Published online Mar 9, 2022. doi: 10.5492/wjccm.v11.i2.102
Peer-review started: October 4, 2021
First decision: December 9, 2021
Revised: December 21, 2021
Accepted: February 23, 2022
Article in press: February 23, 2022
Published online: March 9, 2022
Processing time: 149 Days and 9.7 Hours
The coronavirus disease 2019 (COVID-19) course may be affected by environmental factors. Ecological studies previously suggested a link between climatological factors and COVID-19 fatality rates. However, individual-level impact of these factors has not been thoroughly evaluated yet.
To study the association of climatological factors related to patient location with unfavorable outcomes in patients.
In this observational analysis of the Society of Critical Care Medicine Discovery Viral Infection and Respiratory Illness Universal Study: COVID-19 Registry cohort, the latitudes and altitudes of hospitals were examined as a covariate for mortality within 28 d of admission and the length of hospital stay. Adjusting for baseline parameters and admission date, multivariable regression modeling was utilized. Generalized estimating equations were used to fit the models.
Twenty-two thousand one hundred eight patients from over 20 countries were evaluated. The median age was 62 (interquartile range: 49-74) years, and 54% of the included patients were males. The median age increased with increasing latitude as well as the frequency of comorbidities. Contrarily, the percentage of comorbidities was lower in elevated altitudes. Mortality within 28 d of hospital admission was found to be 25%. The median hospital-free days among all included patients was 20 d. Despite the significant linear relationship between mortality and hospital-free days (adjusted odds ratio (aOR) = 1.39 (1.04, 1.86), P = 0.025 for mortality within 28 d of admission; aOR = -1.47 (-2.60, -0.33), P = 0.011 for hospital-free days), suggesting that adverse patient outcomes were more common in locations further away from the Equator; the results were no longer significant when adjusted for baseline differences (aOR = 1.32 (1.00, 1.74), P = 0.051 for 28-day mortality; aOR = -1.07 (-2.13, -0.01), P = 0.050 for hospital-free days). When we looked at the altitude’s effect, we discovered that it demonstrated a non-linear association with mortality within 28 d of hospital admission (aOR = 0.96 (0.62, 1.47), 1.04 (0.92, 1.19), 0.49 (0.22, 0.90), and 0.51 (0.27, 0.98), for the altitude points of 75 MASL, 125 MASL, 400 MASL, and 600 MASL, in comparison to the reference altitude of 148 m.a.s.l, respectively. P = 0.001). We detected an association between latitude and 28-day mortality as well as hospital-free days in this worldwide study. When the baseline features were taken into account, however, this did not stay significant.
Our findings suggest that differences observed in previous epidemiological studies may be due to ecological fallacy rather than implying a causal relationship at the patient level.
Core Tip: We detected an association between latitude and mortality within 28 d of admission and hospital-free days in this worldwide study. When the baseline features were taken into account, however, this did not stay significant. Our findings suggest that differences observed in previous epidemiological studies may be due to ecological fallacy rather than implying a causal relationship at the patient level.
- Citation: Tekin A, Qamar S, Singh R, Bansal V, Sharma M, LeMahieu AM, Hanson AC, Schulte PJ, Bogojevic M, Deo N, Zec S, Valencia Morales DJ, Belden KA, Heavner SF, Kaufman M, Cheruku S, Danesh VC, Banner-Goodspeed VM, St Hill CA, Christie AB, Khan SA, Retford L, Boman K, Kumar VK, O'Horo JC, Domecq JP, Walkey AJ, Gajic O, Kashyap R, Surani S, The Society of Critical Care Medicine (SCCM) Discovery Viral Infection and Respiratory Illness Universal Study (VIRUS): COVID-19 Registry Investigator Group. Association of latitude and altitude with adverse outcomes in patients with COVID-19: The VIRUS registry. World J Crit Care Med 2022; 11(2): 102-111
- URL: https://www.wjgnet.com/2220-3141/full/v11/i2/102.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v11.i2.102
After being identified at the end of 2019, Coronavirus disease 2019 (COVID-19) rapidly disseminated worldwide and affected millions[1,2]. Although studies have shown the efficacy of some medications or the impact of certain conditions on the disease process[3-8], there are still unknown factors that affect the patient outcomes. The investigation of the relationship of disease severity with different environmental settings might provide better insight into the pathogenesis of COVID-19.
