Published online Mar 18, 2025. doi: 10.5500/wjt.v15.i1.99642
Revised: October 17, 2024
Accepted: November 6, 2024
Published online: March 18, 2025
Processing time: 123 Days and 17.4 Hours
Machine learning (ML), a major branch of artificial intelligence, has not only demonstrated the potential to significantly improve numerous sectors of health
To conduct a comprehensive bibliometric analysis of publications on the use of ML in transplantation to understand current research trends and their implications.
On July 18, a thorough search strategy was used with the Web of Science da
Of the 529 articles that were first identified, 427 were deemed relevant for bibliometric analysis. A surge in publications was observed over the last four years, especially after 2018, signifying growing interest in this area. With 209 publications, the United States emerged as the top contributor. Notably, the "Journal of Heart and Lung Transplantation" and the "American Journal of Transplantation" emerged as the leading journals, publishing the highest number of relevant articles. Frequent keyword searches revealed that patient survival, mortality, outcomes, allocation, and risk assessment were significant themes of focus.
The growing body of pertinent publications highlights ML's growing presence in the field of solid organ transplantation. This bibliometric analysis highlights the growing importance of ML in transplant research and highlights its exciting potential to change medical practices and enhance patient outcomes. Encouraging collaboration between significant contributors can potentially fast-track advancements in this interdisciplinary domain.
Core Tip: Machine learning (ML) is transforming solid organ transplantation by improving donor-recipient matching, post-transplant monitoring, and patient care via advanced data analysis and outcome forecasting. This bibliometric analysis of 427 relevant publications shows a significant increase in interest and research, especially since 2018, with the United States leading the way. Key themes include patient survival, mortality, outcomes, allocation, and risk assessment, demonstrating ML's promising ability to transform medical practices and improve patient outcomes in transplantation. Collaboration among key contributors is critical for accelerating progress in this interdisciplinary field.
- Citation: Rawashdeh B, Al-abdallat H, Arpali E, Thomas B, Dunn TB, Cooper M. Machine learning in solid organ transplantation: Charting the evolving landscape. World J Transplant 2025; 15(1): 99642
- URL: https://www.wjgnet.com/2220-3230/full/v15/i1/99642.htm
- DOI: https://dx.doi.org/10.5500/wjt.v15.i1.99642
Machine learning (ML) is a subfield of artificial intelligence (AI) that concentrates on the creation of algorithms that are capable of learning and generating predictions or decisions without explicit programming[1,2]. It enables computers to analyze large volumes of data, identify patterns, and learn from examples to improve performance on certain tasks[3].
ML has found numerous applications in the field of medicine, revolutionizing healthcare practices[1,3]. Medical diagnostics has made use of ML algorithms for the analysis of medical imaging, such as computed tomography and X-ray scans. Diseases have been better identified and categorized as a result of this[4]. ML algorithms have been utilized to predict patient outcomes too[5], such as mortality rates[6], response to the treatment[7], and progression of the diseases[8], based on clinical information and patient data. Additionally, ML has facilitated the development of personalized medicine, enabling tailored treatment plans by considering individual patient variables[9].
In the field of solid organ transplantation, ML has emerged as a valuable tool for improving outcomes of the patients and optimizing allocation of the organs[10]. ML algorithms were utilized to develop models that assess the suitability of potential organ-recipient matching, taking into account various factors such as donor-recipient compatibility, organ quality, and recipient medical characteristics[11-13]. These models help transplant programs make more informed decisions and maximize the chances of successful transplantations[10]. Furthermore, ML has been applied to predict post-transplant complications and outcomes[14,15], such as rejection episodes and graft survival[16].
In this study, we conducted a comprehensive bibliometric analysis of all published articles in the field of the use of ML in solid organ transplantation. By systematically analyzing the vast body of literature, we aimed to gain a deeper understanding of the research trends, key contributors, and the overall impact of ML in this critical area of medicine. Further, by mapping interrelationships and showcasing key works of leading contributors in the field of ML applied to transplantation, we aim to illuminate these connections, paving the way for enhanced collaboration and collective advancements in transplantation research.
On July 18, a systematic search was done using the Web of Science database, a comprehensive database that include high-quality articles. To identify ML articles, topics for the keyword “machine learning” were searched in all fields. Then we used the keywords "kidney transplant*", "liver transplant*", "lung transplant*", "heart transplant" and "pancreas transplant*" with appropriate ‘*’ use to compensate for relevant keywords. The final query was "machine learning" (all fields) and "kidney transplant*" or "liver transplant*" or "lung transplant*" or "heart transplant" or "pancreas transplant*" (all fields).
Importantly, this research focused solely on bibliometric analysis, it did not involve the extraction of patient data and was deemed exempt from obtaining approval from the institutional review board.
We analyzed a variety of bibliometric variables, such as the citations of searched articles, annual publications, top-contributed countries, top-published institutions and authors, journals, keywords, and top-cited articles, after extracting and exporting the data in accordance with the search strategy. We employed VOS viewer software (version 1.6.19) and Microsoft Excel 2016 to generate tables and figures. VOS viewer is a software that has been developed in the Java programming language by Van Eck and Waltman from Leiden University[17]. VOS viewer can calculate how strongly an author, an affiliation, or a country is connected to others via citation references using an indicator called “total link strength". This measure aids in assessing the strength of connections between variables within the network.
In VOS viewer network visualizations, terms are shown as circles/squares, and their sizes are determined by their respective weights, with larger circles indicating higher occurrences. Different clusters of terms are assigned specific colors, facilitating the identification of related groups. Lines connecting the circles represent co-citation relationships, and thicker lines indicate stronger connections between the terms. The distance between the circles roughly signifies the level of relatedness based on co-citation; closer circles suggest a stronger relationship between the terms. The visualization offers a clear representation of the relationships, significance and weight (size), and associations (proximity and links) among the terms in the network map.
The preliminary inquiry yielded a total of 529 articles. Following a meticulous manual review process to eliminate irrelevant articles, a subset of 427 articles deemed pertinent were selected for inclusion in the bibliometric analysis. These selected articles collectively garnered 3979 citations, averaging approximately 9.32 citations per article.
