Published online Jul 18, 2022. doi: 10.5500/wjt.v12.i7.175
Peer-review started: December 29, 2021
First decision: April 19, 2022
Revised: April 20, 2022
Accepted: June 18, 2022
Article in press: June 18, 2022
Published online: July 18, 2022
Processing time: 197 Days and 16.8 Hours
Reconstructive surgery of the eyelid after tumor excision, trauma or other causes can be challenging, especially due to the complexities of the anatomic structures and to the necessity of both functional and aesthetic successful outcomes. The aim of this minireview was to investigate the use of tissue transplantation in eyelid reconstruction. Surgical procedures are various, based on the use of both flaps, pedicled or free, and grafts, in order to guarantee adequate tissue reconstruction and blood supply, which are necessary for correct healing. Common techniques normally include the use of local tissues, combining non-vascularized grafts with a vascularized flap for the two lamellae repair, to attempt a reconstruction similar to the original anatomy. When defects are too wide, vast, deep, and complex or when no adjacent healthy tissues are available, distant area tissues need to be recruited as free flaps or grafts and paired with mucosal layer reconstruction. With regards to the anterior lamella, full thickness skin grafts are commonly preferred. With regards to the reconstruction of posterior lamella, there are different graft options, which include conjunctival or tarsoconjunctival, mucosal or palatal or cartilaginous grafts usually combined with local flaps. Free flap transplantation, normally reserved for rare select cases, include the use of the radial forearm and anterolateral flaps combined with mucosal grafts, which are surgical options currently reported in the literature.
Core Tip: Transplantation tends to be a viable option in eyelid reconstruction surgery. The most commonly used technique involves the use of grafts for the reconstruction of one or both eyelid structures. The use of free flaps are seldom used and are reserved for cases of extensive tissue lost. In these cases, favorable flaps considered are those that are anatomically thin and pliable.
- Citation: Miotti G, Zeppieri M, Rodda A, Salati C, Parodi PC. How and when of eyelid reconstruction using autologous transplantation. World J Transplant 2022; 12(7): 175-183
- URL: https://www.wjgnet.com/2220-3230/full/v12/i7/175.htm
- DOI: https://dx.doi.org/10.5500/wjt.v12.i7.175
Eyelid reconstruction tends to be complex and difficult and can be needed after oncological surgery or trauma. There are also cases, which are not frequent, in which reconstructive surgery is needed to repair damage caused by aesthetic surgery, such as lagophthalmos post-blepharoplasty or scarring eyelid retraction. In patients with invasive and relatively large eyelid tumors, the need to perform complete oncologic excision with margins adapted to tumor type may result in the removal of an important part of this anatomical structure that encompasses both aesthetic and functional properties[1].
The eyelid consists of an anterior and posterior lamella. The anterior portion of the lid is composed of skin and orbicularis muscles, while the posterior portion includes the posterior tarsal plate, retractors (in the lower eyelid), and conjunctiva[2]. In most eyelid reconstruction surgical procedures, both lamellae need to be replaced. At least one lamella needs to include a functioning blood supply and therefore has to be pediculated, otherwise the reconstructed tissue cannot properly grow and heal, resulting in poor and/or no wound closure[3].
Several surgical techniques are currently available for lower eyelid reconstruction; the choice of the technique and postoperative results mainly depend on the preference and experience of the surgeon and on the etiology of the eyelid defect. Most surgical techniques combine different flaps and grafts in order to reconstruct both lamellae. The most commonly used reconstructive techniques are based on local flaps, which are widely described in the literature[4-6], and possible grafts to complete lid reconstruction. The main objectives of surgery include obtaining postsurgical outcomes that reflect the normal eyelid in terms of anatomy, aesthetics, and function. The aim of our minireview was to present a brief overview of reconstructive techniques based on autologous tissue transplantation for eyelid reconstruction surgery, including the use of grafts and/or free flaps, which have been reported in the literature in the past 10 years.
We conducted a search of the literature published between January 1, 2011 to November 1, 2021 using MEDLINE (PubMed). The database was first searched using the key words “eyelid reconstruction, eyelid reconstruction AND grafts, free flaps, tissue transplantation, autologous grafts, autologous tissues”. We considered only studies in English and those referring to humans and with an abstract, thus reducing the count to 1473 papers. The reference lists of all retrieved articles were assessed to identify additional relevant studies. The research of articles was preformed using PubMed (https://pubmed.ncbi.nlm.nih.gov) and Reference Citation Analysis (https://www.referencecitation
Only articles with an abstract were considered. After excluding all works in which only local flaps were used for reconstruction, 63 studies were analyzed. A quality score was calculated for each article using a check list from the American Society of Plastic Surgeons guideline for therapeutic studies[7]. Each study was independently assessed by at least two reviewers (Miotti G and Zeppieri M), and rating decisions were based on the consensus of the reviewing authors. The results of the most relevant studies are shown in Table 1.