A link between climatological factors and Coronavirus Disease 2019 (COVID-19) fatality rates was previously suggested by ecological studies[9-13]. Geographic factors were also demonstrated to impact other respiratory infection processes[14,15]. However, these studies may be subject to the ecological fallacy, in which grouped population-level associations are not observed at the individual level[16]. Large-scale, patient-level cohort studies have thus far not evaluated associations between factors such as altitude and latitude with COVID-19 severity.
The Society of Critical Care Medicine Discovery Viral Infection and Respiratory Illness Universal Study (VIRUS): COVID-19 registry[17-19] is a global collaboration of partners from 27 countries that provides a novel resource for the investigation of associations between altitude and latitude, with outcomes of individuals with COVID-19, allowing adjustment for baseline factors to evaluate the relationship between COVID-19 disease severity and geographical factors. Using this large cohort, we targeted to assess the relationship of altitude and latitude with unfavorable patient outcomes.
This study was conducted on the data collected within the scope of the VIRUS: COVID-19 registry. The project was approved as exempt by the institutional review board at Mayo Clinic (IRB:20-002610). Clinical Trials Database registration number for the registry is NCT04323787.
All subjects hospitalized with a COVID-19 associated indication (laboratory-confirmed or clinically diagnosed infection) at participating institutions were eligible for inclusion in the VIRUS: COVID-19 registry[20]. The exclusion criteria for the VIRUS Registry study are non-COVID-19 related admissions, Minnesota patients who have not provided research authorization, and readmissions of already included patients. De-identified data were collected through Research Electronic Data Capture software (REDCap, version 8.11.11, Vanderbilt University, Nashville, Tennessee) and stored in a central database hosted by Mayo Clinic[21].
Regarding the analysis for this particular study, all adult subjects admitted between March 15, 2020, and January 15, 2021, were screened for inclusion. Although enrolled in the VIRUS: COVID-19 registry, we excluded pediatric patients (< 18 years old) from this project. Another exclusion criterion was patients enrolled from institutions reporting fewer than 65% of subjects with hospital discharge status. Since those participating centers were unlikely to represent a realistic distribution of outcomes, they were omitted as non-participating. After the application of exclusion criteria, patients of 143 participating hospitals in 21 countries were found to be eligible for inclusion. Detailed inclusion and exclusion criteria for the VIRUS Registry and this project is provided in Supplementary Figure 1.
The patients' residential addresses at the time of diagnosis were not accessible due to the de-identified database. As a surrogate, the location of the participating institutions, which was available for all enrolled patients, was used to determine geographical variables. Latitude and altitude information was retrieved from the Google Earth software[22]. Based on their locations, subjects were grouped according to the elevation above the sea level and the distance from the Equator, regardless of the hemisphere of location[23,24]. Baseline information and disease-related specifics were gathered from the VIRUS Registry.
The primary outcome was mortality within 28 d of admission, and the secondary outcome was length of hospital stay. The variable "hospital-free days" (HFD) was used to analyze the impact on hospital length of stay[25], calculated by subtracting the number of admission days from 28; which was 0 for patients who died in the hospital or stayed in the hospital for longer than 28 d. Both outcomes were evaluated independently.
The statistical methodology was reviewed by our co-authors from the Division of Clinical Trials and Biostatistics, Department of Quantitative Health Sciences, Mayo Clinic, Rochester.
The median and interquartile range (IQR) were used to summarize continuous data. Categorical variables were reported as numbers and percentages. Unadjusted and multivariable-adjusted logistic regression assessed the association with outcomes. To account for the clustering of patients within sites, models were fitted using generalized estimating equations using an exchangeable working correlation for individual hospitals. When the results indicated a non-linear functional structure, they were graphically summarized using the restricted cubic spline fit; otherwise, the linear relationship was defined. Age, gender, race, body mass index, number of days with symptoms prior to admission, symptom groups, the timing of admission with regards to the start of the pandemic, and comorbidities were factored into the models. Unadjusted and multivariable linear regression models assessed the association with HFD using a similar approach. Odds ratios (OR) and 95% confidence intervals for the mortality endpoint were determined per 10-degrees of latitude and 250-meters of altitude in relation to the median reference points, i.e., 39° and 148 meters above sea-level (MASL), respectively. For HFD, the estimate is the expected difference in mean days, similarly displayed per 10 degrees of latitude and 250 meters of altitude.
For missing data among included institutions and patients, multiple imputations assuming data were missing at random using fully conditional specification with 100 imputations was used to impute missing covariates or outcomes. Analyses were performed on each dataset, and results combined to reflect uncertainty due to missingness. Without correcting for multiplicity related to testing the outcomes or testing both altitude and latitude in regression models, statistical significance was specified as P < 0.05.
