Published online Sep 9, 2025. doi: 10.5492/wjccm.v14.i3.107513
Revised: April 6, 2025
Accepted: May 21, 2025
Published online: September 9, 2025
Processing time: 115 Days and 20.2 Hours
The Jahi McMath case represents a pivotal moment in the reevaluation of brain death or death by neurological criteria (BD/DNC) and disorders of consciousness. Declared brain dead on December 12, 2013, following surgical complications, Jahi’s case became a landmark in challenging conventional BD/DNC definitions. As an independent consultant for the International Brain Research Foundation, I recommended advanced ancillary tests, including neuroimaging, electrophysiological, and heart rate variability assessments, conducted at Rutgers University Hospital and Jahi’s apartment in New Jersey. My analyses revealed unprecedented findings: Significant preservation of intracranial structures, including the upper brainstem, despite extensive white matter damage and partial herniation. I identified residual cognitive processing and autonomic responses, which suggested a novel disorder of consciousness distinct from both BD/DNC, the unresponsive unawareness syndrome, the minimally conscious state, and the locked-in syndrome. These insights, reinforced by complementary evaluations by Dr. Alan Shewmon, who later documented Jahi’s purposeful responses to com
Core Tip: This study provides groundbreaking insights into the case of Jahi McMath, identifying a novel disorder of con
- Citation: Machado C. Jahi McMath case: A comprehensive and updated narrative. World J Crit Care Med 2025; 14(3): 107513
- URL: https://www.wjgnet.com/2220-3141/full/v14/i3/107513.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v14.i3.107513
On December 12, 2013, Jahi McMath was declared brain dead following a severe hemorrhagic complication during surgery. However, her family’s refusal to accept the diagnosis led to a legal and medical odyssey that challenged conventional definitions of brain death or death by neurological criteria (BD/DNC). At the center of this controversial case, the International Brain Research Foundation invited me as an independent consultant to provide expert insight into Jahi’s condition[1-7].
I emphasized that United States BD/DNC guidelines recommend ancillary tests when clinical examination findings are uncertain or inconclusive[8]. Due to the case's legal complexities, I recommended advanced electrophysiologic tests and neuroimaging. These assessments were conducted at Rutgers University Hospital (RUH) in Newark, New Jersey, and at Jahi’s apartment in New Jersey. I analyzed the magnetic resonance (MR) imaging (MRI), MR-angiogram, MR-venogram, electroencephalography (EEG), and heart rate variability (HRV) studies, including follow-up EEGs recorded at her apartment in New Jersey.
My evaluations provided unprecedented insights into Jahi’s condition, ultimately reshaping the discourse on BD/DNC and disorders of consciousness. My findings not only contradicted the initial diagnosis but also suggested the presence of a novel disorder of consciousness that had never been described in medical literature[9-14].
