Published online Nov 9, 2021. doi: 10.5492/wjccm.v10.i6.369
Peer-review started: June 24, 2021
First decision: July 27, 2021
Revised: August 5, 2021
Accepted: September 16, 2021
Article in press: September 16, 2021
Published online: November 9, 2021
Processing time: 133 Days and 15.7 Hours
There is limited data on the difference in the clinical characteristics and outcomes of patients with severe coronavirus disease 2019 (COVID-19) infection in the summer compared to the fall surge.
To compare the sociodemographic, clinical characteristics, and outcomes among mechanically ventilated patients with severe COVID-19 infection admitted to the intensive care unit (ICU) during the summer and fall surges in the year 2020.
We included patients admitted to the ICU and treated with invasive mechanical ventilation for COVID-19 associated respiratory failure between April 1 and December 31, 2020. Patients were categorized into summer surge for ICU admissions between June 15, 2020, and August 15, 2020, and fall surge between October 15, 2020, and December 31, 2020. We compared patients' characteristics and outcomes using descriptive and inferential statistics.
A total of 220 patients were admitted to the Grady Memorial Hospital ICU and mechanically ventilated for COVID-19 associated hypoxemic respiratory failure during the period considered (125 during the summer surge and 95 during the fall surge). More women were admitted in the fall compared to summer (41.1% vs 36.8%, difference, 4.3%; 95%CI: 1.2, 7.5). Patients admitted in the fall had fewer comorbidities (chronic obstructive pulmonary disease, stroke, diabetes mellitus, obstructive sleep apnea and body mass index ≥ 35 kg/m2). Overall, patients in the fall had a lower ICU mortality rate (27.4% vs 38.4%, difference, -11.0; 95%CI: -6.4, -18.2), shorter length of stay on the mechanical ventilator (7 d vs 11 d, difference, 4 d; 95%CI: 2.1, 6.6) and shorter ICU length of stay (9 d vs 14 d, difference, 5 d; 95%CI: 2.7, 9.4).
Patients admitted with severe COVID-19 infection requiring mechanical ventilation had better outcomes in the fall than summer. This difference observed is likely attributable to a better understanding of the condition and advances in treatment strategies.
Core Tip: In this observational study, we compared the sociodemographic, clinical characteristics, and outcomes among mechanically ventilated patients with coronavirus disease 2019 (COVID-19) infection admitted to the intensive care unit (ICU) during the summer and fall surges in the year 2020. Compared to patients admitted with severe COVID-19 in the summer, those in the fall had better outcomes including decreased mortality and low length of stay in the ICU. This is likely due to the improved understanding of COVID-19 and the advances in treatment strategies.
- Citation: Olanipekun T, Abe TA, Effoe VS, Musonge-Effoe JE, Chuks A, Kwara E, Caldwell A, Obeng S, Bakinde N, Westney G, Snyder R. Intensive care unit hospitalizations and outcomes in patients with severe COVID-19 during summer and fall surges in Georgia. World J Crit Care Med 2021; 10(6): 369-376
- URL: https://www.wjgnet.com/2220-3141/full/v10/i6/369.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v10.i6.369
Coronavirus disease 2019 (COVID-19) was first reported in the United States on January 20, 2020. The World Health Organization declared the novel viral infection a pandemic on March 11, 2020[1]. Within 1 year of the pandemic, more than 31 million cases and 500000 deaths have been recorded in the United States[2].
In the United States the pandemic has been characterized by waves of case surges attributed to holiday gatherings, relaxation of social distancing guidelines and removal of COVID-19 restriction during reopening after lockdown in different states[3,4]. Surges in COVID-19 cases are associated with increased hospitalizations including the intensive care units (ICU) placing significant strains on hospital resources[3]. The state of Georgia experienced resurgence of cases during the summer and fall seasons of 2020 with increased rates of hospitalizations[5].
