Published online Dec 18, 2025. doi: 10.5500/wjt.v15.i4.102807
Revised: March 10, 2025
Accepted: April 8, 2025
Published online: December 18, 2025
Processing time: 385 Days and 22.5 Hours
Liver transplantation is a vital intervention for patients with end-stage liver disease; however, the Arab world faces significant barriers that hinder access to this life-saving procedure in terms of both practice and research. This narrative review explores the multifaceted challenges, including financial constraints, limited healthcare infrastructure, cultural factors, and the prevalence of infectious diseases. In the Arab countries, both culture and religion were found to play major roles in the acceptability of liver transplantation. High rates of misconceptions and financial strain on patients and healthcare systems necessitate more transplantation programs and improved financial coverage and insurance policies. Enhancing healthcare facilities and improving access to innovative technologies through research is essential for optimizing transplantation outc
Core Tip: Liver transplantation is a vital intervention for patients with end-stage liver disease; however, the Arab world faces significant barriers that hinder access to this life-saving procedure, in relation to the practice and research of liver transplantation. In the Arab countries, both culture and religion have been found to play major roles in the acceptability of liver transplantation. This narrative review explores the multifaceted challenges, including financial constraints, limited healthcare infrastructure, cultural factors, and the prevalence of infectious diseases.
- Citation: Hawwa S, Morad AK, Rifi R, El Masri D, Obeid K, Baroud T, Afyouni A, Tlayss M, Al Chaar S, Masri JE, Salameh P. Barriers to liver transplantation in the Arab world. World J Transplant 2025; 15(4): 102807
- URL: https://www.wjgnet.com/2220-3230/full/v15/i4/102807.htm
- DOI: https://dx.doi.org/10.5500/wjt.v15.i4.102807
Organ transplantation has made significant advancements in recent decades, despite the limited accessibility of organs, which continues to be the main challenge and rate-limiting factor[1]. Currently, organ transplantation is the treatment of choice for several diseases. The most frequently transplanted organs and tissues are the heart, intestine, kidney, liver, lung, pancreas, blood vessels, bone, cartilage, cornea, heart valves, skin, and tendons[2]. According to data on organ donation in 2023, at least 17 individuals waiting for transplants pass away every day, for a total of about 6000 deaths annually[3]. Among organ transplants, the need of livers stands out as a crucial area of focus because of its increasing significance in treating the rising prevalence of liver disorders. The rates of liver transplantation vary among different regions, because of differences in the barriers involved. For example, the socioeconomic, health, and religious aspects that are prevalent in the Middle East have a significant impact on the availability of the transplantation process. These factors, and many others, may have a detrimental impact on the public's attitudes toward transplantation, thus widening the gap between donors and recipients[4].
Liver problems and the need for liver transplantation are rising globally, but the Arab world is considered to be of particular importance due to a higher prevalence of liver diseases that uniquely affect that region[5]. For example, in Egypt alone, an estimated 8-10 million people suffer from viral hepatitis, which makes it a significant threat to the nation's health. Liver disease is a major cause of death in Egypt, and mathematical models predict an increase in the number of cases of liver cancer and liver cirrhosis in the coming decades[6]. Additionally, the Saudi Cancer Registry's most recent data on cancer incidence indicate that liver cancer was the sixth most frequent cancer in Saudi men and the 12th most common cancer in Saudi women in 2015[7].
The demand for liver transplants is rising in parallel with an ongoing increase in liver disorders. However, a variety of specific challenges are limiting this expanding requirement. One of these difficulties is the unusually low organ donor pool, which severely restricts the ability to perform vital liver transplants. Thus, although the need for transplants is increased due to the high incidence of liver disease in the Arab world, there are significant barriers to successfully addressing this critical health issue, including a small pool of potential donors and other regional issues[8].
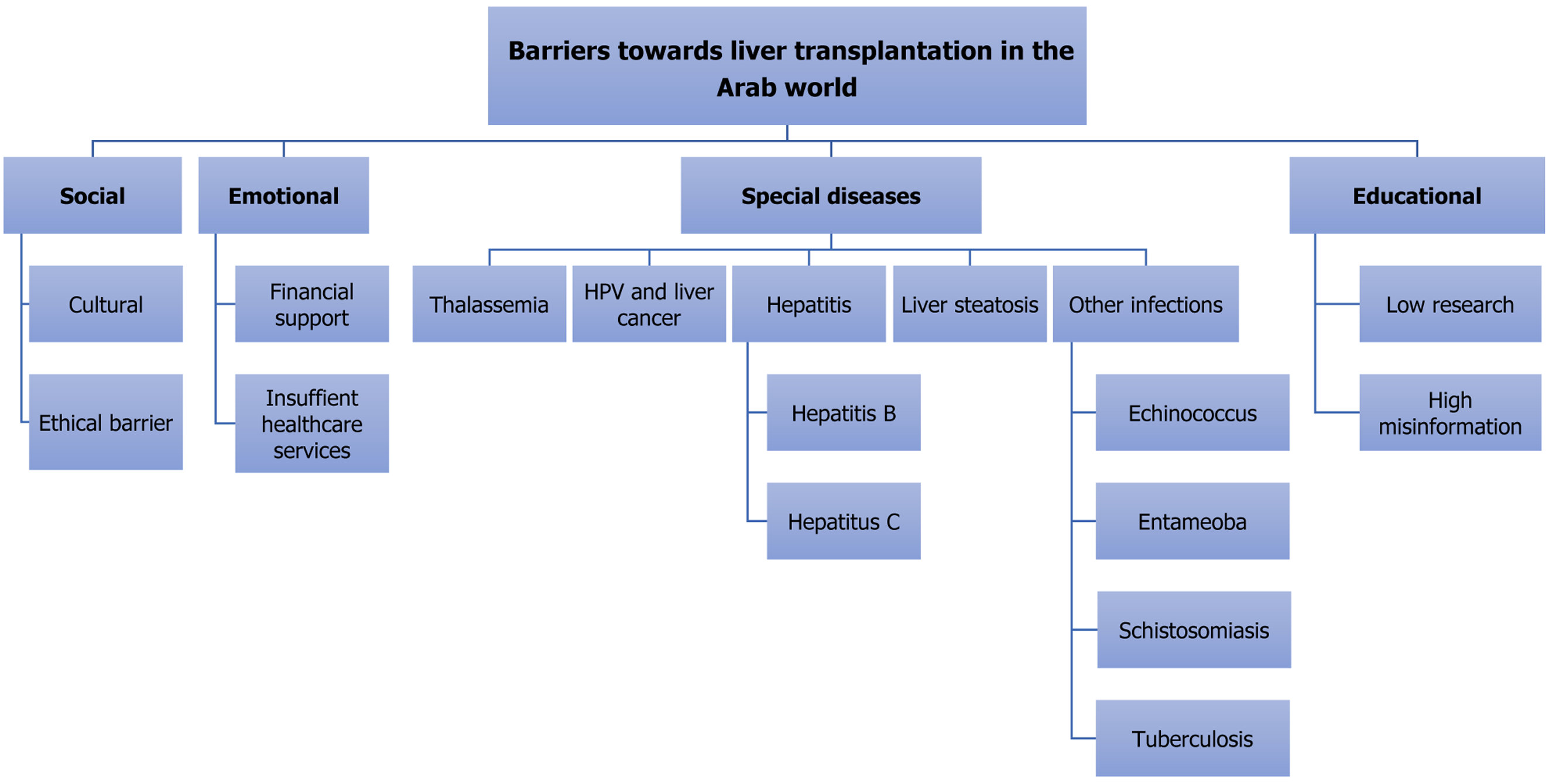
The main factors preventing the growth of the donor pool in the Arab world include religious and cultural considerations, disagreement among religious leaders regarding organ donation, insufficient health infrastructure, low public and medical professional awareness, and a lack of government support[9]. Figure 1 summarizes the barriers to liver transplantation in the Arab world. Addressing these barriers is the first step in overcoming potential obstacles leading to an increase in the rate of liver transplantation and improving the related quality of life. The aim of this review is to examine potential barriers to liver transplantation in the Arab world.