| What | Where | Type of tissue transplant | Ref. | Conclusions |
| Grafts | Bilamellar reconstruction | Skin graft + tarsoconjunctival graft with orbicularis oculi muscle advancement | Doxanas[11], 1986; Kakizaki et al[10], 2009 | Orbital part muscle mobilization allows full thickness eyelid reconstruction using two grafts due to its vascular support |
| Skin graft + tarsal graft | Bortz et al[12], 2020 | Reconstruction of lower eyelid defects with a free tarsal graft and overlying free skin graft resulted in an acceptable functional and aesthetic lower eyelid suggesting that retention of or provision of vascular support in either the anterior or posterior lamella may not be necessary | ||
| Anterior lamella | Skin graft | Alghoul et al[9], 2013 | Anterior lamellar defects can be reconstructed with a full-thickness skin graft. Split-thickness skin grafts should not be used | |
| Skin graft | Shorr et al[14], 2003 | Upper eyelid skin grafting can be performed with good cosmetic results to address corneal decompensation in patients who have acquired lagophthalmos from anterior lamellar insufficiency | ||
| Posterior lamella | Tarsoconjunctival graft | Hawes et al[17], 2011 | Essential component of eyelid reconstruction as it provides an anatomically similar tissue for the inner layer of reconstructed eyelids. Patients receiving a free tarsoconjunctival graft were less likely to require surgery to repair eyelid margin erythema than those receiving a Hughes tarsoconjunctival flap | |
| Yazici et al[23], 2020 | Lateral periorbital bilobed flap with tarsoconjunctival graft can be a good alternative for the single-stage reconstruction of large upper eyelid defects | |||
| Bengoa-González et al[24], 2019 | Reconstruction of upper eyelid defects secondary to malignant tumors with a newly modified Cutler-Beard technique with tarsoconjunctival graft gives stability to the new upper eyelid, avoiding retraction caused by scarring | |||
| Hard-palate mucoperiosteal | Yue et al[26], 2020; Ito et al[27], 2007 | HPM may be considered the optimal choice for reconstructing the posterior lamella of the eyelids because it has similar histological composition and texture to the tarsoconjunctiva | ||
| Hendriks et al[28], 2020 | The use in upper eyelid reconstruction is controversial because hard-palate mucosa is composed of keratinized, stratified squamous epithelium, which can irritate the cornea. Despite this, excellent results were reported for its use in upper eyelid posterior lamellar reconstruction | |||
| Chondromucosal graft | Yamamoto et al[33], 2017 | Ear cartilage is useful because it is easy to harvest and fabricate, has suitable flexibility, and provides adequate support. Chondromucosal grafts from the nasal septum consist of highly supportable tissue. It lacks softness and flexibility, and harvesting is limited | ||
| Suga et al[34], 2016 | Ear cartilage fits well to bulbar surface. It has lower complication rate, while in the nose septal perforation and more bleeding can occur | |||
| Hendriks et al[28], 2020 | The use of alar or triangular cartilage provides a thinner but smaller sized sample, with good adaptability in eyelid reconstruction but raised the problem of donor site morbidity | |||
| Scapha chondrocutaneous graft | Uemura et al[36], 2016 | The scapha cartilage graft with small skin, round and soft with a shape similar to that of the lower lid, affords a good fit to the eye globe | ||
| Dermis fat graft | Kuzmanović Elabjer et al[39], 2018 | Provides stiffness, additional surface area, and a scaffold. Helps with vascularization and decreases fat tissue atrophy. It can be flat or domed | ||
| Venous graft | Barbera et al[40], 2008 | VGs obtained by propulsive venous vessels are the most suitable for this reconstruction because of their thinness, texture, and anatomical structure | ||
| Tomassini et al[41], 2012 | By properties of elasticity, smoothness, and concavity, the VG conforms to the globe without inducing a chronic inflammatory reaction on the bulbar conjunctiva or on the cornea | |||
| Scevola et al[42], 2015 | Safe, fast, and easily reproducible compared with chondroseptal graft | |||
| Galea or pericranium graft | Ibáñez-Flores et al[43], 2019 | Pericranial graft provides enough tissue to cover large defects, with an appropriate volume and a non-painful postoperative period | ||
| Buccal mucosa graft | Grixti and Malhotra[44], 2018; Jin and Cao[45], 2021 | It lacks structural integrity. It is too weak and small to support the lower eyelid, shrinking substantially during the postoperative period, so it should be used in combination with cartilage | ||
| Flaps | Bilamellar reconstruction | Neurovascular free flap from the first web space of the foot | Chait et al[46], 1980 | |
| Free flap based on the second metacarpal artery | Yap et al[47], 1997 | |||
| Free dorsalis pedis flap | Thai et al[48], 1999 | Free flap used for outer lamella and conjunctival flap for inner lamella | ||
| Free forearm flap | Kushima et al[49], 2003 | Entire upper eyelid reconstruction and a hard palate graft for the posterior one | ||
| Ghadiali et al[50], 2016 | Upper and lower eyelid total reconstruction where an extensive tissue loss of the ipsilateral forehead and temple. Tarsal plate of the eyelids was rebuilt by palmaris tenon grafts | |||
| Iwanaga et al[51], 2019 | 2 cases of functional upper eyelid defect reconstruction. They used a free flap elevated with palmaris longus tenon split into two strips: One fixed to the frontalis muscle to achieve the opening function and the second to the medial palpebral ligament and the lateral orbicularis muscle to achieve the closing function | |||
| ALT flap | Rubino et al[52], 2008 | Upper and lower eyelid unilateral full thickness reconstruction with ALT free flap in a patient with no available adjacent tissues, involved in extended burns, and no possibility of using RFF |
The particular eyelid anatomy must always be considered when reconstructing it. In doing so, we must always remember the presence of two lamellae that constitute the two eyelids. Full thickness defects larger than a third of the eyelid should be reconstructed in two planes, which correspond to the posterior and anterior lamellae. In order to avoid necrosis of the reconstruction, at least one lamella should have an intact blood supply. The association of two grafts is therefore not recommended. The two planes must thus consist of the association of either two flaps or a flap and a graft[1]. Most studies reported in the literature follow this common idea; however, some authors have also proposed the use of only grafts.