After exclusion of “non-participating sites,” 23210 patients with complete data enrolled in the VIRUS registry were evaluated. Among those, 22108 met eligibility criteria after excluding pediatric patients (Supplementary Figure 2, Supplementary Table 1). The median age was 62 (IQR 49-74) years, with 54% males. Among the subjects, 51% of the included were White, 26% were Black, and 65% of the patients were non-Hispanic; 86% had at least one comorbid condition, hypertension (46%) being the most prevalent. When baseline data were analyzed within latitude and altitude groups, patients were more often older on high-latitude locations (locations farther from the Equator). The frequency of patients with comorbidities and the proportion of females also increased with latitude. At higher altitudes, however, females and patients with comorbidities were less prevalent (Table 1).
| Variables | Total (n = 22108) | Latitude | Altitude | |||||
| 0-15° (n = 589) | 16-30° (n = 1961) | 31-45° (n = 19163) | 46-60° (n = 395) | < 500 MASL (n = 21122) | 500 - 1000 MASL (n = 765) | > 1000 MASL (n = 221) | ||
| Age, median, IQR | 62 (49-74) | 50 (36-62) | 59 (47-70) | 62 (49-74) | 72 (59-83) | 62 (59-74) | 58 (46-69) | 60 (49-71) |
| Gender | ||||||||
| Female | 9804 (44%) | 198 (34%) | 797 (41%) | 8626 (46%) | 183 (46%) | 9476 (45%) | 255 (33%) | 73 (33%) |
| Male | 12025 (54%) | 391 (66%) | 1163 (59%) | 10259 (54%) | 212 (54%) | 11367 (55%) | 510 (67%) | 148 (67%) |
| Race | ||||||||
| White | 11210 (51%) | 2 (0%) | 471 (24%) | 10449 (55%) | 288 (73%) | 10928 (52%) | 227 (30%) | 55 (25%) |
| African American | 5757 (26%) | 74 (13%) | 505 (26%) | 5145 (27%) | 33 (8%) | 5738 (27%) | 17 (2%) | 2 (1%) |
| Mixed race | 785 (4%) | 164 (28%) | 119 (6%) | 501 (3%) | 1 (0%) | 524 (2%) | 129 (17%) | 132 (60%) |
