Published online Dec 18, 2022. doi: 10.5500/wjt.v12.i12.405
Peer-review started: August 11, 2022
First decision: September 5, 2022
Revised: October 31, 2022
Accepted: December 6, 2022
Article in press: December 6, 2022
Published online: December 18, 2022
Processing time: 127 Days and 4.1 Hours
Over the last few years, the deceased donor organ donation rate was declined or remained stable, whereas the live donor organ donation rate has increased to compensate for the demand. Minimally invasive techniques for live donor nephrectomy (LDN) have also improved the live donor kidney donation rates. This increase has led to an interest in the surgical procedures used for LDN.
To evaluate the LDN techniques performed in Turkey, the structure of surgical teams, and the training received. Additionally, the number of kidney transplantations at different centers, the surgeon experience level, differences in surgical approach during donor surgeries, and outcomes were assessed.
A questionnaire was sent to the Turkish Ministry of Health-accredited transplant centers. It inquired of the number of LDN surgeries, surgical techniques, complications, optimization protocols, the experience of surgeons, and the training. Descriptive statistics were outlined as follows: Discrete numeric variables were expressed as medians (minimum-maximum), while categorical variables were shown as numbers and percentages. As a result of the goodness-of-fit tests, if the significance of the differences between the groups in discrete numerical variables for which the parametric test statistical assumptions were not met, data were analyzed with the Mann Whitney U test and the χ2 test.
The questionnaire was sent to 72 transplant centers, all of which replied. Five centers that reported not performing LDN procedures were excluded. Responses from the remaining 67 centers were analyzed. In 2019, the median number of kidney transplants performed was 45, and the median number of kidney transplants from living donors was 28 (1-238). Eleven (16.5%) centers performed 5-10, while 34 (50.7%) centers performed more than 100 live donor kidney transplants in 2019. While 19 (28.4%) centers performed the LDN procedures using the open technique, 48 (71.6%) centers implemented minimally invasive techniques. Among the centers preferring minimally invasive techniques for LDN, eight (16.6%) used more than one surgical technique. The most and the least common surgical techniques were transperitoneal laparoscopic (43 centers, 89.6%) and single port laparoscopic LDN (1 center, 2.1%) techniques, respectively. A positive association was found between the performance of minimally invasive techniques and the case volume of a transplant center, both in the total number and live donor kidney transplants (15 vs 55, P = 0.001 and 9 vs 42, P ≤ 0001 respectively). The most frequently reported complication was postoperative atelectasis (n = 33, 49.2%). There was no difference between the techniques concerning complications except for the chyle leak.
Turkish transplant centers performed LDN surgeries successfully through various techniques. Centers implementing minimally invasive techniques had a relatively higher number of live donor kidney transplants in 2019.
Core Tip: This study showed that centers using minimally invasive techniques had a relatively higher number of live donor kidney transplants in 2019. It also demonstrated that Turkish transplant teams performed live donor nephrectomy surgeries successfully through various techniques by considering that donor safety and center experience were the essential determinants when selecting the optimal approach for each donor.
- Citation: Mankiev B, Cimen SG, Kaya IO, Cimen S, Eraslan A. Current practice of live donor nephrectomy in Turkey. World J Transplant 2022; 12(12): 405-414
- URL: https://www.wjgnet.com/2220-3230/full/v12/i12/405.htm
- DOI: https://dx.doi.org/10.5500/wjt.v12.i12.405
Over the last few years, deceased donor organ donations have decreased[1]. In 2019, the overall organ donation rate was 46.5 per million population in Turkey[2]. This figure demonstrated a decline from the preceding years. However, this decline was less remarkable than in other European countries since live organ donation was promoted to compensate for demand. In line with this, countries like Turkey reported a rise in the number of living donor kidney transplantations during the pandemic. In 2019 according to the Turkish Ministry of Health data, 3963 kidney transplantations were performed in Turkey[2]. Among these patients, 3548 were transplanted from live donors. This increased living donor rate stimulated interest in Turkey’s surgical techniques and live donor nephrectomy (LDN) practices.
The introduction of laparoscopic donor nephrectomy was by Ratner et al[3]. Various minimally invasive techniques have been described and performed for live kidney donation. These include hand-assisted laparoscopic, retroperitoneoscopic, single port, natural orifice, and robotic nephrectomy techniques[4]. Meanwhile, the open donor nephrectomy technique remained a gold standard for patients with variant anatomies and previous abdominal surgeries. Studies conducted in Europe and the United States showed that minimally invasive donor nephrectomy improved the live kidney donation rates[5,6]. Due to shorter recovery time, less post-surgical pain, and better cosmetic results, live kidney donors preferred minimally invasive techniques. Therefore, many transplant centers implemented these techniques with considerable success.
Despite the high number of live donor kidney transplantations in Turkey, the surgical techniques for LDN have not been widely studied. This study evaluates the LDN techniques performed in Turkey, the structure of surgical teams, and the training received. Additionally, the number of kidney transplantations at different centers, the surgeon experience level, differences in surgical approach during donor surgeries, and outcomes were assessed.
