Published online Dec 9, 2023. doi: 10.5492/wjccm.v12.i5.248
Peer-review started: July 9, 2023
First decision: August 24, 2023
Revised: August 31, 2023
Accepted: October 30, 2023
Article in press: October 30, 2023
Published online: December 9, 2023
Processing time: 151 Days and 0.9 Hours
Pneumorrhachis (PR) is defined as presence of free air in the spinal canal. Trau
Core Tip: Traumatic Pneumorrhachis (PR) is defined as presence of free air in the spinal canal, and is very rare. Differentiation between epidural and intradural PR is important, because the latter is an indication of severe underlying injury. Computed tomography imaging of the entire spine must be performed to look for extension of air, as well as identify concomitant skull, torso or spinal injuries. Most patients are asymptomatic and are managed conservatively, but a few may develop neurological symptoms that need further evaluation and management.
- Citation: Pothiawala S, Civil I. Narrative review of traumatic pneumorrhachis. World J Crit Care Med 2023; 12(5): 248-253
- URL: https://www.wjgnet.com/2220-3141/full/v12/i5/248.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v12.i5.248
Pneumorrhachis (PR) is defined as presence of free air in the spinal canal. The term was coined by Newbold et al[1] in 1987, but the pathology was first described by Gordon in 1977[1,2]. The etiology of PR could be iatrogenic, non-traumatic or traumatic[3]. Iatrogenic causes include lumbar puncture, epidural anesthesia or spinal surgery. Non-traumatic causes include violent coughing or vomiting, spinal dural arteriovenous fistula, gas-producing infections, epidural abscess, malignancy, radiotherapy or drug use[4-6].
Traumatic PR is very rare, and its exact incidence is not known[7]. It has been mainly described in the radiology and spine surgery literature, and the emergency medicine specialists are less familiar with this rare presentation. This clinical review discusses the etiology, pathogenesis and management of traumatic PR.
A comprehensive literature search was performed using the PubMed, Cochrane Library, Google Scholar and Scopus databases to identify articles and case reports relevant to traumatic PR published till January 2023. The following search terms were used: “traumatic pneumorrhachis”, “spinal emphysema”, “epidural emphysema”, “intraspinal air”, “spinal pneumatosis” and “pneumomyelogram”. Studies published in English were included, and the reference lists of relevant articles were also searched. A total of 34 resources were selected for inclusion in this narrative review. Of these, there was 1 systematic review, 2 retrospective studies, 2 narrative reviews and 29 case reports/series. Publications due to non-traumatic or iatrogenic causes were excluded from this review.