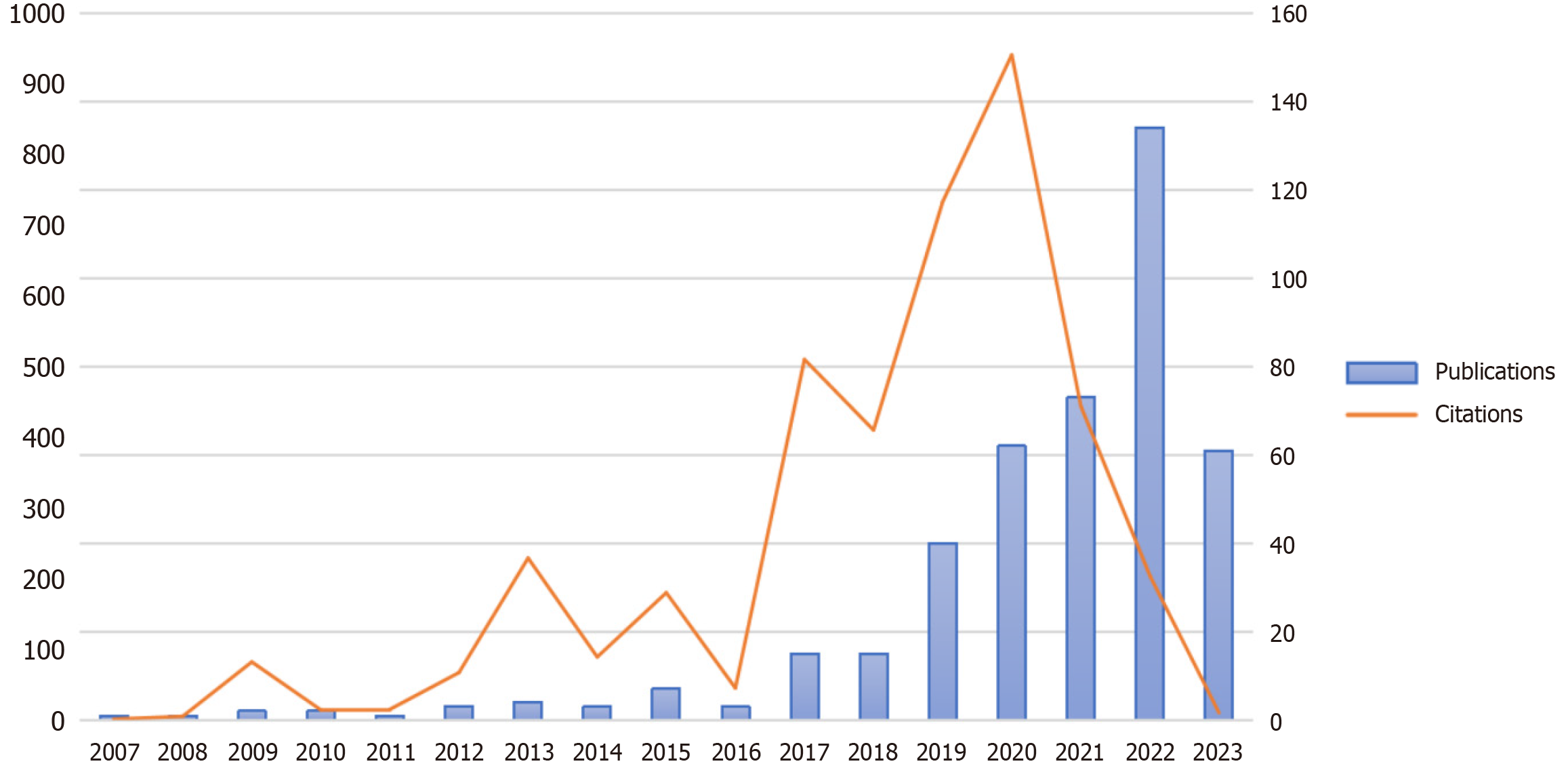
The number of publications discussing ML in transplantation has shown a remarkable trend over the last four years. From 2007 to 2016, the annual publication count was limited to 1 to 7 publications. However, in 2017, there was a notable increase with 15 publications, and this trend continued to grow each year. By 2022, the number of publications reached a peak with 134 publications, indicating the growing interest and potential impact of ML in transplantation research and patient care (Figure 1).
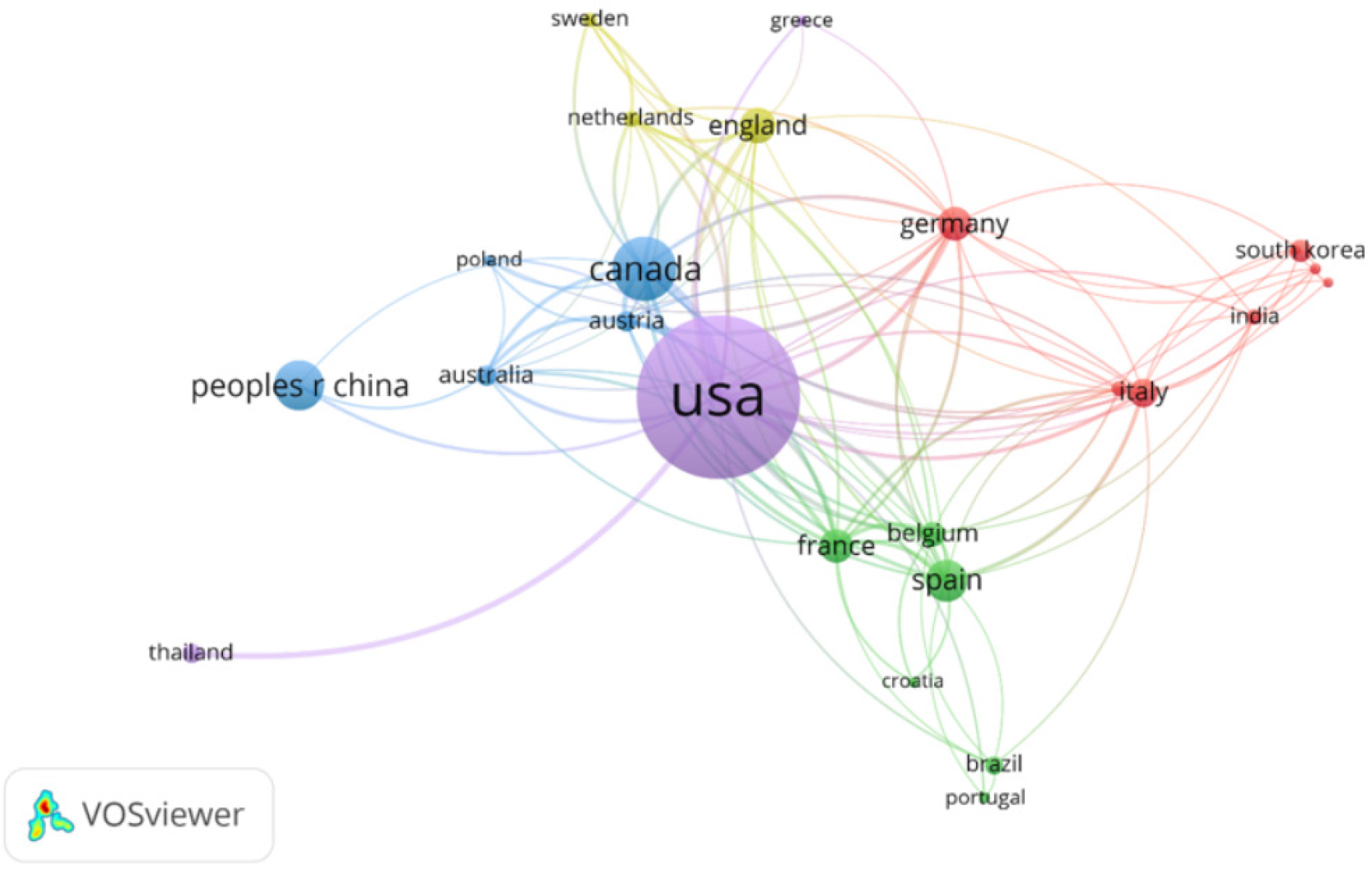
The United States emerged as the leading contributor with 209 publications, 2288 citations (57.5%), and a high total link strength (n = 137). Followed by Canada with 59 publications and 828 citations (20.81%), and China with 43 publications and 336 citations (8.44%) (Figure 2 and Table 1).