This study was conducted by the University of Health Sciences, Diskapi Training and Research Hospital, Department of Surgery after approval from the institutional ethical review committee (83/06). A previously used questionnaire to screen kidney transplant centers in Europe was modified for Turkish transplant centers and used for study purposes[7]. The questionnaire was prepared using online survey software (SurveyMonkey®, California, United States). It was sent via e-mail to the transplant surgeon, nephrologist, or urologist working in the transplant centers registered with the Turkish Ministry of Health. The e-mail addresses were retrieved from the Turkish Ministry of Health database and several national transplant society websites.
In May 2020, the first round of questionnaires was sent out, while the second round was sent in September 2020. Data collection was closed after the last questionnaire was received on December 2, 2020. The questionnaire consisted of questions regarding the number of living donor nephrectomies performed in 2019, surgical techniques used, the experience of primary surgeons, and the training they had received. Data regarding average blood loss, donor warm ischemia time (DWIT), surgical complications, preferred nephrectomy side, and kidney extraction site were also interrogated. All donors included in the study were live and related to the recipient.
Data analysis was performed using IBM SPSS (Statistical Package for Social Sciences) Statistics 17.0 (IBM Corporation, Armonk, NY, United States) software. The Shapiro-Wilk test was used to determine whether the distribution of discrete numerical variables was close to normal. Descriptive statistics were outlined as follows: Discrete numeric variables were expressed as medians (minimum-maximum); and categorical variables were shown as numbers and percentages. As a result of the goodness-of-fit tests, if the significance of the differences between the groups in terms of discrete numerical variables for which the parametric test statistical assumptions were not met, data were analyzed with the Mann-Whitney U test. In the 2 × 2 cross-tabs, if the expected frequency was below 5 in at least one-quarter of the cells, the categorical data were evaluated by Fisher’s exact probability test. The χ2 test with continuity correction was used when the expected frequency was between 5-25. If no more than one-fifth of the cells had expected values equal to or less than 5, the categorical data were evaluated using the Fisher-Freeman Halton test. For P < 0.05, the results were considered statistically significant.
The questionnaire was sent to 72 kidney transplant centers, all of which replied. Five centers that reported not performing live donor kidney transplants were excluded. The responses from the remaining 67 centers were analyzed. In 2019, the median number of kidney transplants performed was 45 (1-484), and the median number of kidney transplants from living donors was 28 (1-238) (Table 1). Eleven centers (16.5%) reported performing 5-10, whereas 34 (50.7%) reported performing more than 100 live donor kidney transplants during 2019. Nineteen (28.4%) centers performed LDN using the open technique and 48 (71.6%) using minimally invasive techniques.
| Characteristics | Values |
| Number of kidney transplants performed in 2019 | 45 (1-484) |
| Number of kidney transplants from living donors in 2019 | 28 (1-238) |
| Number of donor nephrectomies performed in 2019 percenter | |
| 5-10 | 11 (16.5%) |
| 11-25 | 6 (9.0%) |
| 26-50 | 9 (13.4%) |
| 51-100 | 7 (10.4%) |
| > 100 | 34 (50.7%) |
| Primary surgeon | |
| General surgeon | 24 (35.8%) |
| Urologist | 16 (23.9%) |
| Transplant surgeon | 27 (40.3%) |
| Live donor nephrectomy technique | |
| Open donor nephrectomy | 19 (28.4%) |
| Minimally invasive techniques | 48 (71.6%) |
| Number of years using the preferred technique | |
| 1-3 yr | 12 (17.9%) |
| 3-5 yr | 13 (19.4%) |
| > 5 yr | 42 (62.7%) |
| Type of training received by the surgeon | |
| Fellowship training | 28 (41.8%) |
| Residency training | 22 (32.8%) |
| Surgical courses | 14 (20.9%) |
| Other | 13 (19.4%) |
LDNs were carried out by a transplant surgeon in 27 centers (40.3%), by a general surgeon in 24 centers (35.8%), and by a urologist in 16 centers (23.9%) (Table 1). The surgical experience was 5 or more years in 42 centers (62.7%), whereas 12 centers (17.9%) were newly established with 1-3 years of experience in donor nephrectomies. In addition, the technique for LDN was adopted through fellowship training in 28 centers (41.8%), surgical residency training in 22 centers (32.8%), workshops and courses in 14 centers (20.9%), and other routes in 13 centers (19.4%). Fifty-seven centers (85.1%) reported having a second surgeon as a backup. Only 10 centers (14.9%) did not have a backup surgeon. The average blood loss ranged between 0-100 mL during LDN in 52 centers (77.6%). Ten centers (14.9%) reported an average of 100-200 mL blood loss. Sixty-one centers (91%) reported a DWIT of 1-5 min, while DWIT was 5-10 min in 4 centers (0.6%) and 10-15 min in 2 centers (0.3%). Forty-nine centers (73.1%) recorded surgeries for optimization. Technical troubleshooting protocol was in place in 61 centers (91%).
