Published online May 20, 2015. doi: 10.5493/wjem.v5.i2.64
Peer-review started: October 16, 2014
First decision: December 17, 2014
Revised: January 9, 2015
Accepted: February 4, 2015
Article in press: February 9, 2015
Published online: May 20, 2015
Processing time: 217 Days and 14.4 Hours
Over the last decades, nitric oxide (NO) has been definitively recognised as one of the key players involved in immunity and inflammation. NO generation was originally described in activated macrophages, which still represent the prototype of NO-producing cells. Notwithstanding, additional cell subsets belonging to both innate and adaptive immunity have been documented to sustain NO propagation by means of the enzymatic activity of different nitric oxide synthase isoforms. Furthermore, due to its chemical characteristics, NO could rapidly react with other free radicals to generate different reactive nitrogen species (RNS), which have been intriguingly associated with many pathological conditions. Nonetheless, the plethora of NO/RNS-mediated effects still remains extremely puzzling. The aim of this manuscript is to dig into the broad literature on the topic to provide intriguing insights on NO-mediated circuits within immune system. We analysed NO and RNS immunological clues arising from their biochemical properties, immunomodulatory activities and finally dealing with their impact on different pathological scenarios with far prompting intriguing perspectives for their pharmacological targeting.
Core tip: Nitric oxide (NO) is a diffusible molecule, which is responsible for many physiological and pathological conditions. In this work we described some of its chemical characteristics and how it is generated. More, NO could rapidly react with other free radicals to generate different reactive nitrogen species (RNS). Indeed, we addressed the contribution of NO/RNS in different immune cells and how these reactive molecules are pivotal to control cellular responses focusing on inflammatory settings.
- Citation: Predonzani A, Calì B, Agnellini AH, Molon B. Spotlights on immunological effects of reactive nitrogen species: When inflammation says nitric oxide. World J Exp Med 2015; 5(2): 64-76
- URL: https://www.wjgnet.com/2220-315X/full/v5/i2/64.htm
- DOI: https://dx.doi.org/10.5493/wjem.v5.i2.64
Nitric oxide (NO) is a diffusible molecule, which is involved in many different physiological and pathological conditions. It modulates blood flow[1,2], neural activity[3] and immune defence mechanism[4].
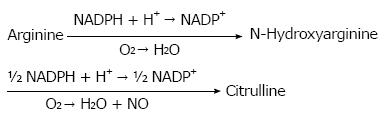
In biological systems, NO is mainly synthesised enzymatically starting from L-argine according to the following chemical reaction:
Math 1
This reaction is catalysed by three different enzymes, identified in the ‘90s, encoded by different genes with different localization, regulation, catalytic properties and inhibitor sensitivity, called respectively neuronal (nNOS or NOS1), inducible (iNOS or NOS2) and endothelial (eNOS or NOS3) nitric oxide synthase.
Genomic organization is similar among these isoforms suggesting a common ancestral progenitor and is composed by a bidomains structure (an oxigenase domain at N-term and a reductase one at C-term) with a intervening calmodulin (CaM) binding region between the two[5]. Calmodulin is necessary for the activity of all these enzymes, even though Ca2+-dependence of NO synthesis distinguishes the NOS isoforms, with nNOS and eNOS having a much higher Ca2+ requirement than iNOS.
nNOS and eNOS are constitutively expressed among several cell types, including the endothelium, platelets, and neurons. Their function is mainly dependent on an intracellular calcium rise, even though other calcium independent mechanisms could impact on it, for example shear stress[6-10].
On the other hand iNOS is largely expressed only after induction by immunologic and inflammatory stimuli and its role in the direct protection against pathogens has been clearly demonstrated. For example, the requirement of iNOS for the eradication of Mycobacterium tuberculosis infection has been established[11] as well for other Listeria monocytogenes[12] and the protozoan parasite Leishmania major[13,14] in the '90s. Recent evidence has contributed to clarify mechanisms upon this immune response[15-17].
A fourth enzyme has been more recently characterised in rat liver and named mithocontrial NO synthase or mtNOS[18,19]. This latter enzyme has been shown to be constitutively active, calcium dependent and ascribable for mitochondria homeostasis and bioenergetics. Indeed, it has been shown mainly by the group of Ghafourifar that activation of mtNOS upon chemotherapeutic drug administration induces oxidative and nitrative stress, with consequent apoptosis of cells[20,21].
NO is not only the product of NOS enzymes but it is also generated in tissues by either direct disproportionation or reduction of nitrite to NO under the acidic and highly reduced conditions occurring in disease states, such as ischemia[22-24]. The biological significance of this alternative source of NO production consists in restoring physiological NO level when enzymatic production is uncoupled or dysregulated, as in atherosclerosis[25] or other inflammatory status[26].
Unlike reactive oxygen species (ROS), which are directed into the phagosome, NO is synthesised in the cytoplasm of the cell and diffuse rapidly across cell membrane[4]. Due to its chemical characteristics, NO could rapidly react with other free radicals such as O2-• to generate the highly reactive oxidant peroxinitrite (ONOO-) and other reactive nitrogen species (RNS), which have been intriguingly associated with many pathological conditions such as chronic inflammation, atherosclerosis[27], diabetes[28], inflammatory bowel disease[29] and autoimmune diseases[30]. Peroxynitrite has multiple cytotoxic effects which are ascribable to aberrant generation of proteins, post-translational modification (PTMs) of the existing ones, DNA damage, activation of poly(ADP-ribose), mitochondrial dysfunction and cell death thus widely affecting transcriptional regulation, gene expression and cell signalling[31,32].
Among the several RNS-induced modifications, the prevalent reaction is the coupling of a NO moiety with sulfhydryl groups on proteins, yielding S-nitrosothiols. The most affected residue is tyrosine. Nowadays, the presence of nitro-tyrosine is commonly accepted as a hallmark of in situ inflammation and is associated with many different pathologies, spacing from atherosclerosis, genetic disorders to cancer[33-36]. However, NO alone is not capable of nitrating tyrosine thus the accumulation of 3-nitrotyrosine is the reaction product of the other RNS[37]. Moreover, under inflammatory conditions, tyrosine nitration may be dependent on the activity of myeloperoxidase, secreted by monocytes and polymorphonuclear neutrophils[38].
The biological significance of such modified residues lied in altered protein degradation[39], modification in protein properties[40,41], resulting signalling[42] and many other phenomena[43].
Tyrosine is not the only amino acid that is affected by the presence of RNS. Indeed, most of the amino acids containing aromatic rings could react with RNS and ROS. Among these, modifications of tryptophan were highlighted. Initially, nitration of tryptophan residues in proteins was assessed by means of proteomic assays, such as decreased in tryptophan-associated fluorescence and mass spectrometry, and was associated with decreased functionality of modified proteins[44]. However, the majority of the studies so far was unable to detect nitro-tryptophan derivatives in vivo due to the lack of good antibodies. This gap was recently filled by Ikeda and collaborators, who developed an antibody specifically reactive with nitrated tryptophan residues[45]. This tool boosted the investigation of the presence of such modification in vivo. Ikeda and Yamakura in their studies identified 6-nitrotryptophan residues in extract of PC12 cells, suggesting that NO production drives physiological processes, such as differentiation and morphological changes. These claims were further supported by similar consequences observed upon tyrosine modifications[46-48].
NO has been generally recognised as one of the key players involved in immunity and inflammation. In infectious conditions, NO displays antiviral and antimicrobial activities, both cytotoxic (tissue-damaging) and cytoprotective (tissue-preserving), acting as either an immunostimulatory (proinflammatory) or immunosuppressive (anti-inflammatory) agent. Most of NO-mediated immune effects have been demonstrated to be dependent on the activity of iNOS enzyme which, apart from releasing NO, provokes the depletion of local arginine (together with arginase) in macrophages or other host cells sustaining growth inhibition and death of the parasites[4]. Although it has been proposed that efficient pathogen killing require colocalization of iNOS with pathogen-containing compartments[49,50], the fact that NO can diffuse across cell membranes might allow for an antimicrobial activity at distance, even in those cases where NO acts in cells that do not express iNOS[51]. However, Olekhnovitch et al[52] have recently proposed a novel cooperative mechanism of collective NO production to sustain tissue-wide immunity during infections. Indeed authors provide evidence that the diffusion of NO from numerous phagocytes at the site of infection promotes equally effective parasite killing in NO-producing cells and bystander cells[52].
Further more, over the last decades, several reports attempted to definitively clarify NO appointment in the immune system[4]. Nevertheless, the plethora of heterogeneous NO-mediated responses precludes an univocal definition thus demanding additional investigations. Although NO activity mainly lies on its local spatio-temporal concentration, the phenotype and functional commitment of the immune cells, responsible for its generation, dramatically impact on its own activity. Additionally, given the intrinsic nature of this highly-diffusible uncharged gas, specific immune subsets become selective NO-targets even if not directly involved in its production.
This part of the review aims to provide intriguing spotlights on the role of NO in different immune cell subsets belonging to both innate and adaptive immunity.
Dogmatically, NO is produced by macrophages by means of iNOS activity which is transcriptionally primed by cytokines and microbial stimulation. The sustained generation of NO endows macrophages with cytostatic or cytotoxic activity against pathogens and tumour cells[53,54]. Although the production of NO by human macrophages remains controversial, growing evidence supports this notion providing data for the expression and activity of iNOS and eNOS isoforms in these cells[55].
Historically, macrophages were divided into two major categories (M1/M2) depending on their activation status and inflammatory attitude, even though this paradigm has been recently expanded to account for their enormous functional plasticity[56,57].