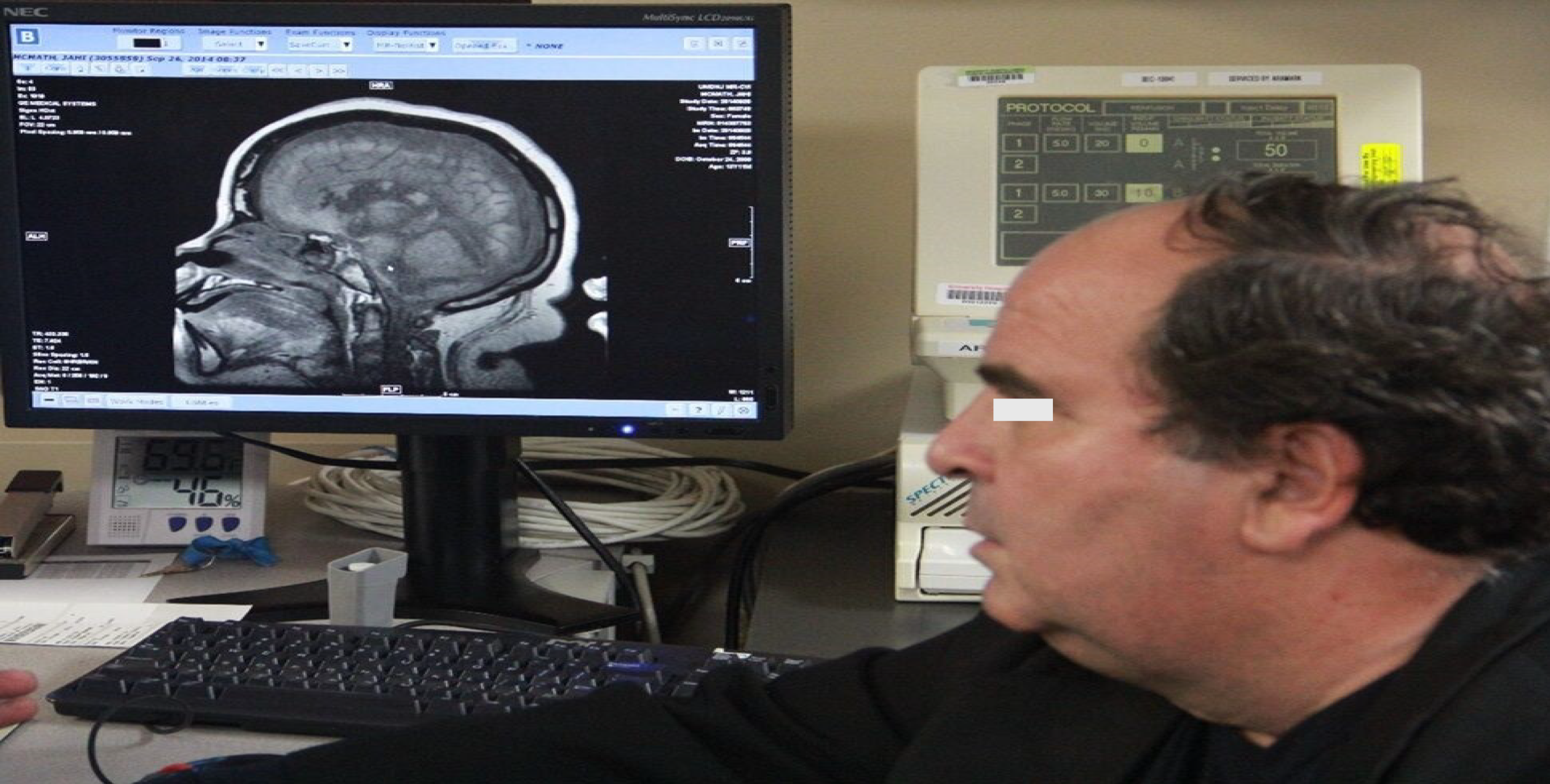
One pivotal moment occurred on September 26, 2014, when Jahi underwent comprehensive evaluations under my supervision at RUH. Dr. Charles Prestigiacomo, a respected neurosurgeon, guided Jahi’s MRI studies. He kindly allowed the MRI to be performed using the sequences and slices I recommended. Although the MR-angiogram and MR-venogram were completed, I requested a computed tomography angiography (CTA) for further clarity. However, this test was not approved due to time constraints and Jahi’s lack of formal admission.
