Published online Jul 9, 2021. doi: 10.5492/wjccm.v10.i4.120
Peer-review started: February 26, 2021
First decision: April 6, 2021
Revised: April 29, 2021
Accepted: May 20, 2021
Article in press: May 20, 2021
Published online: July 9, 2021
Processing time: 130 Days and 1.1 Hours
Central venous catheterization is currently an important procedure in critical care. Central catheterization has important advantages in many clinical situations. It can also lead to different complications such as infection, hemorrhage, and thrombosis. It is important to investigate critically ill patients undergoing catheterization.
To evaluate the characteristics, such as hospitalization, demographic characteristics, post-catheterization complications, and mortality relationships, of patients in whom a central venous catheter was placed in the emergency room.
A total of 1042 patients over the age of 18 who presented to the emergency department between January 2005 and December 2015 were analyzed retros
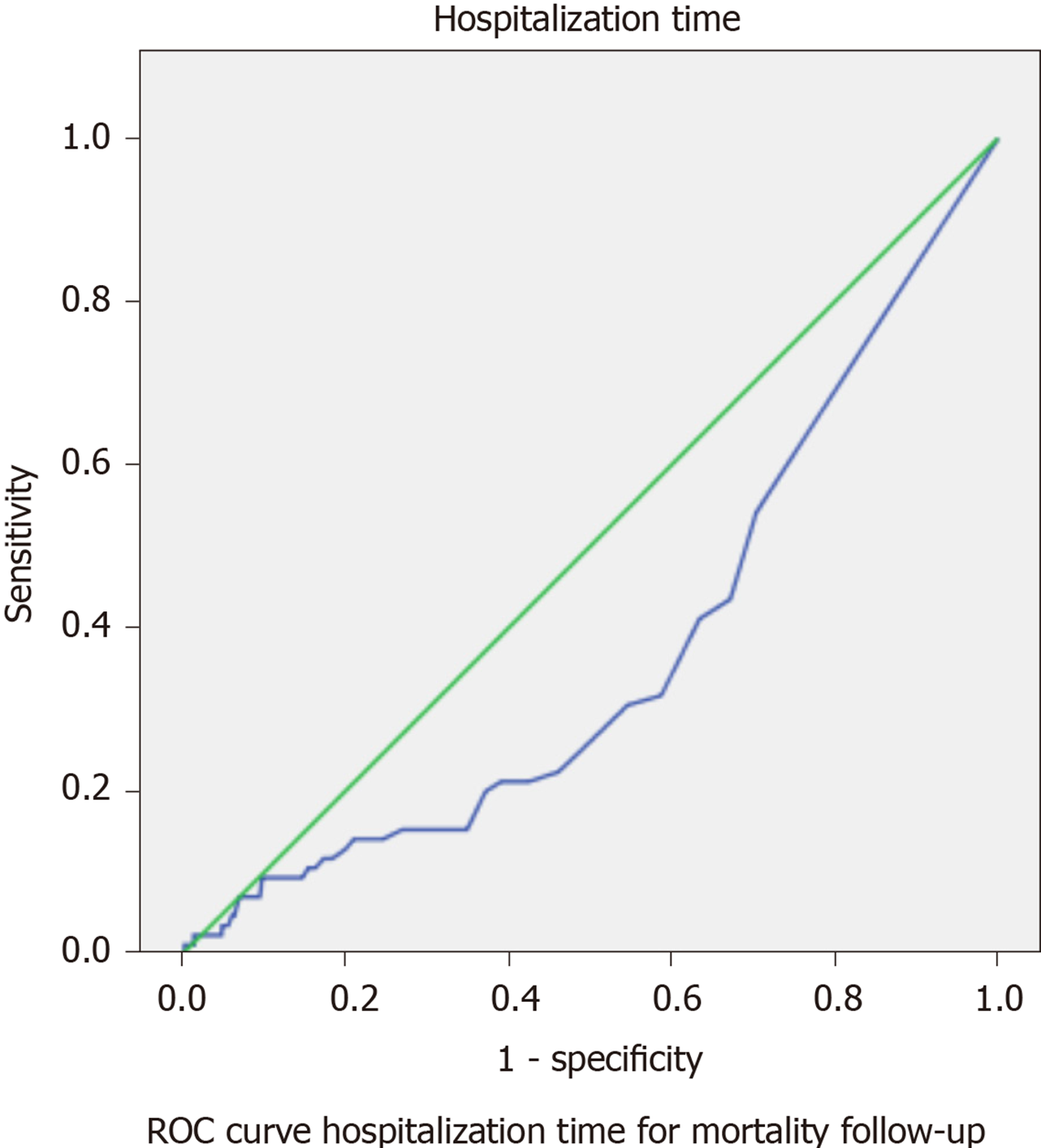
The mean age of the patients was 60.99 ± 19.85 years; 423 (40.6%) of them were women. Hospitalization time was 11.89 ± 16.38 d. There was a significant correlation between the inserted catheters with gender (P = 0.009) and hospitalization time (P = 0.040). Also, blood glucose, blood urea nitrogen, creatinine, and serum potassium values among the biochemical values of the patients who were catheterized were significant. A significant association was observed in the analysis of patients with complications that develop according to the catheter region (P = 0.001) and the outcome stage (P = 0.001). In receiver operating characteristic curve analysis of hospitalization time and mortality area under curve was 0.575, the 95% confidence interval was 0.496-0.653, the sensitivity was 71%, and the specificity was 89% (P = 0.040).