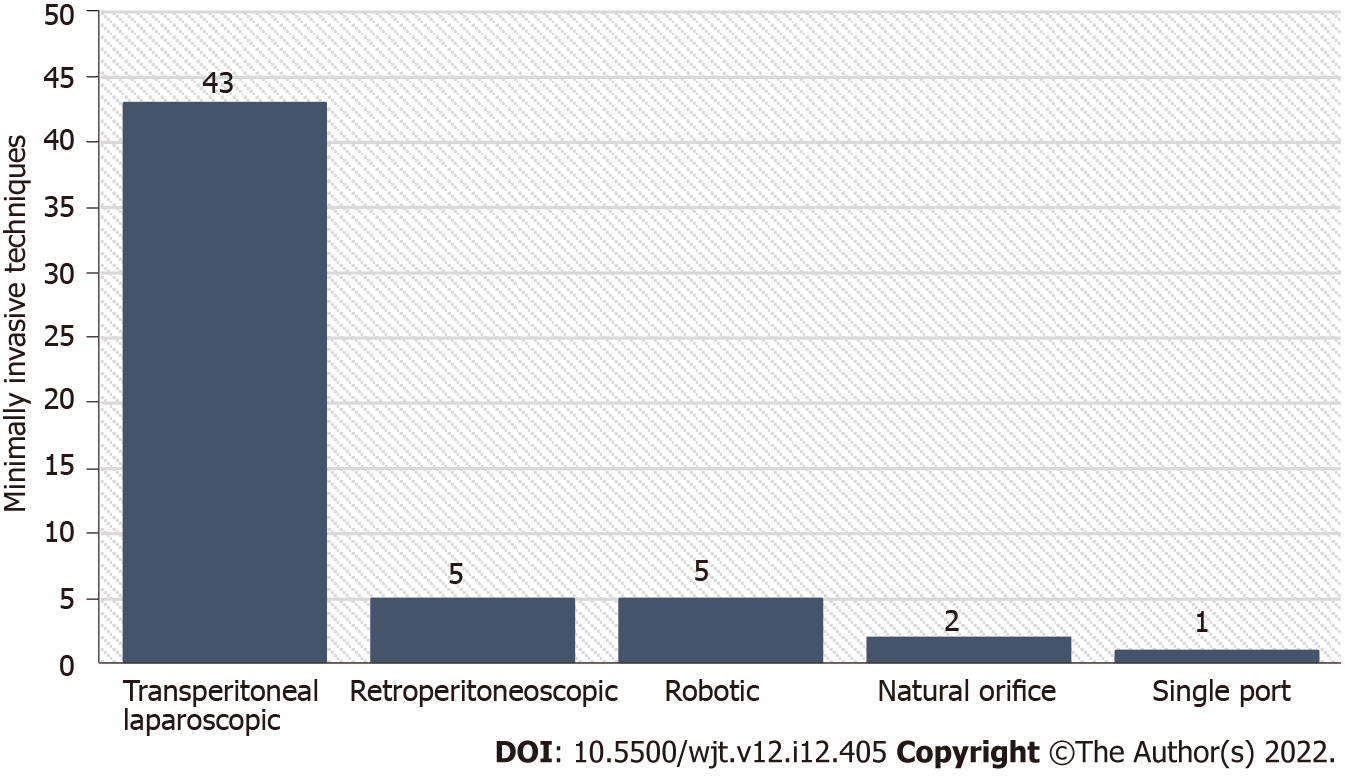
Among the 48 centers preferring minimally invasive techniques for LDN, 8 (16.6%) implemented more than one surgical technique. The surgical techniques and number of centers using these methods are displayed in Figure 1. As can be seen in this figure, transperitoneal laparoscopic donor nephrectomy was the most commonly performed technique, while single port laparoscopic donor nephrectomy was the least common technique.
The left donor nephrectomy was favored in 26 transplant centers (54.3%). The conversion rate was below 1% in 58 centers (86.5%). Eight centers (11.9%) reported a conversion rate between 1%-3%, and only 1 center (1.5%) reported a conversion rate of 3%-5%. The most frequent reason for conversion was venous bleeding (n = 10, 20.8%). Other reasons were abdominal adhesions (n = 8, 16.7%), technical problems related to gadgets and devices (n = 7, 14.6%), arterial bleeding (n = 5, 10.4%), adjacent organ injury (n = 1, 2.1%), and miscellaneous (n = 1, 2.1%).