In 2000, Mills et al[58] ascertained a relevant metabolic discrepancy between M1/M2 subsets mainly due to a remarkable difference in arginine metabolism. Once differentiated, M1 or classically activated macrophages trigger Th1 immune response and secrete high amounts of NO to kill intracellular pathogens and to exert cytotoxicity towards tumour cells[59]. On the other side, M2 macrophages express high levels of arginase-I, which competes with iNOS for their common substrate L-arginine, thus preventing NO generation[60].
It is thus clear that NO represents a remarkable hallmark of macrophage activation states in pathological settings and that both macrophages and NO fulfil relevant and divergent roles in cancer biology. Mechanistically, it has been proposed that in the early stages of tumour progression, macrophages exploit high concentrations of NO and RNS to kill tumour cell clones. Later on, tumour-reprogrammed macrophages produce low levels of NO/RNS, which in turn promote cancer growth and spreading.
Weiss et al[61] postulated that NO, produced by intratumoural macrophages, represents the crucial determinant for the anti-metastatic potential of IL-2/α-CD40 immunotherapy. Conversely, iNOS expression and the coincident NO/RNS generation has been shown to contribute to the immunosuppressive attitude of myeloid-derived suppressor cells (MDSCs), a heterogeneous cell population associated with tumours[42,62,63].
The dichotomous activity of macrophage-derived NO definitely mirrors the aforementioned functional plasticity of these cells in response to environmental cues. The multifaceted role of NO in cancer will be deeply scrutinise in the proper paragraph of this manuscript named “NO, RNS and cancer”.
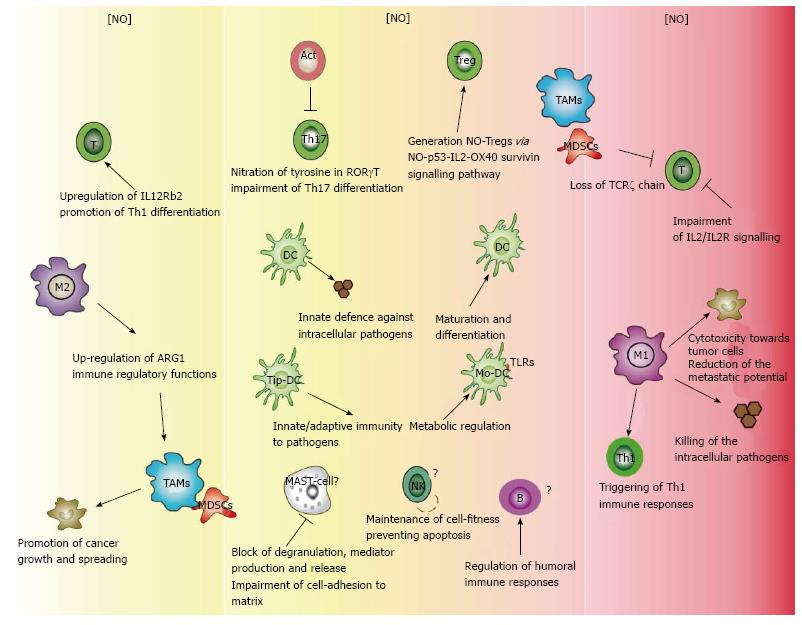
NO represents a master regulator for the activity of other different immune subsets such as T lymphocytes, dendritic cells (DCs), natural killer cells (NKs) and mast cells. As for macrophages, NO potentially exhibits either positive or negative modulatory properties in all these subsets.
In cancer, it has been postulated that high concentration of NO impairs T cell functions by blocking the signalling cascade downstream of IL-2 binding the IL-2 receptors[64]. On the other side, lower concentrations of NO have been shown to promote Th1 differentiation by selectively up-regulating IL-12 receptor beta 2[65].
More recently, a cogent paper demonstrated that NO produced by iNOS in activated T cells impairs TH17 cell differentiation trough the nitration of tyrosine residues in RORγt thus regulating IL-17 expression at the transcriptional level[66]. An interesting report designated NO as the driving force for the generation of a new subset of regulatory cells (NO-Tregs) via the NO-p53-IL-2-OX40-survivin signalling pathway[67]. Nonetheless, by means of syngeneic mouse melanoma model, Jayaraman et al[68] postulated that iNOS, expressed by CD4+ T cells, manifestly inhibits their commitment to Treg by blocking the release of TGF-β1.
Although compelling studies addressed the role of NO in T cell biology, NO contribution to the regulation of B cell activity remains unclear. Very recently, Giordano and colleagues shed light on the role of NO in regulating humoral immune responses. Indeed, authors suggested that NO generated by both inflammatory Mo-DCs and non-hematopoietic cells potentially regulate T cell-independent (TI)-2 antibody responses by inhibiting BAFF production[69].
DCs are the most powerful APCs of the immune system[70,71] representing the bridge between innate and adaptive immunity. In the canonical maturation pathway, microbial products trigger DCs activation, which leads to the production of large amounts of cytokines, especially IL-12 and IFN-α, driving the differentiation of naive T-cells into effector cells[72,73]. Moreover, DCs exposed to inflammatory cytokines rapidly activate other innate protective cells such as NK and NKT cells[74]. So far, the role of DCs as potential NO-producing cells has not been fully investigated and data concerning the impact of NO on DC maturation and functions are still debated. During the last years, several reports investigated this issue. Activated murine DCs do essentially express the iNOS isoform in response to cytokines or pathogen stimulation[75]. Conversely, the expression of iNOS and the production of NO during the commitment of human DCs are still debated. A recent report claimed that in the human immune system nNOS but not iNOS mediated NO synthesis is pivotal for the maturation and differentiation of these cells[76]. Nevertheless, the expression of iNOS as well as NO production clearly participate in the innate defence against intracellular pathogens[77].
Additionally, an interesting study by means of real-time metabolic flux analysis pointed out NO as the key metabolic regulator in inflammatory monocyte-derived DCs, expressing iNOS, in response to TLR stimulation[78]. In 2003, a groundbreaking publication firstly identified a new TNF/iNOS-producing (Tip)-DC subset in the spleens of Listeria monocytogenes-infected mice[79], whose role was recently clarified. Specifically, these cells act as sources of NO in a variety of infections clearly indicating that NO produced by DCs actively participates in both innate and adaptive immunity to pathogens[80,81].
NK cells are effectors of the innate immune system, instrumental for host defence toward infection from bacteria, virus and parasites[82]. Moreover, NKs actively participate in tumour surveillance and rejection of transplanted organs[83]. Nonetheless, the role of NO in NK cell activation is not completely understood. NOS isoform activity correlates with rodent NK cell-mediated cytotoxicity, as proved by both nitrite accumulation and pharmacological enzymatic interference[84]. In humans, the mechanism of NO production in NK cells needs to be clarified. It was proposed that the endogenous NO generation by active eNOS isoform prevents NK cells from activation-induced apoptosis, thereby maintaining cell fitness[85].
Mast cells (MCs) are widely distributed throughout the extravascular area in the body where they play versatile roles dealing with innate immunity, IgE-mediated allergy and inflammation. Indeed, they promote neutrophil phagocytosis, lymph node hyperplasia and can directly phagocytise and kill bacteria[86].
Data concerning NO/RNS generation by either rodent or human mast cells are still controversial. While investigating this topic in 2004, Swindle and colleagues concluded that activated rodent and human mast cells were unable to generate intracellular NO or to express iNOS[87]. According to this study, foregoing reports, indicating a potential NO-like activity in peritoneal mast cells, were misled by the presence of NO-producing macrophage in their cell preparation[88].
Conversely, a different group demonstrated the expression of NOS isoforms and production of NO by various MC populations including rat peritoneal MCs, human skin MCs (HSMC) and human mast cell lines (HMC-1 and LAD-2)[89,90].
Nevertheless, as reviewed for other immune subsets, it is well accepted that exogenous NO centrally impacts on mast cell functions. Exploiting a variety of either NO chemical donors or NOS inhibitors on both primary or mast cell lines, introductory reports in the field showed that NO blocks antigen-induced degranulation, mediator production and release[91]. Moreover, NO has been shown to promote CD8α up-regulation trough NO-cGMP pathway in rat peritoneal MCs. This remarkable event enlarges CD8 receptor sensitivity to alternative signals and coincidently boosts MC-mediated immune responses[92]. It is well known that during activation processes, MCs adhere to the extracellular matrix basically interacting with fibronectin, vitronectin, collagen type I, collagen type IV, and laminin. NO impairs human MC adhesion to the matrix by an alternative mechanism that is mainly independent of the direct activation of sGC or RNS generation[93] (Table 1 and Figure 1).
