Published online Jun 18, 2025. doi: 10.5500/wjt.v15.i2.101986
Revised: October 30, 2024
Accepted: November 20, 2024
Published online: June 18, 2025
Processing time: 140 Days and 10.1 Hours
The coronavirus disease 2019 (COVID-19) pandemic had a profound societal impact in the United States which was associated with a decrease in overall life expectancy and an increase in substance abuse and firearm injury. Our under
To examine the trends of substance abuse and firearm injury fatalities during COVID-19 and a potential correlation with organ transplantation.
Crude rates of population-based deaths among adults (18-75 years) from firearm injury and substance abuse from the period of 2014-2021 were obtained from centers of disease control wide-ranging online data for epidemiologic research database. Crude rates of causes of donor (18-75 years) deaths from 2014-2021 were obtained from the united network for organ sharing database.
Average annual percentage change (AAPC) deaths among the United States population were 16.4% from substance abuse and 3.4% from firearm injury. AAPC in cause of death among organ donors was 10.9% from drug intoxication and 2.1% from firearm injury. There was a significant (P < 0.001) and progressive increase in mortality from both causes during the pandemic (2020-2021) and significant correlation (P < 0.001) between population and donor causes of death. COVID-19 exacerbated trends in substance abuse and firearm mortality with a consequent increase in organ donation from donors who died from these two causes.
Identifying the socioeconomic and regional disparities associated with increase in deaths from substance abuse and firearms can help guide post-pandemic healthcare policies and mitigate their impact on organ transplantation.
Core Tip: Population based deaths from substance abuse and firearm injury increased during the coronavirus disease 2019 (COVID-19) pandemic in the United States. The progressive increase in the crude rate of firearm injury and substance abuse death seen during the early part of COVID-19 pandemic continues to persist, with a higher impact in Black/African American, American Indian or Alaska Natives, and those in United States south central and rural areas. These morality trends correlate with changes in organ donation resulting in rise in donors who died from drug overdose and firearm injury from 2014-2021, with a significant increase seen during the COVID-19 pandemic.
- Citation: Dhand R, Okumura K, Nishida S, Dhand A. Rise in deaths from drug overdose and firearm injury during coronavirus disease 2019 pandemic and its impact on organ transplantation. World J Transplant 2025; 15(2): 101986
- URL: https://www.wjgnet.com/2220-3230/full/v15/i2/101986.htm
- DOI: https://dx.doi.org/10.5500/wjt.v15.i2.101986
Organ transplantation is a potential cure for people with irreversible loss of function for organs including for the kidney, liver, or heart. There has been a steady increase in the number of organ transplantations performed in the United States. In 2022, a total of 42800 organ transplants were performed, marking a 3.7 percent increase compared to 2021 and setting an annual record for number of heart, kidney, and liver transplants in the United States[1].
Intersecting this period of growth in organ transplantation, the coronavirus disease 2019 (COVID-19) pandemic exerted profound societal impact, including on overall population life expectancy. Particularly, this crisis has been associated with an increase in firearm injury and substance misuse, which started early in the pandemic and then persisted or worsened during the pandemic[2,3]. COVID-19 also had severe impact on social factors including the mental health of the general population, which has been linked to the increase in substance abuse and firearm injury mortality during this period[2,3].
During the initial period of the pandemic, an increase in hospitalizations related to substance abuse was observed[4]. Additionally, the death rate from drug overdose rose by 50%[3], with significant variations across geographical regions across the United States. In 2021, the United States observed 106600 deaths related to substance abuse, the highest ever recorded in recent history[3].
The COVID-19 pandemic was also associated with an increase in suicide and homicide caused by firearms. A report released by centers for disease and control (CDC) determined that in the period from 2019 to 2020, firearm homicide rates increased by 34.6% (4.6 to 6.1 per 100000 population)[2], the highest rate recorded since 1994.
Since organ transplants mainly rely on utilizing donated organs from a deceased person, changes in causes of death in society can potentially affect the solid-organ transplantation (SOT) systems across the United States. COVID-19 lockdown procedures and limited in-person interactions led to a significant decline in motor vehicle accidents and violent crimes. Historically, these trauma-induced deaths comprised the majority of organ donors for SOT[5]. In the early stages of the pandemic, uncertainties around COVID-19 led to a temporary shutdown of SOT across the nation. As transplantation carefully resumed in July 2020, an increase in deceased donors related to drug overdose and firearms was noted by transplant centers. A survey of 19 select organ procurement organizations recorded a 35% increase in utilization of organs from donors who had died of drug overdose and a 4.5% decrease in trauma as a cause of death for donors[5]. An analysis of heart transplants reported to the united network for organ sharing (UNOS) database found that the COVID-19 pandemic period (March 2020 to June 2021) observed a 32.7% increase in cardiac allografts from organ donors who died of drug overdose compared to pre-COVID (January 2017 to November 2019)[6].
Therefore, we wanted to examine these mortality trends and then identify their association with potentially modifiable economic, physical, and social risk factors. Identification of such risk factors can help devise local and nationwide strategies aimed at mitigating these disparities and guide strengthening of healthcare policies that not only influence preventable deaths, but also improve the utilization of available organs from such donors.
