Published online Dec 28, 2020. doi: 10.5500/wjt.v10.i12.372
Peer-review started: June 20, 2020
First decision: August 22, 2020
Revised: August 29, 2020
Accepted: October 9, 2020
Article in press: October 9, 2020
Published online: December 28, 2020
Processing time: 186 Days and 10.9 Hours
The aim of the work was to analyze and expose the donor and recipient risk factors in pancreas transplantation. In the following paper, we exposed the 2018 Spanish Consensus Document on Donor and Recipient Selection Criteria for Pancreas Transplantation. An assessment of the previous Selection Criteria for Donors and Recipients of Pancreas Transplantation, published in 2005 by the Spanish Pancreas Transplant Group (GETP) and the National Transplant Organization (ONT) was performed. A literature review was performed using Cochrane Library, PubMed and Google Scholar databases. Some of the following terms were used for the literature search: “Diabetes Mellitus,” “Pancreas Transplantation,” “Insulin-Secreting Cells,” “Pancreas Allograft Thrombosis,” “Allograft Pancreatitis,” “Donors’ Risk Factors,” “Recipients’ Risk Factors,” “Pancreas Allograft Rejection” and “Pancreas Allograft Survival.” After an extended search, different inclusion criteria were established. Articles and documents with abstracts of full text and in English or Spanish language were selected. Subsequently, different scientific meetings took place during 2015 and 2016 by the GETP. Finally, the updated criteria were published by the GETP and ONT in 2018. Several risk factors have been described in pancreas transplantation that can be divided into donor risk factors: Advanced age (> 50 years); high body mass index (BMI) (> 30 kg/m2); cause of death (e.g., stroke); previous hyperglycemia; hyperamylasemia; cold ischemia time (greater than 8 or 12 h, depending on the type of donation); the use of vasopressors in the intensive care unit or cardiac arrest; and the macroscopic aspect of the pancreas allograft. The following are recipient risk factors: Advanced age (> 50 years); active smoking; high BMI (> 30 kg/m2); and peripheral artery disease or sensorimotor polyneuropathy. Based on the aforementioned parameters, different selection criteria have been established for the recipients depending on the type of pancreas transplantation. Knowledge of the risk factors for pancreas transplantation allows the establishment of reliable selection criteria for choosing donors and recipients.
Core Tip: Pancreas transplantation remains the only treatment to restore euglycemia and hemoglobin A1c levels in diabetic patients. However, it presents high morbidity due to different postoperative complications and the effects of the immunosuppressive therapies. The pancreas transplantation complications occur more frequently in specific cases related to donor factors (high body mass index, older age, etc.). Several studies analyzed the donor and recipient risk factors. Knowing these risk factors allows us to establish specific selection criteria in pancreas transplantation and may improve its results.
- Citation: Muñoz-Bellvís L, López-Sánchez J. Donor risk factors in pancreas transplantation. World J Transplant 2020; 10(12): 372-380
- URL: https://www.wjgnet.com/2220-3230/full/v10/i12/372.htm
- DOI: https://dx.doi.org/10.5500/wjt.v10.i12.372
A simple analysis of the donor’s cause of death allowed us to verify that those ideal pancreas donors (healthy and young individuals) are currently decreasing. Therefore, it is very important to optimize all possible pancreas grafts without risking the graft or recipient.
The postoperative complications inherent to pancreatic surgery (e.g., pancreatitis, fistulas, necrosis, etc.) appear similarly in pancreas transplantation. In addition, ischemia-reperfusion injury, immunological factors and immunosuppressive therapy increase the risk of their appearance[1]. Therefore, the quality of the graft is essential to reduce the rate of postoperative surgical complications such as thrombosis, pancreatitis, infection and fistulas. The factors discussed below have been associated to an increase in the incidence of technical complications and are still considered a significant cause of pancreatic graft loss[1-3].
Donor’s age is an important factor in the viability of grafts in all types of transplants. Currently, older donors (> 80 years) are accepted for liver and kidney transplant. Nonetheless, the age in pancreas transplantation remains a strict selection criteria. The use of pediatric donors (< 18 years in the United States) for adult recipients is infrequent due to the fact that these grafts present a lower β-cell mass, require a greater technical challenge and are associated with a greater number of complications, especially vascular thrombosis[4]. Despite this, some authors have presented excellent results using the pancreas from donors < 10 years[5,6].
