Published online Aug 18, 2022. doi: 10.5500/wjt.v12.i8.250
Peer-review started: January 28, 2022
First decision: March 25, 2022
Revised: March 27, 2022
Accepted: July 25, 2022
Article in press: July 25, 2022
Published online: August 18, 2022
Processing time: 201 Days and 18.2 Hours
Several studies have demonstrated that the coronavirus disease 2019 (COVID-19) has affected daily living and the healthcare system. No previous study has described the consequences of COVID-19 on emergency department (ED) visits and hospital admission among kidney transplant (KT) recipients.
To investigate the impact of the COVID-19 pandemic on ED visits and hospital admissions within 1 year in patients who underwent KT in Thailand.
We conducted a retrospective study at a university hospital in Thailand. We reviewed the hospital records of KT patients who visited the ED during the outbreak of COVID-19 (from January 2020 to December 2021). We used the previous 2 years as the control period in the analysis. We obtained baseline demographics and ED visit characteristics for each KT patient. The outcomes of interest were ED visits and ED visits leading to hospital admission within the 1st year following a KT. The rate of ED visits and ED visits leading to hospital admissions between the two periods were compared using the stratified Cox proportional hazards model.
A total of 263 patients were included in this study: 112 during the COVID-19 period and 151 during the control period. There were 34 and 41 ED visits after KT in the COVID-19 and control periods, respectively. The rate of first ED visit at 1 year was not significantly different in the COVID-19 period, compared with the control period [hazard ratio (HR) = 1.02, 95% confidence interval (CI): 0.54-1.92; P = 0.96]. The hospital admission rate was similar between periods (HR = 0.92, 95%CI: 0.50-1.69; P = 0.78).
ED visits and hospital admissions within the 1st year in KT recipients were not affected by the COVID-19 pandemic. Despite these findings, we believe that communication between post-KT patients and healthcare providers is essential to highlight the importance of prompt ED visits for acute health conditions, particularly in post-KT patients.
Core Tip: Coronavirus disease 2019 (COVID-19) affects kidney transplant (KT) recipients in terms of hospital admission rates. This study showed that despite emergency department (ED) visits remaining unchanged during the COVID-19 pandemic, hospital admission rates increased. Although we could not establish the cause-effect relationship of these changes, we encourage healthcare providers to provide post-KT patients recommendations to visit ED promptly for acute health conditions.
- Citation: Wongtanasarasin W, Phinyo P. Emergency department visits and hospital admissions in kidney transplant recipients during the COVID-19 pandemic: A hospital-based study. World J Transplant 2022; 12(8): 250-258
- URL: https://www.wjgnet.com/2220-3230/full/v12/i8/250.htm
- DOI: https://dx.doi.org/10.5500/wjt.v12.i8.250
In the United States, there were approximately 143 million total visits to an emergency department (ED) in 2018[1]. Over the last two decades, the rate of ED visits has increased, exceeding what could be accounted for by population growth[1]. Multiple factors, including extremes of age, women, public insurance, minority race/ethnicity, and country region, are associated with higher rates of ED visits in the general population[2]. Recently, there has been a significant increase in acute care delivery following hospitalization[3,4]. Acute care after hospital treatment is considered an indication of poor quality of care in some contexts, including kidney transplant (KT) patients[4,5]. Patients with end-stage renal disease (ESRD) account for 7.1% of total Medicare expenditures in the United States despite accounting for only 0.9% of Medicare treatments[6,7]. Patients with ESRD have visited the ED at a 6-fold higher rate than the general population; however, most previous studies excluded KT patients, who account for a growing proportion (around 22.8%) of prevalent ESRD patients[7]. The long-term advantages of KT are well documented and include improved survival and quality of life compared to dialysis[8,9]. On the other hand, the management of patients after KT is complex and resource-intensive, necessitating extensive care coordination, frequent laboratory monitoring, and ongoing patient engagement[9,10]. Furthermore, KT recipients frequently have multiple comorbidities, which complicates their care[11,12].