We describe the differences in the sociodemographic, clinical characteristics, and outcomes in mechanically ventilated patients with severe COVID-19 infection admitted to the ICU of Grady Memorial Hospital (GMH) in Atlanta, Georgia across the surges in the summer and fall of year 2020.
We identified patients with positive reverse transcriptase–polymerase chain reaction nasopharyngeal swab test results for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) admitted to the GMH ICU (Morehouse school of medicine and Emory university ICU service) for hypoxemic respiratory failure and treated with invasive mechanical ventilation between April 1 and December 31, 2020. GMH is a level 1 trauma hospital in Atlanta, Georgia with more than 900 beds and one of the largest hospitals in Georgia. GMH played a significant role in the Georgia COVID-19 response by providing care to many COVID-19 patients in Georgia[6].
We extracted information on the age, sex, race/ethnicity, comorbidities, medication use, length of stay (LOS) on the mechanical ventilator, LOS in the ICU and ICU mortality outcomes from the electronic health record system. We obtained data from the Georgia State Department of Health to evaluate the trend of new COVID-19 cases between April 1 and December 31, 2020. Patients were categorized into summer surge for ICU admissions between June 15, 2020 and August 15, 2020 and fall surge between October 15, 2020 and December 31, 2020 based on the resurgence of COVID-19 cases in Georgia during the summer and fall periods. The study was approved by the Morehouse School of Medicine’s Institutional Review Board (IRB). The IRB issued a waiver of HIPAA authorization to access electronic medical records.
We report summary statistics as means or medians and proportions for sociodemographic, clinical, and outcome variables of severe COVID-19 patients hospitalized in the ICU. We computed bivariable comparisons across summer and fall surges and reported the proportional differences with corresponding 95%CIs. All analyses were performed with version 3.5.2 of the R programming language (R Project for Statistical Computing; R Foundation). P values were 2-sided, with statistical significance set at P < 0.05.
