Published online Jul 9, 2021. doi: 10.5492/wjccm.v10.i4.102
Peer-review started: January 20, 2021
First decision: February 15, 2021
Revised: February 18, 2021
Accepted: April 22, 2021
Article in press: April 22, 2021
Published online: July 9, 2021
Processing time: 167 Days and 13.1 Hours
The glucocorticoid receptor (GCR) and the mineralocorticoid receptor (MR) are members of the steroid receptor superfamily of hormone-dependent transcription factors. The receptors are structurally and functionally related. They are localized in the cytosol and translocate into the nucleus after ligand binding. GCRs and MRs can be co-expressed within the same cell, and it is believed that the balance in GCR and MR expression is crucial for homeostasis and plays a key role in normal adaptation. In critical illness, the hypothalamic-pituitary-adrenal axis is activated, and as a consequence, serum cortisol concentrations are high. However, a number of patients exhibit relatively low cortisol levels for the degree of illness severity. Glucocorticoid (GC) actions are facilitated by GCR, whose dysfunction leads to GC tissue resistance. The MR is unique in this family in that it binds to both aldosterone and cortisol. Endogenous GCs play a critical role in controlling inflammatory responses in critical illness. Intracellular GC concentrations can differ greatly from blood levels due to the action of the two 11β-hydroxysteroid dehydrogenase isozymes, type 1 and type 2. 11β-hydroxysteroid dehydrogenases interconvert endogenous active cortisol and intrinsically inert cortisone. The degree of expression of the two isozymes has the potential to dramatically influence local GC availability within cells and tissues. In this review, we will explore the clinical studies that aimed to elucidate the role of MR and GCR expression in the inflammatory response seen in critical illness.
Core Tip: Endogenous glucocorticoids (GCs) play a critical role in controlling inflammatory responses in critical illness. Intracellular GC concentrations can differ greatly due to the action of the two 11β-hydroxysteroid dehydrogenase isozymes. The degree of expression of the two isozymes has the potential to dramatically influence local GC availability. The GC receptor and the mineralocorticoid receptor are members of the steroid receptor superfamily of hormone-dependent transcription factors. The study of the mineralocorticoid receptor and GC receptor expression and function in the inflammatory response seen in critical illness might aid in identifying the patients who will benefit from exogenous corticosteroid administration.
- Citation: Vassiliou AG, Athanasiou N, Vassiliadi DA, Jahaj E, Keskinidou C, Kotanidou A, Dimopoulou I. Glucocorticoid and mineralocorticoid receptor expression in critical illness: A narrative review. World J Crit Care Med 2021; 10(4): 102-111
- URL: https://www.wjgnet.com/2220-3141/full/v10/i4/102.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v10.i4.102
The glucocorticoid receptor (GCR) and the mineralocorticoid receptor (MR) are members of the steroid receptor superfamily of hormone-dependent transcription factors. The receptors are structurally and functionally related. They are localized in the cytosol and translocate into the nucleus after ligand binding. GCRs and MRs can be co-expressed within the same cell, and it is believed that the balance in GCR and MR expression is crucial for homeostasis and plays a key role in normal adaptation.
In critical illness, the hypothalamic-pituitary-adrenal (HPA) axis is activated, and as a consequence, serum cortisol concentrations are high. However, in a number of patients cortisol levels are relatively low for their illness severity. Glucocorticoid (GC) actions are mediated by GCR, whose dysfunction leads to GC tissue resistance. The MR is unique in this family in that it binds to both aldosterone and cortisol.