In recent years, coronavirus disease 2019 (COVID-19) has become the most critical disease and influenced human health across the globe[13]. This pandemic affects not only physical health but also mental health and well-being[14]. Transplant recipients, including KT patients, who are receiving immunosuppressive therapy are at the highest risk of severe illness, and as a result, are at a higher risk of an adverse outcome from COVID-19[15]. One of the unique aspects of the transplant recipient’s life is that, in the post-operative phase, the patient should live in an isolated space, pay special attention to their living environment, and prefer a limited social life because of the immunosuppressive treatment involves immunosuppression in the patient[14]. A previous study demonstrated that the COVID-19 pandemic is associated with a significant reduction in average daily ED visits; however, the admission rates were increased[16]. This research investigated the effect of COVID-19 and the consequences on ED visits and admission rates among KT recipients within 1 year. In addition, this study assessed the differences in the diagnoses of KT patients who visited an ED between COVID-19 and regular periods.
We conducted a single-center retrospective observational study at a university tertiary hospital between January 2018 and December 2021. The study protocol was approved by the institutional review board (IRB) of the Faculty of Medicine, Chiang Mai University (EXEMPTION-8745/65; Chiang Mai, Thailand). The IRB waived informed consent due to its retrospective design. Patient confidentiality was preserved by using anonymous health records. All methods employed in this study were performed following relevant guidelines and regulations.
Maharaj Nakorn Chiang Mai Hospital (MNCMH) is a university hospital with 1500 beds, 151 intensive care units (ICUs) and sub-ICU beds, 28 operating rooms, and doctors from all subspecialties on duty. According to the Canadian Triage and Acuity Scale, the triage categorization is based on a five-level scale, ranging from blue (level 1, resuscitation) to white (level 5, non-urgency). Our ED provides a 24-h service with emergency physicians and skilled nurses. We categorized seven types of dispositions in the current study: ICU admission, general ward admission, observational unit admission, referral to another hospital, discharge, discharge against doctor’s recommendation, and death.