A total of 220 patients were admitted to the GMH ICU and mechanically ventilated for COVID-19 associated hypoxemic respiratory failure during the period considered (125 during the summer surge and 95 during the fall surge). Table 1 describes the differences between the socio-demographic, clinical characteristics, and the outcomes of these patients across the two surge periods. Proportion of females was higher during the fall surge compared to the summer surge (41.1% vs 36.8%, difference, 4.3%; 95%CI: 1.2, 7.5). More patients had private insurance during the fall surge (36.8%vs 30.4%, difference, 6.4%; 95%CI: 1.5, 13.3) while fewer patients were uninsured during the summer (18.9% vs 28%, difference, -9.1%: 95%CI: -6.4, -12.5).
| Variables | Surge 1 (Summer 2020) | Surge 2 (Fall 2020) | Difference (95%CI) | P value |
| Total – n (%) | 125 | 95 | ||
| Age, median (IQR) | 61.5 (51-69) | 61 (51.5-71) | 0.5 | 0.34 |
| < 55 yr | 41 (32.8) | 30 (31.6) | -1.2 (-3.8, 6.5) | 0.39 |
| 55–64 yr | 38 (30.4) | 25 (26.3) | -4.1 (-6.2, -2.3) | 0.04 |
| 65–74 yr | 27 (21.6) | 27 (28.4) | 6.8 (4.5, 10.3) | 0.04 |
| > 75 yr | 19 (15.2) | 13 (13.7) | -1.5 (-5.5, 2.5) | 0.19 |
| Race | ||||
| Non-Hispanic Black | 86 (68.8) | 61 (64.2) | -4.6 (-10.7, 1.1) | 0.1 |
| Non-Hispanic White | 22 (17.6) | 17 (17.9) | 0.3 (-1.7, 2.5) | 0.18 |
| Hispanic | 10 (8) | 8 (8.4) | 0.4 (-1.6, 2.4) | 0.26 |
| Others1 | 7 (5.6) | 8 (8.4) | 2.8 (0.9, 4.9) | 0.09 |
| Gender | ||||
| Female | 46 (36.8) | 39 (41.1) | 4.3 (1.2, 7.5) | < 0.01 |
| Male | 79 (63.2) | 56 (58.9) | -4.3 (-2.4, -6.2) | < 0.01 |
| Health insurance | ||||
| Medicaid only | 7 (5.6) | 5 (5.3) | -0.3 (-2.3, 1.5) | 0.41 |
| Medicare only | 20 (16) | 15 (15.8) | -0.2 (-1.8, 1.3) | 0.12 |
| Medicaid/Medicare | 25 (20) | 22 (23.2) | 3.2 (1.0, 5.8) | 0.05 |
| Private insurance/Self pay | 38 (30.4) | 35 (36.8) | 6.4 (1.5, 13.3) | 0.02 |
| Uninsured | 35 (28) | 18 (18.9) | -9.1 (- 6.4, -12.5) | 0.04 |
| Comorbid diseases | ||||
| Asthma | 13 (10.4) | 9 (9.5) | -0.9 (-4.8, 2.8) | 0.22 |
| Coronary artery disease | 20 (16) | 12 (12.6) | -3.4 (-8.5, 1.7) | 0.11 |
| Cancer (solid organ tumors) | 12 (9.6) | 6 (6.3) | -3.3 (- 8.2, 1.9) | 0.18 |
| Congestive heart failure | 29 (23.2) | 20 (21.1) | -2.1 (- 6.6, 2.1) | 0.4 |
| Chronic kidney disease 3 and above | 17 (13.6) | 16 (16.8) | 3.2 (1.6, 5.1) | 0.02 |
| Chronic liver disease | 10 (8) | 9 (9.5) | 1.5 (0.8, 2.47) | 0.13 |
| Chronic obstructive pulmonary disease | 22 (17.6) | 12 (12.6) | -5.0 (-10.1, -5.6) | 0.04 |
| Cerebrovascular accident | 21 (16.8) | 11 (11.6) | -5.2 (-10.3, -5.8) | 0.02 |
| Diabetes mellitus | 62 (49.6) | 41 (43.2) | -6.4 (-3.1, -9.8) | < 0.01 |
