Published online May 9, 2022. doi: 10.5492/wjccm.v11.i3.178
Peer-review started: January 12, 2022
First decision: February 8, 2022
Revised: February 11, 2022
Accepted: April 24, 2022
Article in press: April 24, 2022
Published online: May 9, 2022
Processing time: 114 Days and 9.6 Hours
In patients with respiratory failure, loop diuretics remain the cornerstone of the treatment to maintain fluid balance, but resistance is common.
To determine the efficacy and safety of common diuretic combinations in critically ill patients with respiratory failure.
We searched MEDLINE, Embase, Cochrane Library and PROSPERO for studies reporting the effects of a combination of a loop diuretic with another class of diuretic. A meta-analysis using mean differences (MD) with 95% confidence interval (CI) was performed for the 24-h fluid balance (primary outcome) and the 24-h urine output, while descriptive statistics were used for safety events.
Nine studies totalling 440 patients from a total of 6510 citations were included. When compared to loop diuretics alone, the addition of a second diuretic is associated with an improved negative fluid balance at 24 h [MD: -1.06 L (95%CI: -1.46; -0.65)], driven by the combination of a thiazide plus furosemide [MD: -1.25 L (95%CI: -1.68; -0.82)], while no difference was observed with the combination of a loop-diuretic plus acetazolamide [MD: -0.40 L (95%CI: -0.96; 0.16)] or spironolactone [MD: -0.65 L (95%CI: -1.66; 0.36)]. Heterogeneity was high and the report of clinical and safety endpoints varied across studies.
Based on limited evidence, the addition of a second diuretic to a loop diuretic may promote diuresis and negative fluid balance in patients with respiratory failure, but only when using a thiazide. Further larger trials to evaluate the safety and efficacy of such interventions in patients with respiratory failure are required.
Core Tip: Loop diuretics are a cornerstone treatment to maintain fluid balance in patients with respiratory failure, but resistance is common. In the caveat of a substantial heterogeneity, this meta-analysis shows a significant increase in urine output with negative fluid balance with the combination of loop diuretics plus thiazides compared to loop diuretics alone in patients with respiratory failure. Further trials are required to confirm the safety and efficacy of such interventions in patients with respiratory failure.
- Citation: Côté JM, Goulamhoussen N, McMahon BA, Murray PT. Diuretic combinations in critically ill patients with respiratory failure: A systematic review and meta-analysis. World J Crit Care Med 2022; 11(3): 178-191
- URL: https://www.wjgnet.com/2220-3141/full/v11/i3/178.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v11.i3.178
Progressive fluid accumulation is a commonly encountered scenario in critically ill patients and in patients with acute kidney injury (AKI), acute heart failure, and other edematous states. Fluid overload is associated with increased mortality[1,2] and numerous systemic complications such as poor wound healing, AKI and pulmonary edema with acute hypoxemic respiratory failure (AHRF)[3]. Interpretation of studies evaluating the relationship between fluid balance and mortality in AHRF is complex, especially in the context of other organ outcomes[4]. Early observational studies of fluid management in the specific context of patients with AHRF have shown that a negative fluid balance is associated with improved survival, particularly in the context of acute respiratory distress syndrome (ARDS)[5,6]. Though, the definitive trial evaluating fluid management during ARDS showed that a conservative fluid balance achieved with diuretics did not statistically affect mortality but did increase the number of ventilator-free days and intensive care unit (ICU)-free days survival[7].
In the ICU, loop diuretics remain the most widely used class of diuretics, and are used in up to 49% of all ICU admissions[8]. However, prolonged use of loop diuretics may be associated with therapeutic resistance, which is a frequent observation in the ICU and associated with increased risk of mortality[9]. Combining multiple diuretics with different mechanisms of action may achieve a sequential nephron blockade, further limiting the kidney's ability to reabsorb fluid and electrolytes. These actions may further increase urine output, but also potentially lead to complications such as electrolyte and acid-base disorders and worsening kidney function[10,11]. Diuretic combinations are routinely used in the management of heart failure, and there is a significant body of evidence supporting that practice[12,13]. Both American and European Heart Failure Guidelines recommend that when diuresis remains inadequate with loop diuretic therapy despite dose escalation, the addition of thiazide diuretics may be considered[14,15]. Recent data have also shown that the addition of a second diuretic can help to mitigate loop-diuretic resistance in a broad cohort of patients hospitalised in the ICU[16].
However, in patients with AHRF, only few data exist on the additional efficacy of various diuretic regimens to promote diuresis in resistant edematous states, despite the use of this approach in up to 6% of all ICU admissions[8]. Instead of progressively escalate the dose in patients resistant to loop diuretics, a proactive administration of a second diuretic may help to quickly increase the urine output, and therefore minimize respiratory complications. On the other hand, as opposed to patients with heart failure where the extravascular fluid retention usually represents multiple liters, patients with AHRF may have a relatively small fluid retention but enough to significantly affect the perturbed pulmonary physiology. In these patients, the risks of quickly increasing the diuresis, and therefore having a substantial negative fluid balance, may be higher regarding renal function, electrolyte homeostasis or hypotension. To date, no systematic review has evaluated different protocols of diuretic combinations in this population regarding their efficacy but also their safety.
The aim of this systematic review was to determine the efficacy of common diuretic combinations to promote negative fluid balance in patients hospitalised in the ICU with AHRF. The objective was to compare the use of loop diuretics in monotherapy to the use of a loop diuretic with an adjunctive non-loop diuretic agent paying particular attention to rates of AKI and electrolyte disturbance.
This systematic review with meta-analysis was reported following the Preferred Reporting Items for Systematic Reviews and Meta-analysis guidelines[17]. The protocol was registered on the PROSPERO international prospective register of systematic reviews (CRD42020218381).
Inclusion criteria: Eligible studies compared diuretic combinations to loop diuretics alone in adult patients hospitalised in ICU with respiratory failure receiving diuretics for volume control. Respiratory failure was defined as receiving invasive or non-invasive positive ventilation for an acute hypoxemic or hypercapnic respiratory failure, or for severe pulmonary edema requiring oxygen therapy. Patients with non-primary pulmonary aetiology, such as acute decompensated heart failure, were included if signs of severe pulmonary edema requiring oxygen, with or without mechanical ventilation, were clearly reported. Studies evaluating a combination of diuretic agents without a comparison group were included in the systematic review if at least one efficacy clinical outcome of interest was reported, but were not included in the final meta-analysis. The following classes of non-loop diuretics in combination with a loop diuretic were included: Thiazide or thiazide-like agents, carbonic anhydrase inhibitors, Epithelial sodium channel (ENaC) inhibitors and mineralocorticoid antagonists. No study design, date or language limits were imposed on the literature search, although only studies in English, Spanish and French were included in the analysis.
Exclusion criteria: Studies reporting patients with peripheral edema only were excluded. Studies reporting patients with chronic kidney disease (CKD) treated with maintenance kidney replacement therapy (KRT) were also excluded. Studies of the use of loop diuretic agents in pediatric populations were excluded.