The largest published series of pancreas donors with ages ranging from 3 to 17 years was from Fernandez LA et al[7]. A comparative study was performed between the group of transplants from young donors [142 simultaneous pancreas kidney (SPK) transplantations] and those from adult donors (538 SPK transplantations) over the same period. After ten years of follow-up, no significant differences were found regarding patient survival. However, a trend towards increased graft survival in pediatric pancreas recipients was observed[7]. A subsequent study of the same group insisted on the safety of pancreas transplantation from pediatric donors over three years of age and with a weight of ≥ 25 kg[8]. Some authors have hypothesized that these donors may benefit recipients who are underweight because kidney and pancreatic function could be maximized[9].
Regarding the upper age limit, numerous authors have shown that the using the pancreas from donors older than 45 years is the most important donor risk factor and leads to reduced graft survival and increased complications[10-19]. Other studies performed under an immunosuppression regimen based on tacrolimus did not find an increase in post-transplant complications using the pancreas from donors ≥ 45 years[11].
Most groups consider using the pancreas of donors older than 45-50 years to present a significant risk in the development of vascular thrombosis, intra-abdominal infections and duodenal or anastomotic leaks, which affects the graft and recipient survival[6,12-22]. Krieger et al[6] analyzed 91 SPK transplantations using grafts from donors older than 45 years. There was a decrease in patient survival at 1 year and 5 years and an increase in the percentage of intra-abdominal infections compared to the group transplanted with donor grafts between 18 years and 45 years. Graft loss occurred mostly in the first 2 wk after surgery. This occurred in 6.6% of recipients from older donors compared to 1.9% in the standard group.
These data show the trend to use the pancreas from donors younger than 50 years. This was recently corroborated by the report of the Organ Procurement and Transplantation Network/Scientific Registry of Transplant Recipients published in 2019 in reference to the year 2017[23]. This report stated that the age range of pancreas donors between 18 and 34 years has remained stable for more than a decade. It is the most frequent group of donors with an overall frequency of more than 60% of the transplants. In relation to the other groups, donors under the age of 18 years obtained percentages of around 20%, and those between 35 years and 49 years have decreased in the last 10 years to around 10%. The proportion of donors over 50 years was less than 1% of total pancreas donors[23].
In contrast, the EXPAND multicenter study[24] showed similar rates of morbidity and graft rejection in transplant patients from donors over 50 years compared to those under 50 years. Therefore, in cases of pancreas donors over 45 years, each group should individualize each case by studying the medical history (especially previous cardiovascular diseases), weight, previous physical activity and lifestyle, cause of death, time in the intensive care unit, etc. This will allow optimization of a currently scarce resource.
The ideal donor for pancreas transplantation is a young man without associated diseases who has died by trauma. Currently, the North American and Spanish registries have shown a progressive trend towards older donors with stroke-related causes of death. In addition, the use of grafts from young donors associated with road traffic accident-related deaths is declining.
In one study from the University of Minnesota[25], donor death due to stroke appeared as an independent risk factor for allograft thrombosis after an SPK transplantation. However, the donors were not divided by age groups. Therefore, these results should be taken cautiously because the thrombosis could be related to age and not to the cause of death. In fact, the pancreas of young donors who died of congenital brain damage progressed significantly better than those of donors older than 45 who died by stroke. It seems evident that the existence of coronary artery disease and intracranial atherosclerosis are associated with systemic vascular involvement. Therefore, the cause of death would not be a risk factor in itself but rather the vascular disease.
The presence of hyperglycemia in brain-dead patients is not uncommon. Some authors suggest that hyperglycemia may affect post-transplantation evolution, but in general this status is independent of the endocrine functional state of the pancreas. The hyperglycemic status of the donor has different origins. It may be related to the trauma itself (as a consequence of the destruction of areas of the central nervous system related to metabolic functions), result from acute injury and the secondary release of catecholamines and steroids or it may be related to the administration of exogenous glucose and steroids. In the absence of a history of diabetes, this hyperglycemia is not a contraindication to donation[10,26-28].
Hight levels of amylase in the blood are observed in up to 40% of donors and may sometimes contraindicate donation[29]. Hyperamylasemia is frequently associated with death due to traumatic brain injury. Other times it occurs as a result of direct trauma to the salivary glands. It may also be secondary to pancreatitis, metastasis and chronic renal disease, contraindicating donation in all cases. Conversely, an isolated elevation of amylase in the blood without associated lesions is not a contraindication for donation, as the use of this type of pancreas does not affect graft function after transplantation[26-30]. Currently, hyperglycemia or hyperamylasemia are not considered absolute contraindications for transplantation[6,31].