The association of two flaps is the safest combination regarding vascular supply and postoperative recovery. However, the use of two flaps can lead to a thick reconstructed eyelid, which can be limited if each flap is comprised exclusively of the exact missing layer. For this reason, the use of a flap and a graft is the best option for satisfactory aesthetic result. The final choice of the surgical technique depends on several factors, which include the preference and experience of the surgeon, etiology of the eyelid defect, and the availability of flaps and grafts[8]. The quality of local tissues can also modify this choice. History of radiotherapy, previous or planned in the postoperative period, can guide the reconstruction. By determining a reduction of the vascularization of the treated tissues, well vascularized tissue are preferred to repair the defects[3,5]. Local flaps certainly represent a common reconstructive choice and are preferable to grafts, especially for previously irradiated sites. The aim of our study, however, was to assess a narrower and more specific field of literature, to concentrate on studies regarding eyelid reconstruction surgery based on tissue transplantation, to include grafts or free flaps.
Graft transplantation in eyelid reconstruction is perhaps the most commonly used procedure in routine clinical settings. Various tissues can be transplanted to complete the eyelid reconstruction. Both lamellae can be restored with grafts; however, the anterior lamella is the most common segment that tends to be repaired. As a basic rule, grafts should be used when there is an adequate vascular bed to enhance post-transplanted survival. Grafts can also be used in irradiated tissues when needed; however, these types of grafts generally need to be associated with local flaps to enhance the vascularization and guarantee graft survival. Radiotherapy on engrafted areas could cause ulceration or delay the wound healing[9]. Commonly used techniques combine a non-vascularized graft for one lamella with a vascularized flap for the other[9].
As mentioned above, usually only one lamella can be reconstructed with a graft, but techniques to reconstruct both have also been described. Kakizaki et al[10] reported bilamellar graft reconstruction with orbicularis muscle mobilization between grafted areas (“sandwich flap”), first described by Doxanas[11] in 1986. The orbicularis oculi muscle provides an excellent blood supply to grafted tissues in these cases, in addition to enhancing the mobility of the reconstructed lid. In 2020, Bortz et al[12] published a clinical series in which full-thickness lid defects were restored using free tarsal grafts for the posterior lamella and free skin grafts for the anterior lamella. The authors reported this method as an alternative to the “classic” Hughes flap for lower eyelid reconstruction, especially when the occlusion of the eye could be a problem (vision deficit, elderly patients, etc). The evidence reported by Tenland et al[13] led the authors to propose this type of reconstruction. The study showed that tarsoconjunctival (TC) tissue survival does not seem to be dependent on a conjunctival flap, and thus free TC grafts or composite grafts might be considered as viable alternatives.
Anterior lamella is often reconstructed with a full-thickness skin graft[10-14]. Other possibilities of tissue transplantation include tissue cultured autograft, tissue cultured allograft, skin bank allograft, acellular dermal replacement, and xenograft[15]. Ideal donor sites include upper and lower eyelid skin and posterior auricular, preauricular, or supraclavicular skin. Split-thickness skin grafts should not be used, with the exception of cases of extensive burns in which the donor site is limited[9].
Grafts or flaps are viable options for posterior lamellar reconstruction[10]. Grafts include conjunctival or TC grafts, hard palate (or palate) graft, cartilage (auricular or nasal septal) grafts, mucoperichondrium grafts, dermis fat grafts (DFGs), venous grafts (VGs), galea or pericranium grafts, mucosal membrane (buccal or labial) grafts, and temporalis fascia grafts. For lower eyelid reconstruction, for example, single or tandem composite skin muscle TC eyelid grafts from the upper lids or contralateral lower lid may be an option[10].
TC grafts: TC grafts are an excellent choice for posterior lamellar reconstruction considering that this structure reflects the features of a normal eyelid[9]. Tarsal grafts alone, taken from the healthy eyelid, can be used in association with local flaps for anterior lamella reconstruction[16]. TC grafts and flaps are essential components of eyelid reconstruction since these alternatives provide anatomically similar tissues for the inner layer of reconstructed eyelids[17]. First described in 1918 by Blaskovics[18] for lower eyelid reconstruction, autogenous TC grafts have found widespread use, as described by Hughes[19], Leone et al[20], and several others in the literature[21,22]. Hawes et al[17] proposed guidelines for the use of TC flaps and grafts to repair lower eyelid defects.