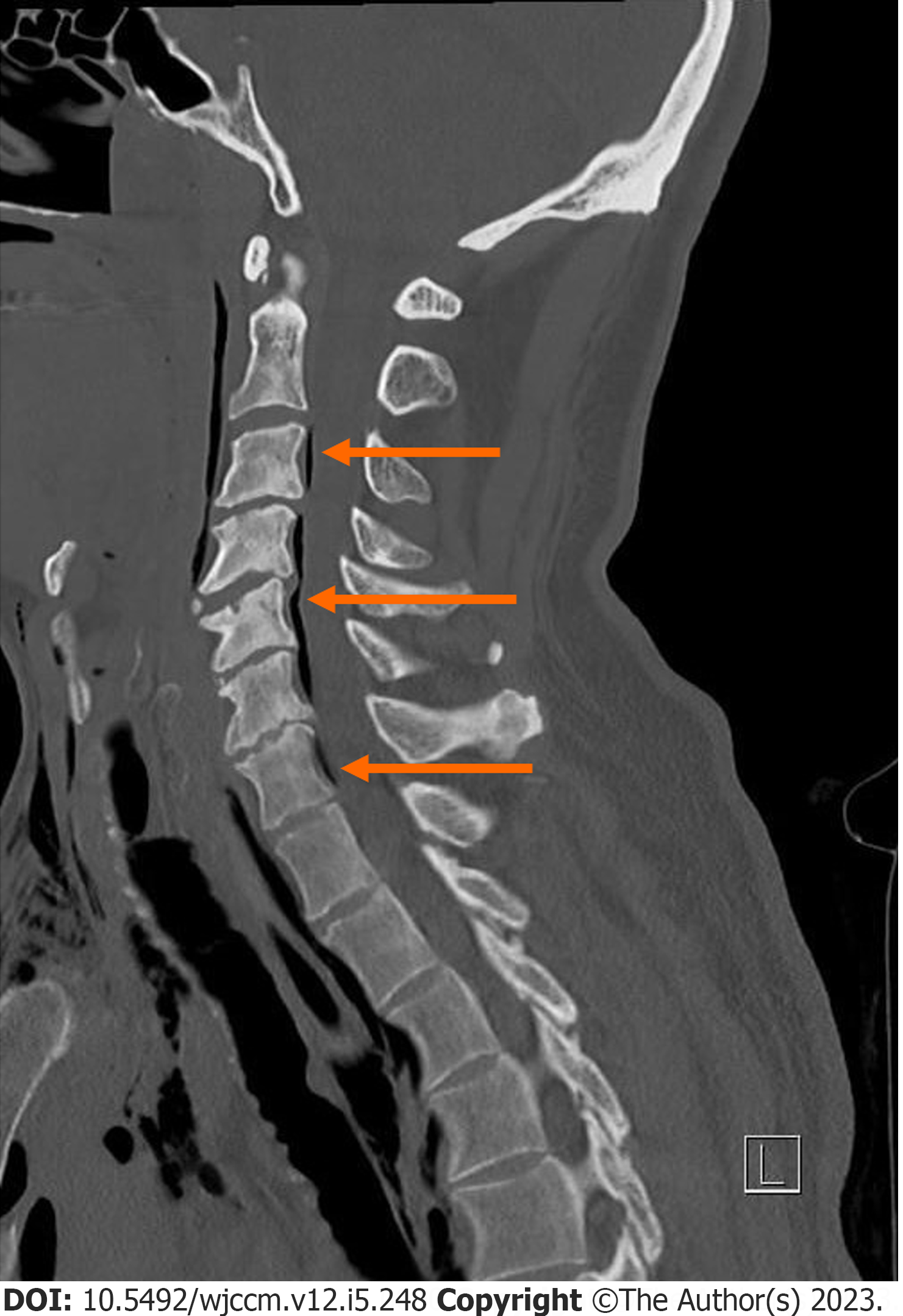
Traumatic PR is very rare. Blunt trauma accounted for 80% of cases of traumatic PR, while the remaining were secondary to penetrating trauma. PR can be classified anatomically into epidural and intradural (subdural/subarachnoid) types, based on location of air in the spinal canal. In the epidural type, air is present peripherally in the spinal canal (Figure 1), while in intradural PR, the air is seen centrally within the spinal canal in the subarachnoid space[8].
There was no correlation between the type of PR and the mechanism of injury, with 60%-65% of the traumatic PR cases being epidural PR, and the remaining 35%-40% cases had intradural PR[4]. Traumatic PR is often localized to isolated cervical, thoracic or lumbar regions, but there are have been limited case reports of PR in two contiguous spinal regions, or even along the entire spinal canal[3].
The location of air within the spinal canal depends on the site of injury causing the air leak, volume of air, capacity of the intraspinal space, and patient position. In epidural PR, air usually collects in the posterior epidural space as result of reduced resistance from the connective tissue, compared to the rich vascular network in the anterior epidural space[9]. But epidural air can also be present in the anterior or lateral epidural space (Figure 2).
There has been a reported case of PR secondary to penetrating spinal injury without an associated skull fracture[10]. In absence of penetrating injury, it can be seen in patients with head injury and basal skull fracture, likely secondary to accompanying tear in the dura mater[11]. PR was reported in a paediatric patient with associated T3 spine fracture, highlighting the need for evaluation for occult spinal fractures in patients without a clear etiology of PR[12]. The presence of traumatic PR is associated with significant injury of the skull, chest, abdomen, pelvis or spine[13], and the patient may have concomitant pneumocephalus, pneumothorax, pneumomediastinum, or subcutaneous emphysema.