Catheter location and length of stay are important risk factors for catheter-borne infections. Because the risk of infection was lower than other catheters, jugular catheters should be preferred at entry points, and preventive measures should be taken by monitoring patients closely to reduce hospitalization infections.
Core Tip: A total of 1042 patients were included in this retrospective study. All central venous catheters were inserted in the emergency room. This study included 10 years of experience in our emergency department. In receiver operating characteristic curve analysis of hospitalization time and mortality, sensitivity was 71%, and specificity was 89% (P = 0.040). Complications in the subclavian vein and femoral vein were observed more frequently in the long term. Jugular vein catheterization can be preferred primarily due to the difficulties in application and due to the low number of complications.
- Citation: Coskun A, Hıncal SÖ, Eren SH. Emergency service results of central venous catheters: Single center, 1042 patients, 10-year experience. World J Crit Care Med 2021; 10(4): 120-131
- URL: https://www.wjgnet.com/2220-3141/full/v10/i4/120.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v10.i4.120
Emergency services are dynamic clinics where acute and emergency aspects of diseases and injuries affecting patients of all age groups are prevented. Resuscitation, primary care, diagnosis, and treatment of emergency cases are performed. Due to the nature of acute illnesses and injuries and their independence from each other, when they will come to emergency services and their number cannot be predicted[1]. Acute procedures should be done as soon as possible in terms of the density, variety, and patient circulation of emergency services.
Intravenous applications in emergency rooms act as a lifeline in saving the life of the patient. For this reason, the process must be done quickly and safely. In a study conducted on patients with penetrating injuries in the emergency department, timely and effective intravenous interventions were reported to increase survival rates[2].
Central venous catheterization (CVC) is an important intervention that is widely used today. Emergency services have a large variety of patient populations where central venous interventions are frequently applied. CVC is necessary for the use of vasoactive or irritant drugs, in insufficient peripheral intravenous routes, rapid infusion of intravenous fluids, parenteral alimentation, frequent therapeutic plas
A central venous catheter is to be placed percutaneously. The main routes of catheterization are the internal jugular vein (IJV), subclavian vein (SCV), and femoral vein (FV). The placement of a catheter in the IJV is gaining in popularity and is preferred in children[4]. Various complications may develop in CVC, such as pneumothorax, hemothorax, venous thrombosis, vertebral and cervical artery injuries, artery puncture, bleeding, arrhythmia, catheter dysfunction such as catheter blockage or catheter breakage, infection, cardiac tamponade, respiratory tract obstruction, and chylothorax[5,6].
Each catheter region to be used has its advantages and disadvantages. IJV catheterization is often used in intensive care units on mechanically ventilated comatose patients. SCV catheterization is not preferred in these patients due to the risk of sudden pneumothorax[7]. The most important disadvantage of IJV catheterization is the difficulty of detecting the skin and restricting neck movements. The risk of pneumothorax, hemothorax, and vena cava superior injury is much less. At the same time, the development of thrombosis and narrowing of the IJV is much less due to the lack of catheter angulation, which is monitored in the SCV[8].
The aim of this study was to analyze the different catheter insertion sites, diagnoses, complications, length of hospitalization, catheter-related local infection, and bacteremia in terms of morbidity and mortality in patients who were followed up in the emergency service.
In this retrospective study, 1042 patients over 18-years-old who were admitted to the emergency room between January 2005 and December 2015 were analyzed. CVC was implanted in patients whose general condition was poor, whose vascular access could not be opened in the emergency room, who needed dialysis and fluid resuscitation, who suffered traffic accidents, falls, burns, malignancy, or acute and chronic renal failure, and who needed blood or cardiopulmonary resuscitation. The exclusion criteria were applied to all patients with severe bleeding diathesis and an indication other than infection in the area where the catheter was to be placed. All patients were divided into three groups: jugular, subclavian, and femoral according to the area of the catheter placed. These catheters were divided into right and left. Seven groups were formed according to complications after catheterization: pneumothorax, guidewire problems, bleeding, catheter location infection, arterial interference, sepsis, and no complications. Patients who were planned to have a catheter application were divided into subgroups according to their diagnosis. The subgroups were renal diseases (acute and chronic renal failure), respiratory diseases (asthma, chronic obstructive pulmonary diseases, pulmonary embolism), endocrine diseases (hypoglycemia, diabetic ketoacidosis, hyperosmolar coma, thyroid crises), multiple organ failure, gastrointestinal bleeding and perforations, cerebrovascular diseases (cerebrovascular infarcts, intraparenchymal hemorrhages, epidural and subdural hemorrhages, cerebral edema, subarachnoid hemorrhages), trauma to the thorax (thoracic open injury, severe pneumothoraces, severe lung parenchymal injuries), traffic accidents (inside and outside the vehicle), malignancies in poor general condition, life-threatening gunshot injuries, cardiac diseases (myocardial infarction, heart failure, cardiac tamponade, cardiomyopathies), cardiovascular diseases (aortic dissection and aneurysms), severe injuries as a result of falls, second and third-degree burns with a large surface area, extremity amputation, penetrating-cutting tool injuries, and cardiopulmonary resuscitation. It could be done in more groups, but the most common diagnoses requiring catheter indication were included in the emergency department.
Sixteen groups were also identified according to the services where catheterized patients were hospitalized. These services were emergency services, infectious diseases, general internal medicine, nephrology, gastroenterology, intensive care unit, cardiology, neurosurgery, thoracic surgery, chest diseases, general surgery, cardiovascular surgery, neurosurgery, plastic surgery, burn unit, and neurology services.