According to the predetermined protocol, a systematic literature search of 4 databases (MEDLINE, Embase, Cochrane Library and PROSPERO) was performed from inception until May 5, 2021 in collaboration with a trained medical librarian (covering from 1946 to May 2021). The literature search strategy was developed using medical subject headings and text words related to all classes of diuretics included and their individual name, fluid balance, respiratory failure and hypoxemia, and critical care (Supplementary Table 1). We also scanned the reference lists of included studies and searched the grey literature for all abstracts listed into the annual meeting archives of the American Society of Nephrology, the European Society of Intensive Care Medicine and the Society of Critical Care Medicine. Finally, a bibliography of all potentially included articles was circulated to all authors, to prompt consideration of any other relevant publications.
Eligible studies were clinical trials, observational cohort studies, case-control studies and cross-sectional studies. Cases series with more than five patients and abstracts not yet published were also included when at least one outcome of interest was described quantitatively. Literature search results were uploaded and screened using Rayyan QCRI application. Two reviewers (JMC and NG) independently screened the titles and abstracts of all identified articles. These reviewers then screened the full-text reports for all potential studies and decided whether these met the inclusion criteria, reporting the reason(s) for exclusions. When necessary, the authors (JMC and BMcM) contacted the corresponding author of potential studies to obtain additional information. Once the final list of included articles was determined, there was no disagreements between authors.
RevMan (Version 5.4, The Cochrane Collaboration, 2020) was used to extract data from each eligible study. Data extracted included eligibility criteria, demographics, methodology, diuretic name, class and dosage, risk of bias and results. The prespecified primary efficacy outcome of interest was the cumulative fluid balance, and secondary outcomes were the 24-h urine output (diuresis), ventilation-free survival, number of days on mechanical ventilation, need of therapeutic paracentesis, hospital and ICU length-of-stay, in-hospital and 90-d mortality. Due to lack of data regarding the cumulative ICU fluid balance for all included studies, the 24-h fluid balance was therefore reported as primary outcome. Safety endpoints included AKI incidence and progression to KRT, electrolyte and acid-base abnormalities, creatinine and electrolyte changes from baseline (sodium, potassium, bicarbonate) and, finally, hypotensive events, arrythmias and ototoxicity occurrence. Reports of 24-h natriuresis, not planned in the original protocol, were also captured as this endpoint was considered clinically relevant.
The risk of bias was assessed using the Cochrane Collaboration tool for assessing the risk of bias for randomised controlled trials (RCTs) (RoB2)[18], and non-randomised trials (n-RCTs)(ROBINS-I)[19], and the Newcastle-Ottawa Scale for observational studies. These assessments were based on the reporting of fluid balance, the primary outcome of the current review. When insufficient details were reported, the risk of bias was judged as unclear.
A meta-analysis using mean differences (MD) with 95% confidence interval (CI) was performed for the primary outcome and for the 24-h urine output (secondary efficacy endpoint), while descriptive statistics were used for all other endpoints reported. The statistical heterogeneity for pooled results was reported using I2. As the clinical heterogeneity of included studies was considered high, a random-effects model was used for both meta-analyses. In studies reporting the endpoint using median and IQR, the statistical method described by Wan et al[20] was used to convert the reported value to mean ± SD allowing meta-analysis. None of the preplanned sub-analyses (dosage of loop diuretics and the type of respiratory failure) were performed due to limited data. All statistical analyses were performed on RevMan (Version 5.4, The Cochrane Collaboration, 2020) and SPSS (Version 26, IBM, Armonk NY).
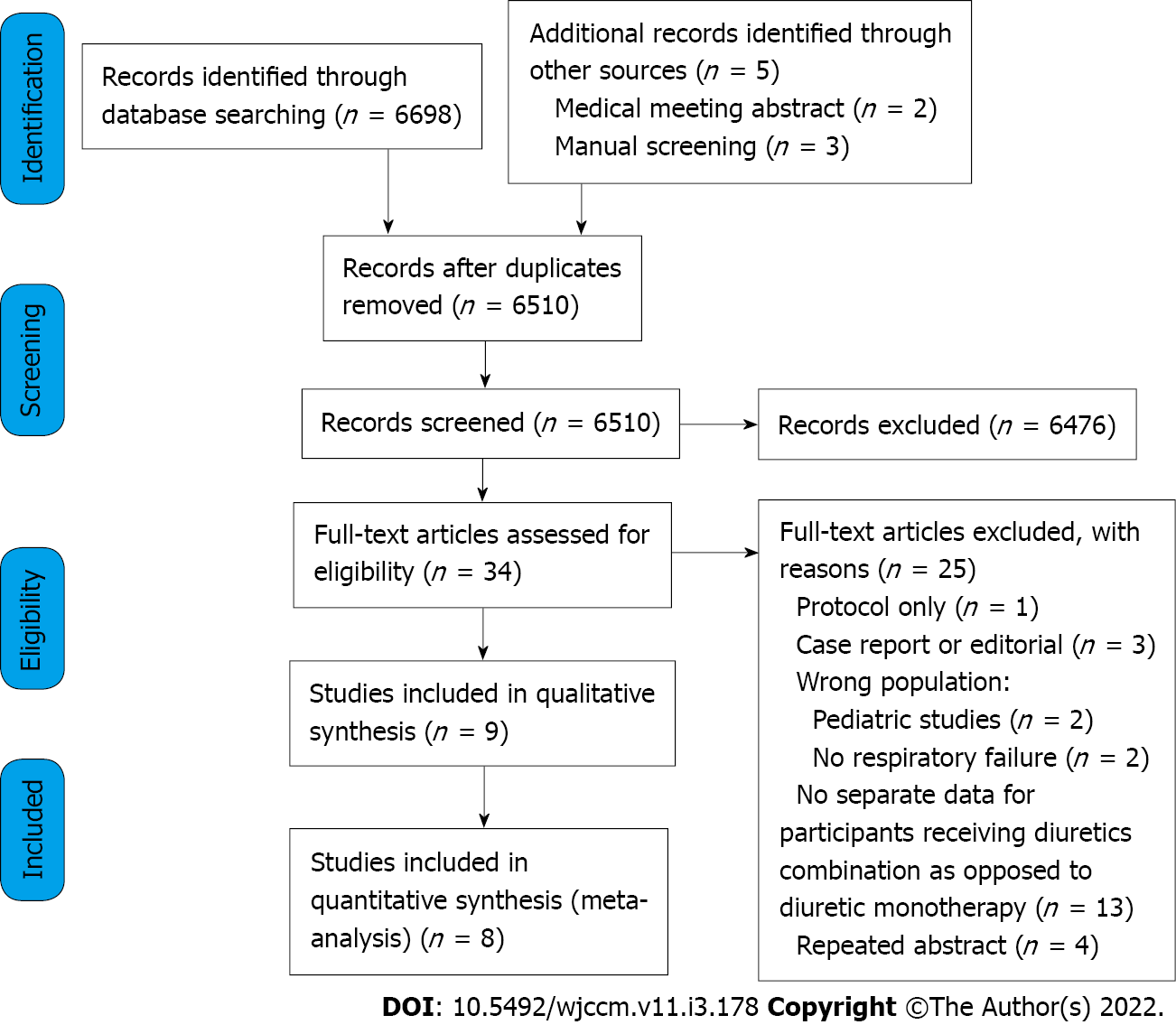
Study selection is depicted in Figure 1. After removal of duplicates, there were 6510 studies. Of these, 6476 were excluded after screening titles and abstracts. A total of 34 studies were assessed for eligibility, from which 25 were excluded for not meeting inclusion criteria (Supplementary Table 2). Therefore, a total of 9 studies were included[21-29], from which 8 presented quantitative results for endpoints meta-analysis[21-23,25-29].