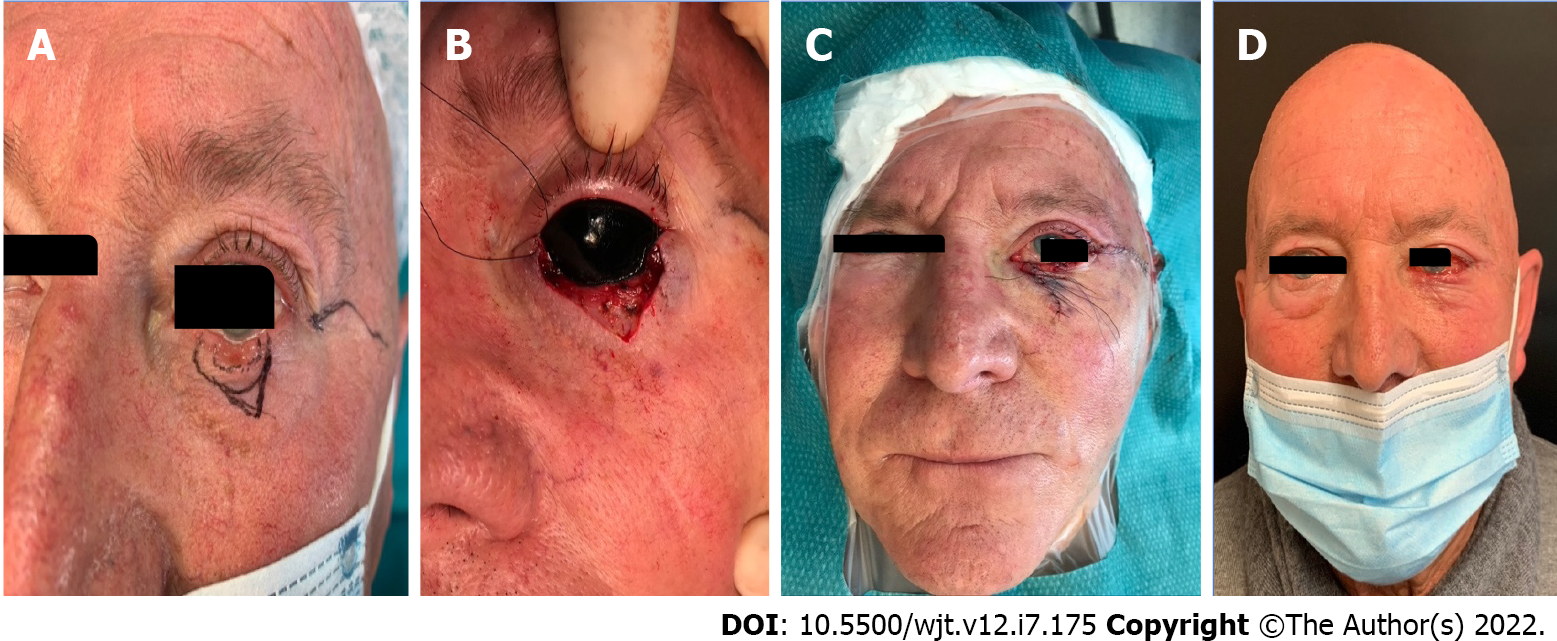
Free grafts are preferred in most cases in which the defect is from one-third to three-quarters of the eyelid length. TC flaps are advantageous when the defects are large (entire lower eyelid loss) and when poor healing can be expected. Usually, this type of reconstruction is completed by a local flap for the anterior lamella and is not limited only to the lower eyelid. Yazici et al[23] recently described the association of a TC graft with a bilobed local flap for the upper eyelid. Bengoa-González et al[24] described the use of the graft to complete and modify the Cutler-Beard technique for the upper eyelid. The TC graft gives stability to the new upper eyelid, avoiding retraction caused by scarring. From a technical point of view, it is fundamental to also avoid complications in the donor site, which usually heals spontaneously by secondary intention[9]. Almost 3-4 mm of tarsus must be maintained to allow donor eyelid stability, and Müller’s muscle should be conserved. To avoid entropion or ectropion to reconstructed eyelid, the tarsal graft should be snug and no wider than the smallest dimension of the defect[17]. Figure 1 shows an example of our patient that underwent left lower eyelid reconstruction after tumor excision using a TC graft (from the left upper eyelid) for the posterior lamella and a local flap for the anterior one.
