Published online Dec 20, 2025. doi: 10.5493/wjem.v15.i4.114554
Revised: October 1, 2025
Accepted: November 26, 2025
Published online: December 20, 2025
Processing time: 87 Days and 22 Hours
Clinical hypnosis has been proposed as a non-pharmacological intervention in pediatric healthcare, drawing on children’s natural capacity for imagination and focused attention. It has been applied across a broad spectrum of medical and psychological conditions, yet its true clinical value remains a matter of debate. This narrative review synthesizes findings from randomized controlled trials, cohort studies, systematic reviews, and clinical case series on pediatric hypno
Core Tip: Clinical hypnosis has emerged as a developmentally appropriate, non-pharmacological tool with potential applications across pediatric medicine. Evidence suggests benefits in acute and chronic pain, functional gastrointestinal disorders, anxiety, habit disorders, and supportive care in chronic illness. By engaging children’s imagination and suggestibility, hypnotherapy may promote self-regulation, reduce symptom burden, and improve quality of life. However, the evidence base remains uneven—strong in some domains but limited or preliminary in others. Misconceptions, limited training op
- Citation: Al-Beltagi M. Clinical hypnosis in pediatric care: An adjunctive tool or therapeutic illusion. World J Exp Med 2025; 15(4): 114554
- URL: https://www.wjgnet.com/2220-315x/full/v15/i4/114554.htm
- DOI: https://dx.doi.org/10.5493/wjem.v15.i4.114554
Clinical hypnosis is a focused therapeutic technique that harnesses guided attention, vivid imagery, and positive su
| Aspect | Clinical hypnosis | Stage hypnosis |
| Primary purpose | Therapeutic: To facilitate healing and positive change for psychological, medical, or behavioral conditions (e.g., anxiety, pain, phobias) | Entertainment: To amuse, impress, and entertain an audience by showcasing unusual hypnotic phenomena |
| Guiding intent | Client-centered: The entire process is designed for the well-being, benefit, and empowerment of the individual client | Audience-centered: The process is designed to be dramatic, funny, and engaging for the people watching the show |
| Setting | Private & confidential: A professional clinical environment (e.g., hospital, therapy office, private practice) | Public & performative: A public stage, performance venue, or social gathering |
| Practitioner | Licensed healthcare professional: A trained and licensed professional (e.g., psychologist, physician, dentist, clinical social worker) with specific certification in hypnotherapy | Performer/entertainer: Often a charismatic performer with training in showmanship and rapid induction techniques, but typically without formal healthcare or psychological credentials |
| Training & certification | Rigorous & accredited: Requires graduate-level healthcare education followed by specialized, accredited training and certification from professional boards (e.g., ASCH, SCEH) | Unregulated: Training varies widely from mentorships to private courses. There are no formal, universally recognized educational or licensing standards |
| Ethical oversight | Strictly governed: Bound by the ethical codes and legal statutes of their respective healthcare professions (e.g., confidentiality, "do no harm") | No Formal governance: Lacks formal ethical oversight. The primary "rule" is to put on a good show, though responsible performers avoid outright harm |
| Subject selection | Client-initiated: Individuals actively seek therapy for a specific problem. Suitability is assessed, but the primary goal is to help the individual seeking treatment | Volunteer-based & screened: Participants are volunteers from the audience, often implicitly or explicitly screened for high suggestibility and extroversion to ensure compliance and a good performance |
| Consent | Informed & specific: A formal process where the client understands the therapeutic goals, methods, potential risks, and benefits, and gives explicit consent for treatment | General & implied: Volunteers agree to be on stage but may not fully understand what will be asked of them. Consent is often influenced by peer pressure and the desire to be part of the show |
| Techniques used | Individualized & evidence-based: Techniques are carefully selected and tailored to the client's specific needs, personality, and therapeutic goals | Standardized & rapid: Uses fast, authoritarian induction methods designed for maximum effect on a group in a short amount of time. The focus is on creating observable behaviors |
| Client safety & dignity | Paramount concern: Protecting the client's physical and emotional safety and dignity is the highest priority. Confidentiality is legally required | Secondary to entertainment: While most performers avoid true danger, participants may be put in embarrassing or undignified situations for comedic effect. There is no expectation of privacy |
| Duration of effect | Designed for long-term change: Aims to create lasting changes in perception, behavior, or symptom management that persist long after the session ends | Transient & short-lived: Effects are intended to last only for the duration of the show. Suggestions are typically removed before the participant leaves the stage |
| Documentation & follow-up | Standard practice: Sessions are meticulously documented in the client's confidential medical record. Follow-up is integral to assessing progress and adjusting treatment | None: No documentation, record-keeping, or follow-up care is provided to participants |
| Examples of use | Pain management (chronic pain, childbirth, surgery), anxiety reduction, habit control (e.g., smoking cessation), phobia treatment, PTSD symptom management | Making participants forget their names, believe they are a celebrity, dance uncontrollably, or react to absurd suggestions for the audience's amusement |
The application of hypnosis in pediatric populations has a rich history, with its roots tracing back over a century to early reports of its use in pain management, surgical preparation, and behavior modification. Hypnosis gained further credibility in the mid-20th century, with growing clinical observations and research highlighting its effectiveness in children[3]. Children, due to their imaginative minds, natural suggestibility, and often reduced psychological resistance, are particularly receptive to hypnotic techniques. Despite these promising attributes, hypnosis largely remained a niche approach until recent years, when the rise of integrative medicine sparked renewed interest in its potential[4].
Modern pediatric care increasingly emphasizes non-invasive, non-pharmacological interventions, driven by concerns about medication overuse, potential side effects, and the overarching need for more holistic patient care. Clinical hypnosis aligns perfectly with this evolving paradigm, offering a safe and adaptable adjunct to conventional treatments across various domains, including procedural pain, anxiety, gastrointestinal (GI) disorders, and behavioral conditions. As healthcare systems continue to prioritize patient-centered approaches and psychological well-being, hypnosis is emerging as a therapeutic tool in the pediatric arsenal[5]. However, despite growing enthusiasm, the clinical evidence remains uneven, and questions persist regarding its true therapeutic efficacy.
The relevance of hypnosis in child health is more pronounced now than ever. Children grappling with chronic illness, challenging medical procedures, or significant psychological distress require management strategies that are both effective and empowering[6]. Hypnosis not only offers symptom relief but also equips children with crucial self-re
This comprehensive review aims to critically evaluate the role of clinical hypnosis in pediatric healthcare. It examines the underlying neurocognitive mechanisms, surveys its diverse clinical applications across a wide range of pediatric conditions, and highlights both its potential advantages and its current limitations compared to conventional treatments. By synthesizing the available evidence and identifying gaps in knowledge, training, and accessibility, this review seeks to inform pediatricians, child psychologists, and allied health professionals about the promise-and the uncertainties-of hypnotherapy. Ultimately, it emphasizes the need for cautious, evidence-based integration of hypnosis into pediatric care while outlining priorities for future research and clinical practice.
We conducted this review through a narrative synthesis of the existing literature on pediatric clinical hypnosis, using a comprehensive search of electronic databases, including PubMed, Scopus, Web of Science, and Google Scholar, for studies published in English up to August 2025. Search terms combined keywords such as “pediatric hypnosis”, “clinical hypnotherapy”, “children”, “adolescents”, “pain management”, “functional disorders”, “anxiety”, and “non-pharmacological therapy”. Both randomized controlled trials (RCTs), cohort studies, systematic reviews, and relevant case series were considered. Reference lists of key papers were also manually screened to identify additional studies. Studies focusing exclusively on adult populations were not included except where a brief reference was necessary to contextualize pediatric findings. Because this is a narrative review, no formal quality assessment tool was applied; instead, emphasis was placed on peer-reviewed studies with clear methodology, adequate sample sizes, and clinical relevance. This approach ensured a broad yet clinically focused synthesis, while acknowledging that methodological diversity may limit direct comparisons between studies.
Clinical hypnosis is a unique and dynamic state of focused attention and increased suggestibility, accompanied by reduced peripheral awareness and a heightened responsiveness to therapeutic guidance. Figure 1 shows the core components of clinical hypnosis. Crucially, this is not a state of unconsciousness or sleep, but a distinct neurocognitive condition that involves both biological and psychological modulation. Advances in functional neuroimaging have significantly clarified the neural mechanisms underlying hypnosis, revealing consistent changes in brain activity, connectivity, and neurochemical signaling[8].
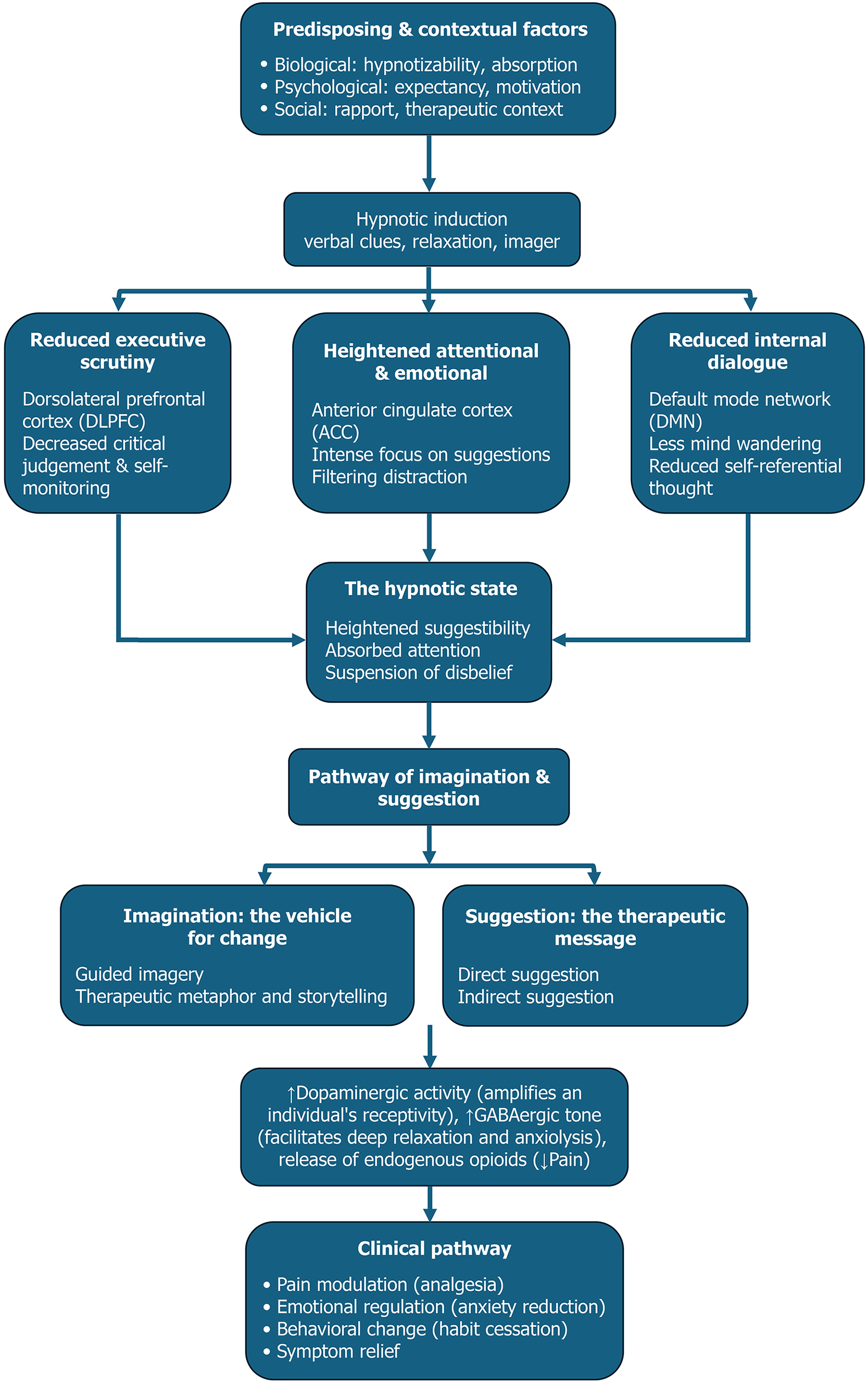
At the core of the hypnotic state lies a functional reorganization of brain networks. The anterior cingulate cortex (ACC)-a region essential for attention control, emotional regulation, and conflict monitoring-is consistently activated during hypnosis. In contrast, there is a reduction in the activity or functional connectivity of the dorsolateral prefrontal cortex, which typically governs executive control and critical evaluation. This decoupling helps explain why individuals under hypnosis become less constrained by rational filtering and more open to therapeutic suggestion[9]. Additionally, hypnosis is associated with a downregulation of the default mode network, which is responsible for self-referential thought and mind-wandering, fostering a deep immersion in the therapeutic experience. These shifts align closely with patients’ subjective reports of narrowed focus, heightened absorption, and diminished internal distraction-especially beneficial in children with shorter attention spans[10].
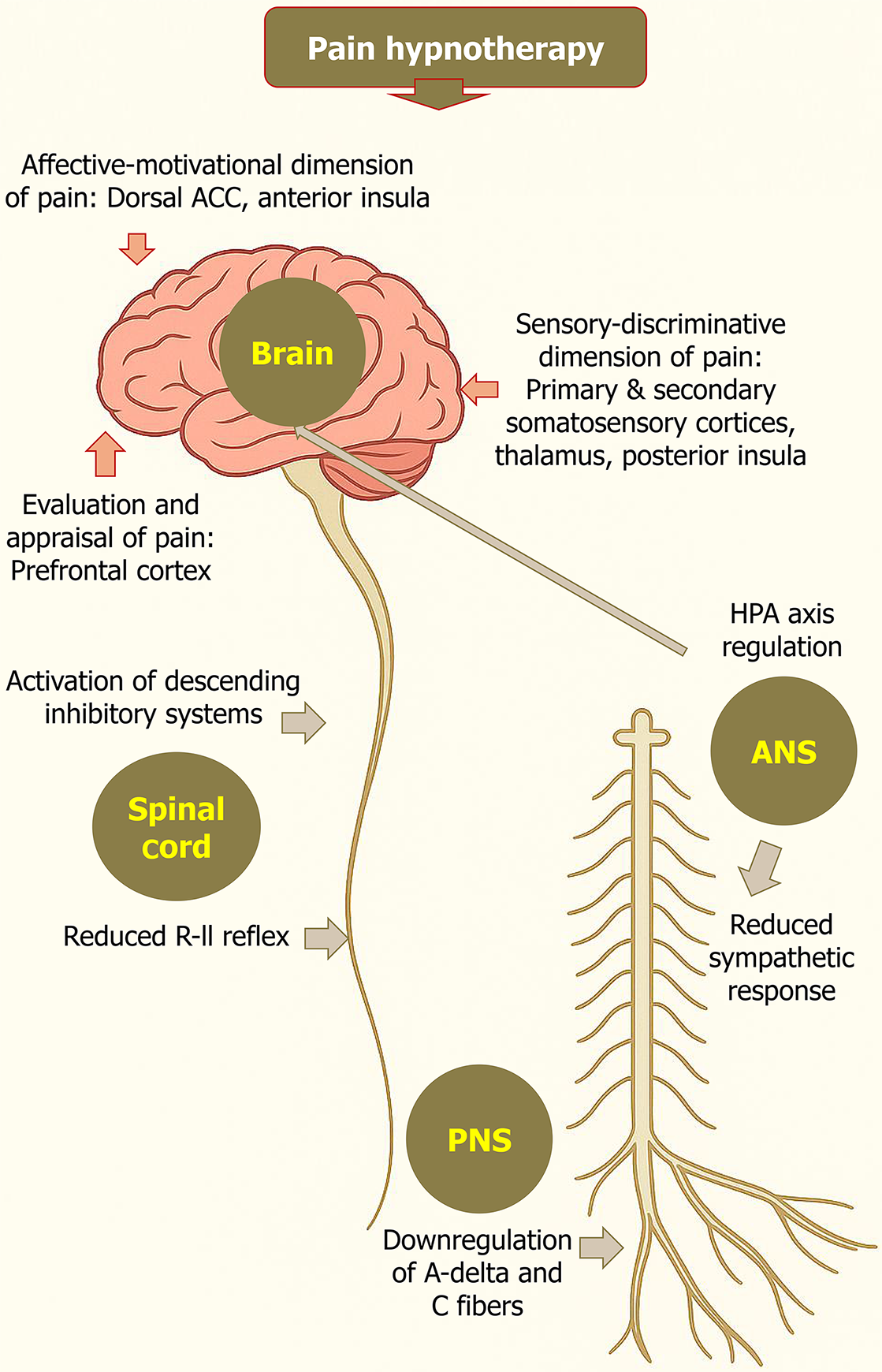
Hypnosis also exerts multi-level effects on pain processing. At the cortical level, it alters the sensory-discriminative aspects of pain via the primary and secondary somatosensory cortices, the thalamus, and the posterior insula. The emotional-motivational dimension of pain is modulated through the anterior insula and dorsal ACC, while cognitive appraisal and re-framing of pain occur in the prefrontal cortex[11]. Hypnosis can also influence pain transmission at the spinal level by activating descending inhibitory pathways and reducing the R-III reflex-a spinal marker of nociception[12]. Moreover, it affects the autonomic nervous system by decreasing sympathetic tone and modulating the hypotha
On a neurochemical level, hypnosis appears to modulate key neurotransmitter systems. Dopaminergic activity, particularly in the striatum, is enhanced-supporting motivation, attention, and reward processing, all of which increase receptivity to suggestion. GABAergic tone is thought to increase during hypnosis, facilitating deep relaxation by da
Of particular interest in children is the brain’s remarkable neuroplasticity. Pediatric hypnosis capitalizes on this developmental window, during which repeated hypnotic sessions-incorporating positive imagery, metaphors, and behavioral reframing-can strengthen beneficial neural circuits through long-term potentiation, the fundamental mechanism of learning and memory[16]. Functional magnetic resonance imaging (MRI) studies suggest that hypnotically induced alterations in connectivity between sensorimotor, limbic, and executive control networks can persist beyond the hypnotic state, supporting long-lasting therapeutic change[9]. For developing brains, this represents a powerful opportunity: Hypnosis is not only a tool for symptom relief but also a method of reshaping maladaptive patterns and reinforcing adaptive ones[17].
Psychologically, two dominant frameworks inform our understanding of hypnosis. The neodissociation theory posits that hypnosis induces a division in consciousness, allowing suggestions to bypass usual cognitive filters while a “hidden observer” retains awareness[18]. In contrast, sociocognitive theories emphasize the influence of expectations, social context, and the therapeutic relationship, viewing hypnotic behavior as an enactment shaped by belief and motivation. These models are not mutually exclusive and likely work in tandem, especially in pediatric patients[19]. Children’s vivid imaginations, fluid cognitive structures, and natural responsiveness to social cues render them particularly susceptible to both dissociative and expectancy-driven mechanisms[20].
Developmental factors further amplify hypnotic responsiveness in children-especially those aged five to twelve-who consistently demonstrate higher suggestibility than adults. This is not due to gullibility, but reflects neurodevelopmental features such as an immature prefrontal cortex, greater reliance on imaginative cognition, and limited internal skepticism[4]. These attributes allow children to enter hypnotic states more easily and respond more deeply to metaphor, guided imagery, and sensory-based suggestions, making hypnosis particularly effective in pediatric settings[16].