Patients were observed from hospitalization until discharge. Outpatients were followed up retrospectively with an automation system for 3 mo after they were discharged, and those who did not come to the hospital were questioned by phone. Diagnoses, admission dates, contact information, demographic, clinical, and laboratory data are included in the registry system of our hospital. As a result, all patients were reached via call and/or hospital records.
Kits prepared for central venous catheter application in the emergency department were used. Components of these kits included: The needle included an injector to allow passage of the guidewire, double or triple catheter, guidewire, plastic sheath in which the guidewire was placed, dilator, 3/0 silk sharp needle suture, and scalpel. A central venous catheter procedure was performed under local anesthesia. The patient was placed in the supine position. The jugular vein catheter was positioned with the head slightly down. For the SCV catheter, the arms were extended to the sides parallel to the body. For the FV catheter, the legs were kept open at a certain angle. During the procedure, the patient was monitored, and heart rhythm was followed. The sterility of the area where the catheter will be applied was provided with 10% povidone-iodine. Lidocaine was used for local anesthesia. The Seldinger technique was used for central venous catheter application[9]. Main lines of central venous catheter application after anesthesia was achieved included: (1) sterilizing the procedure area; (2) proper positioning of the thick needle to which the guidewire will be sent; (3) inserting the guidewire into the vein lumen by applying slight negative pressure; (4) advancing the guidewire into the vein lumen; (5) dilating the path through which the catheter will pass; (6) inserting the catheter into the vein with the help of a guidewire; (7) adequate progression and fixation of the catheter in the vein; and (8) closing in a sterile manner. Lung radiography and ultrasonography were performed for central venous catheter complications.
Catheter-related infection was determined according to the ”Centers for Disease Control” criteria[10]. Catheter tip colonization was accepted if more than 15 colony-forming units microorganisms were produced from the catheter tip. Local signs for catheter-induced local infection (induration, edema, heat increase, purulent yeast arrival) and the reproduction of microorganisms in catheter tip culture were noted.
In the emergency department, ultrasonography was not commonly used until 2018. For this reason, none of the 1042 patients could be subjected to catheter placement accompanied by ultrasonography. Accompanied by ultrasonography, we were unable to learn about complications that may occur as a result of catheter placement. But for catheter placement, all patients were applied with some criteria. These criteria are as follow.
Jugular catheters: Elderly, cachectic, superficial vein structure, lack of coagulopathy barrier, lack of local wound infection, low risk of pneumothorax, rapid venous return, and direct compression in bleeding. Right or left catheter placement was performed according to the current condition of the patient and the experience of the clinician.
Subclavian catheters: Obesity, the dressing was comfortable, the placement procedure was possible while ensuring airway control, there was no local infection, no coagulopathy, and the right or left catheter was placed according to the experience of the clinician.
Femoral catheters: Fast intervention with high success rate, no local infection, no coagulopathy, no division during cardiopulmonary resuscitation and/or intubation, no risk of pneumothorax, no Trendelenburg position, cachectic patients and according to the experience of the clinician, right or left catheters were placed. However, due to the current location of the inguinal region, jugular or subclavian catheters were preferred more because of the high risk of infection, although sterility was taken into consideration.
Laboratory design: Hemogram and biochemical blood samples of the patients were taken at the emergency service. Hemogram was measured using Sysmex DI-60 CBC Analyzer (Istanbul, Turkey). Biochemistry was analyzed by Beckman Coulter Automated AU-680 (Beckman Coulter, Inc., Fullerton, CA, United States). Hemogram and biochemistry results were studied between 45-60 min.
The data obtained from the study were analyzed with the SPSS 20 (SPSS Inc., Chicago, IL, United States) package program. Kolmogorov-Smirnov test was performed while investigating the normal distributions of the variables. Descriptive statistics were presented as mean ± SD or median (minimum-maximum) for continuous variables and as the number of cases and percentage (%) for nominal variables. When examining the differences between groups, Mann-Whitney U and Kruskal-Wallis H tests were used because the variables did not come from the normal distribution. 2 analysis was used when examining the relationships between groups of nominal variables. Receiver operating characteristic curve analysis was performed to predict the development of mortality. While interpreting the results, values below the significance level of 0.05 were considered statistically significant.
The mean age of the patients was 60.99 ± 19.85 years (minimum 18-maximum 99); 423 (40.6%) of them were women. The mean age of jugular vein catheter patients was 60.74 ± 20.20 years, and 339 (40%) were female. The mean age of SCV catheter patients was 59.66 ± 19.17 years, and 42 (27.3%) were female. The mean age of FV catheter patients was 63.67 ± 18.57 years and 42 (42%) were women. Hospitalization time was 11.89 ± 16.38 d. The patients who were catheterized were not statistically significant with age (P = 0.939), but there was a significant correlation with gender (P = 0.009) and hospitalization time (P = 0.040). Also, blood glucose, blood urea nitrogen, creatinine, and serum potassium were statistically significant from the biochemical values of the patients who were catheterized. The relationship with other biochemical values could not be determined. Among the hemogram parameters, it was statistically significant with hemoglobin and mean corpuscular hemoglobin concentration, and no correlation was found with other values (Table 1).
