©The Author(s) 2026.
World J Transplant. Mar 18, 2026; 16(1): 103656
Published online Mar 18, 2026. doi: 10.5500/wjt.v16.i1.103656
Published online Mar 18, 2026. doi: 10.5500/wjt.v16.i1.103656
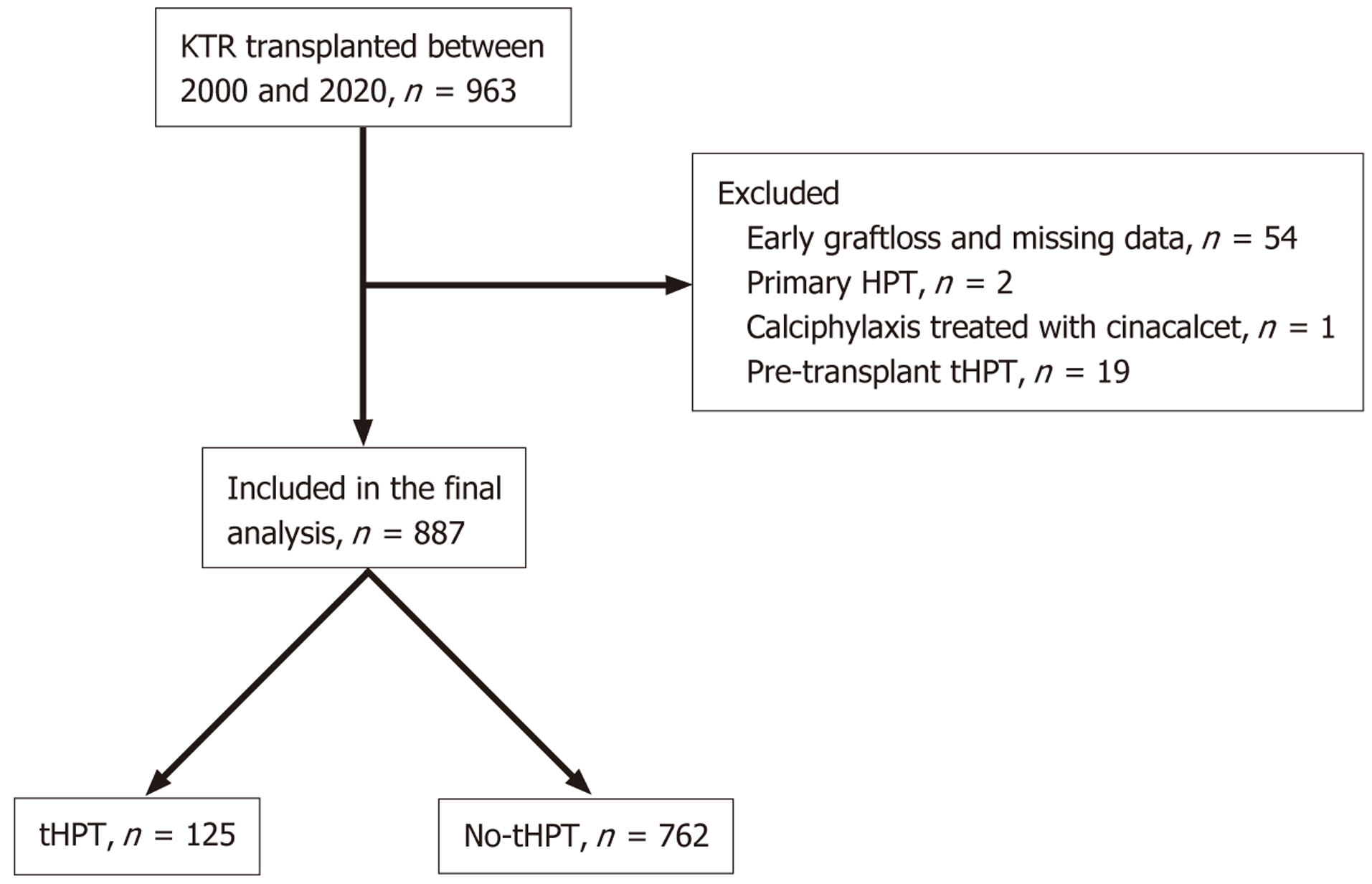
Figure 1 Flow diagram of the study cohort selection.