A detailed summary of each of the study characteristics is presented in Table 1. The included studies investigated the combination of furosemide with either spironolactone[21], indapamide[22], chlorothiazide[23,27,29], metolazone[23,27,28], acetazolamide[24,25] or a combination of hydrochloroth- iazide and amiloride[26] at various doses in patients with respiratory failure. These studies were published between 1997 and 2019, and included a total of 440 participants. Three studies were RCTs[21,22,25] and 5 were observational[23,24,27-29], and one was a prospective non-randomised interventional study[26].
| Ref. | Country, design | Inter-vention duration | Major eligibility criteria | Study groups (sample size) | Median daily dose of diuretic (route) | Patients characteristics | |
| Apte et al[21], 2008 | Australia; RCT | 72 h | (1) Mechanically ventilated; and (2) On continuous IV furosemide | Furosemide + Spironolactone (n = 10) | 97 mg (71-288) (IV); 300 mg (PO) | (1) Age: 68 (55-79); (2) Male sex: 7 (70%); (3) SCr, μmol/L: -; (4) Apache II Score: 21 (15-28); and (5) Positive ventilation: 10 (100%) | ICU admission for (1) Sepsis: 4 (40%); (2) Cardiovascular: 2 (20%); and (3) COPD/Resp. failure: 2 (20%). In-hospital mortality: - |
| Furosemide + Placebo (n = 10) | 168 mg (74-295) (IV) | (1) Age: 67 (52-76); (2) Male sex: 6 (60%); (3) SCr, umol/L: -; (4) Apache II Score: 24 (17-26); and (5) Positive ventilation: 10 (100%) | ICU admission for (1) Sepsis: 6 (60%); (2) Cardiovascular: 1 (10%); and (3) COPD/Resp. failure: 0 (0%). In-hospital mortality: - | ||||
| Bihari et al[22], 2016 | Australia; RCT | 24 h | (1) Fluid overload (> 10% ICU admission weight); and (2) No prior diuretic last 48 h | Furosemide (n = 20) | 1 mg/kg (IV); Median weight: 78 kg | (1) Age: 75 (62-86); (2) Male sex: 12 (60%); (3) SCr, μmol/L: 97 (69-133); (4) Apache III Score: 68 ± 21; and (5) Positive ventilation: 14 (70%) | ICU admission for (1) Sepsis: 3 (15%); (2) Cardiovascular: 3 (15%); and (3) COPD/Resp. failure: 12 (60%). In-hospital mortality: 5 (25) |
| Furosemide + Indapamide (n = 20) | 1 mg/kg (IV); 5 mg (PO) | (1) Age: 70 (53-75); (2) Male sex: 14 (70%); (3) SCr, μmol/L: 91 (63-141); (4) Apache III Score: 74 (29); and (5) Positive ventilation: 10 (50%) | ICU admission for (1) Sepsis: 3 (15%); (2) Cardiovascular: 4 (20%); and (3) COPD/Resp. failure: 10 (50%). In-hospital mortality: 5 (25) | ||||
| Bohn et al[27], 20191 | United States; Observa-tional (paired groups) | 24 h | (1) ADHF with reduced ejection fraction; and (2) Not responding to furosemide monotherapy | Furosemide + Chlorothiazide (n = 34, from 108)1 | ≥ 80 mg (IV); 500 to 1000 mg (IV) | (1) Age: 64 (54-69); (2) Male sex: 74 (69%); (3) SCr, umol/L: 132 (90-187); (4) Apache II Score: 12 (9-15); and (5) Positive ventilation: - | ICU admission for (1) Sepsis: -; (2) Cardiovascular: 108 (100%); and (3) COPD/Resp. failure: -. In-hospital mortality: 21 (19) |
| Furosemide (n = 34, from 108)1 | ≥ 80 mg (IV) | - | - | ||||
| Furosemide + Metolazone (n = 16, from 60)1 | ≥ 80 mg (IV); 5 to 10 mg (PO) | (1) Age: 63 (54-74); (2) Male sex: 41 (68%); (3) SCr, umol/L: 142 (102-188); (4) Apache II Score: 10 (7-14); and (5) Positive ventilation: - | ICU admission for (1) Sepsis: -; (2) Cardiovascular: 60 (100%); and (3) COPD/Resp. failure: -. In-hospital mortality: 1 (2) | ||||
| Furosemide (n = 16, from 60)1 | ≥ 80 mg (IV) | - | - | ||||
| Heming et al[24], 2011 | France; Observa-tional | 24 h | (1) Mechanically ventilated; and (2) Acute respiratory failure | Furosemide + Acetazolamide (n = 29, from 68)2 | 80 mg (40-80) (IV); 500 to 1000 mg (PO) | (1) Age: 77 (73-83); (2) Male sex: 9 (31%); (3) SCr, umol/L: 66 (57-89); (4) Apache II Score: 25 (20-30); and (5) Positive ventilation: 29 (100%) | ICU admission for (1) Sepsis: 6 (21%); (2) Cardiovascular: 5 (17%); and (3) COPD/Resp. failure: 16 (55%). In-hospital mortality: 10 (34) |
| Imiela and Budaj[25], 2017 | Poland; RCT | 96 h | (1) ADHF not responding to furosemide; and (2) Significant pulmonary overload | Furosemide3 + Acetazolamide (n = 10) | 110 mg (± 73) (IV); 250 to 500 mg (PO) | (1) Age: 73 (± 8.6); (2) Male sex: 8 (80%); (3) SCr, μmol/L: 137 (± 42); (4) Apache II Score: -; and (5) Positive ventilation: - | ICU admission for (1) Sepsis: -; (2) Cardiovascular: 10 (100%); and (3) COPD/Resp. failure: -. In-hospital mortality: - |
| Furosemide3 (n = 10) | 152 mg (± 97) (IV) | (1) Age: 71 (± 14); (2) Male sex: 9 (90%); (3) SCr, umol/L: 141 (± 77); (4) Apache II Score: -; and (5) Positive ventilation: - | ICU admission for (1) Sepsis: -; (2) Cardiovascular: 10 (100%); and (3) COPD/Resp. failure: - | ||||
| Michaud and Mintus[23], 2017 | United States; Observa-tional (paired groups) | 24 h | (1) Hospitalized at the ICU; and (2) Received IV furosemide + 2nd diuretics for severe fluid overload | Furosemide + Chlorothiazide (n = 58) | 280 mg (40-720) (IV); 392 mg (± 225) (IV) | (1) Age: 61 (± 12); (2) Male sex: 35 (60%); (3) SCr, μmol/L: 124 (± 53); (4) Apache II Score: -; and (5) Positive ventilation: - | ICU admission for (1) Sepsis: 4 (6.8%); (2) Cardiovascular: 25 (43%); and (3) COPD/Resp. failure: 15 (26%). In-hospital mortality: 11 (19) |