It has been considered that a pancreatic graft can be transplanted up to 30 h after pancreas extraction[32]. Several studies show that within this limit there is no added morbidity[10,15,33,34]. However, other authors have reported an increase in the incidence of complications such as anastomotic leaks, thrombosis, pancreatitis and infections, and they recommended to not exceed the limit of 20 h[35-38]. Recent studies showed a higher rate of graft failure when the cold ischemia time increased[39].
The development of early pancreatitis after transplantation has been associated with several factors, including advanced age and high body mass index (BMI), but it has also been associated with prolonged ischemic times[37,40-42]. Currently, it would be advisable in the brain-dead organ donors a cold ischemia time less than 12 h, and in the donors after circulatory death (category III of the Maastricht classification revisited) a time of cold ischemia less than 8 h.
Donors who are hemodynamically unstable at the time of extraction are considered marginal. In general terms, this corresponds to those donors who require high doses of dopamine (> 10 µg/kg/min) or the use of two vasopressors at the time of extraction. The pancreas is a low-flow organ, so hemodynamic instability before or during extraction may contribute to the presence of inadequate perfusion and the development of graft thrombosis and postoperative pancreatitis[31]. In a donor’s preprocurement cardiac arrest, the functional impact and evolutionary curve over time of liver and pancreatic enzymes should be carefully evaluated to rule out severe damage in both organs. In particular, in brain-dead organ donors, the time of preprocurement cardiac arrest should not exceed 15 min, although the functional impact should always be assessed individually.
The macroscopic appearance of the pancreas at the time of extraction is the most relevant data to decide the graft’s viability. The presence of acute or chronic pancreatitis signs, the existence of pseudocysts or an important fatty infiltration may contraindicate the pancreatic extraction. Also, evidence of traumatic injury to the pancreas is contraindicated for transplantation. The pancreatic edema may be the result of overhydration of the donor during the intensive care unit stay. The use of grafts with edema depend on the direct examination by the surgeon and the improvement of the organ after the administration of albumin and diuretics.
The most important factor for deciding the validity of the pancreas remains the inspection by a senior transplant surgeon. A pancreas with calcifications, fibrosis or fatty infiltration should not be considered valid. Likewise, the existence of vessels with intense atheromatosis is an undoubted risk factor[6,31]. During extraction, color, consistency and the presence of masses, nodules or trauma of the pancreas should be evaluated. The organ should have a soft consistency with no indurated areas on palpation and little or no fatty infiltration. A pale coloration suggests ischemia, while an intense yellow color may be a consequence of fatty infiltration related to obesity or alcoholism.
Donor obesity is an important risk factor for surgical complications following transplantation. These grafts present intra- and periglandular fatty infiltration. Therefore, its preservation is not always optimal. These pancreases are more susceptible to ischemia-reperfusion injury and have an increased incidence of pancreatitis, thrombosis and intra-abdominal infections. Likewise, the role that the possible subclinical diabetes of the obese donor may play in the subsequent function of the graft has been highlighted[8].
Previous studies showed significant differences in pancreatic graft survival results between donors with BMI greater than or less than 30 kg/m2[43]. Other authors found a relationship between a BMI greater than 30 kg/m2 and the presence of peripancreatic fluid collections[44]. According to most of the authors, donor obesity is considered to be one of the factors that contraindicate the use of the pancreas graft. It therefore seems advisable not to accept a pancreas from a donor with a BMI > 30 kg/m2[34,35,37].
A lower donor weight also represents a risk factor. The presence of small vessels increases the technical requirements. A recipient with a pancreas from a donor weighing less than 30 kg showed significantly lower graft survival than a recipient who received a graft from a heavier donor. Graft thrombosis was the main cause of graft loss on these occasions[4,8].
There are well-defined criteria for selecting SPK transplantation recipients: (1) Age ≤ 55 years. Patients of older age should be considered individually; (2) Absence of severe peripheral arterial disease or coronary heart disease; (3) Absence of several motor sensory neuropathy or peripheral autonomic impairment; (4) Fulfillment of the kidney transplantation criteria; (5) Absence of severe mental disorders; and (6) Ability to understand the possible post-surgery complications and the treatment follow-up[37,45].
