Published online Dec 24, 2016. doi: 10.5500/wjt.v6.i4.682
Peer-review started: July 21, 2016
First decision: September 5, 2016
Revised: October 3, 2016
Accepted: October 22, 2016
Article in press: October 24, 2016
Published online: December 24, 2016
Processing time: 149 Days and 1.5 Hours
The risk of contrast-induced nephropathy (CIN) in renal transplant recipients is increased in diabetics, patients with impaired basal kidney function, patients in shock, patients presenting with acute emergency and in old age recipients. Approximately one-third of all hospitalized patients with acute kidney injury is attributed to CIN. In the United States, it is the third leading cause of hospital-acquired renal failure. Therefore, efforts should be directed to minimize CIN-related morbidity and mortality as well as to shorten hospital stay. While the role of peri-procedural prophylactic hydration with saline is unequivocal; the use of acetyl cysteine is not based on robust evidence. The utility of theophylline, aminophylline, calcium channel blockers, natriuretic peptide, and diuretics does not have proven role in attenuating CIN incidence. We aim to analyze the evidence for using various protocols in published literature to limit CIN-associated morbidity and mortality, particularly during surveillance of the renal allograft survival.
Core tip: The renal transplant is usually a solitary kidney with diverse hemodynamic changes and exposed to the immunosuppressive agents for a long period. Any superadded stress such as contrast-induced nephropathy (CIN), will definitely affect allograft function. We provide in this article a comprehensive review of the current evidence on the true incidence, the mechanism of damage induced by CIN and available preventive measures to counteract the possible effect induced by CIN.
- Citation: Abbas FM, Julie BM, Sharma A, Halawa A. “Contrast nephropathy” in renal transplantation: Is it real? World J Transplant 2016; 6(4): 682-688
- URL: https://www.wjgnet.com/2220-3230/full/v6/i4/682.htm
- DOI: https://dx.doi.org/10.5500/wjt.v6.i4.682
Perioperative transplant complications are reported to involve about 15%-20% of the kidney transplant recipients. Diagnostic ultrasound (US) is the most common and first line imaging modality[1], since it is safe, noninvasive, gives a rapid diagnosis and also a portable tool for many surgical emergencies requiring bedside imaging[2-5]. The utility of ultrasonography in management of hydronephrosis, renal masses, renal artery stenosis (RAS) and pyelonephritis in renal allograft is well documented[1].
Computed tomography (CT) scanning and CT-guided interventions play a vital role in investigating post-operative complications. Magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) can be used safely where there is renal dysfunction, since the “Gadolinium-based” contrast media can be safely used with minimal nephrotoxic effects. Post-transplant complications such as vessel thrombosis can also be assessed using these modalities. Allograft “morphology and function” can be effectively assessed by using intravenous Gadopentetate Dimeglumine (DTPA) to the MRA technique[6].
However, the patients with pacemakers, aneurysmal clips, or evident claustrophobia cannot be safely exposed to MRI studies. Gadolinium-based media have been linked to the development of nephrogenic systemic fibrosis (NSF). Another drawback of MRI, is the “layering” of the excreted gadolinium in the urinary bladder causing multiple image artifacts. Alternatively, CT is better for the evaluation of the kidney and urinary bladder for renal stones and ureter and bladder abnormalities. To summarize, MRI is usually dedicated to the evaluation of transplant recipient, whereas CT and CT angiogram are reserved for potential donors[6].
Vasoconstriction induced by the contrast media (CM) can be explained by the direct action of contrast media on vascular smooth muscle and from metabolites such as adenosine and endothelin. Moreover, the osmotic criteria of contrast media, especially in the tubular lumen, affects water reabsorption, leading to a magnifying interstitial pressure. This will be augmented by the increased salt and water load to the distal tubules, will decrease GFR and lead to local compression of the vasa recta. All these factors will aggravate medullary hypoxemia and renal vasoconstriction in an already volume depleted patient.
Finally, contrast media could increase resistance to blood flow by increasing its viscosity and by deranging red blood cells (RBCs) deformability. These manifest as local ischemia leading to activation of reactive oxygen species that result in damage to renal tubules[7].