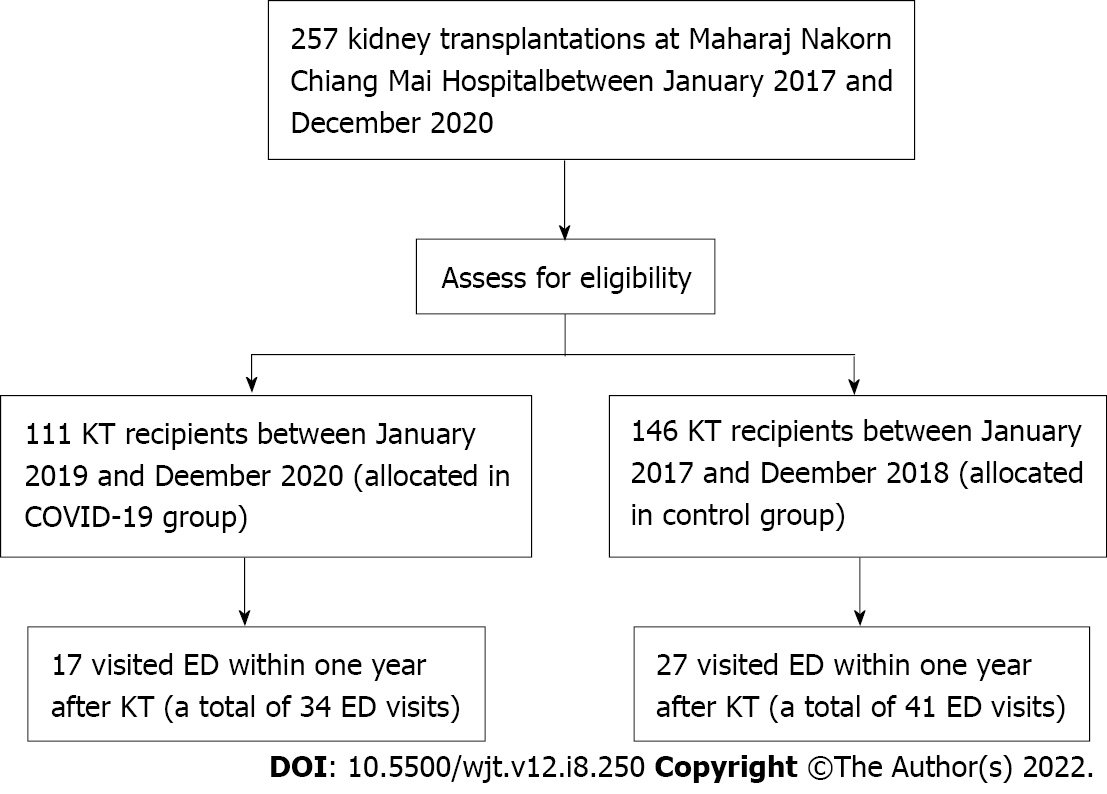
We included all adult patients (age ≥ 18 years) who underwent KT at MNCMH between January 2017 and December 2020. Patients who died in the hospital after KT before hospital discharge were excluded. We collected data only from KT patients who visited the ED of MNCMH within 1 year after the date of transplantation (between January 2018 and December 2021). Extreme outliers and high-volume ED visitors (KT patients using the ED more than ten times per year) were excluded from the study population and were not included in the study analysis.
Data were collected through the electronic medical records and chart review. To assess risk factors for ED visits and admissions following KT, age, sex, donor types, insurance, and Charlson comorbidity index were collected. Specifically, for KT recipients who visited the ED within 1 year after transp
The primary outcome of interest was ED visits in the 1st year following KT. All recipients were followed until death or out of the study period. In-hospital deaths were retrieved from hospital medical records. Patients who did not visit ED at the end of the study period were considered censors. For patients with recurrent ED visits, the time to ED visit was defined as the time from the index date of transplantation to the date of the recurrent ED visit. The risk interval was, therefore, set as marginal since we assumed that the patients were at risk of any ED visit from the date of their transplantation.
Secondary outcomes included ED visits leading to hospital admissions following KT’s 1st year. The number of ED visits and hospital admissions for any reason was calculated and compared between January 2018 and December 2019 and between January 2020 and December 2021. All responsible diagnoses from January 2018 to December 2019 were compared to all diagnoses from January 2020 to December 2021. We described continuous data using the mean ± SD for normally distributed variables. For skewed data, median and interquartile range were calculated. Categorical data were summarized using frequency and percentage. The independent t-test was used to compare continuous variables. For categorical variables, Fisher’s exact probability test was performed. All tests were two-sided, with significance for all tests being determined as P < 0.05. All analyses were performed using STATA 16 (StataCorp, College Station, TX, United States).
