liver transplantation. Serum bilirubin and creatinine were log-transformed before inputting into the model to improve the linearity of the relationship between these factors and LOS. The comorbidities and sex were included as binary variables, while primary liver disease groups, transplant centre and time period of liver transplantation were entered as categorical variables. The remaining variables were included as continuous variables.
LOS may not only depend on disease and patient factors, such as type and severity of liver disease and comorbidities, but also on hospital policy that may change over time. Therefore, we included the information about individual transplant centre and time period of liver transplantation in the models.
The ten primary liver disease groups were mutually exclusive. In the multivariable models, coefficients of primary liver disease groups were compared to cancer group as a reference group because it was one of the most common and shortest LOS groups. To make the comparison easier to interpret, we also presented adjusted mean LOS, which reflects LOS for these groups after taking other variables into account. The adjusted mean TLOS and LLOS for patients in each of the primary liver disease groups were calculated based on the prediction from multivariable linear regression models and presented along with their 95% confidence intervals (CI). This represents the LOS according to primary liver disease groups with an average case-mix profile of other variables in the model.
To ensure that patients with missing values were not excluded from the analyses, missing values were imputed with ten plausible data sets using multiple imputation with chain equations technique[16]. The ten completed data sets were individually analysed, and estimates were then pooled to give final estimates using Rubin’s rules[17]. However, all of the variables in the model had missing values for less than 5% of the patients. All statistical analyses were performed using Stata version 11.2 (StataCorp, College Station, TX, United States). A P-value of less than 0.05 was considered statistically significant.
The primary analysis included only patients who survived the first two years after transplantation as the patients who died early after transplantation would shorten the average of LOS. A sensitivity analysis for TLOS was performed using the whole cohort including patients who died in the first two years after transplantation (4490 patients).
The data used in this study were from 3772 adult patients who had a first liver transplant in England from April 1997 to March 2010 and survived the first two years after liver transplantation. The median (interquartile range: IQR) age was 52 (42 to 59) years, and 58.7% of the patients were male. The most common indication for liver transplantation was alcoholic cirrhosis (20.0%), followed by cancer (13.9%) and primary biliary cirrhosis (13.4%). The most common comorbidity was diabetes mellitus with a prevalence of 20.8%, followed by chronic pulmonary disease (9.1%) and chronic renal disease (6.6%) (Table 1). In terms of pre-transplant status, 74.0% of the patients were at home, while 16.0% were in hospital but not ventilated, and 10.0% were hospitalised and ventilated at the time of transplantation. Some 4.7% of the patients received a liver graft from donation after cardiac death.
| Characteristic | Value | Missing (n) |
| Number | 3772 | |
| Age (yr) | 52 (42-59) | 0 |
| Sex (%) | 0 | |
| Male | 2214 (58.7) | |
| Female | 1558 (41.3) | |
| Primary liver disease (%) | 0 | |
| Cancer | 525 (13.9) | |
| Acute hepatic failure | 455 (12.1) | |
| Hepatitis C cirrhosis | 392 (10.4) | |
| Primary sclerosing cholangitis | 354 (9.4) | |
| Hepatitis B cirrhosis | 98 (2.6) | |
| Primary biliary cirrhosis | 507 (13.4) | |
| Alcoholic cirrhosis | 753 (20.0) | |
| Autoimmune and cryptogenic cirrhosis | 348 (9.2) | |
| Metabolic liver disease | 107 (2.8) | |
| Other liver disease | 233 (6.2) | |
| Comorbidities (%) | ||
| Cardiovascular disease | 200 (5.3) | 0 |
| Congestive cardiac failure | 82 (2.2) | 0 |
| Connective tissue disease | 134 (3.6) | 0 |
| Dementia | 159 (4.2) | 0 |
| Diabetes mellitus | 784 (20.8) | 0 |
| Non-hepatic malignancy | 40 (1.1) | 0 |
| Chronic pulmonary disease | 344 (9.1) | 0 |
| Chronic renal disease | 247 (6.6) | 0 |
| Era of liver transplantation (%) | 0 | |
| April 1997 - September 2000 | 841 (22.3) | |
| October 2000 - September 2003 | 899 (23.8) | |
| October 2003 - September 2006 | 897 (23.8) | |
| October 2006 - March 2010 | 1135 (30.1) | |
| Bilirubin (µmol/L) | 54 (27-124) | 20 |
| Creatinine (µmol/L) | 89 (74-109) | 2 |
| INR | 1.4 (1.2-1.8) | 162 |
| Sodium (mmol/L) | 137 (134-140) | 8 |
| UKELD score | 55 (51-59) | 184 |
Overall, patients spent an average of 24.8 d (95%CI: 24.2 to 25.5) in hospital during their transplant admission, and 24.2 d (22.9 to 25.5) in later admissions in the first two years after transplantation (Table 2).