Imagination, in fact, serves as the cornerstone of pediatric hypnotherapy. Techniques such as storytelling, guided imagery, and symbolic metaphors are developmentally tailored to engage a child’s sensory world and internal narrative. A child afraid of a medical procedure might imagine being in a superhero’s fortress or adjusting a pain “volume dial” in a brain-based control room[21]. These strategies are more than distractions-they actively engage brain regions involved in perception, regulation, and belief, creating a neurological basis for therapeutic transformation. Figure 3 summarizes the neuro-cognitive pathway of hypnosis, from influencing factors to clinical outcomes[8].
Finally, from an ethical and safety standpoint, clinical hypnosis in pediatric populations is considered safe when conducted by qualified professionals. It respects the child’s autonomy and emphasizes collaboration, never control. Informed consent from caregivers and assent from the child are essential[22]. As an adjunct-not a replacement-to standard care, hypnosis aligns with the principles of integrative medicine, offering a low-risk, high-benefit strategy that empowers children to manage symptoms, develop resilience, and participate actively in their own healing process[7]. It is important to note, however, that mechanistic insights-such as altered brain connectivity, neurotransmitter modulation, or engagement of neuroplastic processes-do not automatically translate into consistent clinical benefit. While these findings provide biological plausibility and support for the therapeutic potential of hypnosis, the strength of clinical outcomes in pediatric populations remains variable. It requires confirmation through well-designed, large-scale trials.
While the core principles of hypnosis-inducing a state of focused attention and heightened suggestibility-remain consistent across all ages, the practice of hypnotherapy with children is a specialized discipline that differs fundamentally from its adult counterpart[21]. These distinctions are not superficial; they are rooted in the unique developmental, cognitive, and relational landscape of childhood, demanding significant adaptations in technique, therapeutic alliance, and ethical considerations[23].
The most profound divergence lies in cognitive and developmental factors. Children, particularly in their primary school years, possess a natural and powerful capacity for vivid imagination, coupled with a less developed critical filter. This makes them exceptionally receptive to hypnotic suggestion when delivered through the language they understand best: Storytelling, metaphor, and play[24]. A pediatric therapist might guide a child to imagine a superhero's shield for protection from pain or a magic glove for needle-related procedures. In contrast, adult hypnotherapy must often navigate a more established analytical mindset, potential skepticism, and a lifetime of ingrained beliefs. Consequently, adult-focused techniques frequently rely on more direct suggestions, structured scripts, and insight-oriented approaches that appeal to a mature cognitive framework[4].
These differences directly influence the therapeutic relationship and session structure. Establishing rapport with a child is an active, often playful process that involves using toys, drawing, or engaging in informal conversation to build trust and comfort. With adults, this alliance is typically forged through empathetic conversation and a more formal discussion of goals and concerns[25]. This leads to pediatric sessions being shorter, more flexible, and dynamic, accommodating a child's variable attention span. Furthermore, pediatric hypnotherapy is uniquely characterized by the integral role of parents, creating a triadic therapeutic alliance among the therapist, child, and caregiver. Parents provide crucial background information, offer support during the process, and are essential for reinforcing hypnotic strategies at home-a dynamic entirely absent from adult therapy, where confidentiality and individual autonomy are paramount[26].
Ultimately, the goals and ethical boundaries of therapy are significantly influenced by the client's age. Pediatric hypnotherapy is often targeted and symptom-focused, aiming for relatively rapid relief from specific issues such as procedural anxiety, enuresis, chronic pain, or phobias[27]. While adult hypnotherapy can also be symptom-focused, it frequently delves deeper into complex psychological exploration, trauma resolution, and the unpacking of intricate cognitive-emotional patterns. This distinction informs the ethical framework: For adults, informed consent from the individual is sufficient[28]. For children, a dual process of obtaining informed consent from the legal guardian and, crucially, securing the age-appropriate assent (willing agreement) of the child is an ethical necessity, ensuring the intervention is collaborative, respectful, and empowering for the young client[29]. Table 2 summarizes the differences between pediatric vs. adult hypnotherapy.
| Feature | Pediatric hypnotherapy | Adult hypnotherapy |
| Cognitive & developmental approach | Leverages imagination and reduced critical filtering; techniques are concrete and story-based | Engages analytical reasoning and belief systems; techniques are more direct and insight-oriented |
| Therapeutic alliance & rapport | Built through playful interaction (e.g., games, drawing, storytelling) to foster trust | Built through empathetic conversation, active listening, and discussion of therapy goals |
| Imaginative engagement | Highly responsive to fantasy, symbols, and imaginative play | May be more analytical and less suggestible to symbolic or fantastical content |
| Communication style & techniques | Uses simple, multisensory imagery and playful metaphors (e.g., “magic glove”) | Uses abstract language, sophisticated metaphors, and direct cognitive-behavioral suggestions |
| Language style | Concrete, playful, and developmentally tailored | Abstract, metaphorical, and insight-driven |
| Session structure & pacing | Shorter, flexible, and dynamic to match attention span; includes playful transitions | Longer, more structured; allows sustained exploration of deeper issues |
| Session duration | Typically 20-40 minutes, adapted to the child’s mood and readiness | Typically 45-60 minutes with more consistent pacing |
| Therapeutic focus | Targets specific symptoms (e.g., pain, anxiety, enuresis); goal is rapid relief and empowerment | May address broader emotional patterns, trauma, and psychological insight |
| Support system involvement | Triadic alliance-parents contribute history, encourage participation, and reinforce strategies at home | Client works independently; support system involved only with consent (e.g., in family therapy) |
| Parental role | Actively involved during and between sessions | Not involved unless part of a joint therapeutic approach |
| Consent & ethical framework | Requires dual process: Informed consent from guardian + age-appropriate assent from the child | Solely requires informed consent from the adult client |
Pediatric clinical hypnotherapy is a specialized therapeutic approach that leverages children’s rich imagination, developmental stage, and innate responsiveness to create a safe, engaging, and effective healing experience. In contrast to adult hypnotherapy, which often employs more structured or directive methods, pediatric hypnotherapy is highly adaptable, playful, and centered on the child’s needs and preferences[21]. It emphasizes gentle guidance, collaboration, and the therapeutic power of imagination. There are four core principles essential for a successful clinical hypnotherapy session in children: Child-centered and developmentally tailored, indirect and permissive language, imaginative engagement and playfulness, and strength-based and resource-oriented[7]. Table 3 summarizes the different categories of clinical hypnotherapy techniques for children.
| Category | Technique | Description | Primary clinical application |
| Foundational imaginative techniques | Guided imagery/"safe place" | Guiding the child to create a multi-sensory, immersive experience of a safe, pleasant, or empowering environment (e.g., a beach, spaceship, magical forest) | Anxiety reduction, establishing rapport, creating a receptive state for further therapeutic work |
| Storytelling & therapeutic metaphor | Embedding therapeutic ideas within a narrative structure that reframes the child's problem and offers solutions indirectly (e.g., a story about a scared lion who finds its roar) | Problem-solving, reframing fears, enhancing coping skills in a non-threatening manner | |
| Pain & physical symptom control | Symptom-modifying imagery | Utilizing mental imagery to directly alter the perception of a symptom. Includes: (1) Glove anesthesia: Transferring imagined numbness; (2) Control panel/dials: Adjusting intensity; and (3) Transforming qualities: Changing the color/shape/temperature of pain | Direct modulation of pain, discomfort, or other physical sensations (e.g., itch, nausea) |
| Dissociative imagery | Guiding the child to imagine separating from the sensation, such as watching the pain on a screen, placing it in a box, or floating away from their body | Reducing the emotional component (suffering) of pain; managing overwhelming sensations | |
| Behavioral & habit reversal | Imaginative rehearsal & future pacing | Guiding the child to mentally rehearse successfully navigating a future challenging situation (e.g., a medical procedure, a school presentation) while feeling calm and confident | Building competence and positive expectancy; reducing anticipatory anxiety |
| Gentle aversion imagery | Associating an unwanted habit (e.g., nail-biting) with a mildly unpleasant but not frightening image or sensation (e.g., a bitter taste, a gritty texture) | Discouraging habits like thumb-sucking, nail-biting, or trichotillomania | |
| Ego-strengthening and empowerment | Ego-strengthening suggestions | Using direct suggestions and metaphors focused on building the child's sense of self-worth, resilience, and inner resources (e.g., "You have a special strength inside you") | Universal application to improve self-esteem, coping, and a sense of agency. Often integrated into all other techniques |
| Core linguistic techniques | Permissive & indirect language | Phrasing suggestions in an open, invitational manner ("You might begin to notice...", "Perhaps you can imagine...") that respects the child's autonomy | Bypassing resistance, fostering a sense of control and collaboration, empowering the child |
| Direct suggestion | Clear, positive, goal-oriented statements, often couched in permissive language ("And you can allow yourself to feel calm and relaxed") | Reinforcing desired changes, providing clear direction when the child is highly receptive |
Every session is customized to align with the child’s cognitive level, emotional maturity, interests, and specific challenges. Therapists often incorporate familiar characters, games, or themes the child enjoys, ensuring the experience feels relatable and safe. Rather than using commands, therapists employ permissive and open-ended language such as, “You might begin to notice…” or “Perhaps you can imagine…” This strategy encourages participation without pressure, enhancing the child’s sense of autonomy and reducing resistance[16,30]. Hypnotherapy taps into children's natural capacity for fantasy, pretend play, and storytelling. Therapeutic sessions are framed as creative adventures, making the process enjoyable and non-threatening while fostering emotional openness. The approach focuses on activating the child’s internal resources-such as resilience, creativity, and courage-to build confidence and develop effective coping mechanisms. Positive reinforcement is consistently embedded in the hypnotic work[21].
There are various techniques in pediatric hypnotherapy, including guided imagery and imaginative journeys, storytelling and metaphorical healing, permissive direct suggestions, ego-strengthening techniques, pain management strategies, creative aversion techniques, and future pacing. In guided imagery and imaginative Journeys, children are led through vivid, multi-sensory visualizations to calming or magical “safe spaces” (e.g., enchanted forests, superhero hideouts, underwater kingdoms). These mental environments serve as therapeutic platforms where healing narratives unfold-for example, imagining a “worry monster” shrinking and being locked away during a session on anxiety[31]. In storytelling and metaphorical healing, therapists craft or adapt therapeutic stories embedded with metaphors relevant to the child’s experience[32]. For example, a tale about a young explorer overcoming a storm may represent a child ma
Various pain management strategies, such as glove anesthesia, mental control panels, altering sensory qualities, dissociation techniques, creative aversion techniques, and future pacing, can be used to reduce organic and functional pain in children. In glove anesthesia, children imagine wearing a magical glove that numbs their hand. The numbness is then mentally transferred to a specific area experiencing pain, reducing discomfort[35]. In mental control panels, children are guided to visualize an internal control panel with sliders or dials that can be turned down to relieve pain, anxiety, or other distressing sensations. Therapists can also alter sensory qualities to help children change the sensory characteristics of their discomfort-such as imagining pain becoming smaller, cooler, or changing color-thereby reframing the pain perception[36].
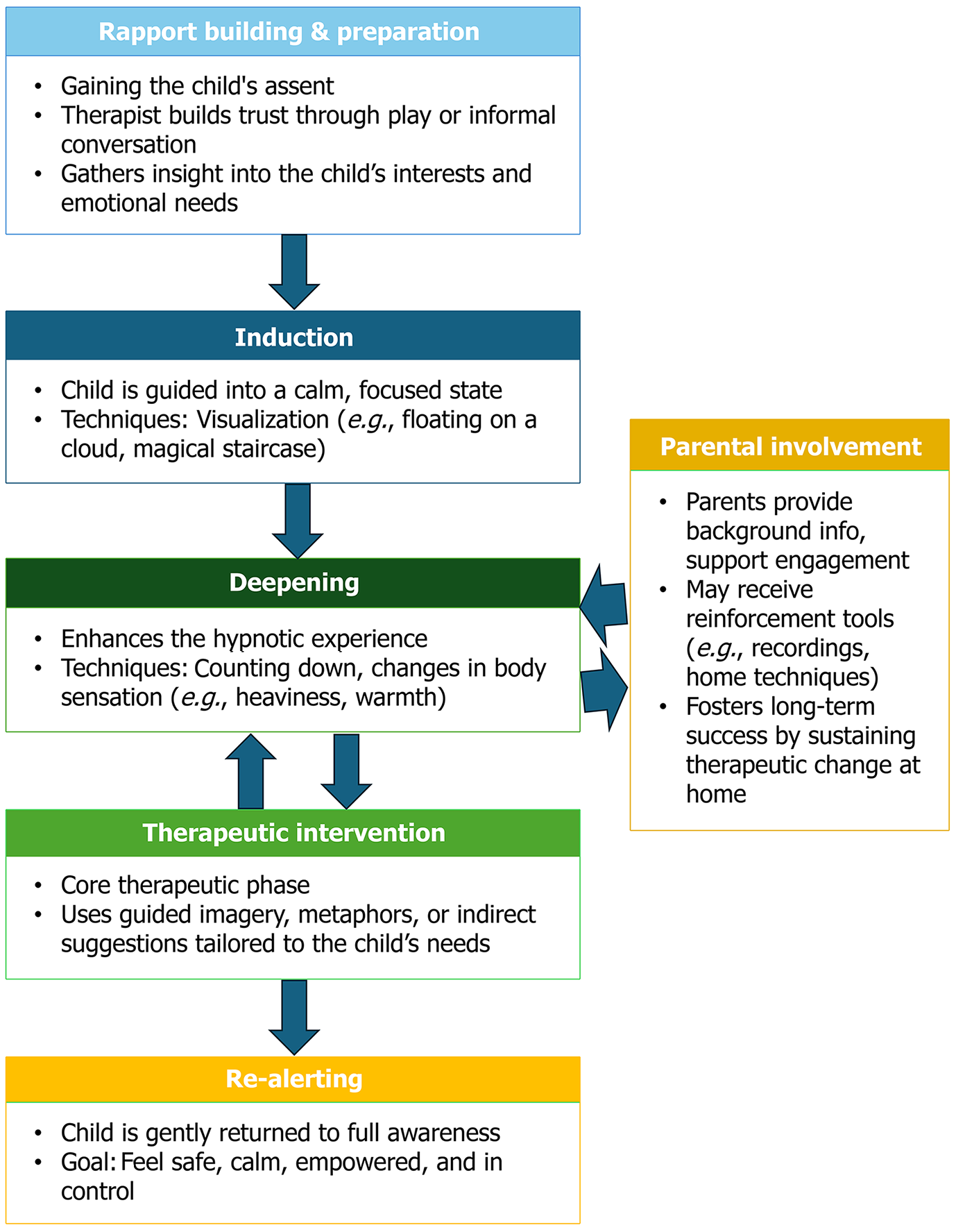
In dissociation techniques, children may be encouraged to imagine their pain floating away, being placed outside their body, or turning into something manageable and distant[37]. Creative aversion techniques can be used to manage habit disorders, such as thumb-sucking, where imaginative aversion can be gently introduced. For example, suggesting that the finger may taste unpleasant when placed in the mouth, while always maintaining a positive, supportive tone. In future pacing, children are encouraged to visualize themselves successfully using their new coping skills in upcoming real-life situations, reinforcing therapeutic gains and building confidence in their self-efficacy[38-40]. In all these techniques, the pediatric hypnotherapist should act as a warm, responsive guide-building rapport through playful interaction, active listening, and empathy. A soft, rhythmic voice and the ability to follow the child’s lead are essential. Flexibility is key, as the therapist must continuously adjust their approach based on the child’s cues and level of engagement to maintain the hypnotic focus[21]. A typical pediatric hypnotherapy session follows a structured, yet flexible format designed to meet the child’s developmental and emotional needs (Figure 4). It begins with rapport building and preparation, where the therapist engages the child through informal conversation or play to establish trust and gain insight into the child's interests and concerns[16]. This is followed by the induction phase, in which the child is guided into a focused, relaxed state using gentle and imaginative techniques such as visualizing themselves floating like a cloud or walking down a magical staircase[41]. The deepening stage follows, involving methods such as counting down or imagining shifts in bodily sensations-such as feeling heavier, lighter, warmer, or cooler-to enhance the depth of the hypnotic experience[1]. Once the child is comfortably immersed, the therapeutic intervention takes place, often involving guided imagery, metaphorical stories, or indirect suggestions carefully tailored to address the child’s specific challenge. The session concludes with re-alerting, where the child is gently and gradually returned to full awareness, typically feeling calm, safe, empowered, and in control[42].
Parents or caregivers play an essential supportive role. They provide background information, encourage the child’s engagement, and often learn simple reinforcement techniques or receive audio recordings for home practice. Repeated exposure to hypnotherapy reinforces new neural pathways and coping strategies, enhancing long-term outcomes and strengthening the child’s sense of control and well-being. Involving the family also fosters a supportive environment that sustains therapeutic change beyond the session[16].