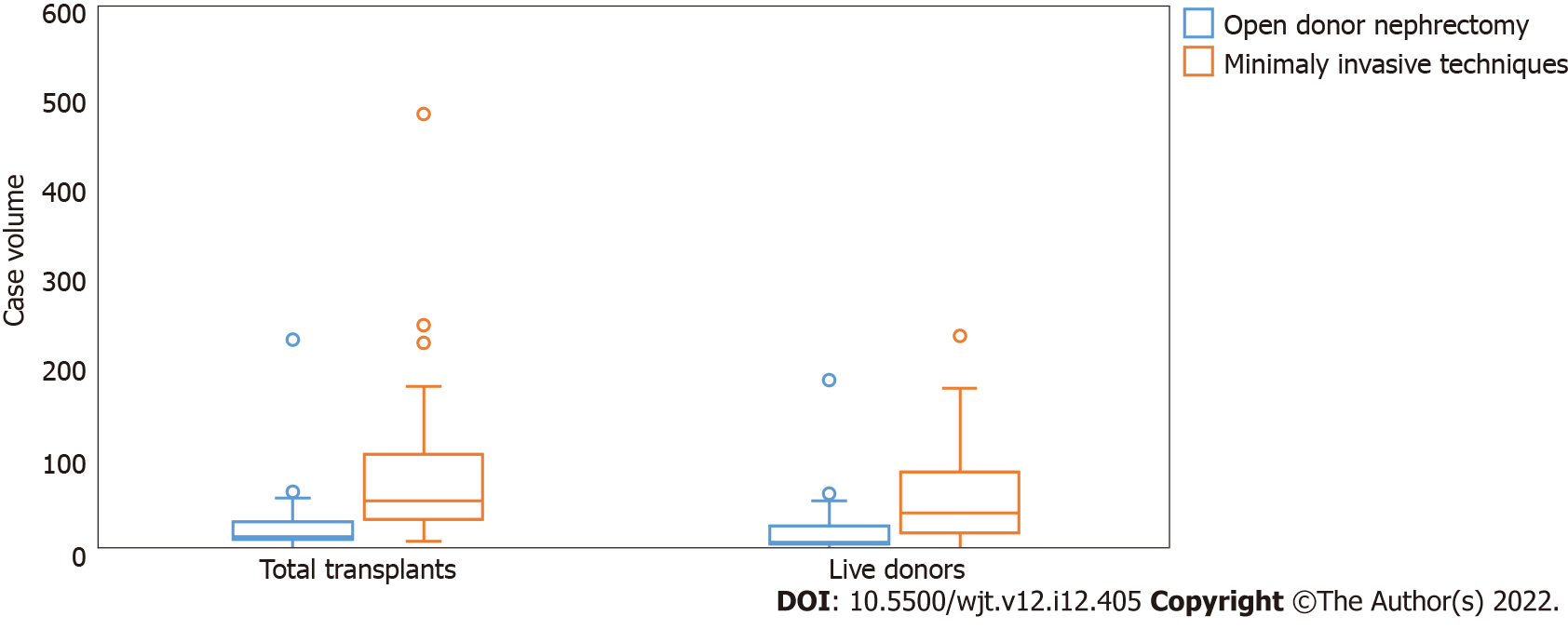
Thirty-four surgeons (50.7%) stated having performed more than 100 donor nephrectomies as the primary surgeon with the accustomed technique in 2019 (Table 1). On the other hand, 11 surgeons (16.5%) reported performing 5-10 donor nephrectomies as the primary surgeon. There was a positive association between the performance of minimally invasive techniques and the case volume of a transplant center regarding both the total number of transplants and live donor kidney transplants (15 vs 55, P = 0.001 and 9 vs 42, P ≤ 0.001 respectively) (Figure 2).
Nine centers (18.8%) reported using hand assistance, whereas 39 centers (81.2%) did not. While 41 centers (85.4%) reported using vascular staplers for division of the renal pedicle, 6 centers (12.5%) used self-locking surgical clips, and 1 center (2.1%) titanium clips. Modification of the surgical technique due to anatomical variations or body mass index of the donor was not preferred in 56.7% and 68.7% of the centers, respectively. Pfannenstiel incision was the most preferred extraction site for the kidney (n = 30, 62.5%). It was followed by the paramedian (n = 9, 18.7%), midline (n = 7, 14.6%), and modified incisions (n = 2, 4.2%).
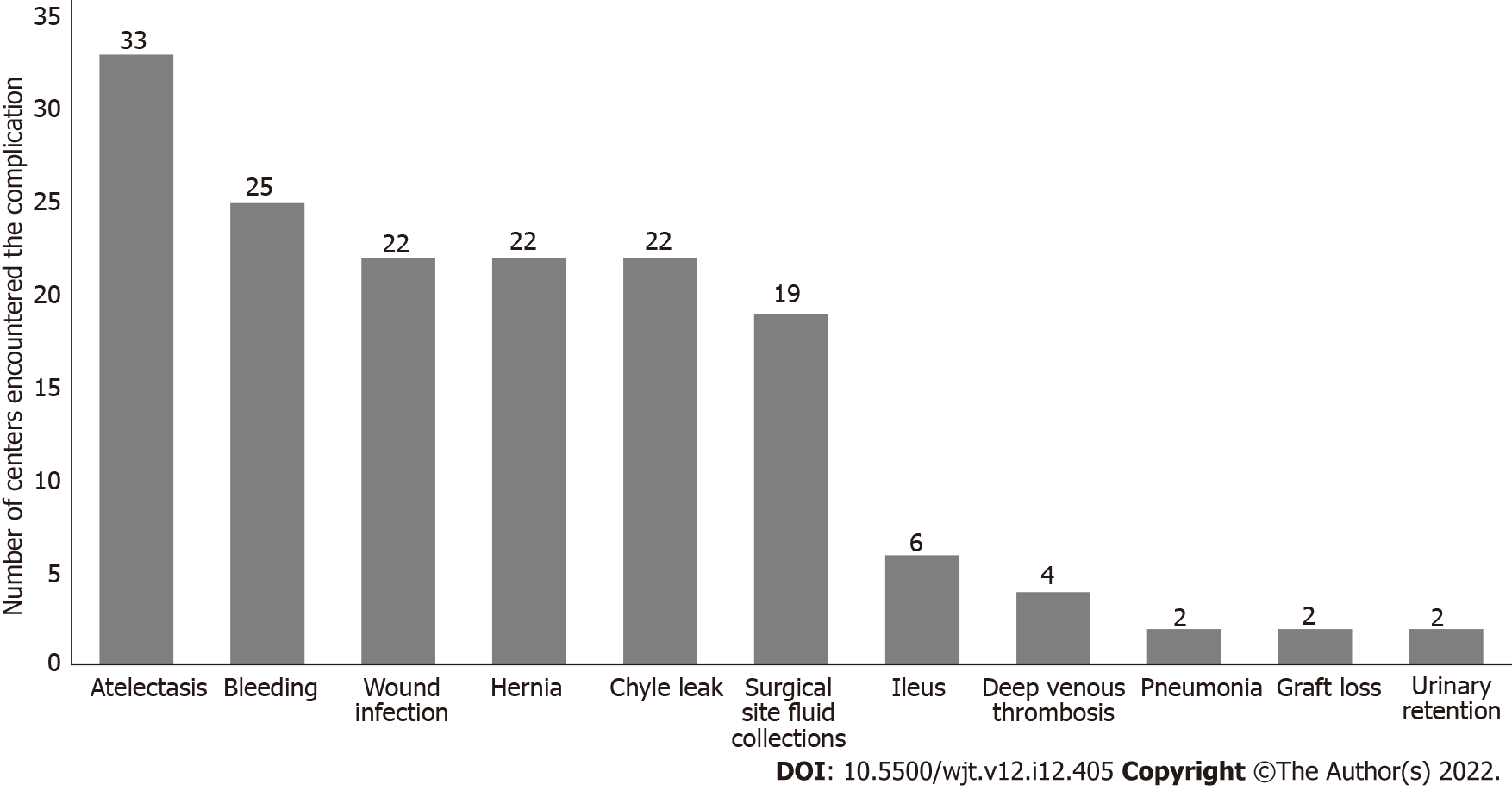
The most frequently reported complication was postoperative atelectasis (n = 33, 49.2%), while the second most frequent complication was bleeding requiring blood transfusion (n = 25, 37.3%) (Figure 3). Wound infection, hernia, and chyle leak were also reported (n = 22, 33.8%). Thirty-nine centers (81.2%) reported an incisional hernia rate of 1%-5%, while 6 centers (12.5%) reported a rate of 5%-10%, and 3 centers (6.3%) reported 10%-20%. Surgical site fluid collections, ileus, deep venous thrombosis, pneumonia, and urinary retention were also reported. Graft loss due to inadvertent intraoperative damage was encountered in two transplant centers (2.9%) (Figure 3). The rates of these declared complications did not differ among the centers using open and minimally invasive techniques except for the chyle leak (Table 2). Chyle leak was reported significantly more frequently by centers using the minimally invasive techniques (P = 0.006).
| Centers performing open donor nephrectomy, n = 19% | Centers performing minimally invasive techniques, n = 48% | P value | |
| Bleeding | 7 (36.8%) | 18 (37.5%) | > 0.999 |
| Chyle leak | 1 (5.3%) | 21 (43.8%) | 0.006 |