Hard-palate mucoperiosteal grafts: Hard-palate mucoperiosteal (HPM) grafts, described for the first time by Siegel[25] in 1985, can be used to replace the posterior lamella due to the ability of this graft to provide structural support and mucosal lining[9]. HPM may be considered the optimal choice for reconstructing the posterior lamella of the eyelids because it has similar histological composition and texture to the tarsoconjunctiva, and an adequately sized graft can easily be acquired[26,27]. HPM tends to be one of the preferred choices for most lower eyelid reconstructions in routine clinical settings[26]. The use of HPM in upper eyelid reconstruction is controversial because hard-palate mucosa is composed of keratinized, stratified squamous epithelium, which can irritate the cornea, especially when the defect is adjacent to the middle part of the cornea[9,28]. Despite this, excellent results without complications have been reported in studies when used in upper eyelid posterior lamellar reconstruction[28,29].
The reconstruction of the anterior lamella requires the use of flaps. Palatal mucosal grafts provide good structural support to the eyelid. This is essential for the inferior eyelid, especially when the graft is combined with a heavy flap such as the Mustardé or the orbito-nasogenien flap. The graft is and remains stiff. The shrinkage is minimal, thus providing a stable, free eyelid margin and limiting ectropion or entropion[28]. Limits of this technique, in addition to the aforementioned corneal irritation, are the described pain and delayed healing at the donor site observed when periosteum is included in the graft[30].
Auricular and nasoseptal cartilage grafts: Auricular and nasoseptal cartilage can also be useful alternatives when considering graft tissues for reconstructive surgery[28,31,32]. In some cases, this graft may prove to be too thick and too stiff to match with the eye convexity, thus needing to be thinned without compromising the supportive strength. Ear cartilage is useful because it is easy to harvest and fabricate, has suitable flexibility, and provides adequate support[33]. The spherical surface fits well with the shape of the external bulbar surface[34]. Chondromucosal grafts from the nasal septum consist of highly supportable tissue. Caution must be taken when harvesting a chondroseptal graft to avoid damage to the remaining mucosa surrounding the vast perforation. Considering this tissue is composed of hyaline cartilage, it lacks softness and flexibility. This may result in difficulty with fabrication and unsuitable contact with the bulbar conjunctiva. In addition, the harvestable size is limited[33]. The use of alar or triangular cartilage provides a thinner but smaller sized sample, with good adaptability in eyelid reconstruction but raises the problem of donor site morbidity[28]. Suga et al[34] published in 2016 a comparison between ear and nasal septum grafts. The study reported that both tissues provide good options for reconstructing an inner layer of the lower eyelid. The authors stressed that the main difference lies on postoperative outcomes at the donor site. Ear cartilage tends to have lower complication rates, while harvesting nose grafts can cause important septal perforation and vast bleeding.
Another option for cartilaginous reconstruction of the posterior lamella of the lower eyelid is a scapha chondrocutaneous graft, first proposed by Yanaga and Mori[35]. Further studies reported by Uemura et al[36] described interesting results with the use of this graft combined with a local propeller flap. The scapha cartilage graft is an interesting alternative because it has a thin coat of skin and is round and soft with a shape similar to that of the lower lid. This tissue can provide a good fit with the eye globe and can be harvested quickly without severe complications.
DFGs: DFGs can provide useful replacement tissue for eyelid and orbit reconstruction. The DFG is composed of a dermis button, obtained by removing the overlying epidermis with the underlying subcutaneous fat. The dermis provides stiffness, additional surface area, and a scaffold. Moreover, the dermis helps with vascularization and decreases fat tissue atrophy. This tissue can be flat or domed shaped[37]. This graft option tends to be considered primarily for socket reconstruction in the context of anophthalmia, either congenital or acquired[38]. Secondary indications are eyelid reconstruction, socket contraction, eyelid contraction (used as spacer[39]), or implant exposure.
VGs: Barbera et al[40] first proposed VGs as a reconstructive possibility in 2008. The study reported that VGs obtained by propulsive venous vessels are the most suitable for this type of surgical reconstruction because of the tissue thinness, texture, and anatomical structure. Moreover, due to the properties of elasticity, smoothness, and concavity, the venous graft conforms to the globe without inducing a chronic inflammatory reaction on the bulbar conjunctiva or on the cornea[41]. Scevola et al[42] showed that VG is a good technique for palpebral reconstruction because it is safe, fast, and easily reproducible when compared with a chondroseptal graft.
Galea and pericranium grafts: Galea and pericranium grafts represent a secondary choice in eyelid reconstruction. These tissues represent a reconstructive possibility in cases of severe periocular trauma, wide tumor resections, or in socket reconstruction[35]. Ibáñez-Flores et al[43] published a series of cases in which pericranium grafts were used. The authors concluded that pericranial grafts provided a sufficient amount of tissue to cover large defects, thus providing appropriate substitutional volume without painful postoperative healing.
Buccal mucosa graft: Buccal mucosa graft is a good lining option[9]. Oral mucosa has similar biological properties to conjunctiva, thus making it a viable alternative to restore the ocular surface[44]. This tissue, however, lacks structural integrity and tends to be too weak and small to support the lower eyelid. Moreover, postoperative shrinking can be substantial during the follow-up period, thus it should be used in combination with cartilage[43,45]. It is important to note that buccal mucosa graft harvesting and postoperative healing tend to be rather painful for most patients.