Pediatric hypnotherapy has become a versatile and evidence-based therapeutic approach that assists children with a wide range of clinical conditions. By harnessing the child's imagination and suggestibility, hypnotherapy can be effectively used in various medical and psychological settings[7]. Its clinical applications include pain management-covering both acute procedural pain, such as needle phobia, and chronic pain conditions like headaches and fibromyalgia-as well as functional somatic disorders, including irritable bowel syndrome (IBS) and enuresis[43]. Additionally, it plays a valuable role in addressing behavioral and psychological issues such as anxiety, phobias, sleep problems, and habitual disorders. Hypnotherapy also functions as a supportive measure for symptom relief in chronic organic illnesses like cancer, cystic fibrosis (CF), and inflammatory bowel disease (IBD), particularly in reducing pain, nausea, and anxiety[44]. It enhances patient comfort during diagnostic and surgical procedures, supports neurodevelopmental [e.g., attention-deficit/hyperactivity disorder (ADHD)] and psychosomatic conditions [e.g., functional neurological disorders (FND)], and aids in addressing pediatric dermatological issues, including warts and eczema[42]. Through its flexibility and child-centered approach, hypnotherapy makes a significant contribution to comprehensive pediatric care. An expanding body of clinical research highlights the therapeutic benefits of hypnotherapy across a wide range of pediatric conditions[21]. Drawing upon key studies and well-established clinical observations, hypnotherapy has demonstrated both efficacy and safety in treating physical and psychological conditions in children and adolescents. This section synthesizes current evidence by condition, age group, and intervention method[45]. Tables 4 and 5 summarize the different clinical applications of hypnosis in pediatric medicine with the degree of recommendation.
| Medical domain | Specific applications & conditions | Degree of recommendation |
| Pain management | Acute procedural pain: Venipuncture, intravenous cannulation, lumbar puncture, bone marrow aspiration, burn dressing, dental procedures, post-operative pain, suturing, catheterization. Chronic/recurrent pain: Functional abdominal pain, migraines, tension headaches, fibromyalgia, sickle cell crises, juvenile arthritis, CRPS, neuropathic, and phantom pain | A |
| Anxiety & phobias | Procedural anxiety, preoperative fear, needle phobia (trypanophobia), dental phobia, “white coat” syndrome, generalized anxiety, separation anxiety, social and performance anxiety, panic attacks | A |
| Oncology | Pain from procedures and treatment, chemotherapy-induced nausea and vomiting (especially anticipatory), procedural anxiety, fatigue, emotional coping, and appetite improvement | A |
| Gastroenterology | IBS, functional abdominal pain, dyspepsia, cyclic vomiting syndrome, functional nausea, encopresis, constipation, rumination syndrome, IBD-related pain, and anxiety | B |
| Neurology/behavioral health | Tics, Tourette's, habit cough, PNES, FND, sleep disorders, nocturnal enuresis, anger and impulse control issues, and bruxism | B |
| Dermatology | Atopic dermatitis (itch-scratch cycle), warts, trichotillomania, excoriation disorder, psoriasis, and neurodermatitis | B |
| Pulmonology | Asthma-related anxiety, hyperventilation syndrome, procedural anxiety in cystic fibrosis, and treatment adherence (e.g., nebulizers/inhalers) | B |
| General health & wellness | Stress management, focus and concentration (non-ADHD specific), self-esteem, habit cessation (e.g., nail biting), body image, sleep hygiene, relaxation training, and reinforcement of a healthy lifestyle | B |
| Urology | Nocturnal enuresis, functional voiding disorders, urgency/frequency syndromes, and anxiety during urodynamic testing | B |
| Rehabilitation & physical therapy | Enhancing pain tolerance during therapy, improving motivation, managing movement fear, and recovering from injury | C |
| Endocrinology & metabolism | Support for insulin injections, blood glucose monitoring, and coping with chronic illness stress (e.g., diabetes) | C |
| Condition treated | Age group | Ref. | Method used | Outcome measures | Efficacy | Level of evidence |
| Pain (acute & chronic, including procedural pain) | 5+ years, often up to adolescence | Chester et al[47], Kendrick et al[49], Miller et al[51] | Guided imagery, relaxation, direct suggestion, self-hypnosis training | Pain intensity (self-report, behavioral observation), anxiety, distress, need for analgesia, hospital stay duration | Significant reduction in pain, anxiety, and distress; reduced need for medication; shorter hospital stays. Often superior to standard care/other psychological interventions | RCTs, meta-analyses, systematic reviews |
| Pediatric headache | Children & adolescents (mean approximately 13 years) with recurrent headaches | Kohen and Zajac[61] | Self-hypnosis training for self-regulation | Headache frequency, intensity, duration | Frequency reduced from 4.5/week to 1.4/week; intensity from 10.3 to 4.7; duration from 23.6 hours to 3 hours; P < 0.01 | Level III (retrospective cohort) |
| 9-18 years with primary headaches (migraine, tension-type) | Jong et al[62] | Randomized trial: Hypnotherapy vs transcendental meditation vs progressive muscle relaxation | ≥ 50% reduction in headache frequency; pain coping; anxiety/depression | All groups improved; approximately 47% achieved ≥ 50% reduction at 9 months; no significance difference between interventions | Level I (randomized controlled trial) | |
| Children & adolescents with unspecified chronic/episodic headaches | Gysin[63] | 5-session hypnosis/self-hypnosis vs behavioral therapy | Frequency, intensity, sense of control | Hypnosis showed superior improvements in symptom control and self-regulation | Level II (comparative trial) | |
| Mean age of 15 years of children with stress-associated headaches | Anbar and Zoughbi[64] | Hypnosis + relaxation & imagery; insight exploration | Frequency/intensity change; relation to stressor type | 96% improved overall; insight generation improved outcomes in patients with fixed stressors | Level III (retrospective chart review) | |
| Adolescents with chronic daily headache | Kohen[65] | Tailored self-hypnosis instruction | Frequency, intensity, duration | Notable symptom reduction in cases unresponsive to other therapies | Level IV (case reports) | |
| IBS & FAP | School-age children, adolescents (e.g., 5-18 years) | Rutten et al[68], Vlieger et al[70], Vlieger et al[72] | Gut-directed hypnotherapy, self-hypnosis training (individual or group sessions, sometimes home-based eHealth) | Abdominal pain severity/frequency, adequate pain relief, quality of life, daily functioning, school absence, somatization | Significant reduction in pain, improved quality of life; often superior to standard medical treatment, with long-term improvements sustained at follow-ups | RCTs, cohort studies, systematic reviews |
| Nocturnal enuresis (bedwetting) | 8-13 years | Edwards and van der Spuy[77] | 6 standardized hypnotherapy sessions over 6 weeks | Decrease in enuretic episodes over 6 months | Significantly effective compared to no-treatment controls; trance induction not essential | Controlled clinical trial |
| 7-12 years | Seabrook et al[76] | Hypnotherapy with nightly audiotapes vs alarm therapy (RCT) | Success (14 dry nights), failure, relapse, self-esteem measures | Alarm therapy more effective (55.3% vs 19.4% success); hypnotherapy had lower relapse (non-significant) | RCT | |
| Anxiety disorders (general anxiety, dental anxiety, phobias) | 5-17 years | Minosh et al[81] | Hypnotherapy by trained nurse practitioner, long-term follow-up | Parent/child subjective rating (1-5 scale) | 55% of anxiety cases rated good-to-excellent; no adverse effects reported | Prospective pilot study |
| 6-10 years | Erappa et al[82] | Hypnosis vs acupressure vs audiovisual distraction | PR, RR, AR | All methods effective, but hypnosis most significant in reducing PR, RR, and AR | Randomized controlled trial | |
| 5-7 years | Girón et al[83] | Hypnosis vs tell-show-do | FLACC scale, heart rate, skin conductance | Significantly lower anxiety and pain in hypnosis group across all measures | Randomized controlled trial | |
| 3-12 years | Rienhoff et al[84] | Hypnosis + low-dose midazolam (0.4 mg/kg) | Venham score (behavior) & Wong-Baker scale | Good compliance; effective for short-term use. Slight decline in behavior over repeated sessions | Retrospective longitudinal observational study | |
| Sleep disorders | 7-17 years with Insomnia (sleep onset delay, nocturnal awakenings) | Anbar and Slothower[86] | Retrospective chart review, self-hypnosis training | Sleep onset latency, frequency of awakenings, somatic complaints | 90% improved sleep-onset latency; 52% resolution & 38% improvement in nocturnal awakenings; 87% improvement in related somatic symptoms | Level III (retrospective study) |
| 8-12 years sleep problems post-trauma (grief/Loss-related) | Hawkins and Polemikos[87] | Qualitative group-based hypnotherapy, self-hypnosis | Caregiver interviews, Southampton sleep management schedule | All participants learned self-hypnosis; qualitative improvement in sleep initiation and sleep-related anxiety reported by children and caregivers | Level IV (qualitative study) | |
| 8-12 years with sleep terror disorder/disorders of arousal | Kohen et al[88] | Case series: Self-hypnosis training ± imipramine | Polysomnography, symptom frequency, long-term follow-up | All 4 children in case report became asymptomatic over 2-3 years; similar success in 7 more patients treated with hypnosis alone | Level IV (case series) | |
| Habit disorders (e.g., habit cough, tic disorders, trichotillomania) | 8-year-old child with habit cough (case study) | Anbar[96] | Self-hypnosis; flexible rapport-building approach | Resolution of persistent cough | Rapid and complete symptom resolution in 1 session | Level IV (case report) |
| 6-17 years (n = 33) with Tics (Tourette syndrome) | Lazarus and Klein[94] | Self-hypnosis + videotaped training | Tic control via subjective report over 6 weeks | 79% showed improvement; 96% responded within 3 visits | Level IV (retrospective case series) | |
| 8-12 years (n = 4) with Tourette syndrome | Kohen and Botts[95] | Self-hypnosis (relaxation + imagery) | Tic frequency, medication reduction | Immediate and sustained improvement; reduced/ceased medication | Level IV (case series) | |
| 6-15 years (n = 5) with trichotillomania | Kohen[98] | Self-monitoring, dissociative techniques, self-hypnosis | Symptom resolution and behavior control | All children achieved control with individualized techniques | Level IV (case series) | |
| 7 years (case study) with thumb sucking | Grayson[97] | Hypnotic imagery, role-modeling, validation in trance | Cessation of habit | Successful resolution in one session | Level IV (case report) | |
| ASD | 5-10.99 years with GI symptoms, anxiety, and behavior in ASD with DGBI | Mitchell et[102] | Synbiotics alone vs synbiotics + GDHT, 12-week RCT | GI scores, anxiety levels, irritability behaviors, microbiota composition | GDHT group showed significant reductions in GI pain, anxiety, and irritability; synbiotics helped both groups | Level II (randomized controlled trial) |
| 6-year-old child with atypical autism & severe ego deficits | Gardner and Tarnow[103] | Adjunctive hypnotherapy with music integration | Specific behavior change, social/cognitive skill improvement | Behavioral goals achieved; sustained gains at 18-month follow-up | Level IV (case report) | |
| 6-12 years (approximately) who need dental cooperation and hyperactivity in ASD | Sartika et al[104] | Hypnotherapy before dental scaling (quasi-experimental) | Cooperative attitude, calculus index | Significant improvement in cooperation and reduction in calculus (P = 0.000) | Level III (Quasi-experimental design) | |
| 14-15 years with engagement, anxiety, attention in ASD | Austin et al[105] | Virtual reality hypnosis (4 sessions, feasibility study) | Engagement, parental reports on behavior and anxiety | No change in autistic symptoms, but improved engagement and relaxation; parental satisfaction noted | Level V (feasibility/pilot study) | |
| ADHD | Children (mean age approximately 10) with ADHD | Calhoun and Bolton[100] | Hypnotherapy by psychologists/physicians; attempts to hypnotize 11 children, 1 completed full session | Pre- and post-hypnosis behavioral observations | Significant improvement in behavior in the successfully hypnotized child | Low (small sample, non-randomized) |
| Children (median age 122) with low self-esteem in ADHD, epilepsy, anxiety | Hazard et al[112] | Standardized hypnosis protocol, single therapist, prospective single-center study | Self-esteem measured via Jodoin 40 scale, Piers-Harris self-concept scale, and self-rated score | Statistically significant improvement in self-esteem (P ≤ 0.05), no side effects | Moderate (pilot exploratory study) | |
| 11-year-old child with ADHD & written language disorder | Hery-Niaussat et al[113] | SCED, 4 hypnosis sessions over 8 weeks | Reading tests, phonological processing, attention, self-esteem | Statistically significant improvement in text reading (P = 0.028), attention (P = 0.031), and self-esteem (P = 0.002) | Moderate (SCED, but detailed measures) | |
| Oncology support | Children (3 cases, female) with cancer-related anxiety | Talebiazar et al[121] | Classical hypnotherapy, 8 sessions with 1-month follow-up | HADS at 5 time points | Significant reduction in hospital anxiety during and after intervention | Level 4 (case report) |
| Children (11-17 years) with Cancer-related distress & QoL | Grégoire et al[120] | Hypnosis-based group intervention with monthly 2-hour sessions | Self-reported emotional well-being, relaxation, assertiveness, and parent-child communication | High acceptability; perceived improvement in quality of life, emotional regulation, and family coping | Level 3 (pilot/quasi-experimental) | |
| Children and adolescents (0-25 years) with cancer and had Procedural anxiety & pain in | Nunns et al[118] | Meta-analysis of RCTs, 8 hypnosis studies included | Procedural anxiety, fear, distress, and pain | Large, statistically significant reductions in procedural anxiety (d = 2.30) and pain (d = 2.16) | Level 1a (meta-analysis of RCTs) | |
| CINV | Richardson et al[119] | Meta-analysis of 6 RCTs (5 in pediatric population) | Frequency/severity of anticipatory and acute CINV | Statistically significant reduction in anticipatory and acute CINV; effect comparable to CBT | Level 1a (meta-analysis of RCTs) | |
| Asthma | Children with chronic asthma | Alexander et al[128] | Relaxation training (5 sessions after control phase) | Pulmonary function, muscle tension, heart & respiratory rates, skin conductance | No significant improvement in pulmonary function; relaxed state achieved | Level III (quasi-experimental, physiological measures) |
| Pediatric to adolescent age (exact age not specified) | Morrison[127] | Hypnotherapy over 1 year | Hospital admissions, medication use, airflow, patient-reported improvement | Reduced admissions, reduced drug use, improved perceived symptoms; variable objective airflow | Level II (controlled clinical trial, small sample) | |
| Pediatric (age varied across 251 RCTs) | Moher et al[129] | Systematic review of CAM RCT reporting (including hypnosis and relaxation interventions) | CONSORT adherence, Jadad score, allocation bias, adverse event reporting | Revealed poor methodological quality and underreporting in pediatric CAM RCTs | Level I (systematic review of RCTs -methodology focus) | |
| 8-18 years with chronic dyspnea (non-organic) | Anbar[125] | Self-hypnosis instruction (1-2 sessions) with follow-up | Dyspnea frequency/severity, associated symptoms, self-reported resolution, treatment withdrawal | 13/16 resolved within 1 month; 11/16 attributed improvement to hypnosis; no recurrence during follow-up | Level IV, retrospective chart review; small number, good follow-up | |
| Cystic fibrosis | 7-18 years | Belsky and Khanna[134] | Self-hypnosis (pilot RCT with matched control) | Locus of control, trait anxiety, self-concept, peak expiratory flow rate | Significant psychological and physiological improvements in the experimental group vs control | Level II (small RCT with limitations) |
| 7-49 years (mean 18.1) | Anbar[122] | Self-hypnosis taught in 1-2 sessions, patient-reported outcomes | Symptom control (pain, headache, taste of medication), self-reported efficacy | 86% success rate; no adverse effects; high subjective benefit | Level IV (case series with self-report and no control) | |
| Inflammatory bowel disease (IBD) | 12-65 years with IBS-type symptoms in IBD | Hoekman et al[137] | Gut-directed hypnotherapy (RCT) | ≥ 50% reduction in IBS-SSS score at 6 months | No superiority over standard medical treatment | Level I (RCT) |
| Adolescents (mean age 158) with Crohn’s disease | Lee et al[138] | 1 session CH + self-hypnosis (RCT pilot) | QoL, abdominal pain, school absences | Improved parent-reported QoL & pain reduction | Level II (pilot RCT) | |
| 10-17 years with IBD | Shaoul et al[139] | 4-12 sessions tailored hypnosis | Symptom resolution, reduced inflammatory markers | Symptom resolution in most cases; well-tolerated | Level IV (case series) | |
| Adults with UC-active | Mawdsley et al[140] | 1 session gut-focused hypnosis | IL-6, SP, IL-13, rectal blood flow | Significant reduction in inflammatory markers | Level II (controlled physiological study) | |
| Adults with UC- quiescent | Keefer et al[141] | 7 sessions of gut-directed hypnotherapy vs control | Relapse rate over 1 year | 68% maintained remission vs 40% in control | Level I (RCT) | |
| Atopic dermatitis | Adults & children | Stewart and Thomas[164] | Hypnotherapy; individualized sessions | Subjective (patient reports), objective clinical assessments, long-term follow-up | Significant immediate and sustained improvement in itching, sleep disturbance, and mood (P < 0.01); maintained up to 2 years | Level II (Quasi-experimental study with control, non-randomized) |
| Adults (mean age: 34.5 years) | Delaitre et al[165] | Hypnosis (mean of 6 sessions, range 2-16) | EASI score before and after intervention | Improvement/resolution in 26 of 27 patients; mean EASI score reduced from 12 to 2.8 | Level III (prospective clinical cohort without control group) | |
| Children (> 5 years) | Derrick et al[166] | Self-hypnosis using guided imagery | Clinical assessment of eczema symptoms over 18 weeks | Mild-to-moderate benefit observed; did not reach statistical significance | Level IV (Pilot study; no control group, low statistical power) | |
| Viral warts | Adult women with HPV-related genital warts | Barabasz et al[156] | Hypnosis vs standard medical therapy | Number and size of lesions; complete clearance at 12 weeks | Statistically significant reduction in lesions with hypnosis (P < 0.04); complete clearance 5 × more likely in hypnosis group than medical therapy | Level II (randomized controlled clinical trial) |
| Adults with common warts (cutaneous) | Spanos et al[154] | Hypnotic suggestion vs placebo vs no treatment | Wart regression rates; vividness of imagery | Hypnosis and suggestion led to greater wart regression than placebo or no treatment; imagery vividness predicted better outcomes | Level II (experimental controlled design) | |
| Adults with common warts (cutaneous) | Spanos et al[155] | Hypnosis, salicylic acid, placebo, no treatment | Wart count at 6-week follow-up | Only hypnosis group had significantly more wart regression vs control; equal treatment expectation across all groups | Level I (randomized controlled trial) |
Pain management (acute and chronic): Hypnotherapy has emerged as a promising, valuable, and increasingly re
In the realm of acute pain management, hypnotherapy is frequently and effectively employed in medical settings involving painful or anxiety-provoking procedures. These commonly include venipuncture, intravenous cannulation, lumbar punctures, bone marrow aspirations, wound care, burn dressing changes, dental procedures, and even minor surgical interventions[47]. Hypnotic techniques utilized in these situations primarily focus on potent strategies such as distraction, dissociation (creating a sense of detachment from the physical sensation), and the construction of elaborate, protective mental imagery designed to shift the child's attention dramatically away from the noxious stimulus[48]. For instance, a child might be guided to imagine vividly being transported to a safe and utterly calming place-such as floating weightlessly in outer space, swimming gracefully underwater with friendly dolphins, holding an impenetrable magical shield that completely blocks discomfort, or even transforming into a powerful superhero impervious to pain. These imaginative techniques are highly effective in reducing pre-procedural anxiety, significantly lowering reported pain ratings, and often leading to a decreased reliance on pharmacological analgesics or sedatives. Robust clinical studies have consistently demonstrated that children undergoing hypnotherapy during procedures report substantially less distress, exhibit reduced physiological signs of pain (e.g., lower heart rate, stable blood pressure, decreased cortisol levels), and often experience faster recovery times post-intervention, highlighting its physiological as well as psychological benefits[49].
Within the context of chronic pain, a pervasive and debilitating issue in pediatric populations (e.g., recurrent ab
Crucially, the benefits of hypnotherapy go beyond reducing symptoms to improve important functional outcomes, such as regular school attendance, better sleep quality, increased participation in physical activities, and an overall boost in quality of life[53]. A key element of long-term success is teaching children self-hypnosis techniques, allowing them to practice these skills outside of therapy sessions on their own, which promotes independence, lasting symptom relief, and lifelong coping strategies[54]. Clinical hypnotherapy, utilizing techniques like guided imagery, relaxation, and self-hypnosis training, has consistently demonstrated significant reductions in pain intensity, anxiety, and distress in pediatric patients, often outperforming standard care[55]. This robust efficacy is substantiated by the highest tier of evidence, including RCTs, meta-analyses, and systematic reviews. Notably, research by Kohen et al[56] and Olness[57] revealed that children as young as three years old can effectively apply self-hypnosis techniques, with proficiency generally increasing with age. Their findings also indicated an inverse correlation between clinical success and the number of visits, sug
In both acute and chronic pain settings, the successful implementation of hypnotherapy is critically dependent on its delivery by trained and experienced clinicians who can expertly tailor scripts and techniques to the unique developmental level, cognitive capacity, and individual interests of each child[58]. Sessions typically involve a thoughtfully structured combination of initial rapport-building, gentle induction into the hypnotic state, careful deepening techniques, the delivery of individualized therapeutic suggestions, and "future pacing" to reinforce successful application of new skills in real-life scenarios[59]. Active involvement of caregivers is paramount, as they play a vital role in reinforcing techniques and supporting the child's practice at home, thereby ensuring the sustained integration of hypnotherapeutic benefits into daily life, which is a key component of a comprehensive, integrative pediatric pain management plan[21].