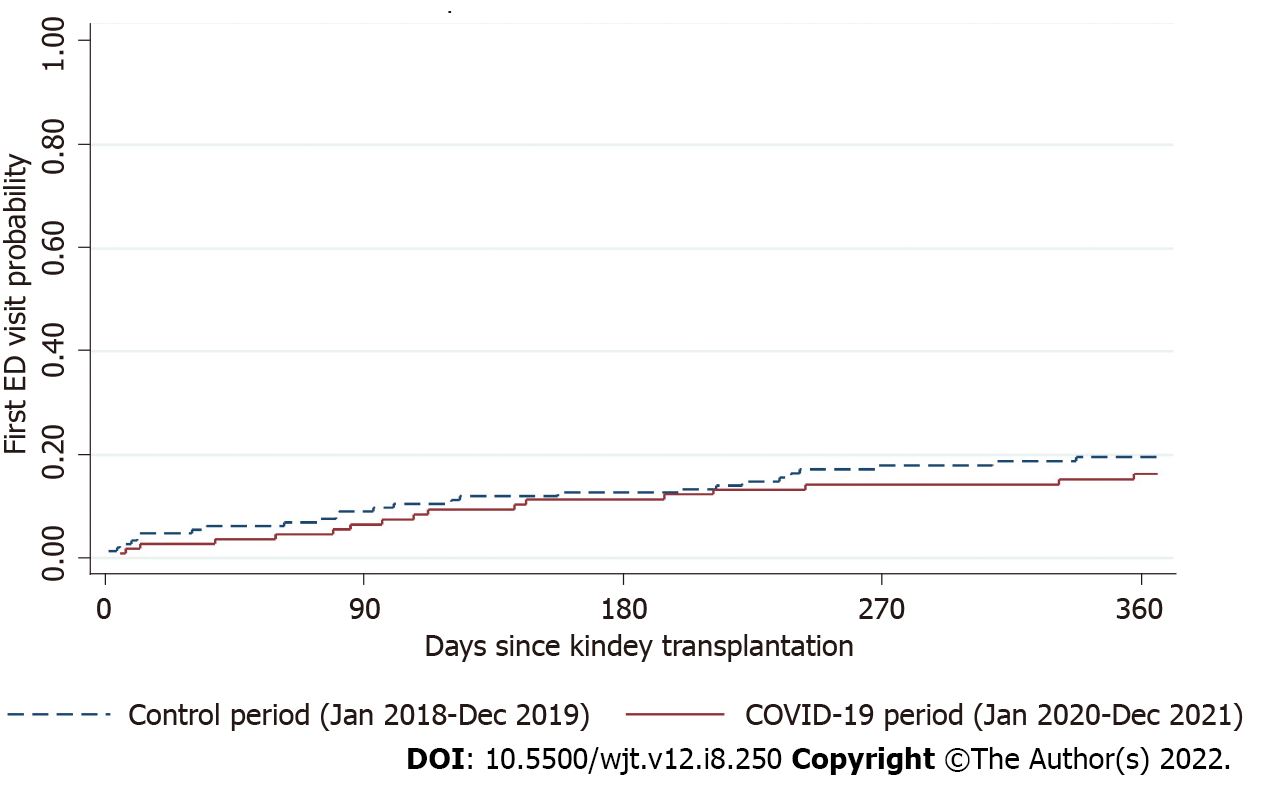
For the primary analysis, the rate of ED visits within 1 year after KT was compared using the stratified Cox proportional hazards model. We presented two analytic approaches for each survival outcome, the rate of first ED visits and any ED visit after transplantation. For the rate of the first ED visit, we restricted the analysis to only the first ED visit, whereas all ED visits during the 1st year period were considered in the analysis of the rate of any ED visits. We employed the modeling method for recurrent events described by Kelly and Lim[17]. The risk interval was defined as the total time (marginal). We used a restricted risk set and assumed event-specific baseline hazards. To quantify the effect of the COVID-19 pandemic period on the control period, hazard ratios (HRs) were estimated from the stratified Cox’s regression model. They were reported with 95% confidence intervals (CI) and P values. Kaplan-Meier curves were demonstrated, and a comparison of differences was made by the log-rank test.
A total of 263 KT recipients were enrolled in this study, 112 in the COVID-19 period (underwent KT between January 2019 and December 2020) and 151 in the control period (underwent KT between January 2017 and December 2018). No recipient died during the follow-up period. Figure 1 illustrates the flow diagram of this study population. The mean ages were 45.5 ± 10.4 years and 43.7 ± 13.4 years for COVID-19 and control groups, respectively. Most of the participants received deceased donors. There were no significant differences in baseline demographics between the two periods (Table 1). Baseline demographics of KT patients who visited an ED during the study periods are summarized in Table 1.