| Variable | n (%) | Unadjusted TLOS | Unadjusted LLOS | ||||
| (d) | 95%CI | P-value | (d) | 95%CI | P-value | ||
| Overall average | 3772 | 25 | 24-26 | N/A | 24 | 23-26 | N/A |
| Primary liver disease groups | |||||||
| Cancer | 525 (13.9) | 22 | 20-24 | < 0.001 | 22 | 18-25 | < 0.001 |
| Acute hepatic failure | 455 (12.1) | 33 | 32-35 | 26 | 22-30 | ||
| Hepatitis C cirrhosis | 392 (10.4) | 27 | 25-29 | 26 | 22-30 | ||
| Primary sclerosing cholangitis | 354 (9.4) | 23 | 20-25 | 27 | 23-31 | ||
| Hepatitis B cirrhosis | 98 (2.6) | 22 | 18-26 | 21 | 13-29 | ||
| Primary biliary cirrhosis | 507 (13.4) | 21 | 20-23 | 20 | 16-23 | ||
| Alcoholic cirrhosis | 753 (20.0) | 24 | 23-26 | 22 | 19-25 | ||
| Autoimmune and cryptogenic | 348 (9.2) | 22 | 20-24 | 23 | 18-27 | ||
| Metabolic liver disease | 107 (2.8) | 26 | 22-30 | 29 | 21-37 | ||
| Other liver disease | 233 (6.2) | 28 | 26-31 | 37 | 32-42 | ||
| Comorbidities | |||||||
| Cardiovascular disease | 200 (5.3) | 33 | 28-39 | < 0.001 | 31 | 24-38 | 0.02 |
| Congestive cardiac failure | 82 (2.2) | 32 | 24-39 | 0.003 | 18 | 13-24 | 0.18 |
| Connective tissue disease | 134 (3.6) | 22 | 20-25 | 0.13 | 25 | 18-32 | 0.91 |
| Dementia | 159 (4.2) | 25 | 21-28 | 0.87 | 26 | 21-32 | 0.54 |
| Diabetes mellitus | 784 (20.8) | 24 | 23-26 | 0.42 | 26 | 23-29 | 0.18 |
| Non-hepatic malignancy | 40 (1.1) | 23 | 17-29 | 0.65 | 24 | 10-37 | 0.91 |
| Chronic pulmonary disease | 344 (9.1) | 27 | 25-30 | 0.04 | 28 | 24-33 | 0.06 |
| Chronic renal disease | 247 (6.6) | 27 | 23-30 | 0.17 | 32 | 25-38 | 0.003 |
Primary liver disease groups were significant predictors of both TLOS and LLOS (Table 2). Using cancer group as a baseline, the multivariable analysis demonstrated that patients in acute hepatic failure (6.1 d longer), other liver disease (5.9 d longer), metabolic and non-alcoholic fatty liver disease (4.3 d longer) and hepatitis C cirrhosis (3.9 d longer) groups had significantly longer TLOS than the baseline. As for LLOS, other liver disease (14.8 d longer) and primary sclerosing cholangitis (8.4 d longer) were significantly associated with longer LLOS than the baseline (Table 3).