| Surgical site fluid collection | 5 (26.3%) | 14 (29.2%) | > 0.999 |
| Urinary retention | 0 (0.0%) | 2 (4.2%) | > 0.999 |
| Atelectasis | 11 (57.9%) | 22 (45.8%) | 0.536 |
| Pneumonia | 0 (0.0%) | 2 (4.2%) | > 0.999 |
| Deep vein thrombosis | 3 (15.8%) | 1 (2.1%) | 0.066 |
| Ileus | 0 (0.0%) | 6 (12.5%) | 0.173 |
| Hernia | 5 (26.3%) | 17 (35.4%) | 0.670 |
| Graft loss | 1 (5.3%) | 1 (2.1%) | 0.490 |
| Wound infection | 7 (36.8%) | 15 (31.3%) | 0.880 |
Persistent organ shortage has led to increased interest in live organ donation. As a result, the number of live kidney transplantations is increasing annually. It was previously reported that minimally invasive techniques for LDN might increase the number of donations. Nonetheless, the critical principle in live organ donation is the safety of the donor[8]. Therefore, donor safety should always be the greatest determinant when deciding on the LDN technique[9]. This study presented a cross-sectional view of the techniques of LDN, transplant team composition, training, and the list of the complications encountered at Turkish kidney transplant centers.
Our findings were similar to those of Klop et al[10]. They reported that 59 of the transplant centers in Europe performed minimally invasive techniques for LDN[10]. In their survey, 48 European transplant centers used the laparoscopic approach, and 9 centers used the retroperitoneoscopic approach. In our study, 48 centers reported performing minimally invasive techniques. Among those, 43 used the laparoscopic approach, and 5 used retroperitoneoscopic methods. In line with the American and European centers, robotic surgery is also used for LDN in Turkey[11,12]. Five transplant centers in our study reported implementing robotic-assisted techniques. In 2009, only two centers in Europe used robotic-assisted techniques. However, this number increased gradually, with several case series being published in the literature[13-16].
In our survey, 19 centers reported using the open technique for donor nephrectomy. This result was in accordance with the findings of the European survey, which reported that 37 centers performed open donor nephrectomies[10]. This similarity indicates the international trend for minimally invasive techniques. As per the literature, the total number of kidney transplants and live donor kidney transplants is in line with the increased use of minimally invasive donor nephrectomy techniques in Turkish transplant centers[4,7,10].