Liver transplantation faces various ethical challenges, particularly in relation to culture and individual beliefs. The two main barriers to organ donation and transplantation are cultural and religious. Regarding culture, some communities believe that the spirit of the donor is transferred to the recipient, and they perform special rituals for this process[10].
A study conducted in Saudi Arabia found that only 19.6% of participants were willing to register as organ or tissue donors. However, 26.6% stated they would consider organ donation after engaging in a discussion with a religious leader and 43.9% indicated they would be more inclined to seriously consider organ donation if approached by a reputable organization[11]. Another study of Saudi Arabian adults reported that when participants were queried about their attitudes and perceptions regarding organ donation, 49.2% expressed agreement, 5.5% were opposed, 11.9% were uncertain, and 33.5% were neutral. In addition, 67.8% of participants stated that they would be willing to donate if supported by law and religion and 3.2% indicated they would not be willing[12]. A cross-sectional study conducted in Palestine found that 55% of participants considered organ donation to be culturally unacceptable. Religious beliefs and concerns of complications were identified as the primary barriers to organ donation[13]. A cross-sectional study in Lebanon showed that only 21.6% of participants were willing to donate, but 59.6% said they were willing if the law and religion favored organ donation[14].
Patients in need and healthcare institutions in the Arab world face serious challenges due to a lack of organ donation programs. The need for liver transplantation in the region is at least 50 per million people, which far exceeds the current capacities of liver transplantation centers[15]. Many nations in the region have logistic, religious, and cultural obstacles that impede the growth and establishment of efficient donation networks. For example, misconceptions and religious concerns are often compounded by a lack of knowledge and education regarding the advantages and procedures of organ donation. Despite approval by the Egyptian parliament in 2010, deceased-donor liver transplantation remains rare in the region[16]. Most transplanted livers in the Middle East are from living donors, even in countries where donation from deceased donors is legal[15]. Moreover, an uncoordinated approach to organ donation results from an inadequate infrastructure and inconsistent policies that prolong patient waiting time and reduce the number of available organs. This deficiency exacerbates the disparity between the availability and demand for organs, leading to avoidable pain and a lower quality of life for patients waiting for transplants.
Poverty continues to be a significant barrier to liver transplantation in the Arab region. It creates a cycle in which inad
Currently, only half of the 22 Arab countries have established liver transplant programs, and 8 of these countries have restricted their services to just one center each[18]. Only a few liver transplants have been carried out in Algeria, Tunisia, and Lebanon[19,20]. Initial transplant initiatives in Libya, Kuwait, and the United Arab Emirates conducted a limited number of procedures before stopping due to logistical and technical challenges. Although Saudi Arabia has the highest success rate in the region, it still meets only 25% of the demand for liver transplants[18].
Many Arab countries face significant challenges that hinder the effectiveness of their healthcare systems, resulting in limited access to advanced medical techniques and procedures[21]. Consequently, the region struggles to implement innovative treatments and technologies that are essential for improving health outcomes, leaving many individuals without the critical medical support that they need. For example, 5 years into the war in Syria, 57% of the country’s public hospitals have sustained damage and 37% are no longer operational[22,23]. Over 15000 of Syria’s approximately 30000 doctors have emigrated and departures are expected to continue[22].
Amid these unfortunate circumstances, the coronavirus disease 2019 (COVID-19) pandemic has jeopardized the economies of several Arab nations, leading to a substantial decline in both demand and supply. For instance, Lebanon is currently experiencing an unprecedented economic crisis that has severely affected various sectors, particularly healthcare[24]. The nationwide lockdown to combat COVID-19 has worsened the economic situation, pushing over 50% of the population below the poverty line and limiting access to essential items and medications[25]. Many skilled healthcare professionals, including American board-certified doctors, have emigrated to countries with more stable conditions, resulting in significant staff shortages, including a 40% decrease in emergency medical personnel at the American University of Beirut Medical Center[26]. In addition, the devastating explosion at Beirut’s port has further strained an already overwhelmed healthcare system, damaging hospitals and critical infrastructure, and leading to a loss of beds and medical supplies. Similarly, the healthcare system in Kuwait was severely impacted by the pandemic, with the number of liver transplants dropping from six in 2019 to none in the first quarter of 2020[27]. Consequently, the number of organ transplants in the Middle East remains critically low, and living-donor transplants are limited to the most critically ill patients who face significant risks if the procedure is delayed[27].
Financial constraints are significant obstacles facing the growth of liver transplant research in the Arab world, primarily related to a lack of funding and budgetary restraints. These restrictions impede the advancement of studies and the development of better transplant methods and patient care guidelines. Compared to international norms, funding for medical research is comparatively scarce in many Arab nations. This lack of funding affects a number of medical research areas, including liver transplantation[28]. Numerous factors, such as low-volume centers still on a learning curve, conflicting national agendas, difficult economic conditions, weak social support, low health literacy[15], and a lack of investment in research infrastructure, contribute to the funding gap. Furthermore, budgetary restrictions on research funding directly impact patient care. The medical community may find it challenging to adopt the latest developments in liver transplantation without ongoing research and development, which could result in a lack of continuous, holistic, and high-quality care. Research is essential for improving surgical procedures, post-transplant care, and understanding the progression of liver disease[29-31]. If these regions receive insufficient funding, liver transplantation programs may be less effective and of lower overall quality. A bibliometric search of PubMed revealed a lack of research activity and trials compared to worldwide productivity. The Arab world was found to contribute only 1% of the published research on liver transplantation (Table 1).