| Furosemide (n = 58) | 193 mg (20-710) (IV) | - | - | ||||
| Furosemide + Metolazone (n = 64) | 240 mg (20-960) (IV); 6.8 mg (± 3.3) (PO) | (1) Age: 65 (± 14); (2) Male sex: 31 (48%); (3) SCr, μmol/L: 115 (± 44); (4) Apache II Score: -; and (5) Positive ventilation: - | ICU admission for (1) Sepsis: 9 (14%); (2) Cardiovascular: 24 (38%); and (3) COPD/Resp. failure: 12 (19%). In-hospital mortality: 17 (27) | ||||
| Furosemide (n = 64) | 130 mg (20-750) (IV) | - | - | ||||
| Ng et al[28], 2013 | United States; Observa-tional (paired groups) | 48 h | (1) Hospitalized at the ICCU; and (2) Failed to respond to intermittent furosemide | Furosemide + Metolazone (n = 42) | 80 mg (80-160) (IV); 5 mg (2.5-10) (PO) | (1) Age: 57 (± 13); (2) Male sex: 22 (52%); (3) SCr, μmol/L: 148 (± 88); (4) Apache II Score: -; and (5) Positive ventilation: - | ICU admission for (1) Sepsis: -; (2) Cardiovascular: 42 (100%); and (3) COPD/Resp. failure: -. In-hospital mortality: 0 (0) |
| Furosemide (n = 42) | 80 mg (0-160) (IV) | - | - | ||||
| Shulenberger et al[29], 2016 | United States; Observa-tional (paired groups) | 24 h | (1) ADHF with loop-diuretic resistance defined as > 160 mg/d of furosemide; and (2) Admitted in the ICU | Furosemide + Chlorothiazide (n = 40, from 88)4 | 346 mg (± 144) (IV); 508 mg (± 273) (IV) | (1) Age: 59 (± 12); (2) Male sex: 26 (65%); (3) SCr, μmol/L: -; (4) Apache II Score: -; and (5) Positive ventilation: - | ICU admission for (1) Sepsis: -; (2) Cardiovascular: 40 (100%); and (3) COPD/Resp. failure: -. In-hospital mortality: 3 (8.5) |
| Furosemide (n = 40)4 | 351 mg (± 143) (IV) | ||||||
| Furosemide + Metolazone (n = 38, from 89)4 | 261 mg (± 111) (IV); 5.7 mg (± 2.5) | (1) Age: 57 (± 13); (2) Male sex: 19 (50%); (3) SCr, umol/L: -; (4) Apache II Score: -; and (5) Positive ventilation: - | ICU admission for (1) Sepsis: -; (2) Cardiovascular: 38 (100%); and (3) COPD/Resp. failure: -. In-hospital mortality: 9 (24%) | ||||
| Furosemide (n = 38)4 | 263 mg (± 102) (IV) | ||||||
| Vánky et al[26], 1997 | Sweden; n-RCT (unpaired groups) | 24 h | (1) Hospitalized at the ICU post-Cardiac surgery; and (2) Received IV furosemide for severe fluid overload | Furosemide + HCTZ + Amiloride (n = 20) | 87 mg (± 4) (IV); 50 mg (PO); 5 mg (PO) | (1) Age: 70 (± 1.4); (2) Male sex: 15 (75%); (3) SCr, μmol/L: 98 (± 3); (4) Apache II Score: -; and (5) Positive ventilation: - | ICU admission for (1) Sepsis: -; (2) Cardiovascular: 20 (100%); and (3) COPD/Resp. failure: -. In-hospital mortality: - |
| Furosemide (n = 57) | 117 mg (± 18) (IV) | (1) Age: 67 (± 1.2); (2) Male sex: 40 (70%); (3) SCr, μmol/L: 105 (± 4); (4) Apache II Score: -; and (5) Positive ventilation: - | ICU admission for (1) Sepsis: -; (2) Cardiovascular: 57 (100%); and (3) COPD/Resp. failure: -. In-hospital mortality: - | ||||
For the study by Heming et al[24], only 29 from the 68 participants were receiving a loop diuretic in addition to acetazolamide. All results reported from this study were calculated using the subset of the entire cohort receiving that combination of diuretics based on the dataset shared by the authors. Similarly, only patients with confirmed ICU admission with respiratory failure from the Shulenberger et al[29] study (n = 78, from 177 in total) were included in this review, after access to the original dataset. Overall, in this review, females were the minority and the median age ranged from 57 to 77 years. Most patients were admitted following cardiac surgery or acute decompensated heart failure. The duration of the diuretic combination intervention varied from 24 to 96 h, while the median furosemide dose (equivalent to intravenous furosemide) ranged from approximately 80 to 351 mg per day. The doses of the second diuretic are reported in Table 1.
The quality assessment and risks of bias are presented in the Supplementary Material (Supplementary Table 3). All 3 RCTs included[21,22,25], despite limited sample size, were good quality with an overall low risk of bias. The non-randomised interventional trial was classified with an overall unclear risk of bias, due to missing data[26] and potential uncontrolled confounders. The observational cohort studies included were of good quality, where the risk of bias was adequately minimized for most components of the Newcastle-Ottawa Assessment Scale. No unpublished data was included in this review. Heterogeneity was substantial across all included studies, regarding study design, intervention duration and timing of administration, dose of loop-diuretics administered, baseline kidney function and safety endpoints reported. Notably, the intervention duration, defined as the period of diuretics administration during which clinical endpoints were measured, ranged between 24 h to 96 h. In addition, regarding the second diuretic, some studies reported a fixed dose for all patients, while other reported a titratable dose. The comparison group receiving only a loop-diuretic was an independent and parallel-group for 4 studies[21,22,25,26], and a sequential paired group–where clinical endpoints were compared before and after the addition of a second diuretic within the same group–for 4 studies[23,27-29].