| HIV/AIDS | 4 (3.2) | 8 (8.4) | 5.2 (2.7, 8.2) | < 0.01 |
| Hypertension | 85 (68) | 67 (70.5) | 2.5 (1.3, 4.9) | < 0.01 |
| Obstructive sleep apnea | 14 (11.2) | 6 (6.3) | -4.9 (-1.9, 8.8) | < 0.01 |
| Body mass index | ||||
| < 30 kg/m2 | 37 (29.6) | 29 (30.5) | 0.9 (0.4, 1.4) | 0.078 |
| ≥ 30 kg/m2 to < 35 kg/m2 | 48 (38.4) | 40 (42.1) | 3.7 (1.6, 5.9) | < 0.01 |
| ≥ 35 kg/m2 | 40 (32) | 26 (27.4) | -4.6 (-1.3, 8.7) | < 0.01 |
| Tobacco use (current smoker) | 51 (40.8) | 45 (47.4) | 6.6 (3.2, 11.8) | < 0.01 |
| No of comorbidities | ||||
| None | 12 (9.6) | 16 (16.8) | 7.2 (2.8, 13.9) | < 0.01 |
| 1 | 8 (6.4) | 5 (5.3) | -1.1 (-3.4, 1.1) | 0.46 |
| > 1 | 105 (84) | 78 (82.1) | -1.9 (-5.1, 1.3) | 0.37 |
| Treatment received in the ICU | ||||
| Hydroxychloroquine | 6 (4.8) | 0 (0) | -4.8 (- 2.5, -7.6) | 0.03 |
| Azithromycin | 25 (20) | 14 (14.7) | -5.3 (- 3.1, -7.9) | 0.04 |
| Hydroxychloroquine + Azithromycin | 36 (28.8) | 0 (0) | -28.8 (-19.4, 41.1) | < 0.01 |
| Remdesivir | 44 (35.2) | 42 (44.2) | 9.0 (3.4, 10.2) | < 0.01 |
| Dexamethasone | 0 | 22 (23.2) | 23.2 (18.3, 29.1) | < 0.01 |
| Length of stay, median (IQR) (range), d | ||||
Patients admitted to the ICU during the fall surge had significantly higher burden of chronic kidney disease 4 and above, human immunodeficiency virus/acquired immune deficiency syndrome, hypertension, class 1 obesity (body mass index, BMI ≥ 30 kg/m2 to < 35 kg/m2) and tobacco use disorder, while fewer patients had chronic obstructive pulmonary disease (COPD), cerebrovascular accidents, diabetes mellitus (DM), obstructive sleep apnea and class 2 or greater obesity (BMI ≥ 35 kg/m2). A significantly higher proportion of patients during the fall had no comorbidities at baseline compared to those in the summer (16.8% vs 9.6%, difference 7.2%; 95%CI: 2.8, 13.9). A greater proportion of patients in the fall surge were treated with remdesivir and dexamethasone.
The ICU mortality rate (27.4% vs 38.4%, difference, -11.0; 95%CI: -6.4, -18.2) was lower in the fall compared to summer. Similarly, patients in the fall had a shorter LOS on the mechanical ventilator (7 d vs 11 d, difference, 4 d; 95%CI: 2.1, 6.6) and shorter LOS in the ICU (9 d vs 14 d, difference, 5 d; 95%CI: 2.7, 9.4).
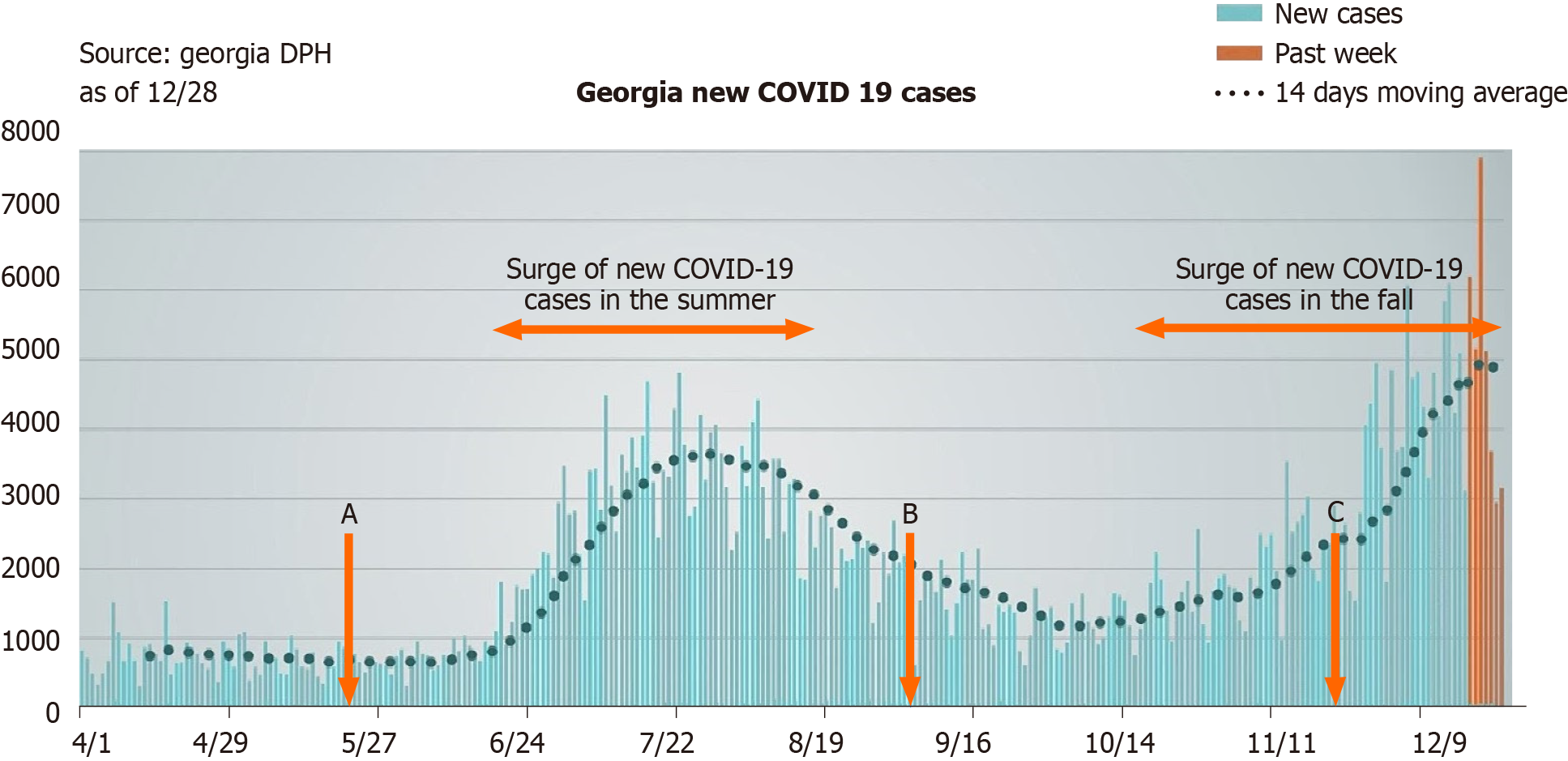