| Country | Publications (n = 427) | Citations | Percentage from total citations (n = 3979) (%) | Total link strength |
| United States | 209 | 2288 | 57.5 | 137 |
| Canada | 59 | 828 | 20.81 | 89 |
| China | 43 | 336 | 8.44 | 7 |
| Spain | 34 | 516 | 12.97 | 46 |
| England | 27 | 737 | 18.52 | 38 |
| France | 25 | 538 | 13.52 | 49 |
| Germany | 25 | 649 | 16.31 | 37 |
| Italy | 20 | 202 | 5.08 | 31 |
| Belgium | 16 | 436 | 10.96 | 37 |
| South Korea | 15 | 163 | 4.1 | 3 |
| Australia | 13 | 538 | 13.52 | 33 |
| Austria | 13 | 607 | 15.26 | 47 |
| Thailand | 12 | 21 | 0.53 | 12 |
| Brazil | 11 | 50 | 1.26 | 7 |
| Netherlands | 10 | 322 | 8.09 | 29 |
| India | 9 | 77 | 1.94 | 9 |
| Switzerland | 9 | 130 | 3.27 | 12 |
| Sweden | 8 | 16 | 0.4 | 17 |
| Portugal | 6 | 4 | 0.1 | 4 |
| Saudi Arabia | 6 | 42 | 1.06 | 8 |
The top-contributed institutions in the field of ML in transplantation were identified based on their publication and citation count. University of Toronto in Canada emerged as the leading institution according to the number of publications with 39 publications (9.13%) and 301 citations. Followed by University of California System in the United States with 34 publications (7.96%) and 263 citations and Mayo Clinic in the United States with 23 publications (5.39%) and 457 citations. Other prominent institutions included Johns Hopkins University in the United States with 19 publications (4.45%), and 458 citations, UDICE French Research Universities in France with 18 publications (4.22%) and 472 citations and University of Texas System in the United States with 18 publications (4.22%) and 638 citations. In terms of the number of citations, University of Texas System in the United States and University of Alberta in Canada, had the highest citations count with 638 and 585 citations, respectively (Table 2).
| Institution | Country | Number of publications | Percentage (%) | Total citations |
| University of Toronto | Canada | 39 | 9.13 | 301 |
| University of California System | United States | 34 | 7.96 | 263 |
| Mayo Clinic | United States | 23 | 5.39 | 457 |
| Johns Hopkins University | United States | 19 | 4.45 | 458 |
| UDICE French Research Universities | France | 18 | 4.22 | 472 |
| University of Texas System | United States | 18 | 4.22 | 638 |
| Harvard University | United States | 17 | 3.98 | 359 |
| Pennsylvania Commonwealth System of Higher Education | United States | 15 | 3.51 | 396 |
| University of Alberta | Canada | 14 | 3.28 | 585 |
| University of Pittsburgh | United States | 14 | 3.28 | 395 |
| Assistance Publique Hopitaux Paris | France | 13 | 3.04 | 458 |
| Inserm, the French National Institute of Health and Medical Research | France | 13 | 3.04 | 465 |
| Paris Cité University | France | 13 | 3.04 | 293 |
| Stanford University | United States | 12 | 2.81 | 17 |
| Thammasat University | Thailand | 12 | 2.81 | 23 |
| University of Pennsylvania | United States | 12 | 2.81 | 79 |
| Medical University of Vienna | Austria | 11 | 2.58 | 576 |
| University of Mississippi | United States | 11 | 2.58 | 15 |
| Columbia University | United States | 10 | 2.34 | 48 |
| Duke University | United States | 10 | 2.34 | 122 |
The leading journal in terms of publications was found to be the "Journal of Heart and Lung Transplantation", accounting for 47 publications, representing approximately 11% of the total research output. The "American Journal of Transplantation" followed closely with 33 publications (7.7%). Other prominent journals included "Transplantation" with 17 publications (3.9%) and "Transplant International" with 12 publications (2.8%) (Table 3).
| Journal | Publications (n = 427) |
| Journal of Heart and Lung Transplantation | 47 (11) |
| American Journal of Transplantation | 33 (7.7) |
| Transplantation | 17 (3.9) |
| Transplant International | 12 (2.8) |
| PLOS One | 11 (2.6) |
| Scientific Reports | 11 (2.6) |
| Hepatology | 10 (2.3) |
| Journal of Clinical Medicine | 9 (2.1) |
| Frontiers in Immunology | 7 (1.6) |
| Lecture Notes in Computer Science | 7 (1.6) |
| Liver Transplantation | 7 (1.6) |
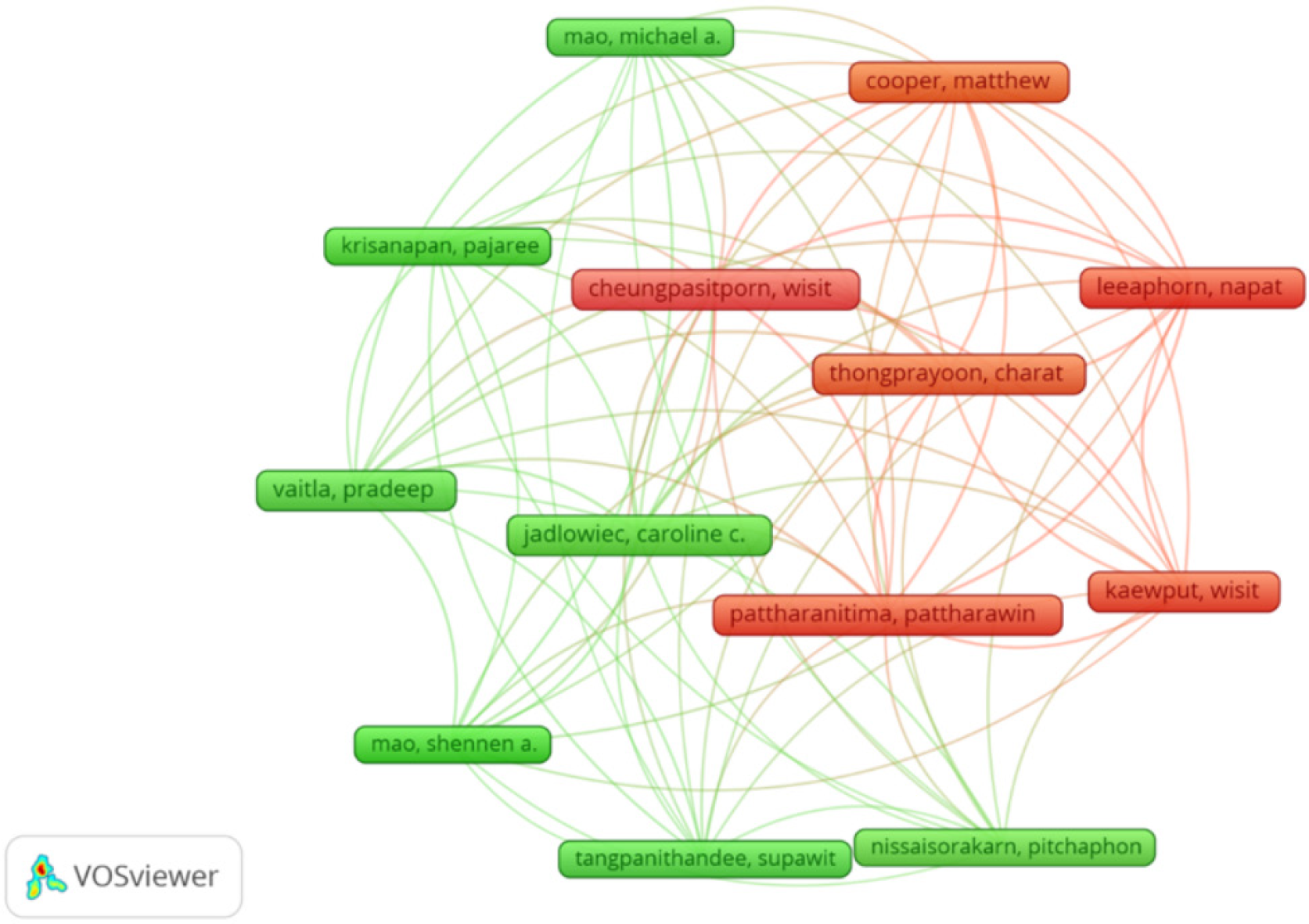
The analysis of author contributions in the field of ML in transplantation revealed the top authors who have made significant research contributions. Cheungpasitporn, Wisit and Thongprayoon, Charat had the highest number of publications in the field of ML in transplantation (n = 13). Followed closely by Leeaphorn, Napat (n = 12), Cooper, Matthew (n = 11), Erdman, Lauren (n = 11), Jadlowiec, Caroline C (n = 11), and Pattharanitima, Pattharawin (n = 11) (Table 4).