Relative contraindications: (1) Patients ≤ 18 years or > 55 years; (2) Recent retinal hemorrhage; (3) Active smoker (it is recommended to stop smoking prior to the inclusion on the waiting list); (4) BMI ≥ 30 kg/m2; and (5) Human immunodeficiency virus, hepatitis C virus or hepatitis B virus positive. (hepatitis C virus treatment is recommended prior to the inclusion on the waiting list).
Before SPK transplantation, dialysis can be performed by hemodialysis or peritoneal dialysis based on what is considered adequate for the patient depending on the moment and time expected on the waiting list. If the patient’s selection criteria are based on achieving the improvement of diabetic lesions, predialysis patients should be recommended for SPK transplantation. Patients with end stage renal disease without dialysis could be included in the waiting list when creatinine levels are lower than 30 mL/min (stage IV). Once included on the waiting list, the nephrologist must report any changes regarding the SPK transplantation selection criteria.
Patients suitable for this transplant must meet the following criteria: (1) Type 1 diabetes mellitus (DM): Previous living or deceased donor kidney transplantation; (2) Pancreatic graft failure after an SPK transplantation; (3) Tolerance for an increase in immunosuppressive therapy; and (4) Stable performance of the renal graft in all the cases (creatinine clearance > 40 mL/min)[37,46].
Pancreas transplant alone is recommended for type 1 DM patients without end stage renal disease. Also, a creatinine clearance > 60 mL/min and a proteinuria < 2 g/d are required. Inclusion criteria: (1) Uncontrolled DM (severe hypoglycemia, hyperglycemia or ketoacidosis) that compromise the quality of life; and (2) Failure of the continuous subcutaneous insulin infusion and continuous glucose monitoring[37,47].
Pancreas transplantation within these patients is limited to a stringent group. Survival of the patients and grafts are similar to type 1 DM if the following selection criteria are fulfilled: (1) 5 or more years with insulin therapy; (2) Insulin requirements < 75 IU/d; (3) BMI ≤ 30 kg/m2; and (4) Fulfillment of type 1 DM indications[37].
Patients with a lower insulin secretion should be noted. Although it is hard to establish these values based on the C-peptide values, a feasible option could be considering C-peptide values < 5 ng/mL.