Up till now, we are sure why renal failure patients are sensitive to contrast utilization. Whether their primary disease is a contributing factor or not, this has to be elucidated by additional future research.
| No. | Trial | Year | No. of KTRs | Need for HDX | CIN | Comments |
| 1 | Light et al[8] | 1975 | 34 | Two | 22 | 20 patients improved after therapy for “graft rejection” |
| 2 | Moreau et al[12] | 1975 | 231 | None | Nil | No increase in risk of CIN in KTRs if contrast studies were performed with normal renal function |
| 3 | Peters et al[11] | 1983 | 93 | None | Very high (84.3%) | No increased risk was found > 120 d post-transplant |
| 4 | Ahuja et al[10] | 2000 | 35 | None | > 21% | Patients received high osmolality contrast, and 94% were on CyA therapy |
| 5 | Charnow et al[16] | 2015 | 76 | None | > 13.2% | CIN did not affect allograft function and survival, according to the researchers |
| 6 | Haider et al[9] | 2015 | 124 | None | 5.60% | The largest retrospective study evaluating incidence of CIN in KTRs. CNIs were being used in 95% patients at the time of contrast administration |
| 7 | Bostock et al[15] | 2016 | 40 | One | 12.50% | Renal dysfunction is 3 times more frequent in KTR treated with EVAR, though overall survival did not differ between groups. Decreased pre-operative eGFR and higher iodine/eGFR ratio are associated with post-operative renal dysfunction |
| 8 | Fananapazir et al[14] | 2016 | 104 | None | 7% and 3% | Incidence of CNI = 7% (7/104) based on a rise of ≥ 0.3 mg/dL and 3% (3/104) based on a rise of ≥ 0.5 mg/dL. With a strict definition (≥ 0.5 mg/dL) had a pre-CT eGFR < 60 mL/min per 1.73 m2. No patients required DX or had allograft loss 30 d after contrast use |
Only a relatively handful of studies have looked into the contrast-induced nephropathy (CIN) in the renal transplant recipients. Light et al[8], 1975 studied thirty-four renal transplant recipients received drip infusion urograms post-transplantation. Twenty-two patients exhibited a change in renal function within 1-4 d of the urogram that was indistinguishable from allograft rejection that is a tender swollen kidney, a rise in serum creatinine, oliguria, diminished urinary sodium, weight gain and hypertension. Two patients developed acute tubular necrosis (ATN) and required hemodialysis, but renal function in the remaining 20 patients improved after therapy for “graft rejection” with intravenous methylprednisolone sodium succinate. Kidneys from older-age donors that were functioning sub-optimally at transplant and kidneys, which exhibited subsequent clinical allograft rejection, were more at risk for CIN. These suggested occult vascular lesions might have been present in the allograft, which was exacerbated when exposed to the irritant vascular effects of contrast media, producing a mild, reversible toxic nephritis. However, several renal grafts with normal function and also those, which never exhibited rejection activity, were also adversely affected by exposure to contrast media. Therefore these agents should be used cautiously, if at all, in the early post-transplant period[8]. CIN was more common and more severe in those with impaired kidney function. This study also found that kidneys from older donors were at higher risk for CIN. In this study, contrast was used before stable creatinine was achieved, these kidney transplant recipients were not on a CNI, and there is no mention of use of any prophylaxis to prevent CIN. More than half of these patients were thought to have acute rejection and were treated as such without consistent biopsy documentation[8].
The incidence of acute kidney injury (AKI) induced by CIN resulting from direct exposure to contrast media in kidney transplants recipients still controversial. The main insult is the ensuing vasoconstriction of the afferent glomerular arterioles and reduction in renal blood flow and glomerular filtration rate. Renal vasoconstriction, as well as direct tubular epithelial toxicity, is the two major mechanisms by which contrast causes AKI as explained by Haider et al[9] in 2015. Immediately after contrast use, there is a transient increase in renal blood flow followed by a prolonged reduction in flow resulting in renal ischemia. So, there is “clustering” of two risk factors here, as both calcineurin inhibitors and IV contrast cause renal ischemia by the dual mechanism: (1) by increasing the release of the vasoconstrictors such as endothelin; and (2) by blocking the release of vasodilators including prostaglandins and nitric oxide[10].