| Author | Publications | Percentage (%) |
| Wisit Cheungpasitporn | 13 | 3.04 |
| Charat Thongprayoon | 13 | 3.04 |
| Napat Leeaphorn | 12 | 2.81 |
| Matthew Cooper | 11 | 2.58 |
| Lauren Erdman | 11 | 2.58 |
| Caroline C Jadlowiec | 11 | 2.58 |
| Pattharawin Pattharanitima | 11 | 2.58 |
| Michael A Mao | 10 | 2.34 |
| Shennen A Mao | 10 | 2.34 |
| Gonzalo Sapisochin | 10 | 2.34 |
| Pradeep Vaitla | 10 | 2.34 |
| Wisit Kaewput | 9 | 2.11 |
| Anna Goldenberg | 8 | 1.87 |
| Philip F Halloran | 8 | 1.87 |
| César Hervas-Martinez | 8 | 1.87 |
| Lawrence Lau | 8 | 1.87 |
| Alexandre Loupy | 8 | 1.87 |
| Maarten Naesens | 8 | 1.87 |
| Mamatha Bhat | 7 | 1.64 |
| Javier Briceno | 7 | 1.64 |
| Shaf Keshavjee | 7 | 1.64 |
| Tommy Ivanics | 6 | 1.41 |
| Pajaree Krisanapan | 6 | 1.41 |
| Carmen Lefaucheur | 6 | 1.41 |
| Pitchaphon Nissaisorakarn | 6 | 1.41 |
Figure 3 shows the network visualization of the top contributed authors and their interconnections.
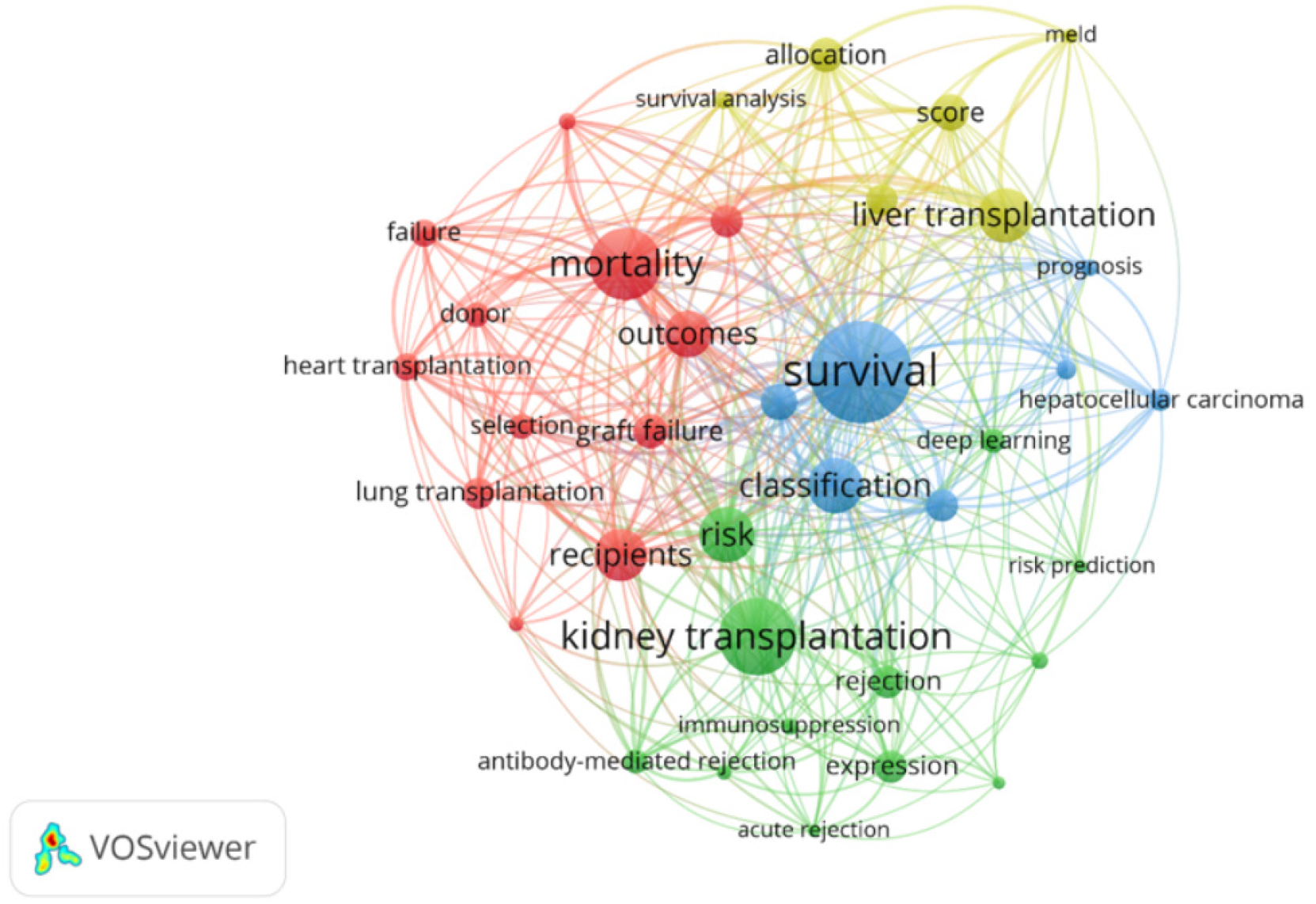
The most frequently encountered keywords were "Survival" (n = 58), "Kidney transplantation" (n = 43), "Mortality" (n = 40), Model (n = 36), Classification (n = 31), Risk (n = 31) and Liver transplantation (n = 30).
