Published online Dec 18, 2025. doi: 10.5500/wjt.v15.i4.108372
Revised: May 3, 2025
Accepted: August 20, 2025
Published online: December 18, 2025
Processing time: 221 Days and 13.1 Hours
This manuscript provides a commentary on the article by Zhang et al. Patients with heart and pulmonary failure who do not respond to standard treatment may benefit from extracorporeal membrane oxygenation (ECMO) support. Advanced heart failure and transplant cardiology (AHFTC) teams play an essential role in managing patients in cardiogenic shock. To determine whether ECMO patient management outcomes differ based on whether AHFTC physicians assume a direct or consultative role, a retrospective cohort study of 51 patients placed on veno-venous and veno-arterial (VA) ECMO between January 2015 and February 2023 was conducted. Results demonstrated a significantly higher 30-day post-discharge survival rate in the AHFTC direct involvement cohort compared to the consultative group (67% vs 30%) for all ECMO patients. This survival benefit was primarily attributable to VA ECMO patients (64% vs 20%). Direct involvement of AHFTC teams in patient selection and management may enhance survival in patients requiring VA ECMO for cardiogenic shock; however, further research is necessary to confirm these findings.
Core Tip: Mortality and morbidity remain substantial among critically ill patients receiving extracorporeal membrane oxygenation (ECMO). Evidence shows that advanced heart failure and transplant cardiology specialists improve outcomes by assuming a direct attending role rather than a solely consultative role. This improvement is especially evident in patients receiving veno-arterial ECMO support.
- Citation: Feyissa GD. Outcomes of patients receiving extracorporeal membrane oxygenation: Direct vs consultative advanced heart failure and transplant cardiology physicians’ role. World J Transplant 2025; 15(4): 108372
- URL: https://www.wjgnet.com/2220-3230/full/v15/i4/108372.htm
- DOI: https://dx.doi.org/10.5500/wjt.v15.i4.108372
Patients with heart failure (HF) often experience symptoms such as fatigue, fluid retention, and dyspnea due to impaired cardiac function[1-3]. Following myocardial infarction, HF remains a leading cause of late morbidity and mortality[4]. Globally, HF affects approximately 64 million individuals[5,6]. Advanced HF (AHF) represents the terminal stage of HF, characterized by persistent and severe symptoms despite guideline-directed medical therapy[7]. Patients with AHF are at increased risk of cardiovascular hospitalization and death, and they typically have a reduced quality of life and functional capacity[8,9]. Heart transplantation remains the gold standard treatment for end-stage HF, although it entails significant perioperative risks and long-term complications[10].
Cardiogenic shock (CS), a state of severe circulatory failure, results in peripheral hypoperfusion, tissue hypoxia, and impaired vascular responsiveness, which can lead to irreversible multisystem organ failure[11,12]. Mechanical circulatory support is often necessary to maintain hemodynamics in CS patients. Many individuals with decompensated HF experiencing severe hemodynamic instability require admission to cardiac intensive care units[13]. AHF and transplant cardi
Extracorporeal membrane oxygenation (ECMO) is a valuable intervention for patients with heart and pulmonary failure unresponsive to conventional treatment, serving both as a lifesaving measure and as a bridge to more definitive therapies[14]. Veno-arterial (VA) ECMO, which provides the highest level of hemodynamic support, is especially beneficial for patients with severe CS[15]. The use of ECMO in adults with profound cardiac dysfunction is increasing, predominantly driven by growing adoption of VA ECMO[16-18]. However, the use of VA ECMO in elderly patients remains controversial and is considered a relative contraindication in many centers[18-20]. Previous studies have demonstrated that the presence of structured multidisciplinary ECMO teams improves patient outcomes[21-23]. For instance, Dalia et al[22] reported that hospital survival significantly improves with a dedicated multidisciplinary ECMO team. This manuscript aims to underscore the role of AHFTC teams in optimizing ECMO patient outcomes and to highlight the potential benefits of ECMO support in patients with AHF.
Patients admitted to cardiac intensive care units have shown improved clinical outcomes when managed directly by AHFTC physicians[24]. In a recent study by Zhang et al[25], 51 patients [26 on VA ECMO and 25 on veno-venous (VV) ECMO] were divided into two groups based on the AHFTC team's role: Direct management vs consultative support. Twenty-one patients received direct AHFTC care, and 30 were managed under a consultative model.