Pediatric headache: Headache is among the most common and disabling pain complaints in children and adolescents, with migraine and tension-type headaches accounting for the majority of cases. These headaches often arise from a complex interplay of genetic predisposition, stress, emotional dysregulation, sleep disturbances, and environmental triggers[60]. While pharmacological treatments remain foundational, increasing attention is being given to mind-body approaches-particularly clinical hypnotherapy-as both adjunct and primary modalities for pediatric headache mana
Hypnotherapy offers a non-invasive, safe, and empowering intervention that helps children regulate pain perception, reduce headache frequency and severity, and gain control over associated physiological and emotional responses[61]. Typically, children are guided into a focused, deeply relaxed state and taught self-hypnosis techniques such as vis
The evidence base for hypnotherapy in pediatric headache is robust and continually expanding. A retrospective study by Kohen and Zajac[61] involving 144 children and adolescents taught self-hypnosis reported significant reductions in headache frequency (4.5-1.4 per week), intensity (10.3-4.7), and duration (23.6-3.0 hours), with no adverse effects. Similarly, a randomized clinical trial by Jong et al[62] compared hypnotherapy, transcendental meditation, and pro
Other research supports hypnotherapy’s superiority in certain domains. In a comparative trial, Gysin[63] found hypnosis/self-hypnosis to be more effective than behavioral therapy or medical counseling alone in reducing headache intensity and improving the sense of self-efficacy in children with chronic or episodic headaches. In a more psychosocially oriented study, Anbar and Zoughbi[64] observed that 96% of children reported improvement with hypnosis, and highlighted the importance of insight generation, especially among children whose headaches were linked to fixed stressors. Finally, Kohen[65] presented compelling case reports of adolescents with chronic daily headaches who found dramatic relief from self-hypnosis after failing to respond to both medication and other therapies-underscoring the potential of hypnotherapy even in treatment-resistant cases.
A key distinguishing feature of hypnotherapy is its integration of deep relaxation, cognitive reframing, and ima
Pediatric functional somatic syndromes: Functional somatic syndromes in children, encompassing conditions like IBS, functional abdominal pain (FAP), and enuresis, are characterized by real and distressing symptoms despite the absence of identifiable organic pathology[67]. These pervasive conditions often lead to significant disruptions in a child's daily life, affecting school attendance, social engagement, and overall psychological well-being. Thankfully, hypnotherapy has emerged as a compelling, evidence-supported therapeutic option for these disorders. Its effectiveness lies in its unique ability to influence autonomic, GI, and urinary function through powerful psychophysiological mechanisms and ima
IBS and FAP stand as some of the most extensively studied pediatric conditions where hypnotherapy has demon
In an attempt to investigate factors that could affect the efficacy of hypnosis to relieve FAP, a 2023 exploratory study by de Bruijn et al[73] investigated whether specific genetic polymorphisms (COMT, OPRM1, and MAO-A), previously linked to adult hypnotizability, predict HT response in 144 children aged 8-18 with FAP disorders. The study found no sig
Clinical trials and strong long-term studies have consistently shown that pediatric gut-focused hypnotherapy results in significant and meaningful decreases in symptom severity, the frequency of painful episodes, and related functional disability[74]. Moreover, its effects are often notably long-lasting, with improvements persisting for months or even years after treatment ends. In addition to reducing symptoms, hypnotherapy can also positively affect GI motility, reduce visceral hypersensitivity (the increased perception of normal gut sensations), and help normalize autonomic nervous system responses, offering a truly comprehensive biopsychosocial approach. Its non-invasive, medication-free nature makes it especially attractive to families who are cautious about drug treatments or whose children do not respond to standard therapies[73].
Enuresis, particularly nocturnal enuresis (bedwetting), affects a substantial portion of school-aged children and can carry a significant emotional and social burden. While spontaneous remission is common with age, persistent cases often lead to profound embarrassment, reduced self-esteem, and disrupted sleep patterns for both the child and family[75]. Hypnotherapy provides a highly child-friendly and empowering intervention that actively encourages desired behavioral change. It works through subconscious conditioning, vivid imagery rehearsal, and powerful ego-strengthening su
During hypnotherapy sessions, children may be guided to imagine internal "bladder alarms" that signal them to wake up or "control panels" in their minds that help them manage nighttime urination. Alternatively, they might engage with stories where a character successfully learns to control bedwetting[76]. Therapists consistently incorporate confidence-building suggestions to reduce feelings of shame and foster a strong sense of mastery and achievement. Importantly, hypnotherapy respects the child's individual pace and provides a completely non-threatening, non-punitive environ
Research strongly supports the efficacy of hypnotherapy for treating nocturnal enuresis, particularly in pediatric populations. Multiple controlled studies, including randomized clinical trials, have demonstrated its therapeutic value. For instance, Edwards and van der Spuy[77] reported significant reductions in wet nights in boys aged 8-13 years fo
Pediatric hypnotherapy is a versatile and highly effective tool for addressing a broad spectrum of behavioral and psychological disorders in children and adolescents. These conditions frequently stem from, or are significantly exacerbated by, emotional dysregulation, chronic stress, trauma, or various developmental challenges[79]. Hypnosis offers a non-invasive, child-centered therapeutic modality that powerfully leverages imagination, heightened suggestibility, and inherent self-regulation capacities to address underlying psychological processes and promote adaptive behaviors[80]. Among the most common and well-supported indications for hypnotherapy in pediatric behavioral health are anxiety disorders and phobias, sleep disturbances, and habit disorders.
Anxiety disorders and phobias: Hypnotherapy is particularly effective in managing anxiety-related conditions in children, including generalized anxiety disorder, separation anxiety, social phobia, test anxiety, insomnia, and specific phobias such as trypanophobia (needle phobia) or dental anxiety[79]. A growing body of research supports its efficacy across both psychological and procedural anxiety contexts. For instance, Minosh et al[81] conducted a prospective study involving 53 children treated for anxiety, nocturnal enuresis, or insomnia. They found that 55% of those with anxiety disorders and 59% with enuresis achieved good-to-excellent long-term outcomes. No adverse effects were reported, highlighting the safety and moderate effectiveness of hypnotherapy in pediatric populations.
In dental settings, RCTs have demonstrated even more compelling evidence for hypnosis as a tool for anxiety and pain reduction. Erappa et al[82] compared hypnosis with acupressure, audiovisual aids, and no intervention in 200 children aged 6-10 receiving local anesthesia. Hypnosis led to the most significant reductions in anxiety indicators, including pulse rate, respiratory rate, and observed anxiety behavior, outperforming all other interventions. Similarly, Girón et al[83] found that hypnosis was significantly more effective than the standard tell-show-do behavioral technique in lowering anxiety and pain during pulpotomy procedures, as measured by the FLACC scale, heart rate, and skin conductance throughout all treatment phases.
Children often experience anxiety as a vague, overwhelming sensation that is difficult for them to articulate, un
In cases of procedural or phobia-related anxiety, systematic desensitization can be embedded within the hypnotic trance. For example, a child with needle phobia might imagine themselves as a superhero who grows stronger and braver with each imagined encounter with a needle, eventually translating this confidence into real-life calm. A large-scale observational study by Rienhoff et al[84] involving over 300 children aged 3-12 treated with both midazolam and hy
Sleep disturbances: Sleep disturbances-including insomnia, bedtime resistance, night awakenings, nightmares, and sleep terrors-are common among children, especially during periods of stress, grief, or developmental transition. These issues often overlap with anxiety, somatic complaints, and emotional dysregulation[85]. Hypnotherapy offers a safe, non-pharmacological intervention that targets both the psychological roots and behavioral manifestations of pediatric sleep disorders. Through personalized imagery, ego-strengthening techniques, and relaxation training, children are empo
Neurodevelopmental disorders commonly present with sleep disturbances. In a pivotal retrospective chart review by Anbar and Slothower[86], 84 school-aged children (ages 7-17) with insomnia were treated using self-hypnosis techniques. Remarkably, 90% of those with prolonged sleep-onset latency experienced a significant reduction in the time it took to fall asleep. Additionally, 52% of children with frequent nocturnal awakenings reported complete resolution, while another 38% reported notable improvement. The study also found that 87% of children with related somatic complaints (e.g., chest pain, abdominal pain, habit cough) showed marked improvement following hypnotic intervention, highlighting hyp
Hypnotic strategies for sleep commonly include calming bedtime scripts, progressive muscle relaxation, and guided imagery tailored to the child’s interests and developmental level. For example, children might be led to imagine floating gently on a cloud, drifting along a peaceful river, or being protected by a magical animal companion. These scripts not only lower physiological arousal but also create positive, soothing mental associations with sleep, replacing anxiety-driven narratives with safe and empowering ones[89,90]. Evidence from clinical studies and expert practice indicates that hypnotherapy reduces sleep latency, improves sleep continuity, and decreases nighttime fear and arousals, particularly when combined with psychoeducation and cognitive reframing. As sleep quality improves, children often experience a range of cascading benefits, including better mood regulation, enhanced attention and learning, and improved inter
Tic, functional neurological, and habit disorders: Tic disorders-including Tourette syndrome, FND, and other habit disorders such as nail biting, thumb sucking, trichotillomania, and habit cough- present complex diagnostic and therapeutic challenges in pediatric populations. These conditions often stem from underlying psychological factors such as anxiety, boredom, trauma, stress, or the need for self-regulation and self-soothing[91,92]. Although these behaviors may initially serve adaptive or protective functions, they often become entrenched through repetitive reinforcement, ultimately resulting in physical harm, social embarrassment, and diminished self-esteem.
Hypnotherapy has emerged as a safe, developmentally sensitive, and highly effective intervention for these disorders in children. Rather than relying on aversive or punitive strategies, hypnosis emphasizes positive suggestion, vivid imagination, self-regulation, and empowerment[7,93]. Its versatility allows for both diagnostic and therapeutic benefits, particularly in cases where conventional biomedical approaches have yielded limited success.
Tic disorders and Tourette syndrome: In tic disorders, hypnotherapy has been shown to help children become more attuned to premonitory urges-the sensations that precede tics-and develop voluntary control over tic expression through metaphoric, dissociative, and imagery-based techniques. Children may be guided to imagine a “switch” they can mentally activate to reduce tic frequency or redirect the urge into a less noticeable or calming behavior. This approach complements traditional behavioral therapies such as habit reversal training and is often perceived by children as more playful and engaging[94,95]. In a case series of 33 children with Tourette syndrome, self-hypnosis training supplemented with instructional video modeling led to symptom improvement in 79% of participants-96% of whom responded within three sessions[94]. Similarly, Kohen and Botts[95] documented a sustained reduction in tic frequency and a decreased reliance on medication through the use of relaxation and imagery techniques. These findings support hypnosis as an effective and child-friendly adjunctive therapy.
FND: FND encompasses a spectrum of psychogenic conditions, including functional movement disorders, psychogenic non-epileptic seizures, and functional gait abnormalities. Hypnotherapy plays a dual role here: Diagnostically, it can produce temporary symptom resolution during trance, which helps confirm the psychogenic origin of symptoms. Therapeutically, hypnosis supports emotional reprocessing, reduces somatic hypervigilance, and facilitates motor re
Habit disorders and body-focused repetitive behaviors: Habit disorders such as thumb sucking, nail biting, trichotillomania, and habit cough can significantly interfere with social functioning and physical well-being. These behaviors are often maintained by unconscious reinforcement mechanisms and may be exacerbated by stress or trauma[91]. Hy
For example, Anbar[96] reported the rapid resolution of a habit cough in a child using a rapport-based, functional understanding of symptoms paired with hypnosis. Grayson[97] similarly documented the elimination of thumb-sucking in a 7-year-old girl after a single hypnosis session involving imaginative modeling and affirmation. Kohen[98] treated pediatric trichotillomania through a combination of self-monitoring, dissociative strategies, and customized imagery, successfully helping children gain control without inducing guilt or shame. These interventions consistently emphasize internal mastery and self-efficacy.
Across tic, FND, and habit disorders, hypnotic strategies include empowering imagery (e.g., visualizing protective paint on fingernails), ego-strengthening affirmations, and developmentally tailored metaphors. Children may visualize their fingers resisting the urge to bite or imagine hair becoming stronger each time they resist pulling. In tic and habit disorders, suggestions may also incorporate gentle, symbolic aversion (e.g., fingers tasting “sour” only when placed in the mouth) delivered within a nurturing and affirming therapeutic frame. Parental involvement is crucial in reinforcing treatment gains. Caregivers are coached to provide consistent, nonjudgmental support, celebrate small successes, and encourage practice of hypnotic techniques at home[4,79]. While further large-scale RCTs are warranted, the current body of clinical evidence and expert consensus support the integration of hypnotherapy into treatment plans for pediatric tic disorders, FND, and habit disorders. It offers rapid symptom relief, enhances self-awareness and emotional regulation, and promotes lasting behavioral change-all within a framework that empowers the child and fosters hope and enga
Pediatric hypnotherapy is increasingly recognized as a valuable adjunctive approach in the comprehensive management of certain neurodevelopmental and psychosomatic conditions[99]. This is particularly true when traditional therapies alone may not fully address comorbid symptoms such as anxiety, sleep disturbances, or associated functional im
While hypnotherapy is not a primary treatment for the core neurodevelopmental characteristics of ASD, mounting evidence supports its role as a highly valuable adjunctive intervention, particularly for managing the frequently co-occurring challenges seen in autistic individuals. These challenges include heightened anxiety, emotional dysregulation, sensory sensitivities, behavioral rigidity, low self-esteem, and significant difficulties with cooperation in unfamiliar or demanding settings such as clinical or dental procedures[101].
Several studies have demonstrated the therapeutic potential of hypnosis when tailored to the unique needs of autistic children. For example, Mitchell et al[102] conducted a RCT assessing GDHT in autistic children with disorders of gut-brain interaction. While synbiotics alone improved GI symptoms, the combination of synbiotics and GDHT significantly reduced anxiety and irritability, with sustained improvement in GI pain, indicating GDHT’s value in addressing both physiological and behavioral symptoms through a biopsychosocial lens. Similarly, Gardner and Tarnow[103] reported successful use of adjunctive hypnotherapy in a child with atypical autism and severe ego deficits. By incorporating music-a preferred interest and strength of the child-into hypnotherapy, the intervention led to improvements not only in targeted behaviors but also in broader social and cognitive skills, with effects maintained at 18-month follow-up. This highlights the importance of personalization and strength-based approaches in hypnosis with autistic populations.
Sartika et al[104] found that hypnotherapy prior to dental scaling in autistic children significantly improved cooperation and reduced oral health complications such as calculus accumulation. This evidence suggests that hypnosis can modulate behavioral responses to stressful stimuli, enhance compliance, and make necessary medical or dental procedures less traumatic. Additionally, Austin et al[105] explored the feasibility of virtual reality (VR)-based hypnosis in adolescents with ASD. While core autistic symptoms remained unchanged, participants were attentive and engaged, with parents reporting increased relaxation and willingness to participate-suggesting that hypnotic engagement, through novel modalities like VR, may help bridge therapeutic gaps by increasing accessibility and comfort.
Taken together, these studies underscore the versatility of hypnotherapy in addressing diverse ASD-related concerns-from anxiety and GI distress to cooperation and emotional self-regulation. Hypnotherapeutic techniques such as guided imagery, safe space visualization, metaphor-based coping scripts, and ego-strengthening affirmations can be adapted to support autistic children in emotionally overwhelming or inflexible states. Moreover, when sleep disturbances are present-a common issue in ASD-hypnosis can promote relaxation and improve sleep onset through calming bedtime scripts and anxiety modulation[106]. Crucially, the success of hypnotherapy in ASD depends on a neurodiversity-affirming, highly individualized approach. Interventions must be designed with sensitivity to the child’s communication preferences, sensory processing profile, and interests. Leveraging special interests (e.g., music, animals, or fantasy themes) and using concrete, literal language can significantly enhance receptivity and therapeutic engagement[107]. When integrated into a multidisciplinary care framework and administered by clinicians trained in both hypnotherapy and autism care, hypnotherapy can substantially improve quality of life and psychological resilience in autistic children-empowering them with tools for better self-regulation, reduced anxiety, enhanced cooperation, and a stronger, more positive sense of self.
Children with ADHD often face a constellation of challenges beyond core symptoms of inattention, impulsivity, and hyperactivity. These include heightened anxiety, sleep disturbances, low self-esteem, and specific learning difficulties-each of which can significantly affect quality of life, academic performance, emotional resilience, and social adaptation[108]. While traditional ADHD management often relies on pharmacotherapy and behavioral interventions, hypno
Hypnotherapy does not aim to alter the neurocognitive underpinnings of ADHD directly, but it targets high-impact associated issues like anxiety, sleep dysregulation, and emotional dysregulation. For instance, hypnotic techniques-such as guided imagery, progressive muscle relaxation, breathing-focused induction, and metaphorical storytelling-help children learn to self-soothe, reduce physiological arousal, and transition more smoothly into sleep[110]. Children are often guided to imagine calming scenarios, such as gently floating on a cloud, slowing down a buzzing engine, or en
Emerging research strongly supports this approach. In a pioneering early study by Calhoun and Bolton[100], hyp
In clinical settings, practitioners often incorporate interactive metaphors tailored to children's developmental stages-such as superheroes mastering their impulses, magical calming objects, or adventure journeys into a “quiet mind cave”-to maximize engagement and therapeutic responsiveness. Additionally, children who learn self-hypnosis techniques report greater confidence, improved sleep initiation, fewer nocturnal awakenings, and reduced anxiety. These changes not only improve day-to-day functioning but also create a more receptive psychological state for other interventions, including medication titration or behavioral therapy[7]. Currently, clinical hypnotherapy is increasingly viewed not as a fringe or supplementary technique but as a credible and evidence-informed intervention for children with ADHD-especially those presenting with anxiety, sleep difficulties, learning disorders, or low self-esteem. When delivered by trained clinicians, hypnosis offers a non-invasive, empowering, and child-friendly strategy to support holistic development and psychological well-being in this vulnerable population. However, despite promising preliminary findings, the limited scope of current research makes it premature to draw firm conclusions about hypnosis as a reliable treatment for these conditions.
While often associated with behavioral or functional disorders, hypnotherapy has increasingly demonstrated significant value as an adjunctive intervention in managing symptoms linked to chronic and organic pediatric illnesses. Children confronting diagnoses such as cancer, CF, and IBD not only endure profound physical symptoms but also experience substantial psychological stressors. These stressors can exacerbate their primary condition, diminish treatment adherence, and severely impact their quality of life. Pediatric hypnotherapy, through its remarkable capacity to modulate perception, reduce distress, and enhance coping mechanisms, offers a safe, non-pharmacological strategy to improve overall well-being, alleviate symptom burden, and foster robust psychological resilience in these medically complex young po
Oncology support: Children undergoing cancer treatment frequently endure a multifaceted spectrum of distressing symptoms-including severe procedural pain, anticipatory anxiety, chemotherapy-induced nausea and vomiting, fatigue, and psychological distress related to repeated hospitalizations and invasive interventions. Hypnotherapy has emerged as a highly promising, non-pharmacological intervention to alleviate these burdens, empowering young patients with concrete psychological tools to manage both acute physical discomfort and profound emotional stress[115,116].