| Country | Liver transplant | Total publications | Percentage of total |
| Algeria | 3 | 9156 | 0.033 |
| Bahrain | 6 | 4413 | 0.136 |
| Comoros | 0 | 102 | 0.000 |
| Djibouti | 0 | 221 | 0.000 |
| Egypt | 335 | 135739 | 0.247 |
| Iraq | 1 | 16960 | 0.006 |
| Jordan | 25 | 29028 | 0.086 |
| Kuwait | 14 | 14114 | 0.099 |
| Lebanon | 36 | 27581 | 0.131 |
| Libya | 2 | 2552 | 0.078 |
| Mauritania | 0 | 284 | 0.000 |
| Morocco | 6 | 19722 | 0.030 |
| Oman | 11 | 11,617 | 0.095 |
| Palestine | 0 | 1061 | 0.000 |
| Qatar | 18 | 22425 | 0.080 |
| Saudi Arabia | 276 | 159663 | 0.173 |
| Somalia | 0 | 773 | 0.000 |
| Sudan | 2 | 8329 | 0.024 |
| Syria | 5 | 3916 | 0.128 |
| Tunisia | 17 | 28113 | 0.060 |
| UAE | 33 | 33408 | 0.099 |
| Yemen | 1 | 3711 | 0.027 |
| Total | 721 | 464641 | 0.155 |
| Worldwide | 71904 | 37612220 | 0.002 |
In the Arab world, the incidence of disorders that adversely impact liver function significantly decreases the number of suitable liver donors and creates major medical barriers. Viral infections, including hepatitis B (HBV) and C (HCV), parasitic infections, and disorders like thalassemia, are common in the region. The issue is further complicated by the growing acknowledgment that human papillomavirus (HPV) may play a role in liver cancer. These medical difficulties aggravate existing challenges that already affect liver transplant programs, such as financial limitations, ethical dilemmas, and religious beliefs. These factors work together to create a complicated environment that makes it challenging to find suitable donors and increase the need for a unique approach to overcome these barriers.
The two most common risk factors for thalassemia are reported to be consanguineous marriage and high-risk marriage in which both partners have genetic abnormalities. This type of marriage was identified by Alsaeed et al[32] as a significant risk factor for the occurrence of thalassemia in Saudi Arabia. Consanguineous marriage is common in most Arab groups, in which 20%-50% of marriages are unions of intrafamilial relatives. In several Arab nations, first-cousin unions, especially the paternal parallel subtype, are exceptionally common and account for over 25% of all marriages[33]. For example, in a study involving 1008 Syrian refugees in Lebanon, 51.9% of the people surveyed were in a consanguineous union, 23.9% were the offspring of consanguineous marriages, and 17.9% were consanguineous for three generations[34]. A study of 7584 participants in Jeddah, Saudi Arabia found that 40.0% had alpha-thalassemia, suggesting that this population was susceptible to hemoglobin defects[35]. Similarly, thalassemia was identified as one of the main public health challenges in Oman[36].
Regular blood transfusions are the mainstay of treatment for thalassemia major. Iron overload is the main adverse effect, and it can lead to serious consequences within a few years and death if left untreated. Iron deposition initially occurs in the liver, where it causes fibrosis and then cirrhosis. For individuals with beta-thalassemia major, hematopoietic stem cell transplantation is the only possible curative option. Successful transplantation, however, does not resolve the excess iron accumulating in the liver[37]. A newly emerging issue that influences prognosis is the combination of iron toxicity and viral infection, which leads to liver cancer[38].
Hepatocellular carcinoma (HCC) is one of the most common cancers to occur in both transfusion-dependent thalassemia (TDT) and non-TDT. Patients with thalassemia are at an elevated risk of developing HCC over time because advancements in chelation therapy for iron overload that prolong survival allow sufficient time for HCC to manifest. The development of hepcidin dysregulation, increased reactive oxygen species, and inflammatory cytokines are the pathways linked to HCC associated with iron overload.
Kupffer cells, the primary macrophages in the liver, phagocytose aged and damaged cells, often accumulating excess iron, especially in thalassemia patients. This iron overload leads to the release of pro-inflammatory cytokines such as interleukin-12 and tumor necrosis factor-alpha. This further leads to a chronic inflammatory environment that increases the risk of cirrhosis and creates an oncogenic environment that favors HCC development in thalassemia patients[39]. The main basis for treating HCC in thalassemia patients is the experience gained from non-thalassemic patients. Those diagnosed in the early stages should ideally undergo local ablation or surgical excision, while liver transplantation is another potentially curative therapy option[39]. However, liver transplantation is severely constrained by the interaction between thalassemia and liver health. The high prevalence of thalassemia in the Arab world complicates efforts to effectively manage liver disease by increasing the demand for liver transplants while decreasing the pool of potential donors.
HPV is highly prevalent in the Arab world due to low vaccination rates and insufficient awareness, and it is a potential threat to liver donation. A unique, previously unestablished relationship between HPV and liver cancer has been described in recent studies. This link may further complicate the landscape of liver transplantation, as potential donors with with HPV may not be eligible. Thus, the high frequency of HPV in the Arab world and its possible connection to liver cancer may exacerbate the region’s already challenging donor availability and further affect the efficiency and accessibility of liver transplant programs. In a study conducted in Lebanon, only 18.4% of participants had received an HPV vaccine, and the majority (77%) had poor awareness of the vaccine. It has been demonstrated that misperceptions regarding HPV vaccination, lack of availability, or restricted access decrease vaccination coverage. Most individuals (71.1%) said that they had not received an HPV vaccine. There were two main reasons for this: 32.2% of the participants cited personal reasons for not getting vaccinated, and 52.3% claimed a lack of vaccine availability or access to the vaccine[40]. The pooled HPV prevalence in cervical cancer patients in the MENA region was 81%. The Maghreb countries had the highest prevalence of HPV found in cervical cancer samples. These findings indicate that HPV is highly prevalent in the Arab world, making this population more prone to developing conditions related to the virus[41].
One of the fundamental biological characteristics of the HPV virus is co-infection of host cells. It is unclear whether co-infection with HBV and HPV has a synergistic impact or if HPV contributes to the development of HCC carcinogenesis[42]. It has been reported that HPV may act as a cofactor alongside HBV in the development of HCC. Replication of both HPV and HBV depends on reverse transcriptase, which facilitates the integration of viral DNA into the host genome. By integrating into a specific gene, these viruses have the potential to contribute to the initiation of carcinogenesis[43].
Subsequently, HPV has emerged as a potential barrier to liver transplantation in the Arab world because of its involvement in the pathogenesis of HCC, either independently or in conjunction with HBV as a cofactor, limiting the donor pool in this region. The challenge is made more difficult by the high incidence of HPV, poor vaccination rates, and a lack of knowledge specific to the Arab world.
While the occurrence of HBV infection in the Arab world is significantly greater than in Western nations, there is a lack of disease awareness and knowledge, a lack of proper screening, and a lack of an established referral system[44,45]. Consequently, patients may be diagnosed at advanced stages and be excluded from transplantation. Studies indicate that the rate of chronic HBV infection in the Eastern Mediterranean region ranges from 2% to 8%[46]. Western countries usually report much lower prevalences, often below 1%[45]. The prevalence of HBV varies widely within the Middle East, from about 0.6% in Iraq to over 8% in Sudan[46]. In contrast, high-income countries with a high Human Development Index, like the Gulf states, report lower rates of HBV. Before the introduction of the HBV vaccine in the early 1990s, prevalence rates were as high as 9.38%. However, after 2010, the HBV infection rate dropped to 1.56%, which indicates a low HBV endemicity[47].
Although HBV is cleared spontaneously in 95% of in infections of immunocompetent adults, patients can have acute symptomatic illness that varies from subclinical or anicteric hepatitis to icteric hepatitis, or rarely fulminant hepatitis. Patients with chronic infections may experience an asymptomatic carrier state, chronic hepatitis, cirrhosis, or HCC[48,49]. The increased prevalence of HBV in the Arab world presents a significant barrier to liver transplantation because its widespread occurrence in the general population limits the pool of potential donors. One of the main criteria for donor evaluation in Egypt is the requirement for negative serological tests for HBV, HCV, and human immunodeficiency virus[16].