The following assessments are completed prior to pancreas transplantation: (1) Medical history, physical examination, previous red blood cell transfusions, etc.; (2) Immunological studies: Blood type, human leukocyte antigen, cytotoxic antibodies, luminex, etc.; (3) Radiological exams: Abdominal ultrasound and chest and abdominal X-ray; (4) Endoscopic procedures: Colonoscopy in patients ≥ 50 years old included on the waiting list; (5) Extensive blood test including evaluation of diabetes, viral serology and prostate specific antigen in male patients older than 40 years; and (6) In patients with a history of autoimmune diseases (lupus, vasculitis, etc.), deep vein thrombosis, pulmonary embolism, acute stroke, heart attack or family history of venous thromboembolism, a complete study of thrombophilia should be performed[37,48,49].
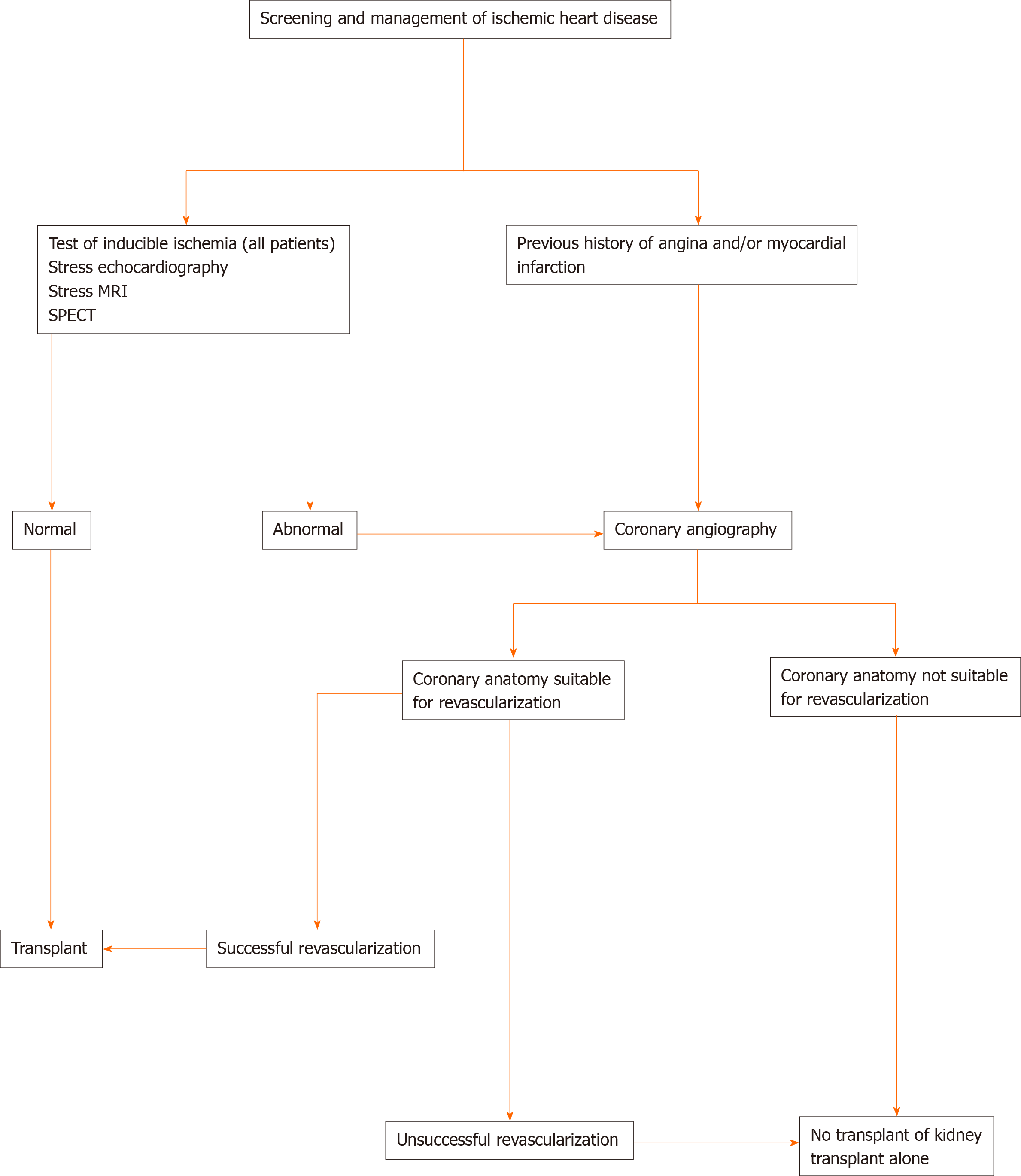
For each patient, besides the aforementioned clinical data and physical examination, a specific complication-oriented study should be performed: (1) Diabetic retinopathy screening (data regarding photocoagulation treatment and possible surgical interventions should be stored); (2) Cardiovascular evaluation: we followed the upcoming algorithm to identify the status of coronary heart disease in all pancreas transplant candidates[49] (Figure 1); (3) Assessment of the peripheral vascular disease. Evaluation of iliac axis by a computed tomographic angiography or magnetic resonance angiography. Moreover, a carotid and aortic-iliac duplex ultrasound should be performed in all patients; (4) Urological status: each recipient should be assessed by the Urology Service to assess the urological status due to the diabetic autonomic neuropathy. A prostate exam should be performed in males > 40 years; (5) Neurological evaluation: clinical assessment of the peripheral neuropathy, the nerve conduction velocity and the autonomic status; (6) Hormonal studies, C-peptide measurement and immunological markers of the DM (anti-insulin and anti-GAD antibodies); (7) Gynecological examination in fertile females (a mammography and vaginal cytology should be included in females > 35 years); (8) Evaluation by the pancreas transplant surgery team: assessment of the intestinal function, existence of associated diseases such as gallstones, state of vascular axis and previous abdominal surgery; (9) Complete infectious diseases screening; and (10) Psychological evaluation (if needed).
The following items are contraindications of a pancreas transplantation: (1) Active infection; (2) Severe coagulation abnormalities; (3) Positive crossmatch; (4) Drug addiction (including alcoholism); (5) Complex coronary artery lesions, ejection fraction < 50% and recent myocardial infarction; (6) Previous history of treatment noncompliance; (7) Severe psychiatric disorder; (8) Neoplasia; (9) Morbid obesity; and (10) Previously indicated contraindications in the kidney-pancreas transplant selection criteria[37].