| Characteristics | COVID-19, n = 112 | Control, n = 151 | P value |
| Male sex, n (%) | 70 (62.5) | 93 (61.6) | 0.92 |
| Age at transplant, mean ± SD | 45.5 ± 10.4 | 43.7 ± 13.4 | 0.23 |
| Age at transplant, n (%) | 0.20 | ||
| < 40 | 35 (31.3) | 55 (36.4) | |
| 40-59 | 68 (6.7) | 77 (51.0) | |
| ≥ 60 | 9 (8.0) | 19 (12.6) | |
| Donor type, n (%) | 0.65 | ||
| Living donor | 41 (36.6) | 59 (39.1) | |
| Deceased donor | 71 (63.4) | 92 (60.9) | |
| Insurance, n (%) | 0.66 | ||
| Universal coverage | 24 (21.4) | 56 (37.1) | |
| Social security scheme | 33 (29.5) | 40 (26.5) | |
| Government officer | 55 (49.1) | 55 (36.4) | |
| Charlson comorbidity index, mean ± SD | 1.7 ± 1.5 | 1.8 ± 1.5 | 0.59 |
A total of 17.1% of KT recipients visited ED within 1 year after transplantation (15.3% in the COVID-19 period and 18.5% in the control period), accounting for 75 ED visits. The mean times to first ED visit since transplantations were 130.8 ± 106.2 and 120.6 ± 105.3 d for the COVID-19 and control periods, respectively. On the other hand, the rates of invasive procedures were similar among both periods. Table 2 summarizes the clinical variables of KT patients who presented to the ED within 1 year after transplantation. The rate of first ED visit at 1 year was not different in the COVID-19 period, compared with the control period when adjusting for confounding variables (HR = 1.02, 95%CI: 0.54-1.92; P = 0.96, Figure 2). Similarly, the rate of any ED visit in the following year was also not different between the two periods (HR = 1.24, 95%CI: 0.73-2.10; P = 0.43, Table 3). The five most responsible diagnoses are demonstrated in Table 4. Fever and abdominal pain were ranked first during the control period, while abdominal pain was the top diagnosis during COVID-19.
| Variables | COVID-19 (January 2020-December 2021), n = 34 | Control (January 2018-December 2019), n = 41 | P value |
| Time to first ED visit since transplantation in day, mean ± SD | 130.8 ± 106.2 | 120.6 ± 105.3 | 0.88 |
| Triage level, n (%) | 0.71 | ||
| Resuscitation | 2 (5.9) | 1 (2.4) | |
| Emergency | 13 (38.2) | 13 (31.7) | |
| Urgency | 12 (35.3) | 20 (48.8) | |
| Less urgency | 5 (14.7) | 6 (14.6) | |
| Non-urgency | 2 (5.9) | 1 (2.4) | |
| Total ED times in min, mean ± SD | 275.8 ± 263.5 | 232.7 (120.6) | 0.35 |
| Total ED times in min, median (IQR) | 210.5 (130-330) | 222 (138-300) | 0.35 |
| Admission, n (%) | 13 (38.2) | 27 (65.9) | 0.02 |
| Type of disposition, n (%) | 0.10 | ||
| ICU admission | 1 (2.9) | 1 (2.4) | |
| General ward admission | 12 (35.3) | 25 (61.0) | |
| OU admission | 0 (0) | 1 (2.4) | |
| Referred | 0 (0) | 0 (0) | |
| Discharge | 21 (61.8) | 14 (34.2) | |
| Against advice | 0 (0) | 0 (0) | |
| Death at ED | 0 (0) | 0 (0) | |
| Intubation, n (%) | 0 (0) | 1 (2.4) | 0.36 |
| CPR, n (%) | 0 (0) | 0 (0) | N/A |
| Outcomes | Multivariable HR1 | 95%CI | P value |
| First ED visit | 1.02 | 0.54-1.92 | 0.96 |
| Any ED visit | 1.24 | 0.73-2.10 | 0.43 |
| ED visit leading to hospital admission | 0.92 | 0.50-1.69 | 0.78 |
| No | ICD-10 | Diagnoses | % |
| January 2018-December 2019 | |||
| 1 | R509 | Fever, unspecified | 12.8 |
| 2 | R104 | Other and unspecified abdominal pain | 12.8 |
| 3 | N185 | Chronic kidney disease, stage 5 | 10.3 |
| 4 | A099 | Gastroenteritis and colitis of unspecified origin | 10.3 |
| 5 | A419 | Septicemia, unspecified | 10.3 |
| January 2020-December 2021 | |||
| 1 | R104 | Other and unspecified abdominal pain | 23.7 |
| 2 | N390 | Urinary tract infection, site not specified | 10.5 |
| 3 | A419 | Septicemia, unspecified | 7.9 |
| 4 | A099 | Gastroenteritis and colitis of unspecified origin | 5.3 |