| Cell compartment | Features | Ref. |
| Innate immunity | ||
| Macrophage | ||
| M1 | High level of NO | [55-59,61] |
| Expression of iNOS | ||
| NO-mediated cytotoxicity | ||
| M2 | Reduced level of NO | |
| Immune suppressive function | ||
| Natural Killer cells | ||
| NO-mediated cytotoxicity | [84,85] | |
| NO-mediated cell fitness | ||
| Mast cells | ||
| NOS expression | [87,89-91,93] | |
| NO-mediated cell adhesion and function | ||
| Myeloid-derived suppressor cell | ||
| iNOS expression | [62,64,94,95] | |
| Immune modulating function | ||
| Dendritic cells | ||
| NOS expression | [72,73,75-77] | |
| Pathogen clearance | ||
| Adaptive immunity | ||
| Lymphocyte | ||
| T-cell | T-cell activation and function | [64-68,72,73] |
| T-cell commitment | ||
| B-cell | Reduced level of NO | [69] |
| T-independent antibody response | ||
In addition to promote an effective immune response in the control of infectious diseases, iNOS-mediated NO production may be involved in the dysregulation of immunity, playing a role in chronic inflammatory disorders. Autoimmune diseases could be considered as a chronic inflammatory status where the breakdown of immune tolerance, a complex process involving both genetic and environmental factors, is mainly caused by the post-translational modification of antigens. This occurrence results in the recognition of host proteins as “non-self” and indeed in the initiation of an adaptive immune response. Many inflammatory autoimmune diseases, which are accompanied by oxidative stress, exhibit an excess of reactive chemical species that are able to post-translationally modify proteins, potentially forming neo-epitopes[30,96-98]. These neo-epitopes may directly elicit an adaptive immune response or indirectly sustaining other mechanisms such as the molecular mimicry (a host antigen being “seen” as a “non-self” protein), the exposure of cryptic epitopes (exposure of amino acid sequences after changes in the three-dimensional structure of a protein), the epitope spreading (spreading of antigenicity from a given epitope to other parts of the same protein or other proteins) and the coupling of an autoantigen to an exogenous antigen[99,100]. Increased generation of neo-epitopes/PAMPs/DAMPs may therefore serve as a mechanism for increased uptake and presentation of autoantigens to the immune system, hence for example the accumulation of nitrotyrosine-containing proteins in tissues might induce an autoimmune response and sustain a chronic inflammatory reaction[96]. Indeed, murine models of systemic lupus erythematosus (SLE) showed abnormally high levels of RNS compared with normal mice and the systemic blockade of RNS production ameliorates the pathology[101]. Further and not surprisingly, elevated levels of anti-nitrotyrosine antibodies have also been measured in the synovial fluid of patients with rheumatoid arthritis and osteoarthritis[102] as well as in serum from patients with SLE[103-105]. This finding was also verified in patients with active lupus nephritis, who have higher levels of serum nitrotyrosine than those without renal disease, suggesting that overproduction of NO and its derived reactive species may have a pathological role in SLE and lupus nephritis[106,107].
Diabetes mellitus is a chronic disease characterised by elevated blood sugar levels resulting from either a lack of insulin production or resistance to insulin[108]. Hyperglycaemia, glucose autoxidation, accumulation of advanced glycosylation end products (AGEs), enhanced receptor for advanced glycation end product (RAGE) and angiotensin II receptor type 1 (AT1R) signalling as well as elevated levels of free fatty acids and leptin, have been reported to contribute to elevated production of ROS and RNS in diabetic vessels and myocardium[109,110]. Several reports suggest a positive correlation between increased serum and/or vascular 3-nitrotyrosine levels, increased blood pressure and/or endothelial dysfunction in diabetic patients[111,112]. Additionally, high oxidative and nitrative stress in diabetes might induce oxidation and/or nitration of various insulin receptors in peripheral tissues, which may contribute to the development of insulin resistance[113]. Moreover, peroxynitrite injury has been implicated in the “metabolic memory” phenomenon, which refers to the therapeutic effects of intensive glycemic control achieved by early intervention in both experimental and clinical studies[28,114]. In diabetic hearts, the persistent myocardial oxidative and nitrative stress might also leads to dysfunction of important antioxidant defense mechanisms, such as the inactivation of superoxide dismutases and catalase and depletion of endogenous antioxidants, as metallothionein and glutathione[115,116] and dysregulation of important redox-dependent transcription factors [e.g., NFE2L2 nuclear factor, erythroid 2-like 2 (Nrf2)][117,118]. However, peroxynitrite-induced protein nitration has been involved in the development of chronic diabetic peripheral neuropathy[119] and has been documented in peripheral nerve[120], vasa nervorum[121], spinal cord and dorsal root ganglion of streptozotocin-diabetic and obese mice[120,122], indicating that diabetes creates not just oxidative, but oxidative-nitrosative stress in the peripheral nervous system.
As in other inflammatory disorders, NO plays a dual role in modulating neuroinflammation. On one hand, NO might induce apoptosis of auto-reactive T cells that enter the central nervous system (CNS)[123]; on the other hand, NO produced by iNOS within the CNS predominantly contributes to multiple sclerosis and experimental autoimmune encephalomyelitis (EAE) pathogenesis[124]. Particularly, NO and peroxynitrite accumulation may affect the components of CNS causing lipid peroxidation and consequent damage of oligodendrocytes[125], disruption of blood-brain barrier integrity[126], activation of matrix metalloproteinases[127], with a block in axonal conduction[128] and finally promoting axonal degeneration[129]. Interestingly, recent findings on CNS of EAE rats demonstrated that iNOS-derived NO potently inhibits CXCL12 gene expression in a p38-dependent manner in vitro and that inhibition in vivo of iNOS activity sustains CXCL12 expression and protection of rats from EAE[130].
Early in the 1990s, various studies based on animal models as well as in humans, indicated that NO may be involved in gastrointestinal inflammation and that it may have a pathogenetic role in inflammatory bowel disease (IBD)[131]. Analysis of rectal biopsy specimens from patients with active ulcerative colitis showed higher concentrations of citrulline, the co-product of NO synthase, with respect to those from patients with quiescent disease or a normal histology, indicating that the increased biosynthesis of citrulline might be a consequence of NO synthase activity[132]. Additionally, NO produced following the up-regulation of iNOS in colonic epithelial cells has been closely associated with the initiation and maintenance of IBD[29]. Notwithstanding, the exact role of NO overproduction in intestinal inflammation remains obscure, since it has been reported that NO production plays a beneficial role in the acute nonspecific colitis settings. On the other hand however, in models of chronic colitis accompanied by a dysregulated immune response, where iNOS is persistently up-regulated, NO displays a detrimental activity on mucosal integrity[29]. High levels of NO from iNOS may in fact exacerbate the clinicopathological features of colitis by direct cytotoxicity, activation of neutrophils[133], vasodilatation and reduced smooth muscle tone[134].
As already mentioned, NO and its derivative have been extensively associated with many different pathologies. The connection between cancer and inflammation dates back to 1863, when Rudolf Virchow noted leucocytes in neoplastic tissues, suggesting that the “lymphoreticular infiltrate” reflected the origin of cancer at sites of chronic inflammation[135]. Moreover, smouldering inflammation increases the risk of developing many types of cancer, including bladder, cervical, gastric, intestinal, oesophageal, ovarian, prostate and thyroid cancer[136,137], thus representing one of the novel additional hallmarks of cancers[138]. As a result of chronic inflammation, tumour microenvironment harbours different corrupted resident or purposely recruited cells which exert conflicting functions establishing a peculiar cytokine milieu[139]. Among these, tumour-associated macrophage (TAM) and myeloid-derived suppressor cells (MDSCs) present in tumour overexpress iNOS and release oxidizing molecules, such as hydrogen peroxide (H2O2) and peroxynitrite (ONOO-) which cause nitration and nitrosylation of components of the T cell receptor (TCR) signalling complex, and the loss of the TCR δ-chain, thereby inhibiting T cell activation through the TCR and contributing to tumour progression[95,140,141]. More recently, Molon et al[142], in 2011, have demonstrated that chemokine nitration prevents intratumoural infiltration of antigen-specific T cells, which remained confined at the edge of tumours being unable to reach the central core due to the nitration of CCL2, a master chemokine. Moreover, several investigators have reported the expression of iNOS by malignant cells or within the tumour microenvironment, both at mRNA and protein level. In breast carcinoma, an initial study suggested that iNOS activity was higher in less differentiated tumours and detected predominantly in TAMs[143]. Subsequently, other reports demonstrated that iNOS was also expressed by breast carcinoma cells and positively correlated with tumour stage[144] and microvessel density[145]. In addition to breast cancer, iNOS is markedly expressed in approximately 60% of human colon adenomas and in 20%-25% of colon carcinomas, while the expression is either low or absent in the surrounding normal tissues. Similar results were obtained for human ovarian cancer and melanoma. Other cancers that express iNOS are head and neck, oesophagus, lung, prostate, bladder and pancreatic carcinomas, brain tumours, Kaposi’ s sarcoma, mesothelioma, and haematological malignancies[63]. Moreover, the eNOS has been found in both endothelial and tumour cells of breast carcinomas, and the nNOS has been detected in some oligodendroglioma and neuroblastoma cell lines. However, the role of NO in cancer biology has not been clearly elucidated yet, since various studies have shown that NO may either promote or inhibit tumour progression and metastasis. The net effect of NO in tumours seems to depend on the activity and localization of NOS isoforms, concentration and duration of NO exposure, cellular sensitivity and hypoxia/re-oxygenation process within tumour microenvironment[146]. In general, high concentrations of NO and RNS can arrest cell cycle (cytostatic effect) or induce cell death, whereas low concentrations may protect cells from apoptosis. In fact, generation of high levels of NO/RNS is a very effective tool to induce cell death, and macrophages use it as a major weapon in their arsenal against invading pathogens and tumour cells[147]. High levels of NO/RNS post-translationally modify death-related target proteins, as the death receptors of the TNF-α superfamily, and block respiration in target cells by affecting the mitochondrial respiratory chain and its outer membrane permeability and thus leading to the release of cytochrome c and apoptosis initiation[148,149]. Moreover, high NO concentrations, oxidizing and/or deaminating the DNA bases, result in DNA breaks, DNA base modifications or DNA cross-links, which cause mutations that may either activate oncogenes or deactivate tumour suppressor genes. In addition, NO/RNS-driven protein modifications such as S-nitrosylation or nitration may inhibit proteins belonging to the DNA repair systems, driving to genomic instability[150,151]. Importantly, DNA damages that cannot be repaired cause apoptosis induction, by the activation of DNA-damage-sensing proteins (e.g., p53, PARP, DNA-PK, BRCA1, ATM)[152]. However, NO has been demonstrated to inhibit programmed cell death in endothelial cells and some liver cancer cell lines, mainly through S-nitrosylation of the active-site cysteine of caspases[153], thus perpetuating mutations and consequently sustaining transformation[154,155]. On the other hand, NO may induce apoptosis either via down-regulation of the anti apoptotic protein survivin, as observed in human lung carcinoma cells[156], or up-regulation of Fas expression, as shown in ovarian carcinoma cell lines, through the specific inactivation of the transcription repressor yin-yang-1, which binds to the silencer region of the Fas promoter[157]. Besides enhancing cytotoxicity, NO plays a role in angiogenesis and metastasis since several reports showed a positive correlation between NOS expression/activity in tumour tissues and lymphatic metastasis in head and neck, thyroid, breast, stomach, gallbladder cancers[146,158] and melanoma[159]. As under physiologic conditions, NO maintains blood flow by dilatation of arterial vessels, promotes perivascular cell recruitment and vessel remodelling and maturation within tumours[146]. NO exposure of A-431 squamous carcinoma cells and MDA-MB-231 breast cancer cells was, in fact, able to induce VEGF-C expression, which mediates lymphangiogenesis and metastasis[160]. However, NO may also inhibit the aggregation of platelets through a cGMP-dependent mechanism, preventing aggregates formation with tumour cells, which may facilitate their adhesion to vascular endothelial cells and haematogeneous dissemination[161]. Finally, as previously mentioned, NO/RNS can suppress tumour-specific adaptive immunity through several mechanisms. One mechanism involves the inhibition of phosphorylation, and thereby the activation of important signalling proteins in the IL-2-receptor pathway [including Janus activated kinase 1 (JAK1), JAK3, STAT5, extracellular-signal-regulated kinase (ERK) and AKT] in T cells[162]. Additionally, NO promotes tumour immunosuppression, by affecting the stability of IL-2 encoding mRNA and the release of IL-2 by activated human T cells[163]. Finally, NO/RNS may dampen anti-tumour immunity through post-translational modifications of key proteins for T cell activation, such as CD8 and TCR complex α/β chains molecules[42] and T lymphocyte recruitment to the tumour site, such as the chemokine CCL2[142]. Thus, interfering with NO/RNS production within tumour microenvironment may represent a promising successful strategy to implement the efficacy of anti-tumour therapy alone or, even better, in combination with conventional chemotherapy, radiotherapy, photodynamic therapy and immunotherapy approaches[164-167] (Table 2).