VA ECMO indications included post-cardiotomy shock (10 patients), myocarditis (7 patients), and other causes of CS (9 patients). VV ECMO was used primarily for acute respiratory distress syndrome (19 patients). Although mechanical ventilation needs were high in both cohorts (90%–100%), the proportions requiring Swan-Ganz catheterization and temporary mechanical circulatory support were comparable. However, renal replacement therapy was more frequently employed in the consultative cohort (60% vs 24%).
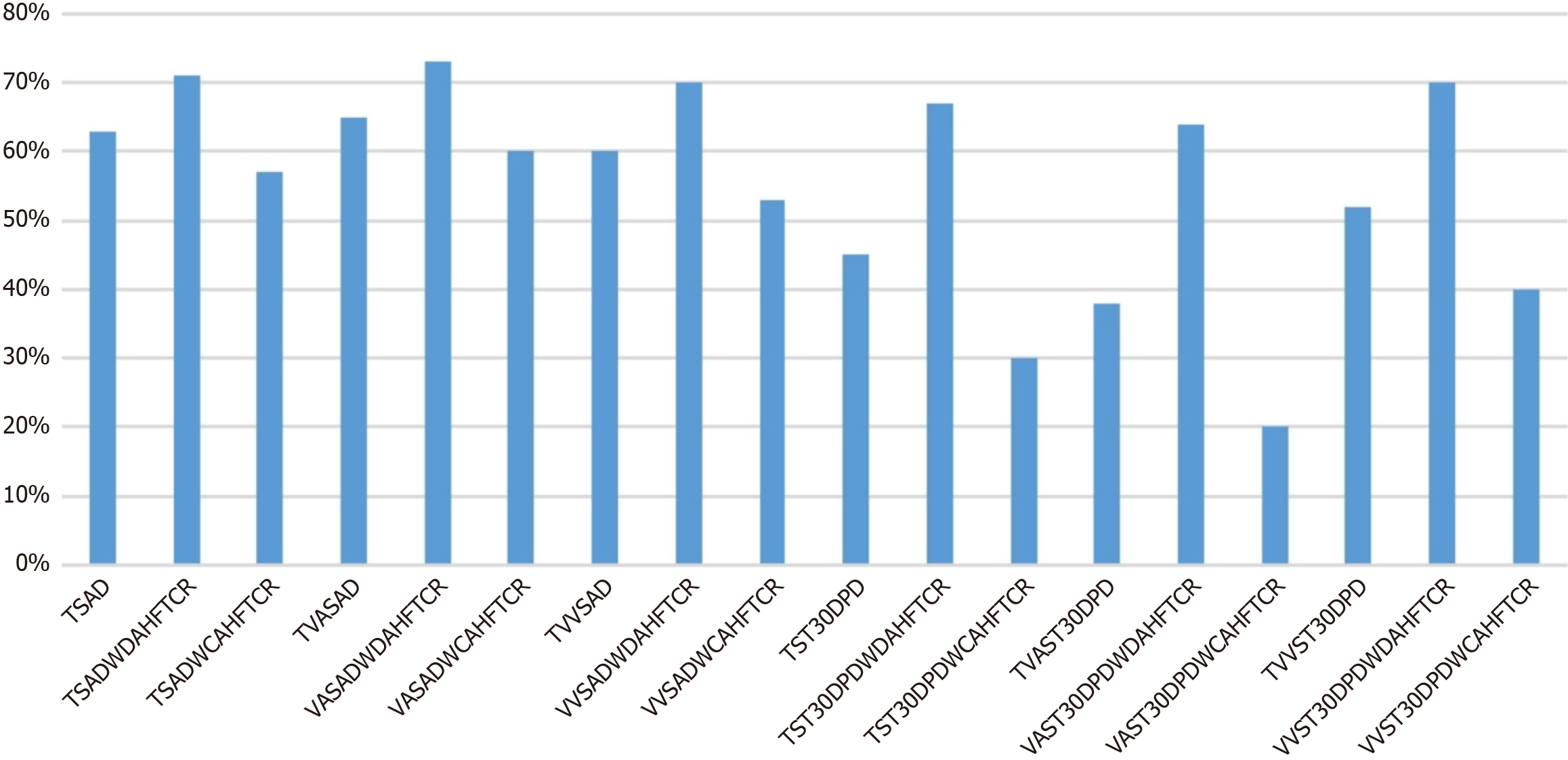
Post-decannulation survival rates favored the AHFTC direct cohort, with combined VA ECMO and VV ECMO survival at 71% vs 57% in the consultative group. Survival among VA ECMO patients was 73% vs 60% post-decannulation, and VV ECMO patients showed 70% vs 53%, respectively, though these differences were not statistically significant.