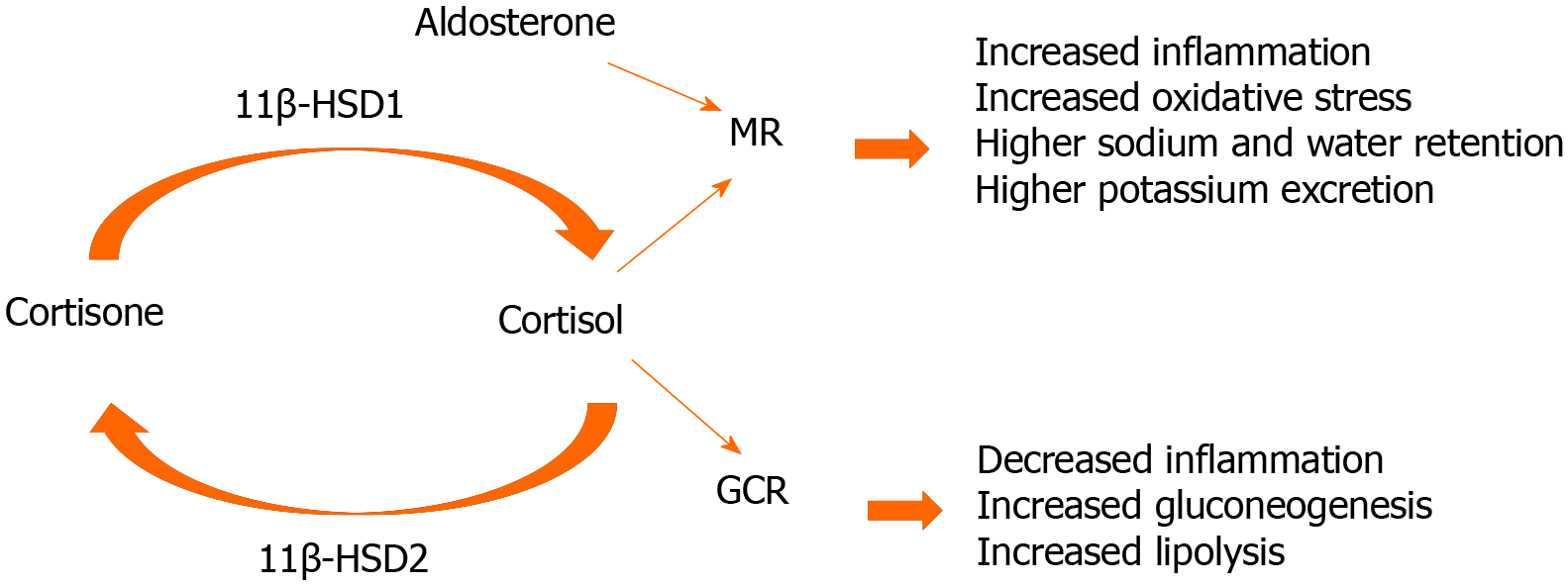
Endogenous GCs play a critical role in controlling inflammatory responses in critical illness. Intracellular GC concentrations may be greatly different compared to blood levels due to the action of the 11β-hydroxysteroid dehydrogenase (11β-HSD) isozymes, type 1 and type 2. 11β-HSDs interconvert endogenous active cortisol and intrinsically inert cortisone. The degree of expression of the two isozymes has the potential to dramatically influence local GC availability within cells and tissues.
During critical illness the HPA axis is activated, resulting in increased serum adrenocorticotropic hormone and cortisol concentrations[1-4]. However, a subset of patients present with low serum cortisol levels despite their illness severity[5,6]. Critical illness-related corticosteroid insufficiency (CIRCI) is characterized by the organism’s inability to produce adequate cortisol or tissue resistance to its actions, or both[7].