Figure 4 presents a network visualization of the top occurring keywords grouped into four clusters. Clusters’ primary focus were kidney transplantation, liver transplantation, survival and mortality outcomes. Cluster number one included kidney transplantation as the dominating keyword with other keywords such as: Rejection, acute rejection, immunosuppression, risk prediction and deep learning. Cluster number two included liver transplantation as the dominating keyword with other keywords such as: Survival analysis and allocation. The third and fourth clusters included survival and mortality related keywords as the dominating keywords with other keywords such as: Hepatocellular carcinoma, heart transplantation, lung transplantation, outcomes and prognosis.
Among the 427 studies that discussed ML and solid organ transplantation, "Decision tree and random forest models for outcome prediction in antibody incompatible kidney transplantation" published in Biomedical Signal Processing and Control Journal, stand out as the most cited (n = 162 citations). Followed by “Machine Learning Algorithms Outperform Conventional Regression Models in Predicting Development of Hepatocellular Carcinoma” published in the American Journal of Gastroenterology (n = 152 citations), and “Prediction of Acute Kidney Injury after Liver Transplantation: Machine Learning Approaches vs. Logistic Regression Model” published in Journal of Clinical Medicine (n = 96 citations) (Table 5).
| Title | First author | Journal | Publication year | Total citations |
| Decision tree and random forest models for outcome prediction in antibody incompatible kidney transplantation | Torgyn Shaikhina | Biomedical Signal Processing and Control | 2019 | 162 |
| Machine learning algorithms outperform conventional regression models in predicting development of hepatocellular carcinoma | Amit Singal | American Journal of Gastroenterology | 2013 | 152 |
| Prediction of acute kidney injury after liver transplantation: Machine learning approaches vs. logistic regression model | Hyung-Chul Lee | Journal of Clinical Medicine | 2018 | 96 |
| Assessing rejection-related disease in kidney transplant biopsies based on archetypal analysis of molecular phenotypes | Jeff Reeve | JCI Insight | 2017 | 90 |
| Application of machine-learning models to predict tacrolimus stable dose in renal transplant recipients | Jie Tang | Scientific Reports | 2017 | 83 |
| Predicting the graft survival for heart-lung transplantation patients: An integrated data mining methodology | Asil Oztekin | International Journal of Medical Informatics | 2009 | 79 |
| Machine-learning algorithms predict graft failure after liver transplantation | Lawrence Lau | Transplantation | 2017 | 76 |
| Applying machine learning in liver disease and transplantation: A comprehensive review | Ashley Spann | Hepatology | 2020 | 66 |
| Predicting graft survival among kidney transplant recipients: A Bayesian decision support model | Kazim Topuz | Decision Support Systems | 2018 | 64 |
| Transcriptional trajectories of human kidney injury progression | Pietro Cippa | JCI Insight | 2018 | 58 |
ML, a groundbreaking technology with the potential to revolutionize various medical fields, has emerged as a powerful tool in transplantation, particularly for predicting post-transplant outcomes and providing invaluable insights into patient prognosis[2,3,18,19]. By analyzing historical patient data, including pre-transplant risk factors and post-transplant complications, ML models offer predictive insights that help clinicians identify patients at higher risk of complications or graft failure[20]. These predictive capabilities enable proactive interventions and personalized treatment plans, leading to improved patient management and long-term transplant survival[10,15,16]. The application of ML in this context involves two main approaches: Algorithm models to determine post-transplant survival time and techniques to assess whether matching pairs surpass specific post-transplant endpoints based on the latest follow-up of the recipient[2,10,14,15].
Unlike traditional statistical methods and regression analyses, ML offers the ability to handle complex datasets by incorporating multiple variables to analyze various end-points in medicine, including both favorable and unfavorable outcomes[21]. This is particularly pertinent in transplantation, where statistical methods may misestimate outcomes like graft loss[22]. ML provides computational tools that can enhance the decision-making process in medicine, particularly in the context of organ transplantation. Despite their complexity, these computational tools hold promise in improving the understanding of complex medical scenarios and facilitating more informed and precise decision-making in transplantation and other medical disciplines[10,23].
Our study contributes to the field by employing a bibliometric analysis to comprehensively assess the research output in the domain of ML usage in solid organ transplantation. By systematically reviewing a wide range of publications over time, this type of analysis is able to shed light on the prevailing research trends in this rapidly evolving field[24-27]. This bibliometric analysis offers valuable insights into the progress and advancements made in the application of ML to transplantation research. Additionally, our study provides a comprehensive overview of the key areas of interest and the major contributors to the field. The findings from our bibliometric analysis serve as a foundation for future researchers and clinicians to further explore and deepen our understanding of ML's role in optimizing transplant procedures and improving patient outcomes; furthermore, it may be a way to communicate and collaborate between centers that contribute most to this field.
Our analysis revealed that specialized transplantation journals have shown significant interest in the field of ML usage in solid organ transplantation. The majority of publications were found in esteemed journals like the Journal of Heart and Lung Transplantation, American Journal of Transplantation, Transplantation, and Transplant International. This emphasis on ML by transplant journals underscores its growing importance in transplant medicine and its potential to enhance patient care and transplant outcomes.
The analysis of the most frequent keywords highlights the current hot topics in the field of ML usage in solid organ transplantation: Patient survival, mortality, outcomes, prediction classification, and risk assessment. The recurrence of these keywords highlights the critical significance of harnessing ML to create predictive algorithms, enabling the identification of high-risk patients, optimizing donor-recipient matching, and personalizing treatment plans (Figure 4).
ML algorithms analyze historical data and find patterns in massive, unstructured, and complex datasets using statistical, probabilistic, and optimization methods. According to their learning methodologies, ML algorithms can be categorized into three primary categories: Supervised learning, unsupervised learning, and reinforcement learning[3].
In supervised learning, the input features and their matching target outputs are supplied in labeled data, from which the algorithm learns. The objective is to acquire an understanding of the relationship between inputs and outputs so that the algorithm can predict new, unseen data with accuracy. Support Vector Machines (SVM), Decision Trees, Random Forests (RF), Naïve Bayes, and Neural Networks are examples of common algorithms in this category. Supervised learning is frequently employed in tasks such as regression, in which the algorithm predicts a continuous value, and classification, in which the algorithm gives a label to input data[28].
Unsupervised learning algorithms operate on unlabeled data, which means that they are not trained with the desired outputs. Without explicit direction, the algorithm explores structures or patterns in the data. Typical tasks in unsupervised learning include clustering and dimensionality reduction. Unsupervised learning algorithms include Principal Component Analysis, K-Means, Hierarchical Clustering, and Autoencoders[29].
In contrast to supervised and unsupervised learning, reinforcement learning does not explicitly correct suboptimal actions and does not require labeled input/output pairs for training. Rather, it emphasizes finding a middle ground between exploring new possibilities and making use of already-existing knowledge. It does this by having an agent learn from interactions with its surroundings in order to accomplish particular objectives. To maximize the cumulative reward, the agent acts, responds to feedback from the environment in the form of incentives or penalties, and modifies its behavior. When the best course of action is unknown ahead of time, reinforcement learning is frequently employed. Popular reinforcement learning algorithms include Q-Learning, Deep Q Networks, and Policy Gradient Methods[30].