| Asian American | 416 (2%) | - | 9 (0%) | 398 (2%) | 9 (2%) | 412 (2%) | 4 (1%) | 0 (0%) |
| Others | 3940 (18%) | 349 (59%) | 857 (44%) | 2670 (14%) | 61 (15%) | 3122 (15%) | 371 (48%) | 32 (1%) |
| Ethnicity | ||||||||
| Hispanic | 4592 (21%) | 88 (15%) | 313 (16%) | 4185 (22%) | 6 (2%) | 4322 (20%) | 197 (26%) | 73 (33%) |
| Non-Hispanic | 14411 (65%) | 354 (60%) | 1250 (64%) | 12571 (66%) | 236 (60%) | 14073 (67%) | 281 (37%) | 57 (26%) |
| BMI | 29.0 (25, 35) | 26.7 (24, 28) | 28.0 (25, 34) | 29.3 (25, 35) | 26.7 (23, 32) | 29.0 (25, 35) | 28.6 (26, 33) | 28 (26, 32) |
| Comorbidities (any) | 18991 (86%) | 295 (50%) | 1580 (81%) | 16753 (87%) | 363 (92%) | 18262 (86%) | 578 (76%) | 151 (68%) |
| Hypertension | 10267 (46%) | 191 (32%) | 1050 (54%) | 8785 (46%) | 241 (61%) | 9865 (47%) | 322 (42%) | 80 (36%) |
| Diabetes | 6473 (29%) | 134 (23%) | 738 (38%) | 5474 (29%) | 127 (32%) | 6163 (29%) | 256 (33%) | 54 (24%) |
| Coronary artery disease | 4124 (19%) | 29 (5%) | 338 (17%) | 3678 (19%) | 79 (20%) | 4017 (19%) | 87 (11%) | 20 (9%) |
| Obesity | 3794 (17%) | 34 (6%) | 394 (20%) | 3304 (17%) | 62 (16%) | 3640 (17%) | 125 (16%) | 29 (13%) |
| Dyslipidemia | 3521 (16%) | 7 (1%) | 315 (16%) | 3168 (17%) | 31 (8%) | 3422 (16%) | 87 (11%) | 12 (5%) |
| Chronic kidney disease | 2609 (12%) | 5 (1%) | 233 (12%) | 2295 (12%) | 76 (19%) | 2543 (12%) | 56 (7%) | 10 (5%) |
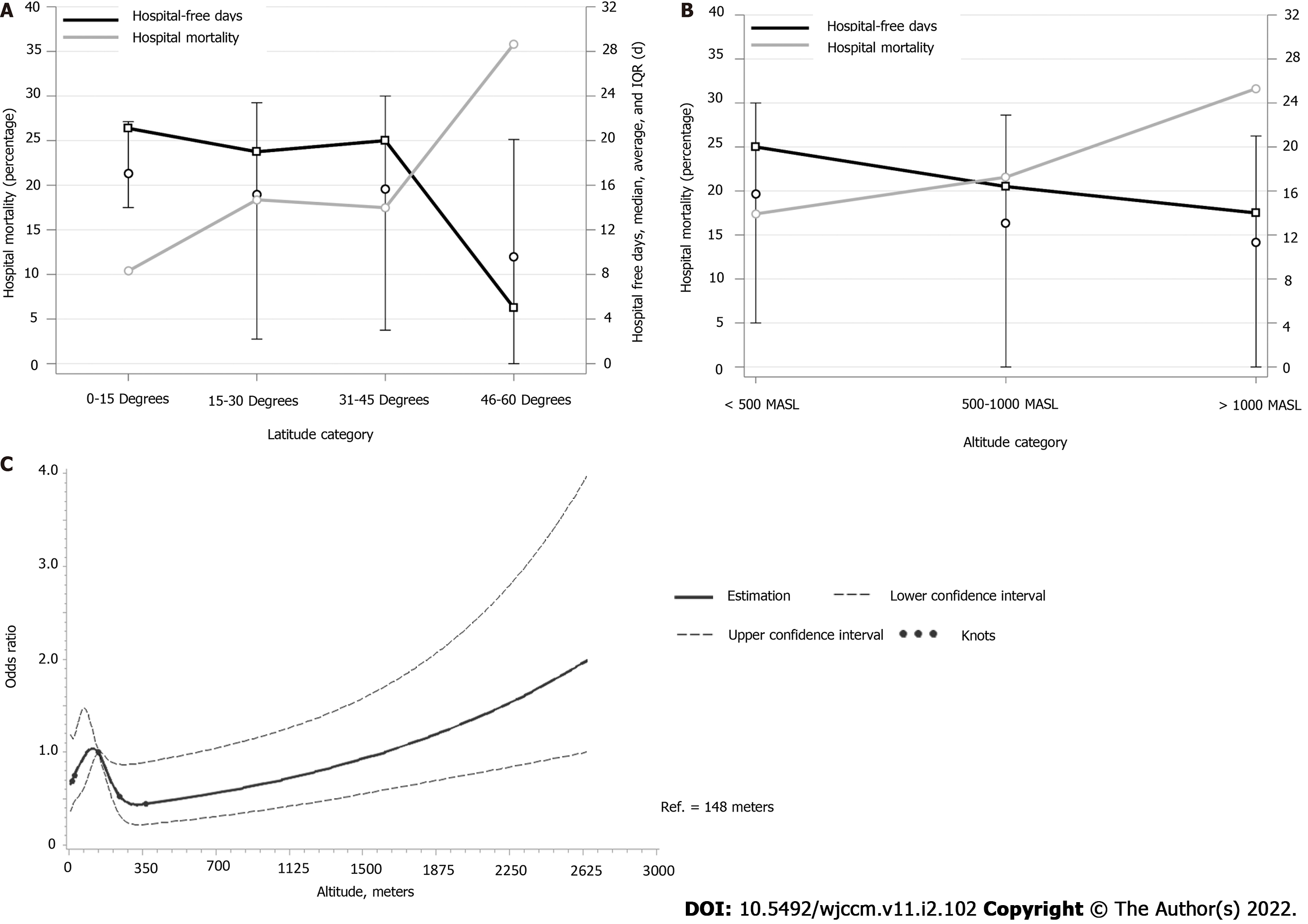
A total of 3451 patients (25% of 13,959 patients with mortality data available) died within 28 d following admission. The median HFD for the general study population was 20 (IQR 3.0-24.0) days. The 28-day mortality rate was higher in higher-latitude locations. Mortality rates were also higher for patients hospitalized in higher altitudes. Additionally, the median HFD was lower for higher latitude and altitude levels (Figure 1).