| 5 | R074 | Chest pain, unspecified | 5.3 |
The admission rate in the COVID-19 period significantly decreased during the study period, compared with the control period (38.2% vs 65.9%; P = 0.02). In addition, the rate of any ED visit leading to hospital admission in the following year was also not different (HR = 0.92, 95%CI: 0.50-1.69; P = 0.78, Table 3).
In this retrospective study of KT patients, about one-sixth of KT recipients had at least 1 ED visit in the 1st year following transplantation. However, the rates of ED visits and hospital admissions were not affected by the impact of the COVID-19 pandemic. We also found that abdominal pain was responsible for most diagnoses across the COVID-19 and control periods. The impact of COVID-19 on ED visits and hospital admissions is demonstrated in several previous studies[15-17]. To the best of our knowledge, this is the first study investigating the effect of the COVID-19 pandemic on ED visits and admission rates among KT patients. KT recipients are usually advised to isolate themselves from the community because of the greater risk of being infected. Consequently, they might not visit the ED promptly. Our previous study showed that an average daily ED visit was significantly reduced during the COVID-19 pandemic, probably due to the fear of reaching COVID-19 in the hospital[15]. However, the present findings showed the difference. Despite the fear of contacting COVID-19, we found that ED visits by post-KT patients were not disturbed. A previous study demonstrated that KT recipients had a higher chance of a more severe course of COVID-19 infection than hemodialysis patients[18]; however, another finding showed that the severity and adverse outcomes were not different between KT recipients and those without for the COVID-19 infection[19].
Recently, telemedicine has become one of the most powerful strategies used to follow-up KT recipients[18,19]. Results from Yadav and Singh’s study found that application of telemedicine in the transplant population enhances medication compliance, reduces hospitalization rates, and makes living donor evaluation convenient[19]. Telemedicine could be recommended as an alternative method, especially in the pandemic era, to avoid and reduce the rate of transmission in the hospital in KT population.
Although ED visits are not different between the two groups in our study, hospital admissions were higher for the COVID-19 group. This may reflect the natural consequence of inappropriate and untimely ED visits, resulting in a higher severity of diseases. We proposed that the reasons for these findings could be multifactorial. First, KT patients have a higher baseline chance of visiting ED than other patients. Previous studies have shown that acute care utilization in the following year after KT is relatively high[4,7,9]. In one retrospective study conducted in the United States, nearly half of KT patients visited the ED within 1 year after KT[7]. Second, post-KT recipients are prescribed immunosuppressive agents. Usually, they are informed to seek medical evaluation even they have minor symptoms, such as low-grade fever or abdominal pain. Furthermore, fever and other unspecified symptoms could be one of the clinical features of COVID-19[20]. KT recipients might intend to visit ED as they considered themselves suspected of having this COVID-19 infection. Interestingly, our study found that hospital admissions were markedly increased in the COVID-19 group. Consistent with previous evidence, hospital admission during this disastrous period is likely higher than usual, mainly because of untimely and delayed ED visits[15].