When defects are too complex to be reconstructed with local flaps or grafts or when no adjacent tissues are available, the operation is challenging, and transplantation of tissues from distant areas is necessary. Mechanical support and mobility for reconstructive surgery can seldom be found in tissues from a distant region, combining thin and pliable skin with mucosal layer reconstruction. The flap needs to provide characteristics that are appropriate both from a functional and an aesthetic prospective. Free flaps are normally not frequently considered in reconstructive surgery. In addition, reconstructions with free flaps have several possible complications. The effect of possible radiotherapy on the recipient site (which is frequent in advanced tumors) is one of the elements that can determine the failure of autologous microsurgical reconstruction. The harmful effects on tissues and blood vessels are well known. There are only a few studies reported in the literature that are based on this surgical option for complete or partial eyelid reconstruction.
One of the first attempts of periocular region reconstruction using free flaps was described by Chait et al[46] who used a neurovascular free flap from the first web space of the foot after exenteration. An alternative distant surgical flap was described in a case report by Yap et al[47] in 1997 in which the eyelids were rebuilt using a free flap based on the second metacarpal artery. Thai et al[48] proposed a free dorsalis pedis flap for the outer lamella and a local conjunctival flap for the inner one for total eyelid surgical reconstruction after deep facial burn in a study published in 1999.
One of the main problems in periocular region reconstruction is represented by the extreme thinness of the tissues that compose it. This represents a limit for the reconstructive techniques due to the thickness of the tissues generally used to cover the defects. This limit is highlighted when the reconstructive choice is a free flap. For this reason, it is quite difficult to find a viable flap that can provide satisfactory surgical reconstruction outcomes. Kushima et al[49] described an entire upper eyelid reconstruction using a free radial forearm flap for the anterior lamella and a hard palate graft for the posterior one. This flap, thanks to its flexibility and thinness, is considered the ideal solution.
The same flap has been used by Ghadiali et al[50] in a case of upper and lower eyelid total reconstruction in which the patient had extensive tissue loss of the ipsilateral forehead and temple. In this specific case, there were no local tissues available for reconstruction. The authors used a 5 cm × 11 cm radial flap to reconstruct the entire area, followed by a fenestration of the flap 4 mo later. The tarsal plate of the eyelids was rebuilt by palmaris tenon grafts. As a result, the patient obtained a visually useful eye, which remained intact after the trauma[50]. Radial forearm flap was also used by Iwanaga et al[51] in 2 cases of functional upper eyelid defect reconstruction surgeries. The authors used a free flap elevated with palmaris longus tenon in a fascinating way. The palmaris longus tenon was split into two strips, in which one strip was fixed to the frontalis muscle to achieve the opening function and the second to the medial palpebral ligament and the lateral orbicularis muscle to achieve functioning closing lids.
Another feasible free flap, especially in thin or super-thin forms, is the anterolateral flap. In 2008, Rubino et al[52] described a case of upper and lower eyelid unilateral full thickness reconstruction with anterolateral free flap in a patient with no available adjacent tissues, who had extensive burns and no possibility of using a radial forearm flap. In this patient, the blepharoraphy was opened after 3 mo from the first surgery, obtaining good skin coverage but incomplete closure of the eye.
Eyelid reconstruction remains extremely complex and fascinating, especially considering that the main aims of surgery include re-establishing the anatomy, providing protection of the eye globe, favoring the sight, and guaranteeing the aesthetics of the face. It is clear that each surgical procedure requires experience, careful planning, and personalized surgical options tailored for each patient. From the analysis of the current literature in this field, it appears significantly advantageous to exploit periocular tissues when possible. However, other options including non-traditional flaps and grafts can prove to be viable alternatives in specific cases, especially when there is extensive damage to the lids and/or neighboring tissues are scarce and not feasible options. Stem cell harvesting and new transplanted autologous tissues can pave the way to future surgical techniques in reconstructive lid surgery.