Knowledge of the risk factors for pancreas transplantation allows the establishment of reliable selection criteria for choosing donors and recipients.
| 1. | Sutherland DE, Gruessner RW, Dunn DL, Matas AJ, Humar A, Kandaswamy R, Mauer SM, Kennedy WR, Goetz FC, Robertson RP, Gruessner AC, Najarian JS. Lessons learned from more than 1,000 pancreas transplants at a single institution. Ann Surg. 2001;233:463-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 504] [Cited by in RCA: 428] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 2. | Sutherland DE, Gruessner R, Gillingham K, Moudry-Munns K, Dunn D, Brayman K, Morel P, Najarian JS. A single institution's experience with solitary pancreas transplantation: a multivariate analysis of factors leading to improved outcome. Clin Transpl. 1991: 141-152. [PubMed] |
| 3. | Cicalese L, Giacomoni A, Rastellini C, Benedetti E. Pancreatic transplantation: a review. Int Surg. 1999;84:305-312. [PubMed] |
| 4. | Schulz T, Schenker P, Flecken M, Kapischke M. Donors with a maximum body weight of 50 kg for simultaneous pancreas-kidney transplantation. Transplant Proc. 2005;37:1268-1270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Van der Werf WJ, Odorico J, D'Alessandro AM, Knechtle S, Becker Y, Collins B, Pirsch J, Hoffman R, Sollinger HW. Utilization of pediatric donors for pancreas transplantation. Transplant Proc. 1999;31:610-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Krieger NR, Odorico JS, Heisey DM, D'Alessandro AM, Knechtle SJ, Pirsch JD, Sollinger HW. Underutilization of pancreas donors. Transplantation. 2003;75:1271-1276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 96] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 7. | Fernandez LA, Turgeon NA, Odorico JS, Leverson G, Pirsch JD, Becker BN, Chin LT, Becker YT, Knechtle SJ, Foley DP, Shames BD, Kalayoglu M, D'Alessandro AM, Sollinger HW. Superior long-term results of simultaneous pancreas-kidney transplantation from pediatric donors. Am J Transplant. 2004; 4:2093-2101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 37] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Neidlinger NA, Odorico JS, Sollinger HW, Fernandez LA. Can 'extreme' pancreas donors expand the donor pool? Curr Opin Organ Transplant. 2008;13:67-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Rhein T, Metzner R, Uhlmann D, Serr F, Caca K, Weinert D, Hauss J, Witzigmann H. Pediatric donor organs for pancreas transplantation: an underutilized resource? Transplant Proc. 2003;35:2145-2146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Gruessner AC, Barrou B, Jones J, Dunn DL, Moudry-Munns K, Najarian JS, Sutherland DE, Gruessner RW. Donor impact on outcome of bladder-drained pancreas transplants. Transplant Proc. 1993;25:3114-3115. [PubMed] |
| 11. | Bonham CA, Kapur S, Dodson SF, Dvorchik I, Corry RJ. Potential use of marginal donors for pancreas transplantation. Transplant Proc. 1999;31:612-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Odorico JS, Heisey DM, Voss BJ, Steiner DS, Knechtle SJ, D'Alessandro AM, Hoffmann RM, Sollinger HW. Donor factors affecting outcome after pancreas transplantation. Transplant Proc. 1998;30:276-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 44] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Douzdjian V, Gugliuzza KG, Fish JC. Multivariate analysis of donor risk factors for pancreas allograft failure after simultaneous pancreas-kidney transplantation. Surgery. 1995;118:73-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Douzdjian V, Rice JC, Carson RW, Gugliuzza KG, Fish JC. Renal allograft failure after simultaneous pancreas-kidney transplantation: univariate and multivariate analyses of donor and recipient risk factors. Clin Transplant. 1996;10:271-277. [PubMed] |
| 15. | Troppmann C, Gruessner AC, Benedetti E, Papalois BE, Dunn DL, Najarian JS, Sutherland DE, Gruessner RW. Vascular graft thrombosis after pancreatic transplantation: univariate and multivariate operative and nonoperative risk factor analysis. J Am Coll Surg. 1996;182:285-316. [PubMed] |