Our findings regarding ED visits and admission rates during the COVID-19 pandemic may serve as a body of literature regarding the impact of COVID-19 in the various spectrum, including KT recipients. Not only the number of ED visits among post-KT patients were not less than the regular period, but also the admission rates were significantly high. Our data also suggest that clinicians and healthcare professionals should encourage KT recipients to visit EDs on time to reduce unfavorable outcomes.
This study had some limitations to be considered. This method could not account for underlying trends in hospital admission and ED attendance despite comparing two time periods. Differences in hospital admission patterns may be associated with the epidemic or the limits by chance. This problem might be solved with additional time series analysis or regression modeling over a longer time. We only conducted the investigation at a single university hospital. As a result, the design may be valid and generalizable to the situation with the same degree of care. Furthermore, some baseline data were not recorded, including causes of ESRD and hospital length of stay during index transplantation. Moreover, another perspective that this study did not address was the quality of life of post-KT patients who visited ED in the first following year. Further research should evaluate this aspect of the patients.
In conclusion, COVID-19 also affects KT recipients in terms of hospital admission rates. The present study points out that despite ED visits not being changed during the COVID-19 pandemic, hospital admission rates were increased. Although we could not determine the exact cause of this change, we believe that communication between post-KT patients and healthcare providers is necessary to emphasize the importance of timely ED visits for acute health conditions, especially in immunocompromised hosts like post-KT patients.
Several investigations have shown that the coronavirus disease 2019 (COVID-19) has an impact on daily life and the healthcare system.
There has been no previous research on the effects of COVID-19 on emergency department (ED) visits and hospitalizations among kidney transplant (KT) patients. We conducted this study to explore the effects of COVID-19 on ED visits among post-KT recipients.
The aim of this study was to investigate the impact of the COVID-19 pandemic on the ED visits and hospital admissions within 1 year in patients who underwent KT in Thailand.
We conducted a retrospective study. We reviewed hospital records of KT patients who visited ED during the outbreak of COVID-19. We used the previous 2 years as the control period in the analysis. We obtained baseline demographics and ED visit characteristics of each KT patient. The outcomes of interest were ED visits and ED visits leading to hospital admission within the 1st year following a KT.
We included a total of 263 patients: 112 during the COVID-19 period and 151 during the control period. There were 34 and 41 ED visits after KT in the COVID-19 and control periods, respectively. The rate of first ED visit at 1 year was not significantly different in the COVID-19 period, compared with the control period. The hospital admission rate was also similar between periods.
The COVID-19 pandemic had no effect on KT recipients’ ED visits or hospital admissions in the 1st year after transplantations.
Despite these findings, we suggest that communication between post-KT patients and healthcare professionals is crucial in emphasizing the significance of timely ED visits for acute health issues, especially in post-KT patients.