We obtained the data regarding the underlying cause of death from 2014-2021 which was produced by the National Center for Health Statistics and made available on the CDC wide-ranging online data for epidemiologic research (WONDER) online database (https://wonder.cdc.gov/). These datasets include the number of adults (18-75 years) who died from firearm injury or substance abuse during the study period. Firearm injury was identified through international classification of diseases, tenth revision (ICD-10) codes: Injury intent, injury mechanism and all other leading causes. These categories include firearm deaths from assault, self-harm, and undetermined intent using various guns (including rifle, shotgun, handgun). Substance abuse was identified through ICD-10 codes: Drug/alcohol induced causes. These categories include mental and behavioral disorders, drug poisoning, and certain organ diseases related to substance use (including alcohol, opioids, cannabinoids, tobacco). Gender categories of male and female were recorded. Race-based categories were integrated into the following: Hispanic or Latino, Asian or Pacific Islander (non-Hispanic), American Indian or Alaska Native (non-Hispanic), Black or African American (non-Hispanic), and White (non-Hispanic). County urbanization data (from 2014-2017) provided a static designation (representing the year 2013) for each individual county. United States geographical categories include all 50 states and standard census divisions.
We obtained data on the underlying cause of donor death data for 2014-2021 which was produced by the organ procurement and transplantation (OPTN) network and made available on the UNOS database. Gender categories of male and female were recorded. Race-based categories were the following: White, Black or African American, Hispanic, Asian, and other. Geographical and socioeconomic data on organ donors were not available on the UNOS database.
The statistical analyses were performed using R-Studio using R Version 4.1.1 (R Studio, Boston, MA, United States). Statistical significance was defined as P < 0.001 throughout data analysis and crude rates were calculated per 100000 population. Crude rates for characteristics of the general population were adjusted with integration of selected racial categories.
Average annual percent change (AAPC) was calculated as a measure of the trend in deaths over the study period and was computed as a weighted average of the annual percent change (APCs) from the join-point model, with the weights equal to the length of the APC interval[7]. A join-point regression analysis was conducted in R-studio to calculate the AAPC of crude rates for the general United States population and donors of organs for transplant.
Spearman’s rank-order correlation was used to measure the strength and direction of association between two ranked variables of AAPC in deaths from drug overdose and firearm injury in the United States population and donor causes of death related to these two etiologies[8].
Poisson Regression analysis was used to establish statistically significant differences in the individual demographic and regional categories.
Missing data was originally handled by the data providers from both CDC-WONDER and UNOS. From the available data, any missing or discrepant items were removed to help reduce bias in results from random missing data.