The characteristics of the problem and the available data determine which algorithm is best. Every type of ML algorithm has specific advantages and disadvantages. Rather than employing unsupervised ML algorithms, the majority of ML applications have been developed using supervised ones. In the supervised version, the model is created by learning a dataset with known labels, allowing predictions to be made about the outcomes of examples without labels[2,3].
Recent years have seen significant advances in solid organ transplantation using ML applications. Various studies have explored the use of different ML algorithms to predict graft survival and other critical outcomes in kidney, liver, heart and lung and pediatric transplantation[13]. Specifically, Shadabi et al[31] employed an ensemble of artificial neural networks (ANN) to predict post kidney transplantation graft survival. Additionally, Ravikumar et al[19] utilized the SVM technique to improve donor and recipient pair matching, increasing the likelihood of graft and recipient survival. These studies illustrate the ways in which ML enhances the outcome of kidney transplantation.
In liver transplantation, the success of the procedure significantly hinges on the compatibility and efficacy of the donor-recipient match. In recognition of this critical aspect, Briceño et al[32] proposed a novel donor-recipient matching model that employs two ANN models. The initial ANN was intended to enhance the probability of graft survival, whereas the second ANN was optimized to reduce the likelihood of graft loss. Their groundbreaking work sought to improve liver transplantation outcomes by developing a powerful decision-making system that maximized the concepts of equity, efficiency, and fairness. In keeping with this line of inquiry, a number of additional investigations have employed ML algorithms to predict diverse facets of organ transplantation, encompassing waitlist mortality and post-transplant consequences[13].
Two ANN models were proposed for matching donors and recipients. The first ANN was designed to enhance the probability of graft survival, whereas the second ANN was designed to reduce the likelihood of graft loss. They aimed to develop an efficient system that enhances the equity, thereby improving the outcome of liver transplantation, by using a dataset with over 1000 donor-recipient pairs and 64 donor, recipient, and transplantation variables.
Several ML algorithms have been used in more recent research to predict liver transplantation outcomes. Nagai et al[33] created an ANN algorithm for predicting 90-day waitlist mortality, with an area under the curve of 0.936. They divided 105140 patients from the Organ Procurement and Transplantation Network/United Network for Organ Sharing registry listed for transplant between 2002 and 2021 into training and validation datasets. In terms of predicting mortality, the ANN 90-day mortality model performed superior to MELD-based models in every subset. In a similar vein, Bertsimas et al[34] proposed an "optimized prediction of mortality" (OPOM) model for 90-day waitlist mortality that makes use of optimal classification trees. The MELD-Na model had an areas under receiver operating characteristic curves (AUROCs) of 0.841, while the OPOM model had 0.859 and could reduce waitlist mortality. In addition to the 90-day prediction timeline, ML models have been tested for cirrhosis patient 1-year mortality. Kanwal et al[35] designed three ML models using extreme gradient descent boosting, logistic regression (LR) with LASSO regularization, and a limited LR model. With 107939 cirrhosis patients included, they were able to predict 1-year mortality with an AUROC of 0.78. Deep neural networks (DNNs), RF, and LR models were compared by Guo et al[36] and their DNN and RF models outperformed the LR model (AUROC = 0.69) for 1-year mortality prediction, with AUROCs of 0.85-0.86. lastly, Kwong et al[37] created an RF model to predict waitlist dropout in patients with hepatocellular carcinoma who were listed for transplant. Using 12 predictive features, they were able to achieve a concordance statistic of 0.74 for waitlist dropout prediction at the 3-, 6-, and 12-month marks. These studies demonstrate the expanding role of ML algorithms in enhancing liver transplant outcome prediction, providing insightful information and possible advantages for liver transplant patient care.
Studies have utilized ML techniques to improve decision-making and predict crucial outcomes in the realm of thoracic organ transplantation. Delen et al[18] relied on the UNOS thoracic transplantation database to employ support vector regression, multilayer perceptron, and regression trees to predict the time frame from transplant to death or last follow-up, yielding positive findings. Oztekin et al[38] predicted post-lung transplant QoL using genetic algorithms for feature selection and ML algorithms. These studies show that ML can improve thoracic organ transplantation outcomes and provide valuable insights.
In the context of pediatric transplantation, ML techniques have also been investigated. For example, a study[39] used RF and conditional inference trees to determine the influence of specific donor variables. factors on pediatric liver transplantation. At the same time, Miller et al[40] assessed a variety of ML algorithms, such as ANN, decision tree, and RF, to predict mortality in the years following pediatric heart transplants. These studies emphasize the potential of ML to enhance outcomes in a variety of transplantation scenarios and its capacity to enhance the field of organ transplantation medicine. Despite the presence of certain obstacles, including small data sizes and insufficient data, the field's ongoing research has the potential to transform transplantation practices and improve patient care.
Overall, use of ML in organ transplantation research has the potential to improve the accuracy of predictions and decision-making processes, thereby optimizing transplantation outcomes and providing medical practitioners with valuable tools. Nevertheless, in order to fully leverage the potential of these techniques and confront the distinctive obstacles that arise in each transplantation scenario, additional research and the standardization of methodologies are imperative.
Emerging frontiers: The intersection between ML and solid organ transplantation is highly promising. As the technology matures and datasets become even more comprehensive, the promise of ML-driven insights in transplantation becomes an exciting frontier, ripe for exploration and innovation.
Predictive analytics: The advanced predictive algorithms of ML show immense promise. It is anticipated that, in the imminent future, these algorithms will serve to markedly refine the process of organ allocation[13]. This requires a system capable of determining recipient compatibility with particular organ donors with an unprecedented degree of accuracy. Utilizing a comprehensive set of variables and analyzing their complex interactions, this evolving methodology has the potential to surpass the current conventional allocation paradigms. Moreover, as we delve deeper into post-transplant scenarios, ML models are being honed to predict individualized patient outcomes following a transplant. Whether it's the potential of organ rejection, susceptibility to infections, or the overall patient survival trajectory, these models leverage extensive datasets to provide these insights.
Advanced imaging and personalized medicine: ML makes advances in analyzing medical images across multiple specialties[4], transplantation is on the cusp of similar advancements. In the near future, transplantation could gain deeper, more nuanced insights into the viability and quality of donor organs, based on the success of ML-powered image analytics in other medical disciplines. These innovations would revolutionize the selection process, enabling medical professionals to make informed decisions regarding organ matches and allocations.
Similarly, as personalized medicine gains traction in other medical fields, transplantation may soon stand to gain. In a future governed by the integration of ML and advanced biomedicine, healthcare practitioners may have the ability to design immunosuppression regimens that are meticulously tailored to the unique biological and physiological profiles of individual recipients. This has the potential to not only mitigate adverse reactions but also significantly decrease the likelihood of organ rejection. Coupled with ML's anticipated predictive capabilities, we may soon be able to predict with unmatched precision how patients will respond to various post-transplant treatments.
Challenges: Although ML has the potential to improve organ transplantation, it also faces a number of challenges[13,23]. Three main areas of concern are the consistency, model security, and quality of the data used in modeling[41-44]. Moreover, a model's generalizability may be restricted and potential biases may be introduced by small sample sizes, variability amongst transplant centers, and inconsistent data collection[13,41-44]. Several models lack external validation and perspective, emphasizing the need for post-implementation monitoring and rigorous external validation in different datasets or data models[13].
