©The Author(s) 2024.
World J Transplant. Jun 18, 2024; 14(2): 93567
Published online Jun 18, 2024. doi: 10.5500/wjt.v14.i2.93567
Published online Jun 18, 2024. doi: 10.5500/wjt.v14.i2.93567
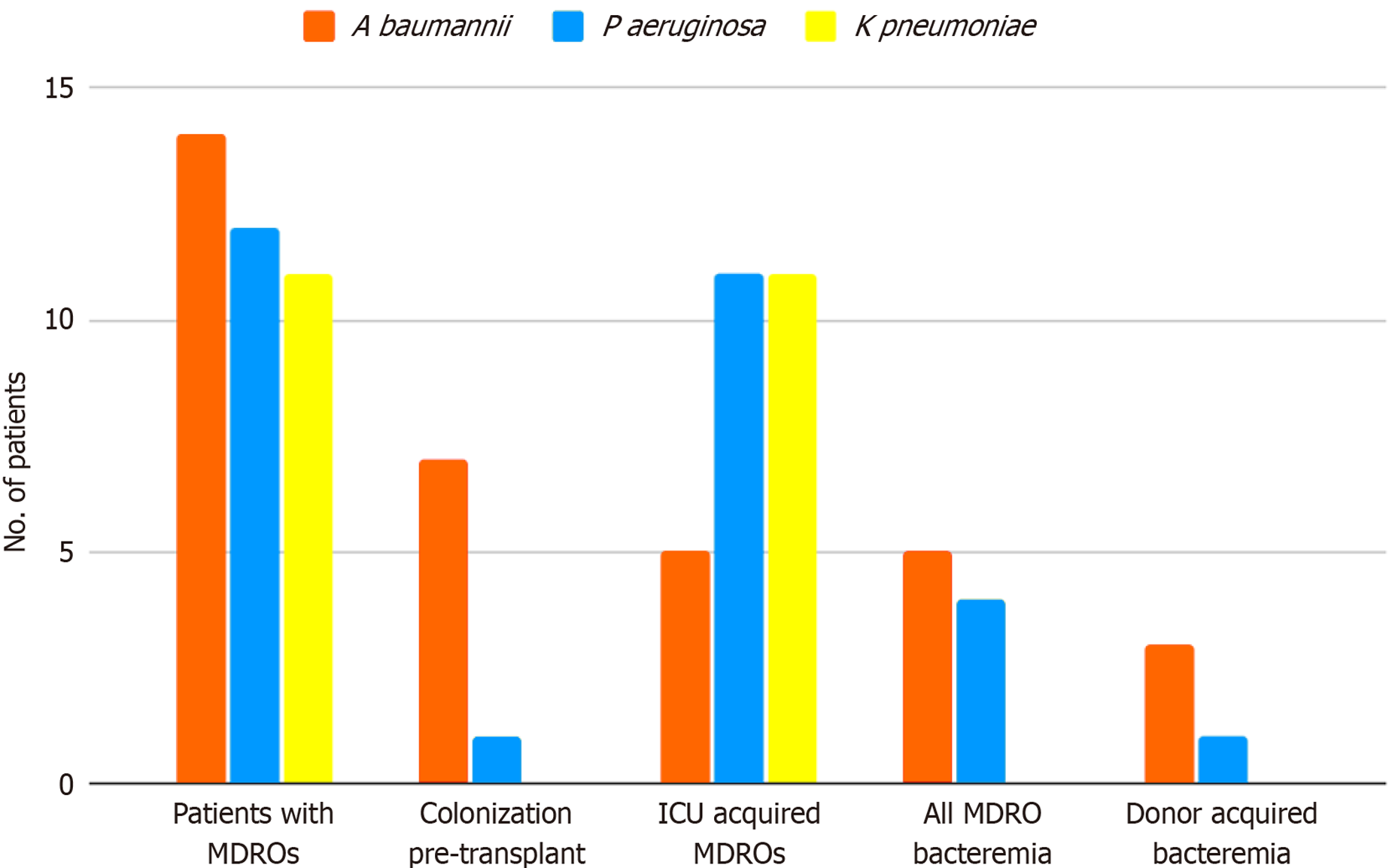
Figure 1 Multidrug-resistant organism carriage and bacteremia in heart transplantation patients (n = 98).
Transplanted patients with multidrug-resistant organisms (MDROs): Acinetobacter baumannii was the most prevalent MDRO, followed by Pseudomonas aeruginosa and Klebsiella pneumoniae. MDRO acquisition: Half of the patients with Acinetobacter and a single patient with Pseudomonas were already colonized pre-transplantation, while most Pseudomonas strains and all Klebsiella strains were intensive care unit acquired. MDRO bacteremia was noted in about a third of Acinetobacter and Pseudomonas carriers. Four cases of MDRO bacteremia were donor-acquired (the donor was subsequently found to have been bacteremic at the time of organ procurement). All MDRO bacteremias were due to Gram-negative pathogens. MDRO: Multidrug-resistant organism.