A comparison of the centers regarding case volumes revealed a significant variation among centers in this regard. Thirty-four centers performed more than 100 live donor kidney transplants in 2019. These centers represented 50.7% of the transplant centers enrolled in our study. While these centers performed more than 3400 kidney transplants, the remaining 33 centers performed approximately 200 live donor kidney transplants in total. This disproportionate distribution can be explained by the higher number of live donations in highly populous cities of Turkey, such as Istanbul and Ankara. On the other hand, in Europe, as of 2009, only four centers were performing more than 100 live donor kidney transplants per year, while 30 centers were performing fewer than 100 live donor kidney transplants[10].
The spectrum of postoperative complications did not differ between the centers performing minimally invasive donor nephrectomy and those performing open donor nephrectomy. Among all complications, only chyle leak was more frequently encountered in the centers using minimally invasive techniques. Two centers reported graft loss due to intraoperative damage of the graft: One from a center using open donor nephrectomy and the other from a minimally invasive center. In our study, the relationship between the caseload of the transplant center and the complication of graft loss could not be analyzed due to the small numbers.
The team setup and staff training in Turkish transplant centers demonstrate similar results with the other transplant centers in the United States and Europe, where 41.8% of the staff have received fellowship training for organ transplantation[17,18]. Our findings revealed that most (i.e., 40.3) of the LDN procedures were performed by transplant surgeons in Turkish transplant centers. A scientific committee that consists of experienced transplant surgeons, nephrologists, transplant coordinators, and hepatologists evaluates the surgical trainee in terms of scientific and surgical qualifications for transplant proficiency. If the requirements are satisfied, then a certificate is given to the surgeon as a transplant surgeon. This certificate grants the surgeon to lead a transplant surgical team and perform transplants in his/her hospital.
The average blood loss ranged between 0-100 mL in 77.6% of the transplant centers in Turkey. The amount of blood loss and DWIT were compatible with the literature[19-22]. Technical troubleshooting protocol was in place and intraoperative video recording was routinely performed in the majority of the transplant centers in Turkey.
Eight centers in our study reported using more than one surgical technique. As a matter of course, performing LDN with more than one surgical technique provides advantages. These advantages are selecting the best technique for the donor and the ability to adapt the preferred technique to the donor anatomy, body mass index, surgical history, and abdominal adhesions. As an additional advantage, it can reduce the risk of conversion to open surgery. For example, in cases of venous bleeding, which was reported as the most common cause of conversion in our study, the surgeon can complete the surgery with a hand-assisted technique by placing an additional hand port.
To our knowledge, this is the first study evaluating donor nephrectomy techniques in Turkey. All transplant centers performing LDN responded to the survey and were included in our analysis. However, this study has some limitations which need to be considered while evaluating its findings. First, it is a survey study, and the reliability of the data depends on the accuracy of the answers and the honesty of the responders. Second, our findings could have been affected by a recall bias. However, this study provides an overview of the centers performing LDN in Turkey despite these limitations. The results of this study and future similar studies may act as instruments revealing any weaknesses that may need improvement.
Turkey is one of the leading countries for live organ donation. In this article we explored the transplant climate in Turkey via a detailed survey sent to transplant program directors. The questionnaire was sent to 72 kidney transplant centers, all of which replied. In 2019, the median number of kidney transplants performed was 45 (1-484), and the median number of kidney transplants from living donors was 28 (1-23). Among the 48 centers preferring minimally invasive techniques for LDN, 8 (16.6%) implemented more than one surgical technique. Transperitoneal laparoscopic donor nephrectomy was the most commonly performed technique, while single port laparoscopic donor nephrectomy was the least common technique. There was a positive association between the performance of minimally invasive techniques and the case volume of a transplant center regarding both the total number of transplants and live donor kidney transplants. To our knowledge, this is the first study evaluating donor nephrectomy techniques in Turkey. Therefore, this study represents the national transplant envir
Minimally invasive surgical techniques for live donor nephrectomy (LDN) are varied. These techniques include hand-assisted laparoscopic, retroperitoneoscopic, single port, natural orifice, and robotic nephrectomy techniques. Turkey has a high number of live kidney donors. The reports regarding LDN in Turkey are missing. In this study, we demonstrated the center volume, preferred techniques for LDN, complications, team setup, and training of transplant teams.
In 2019 according to the Turkish Ministry of Health data, 3963 kidney transplantations were performed in Turkey. Among these patients, 3548 were transplanted from live donors. This increased living donor rate stimulated interest in various surgical techniques applied in Turkey and LDN practice.
To gain insight into the practices of LDNs in Turkish transplant centers.
A questionnaire was sent to the Turkish Ministry of Health-accredited transplant centers. It inquired of the number of LDN surgeries, surgical techniques, complications, optimization protocols, the experience of surgeons, and the training. Descriptive statistics were outlined as follows: Discrete numeric variables were expressed as medians (minimum-maximum), while categorical variables were shown as numbers and percentages. As a result of the goodness-of-fit tests, if the significance of the differences between the groups in discrete numerical variables for which the parametric test statistical assumptions were not met, data were analyzed with the Mann Whitney U test and the χ2 test.
The questionnaire was sent to registered transplant centers in Turkey. All 72 centers replied. In 2019, the median number of kidney transplants performed was 45 per center, and the median number of kidney transplants from living donors was 28. There was a wide range between the centers in terms of transplant numbers (1-238 transplant per year). The open technique was preferred by 19 centers (28.4%). The minimally invasive LDN was performed by 48 centers (71.6%). Among the centers, 8 (16.6%) used more than one surgical technique. A positive correlation between the performance of minimally invasive LDN and the case volume of a transplant center, both in the total number of transplants and live donor kidney transplants, existed (15 vs 55, P = 0.001 and 9 vs 42, P ≤ 0.001 respectively). The most frequently reported complication was postoperative atelectasis (n = 33, 49.2%).