Ahuja et al[10] (2000) also studied 35 kidney transplantation recipients (KTRs) as regard the effect of “volume expansion” as well as the effect of cyclosporine therapy; which documented the presence of CIN in a percentage exceeding 21%, with incidence of CIN was about 15% in patients received volume expansion and exceeds 42% in those who did not. None of these patients had AKI requiring dialysis. In this study, two main insults were reported, first: They received “high osmolality” contrast, and second: 94% were on cyclosporine therapy. The baseline serum creatinine in patients with and without CIN was 1.54 ± 0.17 mg/dL and 1.97 ± 0.20 mg/dL, respectively, P = 0.15, but the volume of contrast was not reported here. Another study- demonstrated by Peters et al[11] in 1983-reported a very high incidence of CIN (84.3%) in the early post-transplant period, but no increased risk was found > 120 d post-transplant.
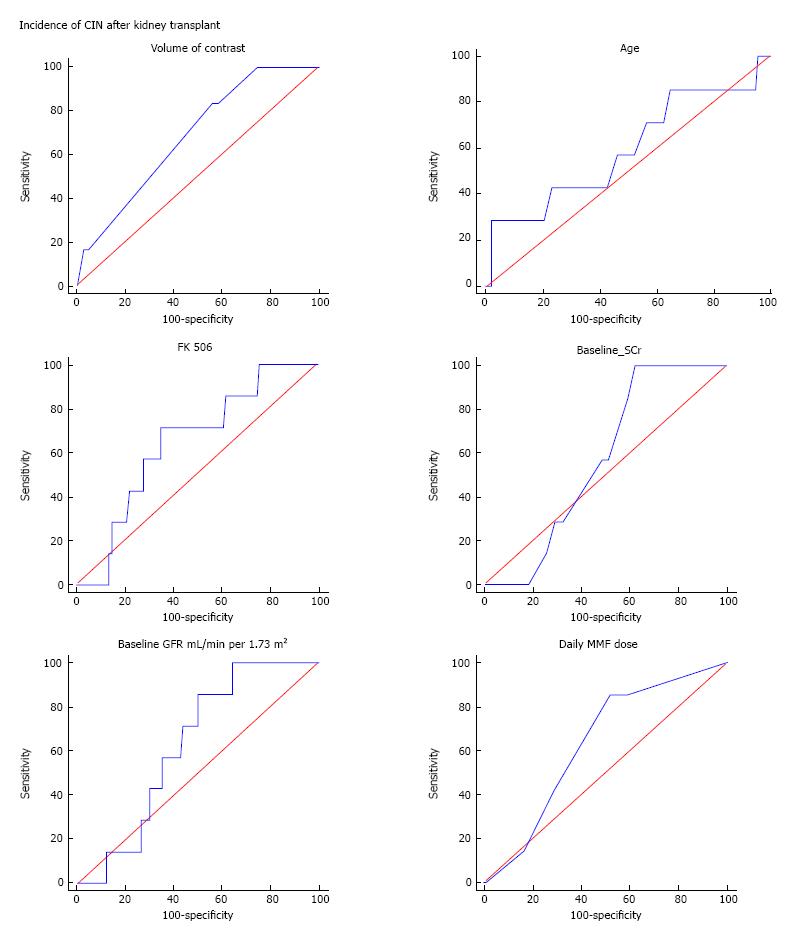
Moreau et al[12] (1975) demonstrated clear evidence that there was no increase in the risk of CIN in kidney transplant recipients if contrast studies were performed against a background of normal renal function. Data observed from these studies showed that older donor kidney, early post-transplant period, impaired baseline kidney function, and lack of prophylactic volume expansion, appear to be important risk factors for increasing the incidence of CIN in kidney transplant recipients (Figure 1). In fact, a direct comparison between these studies regarding the incidence of CIN among is challenging, as the definition of AKI used was not uniform. There were differences in baseline serum creatinine; use of hyper-, hypo-, or iso-osmolar contrast; volume of contrast given; and the proportion of patients with known risk factors for CIN, including: Diabetes Mellitus, congestive heart failure, and concomitant use of CNI, in these studies which make it difficult to conclude the actual incidence of CIN in kidney transplant recipients.