This study was considered exempt by the institutional review board because of secondary use of the de-identified data.
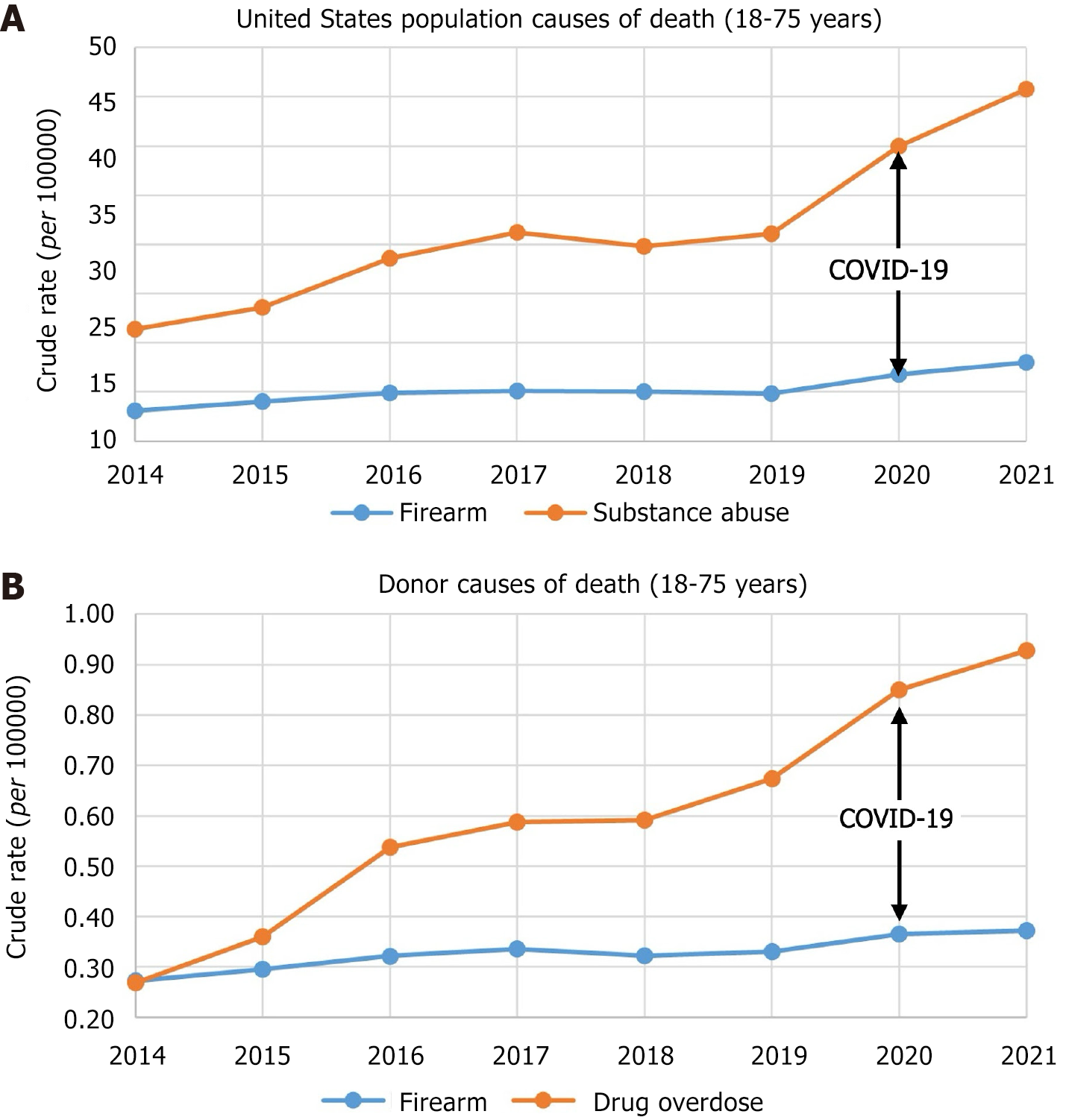
Among the United States population aged 18-75 years, the crude rate of deaths from drug overdose related to substance abuse increased 214% from 2014-2021 with an AAPC in deaths of 16.4%. A statistically significant progressive increase in mortality was noted during the COVID-19 pandemic period of 2020-2021 (Figure 1).
The crude rates of drug overdose death were 2.2 times higher in males (male 66.1 vs females 29.5). There was a statistically significant difference in the race-based crude rates of death per 100000 population from substance abuse, with highest rates among American Indian/Alaska natives (122.0) followed by Whites (54.8), Black or African Americans (46.3), and Hispanic or Latinos (31.6). Highest rates of death were seen in the Mountain region (58.5) including Montana, Idaho, Wyoming, Colorado and Utah and in the New England region (58.4). Medium metro regions had the highest rates of deaths (41.7) compared to predominantly large urban central metro regions (36.6) (Table 1).
| Characteristics | Firearm crude rate (per 100000) | Substance abuse crude rate (per 100000) | P value | |
| Race or ethnicity | Hispanic or Latino | 9.3 | 31.6 | < 0.001 |
| American Indian or Alaska Native (non-Hispanic) | 18.6 | 122.0 | ||
| Asian or Pacific Islander (non-Hispanic) | 3.4 | 8.4 | ||
| Black or African American (non-Hispanic) | 33.4 | 46.3 | ||
| White (non-Hispanic) | 13.9 | 54.8 | ||
| Gender | Female | 4.4 | 29.5 | < 0.001 |
| Male | 25.8 | 66.1 | ||
| Census division | Division 1: New England | 6.7 | 58.4 | < 0.001 |
| Division 2: Middle Atlantic | 8.6 | 46.9 | ||
| Division 3: East north central | 15.6 | 53.3 | ||
| Division 4: West north central | 16.3 | 41.0 | ||
| Division 5: South Atlantic | 17.2 | 48.6 | ||
| Division 6: East south central | 24.5 | 53.6 | ||
| Division 7: West south central | 18.8 | 34.6 | ||
| Division 8: Mountain | 19.2 | 58.5 | ||
| Division 9: Pacific | 10.5 | 43.6 | ||
| 2013 Urbanization | Large central metro | 13.5 | 36.6 | < 0.001 |
| Large fringe metro | 11.2 | 36.7 | ||
| Medium metro | 15.0 | 41.7 | ||
| Small metro | 15.4 | 39.4 | ||
| Micropolitan (nonmetro) | 16.9 | 40.0 | ||
| Noncore (nonmetro) | 19.2 | 37.2 |
During the period of 2014-2021, AAPC in deaths among the United States population from firearms was 3.4%. A statistically significant progressive increase in mortality was noted during the period of 2020-2021 (Figure 1).
There was a statistically significant difference (P < 0.001) in the race-based crude rates of death per 100000 population from firearms, with highest rates among Black or African American (33.4) followed by American Indian/Alaska natives (18.6), Whites (13.9) and Hispanic or Latinos (9.3). Males had significantly higher crude rates of death from firearm injury (25.8) compared to women (4.4). Highest rates of death were seen in the east south-central region including Alabama, Mississippi, Kentucky, and Tennessee (24.5). Noncore (nonmetro) regions which are designated to be most rural based on the 2013 urbanization scheme had the highest rates of deaths (19.2) compared to predominantly urban large fringe metro regions (11.2) (Table 1).