The unadjusted analysis showed a significant linear association of higher latitude locations associated with increased mortality (OR = 1.39, 95%CI = 1.04, 1.86, P = 0.025) and lower number of HFD (Estimate = -1.47, 95%CI = -2.60, -0.33, P = 0.011) per 10 (degree) latitude. However, after adjustment to the baseline characteristics, there was insufficient evidence to indicate a significant association with both outcomes (adjusted OR (aOR) = 1.32, 95%CI = 1.00, 1.74, P = 0.051 for mortality, and adjusted Estimate = -1.07, 95%CI = -2.13, -0.01, P = 0.050 for HFD) (Table 2).
| Study outcomes | Latitude | Altitude | ||||||||||
| Unadjusted | Adjusted | Unadjusted | Adjusted | |||||||||
| Estimate | 95%CI | P value | Estimate | 95%CI | P value | Estimate | 95%CI | P value | Estimate | 95%CI | P value | |
| 28 d mortality | 1.39 | (1.04, 1.86) | 0.025 | 1.32 | (1.00, 1.74) | 0.051 | RCS, P value non-linearity ≤ 0.001, P value overall association = 0.001 | RCS, P value non-linearity = 0.049, P value overall association = 0.017 | ||||
| Hospital-free days | -1.47 | (-2.60, | 0.011 | -1.07 | (-2.13, | 0.050 | 0.14 | (-0.37, 0.64) | 0.587 | 0.10 | (0.37, 0.56) | 0.683 |
When evaluating the impact of higher altitudes on adverse outcomes, there was a non-linear association with mortality, which remained significant after adjustment (aOR and 95%CIs for the altitude points of 400 MASL and 600 MASL, compared to the reference altitude of 148 MASL were 0.49 (0.22, 0.90), and 0.51 (0.27,0.98), respectively, P = 0.017) (Table 2). The odds of fatal disease course slightly increased at altitude levels between 125 and 145 MASL; decreased to the lowest around the altitude of 350 MASL, and gradually increased after that point with the increasing altitude (Figure 1C). No association was present with HFD and altitude levels either before or after adjustment.
We reported the distribution of patient outcomes to different altitudes and latitudes within an international COVID-19 registry. In our study, even though 28-day mortality increased and the number of HFD decreased in high-latitude locations on unadjusted estimates, the associations were not significant after adjustment for patients’ characteristics. In the adjusted model, the odds of mortality were associated with altitude, gradually increasing after 350 MASL.
Older age and certain comorbidities were shown to be associated with unfavorable disease outcomes for COVID-19 patients[26,27]. Populations living in higher latitudes were shown to have a higher median age and more frequent comorbid conditions[28]. Furthermore, individuals living at higher elevations from the sea level were shown to have less comorbidity burdens[12]. Our study sample also noted a similar distribution of median age and comorbidities to different latitude and altitude levels.
Prior studies suggested that the variation of mortality rates in different latitude settings was partly attributable to baseline characteristics of populations[32,33]. However, others detected a relationship between humidity or sunlight exposure and case rates, which was thought to be related to viral dynamics[11,34]. In this study, the association of mortality within 28 d of admission and HFD with latitude, although statistically significant in the unadjusted analysis, was not statistically significant after case-mix adjustment. Our findings indicate that differences observed in previous epidemiological studies may be due to ecological fallacy rather than implying a causal relationship with environmental factors at the individual level[16].
Studies evaluating the impact of altitude on case and fatality rates of COVID-19 illustrated that higher altitude had a protective effect, possibly due to physiological and habitual characteristics of the individuals and environmental factors impacting virus survival[12,35]. Conversely, in our study, mortality gradually increased with increasing altitude after 350 MASL, suggesting the impact of environmental hypoxia resulting in the fragility of pulmonary functions or coagulation disorders. Although our results might suggest an impact of different elevation levels on disease outcomes, not having enough variation in altitude to test the impact of atmospheric oxygen pressure impedes our ability to conclude the actual effect of higher altitudes. Thus, our analysis results should be interpreted with caution.
Studies that evaluated the effects of latitude and altitude in patients with COVID-19 were epidemiological investigations that were conducted on populations rather than on individual patients. Thus, they are subject to the bias of aggregated variables rather than providing insight for a causal relationship[16]. This is the first study to evade ecological fallacy by considering individual baseline characteristics to the best of our knowledge. Thus, it might provide a better insight into the causal effect of environmental factors on adverse outcomes.