| Variable value | Coefficient for TLOS | Coefficient for LLOS | ||||
| (d) | 95%CI | P-value | (d) | 95%CI | P-value | |
| Primary liver disease groups1 | ||||||
| Cancer | 0 | Reference | < 0.001 | 0 | Reference | < 0.001 |
| Acute hepatic failure | 6.1 | 2.8, 9.4 | 4 | -3.3, 11.3 | ||
| Hepatitis C cirrhosis | 3.9 | 1.3, 6.4 | 5.4 | -0.1, 10.9 | ||
| Primary sclerosing cholangitis | 0.2 | -2.5, 3.0 | 8.4 | 2.6, 14.3 | ||
| Hepatitis B cirrhosis | 1.9 | -2.3, 6.1 | 1 | -7.9, 9.9 | ||
| Primary biliary cirrhosis | -0.5 | -3.2, 2.1 | 0.2 | -5.6, 5.9 | ||
| Alcoholic cirrhosis | 0.6 | -1.6, 2.8 | 0.6 | -4.1, 5.4 | ||
| Autoimmune and cryptogenic | 0.1 | -2.6, 2.9 | 1.4 | -4.4, 7.2 | ||
| Metabolic liver disease | 4.3 | 0.3, 8.4 | 7.1 | -1.5, 15.7 | ||
| Other liver disease | 5.9 | 2.8, 9.1 | 14.8 | 8.1, 21.5 | ||
| Comorbidities2 | ||||||
| Cardiovascular disease | 8.5 | 5.7, 11.3 | < 0.001 | 6 | 0.2, 11.9 | 0.04 |
| Congestive cardiac failure | 7.6 | 3.4, 11.8 | < 0.001 | -5 | -14.0, 3.9 | 0.27 |
| Connective tissue disease | -1.4 | -4.8, 2.0 | 0.42 | 2.3 | -4.9, 9.5 | 0.54 |
| Dementia | 0.2 | -2.9, 3.4 | 0.87 | 3.6 | -3.1, 10.4 | 0.29 |
| Diabetes mellitus | 1 | -0.6, 2.6 | 0.22 | 2.6 | -0.8, 6.0 | 0.13 |
| Non-hepatic malignancy | -0.7 | -6.7, 5.3 | 0.82 | -0.5 | -13.2, 12.2 | 0.94 |
| Chronic pulmonary disease | 1.6 | -0.5, 3.8 | 0.14 | 4.3 | -0.2, 8.9 | 0.06 |
| Chronic renal disease | 1 | -1.6, 3.5 | 0.47 | 4.8 | -0.7, 10.3 | 0.09 |
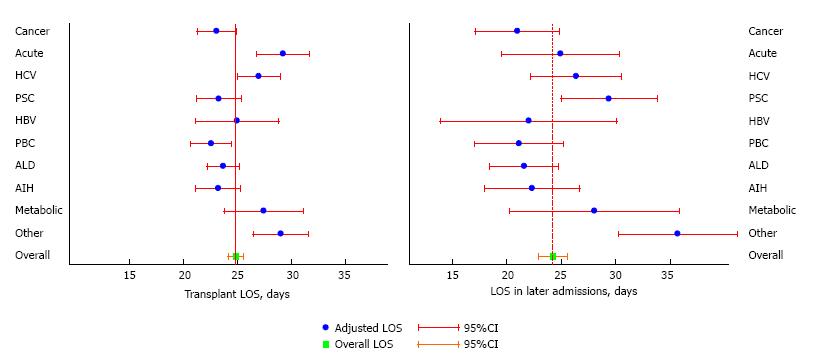
Figure 1 presents the same above results using adjusted means for TLOS and LLOS, and further illustrates that patients with acute hepatic failure, hepatitis C cirrhosis, metabolic and non-alcoholic fatty liver disease and other liver disease had longer than average TLOS and LLOS, although not all significantly so. Whereas, patients with liver diagnosis of cancer, primary biliary cirrhosis, alcoholic cirrhosis and autoimmune hepatitis and cryptogenic cirrhosis groups had shorter than average TLOS and LLOS. Of note, primary sclerosing cholangitis was associated with shorter TLOS, but significantly longer LLOS (Figure 1).