| 1. | Lemaître S, Lévy-Gabriel C, Desjardins L, González-Candial M, Gardrat S, Dendale R, Cassoux N, Couturaud B. Outcomes after surgical resection of lower eyelid tumors and reconstruction using a nasal chondromucosal graft and an upper eyelid myocutaneous flap. J Fr Ophtalmol. 2018;41:412-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (1)] |
| 2. | Pfeiffer MJ. Update on upper lid blepharoplasty. Oculoplastics Orbit. 2006;123-42. [DOI] [Full Text] |
| 3. | Frimmel S, Kniestedt C, Chaloupka K. Eyelid Reconstruction: Pediculated versus Non-Pediculated. Klin Monbl Augenheilkd. 2018;235:398-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Hughes WL. Total lower lid reconstruction: technical details. Trans Am Ophthalmol Soc. 1976;74:321-329. [PubMed] |
| 5. | Tenzel RR, Stewart WB. Eyelid reconstruction by the semicircle flap technique. Ophthalmology. 1978;85:1164-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 110] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Mustardé JC. The use of flaps in the orbital region. Plast Reconstr Surg. 1970;45:146-150. [PubMed] |
| 7. | DePalma JA. Evidence-based clinical practice guidelines. Semin Perioper Nurs. 2000;9:115-120. [PubMed] |
| 8. | Karim A, Schapiro D, Morax S. [Reconstruction of full-thickness lower eyelid defects]. J Fr Ophtalmol. 2005;28:675-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Alghoul M, Pacella SJ, McClellan WT, Codner MA. Eyelid reconstruction. Plast Reconstr Surg. 2013;132:288e-302e. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Kakizaki H, Madge SN, Mannor G, Selva D, Malhotra R. Oculoplastic surgery for lower eyelid reconstruction after periocular cutaneous carcinoma. Int Ophthalmol Clin. 2009;49:143-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Doxanas MT. Orbicularis muscle mobilization in eyelid reconstruction. Arch Ophthalmol. 1986;104:910-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Bortz JG, Al-Shweiki S. Free Tarsal Graft and Free Skin Graft for Lower Eyelid Reconstruction. Ophthalmic Plast Reconstr Surg. 2020;36:605-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Tenland K, Memarzadeh K, Berggren J, Nguyen CD, Dahlstrand U, Hult J, Engelsberg K, Lindstedt S, Sheikh R, Malmsjö M. Perfusion Monitoring Shows Minimal Blood Flow From the Flap Pedicle to the Tarsoconjunctival Flap. Ophthalmic Plast Reconstr Surg. 2019;35:346-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 14. | Shorr N, Goldberg RA, McCann JD, Hoenig JA, Li TG. Upper eyelid skin grafting: an effective treatment for lagophthalmos following blepharoplasty. Plast Reconstr Surg. 2003;112:1444-1448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Merriam JC. A Manual of Systematic Eyelid Surgery. Arch Ophthalmology. 1991;109:929. [DOI] [Full Text] |
| 16. | Toft PB. Reconstruction of large upper eyelid defects with a free tarsal plate graft and a myocutaneous pedicle flap plus a free skin graft. Orbit. 2016;35:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Hawes MJ, Grove AS Jr, Hink EM. Comparison of free tarsoconjunctival grafts and Hughes tarsoconjunctival grafts for lower eyelid reconstruction. Ophthalmic Plast Reconstr Surg. 2011;27:219-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 18. | Blaskovics LV. III. über Totalplastik des unteren Lides. Bildung einer hinteren Lidplatte durch Transplantation eines Tarsus- und Bindehautstreifens aus dem Oberlide. Ophthalmologica. 1918;40:222-227. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Hughes WL. Reconstructive surgery of the eyelids. Adv Ophthalmic Plast Reconstr Surg. 1986;5:25-87. [PubMed] |
| 20. | Leone CR Jr, Hand SI Jr. Reconstruction of the medial eyelid. Am J Ophthalmol. 1979;87:797-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Beyer CK, Bathrick ME. One-stage lower eyelid reconstruction. Ophthalmic Surg. 1982;13:551-554. [PubMed] |
| 22. | Hawes MJ. Free autogenous grafts in eyelid tarsoconjunctival reconstruction. Ophthalmic Surg. 1987;18:37-41. [PubMed] |
| 23. | Yazici B, Ozturker C, Cetin Efe A. Reconstruction of Large Upper Eyelid Defects With Bilobed Flap and Tarsoconjunctival Graft. Ophthalmic Plast Reconstr Surg. 2020;36:372-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Bengoa-González Á, Laslău BM, Martín-Clavijo A, Mencía-Gutiérrez E, Lago-Llinás MD. Reconstruction of Upper Eyelid Defects Secondary to Malignant Tumors with a Newly Modified Cutler-Beard Technique with Tarsoconjunctival Graft. J Ophthalmol. 2019;2019:6838415. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Siegel RJ. Palatal grafts for eyelid reconstruction. Plast Reconstr Surg. 1985;76:411-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 124] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 26. | Yue H, Tian L, Bi Y, Qian J. Hard Palate Mucoperiosteal Transplantation for Defects of the Upper Eyelid: A Pilot Study and Evaluation. Ophthalmic Plast Reconstr Surg. 2020;36:469-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 27. | Ito R, Fujiwara M, Nagasako R. Hard palate mucoperiosteal graft for posterior lamellar reconstruction of the upper eyelid: histologic rationale. J Craniofac Surg. 2007;18:684-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 28. | Hendriks S, Bruant-Rodier C, Lupon E, Zink S, Bodin F, Dissaux C. The palatal mucosal graft: The adequate posterior lamellar reconstruction in extensive full-thickness eyelid reconstruction. Ann Chir Plast Esthet. 