The most important limitation was the small sample variety in lower latitude and higher altitude environments. Especially not having patients from a wide range of altitude levels precluded drawing definitive conclusions about the impact of higher altitudes. Another limitation is being conducted exclusively on hospitalized patients, which might subject our results to collider bias[36]. Although our outcomes of interest might have ameliorated this limitation’s impact, it still hampers the generalizability of our results. Additionally, variations in patient management among different regions might have an impact on our results. Another weakness of our analysis is the lack of information about patients' home location (exempt IRB only allowed de-identified data use) and institutions' geographical locations as a surrogate. However, travel restrictions imposed during the study period might have kept patients confined to their primary residence and resultant nearby hospital admissions. Furthermore, although it was suggested as a contributor to disease severity, especially in higher latitudes, vitamin D levels were not incorporated in the analysis due to the unavailability. However, the timing of the study encompassing enough sunlight hours for the Northern Hemisphere might mitigate this limitation’s impact. Also, the number of patients included from the countries outside of the United States was limited. Moreover, to increase the accuracy of the frequency measurement, several institutions were not included in the study due to incomplete data variables.
Although 28 d mortality and HFD seemed to be associated with latitude, the association did not remain significant after adjustment. Our results might indicate that reported variations in COVID-19 in different environmental conditions might be based on individual patient characteristics rather than geographic factors.
The coronavirus disease 2019 (COVID-19) has taken the world by storm. Several factors were attributed to the spread of the virus including altitude and latitude. We studied the relationship of location with unfavorable patient outcomes in COVID-19.
There were variations in the case and fatality rates in different regions of the world. Using a large cohort, we aimed to assess if latitude or altitude had an impact on the disease course of the COVID-19 on the individual patient level.
To study the association of certain aspects of location with unfavorable outcomes in COVID-19.
An observational study using the Virus COVID-19 Registry was used to analyze for mortality within 28 d of admission and hospital length of stay. Adjusting for baseline parameters and admission date, multivariable regression modeling was utilized.
Twenty-two thousand one hundred eight patients from 21 countries were included. Mortality within 28 d of hospital admission was found to be 25%. The median number of hospital-free days among all included patients was 20 days. Despite the linear association between mortality within 28 d of hospital admission and hospital-free days and increasing latitude being significant, indicating that adverse disease outcomes were more frequent in locations further away from the Equator, the association was not significant after adjusting for baseline characteristics. A non-linear association between altitude and 28-day mortality was seen.
There seemed to be an association of latitude with mortality within 28 d of admission and hospital-free days, which was nonsignificant when adjusted for baseline characteristics.
The differences observed in previous epidemiological studies may be due to ecological fallacy rather than implying a causal relationship with environmental factors at the individual level.
| 1. | WHO. Novel coronavirus china: World Health Organization; 2020. [cited 29 November 2020]. Available from: https://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/. |
| 2. | WHO. Who director-general's opening remarks at the media briefing on COVID-19. [cited 11 March 2020]. World Health Organization; 2020. [DOI] [Full Text] |
| 3. | Bansal V, Mahapure KS, Bhurwal A, Gupta I, Hassanain S, Makadia J, Madas N, Armaly P, Singh R, Mehra I, O'Horo JC, Kashyap R. Mortality Benefit of Remdesivir in COVID-19: A Systematic Review and Meta-Analysis. Front Med (Lausanne). 2020;7:606429. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 4. | Menon T, Sharma R, Kataria S, Sardar S, Adhikari R, Tousif S, Khan H, Rathore SS, Singh R, Ahmed Z. The Association of Acute Kidney Injury With Disease Severity and Mortality in COVID-19: A Systematic Review and Meta-Analysis. Cureus. 2021;13:e13894. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Bansal V, Mahapure KS, Mehra I, Bhurwal A, Tekin A, Singh R, Gupta I, Rathore SS, Khan H, Deshpande S, Gulati S, Armaly P, Sheraton M, Kashyap R. Mortality Benefit of Convalescent Plasma in COVID-19: A Systematic Review and Meta-Analysis. Front Med (Lausanne). 