Most notably, 30-day post-discharge survival was significantly greater in the AHFTC direct cohort for both VA ECMO and VV ECMO patients, especially VA ECMO (64% direct vs 20% consultative). The consultative cohort also experienced a higher incidence of post-ECMO decannulation deaths and stroke, with stroke-associated mortality at nearly 89%. These findings highlight the critical importance of direct AHFTC involvement in stroke prevention, optimal timing of ECMO decannulation, and post-ECMO CS management (Figure 1).
Future multicenter prospective studies are necessary to validate these findings and develop interdisciplinary standardized training for ECMO providers. Healthcare systems should consider early integration of AHFTC physicians into patient management and decision-making processes regarding ECMO candidacy.
VV ECMO is the predominant extracorporeal life support (ECLS) modality for adults with severe refractory respiratory failure. It provides oxygenation without cardiac support by draining deoxygenated blood typically via femoral vein cannulation and reinfusing oxygenated blood through the internal jugular vein. This configuration maintains native cardiac function and offers advantages such as reduced vascular and neurological complications compared to VA ECMO. It is widely utilized as a bridge to lung transplantation[26].
For individuals experiencing refractory CS, VA ECMO may be utilized. It can be used for respiratory failure or haemodynamic support[27]. Cannulation can be done peripherally, typically through femoral arteries, or centrally, draining from the right atrium and reinfused in the aorta. Recent reports have described the use of bicaval venous cannulation to set up a central VA ECMO in patients with pulmonary arterial hypertension and severe cardiomegaly. This allows for lung implantation without experiencing significant haemodynamic effects during cardiac manipulation and provides the best possible cardiac support[26,28].
VA ECMO can be administered centrally or peripherally, but the central setting offers a number of benefits. For example, it guarantees a higher blood flow by utilising a large inflow cannula with a large outflow cannula, preventing problems associated with peripheral ECMO, such as limb ischaemia, blood flow insufficiency, vessel damage, and groin infection. Peripheral ECMO is less invasive, can be put up under local anesthesia, doesn't require a clamshell incision, and can be kept in place after surgery[26]. Comparison between VV ECMO and VA ECMO (Table 1).
| Feature | Veno-arterial ECMO | Veno-venous ECMO |
| Cardiac support | Supports systemic circulation | Does not support systemic circulation |
| Cannulation | Arterial and venous | Venous only |
| Pulmonary circulation | Decreases pulmonary artery pressures | Maintains pulmonary circulation |
| Perfusion rates | Requires lower rates | Requires higher rates |
| Partial pressure of oxygen in arterial blood | Higher achievable | Lower achievable |
| ECMO circuit configuration | Connected in parallel to heart and lungs | Connected in series to heart and lungs |
Patients with CS, including post-cardiotomy CS, acutely decompensated HF with reduced ejection fraction, massive pulmonary thromboembolism, cardiac arrest, refractory ventricular tachycardia, and haemodynamic complications from various invasive procedures can be stabilized with VA ECMO, a bridge-to-recovery therapy that is usually started with cannulation of the common femoral artery and vein[29]. VA ECMO can save individuals with refractory CS. If the patient has entirely or substantially healed from the condition that necessitated the use of ECMO, the device may be effectively withdrawn after a few days of mechanical assistance. Between 31% and 76% of patients with refractory CS are effectively weaned off of ECMO[27].