| Catheter area inserted | |||||
| All patients, n = 1042, mean ± SD | Jugular, n = 743, mean ± SD | Subclavian, n = 155, mean ± SD | Femoral, n = 144, mean ± SD | P value | |
| Baseline characteristics | |||||
| Age, yr | 60.99 ± 19.85 | 60.74 ± 20.20 | 59.66 ± 19.17 | 63.67 ± 18.57 | 0.939 |
| Sex, female/male | 423/619 | 339/449 | 42/112 | 42/58 | 0.009 |
| Hospitalization time | 11.89 ± 16.38 | 12.50 ± 16.03 | 11.00 ± 20.08 | 9.73 ± 13.39 | 0.040 |
| Laboratory finding | |||||
| Biochemistry | |||||
| BS, mg/dL | 139.45 ± 101.56 | 145.21 ± 112.63 | 120.35 ± 55.74 | 130.30 ± 72.49 | 0.008 |
| BUN, mg/dL | 42.77 ± 41.29 | 51.11 ± 44.40 | 19.65 ± 13.91 | 24.58 ± 26.42 | 0.001 |
| Creatinine, mg/dL | 2.62 ± 2.89 | 3.20 ± 3.14 | 0.99 ± 0.68 | 1.37 ± 1.68 | 0.001 |
| TBIL, mg/dL | 0.87 ± 0.84 | 0.82 ± 0.63 | 0.80 ± 0.88 | 1.22 ± 1.43 | 0.485 |
| AST, mg/dL | 37.65 ± 47.22 | 32.56 ± 25.60 | 40.04 ± 60.05 | 61.38 ± 90.77 | 0.508 |
| ALT, mg/dL | 35.81 ± 49.37 | 30.31 ± 26.18 | 38.58 ± 67.59 | 61.21 ± 91.95 | 0.710 |
| ALP, mg/dL | 108.57 ± 64.10 | 104.95 ± 56.71 | 104.66 ± 59.33 | 131.48 ± 93.90 | 0.569 |
| Na, mmol/L | 138.61 ± 5.38 | 138.68 ± 5.33 | 138.22 ± 5.07 | 138.68 ± 5.96 | 0.125 |
| K, mmol/L | 5.00 ± 1.03 | 5.13 ± 1.10 | 5.07 ± 0.71 | 4.79 ± 0.70 | 0.027 |
| Cl, mmol/L | 100.23 ± 6.23 | 100.18 ± 6.11 | 100.41 ± 6.95 | 100.29 ± 6.04 | 0.778 |
| Amylase | 89.98 ± 49.88 | 87.93 ± 47.66 | 91.64 ± 53.25 | 98.78 ± 56.30 | 0.419 |
| CRP, mg/dL | 4.44 ± 8.12 | 3.53 ± 5.14 | 4.32 ± 7.65 | 9.26 ± 15.90 | 0.925 |
| Hemogram | |||||
| WBC, × 103/UL | 10.57 ± 4.51 | 10.26 ± 3.59 | 10.32 ± 4.05 | 12.49 ± 7.72 | 0.228 |
| Hb, g/dL | 13.77 ± 2.07 | 13.63 ± 2.12 | 14.09 ± 1.77 | 14.16 ± 1.98 | 0.017 |
| Hct, % | 42.17 ± 6.62 | 42.07 ± 6.78 | 42.23 ± 5.80 | 42.62 ± 6.65 | 0.737 |
| MCV, fL | 87.74 ± 6.29 | 87.71 ± 6.42 | 87.45 ± 6.18 | 88.24 ± 5.70 | 0.927 |
| MCH, pg | 29.37 ± 2.36 | 29.30 ± 2.41 | 29.48 ± 2.29 | 29.67 ± 2.20 | 0.905 |
| MCHC, g/dL | 33.25 ± 1.36 | 33.19 ± 1.37 | 33.47 ± 1.29 | 33.29 ± 1.36 | 0.002 |
| RDW, % | 14.69 ± 1.73 | 14.74 ± 1.79 | 14.45 ± 1.50 | 14.66 ± 1.61 | 0.082 |
| PLT, × 103/µL | 248.22 ± 80.14 | 248.71 ± 76.33 | 256.88 ± 76.01 | 236.42 ± 100.38 | 0.073 |
| MPV, fL | 8.48 ± 1.01 | 8.54 ± 1.03 | 8.33 ± 1.06 | 8.34 ± 0.86 | 0.085 |
In the analysis of the patients by catheter site, gender (P = 0.004), developing complications (P = 0.009), and final decision stage (P = 0.001) were statistically significant. While 174 (16.7%) of all patients were treated on an outpatient basis, 783 (75.1%) of them were found to be cured, and 85 (8.2%) died (P = 0.001, Table 2).