Patients with atherosclerotic cardiovascular disease had the longest unadjusted TLOS at 33 d, and those with chronic renal disease had the longest unadjusted LLOS at 32 d (Table 2). The multivariable linear regression analysis demonstrated that cardiovascular disease and congestive cardiac failure were significantly associated with longer TLOS. Patients with cardiovascular disease spent an average of 8.5 d longer in transplant admission than those without the comorbidity, and those with a history of congestive cardiac failure spent 7.6 d longer than those without, confirming what previously observed in unadjusted LOS (Table 3).
Patients with cardiovascular disease spent significantly longer time in hospital in the first two years after transplantation than those without the comorbidity (6.0 d longer). Those with chronic renal disease and chronic pulmonary disease spent 4.8 d and 4.3 d longer than those without the comorbidities, respectively, albeit not statistically significant (Table 3).
After including 718 patients who died within the first two years after transplantation, the sensitivity analysis of 4490 patients found that primary liver disease, cardiovascular disease and congestive cardiac failure remained statistically significant in predicting TLOS. In terms of primary liver disease groups, patients in other liver disease group had the longest TLOS, followed by acute hepatic failure group. Cardiovascular disease were associated with 8.7 d longer TLOS than those without the comorbidity, while patients with congestive cardiac failure had 7.7 d longer TLOS than those without, which were similar to those in the primary analysis (Table 4).
| Variable | Coefficient for TLOS | ||
| (d) | 95%CI | P-value | |
| Primary liver disease groups1 | |||
| Cancer | 0.0 | Reference | 0.001 |
| Acute hepatic failure | 3.7 | 0.2, 7.2 | |
| Hepatitis C cirrhosis | 3.3 | 0.6, 6.1 | |
| Primary sclerosing cholangitis | -0.3 | -3.2, 2.7 | |
| Hepatitis B cirrhosis | 0.6 | -4.0, 5.2 | |
| Primary biliary cirrhosis | -1.5 | -4.4, 1.4 | |
| Alcoholic cirrhosis | 1.1 | -1.3, 3.5 | |
| Autoimmune and cryptogenic | 0.5 | -2.5, 3.4 | |
| Metabolic liver disease | 3.3 | -0.9, 7.6 | |
| Other liver disease | 5.9 | 2.5, 9.2 | |
| Comorbidities2 | |||
| Cardiovascular disease | 8.7 | 5.8, 11.5 | < 0.001 |
| Congestive cardiac failure | 7.7 | 3.6, 11.8 | < 0.001 |
| Connective tissue disease | -0.3 | -4.0, 3.3 | 0.86 |
| Dementia | 1.1 | -2.4, 4.6 | 0.54 |
| Diabetes mellitus | 1.1 | -0.6, 2.8 | 0.21 |
| Non-hepatic malignancy | 0.9 | -4.6, 6.3 | 0.76 |
| Chronic pulmonary disease | 1.2 | -1.1, 3.5 | 0.3 |
| Chronic renal disease | 1.7 | -1.0, 4.4 | 0.22 |
Liver transplant recipients spent in total 49 d in hospital during the first two years after transplantation, approximately half in the transplant admission and the other half in subsequent admissions. However, the LOS was affected by primary liver disease and some comorbidities. Patients with liver diagnosis in acute hepatic failure, hepatitis C cirrhosis and other liver disease groups had a longer TLOS than those in any other groups, while patients in primary sclerosing cholangitis and other liver disease groups had longer LLOS. Patients with cardiovascular disease and cardiac failure also had longer TLOS than those without these comorbidities, and patients with cardiovascular disease spent longer time in later admissions than those without.
In terms of primary liver disease, acute hepatic failure, hepatitis C cirrhosis and other liver disease were associated with longer TLOS. Patients with acute hepatic failure are mostly intubated and ventilated and on renal replacement therapy[18]. Therefore, it is not unexpected that they required more time to recover from the liver transplant operation. Hepatitis C cirrhosis may be related to more complications after liver transplantation, and this is probably the reason why patients transplanted for this indication spent longer time in transplant admission. The group of patients with other liver disease is the most heterogeneous group of patients with a wide range of liver diagnoses, consisting mainly of Budd-Chiari syndrome, secondary biliary cirrhosis and polycystic liver disease. Thus, the reason why these patients had longer LOS needs further investigation.