| 1. | Agency for Healthcare Research and Quality. Statistical Brief. [cited 1 January 2022]. Available from: https://www.hcup-us.ahrq.gov/reports/statbriefs/statbriefs.jsp. |
| 2. | Burke RE, Juarez-Colunga E, Levy C, Prochazka AV, Coleman EA, Ginde AA. Patient and Hospitalization Characteristics Associated With Increased Postacute Care Facility Discharges From US Hospitals. Med Care. 2015;53:492-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 76] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 3. | Burke RE, Juarez-Colunga E, Levy C, Prochazka AV, Coleman EA, Ginde AA. Rise of post-acute care facilities as a discharge destination of US hospitalizations. JAMA Intern Med. 2015;175:295-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 104] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 4. | Schold JD, Elfadawy N, Buccini LD, Goldfarb DA, Flechner SM, P Phelan M, Poggio ED. Emergency Department Visits after Kidney Transplantation. Clin J Am Soc Nephrol. 2016;11:674-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Vashi AA, Fox JP, Carr BG, D'Onofrio G, Pines JM, Ross JS, Gross CP. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA. 2013;309:364-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 154] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 6. | CMS. 2013 Edition. [cited 1 January 2022]. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/CMS-Statistics-Reference-Booklet/2013. |
| 7. | Lovasik BP, Zhang R, Hockenberry JM, Schrager JD, Pastan SO, Adams AB, Mohan S, Larsen CP, Patzer RE. Emergency department use among kidney transplant recipients in the United States. Am J Transplant. 2018;18:868-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Tonelli M, Wiebe N, Knoll G, Bello A, Browne S, Jadhav D, Klarenbach S, Gill J. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 2011;11:2093-2109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 896] [Cited by in RCA: 1160] [Article Influence: 77.3] [Reference Citation Analysis (0)] |
| 9. | Weeda ER, Su Z, Taber DJ, Bian J, Morinelli TA, Pilch NA, Mauldin PD, DuBay DA. Hospital admissions and emergency department visits among kidney transplant recipients. Clin Transplant. 2019;33:e13522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Sarier M, Demir M, Goktas S, Duman I, Buyukkinaci M, Yuksel Y, Tekin S, Yavuz AH, Sengul A. Results of Real-time Multiplex Polymerase Chain Reaction Assay in Renal Transplant Recipients With Sterile Pyuria. Transplant Proc. 2017;49:1307-1311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Hollisaaz MT, Aghanassir M, Lorgard-Dezfuli-Nezad M, Assari S, Hafezie R, Ebrahiminia M. Medical comorbidities after renal transplantation. Transplant Proc. 2007;39:1048-1050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Wu C, Evans I, Joseph R, Shapiro R, Tan H, Basu A, Smetanka C, Khan A, McCauley J, Unruh M. Comorbid conditions in kidney transplantation: association with graft and patient survival. J Am Soc Nephrol. 2005;16:3437-3444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 130] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 13. | Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470-473. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4848] [Cited by in RCA: 4441] [Article Influence: 740.2] [Reference Citation Analysis (1)] |
| 14. | De Pasquale C, Pistorio ML, Veroux P, Gioco R, Giaquinta A, Privitera F, Veroux M. Quality of Life and Mental Health in Kidney Transplant Recipients During the COVID-19 Pandemic. Front Psychiatry. 2021;12:645549. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 15. | Mirjalili M, Shafiekhani M, Vazin A. Coronavirus Disease 2019 (COVID-19) and Transplantation: Pharmacotherapeutic Management of Immunosuppression Regimen. Ther Clin Risk Manag. 2020;16:617-629. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 16. | Wongtanasarasin W, Srisawang T, Yothiya W, Phinyo P. Impact of national lockdown towards emergency department visits and admission rates during the COVID-19 pandemic in Thailand: A hospital-based study. Emerg Med Australas. 2021;33:316-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (1)] |
| 17. | Kelly PJ, Lim LL. Survival analysis for recurrent event data: an application to childhood infectious diseases. Stat Med. 2000;19:13-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 18. | Biancone L, Minetti E, De Rosa P, Rigotti P, Stallone G, Volpe M, Citterio F. Telemedicine monitoring in the follow-up of kidney transplant recipients: consensus indications from an Italian panel of surgeons and nephrologists after the COVID-19 experience. J Nephrol. 2022;35:725-733. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Yadav A, Singh P. Telehealth Use by Living Kidney Donor Transplant Programs During the COVID-19 Pandemic and Beyond: a Practical Approach. Curr Transplant Rep. 2021;8:257-262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Esakandari H, Nabi-Afjadi M, Fakkari-Afjadi J, Farahmandian N, Miresmaeili SM, Bahreini E. A comprehensive review of COVID-19 characteristics. Biol Proced Online. 2020;22:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 280] [Cited by in RCA: 270] [Article Influence: 45.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Transplantation
Country/Territory of origin: Thailand
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Eccher A, Italy; Sarier M, Turkey S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Wang JJ