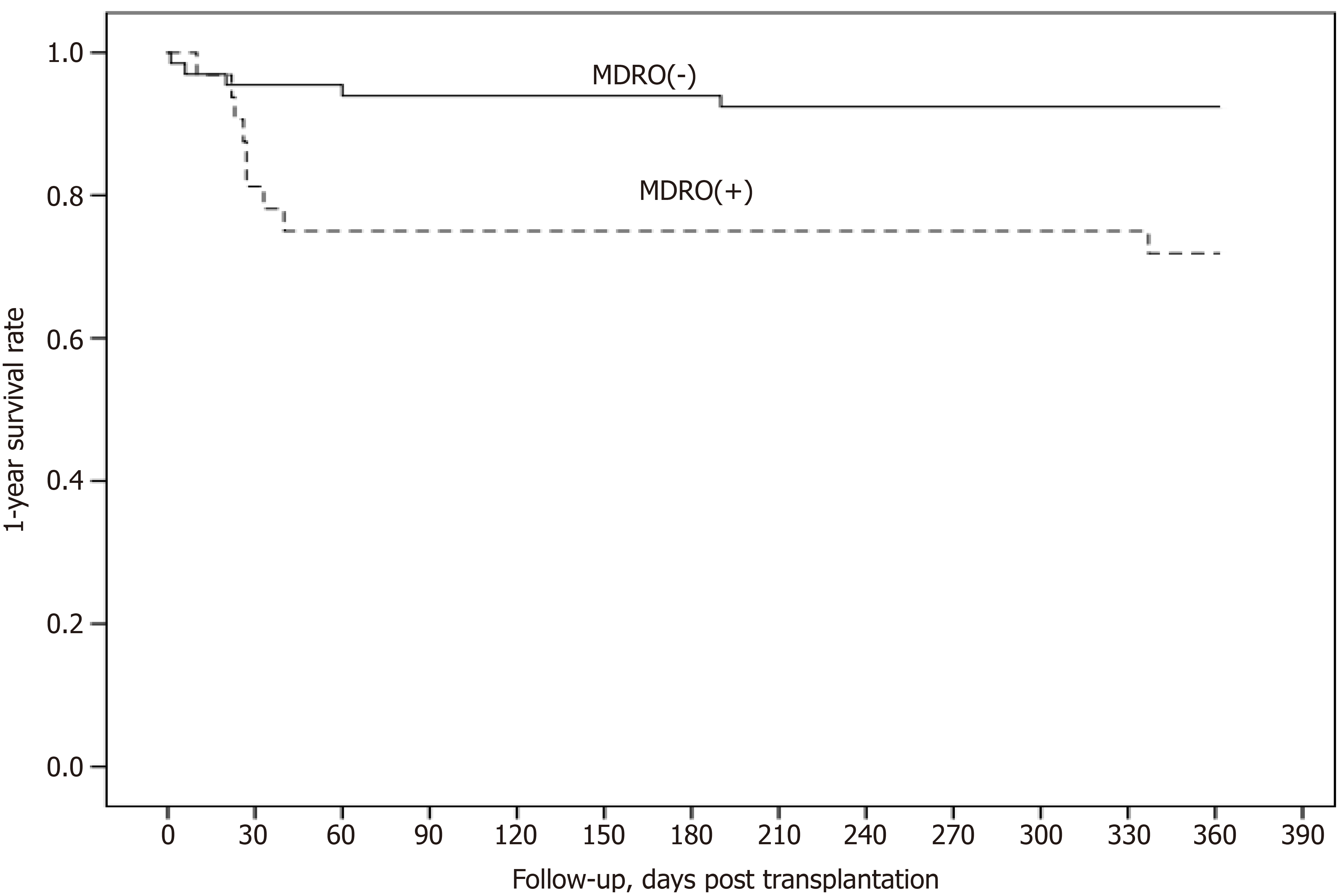
Figure 2 Post-transplantation 1-year survival according to multidrug-resistant organism status.
1-year survival was 72% in heart transplant recipients with multidrug-resistant organism (MDRO) presence (MDRO+) vs 92% in MDRO-free (MDRO-) recipients (P < 0.01). MDRO: Multidrug-resistant organism.
- Citation: Hatzianastasiou S, Vlachos P, Stravopodis G, Elaiopoulos D, Koukousli A, Papaparaskevas J, Chamogeorgakis T, Papadopoulos K, Soulele T, Chilidou D, Kolovou K, Gkouziouta A, Bonios M, Adamopoulos S, Dimopoulos S. Incidence, risk factors and clinical outcome of multidrug-resistant organisms after heart transplantation. World J Transplant 2024; 14(2): 93567
- URL: https://www.wjgnet.com/2220-3230/full/v14/i2/93567.htm
- DOI: https://dx.doi.org/10.5500/wjt.v14.i2.93567