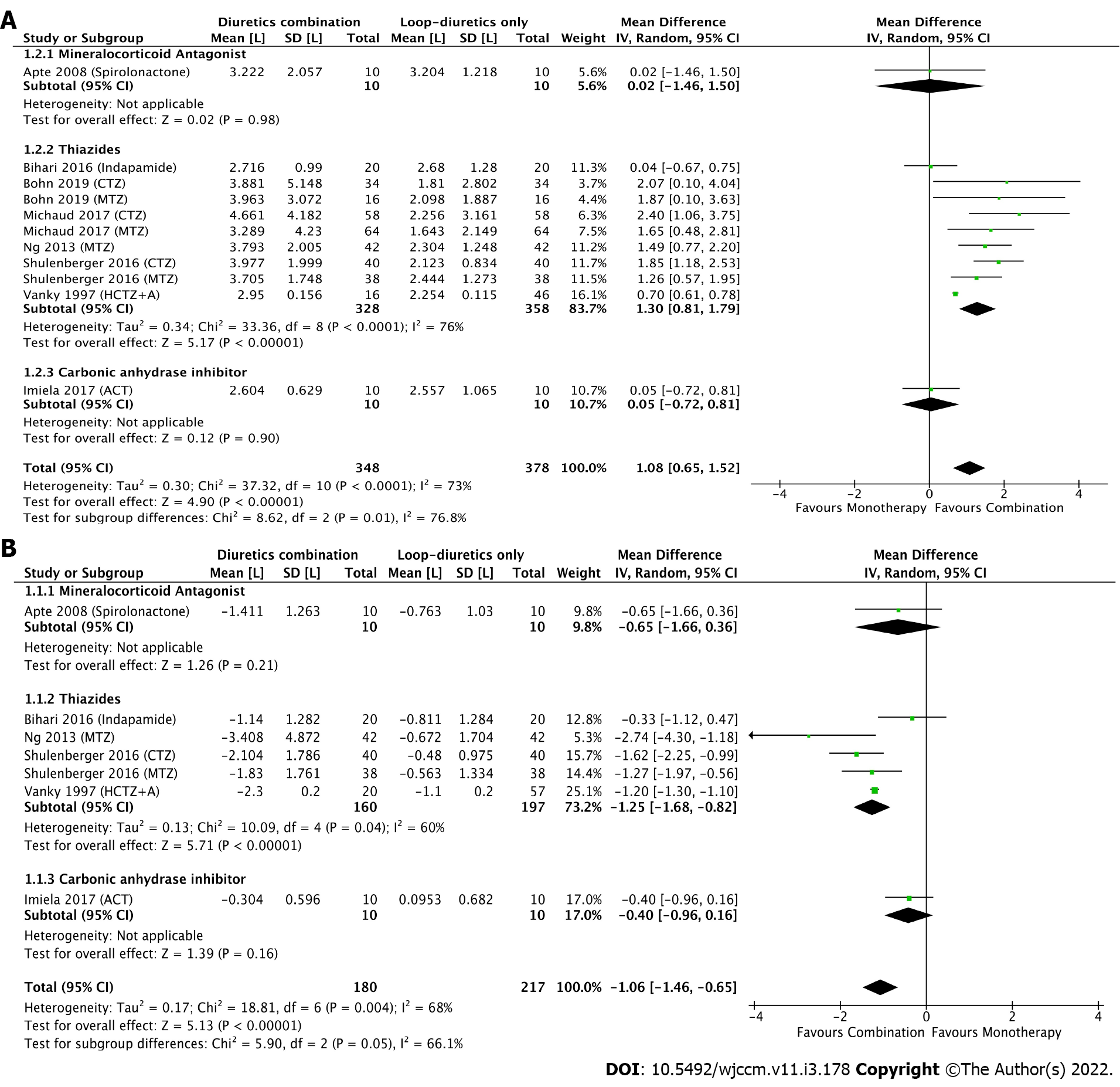
When combining all studies using various combinations of non-loop-diuretic plus loop-diuretic compared to loop-diuretics alone, a significant difference was observed in the primary outcome, with a MD in the 24-h fluid balance in favour of the combination group [overall MD: -1.06 L (95%CI: -1.46; -0.65), I2 = 68%] (Figure 2A). However, when each combination diuretic class was analyzed separately, no significant difference was observed for the spironolactone-furosemide [MD: -0.65 L (95%CI: -1.66; 0.36), I2 = NA] or the acetazolamide-furosemide combination [MD: -0.40 L (95%CI: -0.96; 0.16), I2 = NA]. Thus, the observed effect on the daily fluid balance was mainly driven by the thiazide-furosemide combinations [MD: -1.25 L (95%CI: -1.68; -0.82), I2 = 60%]. Inspection of the funnel plot (Supplemen
Similar findings were reported for the 24-h urine output, where the addition of a second diuretic was associated with an increase in the urine output by 1.08 L (95%CI: 0.65; 1.52, I2 = 73%). Once again, that effect was mainly attributed to the thiazide-furosemide combination [MD: 1.30 L (95%CI: 0.81-1.79), I2 = 76%] as no difference was observed for other combinations (Figure 2B). Overall, while the addition of spironolactone or acetazolamide to furosemide had a limited effect on fluid and sodium balance (Supplementary Table 4), the addition of a thiazide was associated with an increase in urine output by 14% for indapamide, 31% for hydrochlorothiazide plus amiloride, ranged from 52%-101% for metolazone and, finally, from 89%-114% for chlorothiazide, with corresponding effects on the negative fluid balance. In-hospital mortality, ICU length-of-stay, and hospital length-of-stay are depicted in Supplementary Table 5. Due to limited data, no pooled analysis was performed for these outcomes. No study reported the 28-d or 90-d mortality, need of therapeutic paracentesis and ventilation free-survival.
Available data on the physiological effects of these diuretic combinations on electrolytes and serum creatinine is shown in Table 2, but reporting was inconsistent. Due to significant heterogeneity across these studies, results for these endpoints were not pooled, but instead reported separately. No diuretic combination was associated with a substantial serum creatinine change at 24-h from baseline. According to the specific segment of the nephron targeted, varied impacts on electrolytes were observed for these three diuretic classes; for example, whereas a limited increase in serum potassium was observed with the spironolactone combination, a decrease in serum potassium was observed in all thiazide studies reporting this endpoint. Notably, as opposed to thiazide and loop-diuretic combinations, with which an increased in serum bicarbonate was observed, treatment with acetazolamide for 24-h reduced serum bicarbonate levels by 3.6 ± 5.1 mmol/L.
| Ref. | Treatment group | 24-h biochemical changes1 | Safety events, n (%) | ||||
| Creatinine, μmol/L | Sodium, mmol/L | Potassium, mmol/L | Bicarbonate, mmol/L | Hypona-tremia | Hypo-kalemia | ||
| Mineralocortocoid-antagonist | |||||||
| Apte et al[21], 2008 | Spironolactone + Furosemide (n = 10) | +4.8 (4.1-6.9) | -1.0 (?) | +0.13 (?) | - | - | - |
| Furosemide (n = 10) | +23 (-4.4-39) | +3.0 (?) | +0.13 (?) | - | - | - | |
| Thiazides | |||||||
| Bihari et al[22], 2016 | Indapamide + Furosemide (n = 20) | -5.2 ± 38 | 0 ± 0 | -0.4 ± 1.8 | +1.4 ± 6.3 | 0 (0) | 0 (0) |
| Furosemide (n = 20) | -2.3 ± 14 | +2.0 ± 4.0 | -0.2 ± 0.6 | +0.9 ± 2.5 | 0 (0) | 0 (0) | |
| Bohn et al[27], 2019 | CTZ + Furosemide (n = 34) | - | - | - | - | - | 8 (24) |
| MTZ + Furosemide (n = 16) | - | - | - | - | - | 3 (19) | |
| Michaud and Mintus[23], 2017 | CTZ + Furosemide (n = 58) | -18 ± 57 | +0.5 ± 5.6 | -0.4 ± 0.6 | +3.3 ± 5.1 | 15 (26) | 10 (17) |
| MTZ + Furosemide (n = 64) | -18 ± 73 | -1.2 ± 5.3 | -0.3 ± 0.6 | +2.6 ± 5.6 | 25 (39) | 11 (17) | |
| Ng et al[28], 2013 | MTZ + Furosemide (n = 42) | +2.7 ± 28 | - | - | - | 18 (43) | 15 (35) |
| Shulenberger et al[29], 2016 | CTZ + Furosemide (n = 40) | +8.8 ± 27 | +0.1 ± 2.3 | - | - | 2 (5)2 | 34 (85)3 |
| MTZ + Furosemide (n = 38) | +18 ± 35 | -0.7 ± 3.1 | - | - | 2 (5)2 | 27 (71)3 | |
| Vánky et al[26], 1997 | HCTZ + Amiloride + Furosemide (n = 20) | -2.0 ± 7.1 | - | - | - | - | - |
| Furosemide (n = 57) | -2.0 ± 7.6 | - | - | - | - | - | |
| Carbonic anhydrase inhibitor | |||||||
| Heming et al[24], 2011 | Acetazo + Furosemide (n = 29) | +4.3 ± 9.4 | - | -0.3 ± 0.4 | -3.6 ± 5.1 | - | 9 (31) |
| Imiela and Budaj[25], 2017 | Acetazo + Furosemide (n = 10) | - | - | - | - | - | - |
| Furosemide (n = 10) | - | - | - | - | - | - | |
The risk of all other adverse (safety) events, where definitions and follow-up varied across included studies, are reported in Supplementary Table 6. Notably, hypokalemia was documented in 6 studies and ranged from 0% to 85%, while hyponatremia was documented in 4 studies and ranged from 0% to 43% when combining a thiazide with a loop-diuretic. No study reported arrythmia or ototoxicity events.