| 16. | Troppmann C, Gruessner AC, Papalois BE, Sutherland DE, Matas AJ, Benedetti E, Gruessner RW. Delayed endocrine pancreas graft function after simultaneous pancreas-kidney transplantation. Incidence, risk factors, and impact on long-term outcome. Transplantation. 1996;61:1323-1330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 53] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Troppmann C, Gruessner AC, Dunn DL, Sutherland DE, Gruessner RW. Surgical complications requiring early relaparotomy after pancreas transplantation: a multivariate risk factor and economic impact analysis of the cyclosporine era. Ann Surg. 1998;227:255-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 153] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 18. | Humar A, Kandaswamy R, Granger D, Gruessner RW, Gruessner AC, Sutherland DE. Decreased surgical risks of pancreas transplantation in the modern era. Ann Surg. 2000;231:269-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 191] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 19. | Gruessner AC, Sutherland DE. Analysis of United States (US) and non-US pancreas transplants reported to the United network for organ sharing (UNOS) and the international pancreas transplant registry (IPTR) as of October 2001. Clin Transpl. 2001: 41-72. [PubMed] |
| 20. | Boggi U, Del Chiaro M, Signori S, Vistoli F, Amorese G, Croce C, Morelli L, Vanadia Bartolo T, Pietrabissa A, Barsotti M, Rizzo G, Mosca F. Pancreas transplants from donors aged 45 years or older. Transplant Proc. 2005;37:1265-1267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Boggi U, Del Chiaro M, Vistoli F, Signori S, Vanadia Bartolo T, Gremmo F, Marchetti P, Coppelli A, Rizzo G, Mosca F. Pancreas transplantation from marginal donors. Transplant Proc. 2004;36:566-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | Salvalaggio PR, Schnitzler MA, Abbott KC, Brennan DC, Irish W, Takemoto SK, Axelrod D, Santos LS, Kocak B, Willoughby L, Lentine KL. Patient and graft survival implications of simultaneous pancreas kidney transplantation from old donors. Am J Transplant. 2007;7:1561-1571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 68] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 23. | Kandaswamy R, Stock PG, Gustafson SK, Skeans MA, Curry MA, Prentice MA, Fox A, Israni AK, Snyder JJ, Kasiske BL. OPTN/SRTR 2016 Annual Data Report: Pancreas. Am J Transplant. 2018;18 Suppl 1:114-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 62] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 24. | Kandaswamy R, Stock PG, Gustafson SK, Skeans MA, Urban R, Fox A, Odorico JS, Israni AK, Snyder JJ, Kasiske BL. OPTN/SRTR 2017 Annual Data Report: Pancreas. Am J Transplant. 2019;19 Suppl 2:124-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 25. | Gruessner RW, Sutherland DE, Troppmann C, Benedetti E, Hakim N, Dunn DL, Gruessner AC. The surgical risk of pancreas transplantation in the cyclosporine era: an overview. J Am Coll Surg. 1997;185:128-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 106] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 26. | Vinkers MT, Rahmel AO, Slot MC, Smits JM, Schareck WD. How to recognize a suitable pancreas donor: a Eurotransplant study of preprocurement factors. Transplant Proc. 2008;40:1275-1278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 83] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 27. | Axelrod DA, Sung RS, Meyer KH, Wolfe RA, Kaufman DB. Systematic evaluation of pancreas allograft quality, outcomes and geographic variation in utilization. Am J Transplant. 2010;10:837-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 204] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 28. | Schenker P, Vonend O, Ertas N, Wunsch A, Viebahn R. Preprocurement pancreas allocation suitability score does not correlate with long-term pancreas graft survival. Transplant Proc. 2010;42:178-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Hesse UJ, Sutherland DE. Influence of serum amylase and plasma glucose levels in pancreas cadaver donors on graft function in recipients. Diabetes. 1989;38 Suppl 1:1-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 22] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 30. | Nghiem DD, Cottington EM, Corry RJ. Pancreas donor criteria. Transplant Proc. 1988;20:1007-1009. [PubMed] |
| 31. | Kapur S, Bonham CA, Dodson SF, Dvorchik I, Corry RJ. Strategies to expand the donor pool for pancreas transplantation. Transplantation. 1999;67:284-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 68] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 32. | Wright FH, Wright C, Ames SA, Smith JL, Corry RJ. Pancreatic allograft thrombosis: donor and retrieval factors and early postperfusion graft function. Transplant Proc. 1990;22:439-441. [PubMed] |