| Disease | Pathogenesis | Ref. |
| Autoimmune diseases | ||
| Appearance of neo-epitopes | [29,30,96-98,101,123, 126,130] | |
| Disruption of physical barriers | ||
| Amelioration of pathological status | ||
| Metabolic disease | ||
| Deregulated accumulation of proteins or their abnormal modification | [109,110,115,119,120] | |
| Cancer | ||
| Establishment of an immune suppressive environment | [140-142,147,151,152, 155,157,160] | |
| Alteration in DNA repair mechanisms | ||
Over the last decades, the role of NO in the immune system has been extensively reviewed. While investigating NO-mediated responses, a number of reports argued for either a NO-stimulatory or -inhibitory activity in distinctive immune events. Nonetheless, the generation of NO in several immune cell subsets remains still controversial thus demanding additional studies.
So far, a general consensus in the field has been achieved highlighting the indisputably role of this diffusible mediator in shaping immune activities.
This manuscript aims to provide spotlights on NO-moulded biology specifically focussing on its pivotal participation in distinctive inflammatory programs. Indeed throughout this review, we scrutinised the role of NO in selective scenarios starting with the description of its biochemical properties, immunomodulatory activities and finally dealing with its remarkable impact on different pathological settings. Collectively all the aforementioned investigations pointed out the relevance of NO-mediated effects in the regulation of either innate or adaptive immunity.
Additionally, the combination of NO with other reactive species originates RNS, which are actively involved in several pathological conditions such as chronic inflammation, autoimmune diseases and cancer. Basically, RNS generate and amplify distinctive inflammatory circuits by affecting protein structure and functions, gene expression, cell signalling and cell death.
Hence, this manuscript also emphasises the duplicity of NO-mediated responses in distinctive immune cell subsets. This dichotomous attitude apparently hinders the identification of NO as a foolproof target thus preventing the identification of feasible therapeutic strategies that could be rapidly delivered to the clinic. Nonetheless, we believe that the plasticity of NO signals could be potentially exploited for the development of new focussed pharmacological approaches.
Of note, RNS-mediated PTMs potentially represent a novel marker for monitoring the efficacy of therapy during disease treatment or in the follow-up care.
This pursuit requires a thorough understanding of NO/RNS biology in the context of the immune system thus opening the way for intriguing investigations.
| 1. | Wolin MS. Reactive oxygen species and the control of vascular function. Am J Physiol Heart Circ Physiol. 2009;296:H539-H549. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 102] [Cited by in RCA: 95] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 2. | Wolin MS. Reactive Oxygen Species and Nitric Oxide in Vascular Function, in Studies on Pediatric Disorders. New York: Springer 2014; 15-33. |
| 3. | Steinert JR, Robinson SW, Tong H, Haustein MD, Kopp-Scheinpflug C, Forsythe ID. Nitric oxide is an activity-dependent regulator of target neuron intrinsic excitability. Neuron. 2011;71:291-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 86] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 4. | Bogdan C. Nitric oxide and the immune response. Nat Immunol. 2001;2:907-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2383] [Cited by in RCA: 2495] [Article Influence: 99.8] [Reference Citation Analysis (0)] |
| 5. | Smith BC, Underbakke ES, Kulp DW, Schief WR, Marletta MA. Nitric oxide synthase domain interfaces regulate electron transfer and calmodulin activation. Proc Natl Acad Sci USA. 2013;110:E3577-E3586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 84] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 6. | Wang W, Ha CH, Jhun BS, Wong C, Jain MK, Jin ZG. Fluid shear stress stimulates phosphorylation-dependent nuclear export of HDAC5 and mediates expression of KLF2 and eNOS. Blood. 2010;115:2971-2979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 162] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 7. | Suhr F, Brenig J, Müller R, Behrens H, Bloch W, Grau M. Moderate exercise promotes human RBC-NOS activity, NO production and deformability through Akt kinase pathway. PLoS One. 2012;7:e45982. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 74] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 8. | Ramírez-Vélez R, Bustamante J, Czerniczyniec A, Aguilar de Plata AC, Lores-Arnaiz S. Effect of exercise training on eNOS expression, NO production and oxygen metabolism in human placenta. PLoS One. 2013;8:e80225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 9. | Kasamatsu S, Watanabe Y, Sawa T, Akaike T, Ihara H. Redox signal regulation via nNOS phosphorylation at Ser847 in PC12 cells and rat cerebellar granule neurons. Biochem J. 2014;459:251-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Song T, Hatano N, Sugimoto K, Horii M, Yamaguchi F, Tokuda M, Miyamoto Y, Kambe T, Watanabe Y. Nitric oxide prevents phosphorylation of neuronal nitric oxide synthase at serine1412 by inhibiting the Akt/PKB and CaM-K II signaling pathways. Int J Mol Med. 2012;30:15-20. [PubMed] |
| 11. | MacMicking JD, North RJ, LaCourse R, Mudgett JS, Shah SK, Nathan CF. Identification of nitric oxide synthase as a protective locus against tuberculosis. Proc Natl Acad Sci USA. 1997;94:5243-5248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 949] [Cited by in RCA: 873] [Article Influence: 30.1] [Reference Citation Analysis (0)] |
| 12. | MacMicking JD, Nathan C, Hom G, Chartrain N, Fletcher DS, Trumbauer M, Stevens K, Xie QW, Sokol K, Hutchinson N. Altered responses to bacterial infection and endotoxic shock in mice lacking inducible nitric oxide synthase. Cell. 1995;81:641-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1125] [Cited by in RCA: 1077] [Article Influence: 34.7] [Reference Citation Analysis (0)] |
| 13. | Wei XQ, Charles IG, Smith A, Ure J, Feng GJ, Huang FP, Xu D, Muller W, Moncada S, Liew FY. Altered immune responses in mice lacking inducible nitric oxide synthase. Nature. 1995;375:408-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1003] [Cited by in RCA: 973] [Article Influence: 31.4] [Reference Citation Analysis (0)] |
| 14. | Diefenbach A, Schindler H, Donhauser N, Lorenz E, Laskay T, MacMicking J, Röllinghoff M, Gresser I, Bogdan C. Type 1 interferon (IFNalpha/beta) and type 2 nitric oxide synthase regulate the innate immune response to a protozoan parasite. Immunity. 1998;8:77-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 298] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 15. | Elks PM, Brizee S, van der Vaart M, Walmsley SR, van Eeden FJ, Renshaw SA, Meijer AH. Hypoxia inducible factor signaling modulates susceptibility to mycobacterial infection via a nitric oxide dependent mechanism. PLoS Pathog. 2013;9:e1003789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 101] [Cited by in RCA: 110] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 16. | Thi EP, Hong CJ, Sanghera G, Reiner NE. Identification of the Mycobacterium tuberculosis protein PE-PGRS62 as a novel effector that functions to block phagosome maturation and inhibit iNOS expression. Cell Microbiol. 2013;15:795-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 17. | Kuang Z, Lewis RS, Curtis JM, Zhan Y, Saunders BM, Babon JJ, Kolesnik TB, Low A, Masters SL, Willson TA. The SPRY domain-containing SOCS box protein SPSB2 targets iNOS for proteasomal degradation. J Cell Biol. 2010;190:129-141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 89] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 18. | Ghafourifar P, Richter C. Nitric oxide synthase activity in mitochondria. FEBS Lett. 1997;418:291-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 430] [Cited by in RCA: 403] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 19. | Tatoyan A, Giulivi C. Purification and characterization of a nitric-oxide synthase from rat liver mitochondria. J Biol Chem. 1998;273:11044-11048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 241] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 20. | Parihar A, Parihar MS, Ghafourifar P. Significance of mitochondrial calcium and nitric oxide for apoptosis of human breast cancer cells induced by tamoxifen and etoposide. Int J Mol Med. 2008;21:317-324. [PubMed] |
| 21. | Nazarewicz RR, Zenebe WJ, Parihar A, Larson SK, Alidema E, Choi J, Ghafourifar P. Tamoxifen induces oxidative stress and mitochondrial apoptosis via stimulating mitochondrial nitric oxide synthase. Cancer Res. 2007;67:1282-1290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 121] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 22. | Zweier JL, Wang P, Samouilov A, Kuppusamy P. Enzyme-independent formation of nitric oxide in biological tissues. Nat Med. 1995;1:804-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 622] [Cited by in RCA: 586] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 23. | Feelisch M, Fernandez BO, Bryan NS, Garcia-Saura MF, Bauer S, Whitlock DR, Ford PC, Janero DR, Rodriguez J, Ashrafian H. Tissue processing of nitrite in hypoxia: an intricate interplay of nitric oxide-generating and -scavenging systems. J Biol Chem. 2008;283:33927-33934. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 191] [Cited by in RCA: 175] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 24. | Madigan M, Zuckerbraun B. Therapeutic Potential of the Nitrite-Generated NO Pathway in Vascular Dysfunction. Front Immunol. 2013;4:174. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 25. | Swirski FK, Libby P, Aikawa E, Alcaide P, Luscinskas FW, Weissleder R, Pittet MJ. Ly-6Chi monocytes dominate hypercholesterolemia-associated monocytosis and give rise to macrophages in atheromata. J Clin Invest. 2007;117:195-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 944] [Cited by in RCA: 1032] [Article Influence: 54.3] [Reference Citation Analysis (0)] |