| Catheter area inserted | Total, n (%) | P value | ||||||
| R jugular, n (%) | L jugular, n (%) | R subclavian, n (%) | L subclavian, n (%) | R femoral, n (%) | L femoral, n (%) | |||
| Gender | ||||||||
| Female | 248 (42.0) | 73 (47.4) | 20 (29.4) | 23 (26.1) | 30 (39.0) | 29 (45.3) | 423 (40.6) | 0.009 |
| Male | 343 (58.0) | 81 (52.6) | 48 (70.6) | 65 (73.9) | 47 (61.0) | 35 (54.7) | 619 (59.4) | |
| Complication | ||||||||
| No | 583 (98.6) | 149 (96.8) | 63 (92.6) | 75 (85.2) | 49 (63.6) | 46 (71.9) | 965 (92.6) | 0.001 |
| Pntx | 0 | 0 | 1 (1.5) | 3 (3.4) | 0 | 0 | 4 (0.4) | |
| GW | 0 | 0 | 0 | 0 | 1 (1.3) | 1 (1.6) | 2 (0.2) | |
| Bleeding | 2 (0.3) | 0 | 0 | 4 (4.5) | 1 (1.3) | 1 (1.6) | 8 (0.8) | |
| WI | 2 (0.3) | 1 (0.6) | 1 (1.5) | 1 (1.1) | 2 (2.6) | 6 (9.4) | 13 (1.2) | |
| AI | 4 (0.7) | 4 (2.6) | 2 (2.9) | 3 (3.4) | 11 (14.3) | 3 (4.7) | 27 (2.6) | |
| Sepsis | 0 | 0 | 1 (1.5) | 2 (2.3) | 13 (16.9) | 7 (10.9) | 23 (2.2) | |
| Decision | ||||||||
| OPT | 104 (17.6) | 28 (18.2) | 12 (17.6) | 14 (15.9) | 9 (11.7) | 7 (10.7) | 174 (16.7) | 0.001 |
| DWH | 484 (81.9) | 121 (78.6) | 46 (67.6) | 58 (63.6) | 35 (45.5) | 41 (64.1) | 783 (75.1) | |
| Mortality | 3 (0.5) | 5 (3.2) | 10 (14.7) | 18 (20.5) | 33 (42.9) | 16 (25.0) | 85 (8.2) | |
| Total | 591 (100) | 154 (100) | 68 (100) | 88 (100) | 77 (100) | 64 (100) | 1042 (100) | |
In the analysis of patients with their diagnosis according to the catheterized region, in general, the right IJV catheter was inserted most often. In addition, the right FV in multiple organ failure, the left SCV in chest injuries, burns, piercing-cutting tool injuries, and cardiopulmonary resuscitation, and the right SCV in cardiovascular diseases were the most common catheter-inserted vein (Table 3).
| Diagnosis | Catheter area inserted | Total, n (%) | |||||
| R jugular, n (%) | L jugular, n (%) | R subclavian, n (%) | L subclavian, n (%) | R femoral, n (%) | L femoral, n (%) | ||
| Renal diseases | 228 (38.5) | 43 (27.9) | 1 (1.5) | 2 (2.3) | 6 (7.8) | 5 (7.8) | 285 (27.3) |
| Respiratory diseases | 45 (7.6) | 8 (5.1) | 3 (4.4) | 3 (3.4) | 16 (20.8) | 6 (9.4) | 81 (7.8) |
| Endocrine diseases | 34 (5.8) | 7 (4.5) | 1 (1.5) | 0 | 4 (5.2) | 0 | 46 (4.4) |
| Multiple organ insufficiency | 0 | 0 | 1 (1.5) | 2 (2.3) | 12 (15.6) | 7 (10.9) | 22 (2.1) |
| Gastrointestinal system bleeding | 56 (9.5) | 12 (7.8) | 2 (2.9) | 0 | 0 | 3 (4.7) | 73 (7.0) |
| Gastrointestinal system perforations | 27 (4.6) | 2 (1.3) | 2 (2.9) | 0 | 5 (6.5) | 1 (1.6) | 37 (3.6) |
| Cerebrovascular diseases | 61 (10.3) | 16 (10.4) | 0 | 1 (1.1) | 4 (5.2) | 3 (4.7) | 85 (8.2) |
| Thoracic traumas | 1 (0.2) | 0 | 7 (10.3) | 14 (15.9) | 0 | 0 | 22 (2.1) |
| Traffic accidents | 12 (2.0) | 7 (4.5) | 1 (1.5) | 2 (2.3) | 0 | 0 | 22 (2.1) |
| Malignancies | 30 (5.1) | 7 (4.5) | 4 (5.9) | 1 (1.1) | 4 (5.2) | 4 (6.3) | 50 (4.8) |
| Firearm injury | 5 (0.8) | 3 (1.9) | 3 (4.4) | 4 (4.5) | 1 (1.3) | 1 (1.6) | 17 (1.6) |
| Cardiac diseases | 39 (6.6) | 22 (14.3) | 1 (1.5) | 1 (1.1) | 5 (6.5) | 13 (20.3) | 81 (7.8) |
| Cardiovascular diseases | 1 (0.2) | 2 (1.3) | 3 (4.4) | 3 (3.4) | 6 (7.8) | 0 | 15 (1.4) |
| Falls | 26 (4.4) | 15 (9.7) | 12 (17.6) | 7 (8.0) | 3 (3.9) | 6 (9.4) | 69 (6.6) |
| Burns | 22 (3.7) | 9 (5.8) | 18 (26.5) | 27 (30.7) | 8 (10.4) | 12 (18.8) | 96 (9.2) |
| Amputation | 1 (0.2) | 1 (0.6) | 0 | 2 (2.3) | 0 | 0 | 4 (0.4) |
| Penetrating tool injury | 3 (0.5) | 0 | 8 (11.8) | 11 (12.5) | 1 (1.3) | 1 (1.6) | 24 (2.3) |
| Cardiopulmonary resuscitation | 0 | 0 | 1 (1.5) | 8 (9.1) | 2 (2.6) | 2 (3.1) | 13 (1.2) |
| Total | 591 (100) | 154 (100) | 68 (100) | 88 (100) | 77 (100) | 64 (100) | 1042 (100) |
The analysis of the patients according to the services they received while hospitalized after being catheterized is shown in Table 4.