During procedures such as lumbar punctures, bone marrow aspirations, or central line access, clinical hypnosis is frequently employed to significantly reduce procedural pain and anxiety. Children are often guided to dissociate from the clinical environment through vivid imagery, such as floating in space, being protected by a “magic shield”, or visiting a tranquil, imaginary sanctuary. These approaches not only reduce the perception of pain but also improve procedural cooperation and emotional regulation[117]. A meta-analysis by Nunns et al[118] showed large, statistically significant reductions in both procedural anxiety (d = 2.30) and pain (d = 2.16) in children receiving hypnosis, outperforming several other non-pharmacological interventions. Chemotherapy-induced nausea and vomiting, particularly anticipatory nausea-a conditioned response exacerbated by repeated exposure-is another domain where hypnosis shows profound benefit. According to a systematic review by Richardson et al[119], hypnosis resulted in a clinically meaningful reduction in both anticipatory and acute nausea and vomiting among pediatric cancer patients, with effects comparable to cognitive-behavioral therapy, yet with fewer demands on cognitive processing.
From an emotional and psychosocial perspective, hypnotherapy plays a crucial role in fostering resilience, autonomy, and effective coping mechanisms. In a pilot group intervention by Grégoire et al[120], children aged 11-17 and their parents participated in monthly hypnosis-based sessions. Both groups reported improved emotional regulation, reduced stress, and enhanced family communication. Children learned specific self-regulation strategies-such as breathing techniques and positive reframing-to manage fear, sadness, and feelings of helplessness during treatment. Furthermore, individual case studies offer compelling support for hypnosis in managing cancer-related anxiety. For example, Talebiazar et al[121] conducted a structured hypnotherapy protocol with three female pediatric oncology patients, resulting in significant reductions in hospital-related anxiety, sustained through a one-month follow-up. Likewise, Anbar[122] demonstrated that self-hypnosis, taught in just one or two sessions, was successfully used by 86% of children and adolescents to manage symptoms including procedural discomfort, treatment-related anxiety, and even taste aversion from medications. Collectively, these studies underscore that hypnotherapy is far more than an adjunct to pediatric oncology care-it is a robust, adaptable therapeutic modality that directly targets both the somatic and psychological dimensions of cancer treatment. When appropriately tailored and delivered by trained clinicians, hypnotherapy substantially enhances quality of life, increases emotional resilience, and fosters meaningful engagement in the treatment process for children and adolescents facing cancer.
Bronchial asthma: Bronchial asthma remains one of the most prevalent chronic respiratory diseases in childhood, characterized by episodic airway inflammation, bronchoconstriction, and reversible airflow obstruction. These episodes often manifest as wheezing, shortness of breath, coughing, and chest tightness, substantially affecting a child’s daily functioning and psychosocial well-being[123]. Beyond the physical pathology, a critical aspect of asthma management lies in addressing its psychosomatic dimensions-particularly anxiety, fear, and panic, which can independently precipitate or worsen bronchoconstriction. These emotional triggers create a self-reinforcing loop that intensifies both psychological and physiological symptoms[124].
While bronchodilators and anti-inflammatory agents remain the foundation of treatment, clinical hypnotherapy has emerged as a promising adjunctive intervention that targets the emotional and behavioral components of asthma. Hypnotherapy primarily disrupts the anxiety-dyspnea cycle by fostering deep relaxation, slowing respiratory rate, and reducing muscular tension in the chest[125]. Children are typically taught self-hypnosis techniques tailored to their developmental stage, often involving vivid imagery-such as picturing “open tunnels” in their lungs or feeling a “cool breeze” soothing their chest. These tools provide portable, immediate coping strategies for managing panic and promoting a sense of control, which can ultimately reduce attack severity and improve adherence to medical treatment[126].
The clinical literature offers compelling support for this integrative approach. A key example is the work of Morrison[127], who studied sixteen chronic asthmatic patients with poor pharmacologic control and reported that, following one year of hypnotherapy, hospital admissions fell from 44 to 13 and cumulative inpatient days dropped by 249. Additionally, systemic corticosteroids were reduced or withdrawn in the majority of patients, with side effects notably diminished. Although objective measures of airflow showed variability, the reduction in healthcare utilization and medication dependency underscored hypnotherapy’s practical benefits. Complementing this, Anbar[126] conducted a retrospective review of 17 pediatric patients with chronic dyspnea who had normal resting pulmonary function but persistent breathing complaints. Thirteen of the 16 children taught self-hypnosis reported full symptom resolution within one month, and many attributed their recovery directly to the use of hypnosis techniques. This study not only highlights the utility of hypnosis in symptom control but also underscores its relevance in functional or psychogenic breathing disorders that mimic asthma.
In contrast, Alexander et al[128] evaluated the physiological effects of relaxation training in 14 children with severe asthma. Despite evidence of relaxation, as indicated by decreased heart rate and muscle tension, pulmonary function did not improve significantly, suggesting that while relaxation states can be achieved, they do not necessarily translate into measurable changes in lung function in all individuals. This distinction between subjective relief and objective improvement highlights the need to assess both domains when evaluating therapeutic outcomes. The broader landscape of pediatric complementary and alternative medicine (CAM), including hypnotherapy, has been critically examined by Moher et al[129] in a systematic review of 251 RCTs. The authors concluded that although RCTs are increasingly used, the overall quality of reporting remains suboptimal. Deficiencies such as poor allocation concealment and inconsistent outcome reporting limit the strength of conclusions, highlighting the urgent need for more rigorous and transparent trial designs. Nevertheless, their review underscores the growing recognition of CAM, including hypnotherapy, as a valuable area of pediatric research. Taken together, these studies support the growing consensus that clinical hypnotherapy is a safe, well-tolerated, and empowering adjunct to standard asthma management in children. By equipping patients with tools to modulate emotional triggers and build self-efficacy, hypnotherapy not only mitigates the psychological burden of asthma but also contributes to tangible improvements in daily functioning, medication use, and healthcare utilization. As evidence accumulates and methodological rigor improves, hypnotherapy is poised to play an increasingly important role within holistic, child-centered asthma care.
CF: CF is a chronic, life-shortening genetic disorder that primarily affects the respiratory and digestive systems. Children and adolescents with CF endure complex daily treatment routines-including airway clearance techniques, nebulized medications, enzyme replacement therapy, and frequent hospitalizations[130]. These demands, coupled with progressive pulmonary decline, often lead to psychological challenges such as anxiety, treatment fatigue, procedural distress, and depressive symptoms. The cumulative burden can significantly impair quality of life, emotional regulation, and treatment adherence[131].
Clinical hypnotherapy has emerged as a supportive and empowering tool to address these multifaceted challenges. Hypnotic techniques can reduce the perception of breathlessness, ease coughing episodes, and promote a state of deep relaxation during physiotherapy or nebulizer sessions. Children may be guided to visualize “fresh air flowing through crystal-clear tubes” or “lungs opening like flowers in the sun”, which fosters a positive, calming mental environment and facilitates deeper, more effective breathing. This imagery not only reframes distressing treatments but also increases the child's sense of agency and control over their condition[132]. Psychologically, hypnosis has demonstrated utility in decreasing anticipatory anxiety related to medical procedures and hospital stays. It can reduce discomfort during venipuncture, improve mood stability, and counter feelings of helplessness or social withdrawal, especially in adolescents coping with the social isolation and uncertainty inherent to CF. Teaching self-hypnosis enables these patients to apply adaptive coping strategies during daily stressors, leading to enhanced autonomy and resilience[133].
Empirical support for this approach is increasingly robust. In a pilot RCT, Belsky and Khanna[134] demonstrated that children aged 7-18 who practiced self-hypnosis showed significant improvements in psychological domains, including locus of control, self-concept, and trait anxiety, compared to matched controls. Importantly, these children also exhibited improved peak expiratory flow rates immediately following hypnosis sessions, indicating both psychological and physiological benefits. Complementing this, Anbar[122] conducted a case series involving 49 patients aged 7 to 49 years who were taught self-hypnosis by their pulmonologist. The patients used hypnosis for a variety of CF-related challenges-including relaxation, procedural pain, headaches, taste aversion to medications, and symptom control. Notably, 86% of reported applications were effective, and no patient experienced worsening of symptoms. Many participants continued to practice hypnosis independently for six months or longer, suggesting the high acceptability and sustainability of the intervention. Together, these findings support the integration of hypnotherapy into comprehensive CF care. While not a substitute for medical management, hypnotherapy provides an evidence-based, non-pharmacologic adjunct that enhances symptom control, reduces emotional distress, improves adherence, and supports overall well-being. As awareness and clinician training increase, hypnotherapy may become a core supportive therapy in multidisciplinary CF programs.
IBD: Children and adolescents diagnosed with IBD-which includes Crohn’s disease and ulcerative colitis-face a chronic, relapsing condition marked by unpredictable cycles of intense abdominal pain, diarrhea, fatigue, rectal bleeding, and emotional distress[135]. The burden is compounded by frequent invasive procedures, complex medication regimens, and the psychological impact of living with an incurable, fluctuating disease. As a complementary strategy within multidisciplinary IBD management, hypnotherapy has emerged as a promising and evidence-informed modality, particularly for its capacity to modulate the gut-brain axis, reduce stress-related exacerbations, and enhance patients' psychological resilience[136]. GDHT, already established as a highly effective treatment for IBS, is increasingly being adapted for patients with IBD, especially those experiencing IBS-type symptoms during disease remission. A RCT by Hoekman et al[137] demonstrated that although GDHT was not statistically superior to SMT in reducing symptom severity in patients with quiescent IBD and coexisting IBS-like symptoms, both strategies yielded meaningful symptom relief, positioning hypnotherapy as a viable, patient-centered option within this clinical context.
In pediatric populations, clinical hypnosis shows notable potential as an adjunctive therapy. In a pilot randomized controlled study by Lee et al[138] involving adolescents with Crohn’s disease, participants who received self-hypnosis training alongside one in-person session experienced significant improvements in parent-reported quality of life, particularly in social and school functioning, as well as a marked reduction in abdominal pain and school absences. These findings reinforce the acceptability, feasibility, and impact of hypnosis on psychosocial and somatic symptoms in young patients. In earlier work, Shaoul et al[139] explored the use of tailored hypnotherapy in six children with IBD who were facing severe symptoms despite ongoing conventional treatment. Most patients exhibited substantial clinical impro
Supporting the psychoneuroimmunological foundation of hypnosis in IBD, Mawdsley et al[140] conducted a physiological study in adults with active ulcerative colitis, finding that a single session of gut-focused hypnosis significantly reduced key inflammatory markers, including serum interleukin-6, rectal mucosal substance P, histamine, and IL-13. These biochemical changes were accompanied by improved mucosal blood flow and reduced autonomic arousal, underscoring the biological plausibility of hypnosis as an adjunct to anti-inflammation. Moreover, in a landmark prospective randomized study by Keefer et al[141], patients with quiescent ulcerative colitis who received 7 sessions of GDHT demonstrated prolonged clinical remission at 1 year compared with controls (68% vs 40%), with an average of 78 more days in remission. This is the first controlled trial to show that hypnotherapy may significantly influence long-term disease trajectory in IBD, potentially by stabilizing autonomic and immunological reactivity to stress.
Clinically, children undergoing hypnotherapy for IBD are often taught to use healing visual metaphors-such as soothing a “burning bowel” or visualizing immune cells repairing the mucosa-which may enhance their perceived control over symptoms and treatment. Such interventions also reduce procedural anxiety during frequent diagnostic tests and may support adherence to challenging dietary and medical regimens[142]. Although hypnotherapy is not a repla
Support during medical procedures and diagnostics: Medical procedures and diagnostic investigations are frequently highly distressing for children, often eliciting significant fear, anticipatory anxiety, and acute physiological stress responses. Pediatric patients undergoing surgery, complex imaging [such as MRI, computed tomography (CT) scans], or other unfamiliar and potentially invasive procedures may experience profound emotional dysregulation, resistance, and even develop long-term psychological sequelae if these experiences are perceived as traumatic[35]. Hypnotherapy offers an exceptionally valuable, non-pharmacological tool to proactively help children manage procedural anxiety, dramatically enhance their cooperation, and potentially improve a range of clinical outcomes through targeted psychological and physiological regulation[27].
Surgical preparation and recovery enhancement: Preoperative anxiety in children is a well-documented concern, associated with numerous adverse outcomes. These include heightened pain perception, increased requirements for anesthesia and analgesia, delayed post-operative recovery, and greater post-operative behavioral disturbances (e.g., increased irritability, sleep problems). Hypnotherapy has demonstrably proven effective in alleviating anticipatory anxiety and fostering a vital sense of calm, confidence, and control in pediatric surgical candidates[143].
Using carefully tailored hypnotic scripts and guided imagery, children can be guided to vividly visualize a safe, soothing environment where they feel completely at ease, or rehearse a successful and peaceful surgical experience from beginning to end. For example, a child may imagine “taking a brave journey in a comfortable spaceship where the doctors and nurses are kind, helpful astronauts”, creating a positive and empowering narrative around the entire surgical process[16]. Hypnotherapeutic suggestions are also strategically employed to prime the mind for a smooth and com
Imaging procedures (MRI, CT scans, and claustrophobia reduction): Diagnostic imaging procedures-especially MRI and CT scans-pose unique and formidable challenges for children. The enclosed space of an MRI scanner, the loud and unfamiliar noises, the absolute physical stillness required for extended periods, and the general fear of strange equipment can trigger intense anxiety, claustrophobia, and panic[146]. Consequently, these crucial procedures are often delayed, interrupted, or necessitate pharmacological sedation, increasing healthcare costs and potential medication-related risks. Hypnotherapy offers a powerful alternative to significantly reduce distress and vastly improve procedural compliance through expertly guided imagery, systematic desensitization, and deep relaxation techniques[147].
For instance, a child undergoing an MRI might be guided to imagine they are inside a personalized "rocket ship" preparing for an exciting journey to a favorite planet, with the scanner's noises reframed as the thrilling sounds of the mission. Pre-procedure sessions can strategically include exposure to recorded sounds of an MRI and practice hypnosis to simulate the feeling of lying still in a confined space, building familiarity and confidence[148]. By equipping children with these effective hypnotic coping strategies, many can successfully undergo complex scans without the need for pharmacologic sedation, leading to safer, more efficient, and more cost-effective diagnostic processes[149].
Moreover, the utilization of self-hypnosis or brief, targeted hypnosis techniques, delivered by trained personnel or via accessible digital tools (e.g., specialized apps, audio recordings), has shown considerable promise in helping children prepare for and complete diagnostic imaging with greater success[21]. Hypnosis also actively reduces physiological arousal, manifesting as a lower heart rate, blood pressure, and cortisol levels, thereby contributing to a more cooperative, relaxed, and positive state throughout the entire procedure[44]. This not only benefits the child's immediate experience but also potentially impacts the quality of the diagnostic images obtained. Although hypnosis can reduce procedural anxiety and distress, its feasibility in busy clinical environments is challenged by time constraints and limited availability of trained practitioners, underscoring the need for pragmatic trials.
Dermatologic conditions in children, particularly those with chronic or relapsing patterns such as warts and atopic dermatitis (AD) (eczema), frequently exhibit significant psychosomatic components, making them exceptionally ame
Warts, caused by various strains of the human papillomavirus (HPV), are highly prevalent in school-aged children and adolescents. These benign skin lesions, though often medically harmless, can be psychologically distressing due to cosmetic concerns, social embarrassment, and potential peer ridicule[152]. Their resistance to standard treatments such as cryotherapy, topical acids, or surgical removal-many of which are uncomfortable or even painful-has prompted interest in more patient-friendly, mind-body interventions. Hypnosis stands out as one of the most extensively studied and historically significant non-pharmacological options for treating warts, both cutaneous and genital[153].
Warts are among the earliest conditions for which the therapeutic value of hypnosis was formally validated. The immune-mediated nature of wart regression makes them an ideal target for psychoneuroimmunological modulation, and several clinical trials have investigated the potential of hypnosis to enhance immune function and facilitate clearance of HPV-induced lesions. In landmark studies by Spanos et al[154] and Spanos et al[155], hypnosis was shown to outperform placebo, topical salicylic acid, and no treatment in promoting the regression of cutaneous warts on the hands and feet. Participants who underwent hypnotic suggestion-such as envisioning the wart dissolving or disappearing-demonstrated significantly greater wart loss than the control group, independent of their baseline hypnotizability. Beyond cutaneous warts, hypnosis has also been explored for managing genital HPV infections. In a pivotal study by Barabasz et al[156], hypnosis was compared directly to SMT in both urban and rural women with HPV-related genital warts. At 12 weeks, hypnosis not only produced a statistically significant reduction in lesion size and number (P < 0.04) but also de
Hypnotherapeutic techniques typically employ vivid, multi-sensory imagery and age-appropriate suggestion strategies designed to stimulate the immune response. For children, this might include imagining a magical laser beam shrinking the wart, a healing sunbeam dissolving it, or an "immune army" being dispatched to attack the virus. These scripts are customized based on the child's developmental stage and personal interests, which maximizes receptivity and en
The plausible mechanisms underlying the observed wart regression include improved immune surveillance, enhanced local blood flow to the affected tissues, and reduction in psychological stress, which is known to suppress immune function. Importantly, hypnosis offers a painless, empowering, and cost-effective treatment modality, particularly for those with multiple lesions or significant treatment anxiety[158]. While hypnosis should not yet replace conventional treatments as a first-line option in all cases, the growing evidence base strongly supports its integration as a valuable adjunct or alternative, especially in children with treatment-resistant warts or high distress levels. Continued exploration of its mechanisms and efficacy through well-controlled studies is warranted and encouraged[159].
AD is a chronic, relapsing inflammatory skin disease characterized by intense pruritus, xerosis (dryness), and visible eczema lesions. A hallmark feature of AD is the itch-scratch cycle, in which persistent itching leads to compulsive scratching, which in turn worsens inflammation and provokes further itching. This self-perpetuating loop significantly contributes to sleep disturbance, mood dysregulation, social withdrawal, and reduced quality of life, especially in children[160]. Psychological stress and emotional distress-whether stemming from environmental triggers, interpersonal dynamics, or internal anxiety-are well-documented contributors to disease flares and scratching behavior, often exacerbating symptoms beyond dermatological control[161]. Hypnotherapy has emerged as a promising adjunctive strategy in the management of AD, particularly in moderate-to-severe or treatment-resistant cases. It targets both physiological symptoms and psychological contributors by disrupting the itch-scratch cycle, modulating stress responses, and en
The efficacy of hypnosis in eczema has been substantiated in a growing number of clinical studies. Stewart and Thomas[164] demonstrated statistically significant improvements in both subjective symptoms and objective measures in adults and children with severe, treatment-resistant eczema. Follow-up at up to 18 months indicated sustained benefits in itching, sleep disturbance, and mood, with nearly all children showing improvement immediately after the intervention. Delaitre et al[165] further corroborated these findings in a prospective clinical study, where 26 of 27 adult patients experienced significant improvement or resolution of eczema symptoms following hypnosis sessions. The mean Eczema Area and Severity Index score improved dramatically from 12 to 2.8, suggesting hypnosis may even reduce the need for systemic therapies in certain individuals. Derrick et al[166] explored self-hypnosis and guided imagery in children over 5 years with moderately severe chronic eczema. Although statistical significance was not achieved, the study still reported clinically observable improvements, highlighting the technique's potential and the need for larger sample sizes in future pediatric research.