| 26. | Kossmann S, Hu H, Steven S, Schönfelder T, Fraccarollo D, Mikhed Y, Brähler M, Knorr M, Brandt M, Karbach SH. Inflammatory monocytes determine endothelial nitric-oxide synthase uncoupling and nitro-oxidative stress induced by angiotensin II. J Biol Chem. 2014;289:27540-27550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 104] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 27. | Li H, Horke S, Förstermann U. Vascular oxidative stress, nitric oxide and atherosclerosis. Atherosclerosis. 2014;237:208-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 412] [Cited by in RCA: 490] [Article Influence: 40.8] [Reference Citation Analysis (0)] |
| 28. | Kowluru RA, Kanwar M, Kennedy A. Metabolic memory phenomenon and accumulation of peroxynitrite in retinal capillaries. Exp Diabetes Res. 2007;2007:21976. [PubMed] |
| 29. | Kolios G, Valatas V, Ward SG. Nitric oxide in inflammatory bowel disease: a universal messenger in an unsolved puzzle. Immunology. 2004;113:427-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 358] [Cited by in RCA: 413] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 30. | Ryan BJ, Nissim A, Winyard PG. Oxidative post-translational modifications and their involvement in the pathogenesis of autoimmune diseases. Redox Biol. 2014;2:715-724. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 89] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 31. | Pacher P, Beckman JS, Liaudet L. Nitric oxide and peroxynitrite in health and disease. Physiol Rev. 2007;87:315-424. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4983] [Cited by in RCA: 4569] [Article Influence: 240.5] [Reference Citation Analysis (0)] |
| 32. | Szabó C, Ischiropoulos H, Radi R. Peroxynitrite: biochemistry, pathophysiology and development of therapeutics. Nat Rev Drug Discov. 2007;6:662-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1428] [Cited by in RCA: 1753] [Article Influence: 92.3] [Reference Citation Analysis (0)] |
| 33. | Vitner EB, Farfel-Becker T, Eilam R, Biton I, Futerman AH. Contribution of brain inflammation to neuronal cell death in neuronopathic forms of Gaucher‘s disease. Brain. 2012;135:1724-1735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 130] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 34. | Shu L, Vivekanandan-Giri A, Pennathur S, Smid BE, Aerts JM, Hollak CE, Shayman JA. Establishing 3-nitrotyrosine as a biomarker for the vasculopathy of Fabry disease. Kidney Int. 2014;86:58-66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 76] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 35. | Maturu P, Overwijk WW, Hicks J, Ekmekcioglu S, Grimm EA, Huff V. Characterization of the inflammatory microenvironment and identification of potential therapeutic targets in wilms tumors. Transl Oncol. 2014;7:484-492. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 36. | Aulak KS, Miyagi M, Yan L, West KA, Massillon D, Crabb JW, Stuehr DJ. Proteomic method identifies proteins nitrated in vivo during inflammatory challenge. Proc Natl Acad Sci USA. 2001;98:12056-12061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 292] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 37. | Beckman JS. Oxidative damage and tyrosine nitration from peroxynitrite. Chem Res Toxicol. 1996;9:836-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 776] [Cited by in RCA: 752] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 38. | Eiserich JP, Hristova M, Cross CE, Jones AD, Freeman BA, Halliwell B, van der Vliet A. Formation of nitric oxide-derived inflammatory oxidants by myeloperoxidase in neutrophils. Nature. 1998;391:393-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1198] [Cited by in RCA: 1162] [Article Influence: 41.5] [Reference Citation Analysis (0)] |
| 39. | Wagner AH, Hildebrandt A, Baumgarten S, Jungmann A, Müller OJ, Sharov VS, Schöneich C, Hecker M. Tyrosine nitration limits stretch-induced CD40 expression and disconnects CD40 signaling in human endothelial cells. Blood. 2011;118:3734-3742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 40. | Danielson SR, Held JM, Schilling B, Oo M, Gibson BW, Andersen JK. Preferentially increased nitration of alpha-synuclein at tyrosine-39 in a cellular oxidative model of Parkinson‘s disease. Anal Chem. 2009;81:7823-7828. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 107] [Cited by in RCA: 100] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 41. | Osoata GO, Yamamura S, Ito M, Vuppusetty C, Adcock IM, Barnes PJ, Ito K. Nitration of distinct tyrosine residues causes inactivation of histone deacetylase 2. Biochem Biophys Res Commun. 2009;384:366-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 116] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 42. | Nagaraj S, Gupta K, Pisarev V, Kinarsky L, Sherman S, Kang L, Herber DL, Schneck J, Gabrilovich DI. Altered recognition of antigen is a mechanism of CD8+ T cell tolerance in cancer. Nat Med. 2007;13:828-835. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 940] [Cited by in RCA: 913] [Article Influence: 48.1] [Reference Citation Analysis (0)] |
| 43. | Abello N, Kerstjens HA, Postma DS, Bischoff R. Protein tyrosine nitration: selectivity, physicochemical and biological consequences, denitration, and proteomics methods for the identification of tyrosine-nitrated proteins. J Proteome Res. 2009;8:3222-3238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 274] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 44. | Yamakura F, Matsumoto T, Fujimura T, Taka H, Murayama K, Imai T, Uchida K. Modification of a single tryptophan residue in human Cu,Zn-superoxide dismutase by peroxynitrite in the presence of bicarbonate. Biochim Biophys Acta. 2001;1548:38-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 56] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 45. | Ikeda K, Yukihiro Hiraoka B, Iwai H, Matsumoto T, Mineki R, Taka H, Takamori K, Ogawa H, Yamakura F. Detection of 6-nitrotryptophan in proteins by Western blot analysis and its application for peroxynitrite-treated PC12 cells. Nitric Oxide. 2007;16:18-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 34] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 46. | Redondo-Horcajo M, Romero N, Martínez-Acedo P, Martínez-Ruiz A, Quijano C, Lourenço CF, Movilla N, Enríquez JA, Rodríguez-Pascual F, Rial E. Cyclosporine A-induced nitration of tyrosine 34 MnSOD in endothelial cells: role of mitochondrial superoxide. Cardiovasc Res. 2010;87:356-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 47. | Tedeschi G, Cappelletti G, Nonnis S, Taverna F, Negri A, Ronchi C, Ronchi S. Tyrosine nitration is a novel post-translational modification occurring on the neural intermediate filament protein peripherin. Neurochem Res. 2007;32:433-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 48. | Llovera M, Pearson JD, Moreno C, Riveros-Moreno V. Impaired response to interferon-gamma in activated macrophages due to tyrosine nitration of STAT1 by endogenous nitric oxide. Br J Pharmacol. 2001;132:419-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 49. | Chakravortty D, Hansen-Wester I, Hensel M. Salmonella pathogenicity island 2 mediates protection of intracellular Salmonella from reactive nitrogen intermediates. J Exp Med. 2002;195:1155-1166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 286] [Cited by in RCA: 265] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 50. | Davis AS, Vergne I, Master SS, Kyei GB, Chua J, Deretic V. Mechanism of inducible nitric oxide synthase exclusion from mycobacterial phagosomes. PLoS Pathog. 2007;3:e186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 86] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 51. | Bogdan C, Donhauser N, Döring R, Röllinghoff M, Diefenbach A, Rittig MG. Fibroblasts as host cells in latent leishmaniosis. J Exp Med. 2000;191:2121-2130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 159] [Cited by in RCA: 159] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 52. | Olekhnovitch R, Ryffel B, Müller AJ, Bousso P. Collective nitric oxide production provides tissue-wide immunity during Leishmania infection. J Clin Invest. 2014;124:1711-1722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 79] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 53. | MacMicking J, Xie QW, Nathan C. Nitric oxide and macrophage function. Annu Rev Immunol. 1997;15:323-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3127] [Cited by in RCA: 3099] [Article Influence: 106.9] [Reference Citation Analysis (0)] |
| 54. | Farias-Eisner R, Sherman MP, Aeberhard E, Chaudhuri G. Nitric oxide is an important mediator for tumoricidal activity in vivo. Proc Natl Acad Sci USA. 1994;91:9407-9411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 157] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 55. | Nicholson S, Bonecini-Almeida Mda G, Lapa e Silva JR, Nathan C, Xie QW, Mumford R, Weidner JR, Calaycay J, Geng J, Boechat N. Inducible nitric oxide synthase in pulmonary alveolar macrophages from patients with tuberculosis. J Exp Med. 1996;183:2293-2302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 356] [Cited by in RCA: 352] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 56. | Biswas SK, Mantovani A. Macrophage plasticity and interaction with lymphocyte subsets: cancer as a paradigm. Nat Immunol. 2010;11:889-896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2390] [Cited by in RCA: 3011] [Article Influence: 188.2] [Reference Citation Analysis (1)] |
| 57. | Murray PJ, Allen JE, Biswas SK, Fisher EA, Gilroy DW, Goerdt S, Gordon S, Hamilton JA, Ivashkiv LB, Lawrence T. Macrophage activation and polarization: nomenclature and experimental guidelines. Immunity. 2014;41:14-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4289] [Cited by in RCA: 4787] [Article Influence: 398.9] [Reference Citation Analysis (1)] |
| 58. | Mills CD, Kincaid K, Alt JM, Heilman MJ, Hill AM. M-1/M-2 macrophages and the Th1/Th2 paradigm. J Immunol. 2000;164:6166-6173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1965] [Cited by in RCA: 2444] [Article Influence: 94.0] [Reference Citation Analysis (0)] |