During the period of 2014-2021, AAPC in cause of death among donors of organs for transplant was 10.9% from drug overdose and 2.1% from gunshot wounds (Figure 1). There was a statistically significant progressive increase in mortality from both causes in 2020-2021.
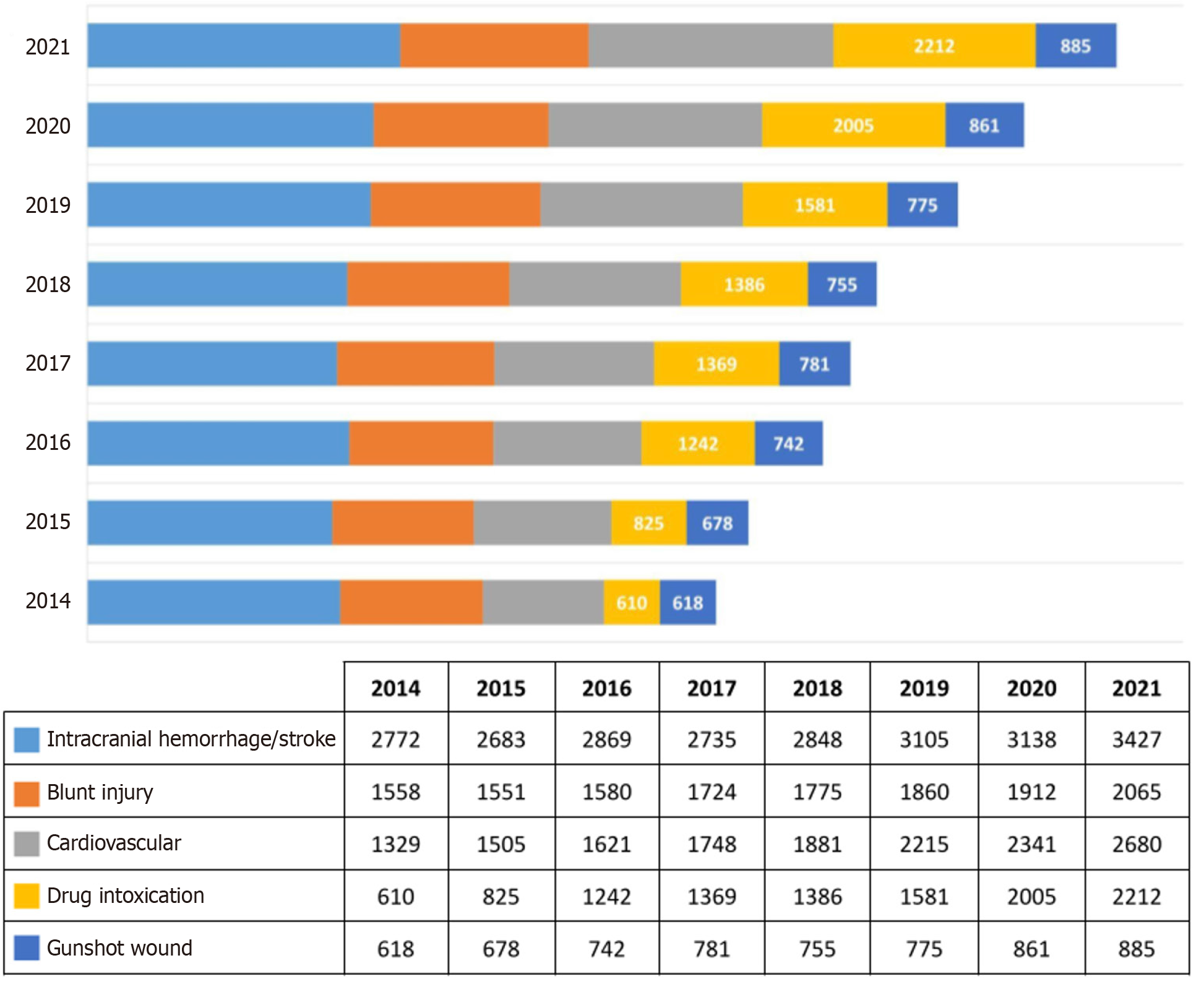
Trends in causes of death among organ donors is summarized in Figure 2. The total number of organ donors in the United States more than doubled from 7755 in 2014 to 12941 in 2021. As a percentage of all causes of donor deaths, drug overdose increased from 7.9% in 2014 to 17.1% in 2021. Drug overdose deaths further increased from 2212 in 2021 to 2423 in 2022. Even though the deaths from gunshot injury increased during the study period from 618 in 2014 to 885 in 2021, they went from being 8.0% of all donations in 2014 to 6.8% in 2021.