The exact pathophysiology of traumatic PR is not known. One of the possible mechanisms is that in patients with base of skull fracture, air in the cranial cavity (pneumocephalus) extends inferiorly through the foramen magnum in the spinal canal leading to PR[14]. In patients with pneumothorax or pneumomediastinum, air migrates along fascial planes of mediastinum into the epidural space through the neural foramina alongside the neurovascular bundle. Due to lack of a fascial barrier between the posterior mediastinum and the spinal canal, air can enter the epidural space without any significant trauma to the surrounding structures[15,16]. Another proposed theory is entry of air in the epidural venous plexus due to embolization of small mediastinal veins[3]. It could also occur due to dural tear following blunt trauma to the trachea or the lungs[17,18]. Air can reach the spinal canal via the intervertebral veins which anastomose with the lumbar veins which are damaged due to pelvic fracture[19,20]. Hollow viscus injuries, like oesophageal perforation associated with cervical spine fractures, or duodenal or jejunal rupture after seat belt injuries and associated spine fracture can also result in PR[21,22]. There has also been a report of intradural PR secondary to subarachnoid- pleural fistula after blunt thoracic trauma[23].
Although challenging, it is important to differentiate between epidural and intradural PR, because the etiology, pathogenesis and clinical presentations are different[15]. Epidural PR is relatively less common, and is associated with traumatic pneumothorax, pneumomediastinum or subcutaneous emphysema[24]. These patients are usually asymptomatic, with only two cases reported in the literature who suffered from neurological deficits[25]. In contrast, intadural PR is frequently associated with traumatic pneumocephalus, skull fractures or thoracic spine fracture, and is a marker of severe trauma. These patients often experience associated neurological symptoms like radicular pain, limb weakness, paraesthesia, and sphincter dysfunction. Some authors suggest that the presence of PR with neurological deficit suggests a focal spinal instability due to an initial fracture-dislocation which reduced spontaneously[14,26,27]. These patients may suffer from potential complications such as tension pneumocephalus or meningitis[28]. Although tension PR has not been reported in trauma patients, intraspinal air can be trapped in the spinal canal due to a one-way valve mechanism, leading to increased pressure, which in turn causes progressive worsening of the neurological deficits.
The majority of the cases of traumatic PR are asymptomatic, thus making its clinical diagnosis extremely challenging. It is usually diagnosed incidentally during radiological evaluation for other injuries[4]. On plain radiography, PR appears as a linear lucency along the spinal canal in the lateral views of cervical and thoracic spine or chest radiographs. It has a sensitivity of about 48% and is only able to detect large volume PR[29]. Computed tomography (CT) is considered to be the diagnostic modality of choice, with a sensitivity of 100%[11]. Even on CT scan, it may sometimes be difficulty to differentiate between intradural and extradural PR, and additional testing with magnetic resonance imaging or intrathecal contrast CT can help in this differentiation[8,29].
As the incidence of traumatic PR is rare with varied underlying etiology, there are no definitive guidelines for its management, and the current management strategies are based on individual case reports[30]. Upon identification of this condition on the initial CT scan, PR is usually managed conservatively if patients are asymptomatic. Traumatic PR usually resolves spontaneously in 96% of the cases[4]. However, the patient requires monitoring for development of any new neurological symptoms[30]. There is no indication for repeat imaging as air in the spinal canal absorbs spontaneously in majority of the patients.
If PR is detected, the physician should evaluate the patient for major underlying injuries such as base of skull fracture, pneumocephalus, pneumothorax, pneumomediastinum or hollow abdominal viscera[4]. Also, in a rare instance, if the patient develops neurological symptoms or signs of raised intracranial pressure, further evaluation for a potential source of air leak is needed. Early surgical or neurosurgical consultation for surgical intervention may be required in these patients to treat the underlying causes of traumatic PR. Routine use of prophylactic antibiotics with an aim to prevent meningitis in these patients is not recommended in both epidural and intradural PR[4,13]. Rarely, traumatic PR can serve as a potential entry point for infection in the spinal canal, and antibiotics should be initiated if the patient shows any signs or symptoms of systemic infection (meningitis) or sepsis[5].