| 33. | Schmid T, Königsrainer A, Steiner E, Koller J, Margreiter R. Do donor age and cold-ischemia time have a detrimental effect on early pancreas-allograft function? Diabetes. 1989;38 Suppl 1:4-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 34. | D'Alessandro AM, Stratta RJ, Sollinger HW, Kalayoglu M, Pirsch JD, Belzer FO. Use of UW solution in pancreas transplantation. Diabetes. 1989;38 Suppl 1:7-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 35. | Humar A. Pancreas donors. Curr Opin Organ Transplant. 2007;12:73-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 36. | Humar A, Ramcharan T, Kandaswamy R, Gruessner RW, Gruessner AC, Sutherland DE. Technical failures after pancreas transplants: why grafts fail and the risk factors--a multivariate analysis. Transplantation. 2004;78:1188-1192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 203] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 37. | National Transplant Organization. Documento de consenso sobre criterios de selección de donante y receptor en trasplante de páncreas. [Internet]. 2018. Available from: http://www.ont.es/infesp/DocumentosDeConsenso/Doc.Consenso Criterios Selección Don y Recep Tx Páncreas3.pdf. |
| 38. | Montero N, Webster AC, Royuela A, Zamora J, Crespo Barrio M, Pascual J. Steroid avoidance or withdrawal for pancreas and pancreas with kidney transplant recipients. Cochrane Database Syst Rev. 2014;(9): CD007669. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 39. | Rudolph EN, Dunn TB, Sutherland DER, Kandaswamy R, Finger EB. Optimizing outcomes in pancreas transplantation: Impact of organ preservation time. Clin Transplant. 2017;31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 40. | Benedetti E, Gruessner AC, Troppmann C, Papalois BE, Sutherland DE, Dunn DL, Gruessner RW. Intra-abdominal fungal infections after pancreatic transplantation: incidence, treatment, and outcome. J Am Coll Surg. 1996;183:307-316. [PubMed] |
| 41. | Khubutia MS, Pinchuk AV, Dmitriev IV, Balkarov AG, Storozhev RV, Anisimov YA. Surgical complications after simultaneous pancreas-kidney transplantation: A single-center experience. Asian J Surg. 2016;39:232-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 42. | Lakey JR, Warnock GL, Rajotte RV, Suarez-Alamazor ME, Ao Z, Shapiro AM, Kneteman NM. Variables in organ donors that affect the recovery of human islets of Langerhans. Transplantation. 1996;61:1047-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 228] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 43. | Humar A, Ramcharan T, Kandaswamy R, Gruessner RW, Gruessner AG, Sutherland DE. The impact of donor obesity on outcomes after cadaver pancreas transplants. Am J Transplant. 2004;4:605-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 70] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 44. | Singh RP, Vrakas G, Hayek S, Hayek S, Anam S, Aqueel M, Olsburgh J, Calder F, Mamode N, Callaghan C, Kessaris N, Pattison J, Hilton R, Koffman G, Taylor JD, Drage MW. Clinically significant peripancreatic fluid collections after simultaneous pancreas-kidney transplantation. Transplantation. 2013;95:1263-1269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 45. | Redfield RR, Scalea JR, Odorico JS. Simultaneous pancreas and kidney transplantation: current trends and future directions. Curr Opin Organ Transplant. 2015;20:94-102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 46. | Siskind E, Maloney C, Akerman M, Alex A, Ashburn S, Barlow M, Siskind T, Bhaskaran M, Ali N, Basu A, Molmenti E, Ortiz J. An analysis of pancreas transplantation outcomes based on age groupings--an update of the UNOS database. Clin Transplant. 2014;28:990-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 47. | Redfield RR, Rickels MR, Naji A, Odorico JS. Pancreas Transplantation in the Modern Era. Gastroenterol Clin North Am. 2016;45:145-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 48. | Alhamad T, Stratta RJ. Pancreas-kidney transplantation in diabetes mellitus: Patient selection and pretransplant evaluation. [Internet]. Available from: https://www.uptodate.com/contents/pancreas-kidney-transplantation-in-diabetes-mellitus-patient-selection-and-pretransplant-evaluation. |
| 49. | Mangus RS, Powelson J, Kinsella SB, Farar DT, Creal CA, Fridell JA. Pretransplant coronary artery disease associated with worse clinical outcomes in pancreas transplantation. Clin Transplant. 2013;27:E442-E447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Transplantation
Country/Territory of origin: Spain
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ching SM S-Editor: Huang P L-Editor: Filipodia P-Editor: Wang LL