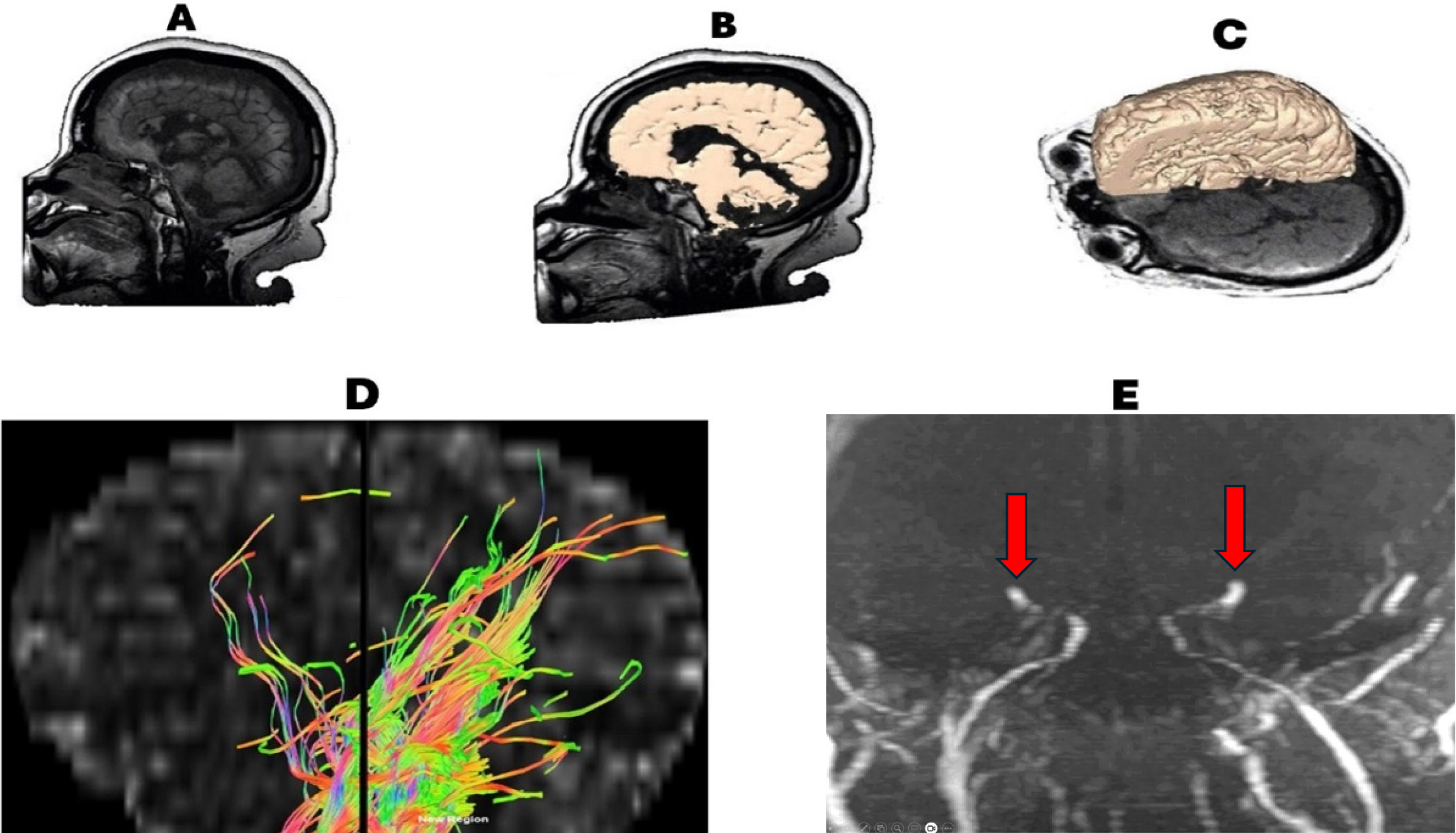
When I reviewed the first MRI image, I was stunned to see significant preservation of intracranial structures. I had anticipated findings consistent with a "respirator brain", such as diffuse brain swelling, chaotic tissue, or liquefaction necrosis. Instead, the MRI revealed astonishing superficial and internal anatomical preservation with minimal cortical atrophy. Despite notable abnormalities observed nine and a half months after Jahi’s cardiac arrest—including massive demyelination in the white matter, abnormal cortical ribbon signals, and cystic degeneration in the corpus callosum—the scans showed remarkable preservation of the upper brainstem. I later created 3D reconstructions, which demonstrated the integrity of the upper brainstem despite a lytic lesion in the lower half (Figure 1)[12,14].