Even though ECMO has positive outcomes in many diseases, treatment can have a number of side effects that increase morbidity and death[30]. Increased in-hospital mortality, limb ischaemia, haemolysis, sepsis, and hemorrhagic and thrombotic events are among the consequences linked to prolonged VA ECMO therapy[31]. The most frequent vascular problems associated with cannulation are retroperitoneal haemorrhage, pseudoaneurysm, and arterial dissection, which affect 7%–14% of patients. Even with minor vascular injuries, retroperitoneal bleeding can happen when anticoagulation is present; signs of this condition include a declining hemoglobin level, an elevated lactate level, and a decline in haemodynamics. However, the presence of thrombi in the circuit is linked to poor neurological outcomes including stroke[32,33]. ECLS for postcardiotomy CS is linked to a high rate of complications and death[34]. According to a study, iatrogenic vascular injuries and consequences necessitated consultation with vascular surgery for 23.6% of patients[35].
Direct involvement of AHFTC teams in the management of ECMO patients, especially those requiring VA ECMO support, is associated with improved survival, particularly 30 days following hospital discharge. Given the complexities surrounding ECMO management and associated complications, direct AHFTC engagement facilitates optimized patient selection, care coordination, and targeted interventions. Nonetheless, larger prospective studies are needed to confirm these benefits and refine best practice protocols.
| 1. | Umeh CA, Torbela A, Saigal S, Kaur H, Kazourra S, Gupta R, Shah S. Telemonitoring in heart failure patients: Systematic review and meta-analysis of randomized controlled trials. World J Cardiol. 2022;14:640-656. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (4)] |
| 2. | Larsson JE, Kristensen SL, Deis T, Warming PE, Schou M, Køber L, Boesgaard S, Rossing K, Gustafsson F. The relation between socioeconomic status and invasive haemodynamics at evaluation for advanced heart failure. ESC Heart Fail. 2025;12:477-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 3. | Curcio F, Amarelli C, Chiappetti R, Mattucci I, Flocco V, Rammal MI, Abete C, Mazzella F, Maiello C, Abete P, Cacciatore F. MELD score predicts outcomes in patients with advanced heart failure: A longitudinal evaluation. ESC Heart Fail. 2025;12:839-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 4. | Cahill TJ, Kharbanda RK. Heart failure after myocardial infarction in the era of primary percutaneous coronary intervention: Mechanisms, incidence and identification of patients at risk. World J Cardiol. 2017;9:407-415. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 117] [Cited by in RCA: 150] [Article Influence: 16.7] [Reference Citation Analysis (5)] |
| 5. | Stewart GC. Not All Hospitalized Heart Failure Patients Are the Same: A New Worldview. JACC Heart Fail. 2025;13:260-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Miyashita S, Alexandrino FB, Vest AR, Fujisaki T, Tang WHW, Tsukamoto Y, Kinugawa K. Challenges in advanced heart failure care in Japan: Bridging the gap in durable mechanical circulatory support utilization and heart transplantation. JHLT Open. 2025;7:100204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Tepetes NI, Kourek C, Papamichail A, Xanthopoulos A, Kostakou P, Paraskevaidis I, Briasoulis A. Transition to Advanced Heart Failure: From Identification to Improving Prognosis. J Cardiovasc Dev Dis. 2025;12:104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 8. | Blum M, McKendrick K, Gelfman LP, Goldstein NE. Symptom prevalence in patients with advanced heart failure and its association with quality of life and activities of daily living. Qual Life Res. 2025;34:485-493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Lehto HR, Jain N, Manning KA, Lakin JR, Sheu C, Reich AJ, Desai AS, Sciacca KR, Lindvall CJ, Tulsky JA, Bernacki RE. Timing and content of serious illness conversations for patients with advanced heart failure in a specialty-aligned palliative care service. Heart Lung. 2025;69:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 10. | Kourek C, Karatzanos E, Nanas S, Karabinis A, Dimopoulos S. Exercise training in heart transplantation. World J Transplant. 2021;11:466-479. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 28] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 11. | Solangi BA, Shah JA, Kumar R, Batra MK, Ali G, Butt MH, Nisar A, Qamar N, Saghir T, Sial JA. Immediate in-hospital outcomes after percutaneous revascularization of acute myocardial infarction complicated by cardiogenic shock. World J Cardiol. 2023;15:439-447. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 12. | Jentzer JC, Schrage B, Holmes DR, Dabboura S, Anavekar NS, Kirchhof P, Barsness GW, Blankenberg S, Bell MR, Westermann D. Influence of age and shock severity on short-term survival in patients with cardiogenic shock. Eur Heart J Acute Cardiovasc Care. 2021;10:604-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 65] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 13. | Uriel N, Fried J, Yunis A, Clerkin K, Lotan D, Elad B, Kelly N, Raikhelkar J, Burkhoff D, Leon M, Kanwar MK, Sayer GT. The Role of Heart Failure Physicians in the Contemporary Cardiac Intensive Care Unit: Impact on Heart Failure as a Career Choice Among Fellowship Applicants. J Card Fail. 2025;31:1062-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 14. | El-Menyar A, Wahlen BM. Cardiac arrest, stony heart, and cardiopulmonary resuscitation: An updated revisit. World J Cardiol. 2024;16:126-136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (3)] |
| 15. | Takahashi K, Kubo S, Ikuta A, Osakada K, Takamatsu M, Taguchi Y, Ohya M, Shimada T, Miura K, Tada T, Tanaka H, Fuku Y, Kadota K. Incidence, predictors, and clinical outcomes of mechanical circulatory support-related complications in patients with cardiogenic shock. J Cardiol. 2022;79:163-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 16. | Yarmohammadi H, Duval S, Jain R. Abstract 18565: Trends and Outcomes in the Use of Extracorporeal Membrane Oxygenation for Adults in the United States: A 10 year survey. Circulation. 2013;128. [DOI] [Full Text] |
| 17. | Nasr DM, Rabinstein AA. Neurologic Complications of Extracorporeal Membrane Oxygenation. J Clin Neurol. 2015;11:383-389. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 111] [Cited by in RCA: 144] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 18. | Lorusso R, Gelsomino S, Parise O, Mendiratta P, Prodhan P, Rycus P, MacLaren G, Brogan TV, Chen YS, Maessen J, Hou X, Thiagarajan RR. Venoarterial Extracorporeal Membrane Oxygenation for Refractory Cardiogenic Shock in Elderly Patients: Trends in Application and Outcome From the Extracorporeal Life Support Organization (ELSO) Registry. Ann Thorac Surg. 2017;104:62-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 100] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 19. | Cheng R, Hachamovitch R, Kittleson M, Patel J, Arabia F, Moriguchi J, Esmailian F, Azarbal B. Complications of extracorporeal membrane oxygenation for treatment of cardiogenic shock and cardiac arrest: a meta-analysis of 1,866 adult patients. Ann Thorac Surg. 2014;97:610-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 514] [Cited by in RCA: 659] [Article Influence: 54.9] [Reference Citation Analysis (0)] |
| 20. | Loforte A, Marinelli G, Musumeci F, Folesani G, Pilato E, Martin Suarez S, Montalto A, Lilla Della Monica P, Grigioni F, Frascaroli G, Menichetti A, Di Bartolomeo R, Arpesella G. Extracorporeal membrane oxygenation support in refractory cardiogenic shock: treatment strategies and analysis of risk factors. Artif Organs. 2014;38:E129-E141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 71] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 21. | Combes A, Brodie D, Bartlett R, Brochard L, Brower R, Conrad S, De Backer D, Fan E, Ferguson N, Fortenberry J, Fraser J, Gattinoni L, Lynch W, MacLaren G, Mercat A, Mueller T, Ogino M, Peek G, Pellegrino V, Pesenti A, Ranieri M, Slutsky A, Vuylsteke A; International ECMO Network (ECMONet). Position paper for the organization of extracorporeal membrane oxygenation programs for acute respiratory failure in adult patients. Am J Respir Crit Care Med. 2014;190:488-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 362] [Article Influence: 30.2] [Reference Citation Analysis (0)] |