Incorporating hypnotherapy into eczema care also brings behavioral and emotional advantages. It enables patients to address itching driven by anxiety, frustration, or boredom-a frequent pattern in pediatric populations. Parental involvement is integral, providing external support and reinforcing relaxation techniques and positive behaviors at home[16]. Hypnosis also enhances treatment adherence, particularly in children who are resistant to applying topical therapies due to discomfort or sensory sensitivities. While hypnosis should not replace standard dermatologic treatments, in
Hypnosis offers a unique and compelling array of advantages that render it particularly well-suited for integration into pediatric healthcare. Its utility extends beyond symptom management, fostering a safe approach, empowering, and is highly effective for children and adolescents. Perhaps one of its most compelling advantages is its nature as a non-pharmacological intervention[26]. This inherently minimizes concerns regarding systemic side effects, drug interactions (especially vital for children on complex polypharmacy), or potential dependency often associated with pharmaceutical solutions. For pediatric patients who may be highly sensitive to medications or for whom certain drugs are contraindicated, hypnotherapy provides a safe, gentle, and often preferred alternative or powerful adjunct to traditional medical approaches. Its application frequently reduces, or even eliminates, the need for sedatives, anxiolytics, or opioid analgesics during distressing procedures, thereby enhancing safety and simplifying post-procedure recovery[167].
A cornerstone advantage of hypnotherapy in pediatrics is its profound capacity to empower children by teaching them self-regulation strategies. Unlike many passive interventions, hypnosis actively engages the child's internal resources. Through expertly guided imagery, relaxation techniques, and positive suggestions, children learn concrete, transferable skills to manage pain, alleviate anxiety, regulate emotions, and overcome behavioral challenges with growing autonomy[16]. These mastery skills not only promote remarkable resilience during acute illness, chronic disease, or challenging medical procedures but also serve as invaluable, lifelong tools for emotional regulation, stress reduction, and overall well-being. This shift towards an internal locus of control can significantly boost a child's self-efficacy and confidence[54].
Furthermore, pediatric hypnotherapy often proves to be remarkably cost-effective over time. While initial sessions require the expertise of trained professionals and a dedicated time investment, the long-term benefits can lead to substantial financial savings. This includes a reduced reliance on costly medications, fewer emergency department visits for functional symptoms, decreased need for repeated specialist consultations, and avoidance of expenses associated with sedation for procedures[21]. Moreover, teaching children self-hypnosis or providing access to guided audio recordings extends the therapeutic benefits with minimal ongoing expense, making it a highly sustainable intervention[168]. A 2002 comparative study by Lang and Rosen[169] found that using adjunct self-hypnotic relaxation with sedation during outpatient interventional radiologic procedures significantly reduced costs compared to standard sedation alone. Their analysis revealed an average saving of $338 per case with hypnosis, costing $300 vs $638 for standard sedation. This cost-effectiveness held true even if hypnosis extended procedural room time, highlighting its economic benefit in these settings.
Crucially, the very process of hypnosis inherently enhances the therapeutic relationship between the child and the healthcare provider. Pediatric hypnotherapists must cultivate a strong foundation of rapport and trust, utilizing empathy, creativity, and genuinely child-centered communication[30]. This collaborative and supportive dynamic fosters a profound sense of safety and connection, which is paramount in pediatric care. Such a positive bond not only deepens therapeutic engagement and compliance with medical recommendations but also positively influences broader health outcomes by significantly reducing procedural fear, increasing adherence to necessary medical care, and mitigating the potential for medical trauma[170]. Finally, hypnotherapy's inherent child-friendliness and adaptability are distinct benefits. It leverages a child's natural capacity for imagination, storytelling, and play, making the therapeutic process engaging and non-threatening. This adaptability allows therapists to tailor interventions to individual developmental stages, cognitive styles, and personal interests, maximizing receptiveness and efficacy across a diverse range of conditions and ages[132]. Taken together, these multifaceted advantages firmly position clinical hypnosis as a powerful, versatile, child-affirming, and increasingly indispensable tool within modern, holistic pediatric practice.
Despite its growing recognition and demonstrated value as a powerful tool in pediatric care, the broader clinical ap
Another considerable obstacle is the pervasive presence of misconceptions and skepticism surrounding clinical hypnosis, prevalent among both healthcare providers and the public, including families. Popular media often sen
The inherent variability in individual responses to hypnosis also represents a known limitation. While many children respond remarkably well to hypnotic interventions, some may exhibit lower hypnotizability due to a range of factors. These can include developmental stage (e.g., very young children may have limited imaginative capacity), specific cognitive profiles (e.g., certain neurological differences), personality traits, or the complex nature of the presenting issue[177]. Hypnotherapy is not a universal "cure-all" and its effectiveness can indeed vary significantly between individuals, necessitating a personalized approach and realistic expectations[178].
Parental involvement and informed consent represent another critical layer of complexity unique to pediatric practice. Effective hypnotherapy with children often necessitates consistent collaboration and robust support from parents or primary caregivers, both for providing comprehensive background information to the therapist and, crucially, for reinforcing therapeutic techniques and suggestions outside of formal sessions[21]. In situations where parental understanding, belief, or support is limited, or where significant skepticism or conflicting views exist within the home environment, the continuity and long-term reinforcement of hypnotherapeutic gains can be severely compromised. Additionally, obtaining truly informed consent requires thorough communication to ensure that parents fully com
Lastly, time constraints in busy clinical settings pose a significant practical challenge. Effective pediatric hypnotherapy requires a calm, unhurried, and comfortable environment that allows sufficient time for building a strong rapport, engaging the child’s imagination deeply, and delivering therapeutic suggestions effectively[30]. In the fast-paced, high-volume environment of many modern healthcare settings, particularly in acute care units, bustling outpatient clinics, or general pediatric practices, carving out sufficient dedicated time for a complete hypnotherapy session may be simply not feasible[180]. This underscores the urgent need for greater institutional support, the development of truly integrated care models, and the exploration of brief intervention protocols or accessible home-based practice tools (e.g., recorded se
The effective, ethical, and safe use of clinical hypnosis in pediatric populations is unequivocally predicated on rigorous training, professional certification, and unwavering adherence to established guidelines. As the evidence base for pediatric hypnotherapy expands, so too does the emphasis on formalizing its educational and regulatory frameworks to ensure competent and responsible practice.
Certification and accreditation programs: To guarantee that clinicians are equipped with the specialized skills and ethical framework necessary for safe and effective practice, multiple reputable professional bodies offer comprehensive certification and accreditation programs. Notably, leading organizations such as the American Society of Clinical Hypnosis, the Society for Clinical and Experimental Hypnosis, and the Society of Psychological Hypnosis (APA Division 30) provide structured, multi-level training pathways[181]. These programs typically encompass extensive didactic education, rigorous supervised clinical practice, and thorough competency evaluations. Increasingly, these accreditation programs are integrating specific pediatric-focused modules, recognizing the unique developmental considerations and ethical nuances involved in working with children[182]. Such training emphasizes evidence-based practice, developmental appropriateness, the critical process of informed consent (involving both the child and guardians), and foundational ethical principles. Participation in these accredited programs ensures that practitioners possess the theoretical knowledge, practical skills, and ethical grounding required to deliver high-quality, safe, and effective hypnotherapy to pediatric patients[183].
In the practical landscape of clinical practice, an array of healthcare professionals play pivotal roles in both delivering and coordinating hypnotherapy interventions for children. Pediatricians, particularly those specializing in developmental-behavioral pediatrics, pain management, or integrative medicine, often serve as the crucial "gatekeepers" or initial points of contact[79]. Their role involves identifying appropriate candidates for hypnotherapy, providing preliminary education to families, and making informed referrals to trained specialists. Clinical psychologists and licensed therapists with specific specialization and certification in pediatric hypnosis are typically the primary direct providers of hypnotherapy[7]. Their extensive expertise in behavioral strategies, developmental psychology, nuanced communication with children, and psychological assessment makes them ideally suited to conduct the in-depth therapeutic sessions. Beyond these core providers, other allied health professionals such as nurses, child life specialists, occupational therapists, and even physical therapists who have received specialized training in hypnotic communication and brief hypnotic techniques can contribute meaningfully to integrated care, especially in dynamic hospital settings, outpatient clinics, or rehabilitation centers[183]. They can utilize hypnotic principles for pain distraction, anxiety reduction during procedures, or to enhance cooperation with physical therapies.
The paramount importance of multidisciplinary collaboration in pediatric hypnotherapy cannot be overstated. Hypnotherapy is most effective and truly transformative when seamlessly integrated into a comprehensive, holistic care model that includes active input and coordination from all relevant medical, psychological, educational, and familial stakeholders[180]. For instance, consider a child undergoing hypnotherapy for chronic pain or anxiety associated with a complex chronic illness like IBD or cancer[3]. Their therapeutic journey benefits immensely from continuous com
As clinical awareness and the evidence base continue to expand, there is a growing trend towards embedding foundational hypnosis training into medical and psychology residency programs and incorporating it into continuing professional development curricula for various healthcare disciplines[185]. Ensuring that a broader spectrum of healthcare providers across diverse specialties has access to standardized, high-quality, and pediatric-focused hypnosis training will be absolutely key to significantly expanding its safe, ethical, and effective utilization within mainstream clinical settings[16].
Despite the compelling and growing body of evidence supporting the efficacy of pediatric hypnotherapy across various clinical domains, several important areas remain critically underexplored. These represent significant opportunities for future advancement, research, and broader implementation, ultimately aiming to solidify hypnotherapy's role within mainstream pediatric care[4].
One of the most pressing and foundational needs is the conduct of large-scale, methodologically rigorous RCTs. While numerous smaller studies, controlled trials, and extensive case series have consistently demonstrated promising and often remarkable outcomes, especially in functional somatic disorders, chronic pain management, and procedural anxiety, broader and more robust RCTs are essential[186]. These trials are crucial not only to definitively validate efficacy across diverse pediatric populations and clinical settings but also to establish standardized treatment protocols, explore optimal dosages (e.g., number and frequency of sessions), and enhance the generalizability of the findings. Such high-quality research is fundamental for achieving wider acceptance, informing clinical guidelines, and securing reimbu
Another critical future direction is the systematic integration of hypnotherapy training into core pediatric residency, fellowship, and allied health professional programs. Currently, formal instruction in clinical hypnosis remains highly limited, often confined to elective workshops, specialized continuing medical education courses, or post-graduate certifications. Embedding comprehensive, developmentally appropriate hypnosis training into standard medical and psychological curricula would not only dramatically increase provider familiarity and competency but also play a pivotal role in overcoming long-standing skepticism by firmly grounding the modality in scientific rigor and clinical relevance[188]. Early and widespread exposure could cultivate a new generation of clinicians who are inherently comfortable offering or confidently referring for hypnosis as a fundamental component of a multimodal, integrative care approach. This also entails developing clear competencies and learning objectives specifically for pediatric applications.
Technological innovation offers expansive and exciting avenues for future expansion, particularly through the development and validation of telehypnosis platforms and sophisticated digital therapeutic interventions[189]. The global coronavirus disease 2019 pandemic unequivocally underscored the feasibility, safety, and widespread acceptance of virtual care delivery[190]. Preliminary efforts in telehypnosis, where guided sessions are delivered effectively via secure video conferencing platforms, have already shown immense promise in terms of accessibility and efficacy, especially for families in remote areas or those with mobility challenges[191]. Moreover, the creation of rigorously evidence-based mobile applications, immersive VR tools, and interactive gamified programs tailored explicitly to pediatric hypnosis could revolutionize accessibility, ensure standardized and high-quality delivery, and profoundly appeal to digitally native children and adolescents[192]. These technologies could facilitate self-hypnosis practice, provide instant coping strategies, and offer engaging content that enhances therapeutic engagement and adherence.
Furthermore, a significant research gap lies in comprehensively investigating the long-term effects and the robust cost-effectiveness of pediatric hypnotherapy. While acute benefits are well-documented, studies examining whether early hypnotherapy interventions result in sustained symptom improvement, durable reductions in medication reliance (e.g., for pain or anxiety), fewer emergency department visits, decreased hospitalizations, or significantly improved psy
Ultimately, future research should also focus on identifying predictors of responsiveness to hypnotherapy in pediatric populations, enabling more precise patient selection and personalized treatment approaches. Investigating the neurobiological mechanisms underlying hypnotherapy's effects in children, perhaps through neuroimaging or psychophy
Despite the promising findings and expanding clinical use of hypnotherapy in pediatric medicine, this review acknowledges several limitations that affect both the current literature and the broader integration of hypnosis into routine pediatric care. Firstly, while many studies support the efficacy of clinical hypnosis across a wide range of pediatric conditions, the overall evidence base remains heterogeneous. Variability in study design, small sample sizes, lack of standardized protocols, and differing outcome measures limit the generalizability and comparability of results. Although RCT exist for certain conditions-such as procedural pain and functional abdominal disorders-many other indications rely heavily on observational studies, case series, or expert consensus. This imbalance in the level of evidence across domains calls for more large-scale, methodologically rigorous studies to establish more straightforward guidelines and protocols.
Secondly, hypnotizability varies widely among individuals, and multiple factors, including age, developmental level, personality traits, and prior exposure to stress or trauma, influence children’s responsiveness to hypnosis. While this individual variability can sometimes be leveraged therapeutically, it also complicates efforts to predict treatment success and develop universally applicable interventions. Another challenge lies in accessibility and training. There is a shortage of clinicians-particularly pediatricians and child psychologists-with formal training in clinical hypnotherapy, and existing certification programs are not yet integrated into most pediatric residency or fellowship curricula. This results in a bottleneck in service availability, especially in underserved areas. Additionally, misconceptions about hypnosis persist among both healthcare providers and the general public, often fueled by media portrayals of stage hypnosis. These misconceptions contribute to skepticism, hesitation, and underutilization of a potentially valuable therapeutic tool.
Parental involvement, although generally beneficial, can sometimes serve as a barrier to using hypnotherapy for child management. Some parents might be hesitant to consent to hypnosis because of cultural beliefs, unfamiliarity, or concerns about safety or control. This highlights the need for improved public education and enhanced clinician con
Clinical hypnosis represents a promising, non-pharmacological intervention in pediatric medicine, harnessing children’s natural imaginative abilities and capacity for focused attention. Evidence indicates potential benefits across a range of conditions-including pain management, functional somatic syndromes, anxiety disorders, dermatological conditions, and supportive care in chronic illness-while also fostering self-regulation and resilience. However, the strength of evidence varies considerably, with robust support in some areas (e.g., acute pain, anxiety) but more limited or preliminary data in others. Barriers such as limited clinician training, misconceptions among healthcare providers and families, and variability in individual responsiveness continue to constrain its broader adoption. To establish hypnosis as a reliable component of integrative pediatric care, further large-scale, RCTs, standardized treatment protocols, and long-term outcome studies are essential. Incorporating hypnotherapy into pediatric training curricula and exploring innovative delivery models such as telehypnosis may expand accessibility. At present, clinical hypnosis should be regarded as a safe and potentially valuable adjunct, but its definitive role in pediatrics remains to be fully determined.