Patients with primary sclerosing cholangitis had relatively shorter TLOS, but relatively longer LLOS. These discrepancies may be a result of a higher rate of recurrent disease, vascular complications or conditions related to ulcerative colitis that need admissions for interventions or procedures[19]. Nevertheless, the reasons for readmissions can be either transplant-related or non-transplant-related, and they were not explored in this study.
With respect to comorbidities, common comorbidities, such as diabetes, chronic pulmonary and renal disease, showed no impact on TLOS, while less common comorbidities, such as cardiovascular disease and congestive cardiac failure, were found to have an impact on TLOS. Cardiovascular disease, which is the grouping of three comorbid conditions in the same disease spectrum (myocardial infarction, peripheral vascular disease and cerebrovascular disease), was significantly associated with longer TLOS as was congestive cardiac failure. We have shown elsewhere that a previous history of cardiovascular disease and cardiac failure were also associated with higher 90-d mortality[15]. This study further showed that these groups of high-risk patients also used more health resources during their transplant admission. This is probably because of a higher risk of cardiac complications following a hemodynamically stressful liver transplant operation in these already compromised patients.
A previous single-centre study carried out in the United States with only 83 patients found that multi-vessel coronary artery disease is associated with higher mortality, increased LOS and post-operative vasopressor requirements[20], which is in line with the results found in our national cohort in England. In addition, we demonstrated that the LOS in later admissions in the first two years in patients with atherosclerotic cardiovascular disease was also longer, particularly in those who survived the first two years. This reflects that these patients with cardiovascular comorbidity have a higher mortality risk and require more healthcare resources during transplant admissions as well as the early period after liver transplantation.
Our results have a number of implications for clinical practice. First, LOS of the transplant admission and of later admissions can be an alternative marker of outcomes after liver transplantation, especially in the era that graft and patient survival after liver transplantation have been excellent. LOS in later admissions after liver transplantation may also reflect the quality of life and functional status of a patient after transplantation. A successful liver transplantation should return a patient back to the healthy status with as few admissions after transplantation as possible. Second, the ability to estimate LOS may be beneficial to the pre-transplant counselling process as it can help to inform patients and their relatives what to expect after liver transplantation. Third, another benefit of estimating LOS is that it would help clinicians and hospitals plan their resource utilisation and bed management. For example, patients transplanted for cancer spent, on average, a total of 44 d in the first two years after transplantation, whereas patients who were transplanted with an indication in other liver disease group, such as Budd-Chiari syndrome, had a total LOS that was 50% longer (66 d) (Figure 1). Fourth, our results can improve economic evaluations of liver transplantation as it provides more accurate estimates of LOS for patients with comorbidities.
We note a number of limitations of this study. Firstly, we have not explored the reasons for later admissions. It may be beneficial to understand the indication for readmissions in particular groups of patients, and this may warrant further research. Secondly, this study includes only patients who had a first liver transplant. It is known that the outcomes of retransplantation are much different to those of first liver transplantation[21]. Retransplantation has also been shown to be associated with longer transplant LOS[4].
We have shown that the time patients spent in hospital after liver transplantation is linked to primary liver disease and comorbidities. LOS was relative short for patient who had a liver transplant for cancer whereas the opposite was true for patients with atherosclerotic cardiovascular disease and congestive cardiac failure.
The authors would like to thank all liver transplant centres for providing data to the United Kingdom Liver Transplant Audit. We would also like to thank all those involved in collecting and handling liver transplant data at the National Health Service Blood and Transplant. The United Kingdom Liver Transplant Audit is supported by the NHS National Specialised Commissioning Group/NHS England. HES data have been re-used with the permission of The Health and Social Care Information Centre. Chutwichai Tovikkai is supported by the Faculty Scholarship from Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand, and is a recipient of the “Raymond and Beverly Sackler Studentship” from the School of Clinical Medicine, University of Cambridge, Cambridge, United Kingdom.