The analysis of the questionnaire answers revealed that Turkish transplant centers successfully performed LDN operations using various techniques. A relatively higher numbers of living donor kidney transplants were performed in 2019 at centers using minimally invasive techniques.
The data regarding the annual kidney transplant numbers, complication rates, and center successes should be released by the Ministry of Health in Turkey. This would allow the control and improvement of the transplant centers when necessary. Despite this, the current status of Turkish transplant centers, as observed in the results of this study, is comparable to transplant centers in Europe and the United States.
Acknowledgment of participating Transplant Centers (Cities are listed in alphabetical order): Ankara: Prof.Dr. Mehmet HABERAL, Prof.Dr. Acar TÜZÜNER, Prof.Dr.Mustafa Hakan SÖZEN, Prof. Dr.Aydin DALGIÇ, Prof.Dr.Fazıl Tuncay AKI, Doç.Dr Sertaç ÇİMEN, Prof.Dr. Sadık ERSÖZ, Prof.Dr. Sedat KARADEMİR, Doç.Dr. Ulaş SÖZENER, Doç Dr. Erkan Ölçücüoğlu, Op.Dr Sedat Taştemur, Op.Dr. Yusuf Kasap Adana: Prof.Dr. Erkan DEMİR, Doç.Dr. Edip AKPINAR, Prof.Dr. Kenan ÇALIŞKAN, Antalya: Prof. Dr.Alper DEMİRBAŞ, Prof.Dr.Bülent AYDINLI, Doç.Dr.Tuğrul ÇAKIR. Aydın Op.Dr. Arif KOL. Bursa: Prof.Dr.A.Bülent OKTAY, Prof.Dr.İsmet YAVAŞÇAOĞLU, Op.Dr. Atilla SATIR. Çanakkale: Prof.Dr. Cabir ALAN. Denizli Doç.Dr. Murat ÖZBAN. Diyarbakır: Doç.Dr. Mehmet Veysi BAHADIR, Op.Dr. Nurettin AY. Edirne Prof.Dr. Tamer SAĞIROĞLU. Elazığ: Prof.Dr. Cüneyt KIRKIL. Erzurum: Prof.Dr.Gürkan ÖZTÜRK. Eskişehir Prof.Dr. Murat ULAŞ, Prof.Dr. Bülent ÜNAL. Gaziantep: Prof.Dr. Sacid ÇOBAN. Isparta: Doç.Dr. Mehmet Zafer SABUNCUOĞlU. İstanbul: Prof.Dr.İbrahim BERBER. Prof. Dr. İsmet NANE, Prof.Dr. Salih PEKMEZCİ, Doç.Dr. Dr. Eyüp Veli KÜÇÜK, Prof.Dr. Gürkan TELLİOĞLU, Prof.Dr. Hüseyin Çağatay AYDIN, Prof. Dr. Volkan TUĞCU, Doç.Dr. Ercüment GÜRLÜLER, Doç.Dr.Selçuk ŞAHİN, Prof. Dr. Alp GÜRKAN, Prof.Dr. Adem AKÇAKAYA, Prof. Dr. Şinasi SEVMİŞ, Prof. Dr. Sinan YOL, Doç. Dr. Sabri TEKİN, Prof. Dr. Muzaffer SARIYAR, Prof.Dr.Remzi EMİROĞLU, Prof.Dr. Cumhur YEĞEN, Prof. Dr. Ali İhsan DOKUCU, Prof.Dr. Bariş AKIN, Doç.Dr. Melih KARA, Op. Dr. Volkan TURUNÇ, Prof. Dr. Feza Yarbuğ KARAKAYALI, Doç. Dr. Mehmet Tokaç, Prof. Dr. Burak KOÇAK, Prof. Dr. Ayhan DİNÇKAN, Doç.Dr. Necdet GÜLER. İzmir: Prof.Dr. Seymen BORA, Doç.Dr. İsmail SERT, Prof.Dr. Adam USLU, Doç.Dr. Fevzi CENGİZ, Op.Dr Uğur SARAÇOĞLU, Doç.Dr. Taylan Özgür SEZER. Kayseri: Dr. Tutkun TALİH. Kocaeli: Op.Dr.Bekir VOYVODA. Konya: Prof.Dr.Tevfik KÜÇÜKKARTALLAR, Prof.Dr. Mehmet ERİKOĞLU. Malatya: Prof. Dr. Turgut PİŞKİN. Mersin: Prof.Dr. Murat BOZLU. Sakarya: Prof.Dr. Fehmi ÇELEBİ. Samsun: Prof.Dr. Şaban SARIKAYA. Trabzon: Prof. Dr. Serdar TURKYILMAZ.