In addition, the high prevalence of HBV in the region not only limits the donor pool but also contributes to an increased rate of recurrence after liver transplantation, which can lead to complications such as allograft dysfunction, cirrhosis, and graft failure[50]. As a result of the elevated levels of HBV DNA in transplant recipients in the Arab world compared to other countries, the rate of post-transplantation HBV recurrence is higher, complicating the process and potentially leading to organ failure[51].
The Arab world has a high prevalence of HCV infection, especially in Egypt[52]. However, it lacks proper screening and effective management strategies, which may delay diagnosis and worsen the prognosis[53]. In addition to being a leading reason for liver transplantation in the Arab region, HCV is one of the main limitations to the donor pool[54], as viremic donors may present a 100% transmission risk during the transplantation process[54]. The prevalence of HCV can reach as high as 6.3% in the general population of Qatar[55], 22.1% in the Egyptian army[56], and 7.7% in Morocco[57]. However, these figures may be significantly higher in specific risk groups, such as hemodialysis patients, healthcare workers, and individuals with hemophilia. For example, while HCV infection ranges between 1.1% and 1.7% in the general population of Saudi Arabia[58], it reaches 40% in hemophilia patients, 94.8% in individuals who inject drugs, and as high as 56% in hemodialysis patients[59,60]. To further emphasize the significantly higher occurrence in specific risk-factor groups, the rate of HCV infection may be as high as 70.4% in Egyptian hemodialysis patients[61], 88.6% in Syrian hemofiltration patients, and 60% in injection-drug users[62].
The extremely high prevalence of HCV in Egypt necessitates liver biopsy and imaging studies, including computed tomography angiography, volumetry, and magnetic resonance cholangiopancreatography[63]. If a donor is found to have more than 10% macrovesicular steatosis or any other pathological findings, they will be rejected for liver donation[63]. This adds additional conditions and financial burdens on donors, making the donation process more complicated, and increasing the likelihood that patients may withdraw from consideration. The high rate of HCV not only limits the availability of suitable liver donors but also complicates the overall management and process of liver transplantation. For example, the recurrence of HCV after liver transplant is about 33% in Saudi Arabia[54], which may lead to graft infection and failure, much like the effects of HBV recurrence after liver transplantation[54].
The prevalence of nonalcoholic fatty liver disease (NAFLD) is notably high in the Middle East, estimated at around 32%, making it the highest in the world[64]. However, with the increase in risk factors for NAFLD and nonalcoholic steatohepatitis (NASH), such as obesity, metabolic syndrome, and diabetes mellitus, the prevalence is expected to rise even further[65]. For example, the prevalence of NAFLD in Saudi Arabia is projected to increase by 48% between 2017 and 2030. In the UAE, it is expected to increase by 46% during the same period.
This anticipated increase corresponds to the increase in obesity and type 2 diabetes mellitus in the general population[66]. The occurrence of NASH is projected to increase significantly by 2030, rising by 96% in Saudi Arabia and 87% in the UAE from the 2017 rates of 4.2% and 4.1% of the total population[66]. In Saudi Arabia, the number of cases of decompensated cirrhosis is projected to increase by 273% by 2030, reaching nearly 7000 cases. The UAE is expected to see a 241% rise in similar cases. In addition, the occurrence of HCC related to NAFLD is anticipated to grow significantly, with Saudi Arabia experiencing a 209% increase from 580 cases to 1790 cases and the UAE experiencing a 181% increase from 18 to 51 cases. Furthermore, liver-related deaths are expected to surge by 295% in Saudi Arabia and 270% in the UAE by 2030[66].
The degree of liver steatosis is important when considering its limitation for living-donor transplantation. While livers with mild steatosis (10%-30% of the liver containing fat droplets) can be used for liver transplants due to the shortage of donors, livers with moderate (30%-60%) and severe (> 60%) steatosis, when used, have showed increased risk of primary non-function of the liver post-transplant and higher mortality rate within the first month after the transplant[67,68]. With the projected increase in the rate of nonalcoholic liver disease in the Arab world by 2030, this limitation will become even more prominent and is an increasingly significant barrier to liver transplantation.
Echinococcus granulosus: Echinococcus granulosus is a parasitic tapeworm that causes hydatid cysts, primarily in the liver (55%-70% of cases) and secondarily in the lungs (18%-35%). In approximately 5%-13% of cases, both organs may be affected simultaneously, while the incidence of cysts in unusual sites is about 8%-10%[69,70]. E. granulosus is recognized as the most significant parasitic zoonosis in the Mediterranean region[71,72], maintaining a steady presence in the Middle East owing to the wide variety of intermediate hosts, predominantly sheep and goats, and occasionally camels and cattle[73]. In Lebanon, a recent survey revealed that 62.9% of sheep and 20.9% of goats tested positive for cystic echinococcosis[74]. In Saudi Arabia, 62.9% of slaughtered Najdi sheep were found to have hydatid cysts. E. granulosus has been classified by the World Health Organization as one of seventeen neglected tropical diseases and one of twelve neglected zoonotic diseases[75,76]. It is officially considered endemic in all eastern Mediterranean regions and in north Africa from Morocco to Egypt[72,77]. Furthermore, despite having a more developed economy, Echinococcus remains prevalent in the UAE[78]. Hence, the high prevalence of echinococcosis and its complications, such as hydatid cysts, significantly limits the pool of liver transplant donors and leads to an increased risk of postoperative problems for transplant recipients.
Entamoeba histolytica: Entamoeba histolytica is a protozoan enteropathogen affecting 50 million individuals worldwide[79]. It is ranked as the fourth most common cause of death from parasitic infections globally[80]. Besides being a major cause of protozoal diarrhea and dysentery, E. histolytica is also the most common cause of amebic abscesses[81]. After transmission via the fecal-oral route, the parasite penetrates the intestinal wall and enters the bloodstream, allowing it to travel to the liver. In the liver it can form abscesses containing necrotic liver tissue and inflammatory cells surrounded by a layer of actively invading trophozoites, typically located in the right lobe[82,83]. If left untreated, abscesses can rupture into the peritoneal cavity or pleural space, leading to various complications[84].
E. histolytica is a major public health issue in the Arab world, with prevalence rates differing among various countries. For example, E. histolytica was found to be the most common cause of gastroenteritis in Saudi Arabia, accounting for 20% of cases, which is even higher than the prevalence of rotavirus[85]. In Libya, the occurrence of E. histolytica was reported to vary from 0.8% to 36.6%, with an average of 19.9% between 2000 and 2015[86]. A previous study conducted in Beirut, Lebanon, found that 22.3% of patients with acute gastroenteritis were infected with E. histolytica[87].
Not only does this infection restrict the pool of liver donors due to its much higher prevalence in the Arab region compared to the West, it also increases the risk of liver amebiasis and the risk of infection after liver transplantation. This is exacerbated by poor sanitation and limited access to clean water[88]. Even in more developed nations like Saudi Arabia, the infection remains prevalent[85].