Sepsis and septic shock are the most common causes of mortality in critically-ill patients. GCs, the end-products of the HPA axis, have been used for over 40 years in the treatment of sepsis. The Surviving Sepsis Campaign Guidelines 2016 recom
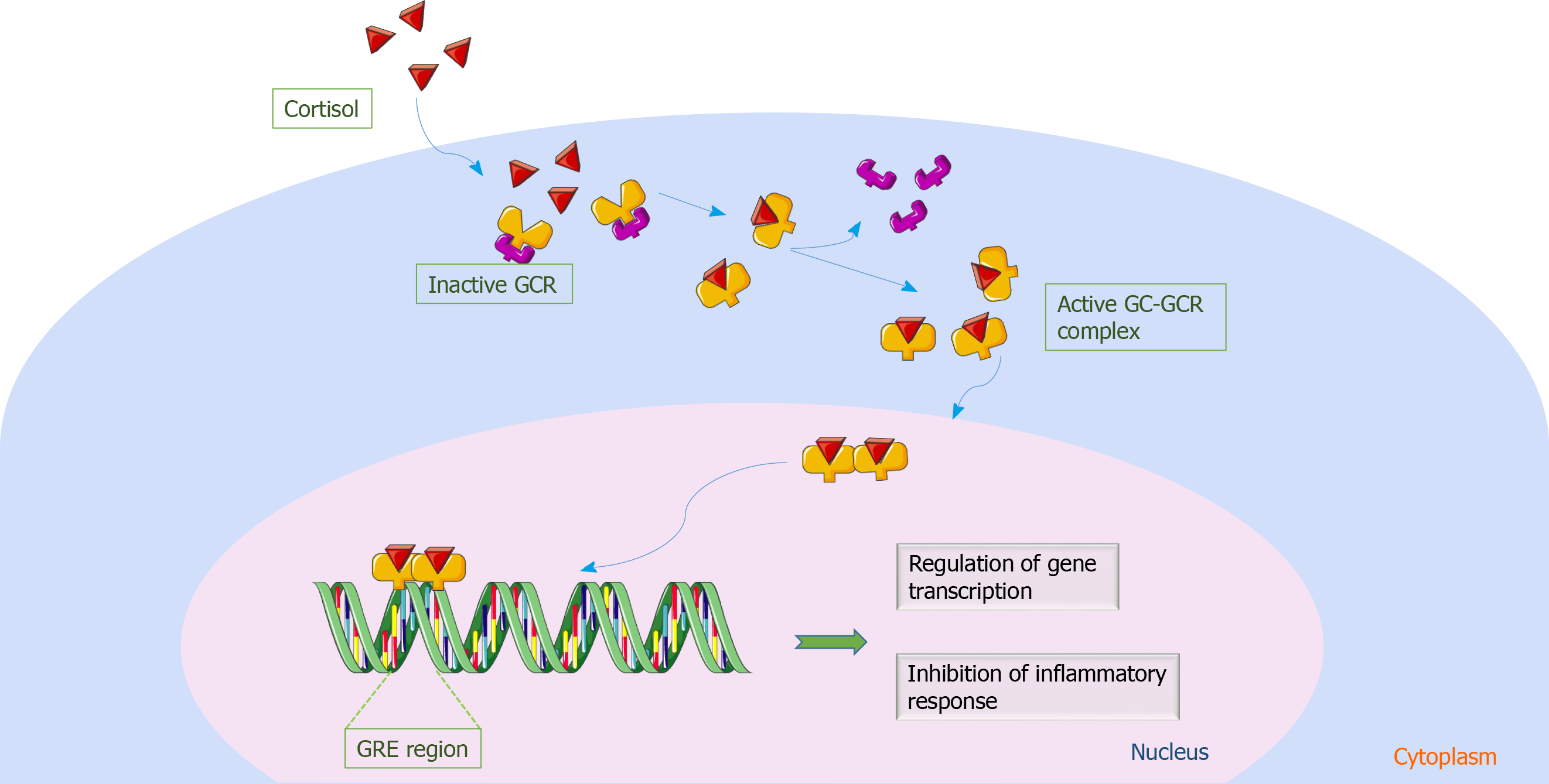
Cortisol signaling is mediated by GCR, a ubiquitous intracellular receptor protein. Alternative splicing of the primary transcript gives rise to two highly homologous GCR isoforms[13]. GCR-α is the functionally active receptor; once it binds to cortisol, the receptor-cortisol complex translocates from the cytosol to the nucleus. In the nucleus, the complex exerts transcriptional activation or repression by directly binding to genes that contain GC responsive elements[14], resulting in the inhibition of the inflammatory response[15,16]. On the contrary, the function of GCR-β has not been well-explored. It is known to suppress GCR-α activity and is unable to bind both natural and synthetic ligands[17-19]. Figure 1 diagrammatically represents cortisol signaling via GCR.