2021;8:624924. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 6. | Singh R, Shaik L, Mehra I, Kashyap R, Surani S. Novel and Controversial Therapies in COVID-19. Open Respir Med J. 2020;14:79-86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Singh R, Rathore SS, Khan H, Bhurwal A, Sheraton M, Ghosh P, Anand S, Makadia J, Ayesha F, Mahapure KS, Mehra I, Tekin A, Kashyap R, Bansal V. Mortality and Severity in COVID-19 Patients on ACEIs and ARBs-A Systematic Review, Meta-Analysis, and Meta-Regression Analysis. Front Med (Lausanne). 2021;8:703661. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 8. | Singh R, Rathore SS, Khan H, Karale S, Bhurwal A, Tekin A, Jain N, Mehra I, Anand S, Reddy S, Sidhu GS, Panagopoulos A, Pattan V, Kashyap R, Bansal V. Association of obesity with covid-19 severity and mortality: A systemic review and meta-regression. [DOI] [Full Text] |
| 9. | Rhodes JM, Subramanian S, Laird E, Kenny RA. Editorial: Low population mortality from covid-19 in countries south of latitude 35 degrees north supports vitamin d as a factor determining severity. Alimentary Pharmacology & Therapeutics. 2020;51:1434. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 159] [Cited by in RCA: 157] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 10. | Sajadi MM, Habibzadeh P, Vintzileos A, Shokouhi S, Miralles-Wilhelm F, Amoroso A. Temperature, Humidity, and Latitude Analysis to Estimate Potential Spread and Seasonality of Coronavirus Disease 2019 (COVID-19). JAMA Netw Open. 2020;3:e2011834. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 268] [Cited by in RCA: 372] [Article Influence: 62.0] [Reference Citation Analysis (0)] |
| 11. | Sehra ST, Salciccioli JD, Wiebe DJ, Fundin S, Baker JF. Maximum Daily Temperature, Precipitation, Ultraviolet Light, and Rates of Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 in the United States. Clin Infect Dis. 2020;71:2482-2487. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 12. | Srivastava S, Garg I, Bansal A, Kumar B. SARS-CoV-2 infection: physiological and environmental gift factors at high altitude. Virusdisease. 2020;1-3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | Liu N, Li H. Letter: population mortality from COVID-19 and latitude-data from China. Aliment Pharmacol Ther. 2020;52:1259-1260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Choudhuri JA, Ogden LG, Ruttenber AJ, Thomas DS, Todd JK, Simoes EA. Effect of altitude on hospitalizations for respiratory syncytial virus infection. Pediatrics. 2006;117:349-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 51] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Bloom-Feshbach K, Alonso WJ, Charu V, Tamerius J, Simonsen L, Miller MA, Viboud C. Latitudinal variations in seasonal activity of influenza and respiratory syncytial virus (RSV): a global comparative review. PLoS One. 2013;8:e54445. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 250] [Cited by in RCA: 317] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 16. | Loney T, Nagelkerke NJ. The individualistic fallacy, ecological studies and instrumental variables: a causal interpretation. Emerg Themes Epidemiol. 2014;11:18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 66] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 17. | Domecq JP, Lal A, Sheldrick CR, Kumar VK, Boman K, Bolesta S, Bansal V, Harhay MO, Garcia MA, Kaufman M, Danesh V, Cheruku S, Banner-Goodspeed VM, Anderson HLI, Milligan PS, Denson JL, St. Hill CA, Dodd KW, Martin GS, Gajic O, Walkey AJ, Kashyap R. Outcomes of patients with coronavirus disease 2019 receiving organ support therapies: The international viral infection and respiratory illness universal study registry. Critical Care Medicine. 2021;49:437. [RCA] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 99] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 18. | Walkey AJ, Kumar VK, Harhay MO, Bolesta S, Bansal V, Gajic O, Kashyap R. The Viral Infection and Respiratory Illness Universal Study (VIRUS): An International Registry of Coronavirus 2019-Related Critical Illness. Crit Care Explor. 2020;2:e0113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 72] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 19. | Walkey AJ, Sheldrick RC, Kashyap R, Kumar VK, Boman K, Bolesta S, Zampieri FG, Bansal V, Harhay MO, Gajic O. Guiding Principles for the Conduct of Observational Critical Care Research for Coronavirus Disease 2019 Pandemics and Beyond: The Society of Critical Care Medicine Discovery Viral Infection and Respiratory Illness Universal Study Registry. Crit Care Med. 2020;48:e1038-e1044. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 20. | Turek J, Bansal V, Tekin A, Sharma M, Bogojevic M, Deo N, Qamar S, Singh R, Kashyap R. Rapid project management in a time of covid-19 crisis: Lessons learned from a global virus: Covid-19 registry (preprint) 2021. [DOI] [Full Text] |