| 59. | Sica A, Mantovani A. Macrophage plasticity and polarization: in vivo veritas. J Clin Invest. 2012;122:787-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3696] [Cited by in RCA: 4961] [Article Influence: 354.4] [Reference Citation Analysis (1)] |
| 60. | Gordon S, Martinez FO. Alternative activation of macrophages: mechanism and functions. Immunity. 2010;32:593-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3290] [Cited by in RCA: 3249] [Article Influence: 203.1] [Reference Citation Analysis (0)] |
| 61. | Weiss JM, Ridnour LA, Back T, Hussain SP, He P, Maciag AE, Keefer LK, Murphy WJ, Harris CC, Wink DA. Macrophage-dependent nitric oxide expression regulates tumor cell detachment and metastasis after IL-2/anti-CD40 immunotherapy. J Exp Med. 2010;207:2455-2467. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 78] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 62. | Serafini P, Borrello I, Bronte V. Myeloid suppressor cells in cancer: recruitment, phenotype, properties, and mechanisms of immune suppression. Semin Cancer Biol. 2006;16:53-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 578] [Cited by in RCA: 590] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 63. | Rahat MA, Hemmerlein B. Macrophage-tumor cell interactions regulate the function of nitric oxide. Front Physiol. 2013;4:144. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 78] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 64. | Bronte V, Zanovello P. Regulation of immune responses by L-arginine metabolism. Nat Rev Immunol. 2005;5:641-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1219] [Cited by in RCA: 1389] [Article Influence: 66.1] [Reference Citation Analysis (0)] |
| 65. | Niedbala W, Wei XQ, Campbell C, Thomson D, Komai-Koma M, Liew FY. Nitric oxide preferentially induces type 1 T cell differentiation by selectively up-regulating IL-12 receptor beta 2 expression via cGMP. Proc Natl Acad Sci USA. 2002;99:16186-16191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 113] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 66. | Jianjun Yang R, Lu G, Shen Y, Peng L, Zhu C, Cui M, Wang W, Arnaboldi P, Tang M, Gupta M. T cell-derived inducible nitric oxide synthase switches off Th17 cell differentiation. J Exp Med. 2013;210:1447-1462. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 109] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 67. | Niedbala W, Cai B, Liu H, Pitman N, Chang L, Liew FY. Nitric oxide induces CD4+CD25+ Foxp3 regulatory T cells from CD4+CD25 T cells via p53, IL-2, and OX40. Proc Natl Acad Sci USA. 2007;104:15478-15483. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 128] [Cited by in RCA: 121] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 68. | Jayaraman P, Alfarano MG, Svider PF, Parikh F, Lu G, Kidwai S, Xiong H, Sikora AG. iNOS Expression in CD4+ T Cells Limits Treg Induction by Repressing TGFβ1: Combined iNOS Inhibition and Treg Depletion Unmask Endogenous Antitumor Immunity. Clin Cancer Res. 2014;20:6439-6451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 69. | Giordano D, Draves KE, Li C, Hohl TM, Clark EA. Nitric oxide regulates BAFF expression and T cell-independent antibody responses. J Immunol. 2014;193:1110-1120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 70. | Banchereau J, Steinman RM. Dendritic cells and the control of immunity. Nature. 1998;392:245-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10867] [Cited by in RCA: 10811] [Article Influence: 386.1] [Reference Citation Analysis (0)] |
| 71. | Villadangos JA, Schnorrer P. Intrinsic and cooperative antigen-presenting functions of dendritic-cell subsets in vivo. Nat Rev Immunol. 2007;7:543-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 457] [Cited by in RCA: 497] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 72. | Smith-Garvin JE, Koretzky GA, Jordan MS. T cell activation. Annu Rev Immunol. 2009;27:591-619. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1648] [Cited by in RCA: 1559] [Article Influence: 91.7] [Reference Citation Analysis (7)] |
| 73. | Haring JS, Badovinac VP, Harty JT. Inflaming the CD8+ T cell response. Immunity. 2006;25:19-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 207] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 74. | Fernandez NC, Lozier A, Flament C, Ricciardi-Castagnoli P, Bellet D, Suter M, Perricaudet M, Tursz T, Maraskovsky E, Zitvogel L. Dendritic cells directly trigger NK cell functions: cross-talk relevant in innate anti-tumor immune responses in vivo. Nat Med. 1999;5:405-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 808] [Cited by in RCA: 787] [Article Influence: 29.1] [Reference Citation Analysis (0)] |
| 75. | Lu L, Bonham CA, Chambers FG, Watkins SC, Hoffman RA, Simmons RL, Thomson AW. Induction of nitric oxide synthase in mouse dendritic cells by IFN-gamma, endotoxin, and interaction with allogeneic T cells: nitric oxide production is associated with dendritic cell apoptosis. J Immunol. 1996;157:3577-3586. [PubMed] |
| 76. | Adler HS, Simon A, Graulich E, Habermeier A, Bacher N, Friebe A, Closs EI, Steinbrink K. Neuronal nitric oxide synthase modulates maturation of human dendritic cells. J Immunol. 2010;184:6025-6034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 77. | Eriksson S, Chambers BJ, Rhen M. Nitric oxide produced by murine dendritic cells is cytotoxic for intracellular Salmonella enterica sv. Typhimurium. Scand J Immunol. 2003;58:493-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 78. | Everts B, Amiel E, van der Windt GJ, Freitas TC, Chott R, Yarasheski KE, Pearce EL, Pearce EJ. Commitment to glycolysis sustains survival of NO-producing inflammatory dendritic cells. Blood. 2012;120:1422-1431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 368] [Cited by in RCA: 448] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 79. | Serbina NV, Salazar-Mather TP, Biron CA, Kuziel WA, Pamer EG. TNF/iNOS-producing dendritic cells mediate innate immune defense against bacterial infection. Immunity. 2003;19:59-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 903] [Cited by in RCA: 915] [Article Influence: 39.8] [Reference Citation Analysis (4)] |
| 80. | De Trez C, Magez S, Akira S, Ryffel B, Carlier Y, Muraille E. iNOS-producing inflammatory dendritic cells constitute the major infected cell type during the chronic Leishmania major infection phase of C57BL/6 resistant mice. PLoS Pathog. 2009;5:e1000494. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 141] [Cited by in RCA: 151] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 81. | Aldridge JR, Moseley CE, Boltz DA, Negovetich NJ, Reynolds C, Franks J, Brown SA, Doherty PC, Webster RG, Thomas PG. TNF/iNOS-producing dendritic cells are the necessary evil of lethal influenza virus infection. Proc Natl Acad Sci USA. 2009;106:5306-5311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 354] [Cited by in RCA: 352] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 82. | Trinchieri G. Biology of natural killer cells. Adv Immunol. 1989;47:187-376. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2111] [Cited by in RCA: 2166] [Article Influence: 58.5] [Reference Citation Analysis (0)] |
| 83. | Vivier E, Tomasello E, Baratin M, Walzer T, Ugolini S. Functions of natural killer cells. Nat Immunol. 2008;9:503-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2338] [Cited by in RCA: 2999] [Article Influence: 166.6] [Reference Citation Analysis (0)] |
| 84. | Cifone MG, Ulisse S, Santoni A. Natural killer cells and nitric oxide. Int Immunopharmacol. 2001;1:1513-1524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 45] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 85. | Furuke K, Burd PR, Horvath-Arcidiacono JA, Hori K, Mostowski H, Bloom ET. Human NK cells express endothelial nitric oxide synthase, and nitric oxide protects them from activation-induced cell death by regulating expression of TNF-alpha. J Immunol. 1999;163:1473-1480. [PubMed] |
| 86. | da Silva EZ, Jamur MC, Oliver C. Mast cell function: a new vision of an old cell. J Histochem Cytochem. 2014;62:698-738. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 429] [Cited by in RCA: 444] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 87. | Swindle EJ, Metcalfe DD, Coleman JW. Rodent and human mast cells produce functionally significant intracellular reactive oxygen species but not nitric oxide. J Biol Chem. 2004;279:48751-48759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 88] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 88. | Salvemini D, Masini E, Anggard E, Mannaioni PF, Vane J. Synthesis of a nitric oxide-like factor from L-arginine by rat serosal mast cells: stimulation of guanylate cyclase and inhibition of platelet aggregation. Biochem Biophys Res Commun. 1990;169:596-601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 106] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 89. | Gilchrist M, McCauley SD, Befus AD. Expression, localization, and regulation of NOS in human mast cell lines: effects on leukotriene production. Blood. 2004;104:462-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 77] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 90. | Gilchrist M, Savoie M, Nohara O, Wills FL, Wallace JL, Befus AD. Nitric oxide synthase and nitric oxide production in in vivo-derived mast cells. J Leukoc Biol. 2002;71:618-624. [PubMed] |
| 91. | Salvemini D. Nitric Oxide: A Regulatory Mediator of Mast Cell Reactivity. J Cardiovas Pharma. 1991;17:S264. |
| 92. | Nohara O, Kulka M, Déry RE, Wills FL, Hirji NS, Gilchrist M, Befus AD. Regulation of CD8 expression in mast cells by exogenous or endogenous nitric oxide. J Immunol. 2001;167:5935-5939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 93. | Forsythe P, Befus AD. Inhibition of calpain is a component of nitric oxide-induced down-regulation of human mast cell adhesion. J Immunol. 2003;170:287-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 94. | Hammami I, Chen J, Bronte V, DeCrescenzo G, Jolicoeur M. L-glutamine is a key parameter in the immunosuppression phenomenon. Biochem Biophys Res Commun. 2012;425:724-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 42] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 95. | Gabrilovich DI, Ostrand-Rosenberg S, Bronte V. Coordinated regulation of myeloid cells by tumours. Nat Rev Immunol. 2012;12:253-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2369] [Cited by in RCA: 2952] [Article Influence: 210.9] [Reference Citation Analysis (0)] |