To our knowledge, this is the most comprehensive systematic review and meta-analysis to address the clinical efficacy and safety of various diuretic combinations in the context of patients hospitalised at the ICU with fluid overload and respiratory failure. A significant increase in the 24-h urine output leading to a negative fluid balance was observed in the pooled analyses, mainly attributed to the thiazide-furosemide combination. Reporting of other clinical endpoints including the efficacy, safety, and clinical outcomes of groups treated with each combination was inconsistent and generally incomplete.
Currently, strategies to manage fluid balance in critically ill patients with acute lung injury and other causes of respiratory failure include fluid restriction but this may be difficult given the requirement of fluid for carriers for vasopressors, antibiotics, and nutrition. A preferred option is augmenting urine output with diuretics. In addition, positive sodium balance specifically, rather than simple fluid balance, has recently been associated with respiratory dysfunction in mechanically ventilated patients[30,31], and with worsening prognosis in decompensated heart failure[32]. Ensuring adequate negative sodium balance along with increased urine output may be crucial to optimising extracellular fluid volume and outcomes. This approach is now endorsed by the European Society of Cardiology[33]. Also, as recently confirmed by the STARRT-AKI trial, delaying initiation of KRT based on a watchful waiting approach (in the absence of emergency indications for RRT initiation) can be beneficial by reducing RRT complications including prolonged KRT requirement[34]. Therefore, refining the ways to achieve a negative fluid balance with a diuretic combination strategy might potentially delay or avoid the need for RRT initiation (including ultrafiltration) to treat volume overload and control fluid balance in patients with loop-diuretic resistance.
The mechanisms of resistance to furosemide and other loop diuretics is multifactorial[35]. They include a decrease in sodium delivery to the site of action by systemic and renal hypoperfusion[36], as well as an increase in sodium and water retention due to neurohormonal, renin-angiotensin-aldosterone and antidiuretic hormone systems activation in critically ill patients. In addition, proximal tubular injury or loss in AKI or CKD results in diminished loop diuretic secretion into the tubular lumen and reduced effects more distally in the thick ascending limb of Henle’s loop, while in chronic exposure to furosemide, adaptive changes in the nephron occur with hypertrophy of the distal tubule leading to an increase of its reabsorptive capacity[37]. For patients who do not respond to an increasing dose of furosemide, sequential nephron blockade of sodium reabsorption with other classes of diuretics can overcome these resistance mechanisms[16], which was confirmed in the current review focusing on patients with AHRF.
In order to promote liberation from mechanical ventilation in patients with metabolic alkalosis and associated hypoventilation, normalisation of the acid-base state while improving fluid balance with acetazolamide has also been investigated[38-40]. Also, the combination of an aldosterone receptor antagonist with furosemide is recommended as first line therapy in cirrhotic patients with ascites[41], due to the efficacy of that combination to promote natriuresis while minimising the risk of hypokalemia. This combination is also widely recommended in the management of patients with chronic heart failure and has been shown to reduce morbidity and mortality in patients with reduced ejection fraction[42].
In this review, various factors may explain the limited efficacy of these combinations to promote diuresis and a negative fluid balance in some included studies. First, the dose of furosemide was not maximised for most studies, unlike recent RCTs on acute heart failure[12]. Indeed, the studies with higher median daily doses of furosemide were associated with higher and significant increases in urine output, even before addition of the second diuretic[23,29], which was also confirmed in previous cohorts[16]. On the other hand, the use of sub-maximal doses of multiple drugs in combination may additively or synergistically augment efficacy, while avoiding the adverse effects of higher doses of these drugs. Secondly, in the context of respiratory failure, the total negative fluid balance required to improve respiratory parameters may be less than the diuresis desired in patients with acute heart failure, in which the cumulative volume overload is usually greater[1]. As this review focused on the net fluid balance achieved instead of respiratory outcomes, it is still possible that the limited diuresis observed for these patients was judged as clinically sufficient to maintain an even fluid balance (rather than targeting negative fluid balance), as opposed to a fluid-liberal approach[7]. Also, none of these studies reported the use of an integrated tool, such as point-of-care ultrasound, bioimpedance, or other hemodynamic and volume measures[3], to evaluate the volume status of these patients, once again limiting the capacity to determine if the urine output achieved was adequate to optimise volume status.
All diuretic agents have a safety profile that varies according to their intrinsic mechanism of action. This review showed that combination of acetazolamide and furosemide may reduce serum bicarbonate and induce potassium loss, causing hypokalemia in up to 31% of patients[24] after only 24 h of treatment. In contrast, when furosemide is combined with thiazides, a trend toward an increase in bicarbonate and lower potassium levels was observed, reflecting the greater natriuretic and kaliuretic effects of reabsorption blockade in sequential nephron segments. The rate of hypokalemia was considerable, emphasizing the need to regularly monitor electrolyte levels, acid-base parameters, and kidney function (which is under-reported in this literature) when choosing such combinations. The role of potassium-sparing diuretics in the prevention of hypokalemia with aggressive diuretic regimens warrants further research.
In sum, this study brings new data on the use of diuretic combinations in the subgroup of ICU patients with AHRF, which has never been systematically reported before. The pooled analysis confirmed an increased efficacy regarding urine output and net fluid balance, which is interesting in a clinical setting, but also brings relevant data on the potential risk of substantial electrolyte disturbances in patients exposed to these combinations. Indeed, the study also confirms the need for additional lab monitoring when prescribing such combinations especially if no pre-emptive electrolytes administration is planned.
There are several limitations to the current systematic review. First, no study reported the pre-planned endpoint of cumulative fluid balance, which required us to deviate from the original protocol and to use the daily fluid balance as primary outcome. Also, no study reported the use of ENaC inhibitors alone (e.g. triamterene, amiloride) in conjunction with furosemide, which did not allow this review to evaluate that combination. This highlights the importance of future studies using ENaC inhibitors in combination with loop-diuretics in the management of respiratory failure. In addition, the literature strategy was limited to generic name. The limited duration of these interventional periods, from 24 to 96 h, may not have substantially affected clinical outcomes such as in-hospital mortality, ICU length-of-stay and ventilation-free survival, which were only partially reported in these studies. Most importantly, the heterogeneity across all included studies was high, including for diuretics doses, renal function, reasons of ICU admission with notable inconsistencies in clinical endpoints reporting. We contacted corresponding authors of all included references to confirm eligibility criteria, but we cannot independently confirm with certainty that all included patients were on mechanical ventilation or required high oxygen volume as some did not respond. Finally, the risk of publication bias is significant, since only limited data has been published in the context of critically ill patients receiving such diuretic strategies.