To date, Haider et al[9] (2015) study is considered the largest retrospective study evaluating the incidence of CIN in kidney transplantation. The incidence of CIN in this study was low (5.6%), much lower than reported by Ahuja et al[10] (2000). Two fundamental factors were implicated in this low incidence of CIN in this landmark study first: the relatively elevated baseline eGFR (> 70 mL/min per 1.73 m2) and second: The use of “hypo-osmolar” contrast applied in this procedure[9].
Another possible explanation for the low incidence of CIN in this study is that Diabetes Mellitus and hypertension in these patients may not have damaged the renal allograft to the extent to potentiate CIN. Another important factor is the age of the kidney rather than the age of recipient may affect the susceptibility for CIN. Furthermore, among all procedures utilizing iodine-based contrast, coronary angiography with the percutaneous intervention was responsible for 49% of cases of CIN[13]. However in Haider et al[9] (2015) work, only 4.8% of patients have had cardiac catheterization (none of them had CIN), and this might also have leading to low incidence of CIN-AKI in this group of patients. Their inability to identify association with known risk factors for CIN may be explained by the very small number of patients complicated by CIN events.
On the other hand, Fananapazir et al[14], 2016, declared in the most recent trial that CIN incidence was very low, i.e., 7% and 3% according to an elevation of SCr of > 0.3 and 0.5 respectively, after a low osmolality contrast administration. There was with no need for emergent dialysis or an allograft loss 30 d post-operative[14].
Moreover, Bostock et al[15] in 2016, also demonstrated that CIN following endovascular aortic aneurysm repair (EVAR) in kidney transplant recipients could have deranging sequelae. The Vascular Quality Initiative (VQI) database was interrogated to select all kidney transplant recipients who underwent EVAR between 01/2003 and 12/2014. Their primary outcome was renal dysfunction, defined as AKI (rise in serum creatinine concentration > 0.5 mg/dL above the baseline or new post-operative hemodialysis requirement). Within the EVAR VQI dataset, 40 subjects were kidney transplant recipients (40/17, 213, 0.2%). Renal dysfunction occurred in 5/40 patients in the kidney transplant recipients group in comparison to 779/17173 patients in the non-transplanted group (12.5% vs 4.5%, P < 0.01). Emergency EVAR was indicated in 2 (5%) patients who required hemodialysis after surgery and died later. One-year survival after EVAR was similar in both groups (92.9% vs 93.1%, P = 0.73). Kidney transplant recipients who developed renal dysfunction had significantly lower pre-operative eGFR’s (29.5 vs 54.7, P = 0.007) and a significantly higher iodine/eGFR ratio (0.78 vs 0.39, P = 0.02) despite receiving a similar volume of contrast (70.0 vs 68.8, P = 0.97). Renal impairment was three times more frequent in kidney transplant recipients treated with EVAR, despite the overall survival did not differ between groups. Diminished pre-operative eGFR and a higher iodine/eGFR ratio were associated with post-operative renal dysfunction[15]. Charnow et al[16] 2015, showed an incidence about 13% of CIN in allograft recipients undergoing CT or cardiac catheterization with contrast media. CIN was relatively common in kidney transplant recipients undergoing (CT) or cardiac catheterization with contrast media. Charnow et al[16] (2015) at the University of Cincinnati in Ohio studied 76 contrast exposures (45 CT scans and 31 catheterizations) in 50 kidney transplant recipients (50% male) with a mean age of 53.3 years and means. Cr level of 1.46 mg/dL. The investigators reported CIN - defined as a rise in s. Cr by > 0.3 mg/dL or 25% from baseline within 4 d. after the procedure - in 10 of 76 procedures (13.2%). Results demonstrated: 6 (13.3%) of the 45 CT scans and 4 (12.9%) of the 31 catheterizations resulted in CIN[16].