Epidural PR is generally benign and self-limiting, and the air gets spontaneously reabsorbed into the blood without any recurrence. Patients are generally managed conservatively, and they recover without any neurological sequelae[4,31]. The management of epidural PR depends on management of the underlying cause like pneumothorax or pneumomediastinum. In the case of traumatic pneumothorax, the patient may need to be undergo chest tube insertion or surgery in case of persistent air leak[32].
Presence of intradural/subarachnoid air in the spinal canal is a marker of concomitant major trauma like base of skull fracture, spinal fracture, or lung or hollow abdominal viscus injury[32]. These cases need to be referred promptly to the relevant specialty like neurosurgery or cardio-thoracic surgery for definitive management of the associated serious injuries. Persistent cerebrospinal fluid leak can be treated by repair of dural tears or placement of a lumbar spinal catheter[12]. Intradural PR may be complicated by tension pneumocephalus and meningitis[33]. Tension PR can occur rarely due to the unidirectional valve mechanism, wherein the air can occupy a significant portion of the intradural space increasing the intraspinal pressure, and by extension leading to raised intracranial pressure as well[27]. This can lead to increasing pain or development of neurologic deficits in the patient, requiring urgent treatment by neurosurgery or interventional radiology, with interventions such as air decompression using a Tuohy needle, surgical decompressive laminectomy or repair of the dural tear[34].
Traumatic PR is a rare phenomenon, often found incidentally on CT scan. Differentiation between epidural and intradural PR is important, because the latter is an indication of severe underlying injury, with potential complications of tension pneumocephalus or meningitis. CT imaging of the entire spine must be performed to look for extension of air, as well as identify concomitant skull, torso or spinal injuries. Traumatic PR is usually self-limiting, with most patients being managed conservatively, but a few may develop neurological symptoms that need further evaluation and management.
| 1. | Newbold RG, Wiener MD, Vogler JB 3rd, Martinez S. Traumatic pneumorrhachis. AJR Am J Roentgenol. 1987;148:615-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 63] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Gordon IJ, Hardman DR. The traumatic pneumomyelogram. A previously undescribed entity. Neuroradiology. 1977;13:107-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 53] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Gelalis ID, Karageorgos A, Arnaoutoglou C, Gartzonikas D, Politis A, Georgakopoulos N, Petsanas AP, Matzaroglou C, Xenakis T. Traumatic pneumorrhachis: etiology, pathomechanism, diagnosis, and treatment. Spine J. 2011;11:153-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Osunronbi T, Sofela A, Sharma H, Muquit S. Traumatic pneumorrhachis: systematic review and an illustrative case. Neurosurg Rev. 2021;44:731-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Pfeifle C, Henkelmann R, von der Höh N, Jarvers JS, Spiegl U, Josten C, Heyde CE. Traumatic pneumorrhachis. Injury. 2020;51:267-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Fujisawa H, Hasegawa M, Tsukada T, Kita D, Tachibana O, Yamashita J. Intraspinal air: an unusual finding of cervical epidural abscess. Acta Neurochir (Wien). 1998;140:287-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Raswan US, Arif SH, Ramzan AU. Posttraumatic pneumorrhachis. Neurol India. 2018;66:1522-1523. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Yang YY, Chua CB, Hsu CW, Lee KH. Traumatic epidural pneumorrhachis: a case report. Hong Kong Med J. 2020;26:528-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 9. | El-Halabi D, Alkandari T, Yaktien MM. Traumatic air in spinal canal (pneumorrhachis). Anaesthesiol Intensive Ther. 2012;44:25-27. [PubMed] |
| 10. | Alkan A, Baysal T, Saras K, Sigirci A, Kutlu R. Early MRI findings in stab wound of the cervical spine: two case reports. Neuroradiology. 2002;44:64-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | White P, King M, Civil I. Pneumorrhachis following head trauma. Emerg Med Australas. 1997;9:337-338. [DOI] [Full Text] |