| 96. | Birnboim HC, Lemay AM, Lam DK, Goldstein R, Webb JR. Cutting edge: MHC class II-restricted peptides containing the inflammation-associated marker 3-nitrotyrosine evade central tolerance and elicit a robust cell-mediated immune response. J Immunol. 2003;171:528-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 77] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 97. | Ohmori H, Oka M, Nishikawa Y, Shigemitsu H, Takeuchi M, Magari M, Kanayama N. Immunogenicity of autologous IgG bearing the inflammation-associated marker 3-nitrotyrosine. Immunol Lett. 2005;96:47-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 98. | Hardy LL, Wick DA, Webb JR. Conversion of tyrosine to the inflammation-associated analog 3‘-nitrotyrosine at either TCR- or MHC-contact positions can profoundly affect recognition of the MHC class I-restricted epitope of lymphocytic choriomeningitis virus glycoprotein 33 by CD8 T cells. J Immunol. 2008;180:5956-5962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 99. | Kalluri R, Cantley LG, Kerjaschki D, Neilson EG. Reactive oxygen species expose cryptic epitopes associated with autoimmune goodpasture syndrome. J Biol Chem. 2000;275:20027-20032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 60] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 100. | Binder CJ, Hörkkö S, Dewan A, Chang MK, Kieu EP, Goodyear CS, Shaw PX, Palinski W, Witztum JL, Silverman GJ. Pneumococcal vaccination decreases atherosclerotic lesion formation: molecular mimicry between Streptococcus pneumoniae and oxidized LDL. Nat Med. 2003;9:736-743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 553] [Cited by in RCA: 579] [Article Influence: 25.2] [Reference Citation Analysis (0)] |
| 101. | Habib S, Moinuddin R. Peroxynitrite-modified DNA: a better antigen for systemic lupus erythematosus anti-DNA autoantibodies. Biotechnol Appl Biochem. 2006;43:65-70. [PubMed] |
| 102. | Khan F, Siddiqui AA. Prevalence of anti-3-nitrotyrosine antibodies in the joint synovial fluid of patients with rheumatoid arthritis, osteoarthritis and systemic lupus erythematosus. Clin Chim Acta. 2006;370:100-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 56] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 103. | Khan F, Ali R. Antibodies against nitric oxide damaged poly L-tyrosine and 3-nitrotyrosine levels in systemic lupus erythematosus. J Biochem Mol Biol. 2006;39:189-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 104. | Dixit K, Khan MA, Sharma YD, Moinuddin K. Peroxynitrite-induced modification of H2A histone presents epitopes which are strongly bound by human anti-DNA autoantibodies: role of peroxynitrite-modified-H2A in SLE induction and progression. Hum Immunol. 2011;72:219-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 105. | Ahsan H. 3-Nitrotyrosine: A biomarker of nitrogen free radical species modified proteins in systemic autoimmunogenic conditions. Hum Immunol. 2013;74:1392-1399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 202] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 106. | Gilkeson G, Cannon C, Oates J, Reilly C, Goldman D, Petri M. Correlation of serum measures of nitric oxide production with lupus disease activity. J Rheumatol. 1999;26:318-324. [PubMed] |
| 107. | Oates JC, Christensen EF, Reilly CM, Self SE, Gilkeson GS. Prospective measure of serum 3-nitrotyrosine levels in systemic lupus erythematosus: correlation with disease activity. Proc Assoc Am Physicians. 1999;111:611-621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 60] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 108. | Rochette L, Zeller M, Cottin Y, Vergely C. Diabetes, oxidative stress and therapeutic strategies. Biochim Biophys Acta. 2014;1840:2709-2729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 302] [Cited by in RCA: 360] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 109. | Giacco F, Brownlee M. Oxidative stress and diabetic complications. Circ Res. 2010;107:1058-1070. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3956] [Cited by in RCA: 3767] [Article Influence: 235.4] [Reference Citation Analysis (11)] |
| 110. | Jay D, Hitomi H, Griendling KK. Oxidative stress and diabetic cardiovascular complications. Free Radic Biol Med. 2006;40:183-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 315] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 111. | Szabó C, Zanchi A, Komjáti K, Pacher P, Krolewski AS, Quist WC, LoGerfo FW, Horton ES, Veves A. Poly(ADP-Ribose) polymerase is activated in subjects at risk of developing type 2 diabetes and is associated with impaired vascular reactivity. Circulation. 2002;106:2680-2686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 139] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 112. | Hoeldtke RD, Bryner KD, McNeill DR, Hobbs GR, Baylis C. Peroxynitrite versus nitric oxide in early diabetes. Am J Hypertens. 2003;16:761-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 113. | Stadler K. Peroxynitrite-driven mechanisms in diabetes and insulin resistance - the latest advances. Curr Med Chem. 2011;18:280-290. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 114. | Ihnat MA, Thorpe JE, Ceriello A. Hypothesis: the ‘metabolic memory’, the new challenge of diabetes. Diabet Med. 2007;24:582-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 122] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 115. | Wang Y, Feng W, Xue W, Tan Y, Hein DW, Li XK, Cai L. Inactivation of GSK-3beta by metallothionein prevents diabetes-related changes in cardiac energy metabolism, inflammation, nitrosative damage, and remodeling. Diabetes. 2009;58:1391-1402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 142] [Cited by in RCA: 141] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 116. | Cong W, Zhao T, Zhu Z, Huang B, Ma W, Wang Y, Tan Y, Chakrabarti S, Li X, Jin L. Metallothionein prevents cardiac pathological changes in diabetes by modulating nitration and inactivation of cardiac ATP synthase. J Nutr Biochem. 2014;25:463-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 117. | He X, Kan H, Cai L, Ma Q. Nrf2 is critical in defense against high glucose-induced oxidative damage in cardiomyocytes. J Mol Cell Cardiol. 2009;46:47-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 209] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 118. | Li B, Liu S, Miao L, Cai L. Prevention of diabetic complications by activation of Nrf2: diabetic cardiomyopathy and nephropathy. Exp Diabetes Res. 2012;2012:216512. [PubMed] |
| 119. | Stavniichuk R, Shevalye H, Lupachyk S, Obrosov A, Groves JT, Obrosova IG, Yorek MA. Peroxynitrite and protein nitration in the pathogenesis of diabetic peripheral neuropathy. Diabetes Metab Res Rev. 2014;30:669-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 61] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 120. | Obrosova IG, Mabley JG, Zsengellér Z, Charniauskaya T, Abatan OI, Groves JT, Szabó C. Role for nitrosative stress in diabetic neuropathy: evidence from studies with a peroxynitrite decomposition catalyst. FASEB J. 2005;19:401-403. [PubMed] |
| 121. | Yorek MA. The role of oxidative stress in diabetic vascular and neural disease. Free Radic Res. 2003;37:471-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 141] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 122. | Drel VR, Mashtalir N, Ilnytska O, Shin J, Li F, Lyzogubov VV, Obrosova IG. The leptin-deficient (ob/ob) mouse: a new animal model of peripheral neuropathy of type 2 diabetes and obesity. Diabetes. 2006;55:3335-3343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 198] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 123. | Zettl UK, Mix E, Zielasek J, Stangel M, Hartung HP, Gold R. Apoptosis of myelin-reactive T cells induced by reactive oxygen and nitrogen intermediates in vitro. Cell Immunol. 1997;178:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 62] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 124. | Mitrovic B, Ignarro LJ, Vinters HV, Akers MA, Schmid I, Uittenbogaart C, Merrill JE. Nitric oxide induces necrotic but not apoptotic cell death in oligodendrocytes. Neuroscience. 1995;65:531-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 143] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 125. | Cross AH, Manning PT, Stern MK, Misko TP. Evidence for the production of peroxynitrite in inflammatory CNS demyelination. J Neuroimmunol. 1997;80:121-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 133] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 126. | Smith KJ, Lassmann H. The role of nitric oxide in multiple sclerosis. Lancet Neurol. 2002;1:232-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 384] [Cited by in RCA: 380] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 127. | Maeda H, Okamoto T, Akaike T. Human matrix metalloprotease activation by insults of bacterial infection involving proteases and free radicals. Biol Chem. 1998;379:193-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 65] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 128. | Redford EJ, Kapoor R, Smith KJ. Nitric oxide donors reversibly block axonal conduction: demyelinated axons are especially susceptible. Brain. 1997;120:2149-2157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 215] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 129. | Aboul-Enein F, Weiser P, Höftberger R, Lassmann H, Bradl M. Transient axonal injury in the absence of demyelination: a correlate of clinical disease in acute experimental autoimmune encephalomyelitis. Acta Neuropathol. 2006;111:539-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 60] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 130. | Petković F, Blaževski J, Momčilović M, Mostarica Stojkovic M, Miljković D. Nitric oxide inhibits CXCL12 expression in neuroinflammation. Immunol Cell Biol. 2013;91:427-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 131. | Boughton-Smith NK. Pathological and therapeutic implications for nitric oxide in inflammatory bowel disease. J R Soc Med. 1994;87:312-314. [PubMed] |