| 1. | Caliskan G, Sayan A, Kilic I, Haki C, Kelebek Girgin N. Has the COVID-19 Pandemic Affected Brain Death Notifications and Organ Donation Time? Exp Clin Transplant. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Böbrek Sağlığı Hakkında. Güncel Organ Bağış Ve Nakil İstatistikleri. [cited 16 July 2022]. Available from: https://www.tbv.com.tr/bobrek-sagligi/guncel-organ-bagis-ve-nakil-i-statistikleri/. |
| 3. | Ratner LE, Ciseck LJ, Moore RG, Cigarroa FG, Kaufman HS, Kavoussi LR. Laparoscopic live donor nephrectomy. Transplantation. 1995;60:1047-1049. [PubMed] |
| 4. | Dols LF, Kok NF, Ijzermans JN. Live donor nephrectomy: a review of evidence for surgical techniques. Transpl Int. 2010;23:121-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 62] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Mjøen G, Holdaas H, Pfeffer P, Line PD, Øyen O. Minimally invasive living donor nephrectomy - introduction of hand-assistance. Transpl Int. 2010;23:1008-1014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Schweitzer EJ, Wilson J, Jacobs S, Machan CH, Philosophe B, Farney A, Colonna J, Jarrell BE, Bartlett ST. Increased rates of donation with laparoscopic donor nephrectomy. Ann Surg. 2000;232:392-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 217] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 7. | Kok NF, Weimar W, Alwayn IP, Ijzermans JN. The current practice of live donor nephrectomy in Europe. Transplantation. 2006;82:892-897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 50] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Kortram K, Lafranca JA, IJzermans JN, Dor FJ. The need for a standardized informed consent procedure in live donor nephrectomy: a systematic review. Transplantation. 2014;98:1134-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Merlin TL, Scott DF, Rao MM, Wall DR, Francis DM, Bridgewater FH, Maddern GJ. The safety and efficacy of laparoscopic live donor nephrectomy: a systematic review. Transplantation. 2000;70:1659-1666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 91] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Klop KW, Dols LF, Kok NF, Weimar W, Ijzermans JN. Attitudes among surgeons towards live-donor nephrectomy: a European update. Transplantation. 2012;94:263-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Serni S, Pecoraro A, Sessa F, Gemma L, Greco I, Barzaghi P, Grosso AA, Corti F, Mormile N, Spatafora P, Caroassai S, Berni A, Gacci M, Giancane S, Tuccio A, Sebastianelli A, Li Marzi V, Vignolini G, Campi R. Robot-Assisted Laparoscopic Living Donor Nephrectomy: The University of Florence Technique. Front Surg. 2020;7:588215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 12. | Geffner S, Klaassen Z, Tichauer M, Chamberlain RS, Paragi PR. Robotic-assisted laparoscopic donor nephrectomies: early experience and review of the literature. J Robot Surg. 2011;5:115-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Janki S, Klop KWJ, Hagen SM, Terkivatan T, Betjes MGH, Tran TCK, Ijzermans JNM. Robotic surgery rapidly and successfully implemented in a high volume laparoscopic center on living kidney donation. Int J Med Robot. 2017;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Giffen ZC, Cairl N, Ortiz J, Sindhwani P, Ekwenna O. Robotic-assisted Donor Nephrectomy: As Safe as Laparoscopic Donor Nephrectomy. Surg Technol Int. 2020;37:171-174. [PubMed] |
| 15. | LaMattina JC, Alvarez-Casas J, Lu I, Powell JM, Sultan S, Phelan MW, Barth RN. Robotic-assisted single-port donor nephrectomy using the da Vinci single-site platform. J Surg Res. 2018;222:34-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 16. | Cohen AJ, Williams DS, Bohorquez H, Bruce DS, Carmody IC, Reichman T, Loss GE Jr. Robotic-assisted laparoscopic donor nephrectomy: decreasing length of stay. Ochsner J. 2015;15:19-24. [PubMed] |
| 17. | Özdemir-van Brunschot DM, Warlé MC, van der Jagt MF, Grutters JP, van Horne SB, Kloke HJ, van der Vliet JA, Langenhuijsen JF, d'Ancona FC. Surgical team composition has a major impact on effectiveness and costs in laparoscopic donor nephrectomy. World J Urol. 2015;33:733-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Raque J, Billeter AT, Lucich E, Marvin MM, Sutton E. Training techniques in laparoscopic donor nephrectomy: a systematic review. Clin Transplant. 2015;29:893-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Gimenez E, Leeser DB, Wysock JS, Charlton M, Kapur S, Del Pizzo JJ. Laparoendoscopic single site live donor nephrectomy: initial experience. J Urol. 2010;184:2049-2053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 20. | Friedman AL, Peters TG, Jones KW, Boulware LE, Ratner LE. Fatal and nonfatal hemorrhagic complications of living kidney donation. Ann Surg. 2006;243:126-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 130] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 21. | Biancofiore G, Amorose G, Lugli D, Bindi L, Esposito M, Fossati N, Meacci L, Pasquini C, Pieri M, Boggi U, Pietrabissa A, Mosca F. Perioperative management for laparoscopic kidney donation. Minerva Anestesiol. 2003;69:681-686, 686. [PubMed] |
| 22. | Mateo R, Henderson R, Jabbour N, Gagandeep S, Goldsberry A, Sher L, Qazi Y, Selby RR, Genyk Y. Living related donor nephrectomy in transfusion refusing donors. Transpl Int. 2007;20:490-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author’s Membership in Professional Societies: Turkish Society of Gastroenterology, 0233.
Specialty type: Transplantation
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mubarak M, Pakistan; Tsoulfas G, Greece S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Wang JJ