Time patients spent in hospital after transplantation is directly related with health care resource use and partly reflects the success of liver transplantation. Identifying factors predicting longer length of stay will help clinicians and hospitals to plan and maximise the resource utilisation.
Several recipient and donor factors have been found to be associated with prolonged transplant length of stay. However, primary liver disease and comorbidities have rarely been investigated in this issue. Length of stay in later admissions after transplantation also reflects quality of life after liver transplantation and can represent the success of liver transplantation. This has never been investigated in liver transplantation.
Based on the United Kingdom national liver transplant cohort, the authors demonstrated that transplant length of stay was affected by primary liver disease and comorbidities. Patients with acute hepatic failure, hepatitis C cirrhosis, atherosclerotic cardiovascular disease and a history of congestive cardiac failure stayed longer in hospital in their transplant admissions, while patients with primary sclerosing cholangitis spent more time in subsequent admissions in the first two years after liver transplantation.
Estimating length of stay will help clinicians and hospitals plan their health care resource utilisation including bed management. Moreover, knowing the estimated length of stay will be beneficial to the pre-transplant counselling process. It can help inform patients and relatives what they expect after liver transplantation. Finally, in the era that graft and patient survival after liver transplantation have been excellent, length of stay of the transplant admission and of later admissions can be a surrogate of outcomes after liver transplantation. Length of stay in later admissions after liver transplantation also specifically reflects the quality of life of patients after transplantation and the success of liver transplantation as it should return a patient back to the healthy status with as few admissions after transplantation as possible.
Transplant length of stay (TLOS) was calculated from date of transplant to date of discharge, not including time patients spent in hospital in the pre-transplant period. Length of stay in later admissions was a sum of length of stay of every admission in any National Health Service hospital in England that had an admission date within the first two years from the date of transplant. Cardiovascular comorbidity comprises of a history of myocardial infarction, peripheral vascular disease and cerebrovascular disease coded in the administrative hospital database in any previous admission in the preceding year before the transplant. Congestive cardiac failure is defined by a history of congestive cardiac failure coded in the administrative hospital database in any previous admission in the preceding year before the transplant. Other liver disease is a group of indications for liver transplantation that is consisted of less common indications grouped together. It is the most heterogenous group of indications, including mainly Budd-Chiara syndrome, secondary biliary cirrhosis and polycystic liver disease.
This study investigated the time after surgery after liver transplantation. The aim was clear, and methods were appropriate.
Manuscript source: Invited manuscript
Specialty type: Transplantation
Country of origin: Thailand
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Balaban Y, Fava G, Feltracco P, Tomizawa M S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Showstack J, Katz PP, Lake JR, Brown RS, Dudley RA, Belle S, Wiesner RH, Zetterman RK, Everhart J. Resource utilization in liver transplantation: effects of patient characteristics and clinical practice. NIDDK Liver Transplantation Database Group. JAMA. 1999;281:1381-1386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 160] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 2. | Markmann JF, Markmann JW, Desai NM, Baquerizo A, Singer J, Yersiz H, Holt C, Ghobrial RM, Farmer DG, Busuttil RW. Operative parameters that predict the outcomes of hepatic transplantation. J Am Coll Surg. 2003;196:566-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Bucuvalas JC, Zeng L, Anand R. Predictors of length of stay for pediatric liver transplant recipients. Liver Transpl. 2004;10:1011-1017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Washburn WK, Meo NA, Halff GA, Roberts JP, Feng S. Factors influencing liver transplant length of stay at two large-volume transplant centers. Liver Transpl. 2009;15:1570-1578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 49] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Smith JO, Shiffman ML, Behnke M, Stravitz RT, Luketic VA, Sanyal AJ, Heuman DM, Fisher RA, Cotterell AH, Maluf DG. Incidence of prolonged length of stay after orthotopic liver transplantation and its influence on outcomes. Liver Transpl. 