Schistosomiasis: Schistosomiasis, caused by parasites of the genus Schistosoma, can lead to serious liver complications. The parasite is transmitted by direct contact with surface water containing its free-living form, the cercariae, which penetrates the skin. The pathophysiology of schistosomiasis is primarily caused by the eggs, not the worms. Eggs remaining in host tissues cause the infection-related symptoms[89]. As the eggs become lodged in the hepatic portal venules, they trigger inflammation and granuloma formation. Over time, this can progress to hepatic fibrosis and portal hypertension, resulting in significant liver damage 5 years to 15 years after the onset of infection[90].
Schistosomiasis is an ancient parasitic disease that has plagued Egyptians since the time of the pharaohs[89]. Historically, the prevalence of schistosomiasis in Egypt has always been high, with an estimated 7.2 million cases reported in 2012[91]. The same report indicated that Yemen had 2.9 million cases and Algeria had 2.3 million cases[91]. In the White Nile River basin in Sudan, it was reported that one in every two school children tested positive for schistosomiasis[92]. Once again, the high prevalence of this infection in the Arab world creates a significant barrier to the number of potential donors and puts recipients at a disadvantage, particularly in Egypt where it is very common.
Tuberculosis: Most liver transplant recipients are on three immunosuppressants for the first 6 months after trans
While the prevalence of active post-transplant TB is estimated to be around 3%, especially in the first year after surgery, post-transplant TB primarily results from the reactivation of a latent TB infection[95,96]. The risk is significantly higher in TB-endemic areas like Saudi Arabia, with some reports suggesting that solid organ transplant recipients may have a 20 to 74 times greater risk of developing active TB compared with the general population[97,98].
The increased risk of contracting TB after a liver transplant is a significant problem, as it not only heightens the risk of graft failure resulting from the infection but also because of TB-related therapy. The optimal therapies for both active and latent TB can have liver toxicicity and may interact with immunosuppressive agents[93]. Therefore, patients undergoing anti-TB therapy should be closely monitored for potential liver-related side effects and signs of acute rejection[54].
A comprehensive strategy is needed to address the barriers to liver transplantation in the Arab world, particularly regarding financial strain on patients and healthcare systems. Future initiatives should focus on improving financial coverage and access to transplantation procedures. Targeted research on liver disease specific to the region is essential, as is fostering discussion of cultural and religious factors that affect donor and recipient eligibility. Enhancing healthcare facilities and access to technology will also be crucial. Public health initiatives should aim to control prevalent liver diseases, such as hepatitis and ensure high-risk patients receive appropriate therapies before transplantation. Stricter regulations and early screening, especially considering high consanguinity rates, are important for managing inherited blood disorders and infectious diseases. Overall, addressing these complex challenges can lead to a more effective liver transplantation system and improved patient outcomes in the region[50,99].
This literature review has some limitations, mainly those inherent to narrative reviews. Despite the use of MeSH keyword searches, the systematic review methodology was not followed. For instance, the inclusion of narrative reviews is subject to selection bias. Furthermore, no quantitative analyses were performed.
Addressing the barriers to liver transplantation in the Arab world is crucial for improving organ access and patient outcomes. Financial constraints, inadequate healthcare infrastructure, cultural attitudes, and the prevalence of infectious diseases pose significant challenges. To promote a more equitable and effective transplantation system, it is essential to increase financial coverage, improve healthcare facilities, and encourage dialogue around cultural and religious factors affecting eligibility. Additionally, targeted research and public health initiatives aimed at controlling liver diseases will be vital to mitigating infection risk. By taking concerted action to overcome these obstacles, the Arab world can significantly enhance the quality of life for individuals affected by liver disease and ensure that liver transplantation is a viable option for all in need.
| 1. | Carrier AN, Verma A, Mohiuddin M, Pascual M, Muller YD, Longchamp A, Bhati C, Buhler LH, Maluf DG, Meier RPH. Xenotransplantation: A New Era. Front Immunol. 2022;13:900594. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 2. | Muco E, Yarrarapu SNS, Douedi H, Burns B. Tissue and Organ Donation. In: StatPearls. Treasure Island (FL): StatPearls Publishing, 2025. [PubMed] |
| 3. | Ghazi M, Saleh A, Abdallah M, El Masri D, El Masri J, El Ayoubi LM, Hawi J, Jurjus A. Barriers toward xenotransplantation in Arab World. Xenotransplantation. 2024;31:e12852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | El Ayoubi LM, El Masri J, Machaalani M, El Hage S, Salameh P. Contribution of Arab world in transplant research: A PubMed-based bibliometric analysis. Transpl Immunol. 2021;68:101432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Xiao J, Wang F, Wong NK, He J, Zhang R, Sun R, Xu Y, Liu Y, Li W, Koike K, He W, You H, Miao Y, Liu X, Meng M, Gao B, Wang H, Li C. Global liver disease burdens and research trends: Analysis from a Chinese perspective. J Hepatol. 2019;71:212-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 423] [Article Influence: 60.4] [Reference Citation Analysis (1)] |
| 6. | Cheemerla S, Balakrishnan M. Global Epidemiology of Chronic Liver Disease. Clin Liver Dis (Hoboken). 2021;17:365-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 360] [Article Influence: 72.0] [Reference Citation Analysis (1)] |
| 7. | Alqahtani SA, Sanai FM, Alolayan A, Abaalkhail F, Alsuhaibani H, Hassanain M, Alhazzani W, Alsuhaibani A, Algarni A, Forner A, Finn RS, Al-Hamoudi WK. Saudi Association for the Study of Liver diseases and Transplantation practice guidelines on the diagnosis and management of hepatocellular carcinoma. Saudi J Gastroenterol. 2020;26:S1-S40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Alghamdi THT, Alibrahim SRA, Alzahrani SSS, Alhaddad YHA, Alghamdi NKM, Alghamdi RAS. Assessment of the level of willingness to donate liver and kidney among the general population in Saudi Arabia. 2022. Available from: http://www.mejfm.com/January%202023/Organ%20donation.htm. |
| 10. | Molzahn AE, Starzomski R, McDonald M, O'Loughlin C. Aboriginal beliefs about organ donation: some Coast Salish viewpoints. Can J Nurs Res. 2004;36:110-128. [PubMed] |
| 11. | Alobaidi S. Beliefs and Intention to Organ Donation in Saudi Arabia: An Online Cross-Sectional Survey. Healthcare (Basel). 2023;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 12. | Somaili M, Masmali A, Haqawi I, Al-Hulaibi M, AlHabji AA, Salami A, Ageel AA, Sultan Y, Alhazemi A, Moharg F, Almansour O, Ahmed AE. Knowledge and Attitude Toward Organ Donation Among the Adult Population in Jazan, Saudi Arabia. Cureus. 2022;14:e27002. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 13. | Abukhaizaran N, Hashem M, Hroub O, Belkebir S, Demyati K. Knowledge, attitudes, and practices of Palestinian people relating to organ donation in 2016: a cross-sectional study. Lancet. 2018;391 Suppl 2:S45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | El Abed El Rassoul A, Razzak RA, Alwardany A, Moubarak M, Hashim HT. Attitudes to organ donation in Lebanon: A cross-sectional survey. Ethics, Med Public Health. 2023;31:100952. [DOI] [Full Text] |