A total of 963 kidney transplant recipients transplanted between 2000 and 2020 were screened. Of these, 76 patients were excluded due to early graft loss or missing data (n = 54), primary hyperparathyroidism (HPT) (n = 2), calciphylaxis treated with cinacalcet (n = 1), or pre-transplant tertiary HPT (tHPT) (n = 19). The final analysis included 887 patients, of whom 125 developed post-transplant tHPT and 762 did not. HPT: Hyperparathyroidism; KTR: Kidney transplant recipient; tHPT: Tertiary hyperparathyroidism.
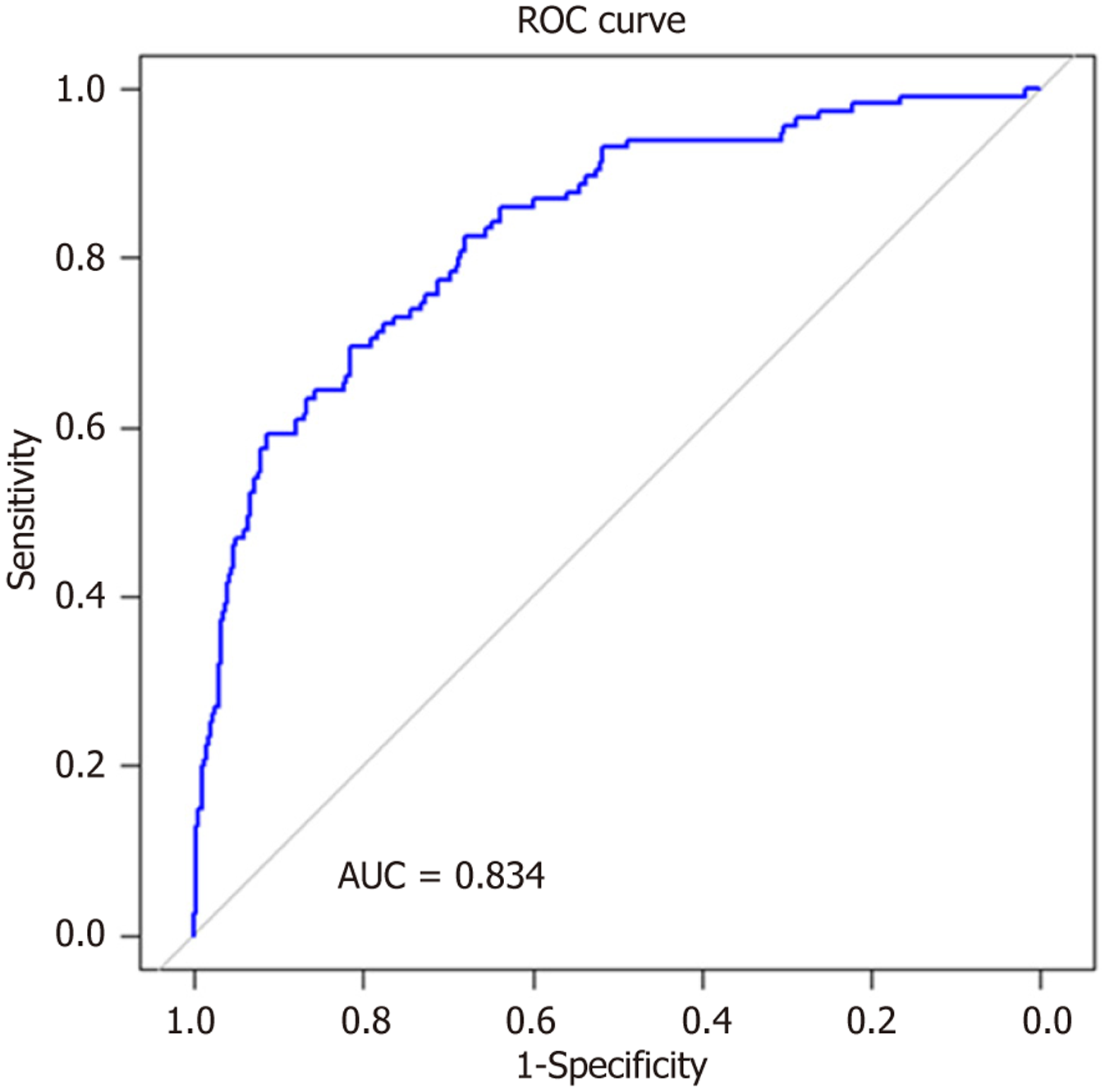
Figure 2 Receiver operating characteristic curve for the logistic regression model predicting post-transplant tertiary hyperparathyr