| Hospital services | Catheter area inserted | Total, n (%) | |||||
| R jugular, n (%) | L jugular, n (%) | R subclavian, n (%) | L subclavian, n (%) | R femoral, n (%) | L femoral, n (%) | ||
| Emergency department | 94 (15.9) | 27 (17.5) | 12 (17.6) | 14 (15.9) | 10 (13.0) | 10 (15.6) | 167 (16) |
| Infectious diseases service | 11 (1.9) | 2 (1.3) | 1 (1.5) | 1 (1.1) | 3 (3.9) | 4 (6.3) | 22 (2.1) |
| General internal medicine service | 173 (29.3) | 45 (29.2) | 5 (7.4) | 1 (1.1) | 9 (11.7) | 8 (12.5) | 241 (23.1) |
| Nephrology service | 99 (16.8) | 21 (13.6) | 0 | 3 (3.4) | 7 (9.1) | 5 (7.8) | 135 (13) |
| Gastroenterology service | 29 (4.9) | 7 (4.5) | 0 | 0 | 0 | 2 (3.1) | 38 (3.6) |
| Intensive care unit | 40 (6.8) | 10 (6.5) | 13 (19.1) | 17 (19.3) | 31 (40.3) | 20 (31.3) | 131 (12.6) |
| Cardiology service | 12 (2.0) | 3 (1.9) | 1 (1.5) | 2 (2.3) | 1 (1.3) | 1 (1.6) | 20 (1.9) |
| Brain surgery service | 24 (4.1) | 7 (4.5) | 5 (7.4) | 7 (8.0) | 2 (2.6) | 3 (4.7) | 48 (4.6) |
| Thoracic surgery service | 4 (0.7) | 4 (2.6) | 6 (8.8) | 13 (14.8) | 4 (5.2) | 2 (3.1) | 33 (3.2) |
| Chest diseases service | 18 (3.0) | 7 (4.5) | 0 | 1 (1.1) | 1 (1.3) | 1 (1.6) | 28 (2.7) |
| General surgery service | 46 (7.8) | 3 (1.9) | 8 (11.8) | 9 (10.2) | 7 (9.1) | 4 (6.3) | 77 (7.4) |
| Cardiovascular surgery service | 10 (1.7) | 0 | 7 (10.3) | 10 (11.4) | 1 (1.3) | 1 (1.6) | 29 (2.8) |
| Orthopedics and traumatology service | 10 (1.7) | 13 (8.4) | 10 (14.7) | 6 (6.8) | 0 | 2 (3.1) | 41 (3.9) |
| Plastic and reconstructive surgery service | 4 (0.7) | 2 (1.3) | 0 | 4 (4.5) | 0 | 1 (1.6) | 11 (1.1) |
| Neurology service | 17 (2.9) | 3 (1.9) | 0 | 0 | 1 (1.3) | 0 | 21 (2.0) |
| Total | 591 (100) | 154 (100) | 68 (100) | 88 (100) | 77 (100) | 64 (100) | 1042 (100) |
In receiver operating characteristic curve analysis of hospitalization time and mortality, the area under curve was 0.575, the 95% confidence interval was 0.496-0.653, the sensitivity was 71%, and the specificity was 89% (P = 0.001) (Figure 1).
Intravenous catheters, one of the indispensable tools in modern medical practices, are applied for specific purposes and can be used for a long time. Although central venous catheters provide great benefits for patients, they also cause significant mortality and morbidity due to both mechanical and infectious complications[11,12]. In emergencies and critical patient follow-up, CVC is often needed. However, there are important points to be considered in CVC. First of all, it should be preferred to use a central vein with a large flow rate and high current. For this purpose, percutaneous IJV, SCV, and FV are used in CVC[4]. Right IJV is preferred primarily because of its straight connection with the superior vena cava and its short distance to the right atrium[7]. Left IJV should be the next choice because it reaches the superior vena cava by angulation twice, and catheterization is technically difficult. If there are coagulation and bleeding disorders, SCV catheterization is high risk, and in these cases, extrathoracic veins such as IJV or FV should be used[3,7,8]. Mickley[8] stated that the right IJV should be used if possible for central venous interventions and hemodialysis catheters. Central vein catheterization is a generally accepted protocol using the original Seldinger technique[9]. The Seldinger technique was used in all cases, and the rules of asepsis were adhered to. Right IJV was observed in 56.7% of the cases, left IJV in 14.8%, right SCV in 6.5%, left SCV in 8.4%, right FV in 7.4%, and left FV in 6.1%.
CVC can cause some complications. Early complications include arterial puncture, development of hematoma, nerve injury, pneumothorax, hemothorax, difficulty in cannulation, and arrhythmia. No complications were observed in 92.9% of our patients, most of whom had IJV intervention. In addition to expected complications such as pneumothorax and hemothorax, complications such as brachial plexus injury due to SCV catheterization or massive retroperitoneal hemorrhage due to femoral catheterization can be seen[13,14]. Pneumothorax was seen in 4 (0.4%) cases, one right subclavian and three left subclavian cases. All of these patients were cachectic and in poor general condition. Catheter dysfunction is caused by catheter malposition, catheter kinking, or catheter compression[15,16]. Bending and breaking of the guidewire in the vein was detected in a total of 2 (0.2%) patients, one in the left SCV and the other in the right FV. In preventing early catheter dysfunction, IJV catheterization may be an advantage in priority. In total, 8 (0.8%) of the patients had bleeding, 30 patients (2.9%) had artery puncture, 1 patient had hematoma, and 2 patients had difficulty catheterizing. In similar studies, the incidence of carotid artery puncture was reported between 2.0%-9.9% during catheterization of IJV[5]. Most of the difficulties in arterial puncture and cannulation observed in our catheterization-related cases were obesity, short neck, elderly, and poor general condition as the main cause of these early complications.