| 132. | Middleton SJ, Shorthouse M, Hunter JO. Increased nitric oxide synthesis in ulcerative colitis. Lancet. 1993;341:465-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 235] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 133. | Ribbons KA, Zhang XJ, Thompson JH, Greenberg SS, Moore WM, Kornmeier CM, Currie MG, Lerche N, Blanchard J, Clark DA. Potential role of nitric oxide in a model of chronic colitis in rhesus macaques. Gastroenterology. 1995;108:705-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 67] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 134. | Middleton SJ, Shorthouse M, Hunter JO. Relaxation of distal colonic circular smooth muscle by nitric oxide derived from human leucocytes. Gut. 1993;34:814-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 135. | Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001;357:539-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5245] [Cited by in RCA: 5852] [Article Influence: 234.1] [Reference Citation Analysis (1)] |
| 136. | Sica A, Porta C, Morlacchi S, Banfi S, Strauss L, Rimoldi M, Totaro MG, Riboldi E. Origin and Functions of Tumor-Associated Myeloid Cells (TAMCs). Cancer Microenviron. 2012;5:133-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 83] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 137. | Porta C, Riboldi E, Sica A. Mechanisms linking pathogens-associated inflammation and cancer. Cancer Lett. 2011;305:250-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 83] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 138. | Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51728] [Cited by in RCA: 48749] [Article Influence: 3249.9] [Reference Citation Analysis (12)] |
| 139. | Hanahan D, Coussens LM. Accessories to the crime: functions of cells recruited to the tumor microenvironment. Cancer Cell. 2012;21:309-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2921] [Cited by in RCA: 3459] [Article Influence: 247.1] [Reference Citation Analysis (0)] |
| 140. | Sica A, Bronte V. Altered macrophage differentiation and immune dysfunction in tumor development. J Clin Invest. 2007;117:1155-1166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 898] [Cited by in RCA: 974] [Article Influence: 51.3] [Reference Citation Analysis (4)] |
| 141. | Solinas G, Germano G, Mantovani A, Allavena P. Tumor-associated macrophages (TAM) as major players of the cancer-related inflammation. J Leukoc Biol. 2009;86:1065-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 960] [Cited by in RCA: 1031] [Article Influence: 60.6] [Reference Citation Analysis (0)] |
| 142. | Molon B, Ugel S, Del Pozzo F, Soldani C, Zilio S, Avella D, De Palma A, Mauri P, Monegal A, Rescigno M. Chemokine nitration prevents intratumoral infiltration of antigen-specific T cells. J Exp Med. 2011;208:1949-1962. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 443] [Cited by in RCA: 534] [Article Influence: 35.6] [Reference Citation Analysis (0)] |
| 143. | Thomsen LL, Miles DW, Happerfield L, Bobrow LG, Knowles RG, Moncada S. Nitric oxide synthase activity in human breast cancer. Br J Cancer. 1995;72:41-44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 453] [Cited by in RCA: 434] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 144. | Reveneau S, Arnould L, Jolimoy G, Hilpert S, Lejeune P, Saint-Giorgio V, Belichard C, Jeannin JF. Nitric oxide synthase in human breast cancer is associated with tumor grade, proliferation rate, and expression of progesterone receptors. Lab Invest. 1999;79:1215-1225. [PubMed] |
| 145. | Zhang Y, He N, Zhou J, Chen Y. The relationship between MRI invasive features and expression of EMMPRIN, galectin-3, and microvessel density in pituitary adenoma. Clin Imaging. 2011;35:165-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 146. | Fukumura D, Kashiwagi S, Jain RK. The role of nitric oxide in tumour progression. Nat Rev Cancer. 2006;6:521-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 923] [Cited by in RCA: 975] [Article Influence: 48.8] [Reference Citation Analysis (0)] |
| 147. | Weigert A, Brüne B. Nitric oxide, apoptosis and macrophage polarization during tumor progression. Nitric Oxide. 2008;19:95-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 115] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 148. | Jeannin JF, Leon L, Cortier M, Sassi N, Paul C, Bettaieb A. Nitric oxide-induced resistance or sensitization to death in tumor cells. Nitric Oxide. 2008;19:158-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 149. | Leon L, Jeannin JF, Bettaieb A. Post-translational modifications induced by nitric oxide (NO): implication in cancer cells apoptosis. Nitric Oxide. 2008;19:77-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 68] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 150. | Lechner M, Lirk P, Rieder J. Inducible nitric oxide synthase (iNOS) in tumor biology: the two sides of the same coin. Semin Cancer Biol. 2005;15:277-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 289] [Cited by in RCA: 304] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 151. | Jones LE, Ying L, Hofseth AB, Jelezcova E, Sobol RW, Ambs S, Harris CC, Espey MG, Hofseth LJ, Wyatt MD. Differential effects of reactive nitrogen species on DNA base excision repair initiated by the alkyladenine DNA glycosylase. Carcinogenesis. 2009;30:2123-2129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 152. | Norbury CJ, Zhivotovsky B. DNA damage-induced apoptosis. Oncogene. 2004;23:2797-2808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 485] [Cited by in RCA: 523] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 153. | Dimmeler S, Haendeler J, Nehls M, Zeiher AM. Suppression of apoptosis by nitric oxide via inhibition of interleukin-1beta-converting enzyme (ICE)-like and cysteine protease protein (CPP)-32-like proteases. J Exp Med. 1997;185:601-607. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 671] [Cited by in RCA: 656] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 154. | Török NJ, Higuchi H, Bronk S, Gores GJ. Nitric oxide inhibits apoptosis downstream of cytochrome C release by nitrosylating caspase 9. Cancer Res. 2002;62:1648-1653. [PubMed] |
| 155. | Muntané J, De la Rosa AJ, Marín LM, Padillo FJ. Nitric oxide and cell death in liver cancer cells. Mitochondrion. 2013;13:257-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 156. | Chao JI, Kuo PC. Role of p53 and p38 MAP kinase in nitric oxide-induced G2/M arrest and apoptosis in the human lung carcinoma cells. Carcinogenesis. 2004;25:645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 157. | Garbán HJ, Bonavida B. Nitric oxide inhibits the transcription repressor Yin-Yang 1 binding activity at the silencer region of the Fas promoter: a pivotal role for nitric oxide in the up-regulation of Fas gene expression in human tumor cells. J Immunol. 2001;167:75-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 107] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 158. | Lahdenranta J, Hagendoorn J, Padera TP, Hoshida T, Nelson G, Kashiwagi S, Jain RK, Fukumura D. Endothelial nitric oxide synthase mediates lymphangiogenesis and lymphatic metastasis. Cancer Res. 2009;69:2801-2808. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 124] [Cited by in RCA: 118] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 159. | Massi D, De Nisi MC, Franchi A, Mourmouras V, Baroni G, Panelos J, Santucci M, Miracco C. Inducible nitric oxide synthase expression in melanoma: implications in lymphangiogenesis. Mod Pathol. 2009;22:21-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 160. | Franchi A, Massi D, Santucci M, Masini E, Rossi Degl’Innocenti D, Magnelli L, Fanti E, Naldini A, Ardinghi C, Carraro F. Inducible nitric oxide synthase activity correlates with lymphangiogenesis and vascular endothelial growth factor-C expression in head and neck squamous cell carcinoma. J Pathol. 2006;208:439-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 161. | Mehta P. Potential role of platelets in the pathogenesis of tumor metastasis. Blood. 1984;63:55-63. [PubMed] |
| 162. | Bingisser RM, Tilbrook PA, Holt PG, Kees UR. Macrophage-derived nitric oxide regulates T cell activation via reversible disruption of the Jak3/STAT5 signaling pathway. J Immunol. 1998;160:5729-5734. [PubMed] |
| 163. | Macphail SE, Gibney CA, Brooks BM, Booth CG, Flanagan BF, Coleman JW. Nitric oxide regulation of human peripheral blood mononuclear cells: critical time dependence and selectivity for cytokine versus chemokine expression. J Immunol. 2003;171:4809-4815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 42] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 164. | Dave B, Granados-Principal S, Zhu R, Benz S, Rabizadeh S, Soon-Shiong P, Yu KD, Shao Z, Li X, Gilcrease M. Targeting RPL39 and MLF2 reduces tumor initiation and metastasis in breast cancer by inhibiting nitric oxide synthase signaling. Proc Natl Acad Sci USA. 2014;111:8838-8843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 98] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 165. | Godoy LC, Anderson CT, Chowdhury R, Trudel LJ, Wogan GN. Endogenously produced nitric oxide mitigates sensitivity of melanoma cells to cisplatin. Proc Natl Acad Sci USA. 2012;109:20373-20378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 166. | Lampson BL, Kendall SD, Ancrile BB, Morrison MM, Shealy MJ, Barrientos KS, Crowe MS, Kashatus DF, White RR, Gurley SB. Targeting eNOS in pancreatic cancer. Cancer Res. 2012;72:4472-4482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 54] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 167. | Cali B, Ceolin S, Ceriani F, Bortolozzi M, Agnellini AH, Zorzi V, Predonzani A, Bronte V, Molon B, Mammano F. Critical role of gap junction communication, calcium and nitric oxide signaling in bystander responses to focal photodynamic injury. Oncotarget. 2015;Mar 12; Epub ahead of print. [PubMed] |
P- Reviewer: Wu S S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/