| 12. | Chang JG, Fisher LS, Choudhary D. Pneumorrhachis in a Pediatric Patient with an Isolated Back Injury. J Emerg Med. 2021;61:e116-e119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Oertel MF, Korinth MC, Reinges MH, Krings T, Terbeck S, Gilsbach JM. Pathogenesis, diagnosis and management of pneumorrhachis. Eur Spine J. 2006;15 Suppl 5:636-643. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 123] [Cited by in RCA: 153] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 14. | Kara H, Akinci M, Degirmenci S, Bayir A, Ak A. Traumatic pneumorrhachis: 2 cases and review of the literature. Am J Emerg Med. 2015;33:861.e1-861.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Chun BJ, Moon JM. Symptomatic epidural pneumorrhachis associated with an occult pneumomediastinum due to minor trauma. Spine (Phila Pa 1976). 2009;34:E979-E982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Allard E, Selim J, Veber B. Pneumocephalus and pneumorachis after blunt chest trauma without spinal fractures: a case report. J Med Case Rep. 2019;13:317. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Scialdone CJ, Wagle W. Intraspinal air: an unusual manifestation of blunt chest trauma. Clin Imaging. 1990;14:59-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Delamarter RB, Heller J, Bohlman HH. Cervical pneumomyelogram secondary to a closed fracture-dislocation of the thoracic spine. A case report. Spine (Phila Pa 1976). 1989;14:1421-1422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Gautschi OP, Hermann C, Cadosch D. Spinal epidural air after severe pelvic and abdominal trauma. Am J Emerg Med. 2008;26:740.e3-740.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Chimon JL, Cantos EL. CT recognition of spinal epidural air after pelvic trauma. J Comput Assist Tomogr. 1990;14:795-796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Agha FP, Raji MR. Oesophageal perforation with fracture dislocation of cervical spine due to hyperextension injury. Br J Radiol. 1982;55:369-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Dehner JR. Seatbelt injuries of the spine and abdomen. Am J Roentgenol Radium Ther Nucl Med. 1971;111:833-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Szlachcińska A, Kozak A. Subarachnoid-pleural fistula in a patient with blunt chest trauma. Kardiochir Torakochirurgia Pol. 2012;9:66-68. |
| 24. | Copetti R, Mattei G. Traumatic epidural pneumorrhachis. BMJ Case Rep. 2010;2010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 25. | Koktekir E, Tatarli N, Ceylan D, Koktekir BE, Akdemir G. Symptomatic pneumorrhachis. J Neurol Surg A Cent Eur Neurosurg. 2014;75:140-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Ould-Slimane M, Ettori MA, Lazennec JY, Pascal-Moussellard H, Catonne Y, Rousseau MA. Pneumorachis: a possible source of traumatic cord compression. Orthop Traumatol Surg Res. 2010;96:825-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Kim KY, Kang JH, Lee MH, Han Y, Choi DW. Atypical traumatic pneumorrhachis accompanied by paraparesis. Ann Rehabil Med. 2014;38:410-414. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 28. | Mistry R, Wongseelashote S, Freebairn R. Subarachnoid pneumorrhachis following blunt thoracic and spinal trauma. Crit Care Shock. 2019;22:322-326. |
| 29. | Goh BK, Yeo AW. Traumatic pneumorrhachis. J Trauma. 2005;58:875-879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 60] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 30. | Arora S, Aggarwal P, Cheema GS, Singla J. Pneumorachis of the cervical spine with associated pneumocephalus and subcutaneous emphysema. Indian J Orthop. 2011;45:372-375. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 31. | Behr G, Mema E, Costa K, Garg A. Proportion and Clinical Relevance of Intraspinal Air in Patients With Pneumomediastinum. AJR Am J Roentgenol. 2018;211:321-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 32. | Katz DS, Groskin SA, Wasenko JJ. Pneumorachis and pneumocephalus caused by pneumothorax and multiple thoracic vertebral fractures. Clin Imaging. 1994;18:85-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 32] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 33. | Kim SD, Kim JS, Seong JY, Choi YG, Park IS, Baik MW. Traumatic pneumorrhachis. Kor Neurotraumatol Soc. 2007;3:113-115. |
| 34. | Song KJ, Lee KB. Spontaneous extradural pneumorrhachis causing cervical myelopathy. Spine J. 2009;9:e16-e18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Critical care medicine
Country/Territory of origin: New Zealand
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ferreira GSA, Brazil; Md Reazaul Karim H, India S-Editor: Fan JR L-Editor: A P-Editor: Cai YX