2020;65:61-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 29. | Cohen MS, Shorr N. Eyelid reconstruction with hard palate mucosa grafts. Ophthalmic Plast Reconstr Surg. 1992;8:183-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 105] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 30. | Pedlar J. Healing following full thickness excision of human palatal mucosa. Br J Plast Surg. 1985;38:347-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 31. | Mehrotra ON. Repairing defects of the lower eyelid with a free chondromucosal graft. Plast Reconstr Surg. 1977;59:689-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 17] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 32. | Parodi PC, Calligaris F, De Biasio F, De Maglio G, Miani F, Zeppieri M. Lower lid reconstruction utilizing auricular conchal chondral-perichondral tissue in patients with neoplastic lesions. Biomed Res Int. 2013;2013:837536. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 33. | Yamamoto N, Ogi H, Yanagibayashi S, Yoshida R, Takikawa M, Nishijima A, Kiyosawa T. Eyelid Reconstruction Using Oral Mucosa and Ear Cartilage Strips as Sandwich Grafting. Plast Reconstr Surg Glob Open. 2017;5:e1301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 34. | Suga H, Ozaki M, Narita K, Kurita M, Shiraishi T, Ohura N, Takushima A, Harii K. Comparison of Nasal Septum and Ear Cartilage as a Graft for Lower Eyelid Reconstruction. J Craniofac Surg. 2016;27:305-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 35. | Yanaga H, Mori S. Eyelids and eye socket reconstruction using the expanded forehead flap and scapha composite grafting. Plast Reconstr Surg. 2001;108:8-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 36. | Uemura T, Watanabe H, Masumoto K, Kikuchi M, Satake Y, Yanai T, Harada Y, Ishihara Y, Yasuta M. Aesthetic Total Reconstruction of Lower Eyelid Using Scapha Cartilage Graft on a Vascularized Propeller Flap. Plast Reconstr Surg Glob Open. 2016;4:e696. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 37. | Migliori ME, Putterman AM. The domed dermis-fat graft orbital implant. Ophthalmic Plast Reconstr Surg. 1991;7:23-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 38. | Jovanovic N, Carniciu AL, Russell WW, Jarocki A, Kahana A. Reconstruction of the Orbit and Anophthalmic Socket Using the Dermis Fat Graft: A Major Review. Ophthalmic Plast Reconstr Surg. 2020;36:529-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 39. | Kuzmanović Elabjer B, Miletić D, Bušić M, Bišćan Tvrdi A, Bosnar D, Bjeloš M. Dermis-Fat Graft for Correction of Recurrent Severe Upper Eyelid Retraction in Graves' Orbitopathy. Acta Clin Croat. 2018;57:173-176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 40. | Barbera C, Manzoni R, Dodaro L, Ferraro M, Pella P. Reconstruction of the tarsus-conjunctival layer using a venous wall graft. Ophthalmic Plast Reconstr Surg. 2008;24:352-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 41. | Tomassini GM, Ansidei V, Ricci AL, Cagini C, Cencetti F, Simonetti S, Covarelli P. Venous graft for reconstruction of neoplastic and post-traumatic eyelid defects. In Vivo. 2012;26:447-451. [PubMed] |
| 42. | Scevola A, Sanna MP, Maxia S, Esposito S, Di Giulio S, Sartore L. Venous Graft for Full-thickness Palpebral Reconstruction. Plast Reconstr Surg Glob Open. 2015;3:e344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 43. | Ibáñez-Flores N, Bruzual-Lezama C, Castellar-Cerpa JJ, Fernández-Montalvo L. Lower eyelid reconstruction with pericranium graft and Mustarde flap. Arch Soc Esp Oftalmol (Engl Ed). 2019;94:514-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 44. | Grixti A, Malhotra R. Oral mucosa grafting in periorbital reconstruction. Orbit. 2018;37:411-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 45. | Jin MJ, Gao Y. Using Buccal Mucosa and Auricular Cartilage With a Local Flap for Full-Thickness Defect of Lower Eyelid. J Craniofac Surg. 2021;32:e660-e661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 46. | Chait LA, Cort A, Braun S. Upper and lower eyelid reconstruction with a neurovascular free flap from the first web space of the foot. Br J Plast Surg. 1980;33:132-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 47. | Yap LH, Earley MJ. The free 'V': a bipennate free flap for double eyelid resurfacing based on the second dorsal metacarpal artery. Br J Plast Surg. 1997;50:280-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 48. | Thai KN, Billmire DA, Yakuboff KP. Total eyelid reconstruction with free dorsalis pedis flap after deep facial burn. Plast Reconstr Surg. 1999;104:1048-1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 49. | Kushima H, Yuzuriha S, Kondo S, Osada Y. Reconstruction of an inner layer defect of the upper eyelid with avulsion of the superior levator palpebrae muscle and orbital fat. Ann Plast Surg. 2003;51:321-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 50. | Ghadiali LK, Patel P, Levine JP, Gold KG, Lisman RD. Microvascular Free Flap for Total Eyelid Reconstruction With a Visually Useful Eye. Ophthalmic Plast Reconstr Surg. 2016;32:e109-e111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 51. | Iwanaga H, Nuri T, Okada M, Ueda K. Functional reconstruction of total upper eyelid defects with a composite radial forearm-palmaris longus tenocutaneous free flap: A report of two cases. Microsurgery. 2019;39:559-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 52. | Rubino C, Farace F, Puddu A, Canu V, Posadinu MA. Total upper and lower eyelid replacement following thermal burn using an ALT flap--a case report. J Plast Reconstr Aesthet Surg. 2008;61:578-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Transplantation
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ren M, China S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Wang JJ