Additionally, it is imperative to incorporate both clinical and non-clinical characteristics into research to guarantee equitable transplantation outcomes. Factors such as resource availability, donor-recipient physical compatibility, and geographic disparity can have a significant impact on the results. Depending on how the ML model is developed, certain important population segments may not be well represented, potentially leading to biased predictions[13]. The focus should be placed on procedures that guarantee objectivity in model evaluations. Moreover, If trained on biased or incomplete data, ML can result in inaccurate predictions for donor-recipient matching or post-transplant care, which can lead to misinformation[43,45]. The risk of suboptimal clinical outcomes is heightened by the challenge of comprehending the rationale behind the decisions made by complex ML models ("black-box" models)[45].
Converting ML results into practical clinical insights presents challenges outside of the data itself. Although ML can spot trends, the clinical or physiological justification for them may be elusive, thus results must be both accurate and interpretable[13]. The need for real-time predictions in some transplant scenarios increases this demand. Furthermore, the performance of a model can vary depending on the patient population to which it is applied. As a result, a model developed for one population may not be suitable for another, highlighting the necessity of thorough validation on separate datasets[23,41,42]. Additionally, the steep learning curve that healthcare professionals have is one of the possible bottlenecks brought about by applying ML. However, with recent advances, many ML libraries are developing user-friendly functions to improve interpretability[43].
This bibliometric analysis underscores the growing significance of ML in solid organ transplantation, especially in donor-recipient matching, post-transplant monitoring, and patient management. The increase in publications, driven by contributions from the United States and prominent journals, indicates a heightened interest in the field. The potential of ML to enhance patient outcomes is clear; however, ongoing research and collaboration are crucial to overcome existing challenges and optimize its influence on transplantation practices.
| 1. | Deo RC. Machine Learning in Medicine. Circulation. 2015;132:1920-1930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1155] [Cited by in RCA: 2156] [Article Influence: 215.6] [Reference Citation Analysis (7)] |
| 2. | Haug CJ, Drazen JM. Artificial Intelligence and Machine Learning in Clinical Medicine, 2023. N Engl J Med. 2023;388:1201-1208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 685] [Cited by in RCA: 641] [Article Influence: 213.7] [Reference Citation Analysis (1)] |
| 3. | Choi RY, Coyner AS, Kalpathy-Cramer J, Chiang MF, Campbell JP. Introduction to Machine Learning, Neural Networks, and Deep Learning. Transl Vis Sci Technol. 2020;9:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 319] [Reference Citation Analysis (5)] |
| 4. | Currie G, Hawk KE, Rohren E, Vial A, Klein R. Machine Learning and Deep Learning in Medical Imaging: Intelligent Imaging. J Med Imaging Radiat Sci. 2019;50:477-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 236] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 5. | Heo J, Yoon JG, Park H, Kim YD, Nam HS, Heo JH. Machine Learning-Based Model for Prediction of Outcomes in Acute Stroke. Stroke. 2019;50:1263-1265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 379] [Article Influence: 63.2] [Reference Citation Analysis (0)] |
| 6. | Moll M, Qiao D, Regan EA, Hunninghake GM, Make BJ, Tal-Singer R, McGeachie MJ, Castaldi PJ, San Jose Estepar R, Washko GR, Wells JM, LaFon D, Strand M, Bowler RP, Han MK, Vestbo J, Celli B, Calverley P, Crapo J, Silverman EK, Hobbs BD, Cho MH. Machine Learning and Prediction of All-Cause Mortality in COPD. Chest. 2020;158:952-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 80] [Article Influence: 13.3] [Reference Citation Analysis (3)] |
| 7. | Sammut SJ, Crispin-Ortuzar M, Chin SF, Provenzano E, Bardwell HA, Ma W, Cope W, Dariush A, Dawson SJ, Abraham JE, Dunn J, Hiller L, Thomas J, Cameron DA, Bartlett JMS, Hayward L, Pharoah PD, Markowetz F, Rueda OM, Earl HM, Caldas C. Multi-omic machine learning predictor of breast cancer therapy response. Nature. 2022;601:623-629. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 243] [Cited by in RCA: 387] [Article Influence: 96.8] [Reference Citation Analysis (0)] |
| 8. | Grueso S, Viejo-Sobera R. Machine learning methods for predicting progression from mild cognitive impairment to Alzheimer's disease dementia: a systematic review. Alzheimers Res Ther. 2021;13:162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 136] [Article Influence: 27.2] [Reference Citation Analysis (0)] |
| 9. | Cammarota G, Ianiro G, Ahern A, Carbone C, Temko A, Claesson MJ, Gasbarrini A, Tortora G. Gut microbiome, big data and machine learning to promote precision medicine for cancer. Nat Rev Gastroenterol Hepatol. 2020;17:635-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 191] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 10. | Balch JA, Delitto D, Tighe PJ, Zarrinpar A, Efron PA, Rashidi P, Upchurch GR Jr, Bihorac A, Loftus TJ. Machine Learning Applications in Solid Organ Transplantation and Related Complications. Front Immunol. 2021;12:739728. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | Vagefi PA, Bertsimas D, Hirose R, Trichakis N. The rise and fall of the model for end-stage liver disease score and the need for an optimized machine learning approach for liver allocation. Curr Opin Organ Transplant. 2020;25:122-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Bishara AM, Lituiev DS, Adelmann D, Kothari RP, Malinoski DJ, Nudel JD, Sally MB, Hirose R, Hadley DD, Niemann CU. Machine Learning Prediction of Liver Allograft Utilization From Deceased Organ Donors Using the National Donor Management Goals Registry. Transplant Direct. 2021;7:e771. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 13. | Gotlieb N, Azhie A, Sharma D, Spann A, Suo NJ, Tran J, Orchanian-Cheff A, Wang B, Goldenberg A, Chassé M, Cardinal H, Cohen JP, Lodi A, Dieude M, Bhat M. The promise of machine learning applications in solid organ transplantation. NPJ Digit Med. 2022;5:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 54] [Reference Citation Analysis (0)] |
| 14. | Bhat M, Rabindranath M, Chara BS, Simonetto DA. Artificial intelligence, machine learning, and deep learning in liver transplantation. J Hepatol. 2023;78:1216-1233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 122] [Article Influence: 40.7] [Reference Citation Analysis (0)] |
| 15. | Chen C, Chen B, Yang J, Li X, Peng X, Feng Y, Guo R, Zou F, Zhou S, Hei Z. Development and validation of a practical machine learning model to predict sepsis after liver transplantation. Ann Med. 2023;55:624-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 23] [Reference Citation Analysis (0)] |
| 16. | Fusfeld L, Menon S, Gupta G, Lawrence C, Masud SF, Goss TF. US payer budget impact of a microarray assay with machine learning to evaluate kidney transplant rejection in for-cause biopsies. J Med Econ. 2022;25:515-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84:523-538. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4505] [Cited by in RCA: 5693] [Article Influence: 334.9] [Reference Citation Analysis (2)] |