During jugular catheterization, complications such as Horner Syndrome, arrhythmia, and cardiac tamponade have been reported, as well as the development of carotid-jugular arteriovenous fistula due to carotid puncture[17,18]. In a total of 4 (0.4%) cases, no other complications were observed except arrhythmia. It is recom
The average staying time of temporary catheters should not exceed 3-4 wk for IJV and SCV catheters and 2 wk for femoral catheters[5]. The average length of stay in our study did not exceed 2 wk. The length of stay of the catheter is associated with both thrombotic complications and the risk of infection[20].
In the study of Cook et al[21], it was stated that changing catheters at short intervals did not decrease the frequency of colonization and infection. Because catheter insertion is a traumatic procedure and there is a risk that asepsis conditions may deteriorate during catheter insertion, installing a new catheter in itself poses a risk of catheter-related infection. It is known that there is a directly proportional relationship between catheter insertion time and catheter colonization and catheter-related infection[22,23]. Chen et al[24] found that the stay of the catheter for more than 7 d was significant in terms of catheter-related infection.
Infections developing in CVC for various reasons lead to very serious complications including patient mortality[25]. Early infection is associated with contamination during catheter insertion, skin infection, or catheter pathway infection. Late infection is often accompanied by endoluminal catheter contamination[26]. Two types of infections are observed: local infection and systemic infections. Staphylococcus aureus (S. aureus) and S. epidermiditis are the most common microorganisms isolated during catheter-related bacteremia. This risk increases in the presence of wound infection. The risk of infection is higher with FV catheters than with SCV and IJV catheters[27]. In our study, wound infection due to catheters was detected in 13 (1.2%) cases. Localized infection findings were observed in 8 (0.7%) FV, 3 (0.3%) IJV, and 2 (0.2%) SCV. Although S. aureus and S. epidermiditis grew in the samples taken from the wound site, there was no growth in the samples taken from the catheter tip. Blood cultures were not routinely sent from the patients. We think that there was no growth in the catheter tip cultures, care for sterility while inserting the catheter, careful and regular dressing of the insertion site, and not using the catheters for more than 3 wk.
Blot et al[28] found that S. aureus, coagulase negative Staphylococcus, and Pseudo
CVC is an indispensable application especially for emergency services and brings with it the risk of many complications. Complications in the subclavian and FVs are more common in long-term use. Jugular vein catheterization can be preferred primarily due to the difficulties in application and the low number of complications. In addition, prevention of risk factors with infection control policies and measures developed can significantly reduce catheter-related infection rates.
Risk assessment in patients with a central venous catheter is necessary to prevent some unwanted consequences associated with invasive procedures.
The impact on the clinical, morbidity, and mortality of patients with central venous catheters in the emergency room population is worth investigating.
We aimed to determine whether there is a definite risk factor in short-term emergency room stay as the primary outcome of patients with central venous catheters and as a secondary outcome whether there is long-term morbidity and mortality at the time of hospitalization.
In this study, 1042 patients who were admitted to the emergency department between 2005 and 2015 were analyzed, retrospectively. The patients in whom a central venous catheter was placed in the study were divided into three groups as jugular, subclavian, and femoral. Complications, diagnosis, and hospital stay after catheter insertion were evaluated.
The mean age of the patients was 60.99 ± 19.85 years; 423 (40.6%) of them were women. Hospitalization time was 11.89 ± 16.38 d. The mean age of the patients with jugular catheters was 60.74 ± 20.20 years, and 339 (40%) of them were women. The mean age of subclavian catheter patients was 59.66 ± 19.17 years, and 42 (27.3%) of them were women. In femoral catheters, the mean age was 63.67 ± 18.57 years, and 42 (42%) were women. There was a significant relationship between the inserted catheters with gender (P = 0.009) and hospitalization time (P = 0.040). , the biochemical values of the placed catheters were statistically significant with blood glucose, blood urea nitrogen, creatinine, and serum potassium. A significant association was observed in the analysis of patients according to complications (P = 0.001) and outcome stage (P = 0.001). While 174 (16.7%) of all patients were treated on an outpatient basis, 783 (75.1%) of them were found to be cured, and 85 (8.2%) died. In receiver operating characteristic curve analysis of hospitalization time and mortality, the area under curve was 0.575, the 95% confidence interval was 0.496-0.653, the sensitivity was 71%, and the specificity was 89% (P = 0.040).
The jugular vein is safer and more comfortable for patient compliance between central venous catheters. Femoral vein catheters are at higher risk for infection. Changing central catheters frequently does not reduce the risk of infection and complications.
Subclavian catheters have a high risk of hemopneumothorax in cachectic patients. Jugular catheters are safe. However, it is not preferred due to the discomfort of the patients and the limited neck movements. It is difficult to attach a jugular catheter to short and obese patients. Also, artery puncture is common. Femoral catheters are the group with the highest infection rate.