Abu Jawdeh’s group (2015)[16] also examined the risk factors for CIN. In a multivariate model, exposure to N-acetylcysteine (NAC) and a lower hemoglobin level was significantly associated with an increased risk of CIN, but not with CNI use. They assumed that NAC might have been used in high-risk subjects for CIN, a bias that could explain the increased risk of CIN associated with NAC use. At the last follow-up, CIN did not affect allograft function and survival, according to the investigator[16].
CIN is accompanied by a significant rise in mortality and morbidity; Abu Jawdeh suggested that extrapolation of knowledge about CIN affecting the native kidneys and applying this to allografts might not necessarily reflect the best practice. Allografts are solitary kidneys that exposed to significant hemodynamic alterations and also under the effect of lifelong immuno-suppressive agents. Both these factors might affect susceptibility to contrast-induced renal injury. They also suggested that CIN is potentially modifiable if risk factors are well identified and the proper preventive precautions are performed. The 13.3% incidence of CIN identified in this study is consistent with previous studies looking at native kidneys[16]. Due to the retrospective nature of this study and the small sample size, this study should be interpreted with caution.
Finally, it appears that the strict “definition of CIN” in various studies was not universal. While Charnow et al[16] defined CIN as a rise in s. Cr by > 0.3 mg/dL or 25% rise from baseline within four days of contrast exposure, Bostock et al[15] defined CIN as an AKI with elevation of SCr > 0.5 mg/dL from baseline, or new post-operative hemodialysis (HD) requirement%. Haider et al[9] (2015) defined CIN as either an absolute rise in serum creatinine of ≥ 0.5 mg/dL or a ≥ 25% drop in estimated glomerular filtration rate (eGFR) after contrast administration. On the other hand Fananapazir et al[14] (2016) applied two definitions for CIN in the most recent study, they found CIN in 7% based on a rise of ≥ 0.3 mg/dL and 3% based on a rise of ≥ 0.5 mg/dL. Patients with the more strict definition (≥ 0.5 mg/dL) had a pre-contrast eGFR < 60 mL/min per 1.73 m2.
“Ultrasound with contrast”: Contrast enhanced ultrasound (CEUS) is a promising radiological technique with increased popularity. It has a superiority over the color Doppler ultrasound in evaluation of kidney microvasculature studies. A wide variety of diagnoses can be applied including differentiation of cystic from solid lesion, solid mass assessment, pseudotumor and RAS. Moreover, CEUS can help in elucidating the hemodynamic changes associated with chronic allograft nephropathy (CAN)[17].
US contrasts are gas microbubbles of nearly the same size of RBCs, which enclosed in a protein, lipid or polymer shell[18]. They last intravascular only for few minutes (time of CEUS examination), after that, the gas exhaled through the lungs and the shell metabolized by the liver[19], so renal excretion is not a possibility. As these contrast agents is not excreted through the kidney, allograft integrity cannot be deranged. So, their use in KTRs with impaired renal function is completely safe. Furthermore, CEUS is the sole available technique for dynamic evaluation of kidney perfusion, particularly so, when the use of contrast media is mandatory in CT and MR studies in patients with renal dysfunction. CEUS has a wide safety margin in comparison with other radiological modalities[20,21].
Prevention of CIN-induced AKI in the renal transplant recipient: There are no specific measures dedicated to prevent CIN-induced AKI in the renal allograft, but rather universal recommendations. The optimal recommendations for CIN prevention are still uncertain.