Dr. Alan Shewmon later confirmed similar findings after analyzing the MRI studies performed at RUH on September 26, 2014, highlighting the preservation of the cortex, basal ganglia, thalamus, and upper brainstem. These findings suggested that the preserved upper brainstem and thalamus might explain Jahi’s intermittent awareness despite severe motor disabilities and absent brainstem reflexes[3,5].
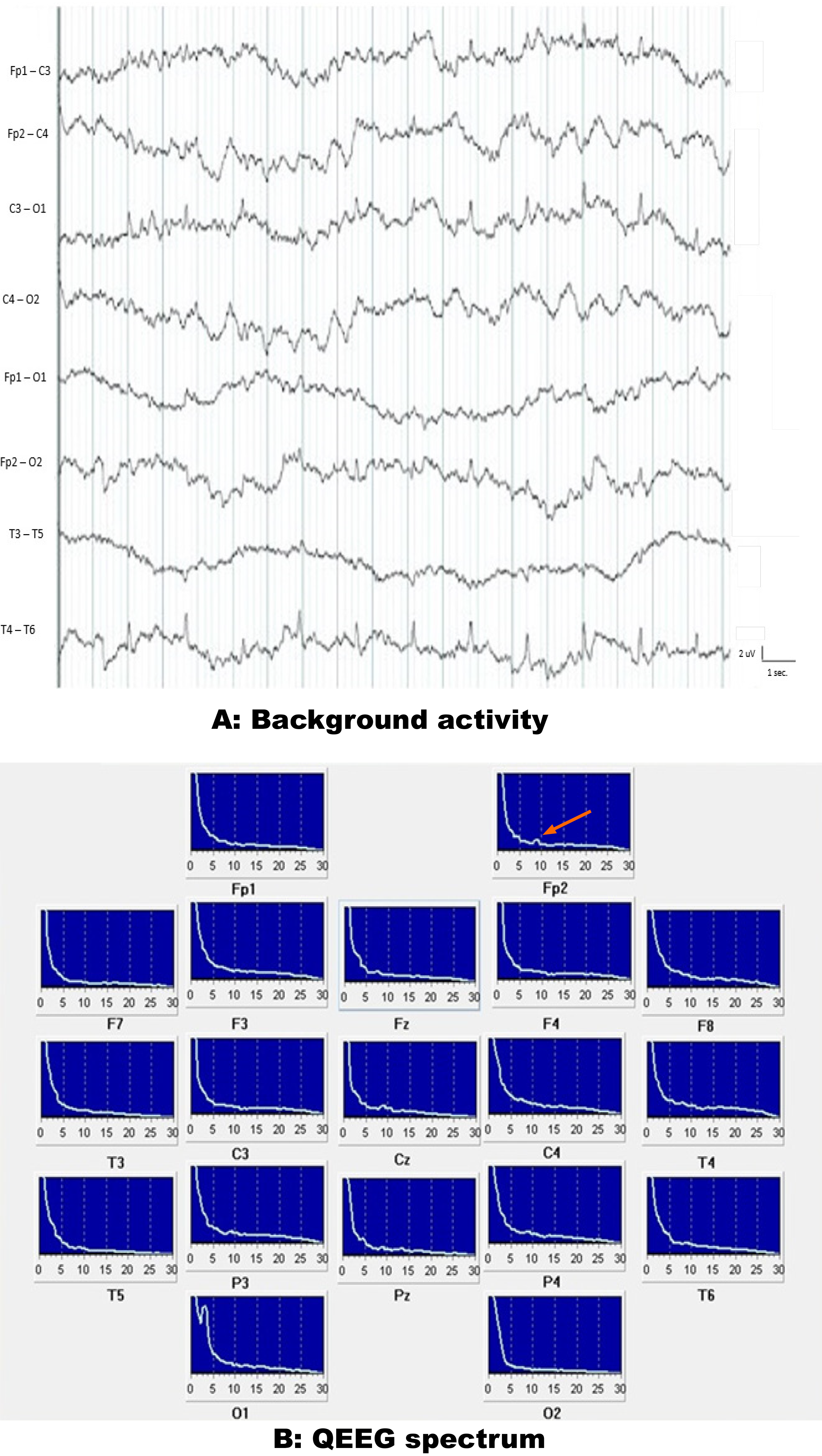
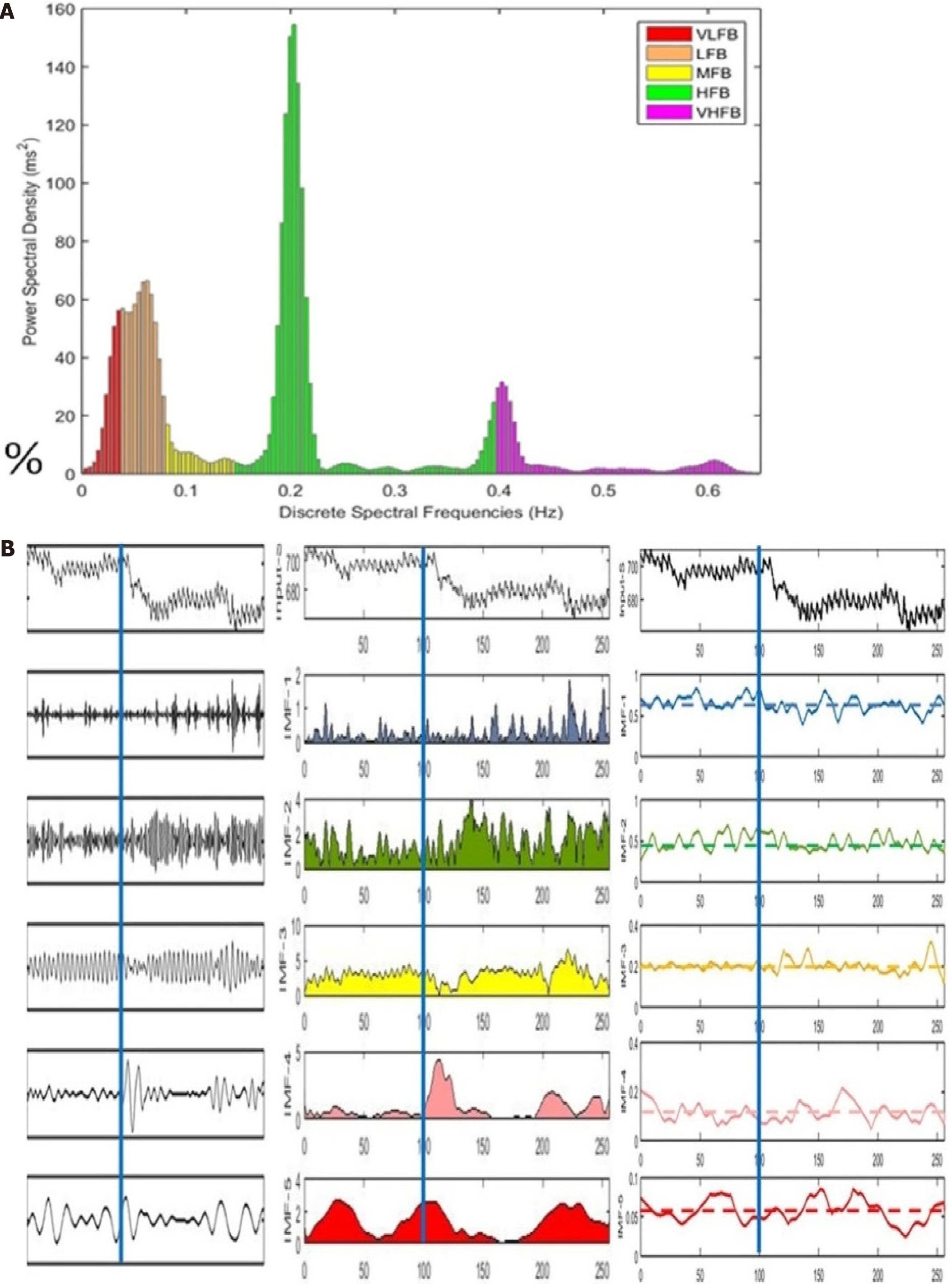
Since early 2014, Jahi’s mother, Nailah Winkfield, reported that Jahi responded to simple commands. Nailah observed that when Jahi’s heart rate exceeded 80, she was more likely to respond, possibly reflecting fluctuating arousal levels[5]. These episodes occurred approximately five times per week and lasted several minutes. During my four-week stay in New Jersey in September 2014, I observed these responses and recorded EEG and ECG data before and after commands. Nailah provided written consent for me to publish Jahi’s data. The EEG results confirmed disorganized cortical activity, ruling out electrocerebral inactivity. Spectral analysis revealed delta-theta activity with noted inter-hemispheric asymmetries. HRV analysis further demonstrated preserved autonomic responses to auditory stimuli, especially to her mother’s voice. These findings were inconsistent with BD/DNC and indicated residual cognitive processing and autonomic integration (Figures 2, 3, and 4).