| 1. | Williamson A. What is hypnosis and how might it work? Palliat Care. 2019;12:1178224219826581. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Alman B. Hypnosis. Perm J. 2001;5. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Rogovik AL, Goldman RD. Hypnosis for treatment of pain in children. Can Fam Physician. 2007;53:823-825. [PubMed] |
| 4. | Geagea D, Tyack Z, Kimble R, Eriksson L, Polito V, Griffin B. Hypnotherapy for Procedural Pain and Distress in Children: A Scoping Review Protocol. Pain Med. 2021;22:2818-2826. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Jones HG, Rizzo RRN, Pulling BW, Braithwaite FA, Grant AR, McAuley JH, Jensen MP, Moseley GL, Rees A, Stanton TR. Adjunctive use of hypnosis for clinical pain: a systematic review and meta-analysis. Pain Rep. 2024;9:e1185. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 6. | Catarino M, Charepe Z, Festas C. Promotion of Self-Management of Chronic Disease in Children and Teenagers: Scoping Review. Healthcare (Basel). 2021;9:1642. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Kohen DP, Kaiser P. Clinical Hypnosis with Children and Adolescents-What? Why? How?: Origins, Applications, and Efficacy. Children (Basel). 2014;1:74-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Wolf TG, Faerber KA, Rummel C, Halsband U, Campus G. Functional Changes in Brain Activity Using Hypnosis: A Systematic Review. Brain Sci. 2022;12:108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 9. | Jiang H, White MP, Greicius MD, Waelde LC, Spiegel D. Brain Activity and Functional Connectivity Associated with Hypnosis. Cereb Cortex. 2017;27:4083-4093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 77] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 10. | Deeley Q, Oakley DA, Toone B, Giampietro V, Brammer MJ, Williams SC, Halligan PW. Modulating the default mode network using hypnosis. Int J Clin Exp Hypn. 2012;60:206-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 75] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 11. | Miltner WHR, Franz M, Naumann E. Neuroscientific results of experimental studies on the control of acute pain with hypnosis and suggested analgesia. Front Psychol. 2024;15:1371636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 12. | Kiernan BD, Dane JR, Phillips LH, Price DD. Hypnotic analgesia reduces R-III nociceptive reflex: further evidence concerning the multifactorial nature of hypnotic analgesia. Pain. 1995;60:39-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 130] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 13. | De Benedittis G. Hypnotic Modulation of Autonomic Nervous System (ANS) Activity. Brain Sci. 2024;14:249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 11] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 14. | De Benedittis G. Brain Mechanisms of Hypnosis. Brain Sci. 2025;15:142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Bagley EE, Ingram SL. Endogenous opioid peptides in the descending pain modulatory circuit. Neuropharmacology. 2020;173:108131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 123] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 16. | Kaiser P, Kohen DP, Brown ML, Kajander RL, Barnes AJ. Integrating Pediatric Hypnosis with Complementary Modalities: Clinical Perspectives on Personalized Treatment. Children (Basel). 2018;5:108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Raz A. Hypnosis: a twilight zone of the top-down variety Few have never heard of hypnosis but most know little about the potential of this mind-body regulation technique for advancing science. Trends Cogn Sci. 2011;15:555-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Knafo G, Weinberger J. Exploring the Role of Conscious and Unconscious Processes in Hypnosis: A Theoretical Review. Brain Sci. 2024;14:374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 19. | Lynn SJ, Green JP. The sociocognitive and dissociation theories of hypnosis: toward a rapprochement. Int J Clin Exp Hypn. 2011;59:277-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 20. | Giesbrecht T, Lynn SJ, Lilienfeld SO, Merckelbach H. Cognitive processes in dissociation: an analysis of core theoretical assumptions. Psychol Bull. 2008;134:617-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 155] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 21. | Bastek V, van Vliet M. A whole new world of healing: exploring medical hypnotherapy for pediatric patients : A review. Eur J Pediatr. 2023;182:3021-3032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 22. | Kravits K. Hypnosis: adjunct therapy for cancer pain management. J Adv Pract Oncol. 2013;4:83-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Nuñez L, Fernández S, Alamo N, Midgley N, Capella C, Krause M. The therapeutic relationship and change processes in child psychotherapy: a qualitative, longitudinal study of the views of children, parents and therapists. Res Psychother. 2022;25:556. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 24. | Heyman GD. Children's Critical Thinking When Learning From Others. Curr Dir Psychol Sci. 2008;17:344-347. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 34] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 25. | Thompson SJ, Bender K, Lantry J, Flynn PM. Treatment Engagement: Building Therapeutic Alliance in Home-Based Treatment with Adolescents and their Families. Contemp Fam Ther. 2007;29:39-55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 56] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 26. | Friedrichsdorf SJ, Kohen DP. Integration of hypnosis into pediatric palliative care. Ann Palliat Med. 2018;7:136-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 27. | Geagea D, Griffin B, Kimble R, Polito V, Terhune DB, Tyack Z. Hypnotherapy for procedural pain, itch, and state anxiety in children with acute burns: a feasibility and acceptability study protocol. Pilot Feasibility Stud. 2022;8:58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 28. | Sweeney A, Filson B, Kennedy A, Collinson L, Gillard S. A paradigm shift: relationships in trauma-informed mental health services. BJPsych Adv. 2018;24:319-333. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 126] [Cited by in RCA: 202] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 29. | Spriggs M. Children and bioethics: clarifying consent and assent in medical and research settings. Br Med Bull. 2023;145:110-119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 26] [Reference Citation Analysis (0)] |
| 30. | Pendergrast RA. Incorporating Hypnosis into Pediatric Clinical Encounters. Children (Basel). 2017;4:18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 31. | Zemla K, Sedek G, Wróbel K, Postepski F, Wojcik GM. Investigating the Impact of Guided Imagery on Stress, Brain Functions, and Attention: A Randomized Trial. Sensors (Basel). 2023;23:6210. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 32. | Cochrane G. The use of indirect hypnotic suggestions for insomnia arising from generalized anxiety: a case report. Am J Clin Hypn. 1989;31:199-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 33. | Vlieger AM, Vermetten EV. [Hypnosis and hypnotic suggestions: applications in medical disorders]. Ned Tijdschr Geneeskd. 2020;164:D4877. [PubMed] |
| 34. | Yarmohamadi Vasel M, Farhadi M, Zoghi Paidar MR, Chegini AA. The Efficacy of Hypnotherapy for Ego Strengthening and Negative Self-Talk in Female Heads of Households. Sleep Hypn. 2016;18:74-81. [DOI] [Full Text] |
| 35. | Trottier ED, Doré-Bergeron MJ, Chauvin-Kimoff L, Baerg K, Ali S. Managing pain and distress in children undergoing brief diagnostic and therapeutic procedures. Paediatr Child Health. 2019;24:509-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 81] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 36. | Passarello N, Tarantino V, Chirico A, Menghini D, Costanzo F, Sorrentino P, Fucà E, Gigliotta O, Alivernini F, Oliveri M, Lucidi F, Vicari S, Mandolesi L, Turriziani P. Sensory Processing Disorders in Children and Adolescents: Taking Stock of Assessment and Novel Therapeutic Tools. Brain Sci. 2022;12:1478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 37. | Hulette AC, Freyd JJ, Pears KC, Kim HK, Fisher PA, Becker-Blease KA. Dissociation and Posttraumatic Symptoms in Maltreated Preschool Children. J Child Adolesc Trauma. 2008;1:93-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 38. | Miller MM. Hypnotic-aversion treatment of homosexuality. J Natl Med Assoc. 1963;55:411-415. [PubMed] |
| 39. | Shenefelt PD. Biofeedback, cognitive-behavioral methods, and hypnosis in dermatology: is it all in your mind? Dermatol Ther. 2003;16:114-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 55] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 40. | Culbert TP, Kajander RL, Kohen DP, Reaney JB. Hypnobehavioral approaches for school-age children with dysphagia and food aversion: a case series. J Dev Behav Pediatr. 1996;17:335-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 41. | Vickers A, Zollman C, Payne DK. Hypnosis and relaxation therapies. West J Med. 2001;175:269-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 42. | Geagea D, Tyack Z, Kimble R, Polito V, Ayoub B, Terhune DB, Griffin B. Clinical Hypnosis for Procedural Pain and Distress in Children: A Scoping Review. Pain Med. 2023;24:661-702. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 21] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 43. | Langlois P, Perrochon A, David R, Rainville P, Wood C, Vanhaudenhuyse A, Pageaux B, Ounajim A, Lavallière M, Debarnot U, Luque-Moreno C, Roulaud M, Simoneau M, Goudman L, Moens M, Rigoard P, Billot M. Hypnosis to manage musculoskeletal and neuropathic chronic pain: A systematic review and meta-analysis. Neurosci Biobehav Rev. 2022;135:104591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 52] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 44. | Leo DG, Keller SS, Proietti R. "Close your eyes and relax": the role of hypnosis in reducing anxiety, and its implications for the prevention of cardiovascular diseases. Front Psychol. 2024;15:1411835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 45. | Rosendahl J, Alldredge CT, Haddenhorst A. Meta-analytic evidence on the efficacy of hypnosis for mental and somatic health issues: a 20-year perspective. Front Psychol. 2023;14:1330238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 23] [Reference Citation Analysis (0)] |
| 46. | Taylor DA, Genkov KA. Hypnotherapy for the Treatment of Persistent Pain: A Literature Review. J Am Psychiatr Nurses Assoc. 2020;26:157-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 47. | Chester SJ, Stockton K, De Young A, Kipping B, Tyack Z, Griffin B, Chester RL, Kimble RM. Effectiveness of medical hypnosis for pain reduction and faster wound healing in pediatric acute burn injury: study protocol for a randomized controlled trial. Trials. 2016;17:223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 48. | Madrid AD, Barnes SH. A hypnotic protocol for eliciting physical changes through suggestions of biochemical responses. Am J Clin Hypn. 1991;34:122-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 49. | Kendrick C, Sliwinski J, Yu Y, Johnson A, Fisher W, Kekecs Z, Elkins G. Hypnosis for Acute Procedural Pain: A Critical Review. Int J Clin Exp Hypn. 2016;64:75-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 61] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 50. | McKillop HN, Banez GA. A Broad Consideration of Risk Factors in Pediatric Chronic Pain: Where to Go from Here? Children (Basel). 2016;3:38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 51. | Miller MM, Meints SM, Hirsh AT. Catastrophizing, pain, and functional outcomes for children with chronic pain: a meta-analytic review. Pain. 2018;159:2442-2460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 58] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 52. | Coogle J, Coogle B, Quezada J. Hypnosis in the Treatment of Pediatric Functional Neurological Disorder: The Magic Glove Technique. Pediatr Neurol. 2021;125:20-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 53. | Chamine I, Atchley R, Oken BS. Hypnosis Intervention Effects on Sleep Outcomes: A Systematic Review. J Clin Sleep Med. 2018;14:271-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 39] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 54. | Lombard L. A vision to enhance self-regulation in children: The promise of pediatric hypnosis. Am J Clin Hypn. 2024;66:316-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 55. | Walter N, Leyva MT, Hinterberger T, Rupp M, Loew T, Lambert-Delgado A, Mena AEC. Hypnosis as a non-pharmacological intervention for invasive medical procedures - A systematic review and meta-analytic update. J Psychosom Res. 2025;192:112117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 56. | Kohen DP, Olness KN, Colwell SO, Heimel A. The use of relaxation-mental imagery (self-hypnosis) in the management of 505 pediatric behavioral encounters. J Dev Behav Pediatr. 1984;5:21-25. [PubMed] |
| 57. | Olness K. Hypnotherapy: a cyberphysiologic strategy in pain management. Pediatr Clin North Am. 1989;36:873-884. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 58. | Gardner T, O'Hagan E, Gilanyi YL, McAuley JH, Jensen MP, Rizzo RR. Using hypnosis in clinical practice for the management of chronic pain: A qualitative study. Patient Educ Couns. 2024;119:108097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 59. | Casula CC. The Importance of Rapport in Hypnotic Clinical Practice. OBM Integr Complement Med. 2020;5:1-13. [DOI] [Full Text] |
| 60. | Baglioni V, Orecchio S, Esposito D, Faedda N, Natalucci G, Guidetti V. Tension-Type Headache in Children and Adolescents. Life (Basel). 2023;13:825. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 61. | Kohen DP, Zajac R. Self-hypnosis training for headaches in children and adolescents. J Pediatr. 2007;150:635-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 62. | Jong MC, Boers I, van Wietmarschen HA, Tromp E, Busari JO, Wennekes R, Snoeck I, Bekhof J, Vlieger AM. Hypnotherapy or transcendental meditation versus progressive muscle relaxation exercises in the treatment of children with primary headaches: a multi-centre, pragmatic, randomised clinical study. Eur J Pediatr. 2019;178:147-154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 63. | Gysin T. [Clinical hypnotherapy/self-hypnosis for unspecified, chronic and episodic headache without migraine and other defined headaches in children and adolescents]. Forsch Komplementarmed. 1999;6 Suppl 1:44-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 64. | Anbar RD, Zoughbi GG. Relationship of headache-associated stressors and hypnosis therapy outcome in children: a retrospective chart review. Am J Clin Hypn. 2008;50:335-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 65. | Kohen DP. Chronic daily headache: helping adolescents help themselves with self-hypnosis. Am J Clin Hypn. 2011;54:32-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 66. | Haine-Schlagel R, Walsh NE. A review of parent participation engagement in child and family mental health treatment. Clin Child Fam Psychol Rev. 2015;18:133-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 195] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 67. | Kangas M, Kallesoe KH, Rask CU. Functional Somatic Syndromes (FSS) in Children and Adolescents. Zeitschrift für Psychologie. 2020;228:81-92. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 68. | Rutten JM, Vlieger AM, Frankenhuis C, George EK, Groeneweg M, Norbruis OF, Tjon a Ten W, Van Wering H, Dijkgraaf MG, Merkus MP, Benninga MA. Gut-directed hypnotherapy in children with irritable bowel syndrome or functional abdominal pain (syndrome): a randomized controlled trial on self exercises at home using CD versus individual therapy by qualified therapists. BMC Pediatr. 2014;14:140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 69. | Atay O, David J, Mehta A. A Hypothetical Case Example Illustrating the Importance of a Multidisciplinary Approach to Treating Chronic/Functional Abdominal Pain in Pediatric Patients. Pediatr Clin North Am. 2022;69:917-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 70. | Vlieger AM, Menko-Frankenhuis C, Wolfkamp SC, Tromp E, Benninga MA. Hypnotherapy for children with functional abdominal pain or irritable bowel syndrome: a randomized controlled trial. Gastroenterology. 2007;133:1430-1436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 170] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 71. | Gulewitsch MD, Schlarb AA. Comparison of gut-directed hypnotherapy and unspecific hypnotherapy as self-help format in children and adolescents with functional abdominal pain or irritable bowel syndrome: a randomized pilot study. Eur J Gastroenterol Hepatol. 2017;29:1351-1360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 72. | Vlieger AM, Rutten JM, Govers AM, Frankenhuis C, Benninga MA. Long-term follow-up of gut-directed hypnotherapy vs. standard care in children with functional abdominal pain or irritable bowel syndrome. Am J Gastroenterol. 2012;107:627-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 104] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 73. | de Bruijn CMA, Hovy SW, Tromp E, Benninga MA, Hall KT, Vlieger AM. Do Polymorphisms Predict Hypnotherapy Response in Children With Functional Abdominal Pain Disorders: An Explorative Study. J Pediatr Gastroenterol Nutr. 2023;77:486-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 74. | Vasant DH, Hasan SS, Cruickshanks P, Whorwell PJ. Gut-focused hypnotherapy for children and adolescents with irritable bowel syndrome. Frontline Gastroenterol. 2021;12:570-577. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 75. | Elbahnasawy TH, Elnagar MA. Psychological Impact of Nocturnal Enuresis on Self-esteem of School Children. Am J Nurse Res. 2015;3:14-20. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 76. | Seabrook JA, Gorodzinsky F, Freedman S. Treatment of primary nocturnal enuresis: A randomized clinical trial comparing hypnotherapy and alarm therapy. Paediatr Child Health. 2005;10:609-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 77. | Edwards SD, van der Spuy HI. Hypnotherapy as a treatment for enuresis. J Child Psychol Psychiatry. 1985;26:161-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 30] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 78. | Olness K. The use of self-hypnosis in the treatment of childhood nocturnal enuresis. A report on forty patients. Clin Pediatr (Phila). 1975;14:273-275, 278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 54] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 79. | Huynh ME, Vandvik IH, Diseth TH. Hypnotherapy in child psychiatry: the state of the art. Clin Child Psychol Psychiatry. 2008;13:377-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 80. | Landry M, Lifshitz M, Raz A. Brain correlates of hypnosis: A systematic review and meta-analytic exploration. Neurosci Biobehav Rev. 2017;81:75-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 143] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 81. | Minosh C, Schwartz RH, Vahe Badalyan V. Hypnosis in 53 Children With Anxiety Disorders, Nocturnal Enuresis, or Insomnia. Int J Clin Pediatr. 2013;2:61-67. [DOI] [Full Text] |
| 82. | Erappa U, Konde S, Agarwal M, Peethambar P, Devi V, Ghosh S. Comparative Evaluation of Efficacy of Hypnosis, Acupressure and Audiovisual Aids in Reducing the Anxiety of Children during Administration of Local Anesthesia. Int J Clin Pediatr Dent. 2021;14:S186-S192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 83. | Girón CB, Ramírez-Carrasco A, Cappello OS, Pozos-Guillén A, Pierdant-Pérez M. The efficacy of hypnosis compared with the tell/show/do technique for the reduction of anxiety/pain in children undergoing pulpotomies: a randomized controlled trial. J Clin Pediatr Dent. 2024;48:69-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 84. | Rienhoff S, Splieth CH, Veerkamp JSJ, Rienhoff J, Krikken JB, Campus G, Wolf TG. Hypnosis and Sedation for Anxious Children Undergoing Dental Treatment: A Retrospective Practice-Based Longitudinal Study. Children (Basel). 2022;9:611. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 85. | Shelton AR, Malow B. Neurodevelopmental Disorders Commonly Presenting with Sleep Disturbances. Neurotherapeutics. 2021;18:156-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 86. | Anbar RD, Slothower MP. Hypnosis for treatment of insomnia in school-age children: a retrospective chart review. BMC Pediatr. 2006;6:23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 87. | Hawkins P, Polemikos N. Hypnosis treatment of sleeping problems in children experiencing loss. Contemp Hypn. 2002;19:18-24. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 88. | Kohen DP, Mahowald MW, Rosen GM. Sleep-terror disorder in children: the role of self-hypnosis in management. Am J Clin Hypn. 1992;34:233-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 89. | Toussaint L, Nguyen QA, Roettger C, Dixon K, Offenbächer M, Kohls N, Hirsch J, Sirois F. Effectiveness of Progressive Muscle Relaxation, Deep Breathing, and Guided Imagery in Promoting Psychological and Physiological States of Relaxation. Evid Based Complement Alternat Med. 2021;2021:5924040. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 96] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 90. | Tsitsi T, Raftopoulos V, Papastavrou E, Charalambous A. Progressive Muscle Relaxation and guided imagery as techniques to enhance the way of coping of parents of children with malignancies: Findings from a randomized controlled trial. Eur J Oncol Nurs. 2020;46:101718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 91. | Okumuş HG, Akdemir D. Body Focused Repetitive Behavior Disorders: Behavioral Models and Neurobiological Mechanisms. Turk Psikiyatri Derg. 2023;34:50-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 92. | Nilles C, Hartmann A, Roze E, Martino D, Pringsheim T. Tourette syndrome and other tic disorders of childhood. Handb Clin Neurol. 2023;196:457-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 93. | Gardner GG. Hypnotherapy in the management of childhood habit disorders. J Pediatr. 1978;92:838-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 17] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 94. | Lazarus JE, Klein SK. Nonpharmacological treatment of tics in Tourette syndrome adding videotape training to self-hypnosis. J Dev Behav Pediatr. 2010;31:498-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 95. | Kohen DP, Botts P. Relaxation-imagery (self-hypnosis) in Tourette syndrome: experience with four children. Am J Clin Hypn. 1987;29:227-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 96. | Anbar RD. User friendly hypnosis as an adjunct for treatment of habit cough: a case report. Am J Clin Hypn. 2007;50:171-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 97. | Grayson DN. Hypnotic intervention in a 7-year-old thumbsucker: a case study. Am J Clin Hypn. 2012;54:195-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 98. | Kohen DP. Hypnotherapeutic management of pediatric and adolescent trichotillomania. J Dev Behav Pediatr. 1996;17:328-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 99. | Olness KN. Hypnotherapy in children. New approach to solving common pediatric problems. Postgrad Med. 1986;79:95-100, 105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 100. | Calhoun G Jr, Bolton JA. Hypnotherapy: a possible alternative for treating pupils affected with attention deficit disorder. Percept Mot Skills. 1986;63:1191-1195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 101. | Sugarman LI, Garrison BL, Williford KL. Symptoms as solutions: hypnosis and biofeedback for autonomic regulation in autism spectrum disorders. Am J Clin Hypn. 2013;56:152-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 102. | Mitchell LK, Heussler HS, Burgess CJ, Rehman A, Steinert RE, Davies PSW. Gastrointestinal, Behaviour and Anxiety Outcomes in Autistic Children Following an Open Label, Randomised Pilot Study of Synbiotics vs Synbiotics and Gut-Directed Hypnotherapy. J Autism Dev Disord. 2024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 103. | Gardner GG, Tarnow JD. Adjunctive hypnotherapy with an autistic boy. Am J Clin Hypn. 1980;22:173-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 104. | Sartika D, Supriyana S, Wiyatini T, Djamil M, Eko Ningtyas EA. Pengaruh Hipnoterapi dalam Penatalaksanaan Scaling pada Anak Autis. Syntax Idea. 2023;5:621-628. [DOI] [Full Text] |