| 18. | Delen D, Oztekin A, Kong ZJ. A machine learning-based approach to prognostic analysis of thoracic transplantations. Artif Intell Med. 2010;49:33-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 19. | Ravikumar A, Saritha R, Chandra V. Support vector machine based prognostic analysis of renal transplantations. 2013 Fourth Int Conf Computi, Commun Netw Technol (ICCCNT). 2013;9:1-6. [DOI] [Full Text] |
| 20. | Lau L, Kankanige Y, Rubinstein B, Jones R, Christophi C, Muralidharan V, Bailey J. Machine-Learning Algorithms Predict Graft Failure After Liver Transplantation. Transplantation. 2017;101:e125-e132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 124] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 21. | Briceño J, Calleja R, Hervás C. Artificial intelligence and liver transplantation: Looking for the best donor-recipient pairing. Hepatobiliary Pancreat Dis Int. 2022;21:347-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 22. | Kampaktsis PN, Tzani A, Doulamis IP, Moustakidis S, Drosou A, Diakos N, Drakos SG, Briasoulis A. State-of-the-art machine learning algorithms for the prediction of outcomes after contemporary heart transplantation: Results from the UNOS database. Clin Transplant. 2021;35:e14388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 23. | Guijo-Rubio D, Gutiérrez PA, Hervás-Martínez C. Machine learning methods in organ transplantation. Curr Opin Organ Transplant. 2020;25:399-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Rawashdeh B, AlRyalat SA, Abuassi M, Prasad R, Cooper M. Unveiling transplantation research productivity of United States: A bibliometric analysis. World J Transplant. 2023;13:391-402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (2)] |
| 25. | Rawashdeh B, AlRyalat SA, Abuassi M, Syaj S, Jeyyab MA, Pearson T, Kim J. Impact of COVID-19 on abdominal organ transplantation: A bibliometric analysis. Transpl Infect Dis. 2023;25:e14027. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 26. | Rawashdeh B, Arpali E, Al Abdallat H, Cooper M, Dunn T. Four Decades of Research Productivity and Hot Spots in Pancreas Transplantation. Prog Transplant. 2024;34:119-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 27. | Rawashdeh B, Kim J, Prasad R, Cooper M. A Global Overview on the Evolution, Debate, and Research Output on Liver Transplant Perfusion Machines. Exp Clin Transplant. 2024;22:35-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 28. | Uddin S, Khan A, Hossain ME, Moni MA. Comparing different supervised machine learning algorithms for disease prediction. BMC Med Inform Decis Mak. 2019;19:281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 288] [Cited by in RCA: 619] [Article Influence: 88.4] [Reference Citation Analysis (0)] |
| 29. | Iqbal T, Elahi A, Wijns W, Shahzad A. Exploring Unsupervised Machine Learning Classification Methods for Physiological Stress Detection. Front Med Technol. 2022;4:782756. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 30. | Liu E, He R, Chen X, Yu C. Deep Reinforcement Learning Based Optical and Acoustic Dual Channel Multiple Access in Heterogeneous Underwater Sensor Networks. Sensors (Basel). 2022;22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 31. | Shadabi F, Cox RJ, Sharma D, Petrovsky N. A Hybrid Decision Tree – Artificial Neural Networks Ensemble Approach for Kidney Transplantation Outcomes Prediction. Lecture Notes in Computer Science. 2005. [DOI] [Full Text] |
| 32. | Briceño J, Cruz-Ramírez M, Prieto M, Navasa M, Ortiz de Urbina J, Orti R, Gómez-Bravo MÁ, Otero A, Varo E, Tomé S, Clemente G, Bañares R, Bárcena R, Cuervas-Mons V, Solórzano G, Vinaixa C, Rubín A, Colmenero J, Valdivieso A, Ciria R, Hervás-Martínez C, de la Mata M. Use of artificial intelligence as an innovative donor-recipient matching model for liver transplantation: results from a multicenter Spanish study. J Hepatol. 2014;61:1020-1028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 101] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 33. | Nagai S, Nallabasannagari AR, Moonka D, Reddiboina M, Yeddula S, Kitajima T, Francis I, Abouljoud M. Use of neural network models to predict liver transplantation waitlist mortality. Liver Transpl. 2022;28:1133-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 34. | Bertsimas D, Kung J, Trichakis N, Wang Y, Hirose R, Vagefi PA. Development and validation of an optimized prediction of mortality for candidates awaiting liver transplantation. Am J Transplant. 2019;19:1109-1118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 89] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 35. | Kanwal F, Taylor TJ, Kramer JR, Cao Y, Smith D, Gifford AL, El-Serag HB, Naik AD, Asch SM. Development, Validation, and Evaluation of a Simple Machine Learning Model to Predict Cirrhosis Mortality. JAMA Netw Open. 2020;3:e2023780. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 62] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 36. | Guo A, Mazumder NR, Ladner DP, Foraker RE. Predicting mortality among patients with liver cirrhosis in electronic health records with machine learning. PLoS One. 2021;16:e0256428. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 37. | Kwong A, Hameed B, Syed S, Ho R, Mard H, Arshad S, Ho I, Suleman T, Yao F, Mehta N. Machine learning to predict waitlist dropout among liver transplant candidates with hepatocellular carcinoma. Cancer Med. 2022;11:1535-1541. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 38. | Oztekin A, Al-ebbini L, Sevkli Z, Delen D. A decision analytic approach to predicting quality of life for lung transplant recipients: A hybrid genetic algorithms-based methodology. Eur J Oper Res. 2018;266:639-651. [DOI] [Full Text] |
| 39. | Wadhwani SI, Hsu EK, Shaffer ML, Anand R, Ng VL, Bucuvalas JC. Predicting ideal outcome after pediatric liver transplantation: An exploratory study using machine learning analyses to leverage Studies of Pediatric Liver Transplantation Data. Pediatr Transplant. 2019;23:e13554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 40. | Miller R, Tumin D, Cooper J, Hayes D Jr, Tobias JD. Prediction of mortality following pediatric heart transplant using machine learning algorithms. Pediatr Transplant. 2019;23:e13360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 41. | Dou B, Zhu Z, Merkurjev E, Ke L, Chen L, Jiang J, Zhu Y, Liu J, Zhang B, Wei GW. Machine Learning Methods for Small Data Challenges in Molecular Science. Chem Rev. 2023;123:8736-8780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 161] [Article Influence: 53.7] [Reference Citation Analysis (0)] |
| 42. | Alafif T, Tehame AM, Bajaba S, Barnawi A, Zia S. Machine and Deep Learning towards COVID-19 Diagnosis and Treatment: Survey, Challenges, and Future Directions. Int J Environ Res Public Health. 2021;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 63] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 43. | Tran J, Sharma D, Gotlieb N, Xu W, Bhat M. Application of machine learning in liver transplantation: a review. Hepatol Int. 2022;16:495-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 44. | Dinsdale NK, Bluemke E, Sundaresan V, Jenkinson M, Smith SM, Namburete AIL. Challenges for machine learning in clinical translation of big data imaging studies. Neuron. 2022;110:3866-3881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 45. | Obermeyer Z, Emanuel EJ. Predicting the Future - Big Data, Machine Learning, and Clinical Medicine. N Engl J Med. 2016;375:1216-1219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1493] [Cited by in RCA: 1764] [Article Influence: 176.4] [Reference Citation Analysis (2)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/