After returning from New Jersey in late September 2014, I processed all the data and completed my paper by year’s end. However, my manuscript was rejected by over ten prominent neurological journals in the U.S. and Europe. Ultimately, I published my findings in Functional Neurology, Rehabilitation, and Ergonomics in 2016[14]. While this journal had a lower impact factor, my paper was the first to present detailed anatomical and functional findings from Jahi’s brain. Unfortunately, the paper’s limited reach left the broader scientific community unaware of my results. I proposed that Jahi’s condition represented a new state of consciousness distinct from BD/DNC, the unresponsive unawareness syndrome, the minimally conscious state, and the locked-in syndrome[10].
At the meeting celebrating “The 50th Anniversary of the Harvard Criteria for Brain Death”, Dr. Robert Truog organized a special session titled “Brain Death and the Controversial Case of Jahi McMath”[6,7]. While I was not included in the program, Dr. Shewmon presented a lecture discussing Jahi’s anatomic and functional brain findings. I sent a PDF of my pioneering paper[14] to Shewmon before the meeting, and he gently included a slide of my publication in his lecture in Boston. I also distributed reprints during that special session about Jahi in Boston in 2018.
During the “VIII International Symposium on Brain Death and Disorders of Consciousness”, held in Havana from December 4-7, 2018, I presented a lecture titled "Vegetative State (PVS-UWS), Minimally Conscious State, Brain Death, or a New State of Disorder of Consciousness?" in which I summarized my findings on Jahi. At the same conference, I organized a round table discussion, “Jahi McMath and Other Controversial Brain-Death Cases”, featuring prominent leaders in the field (Figure 5).
Dr. Alan Shewmon, who independently evaluated Jahi’s condition after my assessments, analyzed videos provided by Nailah Winkfield. He concluded that Jahi’s movements were purposeful and anatomically related to commands, indicating preserved cortical activity[3-5,15]. My findings on autonomic reactivity aligned with his observations, reinforcing the evidence that Jahi’s condition transcended existing classifications of disorders of consciousness[10].
I received written consent from Nailah Winkfield, Jahi McMath’s mother, to publish my results. The IRB of the Institute of Neurology and Neurosurgery, Havana, Cuba, approved this paper.
The Jahi McMath case underscores my pivotal role in challenging the boundaries of BD/DNC and advancing our understanding of consciousness. My meticulous evaluations and innovative use of diagnostics contributed to the recognition of a new disorder of consciousness. I consider that this manuscript presents a compelling, detailed, and pioneering account of the Jahi McMath case, which has been a focal point in the discourse on brain death and disorders of consciousness.
My findings challenge conventional definitions of brain death by neurological criteria (BD/DNC) and propose a novel disorder of consciousness. Advanced diagnostic tools, including neuroimaging and electrophysiological assessments, provide unprecedented insights into Jahi's condition. Identifying preserved intracranial structures, residual cognitive processing, and autonomic responses is groundbreaking and has significant implications for the field.