Figures 1 and 2 present trends of new COVID-19 cases and ICU hospitalizations in Georgia and GMH between April 1 – December 31, 2020. There was an increase in COVID-19 cases and ICU hospitalizations at GMH correlating with the summer and fall surges in Georgia. Dates corresponding to specific US national holidays are highlighted in Figure 1. Notably, the memorial holiday (May 25, 2020) preceded the surge of cases in the summer while the Labor Day (September 7, 2020) and Thanksgiving (November 26, 2020) holidays preceded the Fall surge.
We observed increased ICU hospitalizations for COVID-19 associated respiratory failure requiring invasive mechanical ventilation corresponding to the surges of cases during the summer and fall of 2020 in Georgia. ICU hospitalizations during the reporting period were consistently guided by severity of symptoms, comorbidities, clinical and diagnostic findings, respiratory status, and indications for mechanical ventilation. Therefore, the higher ICU census noted during the surges likely reflects increased rates of COVID-19 prevalence in the community.
ICU mortality was 11% lower among patients in the fall cohort than those in the summer. Also, the length of time a patient spent on the mechanical ventilator and in the ICU were shorter during the fall when compared to the summer. These observed differences could be explained by a number of factors. First, patients in the fall cohort had a higher proportion of patients with no comorbidities at baseline and fewer patients relative to the summer cohort, with specific chronic medical problems such as DM, COPD and class 2 obesity or greater, which have been associated with severe COVID-19 course and poorer outcomes. Second, more patients in the fall surge received Food and Drug Administration (FDA)-approved and Centers for Disease Control and Prevention (CDC) recommended treatments, including dexamethasone and remdesivir, which have been shown to improve outcomes among COVID-19 patients. The Randomized Evaluation of Covid-19 Therapy (RECOVERY) trial demonstrated a lower 28 d mortality among COVID-19 patients treated with dexamethasone compared to placebo[7]. There is also evidence that remdesivir, when compared to placebo is associated with a shorter duration of mechanical ventilation or extracorporeal membrane oxygenation (ECMO) for COVID-19 respiratory failure[8]. Third, the improved outcomes likely mirror a combination of better understanding of COVID-19 pathophysiology, availability of novel therapies and better medical management.