Gender and racial disparities in the causes of death among UNOS deceased donors from 2014-2021 are summarized in Table 2. 60.6% of donors were male but comprised a larger majority of all donors who died of firearm injury (83.3%). White persons comprised 66.7% of all organ donors but had a much higher rate of death from drug overdose (79.5%). African American persons comprised 15.2% of all organ donors and had the highest rate of death from firearm injury (25.4%).
| Baseline characteristics | All donors | Drug overdose donors | Firearm injury donors | P value | |||||
| n | % | n | % | n | % | ||||
| Total donors | 79790 | 11230 | 14.1 | 6095 | 7.6 | ||||
| Gender | Male | 48391 | 60.6 | 6787 | 60.4 | 5077 | 83.3 | < 0.001 | |
| Race | White | 53224 | 66.7 | 8929 | 79.5 | 3530 | 57.9 | < 0.001 | |
| African American | 12099 | 15.2 | 987 | 8.8 | 1550 | 25.4 | |||
| Hispanic | 11476 | 14.4 | 1108 | 9.9 | 879 | 14.4 | |||
| Asian | 2027 | 2.5 | 100 | 0.9 | 57 | 0.9 | |||
| Others | 964 | 1.2 | 106 | 0.9 | 79 | 1.3 | |||
There was a significant positive correlation (P < 0.001) between deaths related to firearm and substance use among the general United States population and organ donors from 2014-2021.
Our study shows that the impact of COVID-19 on worsening trends in death among the United States population from both substance abuse and firearm arm injury has persisted beyond the initial increase noted early in the pandemic (2019-2020). These trends have noticeable differences based on gender, race and geographic regions, highlighting the disparities in care and exposing the weakness in resiliency of the societal social support structures when exposed to unforeseen public health disasters. The change in deaths in the United States population also impacted the donor organ availability and utilization for transplantation, along with unique potential risk factors associated with deaths from drug overdose and firearm injury.
The geographic areas with higher mortality from substance abuse run concurrently with states of high percentage population in poverty, increased income inequality (Gini index), and higher uninsured populations (Figure 3).
Over 75% of the nearly 107000 drug overdose deaths in 2021 involved an opioid, with deaths from synthetic opioid, including fentanyl induced death rates, increasing by over 22%[9]. During the early part of COVID-19 pandemic, drug overdose deaths increased more than 20% in 25 states and the district of Columbia, 10% to 19% in 11 states and New York City, and 0% to 9% in 10 states[10]. The increase in substance abuse fatalities during COVID-19 pandemic can partially be attributed to its impact on mental health within the United States population. This impact was likely multifactorial, including increased stress from the closure of educational institutions, loss of family members, transition to remote work, financial instability, job loss, and increase in social isolation leading to loneliness[3]. A survey conducted in June 2020 found that 13% of adults reported new or increased substance misuse to cope with pandemic-related stress[11]. Further, in a population-based survey in January 2021, 41% of adults reported symptoms of anxiety or depression[3]. These trends were likely exacerbated by limitations in access to various outpatient facilities including substance abuse counseling and therapy during the COVID-19 pandemic. This risk was noted to be higher in young adults and Black adults, exposing worsening of pre-existent inequitable access to mental health care during the pandemic[3]. Significant increase in drug overdose deaths is likely from a combination of additional factors, including higher potency of semi-synthetic opioids with increased risk of overdose, decreased access to risk mitigation strategies like outpatient counseling, rehabilitation centers, and mental health clinics, and divergence of public health personnel and resources from drug management of opioid overdose to COVID-19 efforts.
Of all homicide deaths, 73% are associated with firearms, with the highest rates seen in young Black males aged 10-24 years[12], whose firearm homicide death rate was 21.6 times higher than White males of the same age in 2020[2]. In 2021, Black or African American populations had the highest firearm injury crude rate, which was more than double that of Hispanic and Asian or Pacific Islander populations. American Indians and Alaskan Natives observed the second highest rate of firearm injury, which was likely associated with the historically higher rates of suicides among this population. Males died at 6 times the rate compared to females from firearms, which is consistent with the long-standing gender disparity observed in firearm homicide and suicide rates. In 2020, age-adjusted suicide by firearm rate was lowest in states with the most gun laws (4.9 per 100000) and highest in states with the fewest gun laws (10.8 per 100000)[13]. The states that ranked lower with gun provisions (< 11) including Alabama, Missouri, Wyoming, and Arkansas, continued to exhibit relatively high firearm injury rates in 2021 shown in Figure 3. In 2022, 30 million American children lived in a household with a firearm, which has increased from 7 million in 2015. From 2016 to 2021, boys and young men repre
Deaths from firearm injury are related to suicide (60%), homicide (36%) and mass shootings (< 0.2%). United States gun ownership is on the rise with gun sales being 22 million in 2020, which is a 64% increase from the previous year. The first quarter of 2021 observed a 21% increase in firearm sales compared to the first quarter in 2020[12]. During the early part of the pandemic, rates of suicide by firearms remained high, with notable increase among American Indian or Alaska Native populations (7.7 to 10.9 per 100000 population). It was also seen that counties with the highest poverty level had firearm homicide 4.5 times as high and firearm suicide rates 1.3 times as high compared to the lowest poverty level counties[2]. During the COVID-19 pandemic, a surge in gun ownership was noted[15,16], which arose concerns about an incoming wave of suicide deaths. Subsequent studies revealed that people who purchased or intended to purchase a firearm during the pandemic had higher rates of mental health problems and suicidal ideation than non-gun owners and pre-pandemic owners[17,18].