In critically ill patients with respiratory failure receiving a loop diuretic, we showed that addition of another class of diuretic is associated with an increased 24-h urine output leading to a negative fluid balance, where the thiazide and loop-diuretic combination had the higher efficacy. However, given the significant heterogeneity, the risk of publication bias and the lack of adequately powered RCTs, no definitive evidence can be drawn, especially for non-thiazide combinations. In addition, electrolytes disturbance secondary to the use of these adjunctive diuretics in combination with a loop diuretic warrants additional monitoring to ensure their safety. This limited evidence emphasizes the need for further high-quality trials investigating the efficacy, safety profile and clinical outcomes of such therapeutic interventions for patients with respiratory failure requiring diuretics to control fluid balance.
Diuretics are essential to maintain fluid balance in patients admitted to intensive care units (ICUs). However, resistance to loop-diuretics is common and diuretic combinations are often used in order to mitigate this resistance.
As opposed to patients with heart failure where combinations of different classes of diuretics have been extensively studied and are now recommended, the body of evidence regarding diuretic combinations in ICU patients with hypoxemic respiratory failure is scarce.
This study systematically reviewed the efficacy and safety of common diuretics combinations in ICU patients with respiratory failure when compared to loop-diuretics in monotherapy.
A systematic review and meta-analysis were performed. A pooled analysis of the mean difference for the 24-h urine output and the 24-h fluid balance between loop-diuretics in monotherapy and common diuretics combinations (thiazides, carbonic anhydrase inhibitors and mineralocorticoid antagonists) was performed. Descriptive statistics were used to report the occurrence of safety events, such as electrolyte disturbances, hypotension and acute kidney injury.
From 6510 citations, nine studies totalling 440 patients were included. When compared to loop diuretics alone, the addition of a second diuretic is associated with an improved negative fluid balance at 24 h mean differences (MD) of -1.06 L [95% confidence interval (CI): -1.46; -0.65], mainly driven by the combination of a thiazide plus furosemide [MD: -1.25 L (95%CI: -1.68; -0.82)]. The heterogeneity on the report of clinical and safety endpoints was high, but electrolytes anomalies were frequent and confirms the need for additional monitoring when prescribing such combinations.
Larger trials are required to confirm the efficacy and safety of diuretic combinations in this population. However, based on limited evidence the combination of thiazide plus loop-diuretics is associated with an increase in urine output and negative fluid balance.
The study has highlighted the paucity of data on the optimal strategy to optimise fluid balance in patients with respiratory failure and relative diuretics resistance.
The authors would like to thank Diarmuid Stokes, biomedical librarian, University College Dublin, for his assistance with the systematic review search. The authors would also like to thank Dr Nicholas Heming, Georges Pompidou Hospital, and his team to have agreed to share the data required for the reanalysis of the subgroup of patients receiving the combination of diuretics. The authors would also like to thank Dr. Brent N. Reed, University of Maryland, Baltimore, and his team to have agreed to share the data required for the reanalysis of the subgroup of patients admitted to the ICU.
| 1. | Bouchard J, Soroko SB, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, Mehta RL; Program to Improve Care in Acute Renal Disease (PICARD) Study Group. Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int. 2009;76:422-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 702] [Cited by in RCA: 722] [Article Influence: 42.5] [Reference Citation Analysis (0)] |
| 2. | Grams ME, Estrella MM, Coresh J, Brower RG, Liu KD; National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome Network. Fluid balance, diuretic use, and mortality in acute kidney injury. Clin J Am Soc Nephrol. 2011;6:966-973. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 306] [Cited by in RCA: 277] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 3. | Claure-Del Granado R, Mehta RL. Fluid overload in the ICU: evaluation and management. BMC Nephrol. 2016;17:109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 194] [Cited by in RCA: 229] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 4. | Liu KD, Thompson BT, Ancukiewicz M, Steingrub JS, Douglas IS, Matthay MA, Wright P, Peterson MW, Rock P, Hyzy RC, Anzueto A, Truwit JD; National Institutes of Health National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome Network. Acute kidney injury in patients with acute lung injury: impact of fluid accumulation on classification of acute kidney injury and associated outcomes. Crit Care Med. 2011;39:2665-2671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 270] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 5. | Sakr Y, Vincent JL, Reinhart K, Groeneveld J, Michalopoulos A, Sprung CL, Artigas A, Ranieri VM; Sepsis Occurence in Acutely Ill Patients Investigators. High tidal volume and positive fluid balance are associated with worse outcome in acute lung injury. Chest. 2005;128:3098-3108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 280] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 6. | Schuller D, Mitchell JP, Calandrino FS, Schuster DP. Fluid balance during pulmonary edema. Is fluid gain a marker or a cause of poor outcome? Chest. 1991;100:1068-1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 130] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 7. | National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network. , Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354:2564-2575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2310] [Cited by in RCA: 2349] [Article Influence: 117.5] [Reference Citation Analysis (0)] |
| 8. | McCoy IE, Chertow GM, Chang TI. Patterns of diuretic use in the intensive care unit. PLoS One. 2019;14:e0217911. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Neuberg GW, Miller AB, O'Connor CM, Belkin RN, Carson PE, Cropp AB, Frid DJ, Nye RG, Pressler ML, Wertheimer JH, Packer M; PRAISE Investigators. Prospective Randomized Amlodipine Survival Evaluation. Diuretic resistance predicts mortality in patients with advanced heart failure. Am Heart J. 2002;144:31-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 268] [Cited by in RCA: 273] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 10. | Rosenberg J, Gustafsson F, Galatius S, Hildebrandt PR. Combination therapy with metolazone and loop diuretics in outpatients with refractory heart failure: an observational study and review of the literature. Cardiovasc Drugs Ther. 2005;19:301-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 101] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 11. | Brisco-Bacik MA, Ter Maaten JM, Houser SR, Vedage NA, Rao V, Ahmad T, Wilson FP, Testani JM. Outcomes Associated With a Strategy of Adjuvant Metolazone or High-Dose Loop Diuretics in Acute Decompensated Heart Failure: A Propensity Analysis. J Am Heart Assoc. 2018;7:e009149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 69] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 12. | Cox ZL, Hung R, Lenihan DJ, Testani JM. Diuretic Strategies for Loop Diuretic Resistance in Acute Heart Failure: The 3T Trial. JACC Heart Fail. 2020;8:157-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 129] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 13. | Felker GM, Ellison DH, Mullens W, Cox ZL, Testani JM. Diuretic Therapy for Patients With Heart Failure: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;75:1178-1195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 293] [Article Influence: 48.8] [Reference Citation Analysis (0)] |