| 15. | Lankarani KB, Hosseini SAM. The Status of Liver Transplantation in the Middle East. Clin Liver Dis (Hoboken). 2019;14:215-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Amer KE, Marwan I. Living donor liver transplantation in Egypt. Hepatobiliary Surg Nutr. 2016;5:98-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 17. | Peters DH, Garg A, Bloom G, Walker DG, Brieger WR, Rahman MH. Poverty and access to health care in developing countries. Ann N Y Acad Sci. 2008;1136:161-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 639] [Cited by in RCA: 768] [Article Influence: 40.4] [Reference Citation Analysis (0)] |
| 18. | Khalaf H, Marwan I, Al-Sebayel M, El-Meteini M, Hosny A, Abdel-Wahab M, Amer K, El-Shobari M, Kamel R, Al-Qahtani M, Khan I, Bashir A, Hammoudi S, Smadi S, Khalife M, Faraj W, Bentabak K, Khalfallah T, Hassoun A, Bukrah A, Mustafa I. Status of liver transplantation in the Arab world. Transplantation. 2014;97:722-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Faraj W, Deborah Mukherji D, Fakih H, Majzoub N, Khalife M. Liver transplantation in Lebanon: A hard lesson to learn. Ann Transplant. 2010;15:25-29. [PubMed] |
| 20. | Bentabak K, Graba A, Boudjema K, Griène B, Debzi N, Bekkouche N, Yahiatène S, Fellah N, Benmoussa D, Faraoun SA, Bodin JM, Lakehal M, Bendib SE, Boucekkine T. Adult-to-adult living related liver transplantation: preliminary results of the Hepatic Transplantation Group in Algiers. Transplant Proc. 2005;37:2873-2874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Ganesan P, El Cheikh J, Isidori A, Kuo SH, Saleh M, Nair R. Editorial: The management of hematologic malignancies in lower-income countries. Front Oncol. 2023;13:1218718. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Brookings. The war on Syria’s health system. Available from: https://www.brookings.edu/articles/the-war-on-syrias-health-system/. |
| 23. | PHR. Physicians for Human Rights - Syrias Medical Community Under Assault. Available from: https://phr.org/our-work/resources/syrias-medical-community-under-assault/. |
| 24. | Shallal A, Lahoud C, Zervos M, Matar M. Lebanon is losing its front line. J Glob Health. 2021;11:03052. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 53] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 25. | Global History Dialogues. How did the economic crisis affect the healthcare in Lebanon? Glob. Available from: https://globalhistorydialogues.org/projects/how-did-the-economic-crisis-affect-the-healthcare-in-lebanon/. |
| 26. | Fleifel M, Abi Farraj K. The Lebanese Healthcare Crisis: An Infinite Calamity. Cureus. 2022;14:e25367. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 27. | Zidan A, Alabbad S, Ali T, Nizami I, Haberal M, Tokat Y, Kamel R, Said H, Abdelaal A, Elsharkawy M, El Fouly A, Sayed H, Al-Mousawi M, AlGhonaim M, Broering D. Position Statement of Transplant Activity in the Middle East in Era of COVID-19 Pandemic. Transplantation. 2020;104:2205-2207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 28. | Almuhaidib S, Alqahtani R, Alotaibi HF, Saeed A, Alnasrallah S, Alshamsi F, Alqahtani SA, Alhazzani W. Mapping the landscape of medical research in the Arab world countries: A comprehensive bibliometric analysis. Saudi Med J. 2024;45:387-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 29. | FDA. Source Animal, Product, Preclinical, and Clinical Issues Concerning the Use of Xenotransplantation Products in Humans; Guidance for Industry. Available from: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/source-animal-product-preclinical-and-clinical-issues-concerning-use-xenotransplantation-products. |
| 30. | Khan RL, Khraibi AA, Dumée LF, Corridon PR. From waste to wealth: Repurposing slaughterhouse waste for xenotransplantation. Front Bioeng Biotechnol. 2023;11:1091554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 31. | El Masri J, El Ayoubi LM, Zreika B, Adhami F, El Masri D, El Hage S, Abou-Jaoudé M. Current state of clinical trials regarding liver transplant rejection. Transpl Immunol. 2022;70:101522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 32. | Alsaeed ES, Farhat GN, Assiri AM, Memish Z, Ahmed EM, Saeedi MY, Al-Dossary MF, Bashawri H. Distribution of hemoglobinopathy disorders in Saudi Arabia based on data from the premarital screening and genetic counseling program, 2011-2015. J Epidemiol Glob Health. 2018;7 Suppl 1:S41-S47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 33. | Hamamy HA, Al-Allawi NA. Epidemiological profile of common haemoglobinopathies in Arab countries. J Community Genet. 2013;4:147-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 89] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 34. | El Sabeh M, Kassir MF, Ghanem P, Saifi O, El Hadi D, Khalifeh Y, Akkawi AR, Ghabach M, Chaaya M, Nemer G, Abbas O, Kurban M. Consanguinity rates among Syrian refugees in Lebanon: a study on genetic awareness. J Biosoc Sci. 2021;53:356-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 35. | Abu-Shaheen A, Heena H, Nofal A, Abdelmoety DA, Almatary A, Alsheef M, AlFayyad I. Epidemiology of Thalassemia in Gulf Cooperation Council Countries: A Systematic Review. Biomed Res Int. 2020;2020:1509501. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 36. | Hassan SM, Harteveld CL, Bakker E, Giordano PC. Broader spectrum of β-thalassemia mutations in Oman: regional distribution and comparison with neighboring countries. Hemoglobin. 2015;39:107-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 37. | Ghavamzadeh A, Mirzania M, Kamalian N, Sedighi N, Azimi P. Hepatic iron overload and fibrosis in patients with beta thalassemia major after hematopoietic stem cell transplantation: A pilot study. Int J Hematol Oncol Stem Cell Res. 2015;9:55-59. [PubMed] |
| 38. | Dessì C, Leoni G, Moi P, Danjou F, Follesa I, Foschini ML, Morittu M, Zappu A, Defraia E, Bina P, Cunico A, Civolani A, Podda RA, Origa R. Thalassemia major between liver and heart: Where we are now. Blood Cells Mol Dis. 2015;55:82-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 39. | Lin PC, Hsu WY, Lee PY, Hsu SH, Chiou SS. Insights into Hepatocellular Carcinoma in Patients with Thalassemia: From Pathophysiology to Novel Therapies. Int J Mol Sci. 2023;24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 40. | Hourani L, Zaatar M, Hoballah J, Kadi K, Yasmine M, Hijazi H, Estelly N, Mrad J, Jaffa MA. Overview of knowledge, attitudes and barriers associated with HPV vaccination in Beirut, Lebanon. Glob Public Health. 2024;19:2356626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 41. | Obeid DA, Almatrrouk SA, Alfageeh MB, Al-Ahdal MNA, Alhamlan FS. Human papillomavirus epidemiology in populations with normal or abnormal cervical cytology or cervical cancer in the Middle East and North Africa: A systematic review and meta-analysis. J Infect Public Health. 