| 21. | Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377-381. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38562] [Cited by in RCA: 40363] [Article Influence: 2374.3] [Reference Citation Analysis (0)] |
| 23. | Lu C, Yu Y, Li L, Yu C, Xu P. Systematic review of the relationship of Helicobacter pylori infection with geographical latitude, average annual temperature and average daily sunshine. BMC Gastroenterol. 2018;18:50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 24. | Arias-Reyes C, Zubieta-DeUrioste N, Poma-Machicao L, Aliaga-Raduan F, Carvajal-Rodriguez F, Dutschmann M, Schneider-Gasser EM, Zubieta-Calleja G, Soliz J. Does the pathogenesis of SARS-CoV-2 virus decrease at high-altitude? Respir Physiol Neurobiol. 2020;277:103443. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 135] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 25. | Ely EW, Angus DC, Williams MD, Bates B, Qualy R, Bernard GR. Drotrecogin alfa (activated) treatment of older patients with severe sepsis. Clin Infect Dis. 2003;37:187-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 69] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 26. | Clift AK, Coupland CAC, Keogh RH, Diaz-Ordaz K, Williamson E, Harrison EM, Hayward A, Hemingway H, Horby P, Mehta N, Benger J, Khunti K, Spiegelhalter D, Sheikh A, Valabhji J, Lyons RA, Robson J, Semple MG, Kee F, Johnson P, Jebb S, Williams T, Hippisley-Cox J. Living risk prediction algorithm (QCOVID) for risk of hospital admission and mortality from coronavirus 19 in adults: national derivation and validation cohort study. BMJ. 2020;371:m3731. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 343] [Cited by in RCA: 377] [Article Influence: 62.8] [Reference Citation Analysis (1)] |
| 27. | Chow DS, Glavis-Bloom J, Soun JE, Weinberg B, Loveless TB, Xie X, Mutasa S, Monuki E, Park JI, Bota D, Wu J, Thompson L, Boden-Albala B, Khan S, Amin AN, Chang PD. Development and external validation of a prognostic tool for COVID-19 critical disease. PLoS One. 2020;15:e0242953. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 29. | Holtgrave DR, Barranco MA, Tesoriero JM, Blog DS, Rosenberg ES. Assessing racial and ethnic disparities using a COVID-19 outcomes continuum for New York State. Ann Epidemiol. 2020;48:9-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 101] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 30. | Sili U, Ay P, Topuzoglu A, Bilgin H, Tigen ET, Sengel BE, Caglayik DY, Balcan B, Kocakaya D, Yildizeli SO, Gul F, Bilgili B, Sarinoglu RC, Yagci AK, Durmusoglu LM, Eryuksel E, Odabasi Z, Direskeneli H, Karakurt S, Cinel I, Korten V. Factors associated with progression to critical illness in 28 d among covid-19 patients: Results from a tertiary care hospital in Istanbul, Turkey. [DOI] [Full Text] |
| 31. | Petrilli CM, Jones SA, Yang J, Rajagopalan H, O'Donnell L, Chernyak Y, Tobin KA, Cerfolio RJ, Francois F, Horwitz LI. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1590] [Cited by in RCA: 1850] [Article Influence: 308.3] [Reference Citation Analysis (1)] |
| 32. | Ouchetto O, Drissi Bourhanbour A. Risk Factors of COVID-19 Patients. Disaster Med Public Health Prep. 2021;1-3. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 33. | Endailalu TB, Hadgu FW. Trends of sars-cov-2 infection worldwide: Role of population density, age structure, and climate on transmission and case fatality. [DOI] [Full Text] |
| 34. | Herman J, Biegel B, Huang L. Inactivation times from 290 to 315 nm uvb in sunlight for sars coronaviruses cov and cov-2 using omi satellite data for the sunlit earth. Air Quality, Atmosphere & Health, 2020. [RCA] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 35. | Arias-Reyes C, Carvajal-Rodriguez F, Poma-Machicao L, Aliaga-Raduán F, Marques DA, Zubieta-DeUrioste N, Accinelli RA, Schneider-Gasser EM, Zubieta-Calleja G, Dutschmann M, Soliz J. Decreased incidence, virus transmission capacity, and severity of COVID-19 at altitude on the American continent. PLoS One. 2021;16:e0237294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 36. | Griffith GJ, Morris TT, Tudball MJ, Herbert A, Mancano G, Pike L, Sharp GC, Sterne J, Palmer TM, Davey Smith G, Tilling K, Zuccolo L, Davies NM, Hemani G. Collider bias undermines our understanding of COVID-19 disease risk and severity. Nat Commun. 2020;11:5749. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 584] [Cited by in RCA: 568] [Article Influence: 94.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Society of Critical Care Medicine; American College of Chest Physicians.
Specialty type: Critical care medicine
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Al-Ani RM, Papadopoulos K S-Editor: Wang LL L-Editor: A P-Editor: Wang LL