2009;15:273-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Croome KP, Hernandez-Alejandro R, Chandok N. Early allograft dysfunction is associated with excess resource utilization after liver transplantation. Transplant Proc. 2009;45:259-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Hakeem AR, Cockbain AJ, Raza SS, Pollard SG, Toogood GJ, Attia MA, Ahmad N, Hidalgo EL, Prasad KR, Menon KV. Increased morbidity in overweight and obese liver transplant recipients: a single-center experience of 1325 patients from the United Kingdom. Liver Transpl. 2013;19:551-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 109] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 8. | Montano-Loza AJ, Meza-Junco J, Baracos VE, Prado CM, Ma M, Meeberg G, Beaumont C, Tandon P, Esfandiari N, Sawyer MB. Severe muscle depletion predicts postoperative length of stay but is not associated with survival after liver transplantation. Liver Transpl. 2014;20:640-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 245] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 9. | Nachmany I, Dvorchik I, Devera M, Fontes P, Demetris A, Humar A, Marsh JW. A validated model for predicting outcome after liver transplantation: implications on transplanting the extremely sick. Transpl Int. 2013;26:1108-1115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | van der Meulen JH, Lewsey JD, Dawwas MF, Copley LP. Adult orthotopic liver transplantation in the United Kingdom and Ireland between 1994 and 2005. Transplantation. 2007;84:572-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Hospital Episode Statistics: The Health and Social Care Information Centre. [accessed 2015 Feb]. Available from: http://www.hscic.gov.uk/hes. |
| 12. | World Health Organization. International Statistical Classification of Diseases and Related Health Problems. 10th revision edition. Geneva: World Health Organization 1992; . |
| 13. | Tovikkai C, Charman SC, Praseedom RK, Gimson AE, Watson CJ, Copley LP, van der Meulen J. Linkage of a national clinical liver transplant database with administrative hospital data: methods and validation. Transplantation. 2014;98:341-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Roberts MS, Angus DC, Bryce CL, Valenta Z, Weissfeld L. Survival after liver transplantation in the United States: a disease-specific analysis of the UNOS database. Liver Transpl. 2004;10:886-897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 252] [Article Influence: 11.5] [Reference Citation Analysis (2)] |
| 15. | Tovikkai C, Charman SC, Praseedom RK, Gimson AE, van der Meulen J. Time-varying impact of comorbidities on mortality after liver transplantation: a national cohort study using linked clinical and administrative data. BMJ Open. 2015;5:e006971. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 16. | White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011;30:377-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6773] [Cited by in RCA: 6308] [Article Influence: 420.5] [Reference Citation Analysis (0)] |
| 17. | Marshall A, Altman DG, Holder RL, Royston P. Combining estimates of interest in prognostic modelling studies after multiple imputation: current practice and guidelines. BMC Med Res Methodol. 2009;9:57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 418] [Cited by in RCA: 638] [Article Influence: 37.5] [Reference Citation Analysis (0)] |
| 18. | Dawwas MF, Gimson AE, Lewsey JD, Copley LP, van der Meulen JH. Survival after liver transplantation in the United Kingdom and Ireland compared with the United States. Gut. 2007;56:1606-1613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 58] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 19. | Strasser S, Sheil AG, Gallagher ND, Waugh R, McCaughan GW. Liver transplantation for primary sclerosing cholangitis versus primary biliary cirrhosis: a comparison of complications and outcome. J Gastroenterol Hepatol. 1993;8:238-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Yong CM, Sharma M, Ochoa V, Abnousi F, Roberts J, Bass NM, Niemann CU, Shiboski S, Prasad M, Tavakol M. Multivessel coronary artery disease predicts mortality, length of stay, and pressor requirements after liver transplantation. Liver Transpl. 2010;16:1242-1248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 64] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Hong JC, Kaldas FM, Kositamongkol P, Petrowsky H, Farmer DG, Markovic D, Hiatt JR, Busuttil RW. Predictive index for long-term survival after retransplantation of the liver in adult recipients: analysis of a 26-year experience in a single center. Ann Surg. 2011;254:444-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 59] [Article Influence: 3.9] [Reference Citation Analysis (0)] |