One cumulative marker of determinants of health and related outcomes is the community resilience estimate (CRE). CRE derives data regarding individual and household characteristics from the American community survey, decennial census, and planning database. Compiling several risk factors, the CRE can help track how at-risk every single neighborhood in the United States is to the impacts of natural disasters including the COVID-19 pandemic by estimating the capacity of individuals and households at absorbing, enduring, and recovering from the external impacts of a disaster. It was noted that crude rates of death from firearm injury and substance abuse were higher in states where the percentage population with > 3 risk factors is higher (Figure 3). States with highest percentage population with more than 3 risk factors were Mississippi (28.48%), New York (25.99%), New Mexico (25.81%), Louisiana (25.6%), Alabama (25.36%) compared to overall United States (21.1%). This reflects the cumulative impact of various heterogeneous social and economic factors that may impact widening of long-standing disparities in causes of death by limiting access to healthcare services and physician supply, both of which likely declined during the COVID-19 pandemic.
Compared to 2020, poverty levels in 2021 increased among percentage of American Indians and Alaskan Natives (24.3 vs 20), Asians (9.3 vs 8.1), persons with more than one race (14.2 vs 13.1), Western region of United States (11 vs 10.6), age > 65 years (10.3 vs 8.9), people residing outside principal cities (9.2 vs 9.1) or outside metropolitan areas (15 vs 14.1) and in persons with either no high school diploma (27.2 vs 24.7) or some college education (9.2 vs 8.4)[19]. Changes in poverty level align with greater firearm injury and substance abuse death rates among minority groups and United States south central and noncore (nonmetro) regions and during the COVID-19 pandemic (Figure 3).
Record rates of ongoing United States population-based deaths from substance abuse and firearms significantly correlated with a concurrent increase in organ donation from deceased donors of these two etiologies from 2014-2021. Donors with firearm injury increased 142% from 618 in 2014 to 885 in 2021. Donors with drug overdose increased 362% from 610 in 2014 to 2212 in 2021, and further increased to 2423 in 2022. While these donors increase the overall donor pool and provide life-saving procedures for various patients with end-organ disease, this progressive loss of life during the current opioid epidemic poses an immense public health challenge.
Donors with drug overdose carry unique risk factors that can impact the short-term and long-term outcomes of the graft function. Because of shared risk factors, these donors are considered to be increased infectious risk donors by the United States public health service due to association with hepatitis C (HCV), hepatitis B, human immunodeficiency virus, blood stream infection, infective endocarditis, and/or tuberculosis[20]. Improvement in the screening processes for detection of latent infections and availability of directly acting antiviral therapy for HCV has contributed to a decrease in discard rate of organs from these donors. In a scientific registry of transplant recipients report from 2000 to 2017, drug overdose donors were more likely to be white (85.1%), aged 21 to 40 years (66.3%), and infected with HCV (18.3%). However, this cohort showed that patient and graft survivals between overdose donors and trauma-death donors were similar[20]. An analysis of heart transplantation outcomes showed that the drug overdose donors compared with all other donors had similar short-term recipient survival rates (85.6% and 83.5%, respectively)[6]. Furthermore, while risk of organ dysfunction from ischemic injury associated with firearm injury exists, availability of interventions like machine perfusion of donor organs prior to transplantation may help with increase in utilization and reduce the organ discard rate from donors of this etiology.
During the period of 2014-2021, males comprised 60.6% of all organ donors and 60.4% of drug overdose donors but comprised 83.3% of firearm death donors. Further, while Black persons comprise 15.2% of all donors, they disproportionately comprise 25.4% of firearm or gunshot wound organ donations. Organ donation hesitancy among minority populations may account for the discrepancy in rates of donation. This also includes how Black or African Americans, while having a high crude rate of substance abuse deaths from 2014-2021, only comprise 8.8% of organ donations from drug overdose. It should be noted that people of color and of lower educational and socioeconomic status are less likely to consent to a request for organ donation or sign a donor card[21].
While certain studies have shown a decline in overall substance abuse cases[3] since the onset of the COVID-19 pandemic, concerns regarding the direct and indirect impact of the health crisis on substance abuse and firearm injury rates are still of major concern to the healthcare system. Historically, the mental health impact of natural disasters including pandemics has outlasted the initial physical impact[3,22]. Even as the United States signals the end of the federal public health emergency, further understanding of the long-term impacts of COVID-19 on societal death trends will help guide future policies and programs.
To develop a resilient society that can withstand the impact of natural disasters, there is an urgent need to further identify modifiable risk factors related to the exposure and outcomes of ongoing and future healthcare challenges. While some risk factors like poverty, education level, and access to health care are well-known, there is a complex interplay between other factors at local and national level that require comprehensive approach and resource allocation to provide a short-term and lasting solution in response to sustained increase in deaths from drug overdose and firearms during the COVID-19 pandemic. Strategies aimed at lowering firearm suicide and homicide rates include education on firearm storage practice and physician counseling with provision of a safety device[23], along with gun control legislation. Policies that enhance economic and household stability such as child care subsidies, tax credits, and housing assistance programs can reduce poverty level and other risk factors that are associated with firearm relate suicides and homicides[2]. Initiatives aimed at mitigating substance abuse are extremely vital in combating disparities among minority populations. Emphasis could be placed on reestablishing the outpatient counseling, rehabilitation centers, and mental health clinics to levels prior to onset of the COVID-19 pandemic and bolstering access for at-risk populations including American Indians or Alaska Natives, the rural population, and young African American males.