| 14. | Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, Drazner MH, Filippatos GS, Fonarow GC, Givertz MM, Hollenberg SM, Lindenfeld J, Masoudi FA, McBride PE, Peterson PN, Stevenson LW, Westlake C. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136:e137-e161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1590] [Cited by in RCA: 2041] [Article Influence: 226.8] [Reference Citation Analysis (0)] |
| 15. | Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; Authors/Task Force Members; Document Reviewers. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18:891-975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4368] [Cited by in RCA: 5010] [Article Influence: 501.0] [Reference Citation Analysis (4)] |
| 16. | Côté JM, Bouchard J, Murray PT, Beaubien-Souligny W. Diuretic strategies in patients with resistance to loop-diuretics in the intensive care unit: A retrospective study from the MIMIC-III database. J Crit Care. 2021;65:282-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6253] [Cited by in RCA: 7899] [Article Influence: 464.6] [Reference Citation Analysis (3)] |
| 18. | Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, Emberson JR, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6581] [Cited by in RCA: 19031] [Article Influence: 2718.7] [Reference Citation Analysis (0)] |
| 19. | Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7683] [Cited by in RCA: 12684] [Article Influence: 1268.4] [Reference Citation Analysis (2)] |
| 20. | Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3433] [Cited by in RCA: 8104] [Article Influence: 675.3] [Reference Citation Analysis (0)] |
| 21. | Apte Y, Bellomo R, Warrillow S, Goldsmith D, Gillies M, McGain F. Pilot randomised double-blind controlled trial of high-dose spironolactone in critically ill patients receiving a frusemide infusion. Crit Care Resusc. 2008;10:306-311. [PubMed] |
| 22. | Bihari S, Holt AW, Prakash S, Bersten AD. Addition of indapamide to frusemide increases natriuresis and creatinine clearance, but not diuresis, in fluid overloaded ICU patients. J Crit Care. 2016;33:200-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Michaud CJ, Mintus KC. Intravenous Chlorothiazide Versus Enteral Metolazone to Augment Loop Diuretic Therapy in the Intensive Care Unit. Ann Pharmacother. 2017;51:286-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Heming N, Faisy C, Urien S. Population pharmacodynamic model of bicarbonate response to acetazolamide in mechanically ventilated chronic obstructive pulmonary disease patients. Crit Care. 2011;15:R213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Imiela T, Budaj A. Acetazolamide as Add-on Diuretic Therapy in Exacerbations of Chronic Heart Failure: a Pilot Study. Clin Drug Investig. 2017;37:1175-1181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (2)] |
| 26. | Vánky F, Broquist M, Svedjeholm R. Addition of a thiazide: an effective remedy for furosemide resistance after cardiac operations. Ann Thorac Surg. 1997;63:993-997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 27. | Bohn BC, Hadgu RM, Pope HE, Shuster JE. Oral Metolazone Versus Intravenous Chlorothiazide as an Adjunct to Loop Diuretics for Diuresis in Acute Decompensated Heart Failure With Reduced Ejection Fraction. Hosp Pharm. 2019;54:351-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 28. | Ng TM, Konopka E, Hyderi AF, Hshieh S, Tsuji Y, Kim BJ, Han SY, Phan DH, Jeng AI, Lou M, Elkayam U. Comparison of bumetanide- and metolazone-based diuretic regimens to furosemide in acute heart failure. J Cardiovasc Pharmacol Ther. 2013;18:345-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 29. | Shulenberger CE, Jiang A, Devabhakthuni S, Ivaturi V, Liu T, Reed BN. Efficacy and Safety of Intravenous Chlorothiazide vs Oral Metolazone in Patients with Acute Decompensated Heart Failure and Loop Diuretic Resistance. Pharmacotherapy. 2016;36:852-860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 30. | Bihari S, Peake SL, Prakash S, Saxena M, Campbell V, Bersten A. Sodium balance, not fluid balance, is associated with respiratory dysfunction in mechanically ventilated patients: a prospective, multicentre study. Crit Care Resusc. 2015;17:23-28. [PubMed] |
| 31. | Bihari S, Baldwin CE, Bersten AD. Fluid balance does not predict estimated sodium balance in critically ill mechanically ventilated patients. Crit Care Resusc. 2013;15:89-96. [PubMed] |
| 32. | Hodson DZ, Griffin M, Mahoney D, Raghavendra P, Ahmad T, Turner J, Wilson FP, Tang WHW, Rao VS, Collins SP, Mullens W, Testani JM. Natriuretic Response Is Highly Variable and Associated With 6-Month Survival: Insights From the ROSE-AHF Trial. JACC Heart Fail. 2019;7:383-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 87] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 33. | Mullens W, Damman K, Harjola VP, Mebazaa A, Brunner-La Rocca HP, Martens P, Testani JM, Tang WHW, Orso F, Rossignol P, Metra M, Filippatos G, Seferovic PM, Ruschitzka F, Coats AJ. The use of diuretics in heart failure with congestion - a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2019;21:137-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 868] [Cited by in RCA: 783] [Article Influence: 111.9] [Reference Citation Analysis (0)] |
| 34. | STARRT-AKI Investigators; Canadian Critical Care Trials Group; Australian and New Zealand Intensive Care Society Clinical Trials Group; United Kingdom Critical Care Research Group; Canadian Nephrology Trials Network; Irish Critical Care Trials Group, Bagshaw SM, Wald R, Adhikari NKJ, Bellomo R, da Costa BR, Dreyfuss D, Du B, Gallagher MP, Gaudry S, Hoste EA, Lamontagne F, Joannidis M, Landoni G, Liu KD, McAuley DF, McGuinness SP, Neyra JA, Nichol AD, Ostermann M, Palevsky PM, Pettilä V, Quenot JP, Qiu H, Rochwerg B, Schneider AG, Smith OM, Thomé F, Thorpe KE, Vaara S, Weir M, Wang AY, Young P, Zarbock A. Timing of Initiation of Renal-Replacement Therapy in Acute Kidney Injury. N Engl J Med. 2020;383:240-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 447] [Cited by in RCA: 461] [Article Influence: 76.8] [Reference Citation Analysis (0)] |
| 35. | McMahon BA, Chawla LS. The furosemide stress test: current use and future potential. Ren Fail. 2021;43:830-839. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 40] [Reference Citation Analysis (0)] |
| 36. | Hoorn EJ, Ellison DH. Diuretic Resistance. Am J Kidney Dis. 2017;69:136-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 94] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 37. | Loon NR, Wilcox CS, Unwin RJ. Mechanism of impaired natriuretic response to furosemide during prolonged therapy. Kidney Int. 1989;36:682-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 136] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 38. | Gulsvik R, Skjørten I, Undhjem K, Holø L, Frostad A, Saure EW, Lejlic V, Humerfelt S, Hansen G, Bruun Wyller T. Acetazolamide improves oxygenation in patients with respiratory failure and metabolic alkalosis. Clin Respir J. 2013;7:390-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 39. | Faisy C, Mokline A, Sanchez O, Tadié JM, Fagon JY. Effectiveness of acetazolamide for reversal of metabolic alkalosis in weaning COPD patients from mechanical ventilation. Intensive Care Med. 2010;36:859-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 40. | Berthelsen P, Gøthgen I, Husum B, Jacobsen E. Oxygen uptake and carbon dioxide elimination after acetazolamide in the critically ill. Intensive Care Med. 1985;11:26-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 41. | European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53:397-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1125] [Cited by in RCA: 1161] [Article Influence: 72.6] [Reference Citation Analysis (10)] |
| 42. | Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:e147-e239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4116] [Cited by in RCA: 4727] [Article Influence: 363.6] [Reference Citation Analysis (1)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Critical care medicine
Country/Territory of origin: Canada
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Luo ZW, China; Yang X, China S-Editor: Fan JR L-Editor: A P-Editor: Fan JR