The following precautions are suggested with increased risk of CIN (S. creatinine ≥ 1.5 mg/dL (132 micromols/L) or an eGFR < 60 m$/1.73 m2), especially in diabetics: (1) Avoid volume depletion and NSAID[22,23]; (2) Avoid use of high osmolar agents (1400-1800 mosmol/kg)[24,25]; (3) Try to use US and MRI without gadolinium contrast, or CT scanning without contrast media when possible; (4) Choose iodixanol or nonionic low-osmolar agents, e.g., iopamidol or ioversol rather than iohexol[25]; (5) Apply lower doses of contrast and avoid repetitive, closely spaced studies (< 48 h apart)[12,13,15,16,25]; (6) In an absence of contraindications to volume expansion, start isotonic intravenous fluids before and continued several hours after contrast use. Optimal type and timing are not well documented. “Isotonic bicarbonate” is preferred to isotonic saline as a “volume expander”[23,26-29]. “Isotonic bicarbonate” regimen: A bolus of 3 mL/kg for one hour prior to the procedure, and continued at a rate of 1 mL/kg per hour for “6” h after the procedure[23,26-29]. Suggested regimen for isotonic saline: Isotonic saline (1 mL/kg per hour), starting at least 2-6 h before, and continued for 6-12 h after the procedure. Duration of intravenous fluid should be directly proportional to the degree of renal dysfunction (i.e., longer duration for severe renal impairment); (7) Based upon potential benefit, low toxicity, and cost, Acetylcysteine (AC) can be given: 1200 mg orally twice/day, the day before and the day of the procedure. Intravenous AC is NOT recommended due to lack of evidence of benefit and potential risk of anaphylactoid reactions[30,31]; and (8) Prophylactic use of “mannitol” or other diuretics is NOT recommended[32,33]. Prophylactic HF/HDX after contrast exposure is NOT advised on stage 3 and 4 CKD[34].
Two documented contrast media are already in use for oral imaging procedures: First: Barium sulphate, a commonly used oral contrast agent (for GI studies); Second: Gastrografin, which is a substitute agent for the barium in special situations. Generally, barium, as well as gastrografin, is safe, passing through the gastrointestinal tract easily like food and drink[35].
Barium sulphate is by far the most common contrast material used orally. It can also be utilized rectally. Multiple forms are available, including powder, liquid, paste and tablets. They are generally safe. Only mild unpleasant taste can be observed. If given by enema, abdominal fullness, change in bowel habits and whitish discoloration may be observed for only a few days[36].
A nephrostogram is a radiological tool performed to check the nephrostomy catheter and to rule out any abnormalities in the kidney and ureters, for example, obstructive uropathy. It is performed by disconnecting the catheter from its drainage bag and injecting the iodinated contrast through its lumen, monitored with fluoroscopy and static X-ray imaging. Nephrostogram is a very safe technique with few documented complications. Only mild pain with the possibility of the introduction of infection can occur. Unfortunately, this procedure has no known alternative technique[37].
The risk of CIN affecting renal allograft function is significant especially in diabetics, old age and in volume depleted subjects. This risk can be greatly mitigated through optimizing the hydration status in peri-procedure period, by avoiding nephrotoxic medications, by careful use of safe and widely spaced contrast media with the possible minimal amount of contrast media and possibly by prophylactic peri-procedural administration of isotonic bicarbonate. Some of the questions remain unanswered that require randomized controlled trials involving larger number of renal transplant recipients in order to maximize safety of the renal allograft.
Manuscript source: Invited manuscript
Specialty type: Transplantation
Country of origin: Kuwait
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Hu XP, Sheashaa HA, Tanaka A S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Noce A, Iaria G, Durante O, Sforza D, Canale MP, Di Villahermosa SM, Castagnola V, Tisone G, Di Daniele N. Bilateral native kidney neoplasia detected by ultrasound in functionning renal allograft recipient. Arch Ital Urol Androl. 2012;84:253-255. [PubMed] |