Limitations of this study are mainly regarding the information available on the databases chosen to represent the general and donor populations. Firstly, given the study period was 2014-2021, the CDC WONDER database has two separate datasets available for underlying causes of death. The 1999-2020 dataset uses bridged-race categories, and the 2018-2021 dataset uses single-race categories. To integrate the datasets, new race categories were developed and people who were “More than one race” from the years 2018-2021 were removed from the study population. Secondly, selection criteria including census region, states, and 2013 urbanization level were not available on the UNOS database. There is no reliable method to identify the regional or economic background of organ donors as their organs are transported between various transplant agencies across a given state or the nation. Additionally, UNOS only provided 5 racial groups (White, Black, Asian, Hispanic, other), excluding non-Hispanic or American Indian/Alaska Native populations that could be impacted by changes in substance abuse or firearm deaths. Further limitations of this study include retrospective design using UNOS and CDC-WONDER databases which may not capture all relevant details regarding the causes of death. Additionally, the study’s design did not allow for an evaluation of the detailed information on patient deaths or risk of donor derived transmission of various infections and other related complications. Reliability and integrity of the data depends on the data entry and is subject to either missing or wrong entry. Data beyond 2021, which was not available till the submission of the manuscript, will be needed to confirm the study results during the post-pandemic period. Future research could benefit from prospective studies that gather more comprehensive data on these factors.
Our study successfully determined the impact of the COVID-19 pandemic on organ transplantation and correlated it to changes in trends of deaths between general population and organ donors. The progressive increase in the crude rate of firearm injury and substance abuse during the early part of COVID-19 pandemic continues to persist with an observable impact on at-risk populations including Black or African American, American Indian or Alaska Native, and young males. Further, greater rates observed in United States south central and noncore (nonmetro) regions align with several other societal risk factors. These morality trends were correlated with changes in organ donation, as there was a progressively increasing number of donors who died from drug overdose and firearm injury from 2014-2021. It is essential that health professionals and policy makers continue to monitor the United States population substance abuse and firearm injury death rates and utilize new CDC WONDER data for 2022, 2023, and upcoming years. To better model geographical disparities, new urbanization rates for 2023 should be used when released by the United States census bureau. Policy makers at local and national levels can develop targeted interventions and provide adequate resource distribution to prevent high firearm injury and substance abuse deaths, while simultaneously working with transplant centers to devise strategies that will optimize the use of available organs for transplant from deceased donors. Given the persistent and ongoing impact of the COVID-19 pandemic, this investigation spanning 2014-2021 helps to identify the trends in population and societal risks for substance abuse and firearm injury in the United States.
The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy of or interpretation by the OPTN or the United States government.
| 1. | OPTN. Organ transplants again set annual records. [cited 15 November, 2024]. Available from: https://optn.transplant.hrsa.gov/news/2022-organ-transplants-again-set-annual-records-organ-donation-from-deceased-donors-continues-12-year-record-setting-trend/. |
| 2. | Kegler SR, Simon TR, Zwald ML, Chen MS, Mercy JA, Jones CM, Mercado-Crespo MC, Blair JM, Stone DM, Ottley PG, Dills J. Vital Signs: Changes in Firearm Homicide and Suicide Rates - United States, 2019-2020. MMWR Morb Mortal Wkly Rep. 2022;71:656-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 129] [Article Influence: 32.3] [Reference Citation Analysis (0)] |
| 3. | Panchal N, Kamal R, Cox C, Garfield R. The Implications of COVID-19 for Mental Health and Substance Use. Kaiser Family Foundation. [cited 15 November, 2024]. Available from: https://pameladwilson.com/wp-content/uploads/4_5-2021-The-Implications-of-COVID-19-for-Mental-Health-and-Substance-Use-_-KFF-1.pdf. |
| 4. | American Psychological Association. Substance use during the pandemic. [cited 15 November, 2024]. Available from: https://www.apa.org/monitor/2021/03/substance-use-pandemic. |
| 5. | Ahmed O, Brockmeier D, Lee K, Chapman WC, Doyle MBM. Organ donation during the COVID-19 pandemic. Am J Transplant. 2020;20:3081-3088. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 56] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 6. | Phillips KG, James L, Rabadi M, Grossi EA, Smith D, Galloway AC, Moazami N. Impact of the coronavirus disease 2019 pandemic on drug overdoses in the United States and the effect on cardiac transplant volume and survival. J Heart Lung Transplant. 2024;43:471-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 7. | NIH. Average Annual Percent Change (AAPC and Confidence Interval. [cited 15 November, 2024]. Available from: https://surveillance.cancer.gov/help/joinpoint/setting-parameters/method-and-parameters-tab/apc-aapc-tau-confidence-intervals/average-annual-percent-change-aapc. |