2020;13:1304-1313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 42. | Ma T, Su Z, Chen L, Liu S, Zhu N, Wen L, Yuan Y, Lv L, Chen X, Huang J, Chen H. Human papillomavirus type 18 E6 and E7 genes integrate into human hepatoma derived cell line Hep G2. PLoS One. 2012;7:e37964. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 43. | Sofiani VH, Veisi P, Rukerd MRZ, Ghazi R, Nakhaie M. The complexity of human papilloma virus in cancers: a narrative review. Infect Agent Cancer. 2023;18:13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 44. | Sanai F, Alkhatry M, Alzanbagi A, Kumar S. Hepatitis B virus infection in Saudi Arabia and the UAE: Public health challenges and their remedial measures. J Infect Public Health. 2023;16:1410-1417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 45. | Gasim GI. Hepatitis B virus in the Arab world: where do we stand? Arab J Gastroenterol. 2013;14:35-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 46. | Alghamdi IG, Alghamdi RM, Alghamdi MS, Alghamdi AM, Alghamdi MI, Alghamdi ZI, Alghamdi KS. Epidemiology of Hepatitis B in Saudi Arabia from 2006 to 2021. Hepat Med. 2023;15:233-247. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 47. | Alali AA, Abo-Shehada MN. Prevalence of Hepatitis B Virus infection in the Gulf Cooperation Council: a systematic review and meta-analysis. BMC Infect Dis. 2022;22: 819. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 48. | Tripathi N, Mousa OY. Hepatitis B. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2025. [PubMed] |
| 49. | Fadlallah H, El Masri D, Bahmad HF, Abou-Kheir W, El Masri J. Update on the Complications and Management of Liver Cirrhosis. Med Sci (Basel). 2025;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 50. | Maiwall R, Kumar M. Prevention and Treatment of Recurrent Hepatitis B after Liver Transplantation. J Clin Transl Hepatol. 2016;4:54-65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 51. | Samuel D, Muller R, Alexander G, Fassati L, Ducot B, Benhamou JP, Bismuth H. Liver transplantation in European patients with the hepatitis B surface antigen. N Engl J Med. 1993;329:1842-1847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 837] [Cited by in RCA: 751] [Article Influence: 22.8] [Reference Citation Analysis (1)] |
| 52. | Chaabna K, Cheema S, Abraham A, Alrouh H, Lowenfels AB, Maisonneuve P, Mamtani R. Systematic overview of hepatitis C infection in the Middle East and North Africa. World J Gastroenterol. 2018;24:3038-3054. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 27] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (1)] |
| 53. | Alavian SM, Rezaee-Zavareh MS. The Middle East and hepatitis C virus infection: does it need special attention? Lancet Infect Dis. 2016;16:1006-1007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 54. | Abaalkhail FA, Al Sebayel MI, Shagrani MA, O'Hali WA, Almasri NM, Alalwan AA, Alghamdi MY, Al-Bahili H, AlQahtani MS, Alabbad SI, Al-Hamoudi WK, Alqahtani SA. Clinical Practice Guidelines for Liver Transplantation in Saudi Arabia. Saudi Med J. 2021;42:927-968. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 55. | Lema AM, Cox EA. Hepatitis C antibodies among blood donors in Qatar. Vox Sang. 1992;63:237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 56. | Paez Jimenez A, Sharaf Eldin N, Rimlinger F, El-Daly M, El-Hariri H, El-Hoseiny M, Mohsen A, Mostafa A, Delarocque-Astagneau E, Abdel-Hamid M, Fontanet A, Mohamed MK, Thiers V. HCV iatrogenic and intrafamilial transmission in Greater Cairo, Egypt. Gut. 2010;59:1554-1560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 51] [Article Influence: 3.2] [Reference Citation Analysis (2)] |
| 57. | Benouda A, Boujdiya Z, Ahid S, Abouqal R, Adnaoui M. [Prevalence of hepatitis C virus infection in Morocco and serological tests assessment of detection for the viremia prediction]. Pathol Biol (Paris). 2009;57:368-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 58. | Madani TA. Hepatitis C virus infections reported over 11 years of surveillance in Saudi Arabia. Trans R Soc Trop Med Hyg. 2009;103:132-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 59. | Nemati E, Alavian SM, Taheri S, Moradi M, Pourfarziani V, Einollahi B. Hepatitis C virus infection among patients on hemodialysis: a report from a single center in Iran. Saudi J Kidney Dis Transpl. 2009;20:147-153. [PubMed] |
| 60. | Alzahrani AJ. Analysis of hepatitis C virus core antigenemia in Saudi drug users. Saudi Med J. 2005;26:1645-1646. [PubMed] |
| 61. | Hanafi MI, Mohamed AM, Kassem MS, Shawki M. Needlestick injuries among health care workers of University of Alexandria Hospitals. East Mediterr Health J. 2011;17:26-35. [PubMed] |
| 62. | Othman BM, Monem FS. Prevalence of hepatitis C virus antibodies among intravenous drug abusers and prostitutes in Damascus, Syria. Saudi Med J. 2002;23:393-395. [PubMed] |
| 63. | Amer KE, Marwan I. Living donor liver transplantation in Egypt. Hepatobiliary Surg Nutr. 2016;5 Available from: https://hbsn.amegroups.org/article/view/8190/html. |
| 64. | Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5322] [Cited by in RCA: 7936] [Article Influence: 793.6] [Reference Citation Analysis (8)] |
| 65. | Sayiner M, Koenig A, Henry L, Younossi ZM. Epidemiology of Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis in the United States and the Rest of the World. Clin Liver Dis. 2016;20:205-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 323] [Cited by in RCA: 407] [Article Influence: 40.7] [Reference Citation Analysis (3)] |
| 66. | Alswat K, Aljumah AA, Sanai FM, Abaalkhail F, Alghamdi M, Al Hamoudi WK, Al Khathlan A, Al Quraishi H, Al Rifai A, Al Zaabi M, Babatin MA, Estes C, Hashim A, Razavi H. Nonalcoholic fatty liver disease burden - Saudi Arabia and United Arab Emirates, 2017-2030. Saudi J Gastroenterol. 2018;24:211-219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 96] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 67. | Veteläinen R, van Vliet AK, van Gulik TM. Severe steatosis increases hepatocellular injury and impairs liver regeneration in a rat model of partial hepatectomy. Ann Surg. 2007;245:44-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 126] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 68. | Elsaid MI, Bridges JFP, Mumtaz K, Li N, Sobotka L, Rustgi VK, Paskett ED. The impact of metabolic syndrome severity on racial and ethnic disparities in Metabolic Dysfunction-Associated Steatotic Liver Disease. PLoS One. 2024;19:e0299836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 69. | Sachar S, Goyal S, Goyal S, Sangwan S. Uncommon locations and presentations of hydatid cyst. Ann Med Health Sci Res. 2014;4:447-452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 75] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 70. | McManus DP, Zhang W, Li J, Bartley PB. Echinococcosis. Lancet. 2003;362:1295-1304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 691] [Cited by in RCA: 737] [Article Influence: 32.0] [Reference Citation Analysis (1)] |