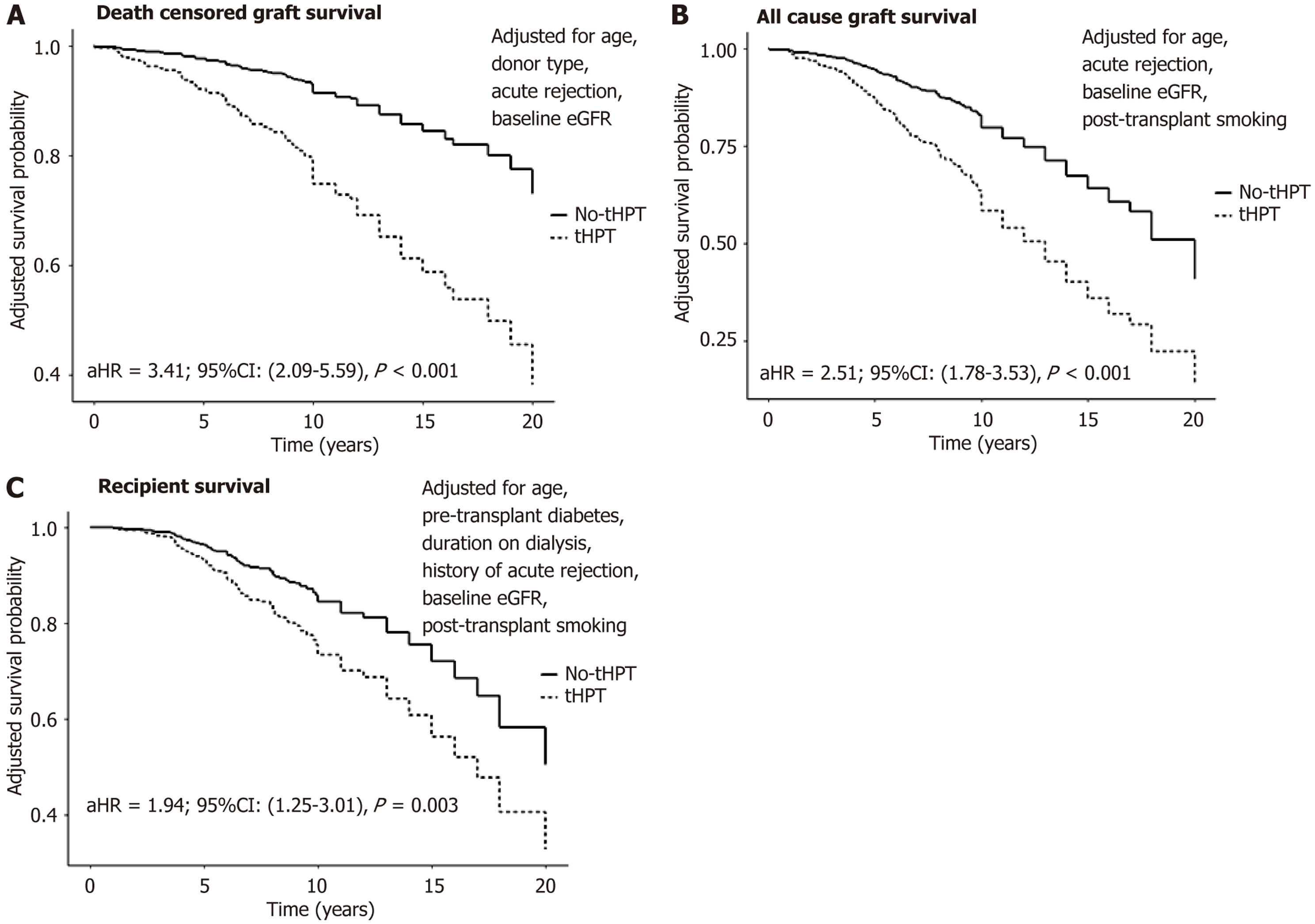
Figure 3 Adjusted survival analysis comparing outcomes in kidney transplant recipients with post-transplant tertiary hyperpara
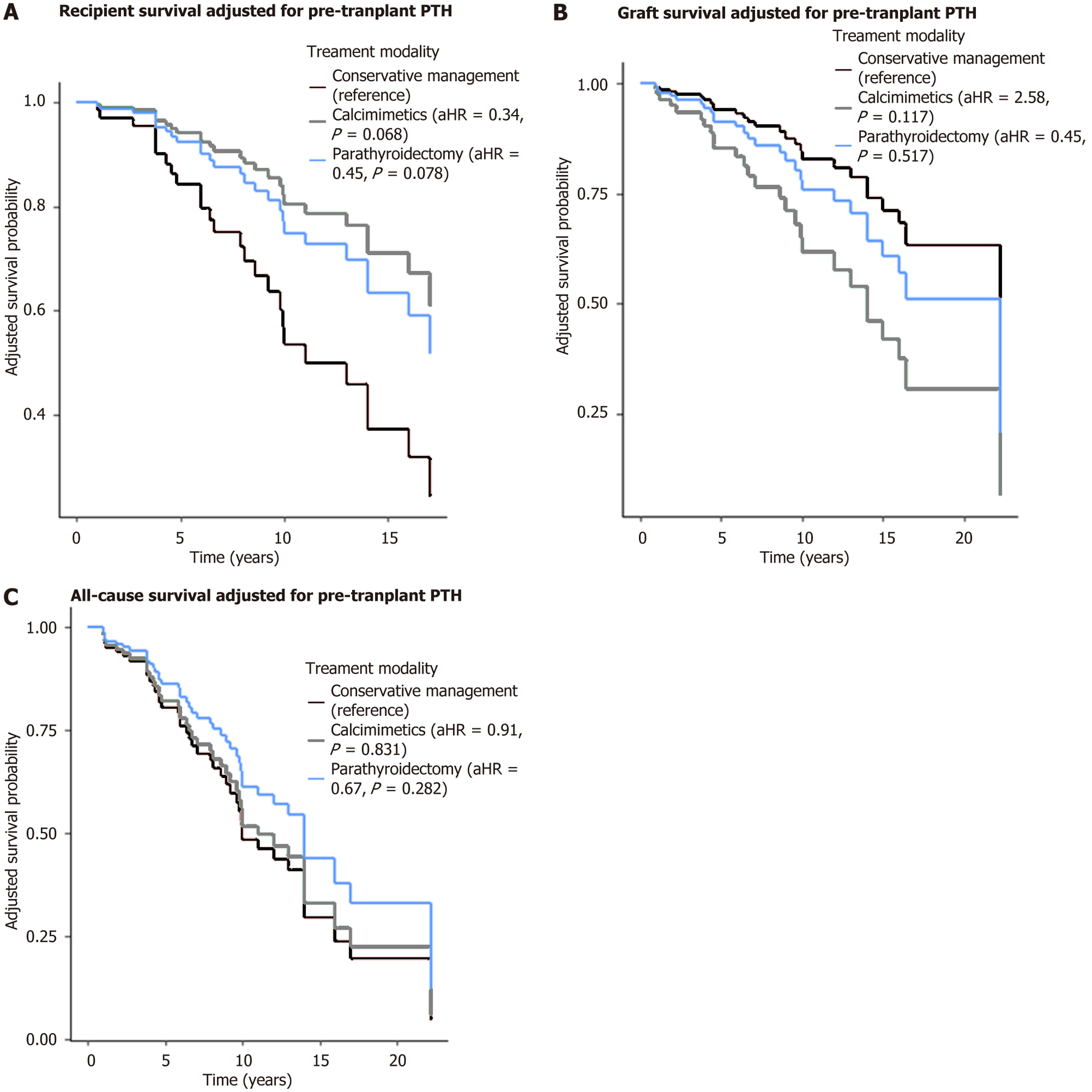
Figure 4 Survival probability (adjusted for pre-transplant parathyroid hormone).
A: Recipient survival by treatment modality; B: Graft survival by treatment modality; C: All-cause survival by treatment modality. Adjusted hazard ratio and P values are shown in the legend for each treatment group, using conservative management as the reference category. There was no statistically significant difference in recipient survival in those who received active treatment compared to those managed conservatively. Cox regression survival curves were adjusted for baseline pre-transplant parathyroid hormone levels using multivariable Cox proportional hazards models. aHR: Adjusted hazard ratio; PTH: Parathyroid hormone.
- Citation: Hanson S, Menendez Lorenzo J, Chukwu CA, Rao A, Middleton R, Kalra PA. Incidence, risk factors and survival outcomes of post-transplant tertiary hyperparathyroidism in kidney recipients. World J Transplant 2026; 16(1): 103656
- URL: https://www.wjgnet.com/2220-3230/full/v16/i1/103656.htm
- DOI: https://dx.doi.org/10.5500/wjt.v16.i1.103656