| 8. | Akoglu H. User's guide to correlation coefficients. Turk J Emerg Med. 2018;18:91-93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1388] [Cited by in RCA: 2790] [Article Influence: 348.8] [Reference Citation Analysis (0)] |
| 9. | CDC. Understanding the Opioid Overdose Epidemic. [cited 15 November, 2024]. Available from: https://www.cdc.gov/overdose-prevention/about/understanding-the-opioid-overdose-epidemic.html. |
| 10. | Baldwin GT, Seth P, Noonan RK. Continued Increases in Overdose Deaths Related to Synthetic Opioids: Implications for Clinical Practice. JAMA. 2021;325:1151-1152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 52] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 11. | Czeisler MÉ, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, Weaver MD, Robbins R, Facer-Childs ER, Barger LK, Czeisler CA, Howard ME, Rajaratnam SMW. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic - United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1049-1057. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1197] [Cited by in RCA: 1782] [Article Influence: 297.0] [Reference Citation Analysis (0)] |
| 12. | Young LJ, Xiang H. US racial and sex-based disparities in firearm-related death trends from 1981-2020. PLoS One. 2022;17:e0278304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 13. | KFF. Do States with Easier Access to Guns have More Suicide Deaths by Firearm? [cited 15 November, 2024]. Available from: https://www.kff.org/mental-health/issue-brief/do-states-with-easier-access-to-guns-have-more-suicide-deaths-by-firearm/. |
| 14. | Everytown. The Rise of Firearm Suicide among Young Americans. [cited 15 November, 2024]. Available from: https://everytownresearch.org/report/the-rise-of-firearm-suicide-among-young-americans/. |
| 15. | Crifasi CK, Ward JA, McGinty EE, Webster DW, Barry CL. Gun purchasing behaviours during the initial phase of the COVID-19 pandemic, March to mid-July 2020. Int Rev Psychiatry. 2021;33:593-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 16. | Kerner L, Losee JE, Higginbotham GD, Shepperd JA. Interest in purchasing firearms in the United States at the outset of the COVID-19 pandemic. J Threat Assess Manag. 2022;9:52-66. [DOI] [Full Text] |
| 17. | Anestis MD, Bryan CJ. Threat perceptions and the intention to acquire firearms. J Psychiatr Res. 2021;133:113-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 18. | Anestis MD, Bond AE, Daruwala SE, Bandel SL, Bryan CJ. Suicidal Ideation Among Individuals Who Have Purchased Firearms During COVID-19. Am J Prev Med. 2021;60:311-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 19. | NADAC. Current Population Survey: Annual Social and Economic Supplement (ASEC), United States, 2019 (ICPSR 37652). [cited 15 November, 2024]. Available from: https://www2.census.gov/programs-surveys/cps/techdocs/cpsmar21.pdf. |
| 20. | Durand CM, Bowring MG, Thomas AG, Kucirka LM, Massie AB, Cameron A, Desai NM, Sulkowski M, Segev DL. The Drug Overdose Epidemic and Deceased-Donor Transplantation in the United States: A National Registry Study. Ann Intern Med. 2018;168:702-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 166] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 21. | Siminoff LA, Burant CJ, Ibrahim SA. Racial disparities in preferences and perceptions regarding organ donation. J Gen Intern Med. 2006;21:995-1000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 56] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 22. | Galea S, Merchant RM, Lurie N. The Mental Health Consequences of COVID-19 and Physical Distancing: The Need for Prevention and Early Intervention. JAMA Intern Med. 2020;180:817-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1231] [Cited by in RCA: 1280] [Article Influence: 213.3] [Reference Citation Analysis (0)] |
| 23. | Houry DE, Simon TR, Crosby AE. Firearm Homicide and Suicide During the COVID-19 Pandemic: Implications for Clinicians and Health Care Systems. JAMA. 2022;327:1867-1868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 24. | CDC. About Underlying Cause of Death, 2018-2022, Single Race. [cited 15 November, 2024]. Available from: http://wonder.cdc.gov/ucd-icd10-expanded.html. |
| 25. | Census. Poverty in States and Metropolitan Areas: 2022. [cited 15 November, 2024]. Available from: https://www.census.gov/library/publications/2023/acs/acsbr-016.html. |
| 26. | Census. Small Area Health Insurance Estimates (SAHIE). [cited 15 November, 2024]. Available from: https://www.census.gov/data-tools/demo/sahie/#/. |
| 27. | Census. Community Resilience Estimates For Equity. [cited 15 November, 2024]. Available from: https://www.census.gov/library/visualizations/interactive/community-resilience-estimates-for-equity.html. |
| 28. | State Health Compare. Income inequality (Gini Coefficient). [cited 15 November, 2024]. Available from: https://statehealthcompare.shadac.org/map/82/income-inequality-gini-coefficient#a/42/119. |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/