It is not surprising that the summer and fall surges were preceded by major holidays as there have been numerous similar reports globally. Attending events that involve large gatherings typically seen during holidays increases the chances of COVID-19 infection[3]. For instance, the Lunar New Year holiday coincided with the start of the pandemic when millions of people left the city of Wuhan in China to visit relatives in other parts of the country and the world[9]. In the United Kingdom, the early COVID-19 epidemic followed a one-week school holiday break from February 17 to February 21, 2020 when thousands of people came back infected with SARS-CoV-2 virus from tourist activities in northern Italy and Spain[10]. Also, Canada reported its highest numbers of COVID-19 infection cases in the two weeks following the Thanksgiving holiday on October 12, 2020[2].
Our study has some limitations. First, this was a single center study with unique institutional practices and findings that may not be generalizable. Second, there are socio-behavioral and political circumstances that may have contributed to the surge of COVID-19 cases during the fall and summer seasons of 2020 that we could not measure in this study.
In this single-center study, we found significant differences in the sociodemographic, clinical characteristics, and outcomes among mechanically ventilated COVID-19 patients in the ICU during the 2020 summer surge compared to the fall surge. ICU mortality, LOS on mechanical ventilator, and LOS in the ICU were all significantly lower in the fall than summer. This finding is likely a result of our improved understanding of COVID-19 and advancement in management strategies.
There is limited data on the difference in the clinical characteristics and outcomes of patients with severe coronavirus disease 2019 (COVID-19) infection in the summer compared to the fall surge.
Surges in COVID-19 cases are associated with increased hospitalizations including the intensive care units (ICU) placing significant strains on hospital resources. Knowledge about the differences in the clinical characteristics and outcomes between each surge will provide useful information on how to decrease related morbidity and mortality.
To compare the sociodemographic, clinical characteristics, and outcomes among mechanically ventilated patients with severe COVID-19 infection admitted to the (ICU) during the summer and fall surges in the year 2020.
The authors included mechanically ventilated COVID-19 patients managed at Grady Memorial Hospital (GMH) from April 1 and December 31, 2020. Patients were categorized into two groups, those admitted in the summer (June 15, 2020 - August 15, 2020) and fall (October 15, 2020 - December 31, 2020). We compared patients' characteristics and outcomes using descriptive and inferential statistics.
A total of 220 patients were admitted to the GMH ICU and mechanically ventilated for COVID-19 (125 during the summer surge and 95 during the fall surge). Patients admitted in the fall had fewer comorbidities, lower mortality rate, shorter length of stay on the mechanical ventilator and shorter ICU length of stay.
Patients admitted with severe COVID-19 infection requiring mechanical ventilation had better outcomes in the fall than in summer.
Further studies are needed to replicate these findings.