The manuscript's contribution to literature is significant, as it offers a new perception of consciousness disorders and underscores the need for advanced diagnostics and multidisciplinary collaboration. My methodological approach is rigorous and well-documented. 3D reconstructions, EEG analysis, and HRV analysis comprehensively evaluate Jahi's brain function. Including figures and detailed descriptions of the findings enhances the manuscript's clarity and credibility.
This case would have needed a CTA, which was not approved due to time constraints and Jahi's lack of formal admission. Nonetheless, the finding of intracranial structures after more than 9 months of the initial diagnosis of BD/DNC indicates the preservation of intracranial cerebral blood flow.
The Jahi McMath case has significant implications for the medical and legal communities, particularly in defining and diagnosing BD/DNC and studying disorders of consciousness. The novel disorder of consciousness might be integrated into existing diagnostic criteria and treatment protocols for BD/DNC and in classifying disorders of consciousness.
Additionally, this case is a clear example of the necessary ethical and legal considerations that clinicians might face, particularly considering the family's refusal to accept the initial diagnosis of brain death.
Despite institutional and academic barriers, my dedication to uncovering the truth about Jahi’s condition remains a testament to the value of scientific inquiry and patient advocacy. Today, my contributions are a foundation for future research, emphasizing the need for nuanced approaches to consciousness disorders[9,10,12,13].
| 1. | Paris JJ, Cummings BM, Moore MP Jr. "Brain death," "dead," and parental denial - the case of Jahi McMath. Camb Q Healthc Ethics. 2014;23:371-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Lewis A. Reconciling the Case of Jahi McMath. Neurocrit Care. 2018;29:20-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Shewmon DA. The Case of Jahi McMath: A Neurologist's View. Hastings Cent Rep. 2018;48 Suppl 4:S74-S76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Shewmon DA. Truly Reconciling the Case of Jahi McMath. Neurocrit Care. 2018;29:165-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 5. | Shewmon DA, Salamon N. The Extraordinary Case of Jahi McMath. Perspect Biol Med. 2021;64:457-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 6. | Truog RD. Lessons from the Case of Jahi McMath. Hastings Cent Rep. 2018;48 Suppl 4:S70-S73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Truog RD. Defining Death-Making Sense of the Case of Jahi McMath. JAMA. 2018;319:1859-1860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 8. | Greer DM, Kirschen MP, Lewis A, Gronseth GS, Rae-Grant A, Ashwal S, Babu MA, Bauer DF, Billinghurst L, Corey A, Partap S, Rubin MA, Shutter L, Takahashi C, Tasker RC, Varelas PN, Wijdicks E, Bennett A, Wessels SR, Halperin JJ. Pediatric and Adult Brain Death/Death by Neurologic Criteria Consensus Guideline. Neurology. 2023;101:1112-1132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 173] [Cited by in RCA: 128] [Article Influence: 42.7] [Reference Citation Analysis (0)] |
| 9. | Cairns H, Oldfield RC, Pennybacker JB, Whitteridge D. Akinetic mutism with an epidermoid cyst of the 3rd ventricle. Brain. 1941;64:273-290. [RCA] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 240] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Machado C. Jahi McMath: a new state of disorder of consciousness. J Neurosurg Sci. 2021;65:211-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Machado C. Brain Death Diagnosis in Primary Posterior Fossa Lesions. Neurol India. 2022;70:670-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 12. | Truog RD. The Uncertain Future of the Determination of Brain Death. JAMA. 2023;329:971-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 13. | Sala A, Gosseries O, Laureys S, Annen J. Advances in neuroimaging in disorders of consciousness. Handb Clin Neurol. 2025;207:97-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Machado C. The Jahi McMath Case: First Detailed Study of Her Brain. Neurol India. 2022;70:2235-2236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 15. | Shewmon DA, Salamon N. The MRI of Jahi McMath and Its Implications for the Global Ischemic Penumbra Hypothesis. J Child Neurol. 2022;37:35-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/