| 22. | Dalia AA, Ortoleva J, Fiedler A, Villavicencio M, Shelton K, Cudemus GD. Extracorporeal Membrane Oxygenation Is a Team Sport: Institutional Survival Benefits of a Formalized ECMO Team. J Cardiothorac Vasc Anesth. 2019;33:902-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 23. | Na SJ, Chung CR, Choi HJ, Cho YH, Sung K, Yang JH, Suh GY, Jeon K. The effect of multidisciplinary extracorporeal membrane oxygenation team on clinical outcomes in patients with severe acute respiratory failure. Ann Intensive Care. 2018;8:31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 24. | Sims DB, Kim Y, Kalininskiy A, Yanamandala M, Josephs J, Rivas-Lasarte M, Ahmed N, Assa A, Jahufar F, Kumar S, Sun E, Rahgozar K, Ali SZ, Zhang M, Patel S, Edwards P, Saeed O, Shin JJ, Murthy S, Patel S, Shah A, Jorde UP. Full-Time Cardiac Intensive Care Unit Staffing by Heart Failure Specialists and its Association with Mortality Rates. J Card Fail. 2022;28:394-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Zhang J, Nagamine T, Vu K, Ali M, Limpruttidham N, Gozun M, Moreno JP, Banerjee D. Comparison of a direct vs consultative advanced heart failure role in the outcomes of extracorporeal membrane oxygenation patients. World J Transplant. 2025;15:102078. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (1)] |
| 26. | Faccioli E, Terzi S, Pangoni A, Lomangino I, Rossi S, Lloret A, Cannone G, Marino C, Catelli C, Dell'Amore A. Extracorporeal membrane oxygenation in lung transplantation: Indications, techniques and results. World J Transplant. 2021;11:290-302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 33] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 27. | Ortuno S, Delmas C, Diehl JL, Bailleul C, Lancelot A, Naili M, Cholley B, Pirracchio R, Aissaoui N. Weaning from veno-arterial extra-corporeal membrane oxygenation: which strategy to use? Ann Cardiothorac Surg. 2019;8:E1-E8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 90] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 28. | Dell'Amore A, Schiavon M, Rea F. Central bicaval cannulation for extracorporeal membrane oxygenation support during double lung transplantation for primary pulmonary artery hypertension. Artif Organs. 2019;43:1112-1113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 29. | Berezin AE. On MANTA vascular closure devices following veno arterial extracorporeal membrane oxygenation: Effectiveness and complications. World J Cardiol. 2025;17:101768. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 30. | Hart JP, Davies MG. Vascular Complications in Extracorporeal Membrane Oxygenation-A Narrative Review. J Clin Med. 2024;13:5170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 31. | Dettling A, Kellner C, Sundermeyer J, Beer BN, Besch L, Bertoldi LF, Blankenberg S, Dauw J, Eckner D, Eitel I, Graf T, Horn P, Jozwiak-Nozdrzykowska J, Kirchhof P, Kluge S, Krais J, von Lewinski D, Linke A, Luedike P, Lüsebrink E, Nordbeck P, Pappalardo F, Pauschinger M, Proudfoot A, Rassaf T, Reichenspurner H, Sag CM, Scherer C, Schulze PC, Schwinger RHG, Skurk C, Sramko M, Tavazzi G, Thiele H, Morici N, Winzer EB, Westermann D, Schrage B, Mangner N. Incidence and predictors of weaning failure from veno-arterial extracorporeal membrane oxygenation therapy in patients with cardiogenic shock. Eur J Heart Fail. 2025;27:832-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 32. | Swedzky F, Barbagelata A, Perrone S, Kaplinsky E, Ducharme A. Emerging concepts in heart failure management and treatment: circulatory support with extracorporeal membrane oxygenation (ECMO). Drugs Context. 2023;12:2022-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 33. | Pillai AK, Bhatti Z, Bosserman AJ, Mathew MC, Vaidehi K, Kalva SP. Management of vascular complications of extra-corporeal membrane oxygenation. Cardiovasc Diagn Ther. 2018;8:372-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 34. | Kienlein RM, Trauzeddel RF, Akbari N, Avalli L, Biancari F, Dini CS, Guenther S, Hagl C, Heringlake M, Kruppa J, Mäkikallio T, Martins R, de Chambrun MP, Rastan AJ, Rubino A, van den Brink F, Nordine M, Treskatsch S. Outcome and complications in postcardiotomy cardiogenic shock treated with extracorporeal life support - a systematic review and meta-analysis. BMC Anesthesiol. 2025;25:29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 35. | Blakeslee-Carter J, Shao C, LaGrone R, Gonzalez-Sigler I, Sutzko DC, Pearce B, Eudailey K, Spangler E, Beck AW, McFarland GE. Vascular complications based on mode of extracorporeal membrane oxygenation. J Vasc Surg. 2022;75:2037-2046.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 26] [Reference Citation Analysis (1)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/