| 2. | Quintela J, Aguirrezabalaga J, Alonso A, Fernandez C, Corbal G, Gomez M. Portal and systemic venous drainage in pancreas and kidney-pancreas transplantation: early surgical complications and outcomes. Transplant Proc. 2009;41:2460-2462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Grotemeyer D, Voiculescu A, Iskandar F, Voshege M, Blondin D, Balzer KM, Rump LC, Sandmann W. Renal cysts in living donor kidney transplantation: long-term follow-up in 25 patients. Transplant Proc. 2009;41:4047-4051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Sinha R, Saad A, Marks SD. Prevalence and complications of chronic kidney disease in paediatric renal transplantation: a K/DOQI perspective. Nephrol Dial Transplant. 2010;25:1313-1320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Smith KM, Windsperger A, Alanee S, Humar A, Kashtan C, Shukla AR. Risk factors and treatment success for ureteral obstruction after pediatric renal transplantation. J Urol. 2010;183:317-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Goyen M, Debatin JF. Gadopentetate dimeglumine-enhanced three-dimensional MR-angiography: dosing, safety, and efficacy. J Magn Reson Imaging. 2004;19:261-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Bansal R, Batuman V, Kaplan AA, Aglieco F. Contrast-Induced Nephropathy. Med Pup, Jan 18. 2016; Available from: http://emedicine.medscape.com/article/246751-overview. |
| 8. | Light JA, Perloff LJ, Etheredge EE, Hill G, Spees EK. Adverse effects of meglumine diatrizoate on renal function in the early post-transplant period. Transplantation. 1975;20:404-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Haider M, Yessayan L, Venkat KK, Goggins M, Patel A, Karthikeyan V. Incidence of contrast-induced nephropathy in kidney transplant recipients. Transplant Proc. 2015;47:379-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Ahuja TS, Niaz N, Agraharkar M. Contrast-induced nephrotoxicity in renal allograft recipients. Clin Nephrol. 2000;54:11-14. [PubMed] |
| 11. | Peters C, Delmonico FL, Cosimi AB, Rubin RH, Tolkoff-Rubin N, Baker G, Russell PS. Risks versus benefits of contrast medium exposure in renal allograft recipients. Surg Gynecol Obstet. 1983;156:467-472. [PubMed] |
| 12. | Moreau JF, Kreis H, Barbanel Cl, Michel JR. [Effects of iodine contrast medias on the function of transplanted kidneys]. Nouv Presse Med. 1975;4:2643-2646. [PubMed] |
| 13. | Nash K, Hafeez A, Hou S. Hospital-acquired renal insufficiency. Am J Kidney Dis. 2002;39:930-936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1317] [Cited by in RCA: 1288] [Article Influence: 53.7] [Reference Citation Analysis (0)] |
| 14. | Fananapazir G, Troppmann C, Corwin MT, Nikpour AM, Naderi S, Lamba R. Incidences of acute kidney injury, dialysis, and graft loss following intravenous administration of low-osmolality iodinated contrast in patients with kidney transplants. Abdom Radiol (NY). 2016;41:2182-2186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Bostock IC, Zarkowsky DS, Hicks CW, Stone DH, Eslami MH, Malas MB, Goodney PP. Outcomes of Endovascular Aortic Aneurysm Repair in Kidney Transplant Recipients: Results From a National Quality Initiative. Am J Transplant. 2016;16:2395-2400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Charnow JA, Jawdeh BGA. Contrast-Induced Nephropathy in Kidney transplantation patients Characterized. USA: Renal & Urology News 2015; . |
| 17. | Schwenger V, Korosoglou G, Hinkel UP, Morath C, Hansen A, Sommerer C, Dikow R, Hardt S, Schmidt J, Kücherer H. Real-time contrast-enhanced sonography of renal transplant recipients predicts chronic allograft nephropathy. Am J Transplant. 2006;6:609-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 77] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 18. | Morin SH, Lim AK, Cobbold JF, Taylor-Robinson SD. Use of second generation contrast-enhanced ultrasound in the assessment of focal liver lesions. World J Gastroenterol. 2007;13:5963-5970. [PubMed] [DOI] [Full Text] |
| 19. | Cosgrove D, Blomley M. Liver tumors: evaluation with contrast-enhanced ultrasound. Abdom Imaging. 2004;29:446-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 39] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Wilson SR, Burns PN. Microbubble-enhanced US in body imaging: what role? Radiology. 2010;257:24-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 334] [Cited by in RCA: 321] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 21. | Piscaglia F, Bolondi L. The safety of Sonovue in abdominal applications: retrospective analysis of 23188 investigations. Ultrasound Med Biol. 2006;32:1369-1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 596] [Cited by in RCA: 541] [Article Influence: 27.1] [Reference Citation Analysis (0)] |