| 1. | Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, Spitters C, Ericson K, Wilkerson S, Tural A, Diaz G, Cohn A, Fox L, Patel A, Gerber SI, Kim L, Tong S, Lu X, Lindstrom S, Pallansch MA, Weldon WC, Biggs HM, Uyeki TM, Pillai SK; Washington State 2019-nCoV Case Investigation Team. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med. 2020;382:929-936. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4155] [Cited by in RCA: 3852] [Article Influence: 642.0] [Reference Citation Analysis (2)] |
| 2. | JHU CSSE. Dataset: GitHub - CSSEGISandData/COVID-19: Novel Coronavirus (COVID-19) Cases. Dataset COVID-19, 2020. Available from: https://github.com/CSSEGISandData/COVID-19. |
| 3. | Duque D, Morton DP, Singh B, Du Z, Pasco R, Meyers LA. Timing social distancing to avert unmanageable COVID-19 hospital surges. Proc Natl Acad Sci U S A. 2020;117:19873-19878. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 4. | Vahidy FS, Drews AL, Masud FN, Schwartz RL, Askary BB, Boom ML, Phillips RA. Characteristics and Outcomes of COVID-19 Patients During Initial Peak and Resurgence in the Houston Metropolitan Area. JAMA. 2020;324:998-1000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 97] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 5. | Moore JX, Langston ME, George V, Coughlin SS. Epidemiology of the 2020 pandemic of COVID-19 in the state of Georgia: Inadequate critical care resources and impact after 7 weeks of community spread. J Am Coll Emerg Physicians Open. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | Jackson BR, Gold JAW, Natarajan P, Rossow J, Neblett Fanfair R, da Silva J, Wong KK, Browning SD, Bamrah Morris S, Rogers-Brown J, Hernandez-Romieu AC, Szablewski CM, Oosmanally N, Tobin-D'Angelo M, Drenzek C, Murphy DJ, Hollberg J, Blum JM, Jansen R, Wright DW, SeweSll WM, Owens JD, Lefkove B, Brown FW, Burton DC, Uyeki TM, Bialek SR, Patel PR, Bruce BB. Predictors at admission of mechanical ventilation and death in an observational cohort of adults hospitalized with COVID-19. Clin Infect Dis. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 7. | RECOVERY Collaborative Group; Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, Staplin N, Brightling C, Ustianowski A, Elmahi E, Prudon B, Green C, Felton T, Chadwick D, Rege K, Fegan C, Chappell LC, Faust SN, Jaki T, Jeffery K, Montgomery A, Rowan K, Juszczak E, Baillie JK, Haynes R, Landray MJ. Dexamethasone in Hospitalized Patients with Covid-19. N Engl J Med. 2021;384:693-704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6762] [Cited by in RCA: 7599] [Article Influence: 1519.8] [Reference Citation Analysis (7)] |
| 8. | Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, Hohmann E, Chu HY, Luetkemeyer A, Kline S, Lopez de Castilla D, Finberg RW, Dierberg K, Tapson V, Hsieh L, Patterson TF, Paredes R, Sweeney DA, Short WR, Touloumi G, Lye DC, Ohmagari N, Oh MD, Ruiz-Palacios GM, Benfield T, Fätkenheuer G, Kortepeter MG, Atmar RL, Creech CB, Lundgren J, Babiker AG, Pett S, Neaton JD, Burgess TH, Bonnett T, Green M, Makowski M, Osinusi A, Nayak S, Lane HC; ACTT-1 Study Group Members. Remdesivir for the Treatment of Covid-19 - Final Report. N Engl J Med. 2020;383:1813-1826. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5829] [Cited by in RCA: 5235] [Article Influence: 872.5] [Reference Citation Analysis (0)] |
| 9. | Chen S, Yang J, Yang W, Wang C, Bärnighausen T. COVID-19 control in China during mass population movements at New Year. Lancet. 2020;395:764-766. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 583] [Cited by in RCA: 442] [Article Influence: 73.7] [Reference Citation Analysis (0)] |
| 10. | du Plessis L, McCrone JT, Zarebski AE, Hill V, Ruis C, Gutierrez B, Raghwani J, Ashworth J, Colquhoun R, Connor TR, Faria NR, Jackson B, Loman NJ, O'Toole Á, Nicholls SM, Parag KV, Scher E, Vasylyeva TI, Volz EM, Watts A, Bogoch II, Khan K; COVID-19 Genomics UK (COG-UK) Consortium, Aanensen DM, Kraemer MUG, Rambaut A, Pybus OG. Establishment and lineage dynamics of the SARS-CoV-2 epidemic in the UK. Science. 2021;371:708-712. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 303] [Cited by in RCA: 299] [Article Influence: 59.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: American Heart Association, No. 000258201449; American College of Cardiology, No. 3332058.
Specialty type: Critical care medicine
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Braga MB S-Editor: Ma YJ L-Editor: A P-Editor: Wang LYT