| 1. | The European Emergency Medicine Core Curriculum. Turkey Emergency Medicine Society, European Society for Emergency Medicine Association (EUSEM), and the European Society for Emergency Medical Specialists (UEMS) Emergency Medicine Multidisciplinary Committee (EMMC) approved, use for the Core Curriculum Workgroup Document 2008. Brussels: Belgium, 2008. |
| 2. | Türkdemir AH, Güleç MA, Eraslan S, Arıca F, Akkaya M, Giray F. Effectiveness of vascular access in penetrating injuries. Academic Emerg Med J. 2007;55:22-38. |
| 3. | Ruesch S, Walder B, Tramèr MR. Complications of central venous catheters: internal jugular vs subclavian access--a systematic review. Crit Care Med. 2002;30:454-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 402] [Cited by in RCA: 385] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 4. | Sznajder JI, Zveibil FR, Bitterman H, Weiner P, Bursztein S. Central vein catheterization. Failure and complication rates by three percutaneous approaches. Arch Intern Med. 1986;146:259-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 145] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. 2003;348:1123-1133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1496] [Cited by in RCA: 1471] [Article Influence: 64.0] [Reference Citation Analysis (0)] |
| 6. | Mansfield PF, Hohn DC, Fornage BD, Gregurich MA, Ota DM. Complications and failures of subclavian-vein catheterization. N Engl J Med. 1994;331:1735-1738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 607] [Cited by in RCA: 551] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 7. | Lefrant JY, Muller L, De La Coussaye JE, Prudhomme M, Ripart J, Gouzes C, Peray P, Saissi G, Eledjam JJ. Risk factors of failure and immediate complication of subclavian vein catheterization in critically ill patients. Intensive Care Med. 2002;28:1036-1041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 101] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 8. | Mickley V. Central venous catheters: many questions, few answers. Nephrol Dial Transplant. 2002;17:1368-1373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | SELDINGER SI. Catheter replacement of the needle in percutaneous arteriography; a new technique. Acta radiol. 1953;39:368-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2369] [Cited by in RCA: 2070] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
| 10. | Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988;16:128-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4280] [Cited by in RCA: 4339] [Article Influence: 114.2] [Reference Citation Analysis (0)] |
| 11. | Henderson DK. Infections caused by percutaneous intravascular devices. In: Mandeli GL, Bennett JE, Dolin R. Principles and Practice of Infectious Diseases. 6th ed. Philadelphia: Churchill-Livingstone IIne, 2005: 3347-3362. |
| 12. | Polderman KH, Girbes AJ. Central venous catheter use. Part 1: mechanical complications. Intensive Care Med. 2002;28:1-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 212] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 13. | Karakaya D, Baris S, Güldogus F, Incesu L, Sarihasan B, Tür A. Brachial plexus injury during subclavian vein catheterization for hemodialysis. J Clin Anesth. 2000;12:220-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Akata T, Nakayama T, Kandabashi T, Kodama K, Takahashi S. Massive retroperitoneal hemorrhage associated with femoral vein cannulation. J Clin Anesth. 1998;10:321-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Puri VK, Carlson RW, Bander JJ, Weil MH. Complications of vascular catheterization in the critically ill. A prospective study. Crit Care Med. 1980;8:495-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 77] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Muhm M, Sunder-Plassmann G, Apsner R, Pernerstorfer T, Rajek A, Lassnigg A, Prokesch R, Derfler K, Druml W. Malposition of central venous catheters. Incidence, management and preventive practices. Wien Klin Wochenschr. 1997;109:400-405. [PubMed] |
| 17. | Droll KP, Lossing AG. Carotid-jugular arteriovenous fistula: case report of an iatrogenic complication following internal jugular vein catheterization. J Clin Anesth. 2004;16:127-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Taskapan H, Oymak O, Dogukan A, Utas C. Horner's syndrome secondary to internal jugular catheterization. Clin Nephrol. 2001;56:78-80. [PubMed] |
| 19. | Gladwin MT, Slonim A, Landucci DL, Gutierrez DC, Cunnion RE. Cannulation of the internal jugular vein: is postprocedural chest radiography always necessary? Crit Care Med. 1999;27:1819-1823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 64] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 20. | Crain MR, Mewissen MW, Ostrowski GJ, Paz-Fumagalli R, Beres RA, Wertz RA. Fibrin sleeve stripping for salvage of failing hemodialysis catheters: technique and initial results. Radiology. 1996;198:41-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 81] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 21. | Cook D, Randolph A, Kernerman P, Cupido C, King D, Soukup C, Brun-Buisson C. Central venous catheter replacement strategies: a systematic review of the literature. Crit Care Med. 1997;25:1417-1424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 201] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 22. | Crump JA, Collignon PJ. Intravascular catheter-associated infections. Eur J Clin Microbiol Infect Dis. 2000;19:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 168] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 23. | Fraenkel DJ, Rickard C, Lipman J. Can we achieve consensus on central venous catheter-related infections? Anaesth Intensive Care. 2000;28:475-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Chen HS, Wang FD, Lin M, Lin YC, Huang LJ, Liu CY. Risk factors for central venous catheter-related infections in general surgery. J Microbiol Immunol Infect. 2006;39:231-236. [PubMed] |
| 25. | Ulusoy S, Akan H, Arat M, Baskan S, Bavbek S, Çakar N, Çetinkaya ŞY, Somer A, Şimşek YS. Intravascular Catheter Infections Prevention Guide. Turkish J Hosp Infect. 2005;9:5-9. |
| 26. | McKinley S, Mackenzie A, Finfer S, Ward R, Penfold J. Incidence and predictors of central venous catheter related infection in intensive care patients. Anaesth Intensive Care. 1999;27:164-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 34] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | Charalambous C, Swoboda SM, Dick J, Perl T, Lipsett PA. Risk factors and clinical impact of central line infections in the surgical intensive care unit. Arch Surg. 1998;133:1241-1246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 28. | Blot F, Nitenberg G, Chachaty E, Raynard B, Germann N, Antoun S, Laplanche A, Brun-Buisson C, Tancrède C. Diagnosis of catheter-related bacteraemia: a prospective comparison of the time to positivity of hub-blood vs peripheral-blood cultures. Lancet. 1999;354:1071-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 323] [Cited by in RCA: 263] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Critical care medicine
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ferreira GSA S-Editor: Gao CC L-Editor: Filipodia P-Editor: Wang LL