| 22. | Pannu N, Wiebe N, Tonelli M. Prophylaxis strategies for contrast-induced nephropathy. JAMA. 2006;295:2765-2779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 296] [Cited by in RCA: 254] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 23. | Marenzi G, Assanelli E, Campodonico J, Lauri G, Marana I, De Metrio M, Moltrasio M, Grazi M, Rubino M, Veglia F. Contrast volume during primary percutaneous coronary intervention and subsequent contrast-induced nephropathy and mortality. Ann Intern Med. 2009;150:170-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 257] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 24. | Kian K, Wyatt C, Schon D, Packer J, Vassalotti J, Mishler R. Safety of low-dose radiocontrast for interventional AV fistula salvage in stage 4 chronic kidney disease patients. Kidney Int. 2006;69:1444-1449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 25. | Lautin EM, Freeman NJ, Schoenfeld AH, Bakal CW, Haramati N, Friedman AC, Lautin JL, Braha S, Kadish EG. Radiocontrast-associated renal dysfunction: a comparison of lower-osmolality and conventional high-osmolality contrast media. AJR Am J Roentgenol. 1991;157:59-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 80] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 26. | Rudnick MR, Goldfarb S, Wexler L, Ludbrook PA, Murphy MJ, Halpern EF, Hill JA, Winniford M, Cohen MB, VanFossen DB. Nephrotoxicity of ionic and nonionic contrast media in 1196 patients: a randomized trial. The Iohexol Cooperative Study. Kidney Int. 1995;47:254-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 637] [Cited by in RCA: 588] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 27. | Cigarroa RG, Lange RA, Williams RH, Hillis LD. Dosing of contrast material to prevent contrast nephropathy in patients with renal disease. Am J Med. 1989;86:649-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 394] [Cited by in RCA: 361] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 28. | Manske CL, Sprafka JM, Strony JT, Wang Y. Contrast nephropathy in azotemic diabetic patients undergoing coronary angiography. Am J Med. 1990;89:615-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 352] [Cited by in RCA: 320] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 29. | McCullough PA, Wolyn R, Rocher LL, Levin RN, O’Neill WW. Acute renal failure after coronary intervention: incidence, risk factors, and relationship to mortality. Am J Med. 1997;103:368-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1214] [Cited by in RCA: 1185] [Article Influence: 40.9] [Reference Citation Analysis (0)] |
| 30. | Merten GJ, Burgess WP, Gray LV, Holleman JH, Roush TS, Kowalchuk GJ, Bersin RM, Van Moore A, Simonton CA, Rittase RA. Prevention of contrast-induced nephropathy with sodium bicarbonate: a randomized controlled trial. JAMA. 2004;291:2328-2334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 818] [Cited by in RCA: 655] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 31. | Briguori C, Airoldi F, D’Andrea D, Bonizzoni E, Morici N, Focaccio A, Michev I, Montorfano M, Carlino M, Cosgrave J. Renal Insufficiency Following Contrast Media Administration Trial (REMEDIAL): a randomized comparison of 3 preventive strategies. Circulation. 2007;115:1211-1217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 32. | Recio-Mayoral A, Chaparro M, Prado B, Cózar R, Méndez I, Banerjee D, Kaski JC, Cubero J, Cruz JM. The reno-protective effect of hydration with sodium bicarbonate plus N-acetylcysteine in patients undergoing emergency percutaneous coronary intervention: the RENO Study. J Am Coll Cardiol. 2007;49:1283-1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 190] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 33. | Ozcan EE, Guneri S, Akdeniz B, Akyildiz IZ, Senaslan O, Baris N, Aslan O, Badak O. Sodium bicarbonate, N-acetylcysteine, and saline for prevention of radiocontrast-induced nephropathy. A comparison of 3 regimens for protecting contrast-induced nephropathy in patients undergoing coronary procedures. A single-center prospective controlled trial. Am Heart J. 2007;154:539-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 120] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 34. | Hoste EA, De Waele JJ, Gevaert SA, Uchino S, Kellum JA. Sodium bicarbonate for prevention of contrast-induced acute kidney injury: a systematic review and meta-analysis. Nephrol Dial Transplant. 2010;25:747-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 75] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 35. | Information about intravenous and oral contrast used in CT. Available from: http://www.imaginis.com/ct-scan/information-about-intravenous-and-oral-contrast-used-in-ct-1. |
| 36. | Radiologyinfo.org for patients. Available from: http://www.radiologyinfo.org. |
| 37. | Stockport NHS. Available from: http://www.stockport.nhs.uk/. |