| 105. | Austin DW, Abbott JM, Carbis C. The use of virtual reality hypnosis with two cases of autism spectrum disorder: a feasibility study. Contemp Hypn. 2008;25:102-109. [RCA] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 106. | Esposito D, Belli A, Ferri R, Bruni O. Sleeping without Prescription: Management of Sleep Disorders in Children with Autism with Non-Pharmacological Interventions and Over-the-Counter Treatments. Brain Sci. 2020;10:441. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 107. | Lerner MD, Gurba AN, Gassner DL. A framework for neurodiversity-affirming interventions for autistic individuals. J Consult Clin Psychol. 2023;91:503-504. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 108. | Singh A, Yeh CJ, Verma N, Das AK. Overview of Attention Deficit Hyperactivity Disorder in Young Children. Health Psychol Res. 2015;3:2115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 109. | Drechsler R, Brem S, Brandeis D, Grünblatt E, Berger G, Walitza S. ADHD: Current Concepts and Treatments in Children and Adolescents. Neuropediatrics. 2020;51:315-335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 198] [Article Influence: 33.0] [Reference Citation Analysis (0)] |
| 110. | Um YH, Hong SC, Jeong JH. Sleep Problems as Predictors in Attention-Deficit Hyperactivity Disorder: Causal Mechanisms, Consequences and Treatment. Clin Psychopharmacol Neurosci. 2017;15:9-18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 111. | Herbert A, Esparham A. Mind-Body Therapy for Children with Attention-Deficit/Hyperactivity Disorder. Children (Basel). 2017;4:31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 112. | Hazard M, Perivier M, Gaisne C, Hicham R, Castelnau P. Hypnosis therapy for self-esteem in pediatric neurology practice: A pilot exploratory study. Arch Pediatr. 2024;31:72-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 113. | Hery-Niaussat C, Ossart V, Penigault P, Robert P, Manera V, Gros A. Therapeutic hypnosis in a child with a written language disorder. Am J Clin Hypn. 2023;65:269-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 114. | Mackner LM, Greenley RN, Szigethy E, Herzer M, Deer K, Hommel KA. Psychosocial issues in pediatric inflammatory bowel disease: report of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr. 2013;56:449-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 143] [Article Influence: 11.0] [Reference Citation Analysis (1)] |
| 115. | Ruggiero A, Rizzo D, Catalano M, Coccia P, Triarico S, Attiná G. Acute chemotherapy-induced nausea and vomiting in children with cancer: Still waiting for a common consensus on treatment. J Int Med Res. 2018;46:2149-2156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 116. | Hooke MC, Linder LA. Symptoms in Children Receiving Treatment for Cancer-Part I: Fatigue, Sleep Disturbance, and Nausea/Vomiting. J Pediatr Oncol Nurs. 2019;36:244-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 78] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 117. | Zeltzer L, LeBaron S. Hypnosis and nonhypnotic techniques for reduction of pain and anxiety during painful procedures in children and adolescents with cancer. J Pediatr. 1982;101:1032-1035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 201] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 118. | Nunns M, Mayhew D, Ford T, Rogers M, Curle C, Logan S, Moore D. Effectiveness of nonpharmacological interventions to reduce procedural anxiety in children and adolescents undergoing treatment for cancer: A systematic review and meta-analysis. Psychooncology. 2018;27:1889-1899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 119. | Richardson J, Smith JE, McCall G, Richardson A, Pilkington K, Kirsch I. Hypnosis for nausea and vomiting in cancer chemotherapy: a systematic review of the research evidence. Eur J Cancer Care (Engl). 2007;16:402-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 81] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 120. | Grégoire C, Chantrain C, Faymonville ME, Marini J, Bragard I. A Hypnosis-based group intervention to improve quality of life in children with cancer and their parents. Int J Clin Exp Hypn. 2019;67:117-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 121. | Talebiazar N, Choobianzali B, Hassanpour A, Goli R, Shakorzadeh S, Ghalandari M. The effect of hypnotherapy on the hospital anxiety in three children with cancer: A case report. Int J Surg Case Rep. 2022;93:106961. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 122. | Anbar RD. Self-hypnosis for patients with cystic fibrosis. Pediatr Pulmonol. 2000;30:461-465. [PubMed] [DOI] [Full Text] |
| 123. | Trivedi M, Denton E. Asthma in Children and Adults-What Are the Differences and What Can They Tell us About Asthma? Front Pediatr. 2019;7:256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 114] [Cited by in RCA: 175] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 124. | Van Lieshout RJ, Macqueen G. Psychological factors in asthma. Allergy Asthma Clin Immunol. 2008;4:12-28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 125. | Anbar RD. Self-hypnosis for anxiety associated with severe asthma: a case report. BMC Pediatr. 2003;3:7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 126. | Anbar RD. Self-hypnosis for management of chronic dyspnea in pediatric patients. Pediatrics. 2001;107:E21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 45] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 127. | Morrison JB. Chronic asthma and improvement with relaxation induced by hypnotherapy. J R Soc Med. 1988;81:701-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 128. | Alexander AB, Cropp GJ, Chai H. Effects of relaxation training on pulmonary mechanics in children with asthma. J Appl Behav Anal. 1979;12:27-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 30] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 129. | Moher D, Sampson M, Campbell K, Beckner W, Lepage L, Gaboury I, Berman B. Assessing the quality of reports of randomized trials in pediatric complementary and alternative medicine. BMC Pediatr. 2002;2:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 130. | Dickinson KM, Collaco JM. Cystic Fibrosis. Pediatr Rev. 2021;42:55-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 80] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 131. | Campagna G, Tagliati C, Giuseppetti GM, Ripani P. Treatment of Psychological Symptoms in Patients with Cystic Fibrosis. J Clin Med. 2024;13:5806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 132. | Sawni A, Breuner CC. Clinical Hypnosis, an Effective Mind-Body Modality for Adolescents with Behavioral and Physical Complaints. Children (Basel). 2017;4:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 133. | Tigges-Limmer K, Brocks Y, Winkler Y, Stock Gissendanner S, Gummert J. Clinical experience with medical hypnosis as an adjunctive therapy in heart surgery. Front Psychol. 2024;15:1356392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 134. | Belsky J, Khanna P. The effects of self-hypnosis for children with cystic fibrosis: a pilot study. Am J Clin Hypn. 1994;36:282-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 135. | Rosen MJ, Dhawan A, Saeed SA. Inflammatory Bowel Disease in Children and Adolescents. JAMA Pediatr. 2015;169:1053-1060. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 335] [Cited by in RCA: 561] [Article Influence: 51.0] [Reference Citation Analysis (0)] |
| 136. | Mourad NF, Hashash JG, Kariyawasam VC, Mourad FH. Management of inflammatory bowel disease: a holistic approach beyond pharmacotherapy. Expert Rev Gastroenterol Hepatol. 2025;19:671-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 137. | Hoekman DR, Vlieger AM, Stokkers PC, Mahhmod N, Rietdijk S, de Boer NK, de Meij TG, Frankenhuis C, D'Haens GR, Benninga MA. Hypnotherapy for Irritable Bowel Syndrome-Type Symptoms in Patients with Quiescent Inflammatory Bowel Disease: A Randomized, Controlled Trial. J Crohns Colitis. 2021;15:1106-1113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 138. | Lee A, Moulton D, Mckernan L, Russell A, Slaughter JC, Acra S, Walker L. Clinical Hypnosis in Pediatric Crohn's Disease: A Randomized Controlled Pilot Study. J Pediatr Gastroenterol Nutr. 2021;72:e63-e70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 139. | Shaoul R, Sukhotnik I, Mogilner J. Hypnosis as an adjuvant treatment for children with inflammatory bowel disease. J Dev Behav Pediatr. 2009;30:268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 140. | Mawdsley JE, Jenkins DG, Macey MG, Langmead L, Rampton DS. The effect of hypnosis on systemic and rectal mucosal measures of inflammation in ulcerative colitis. Am J Gastroenterol. 2008;103:1460-1469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 70] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 141. | Keefer L, Taft TH, Kiebles JL, Martinovich Z, Barrett TA, Palsson OS. Gut-directed hypnotherapy significantly augments clinical remission in quiescent ulcerative colitis. Aliment Pharmacol Ther. 2013;38:761-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 109] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 142. | Moser G. The role of hypnotherapy for the treatment of inflammatory bowel diseases. Expert Rev Gastroenterol Hepatol. 2014;8:601-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 143. | Mustafa MS, Shafique MA, Zaidi SDEZ, Qamber A, Rangwala BS, Ahmed A, Zaidi SMF, Rangwala HS, Uddin MMN, Ali M, Siddiq MA, Haseeb A. Preoperative anxiety management in pediatric patients: a systemic review and meta-analysis of randomized controlled trials on the efficacy of distraction techniques. Front Pediatr. 2024;12:1353508. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 19] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 144. | Lew MW, Kravits K, Garberoglio C, Williams AC. Use of preoperative hypnosis to reduce postoperative pain and anesthesia-related side effects. Int J Clin Exp Hypn. 2011;59:406-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 145. | Schmidt B, Thomas C, Göttermann A, Meißner W, Geißler K, Guntinas-Lichius O, Schirrmeister A. Reducing Perioperative Anxiety and Postoperative Discomfort in Children With Hypnosis Before Tonsillotomy and Adenoidectomy: A Prospective Randomized Trial. Health Sci Rep. 2025;8:e70484. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 146. | Everts R, Muri R, Leibundgut K, Siegwart V, Wiest R, Steinlin M. Fear and discomfort of children and adolescents during MRI: ethical consideration on research MRIs in children. Pediatr Res. 2022;91:720-723. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 147. | Tobias JD, Leder M. Procedural sedation: A review of sedative agents, monitoring, and management of complications. Saudi J Anaesth. 2011;5:395-410. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 137] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 148. | Hallowell LM, Stewart SE, de Amorim E Silva CT, Ditchfield MR. Reviewing the process of preparing children for MRI. Pediatr Radiol. 2008;38:271-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 82] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 149. | Lang EV, Viegas J, Bleeker C, Bruhn J, Geert-Jan van G. Helping Children Cope with Medical Tests and Interventions. J Radiol Nurs. 2017;36:44-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 150. | Ersser SJ, Cowdell F, Latter S, Gardiner E, Flohr C, Thompson AR, Jackson K, Farasat H, Ware F, Drury A. Psychological and educational interventions for atopic eczema in children. Cochrane Database Syst Rev. 2014;2014:CD004054. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 151. | Yosipovitch G, Canchy L, Ferreira BR, Aguirre CC, Tempark T, Takaoka R, Steinhoff M, Misery L. Integrative Treatment Approaches with Mind-Body Therapies in the Management of Atopic Dermatitis. J Clin Med. 2024;13:5368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 152. | Tomecka P, Karwowska A, Kuźnicki J, Skinderowicz K, Wojno A, Markut K, Typek P, Ciesielska U, Kulbacka J, Drąg-Zalesińska M. HPV Infection in Children and Adolescents-A Comprehensive Review. J Clin Med. 2025;14:2425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 153. | Lyszczyk M, Karkhaneh M, Gladwin KK, Funabashi M, Zorzela L, Vohra S. Adverse Events of Mind-Body Interventions in Children: A Systematic Review. Children (Basel). 2021;8:358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 154. | Spanos NP, Stenstrom RJ, Johnston JC. Hypnosis, placebo, and suggestion in the treatment of warts. Psychosom Med. 1988;50:245-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 38] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 155. | Spanos NP, Williams V, Gwynn MI. Effects of hypnotic, placebo, and salicylic acid treatments on wart regression. Psychosom Med. 1990;52:109-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 56] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 156. | Barabasz A, Higley L, Christensen C, Barabasz M. Efficacy of hypnosis in the treatment of human papillomavirus (HPV) in women: rural and urban samples. Int J Clin Exp Hypn. 2010;58:102-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 157. | Gruzelier JH. A review of the impact of hypnosis, relaxation, guided imagery and individual differences on aspects of immunity and health. Stress. 2002;5:147-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 91] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 158. | Kucharczyk E, Pawłuszkiewicz K, Biliński K, Maj J, Ponikowska M. Intralesional Immunotherapy for Non-Genital Viral Warts: A Review of Current Evidence and Future Perspectives. Int J Mol Sci. 2025;26:5644. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 159. | Tušak M, Lapoša A. Treatment of plantar warts using medical hypnosis: a case report. Am J Clin Hypn. 2025;67:152-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 160. | Lugović-Mihić L, Meštrović-Štefekov J, Potočnjak I, Cindrić T, Ilić I, Lovrić I, Skalicki L, Bešlić I, Pondeljak N. Atopic Dermatitis: Disease Features, Therapeutic Options, and a Multidisciplinary Approach. Life (Basel). 2023;13:1419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 45] [Reference Citation Analysis (0)] |
| 161. | Lönndahl L, Abdelhadi S, Holst M, Lonne-Rahm SB, Nordlind K, Johansson B. Psychological Stress and Atopic Dermatitis: A Focus Group Study. Ann Dermatol. 2023;35:342-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 162. | Abdul Latheef E, Riyaz N. Hypnotherapy: A Useful Adjunctive Therapeutic Modality in Hansen's Disease. Indian J Dermatol. 2014;59:166-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 163. | Eason AD, Parris BA. Clinical applications of self-hypnosis: A systematic review and meta-analysis of randomized controlled trials. Psychol Conscious (Wash D C). 2019;6:262-278. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 164. | Stewart AC, Thomas SE. Hypnotherapy as a treatment for atopic dermatitis in adults and children. Br J Dermatol. 1995;132:778-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 50] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 165. | Delaitre L, Denis J, Maillard H. Hypnosis in Treatment of Atopic Dermatitis: A Clinical Study. Int J Clin Exp Hypn. 2020;68:412-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 166. | Derrick E, Karle H, Darley C. The use of self-hypnosis and guided imagery techniques in the management of childhood eczema. J Dermatol Treat. 1994;5:83-84. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 167. | Olness K, Gardner GG. Some guidelines for uses of hypnotherapy in pediatrics. Pediatrics. 1978;62:228-233. [PubMed] |
| 168. | Williams RM, Day MA, Ehde DM, Turner AP, Ciol MA, Gertz KJ, Patterson D, Hakimian S, Suri P, Jensen MP. Effects of hypnosis vs mindfulness meditation vs education on chronic pain intensity and secondary outcomes in veterans: a randomized clinical trial. Pain. 2022;163:1905-1918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 169. | Lang EV, Rosen MP. Cost analysis of adjunct hypnosis with sedation during outpatient interventional radiologic procedures. Radiology. 2002;222:375-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 98] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 170. | Butler LD, Symons BK, Henderson SL, Shortliffe LD, Spiegel D. Hypnosis reduces distress and duration of an invasive medical procedure for children. Pediatrics. 2005;115:e77-e85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 91] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 171. | Gold JI, Kant AJ, Belmont KA, Butler LD. Practitioner review: clinical applications of pediatric hypnosis. J Child Psychol Psychiatry. 2007;48:744-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 172. | Aramideh J, Ogez D, Rondeau É, Duval M, Sultan S. Development and refinement of Rel@x:A training in hypnosis-derived communication for pediatric nurses to prevent procedural pain. Br J Pain. 2022;16:546-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 173. | Neikrug AB, Cho SS, Nguyen ES, Stehli A, Huo S, Garcia C, Au S, Masoumirad M, Cant W, Le-Bucklin KV, Gagliardi JP, Xiong GL, McCarron RM. Improving Behavioral Healthcare Access Disparities by Training Providers in Disadvantaged Communities - Evidence of Strategy Effectiveness. J Gen Intern Med. 2025;40:102-112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 174. | Szmaglinska M, Kirk D, Andrew L. Reporting and Mapping Research Evidence on Perceptions of Clinical Hypnosis Among the General Population and Patients Receiving Health Care Including Cancer Care: A Scoping Review. Int J Clin Exp Hypn. 2024;72:29-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 175. | Geagea D, Ogez D, Kimble R, Tyack Z. Demystifying hypnosis: Unravelling facts, exploring the historical roots of myths, and discerning what is hypnosis. Complement Ther Clin Pract. 2023;52:101776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 176. | Szmaglinska M, Andrew L, Massey D, Kirk D. Exploring the Underutilized Potential of Clinical Hypnosis: A Scoping Review of Healthcare Professionals' Perceptions, Knowledge, and Attitudes. Int J Clin Exp Hypn. 2024;72:109-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 177. | Malloggi E, Santarcangelo EL. Physiological Correlates of Hypnotizability: Hypnotic Behaviour and Prognostic Role in Medicine. Brain Sci. 2023;13:1632. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 178. | Vayne-Bossert P, Hardy J. Is there a role for hypnosis in palliative care? Palliat Care Soc Pract. 2025;19:26323524251321852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 179. | Alotaibi TS. Ethical Challenges with the Informed Consent Process in Pediatric Research Studies. Med Arch. 2024;78:65-67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 180. | Bastek VB, Groeneveld EM, Van Vliet MJ. Medical hypnotherapy; even in a tertiary care setting a promising treatment. Int J Contemp Pediatr. 2022;9:418. [DOI] [Full Text] |
| 181. | Linden JH, Anbar R. Hypnosis Training and Education: Distinctive Features of Training Hypnosis Educators. Am J Clin Hypn. 2017;59:260-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 182. | Lindheim MØ, Helgeland H. Hypnosis Training and Education: Experiences with a Norwegian One-Year Education Course in Clinical Hypnosis for Children and Adolescents. Am J Clin Hypn. 2017;59:282-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 183. | Sultan S, Duval M, Aramideh J, Bőthe B, Latendresse A, Bedu M, Lévesque A, Rondeau É, Le May S, Moussa A, Bourque CJ, Tsimicalis A, Doré Bergeron MJ, Trottier ÉD, Gravel J, Ogez D. Training healthcare professionals in hypnosis-derived communication to mitigate procedural pain in children. Sci Rep. 2025;15:8266. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 184. | Hussain FA. Hypnotherapy as an Adjunct to Medical Treatment: Highlighting Effectiveness and Identifying Barriers to Further Integrative Treatment. J Health Manage. 2021;23:185-196. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 185. | Herbert CP. Teaching hypnosis within a family practice residency program. Fam Med. 1985;17:77-78. [PubMed] |
| 186. | Lam TH, Chung KF, Lee CT, Yeung WF, Yu BY. Hypnotherapy for insomnia: A randomized controlled trial comparing generic and disease-specific suggestions. Complement Ther Med. 2018;41:231-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 187. | Shakhnovich V, Hornik CP, Kearns GL, Weigel J, Abdel-Rahman SM. How to Conduct Clinical Trials in Children: A Tutorial. Clin Transl Sci. 2019;12:218-230. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 188. | Kohlenberg S, Gerson L. Pilot: does clinical hypnosis training impart the confidence needed to use it? Am J Clin Hypn. 2024;66:203-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 189. | Dang A, Arora D, Rane P. Role of digital therapeutics and the changing future of healthcare. J Family Med Prim Care. 2020;9:2207-2213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 109] [Cited by in RCA: 117] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 190. | Al-Beltagi M, Saeed NK, Bediwy AS, Alhawamdeh R, Qaraghuli S. Effects of COVID-19 on children with autism. World J Virol. 2022;11:411-425. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 191. | Hasan SS, Vasant D. The Emerging New Reality of Hypnosis Teletherapy: A Major New Mode of Delivery of Hypnotherapy and Clinical Hypnosis Training. Int J Clin Exp Hypn. 2023;71:153-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 192. | Do NM, Manière MC, Lefebvre F, Clauss F. Efficacy of virtual reality hypnosis versus conscious sedation with nitrous oxide in the management of dental anxiety in pediatric dentistry: protocol for a prospective randomized controlled trial. Trials. 2025;26:201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 193. | Nguyen KH, Comans T, Nguyen TT, Simpson D, Woods L, Wright C, Green D, McNeil K, Sullivan C. Cashing in: cost-benefit analysis framework for digital hospitals. BMC Health Serv Res. 2024;24:694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 194. | Kihlstrom JF. Neuro-hypnotism: prospects for hypnosis and neuroscience. Cortex. 2013;49:365-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 64] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/