| 71. | Dakkak A. Echinococcosis/hydatidosis: a severe threat in Mediterranean countries. Vet Parasitol. 2010;174:2-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 144] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 72. | Borhani M, Fathi S, Lahmar S, Ahmed H, Abdulhameed MF, Fasihi Harandi M. Cystic echinococcosis in the Eastern Mediterranean region: Neglected and prevailing! PLoS Negl Trop Dis. 2020;14:e0008114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 73. | Al Kitani FA, Al Riyami S, Al Yahyai S, Al Rawahi AH, Al Maawali M, Hussain MH. Abattoir based surveillance of cystic echinococcosis (CE) in the Sultanate of Oman during 2010-2013. Vet Parasitol. 2015;211:208-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 74. | Joanny G, Mehmood N, Dessì G, Tamponi C, Nonnis F, Hosri C, Saarma U, Varcasia A, Scala A. Cystic echinococcosis in sheep and goats of Lebanon. Parasitology. 2021;148:871-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 75. | World Health Organization. Working to overcome the global impact of neglected tropical diseases: first WHO report on neglected tropical diseases. Available from: https://www.who.int/publications/i/item/9789241564090. |
| 76. | World Health Organization. The control of neglected zoonotic diseases: community based interventions for NZDs prevention and control. Available from: https://www.who.int/publications/i/item/9789241502528. |
| 77. | Sadjjadi SM. Present situation of echinococcosis in the Middle East and Arabic North Africa. Parasitol Int. 2006;55 Suppl:S197-S202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 208] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 78. | Rahim F, Qasim NH, Zhumagaliuly A, Dzzhusupov K. Human Cystic Echinococcosis in The Populations of MENA Countries, With A Focus on The United Arab Emirates, From 1990 To 2019: From Genetic Epidemiology of Rare Disease to Systematic Analysis for the Global Burden of Disease Study 2019. [DOI] [Full Text] |
| 79. | WHO/PAHO/UNESCO report. A consultation with experts on amoebiasis. Mexico City, Mexico 28-29 January, 1997. Epidemiol Bull. 1997;18:13-14. [PubMed] |
| 80. | GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459-1544. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4683] [Cited by in RCA: 4356] [Article Influence: 435.6] [Reference Citation Analysis (1)] |
| 81. | Mukhopadhyay M, Saha AK, Sarkar A, Mukherjee S. Amoebic liver abscess: presentation and complications. Indian J Surg. 2010;72:37-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 82. | Tharmaratnam T, Kumanan T, Iskandar MA, D'Urzo K, Gopee-Ramanan P, Loganathan M, Tabobondung T, Tabobondung TA, Sivagurunathan S, Patel M, Tobbia I. Entamoeba histolytica and amoebic liver abscess in northern Sri Lanka: a public health problem. Trop Med Health. 2020;48:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 83. | Dolabella SS, Serrano-Luna J, Navarro-García F, Cerritos R, Ximénez C, Galván-Moroyoqui JM, Silva EF, Tsutsumi V, Shibayama M. Amoebic liver abscess production by Entamoeba dispar. Ann Hepatol. 11: 107-117. [PubMed] |
| 84. | Usuda D, Tsuge S, Sakurai R, Kawai K, Matsubara S, Tanaka R, Suzuki M, Takano H, Shimozawa S, Hotchi Y, Tokunaga S, Osugi I, Katou R, Ito S, Mishima K, Kondo A, Mizuno K, Takami H, Komatsu T, Oba J, Nomura T, Sugita M. Amebic liver abscess by Entamoeba histolytica. World J Clin Cases. 2022;10:13157-13166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 85. | Hegazi MA, Patel TA, El-Deek BS. Prevalence and characters of Entamoeba histolytica infection in Saudi infants and children admitted with diarrhea at 2 main hospitals at South Jeddah: a re-emerging serious infection with unusual presentation. Braz J Infect Dis. 2013;17:32-40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 86. | Ghenghesh KS, Ghanghish K, BenDarif ET, Shembesh K, Franka E. Prevalence of Entamoeba histolytica, Giardia lamblia, and Cryptosporidium spp. in Libya: 2000-2015. Libyan J Med. 2016;11:32088. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 87. | Naous A, Naja Z, Zaatari N, Kamel R, Rajab M. Intestinal amebiasis: a concerning cause of acute gastroenteritis among hospitalized lebanese children. N Am J Med Sci. 2013;5:689-698. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 88. | Abuseir S. A systematic review of frequency and geographic distribution of water-borne parasites in the Middle East and North Africa. World Health Organization. Available from: http://www.emro.who.int/emhj-volume-29-2023/volume-29-issue-2/a-systematic-review-of-frequency-and-geographic-distribution-of-water-borne-parasites-in-the-middle-east-and-north-africa.html. |
| 89. | Shaker Y, Samy N, Ashour E. Hepatobiliary Schistosomiasis. J Clin Transl Hepatol. 2014;2:212-216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 90. | Da Silva LC, Chieffi PP, Carrilho FJ. Schistosomiasis mansoni -- clinical features. Gastroenterol Hepatol. 2005;28:30-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 31] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 91. | Hotez PJ, Savioli L, Fenwick A. Neglected tropical diseases of the Middle East and North Africa: review of their prevalence, distribution, and opportunities for control. PLoS Negl Trop Dis. 2012;6:e1475. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 204] [Cited by in RCA: 238] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 92. | Eassa A, Ismail M, Mahgoub A, El-dib N. Review of parasitic zoonotic infections in Egypt. Kasr Al Ainy Med J. 2018;24:91. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 93. | European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Liver transplantation. J Hepatol. 2016;64:433-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 855] [Cited by in RCA: 747] [Article Influence: 74.7] [Reference Citation Analysis (0)] |
| 94. | Kotton CN, Kumar D, Caliendo AM, Asberg A, Chou S, Danziger-Isakov L, Humar A; Transplantation Society International CMV Consensus Group. Updated international consensus guidelines on the management of cytomegalovirus in solid organ transplantation. Transplantation. 2013;96:333-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 604] [Cited by in RCA: 577] [Article Influence: 44.4] [Reference Citation Analysis (0)] |
| 95. | Abad CLR, Razonable RR. Mycobacterium tuberculosis after solid organ transplantation: A review of more than 2000 cases. Clin Transplant. 2018;32:e13259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 71] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 96. | Torre-Cisneros J, Doblas A, Aguado JM, San Juan R, Blanes M, Montejo M, Cervera C, Len O, Carratala J, Cisneros JM, Bou G, Muñoz P, Ramos A, Gurgui M, Borrell N, Fortún J, Moreno A, Gavalda J; Spanish Network for Research in Infectious Diseases. Tuberculosis after solid organ transplant: incidence, risk factors, and clinical characteristics in the RESITRA (Spanish Network of Infection in Transplantation) cohort. Clin Infect Dis. 2009;48:1657-1665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 191] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 97. | Subramanian AK, Theodoropoulos NM; Infectious Diseases Community of Practice of the American Society of Transplantation. Mycobacterium tuberculosis infections in solid organ transplantation: Guidelines from the infectious diseases community of practice of the American Society of Transplantation. Clin Transplant. 2019;33:e13513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 93] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 98. | Singh N, Paterson DL. Mycobacterium tuberculosis infection in solid organ transplant recipients: impact and implications for management. Clin Infect Dis. 1998;27:1266-1277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 439] [Cited by in RCA: 414] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 99. | HCV Guidance. Recommendations for Testing, Managing, and Treating Hepatitis C. Available from: https://www.hcvguidelines.org/. |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/