The Sepsis-3 guidelines suggest the use of hydrocortisone in septic shock patients who are resistant to fluid administration and vasoactive agents[20]. Not all patients respond to this therapy, suggesting the existence of GC resistance. GC resistance is defined as the inability of GCs to exert their effects on target tissues[21]. It is characterized by decreased sensitivity of immune cells to GCs, which under normal conditions terminate the inflammatory response[22]. Therefore, it becomes apparent that apart from cortisol levels, how tissues respond to cortisol is as important. It has been suggested that the extent of cortisol’s effect might be analogous to GCR expression, subtype and affinity in a specific target cell[23]. Such an example is the increased expression of GCR-β in certain tissues in inflammatory diseases, which has been associated with decreased sensitivity to GCs[24].
GC resistance may be a consequence of decreased GCR expression, GCR affinity for the ligand, nuclear translocation and DNA binding or may be due to altered transcription factor interaction. Most data on GC resistance in critical illness originates from experimental models involving sepsis-induced injury[25-29]. Essentially these studies have shown downregulation of GCR-α and induction of GCR-β expression[30-33].
Human clinical studies in critically-ill patients have mostly investigated cortisol availability, while only a few have explored the role of GCR. GC resistance has been described in a cohort of septic patients, demonstrating reduced GCR-α and elevated GCR-β expression levels in septic patients compared to healthy subjects; these results suggest that treatment with steroids might aggravate GC resistance in patients with increased GCR-β levels[34]. A transient, increased GCR-β expression has been reported in sepsis; moreover, the septic patients’ sera could induce GC resistance in vitro[35]. Another study reported reduced GCR-α expression levels in sepsis[36], and diminished GCR protein levels have also been described in various organs during sepsis[37]. A decreased number of GCR-α and increased GCR-β receptors has been shown in heart and liver biopsies in the context of sepsis[25]. It has been shown that in septic shock, GCR expression increased, while GCR binding capacity decreased, proposing that it is the decreased GCR binding capacity and not the number of receptors that interferes with the response to exogenous or endogenous GCs[38]. In contrast, GCR number and affinity in septic patients did not differ from control subjects, suggesting that GCs could be effective in the hemodynamic compensatory phase of sepsis[39]. Increased GCR-α expression has been shown in the acute phase of sepsis, questioning the need for exogenous steroids at this phase[40]. Only one study has demonstrated downregulation of cortisol binding in critically-ill, ventilated patients[41]. Finally, our group was able to demonstrate that critically-ill steroid-free patients have a highly variable expression of both GCR isoforms in peripheral polymorphonuclear cells. Moreover, GCR expression and HPA axis function undergo a biphasic response during acute or subacute critical illness; this dissociation of reduced GCR expression and elevated cortisol might imply an abnormal stress response[42,43].
In coronavirus disease 2019 (COVID-19), results from the RECOVERY trial suggested significant benefits of steroid administration in critically-ill COVID-19 patients[44]. Specifically, the trial demonstrated that dexamethasone reduced mortality risk by 17%. A study in noncritically-ill COVID-19 patients showed that the HPA axis was activated. Patients exhibited an increase in cortisol, which was significantly higher than in those without COVID-19 infection, and these cortisol levels were associated with higher mortality rates[43]. Another study found that cortisol levels were lower in critically-ill COVID-19 patients compared to critically-ill non-COVID-19 patients[45]. In fact, nearly 70% of the COVID-19 critically-ill patients had plasma cortisol concentrations < 10 μg/dL, meeting CIRCI criteria. However, so far, data on COVID-19 and GCR-α expression are lacking.
Ascorbic acid (vitamin C) levels are depleted in critically-ill patients. This vitamin has been shown to play a crucial role in HPA axis function. The adrenal glands contain very high concentrations of ascorbic acid and use it to synthesize cortisol[46]. At the cellular level, vitamin C works synergistically with corticosteroids by restoring GCR function. Specifically, ascorbic acid reverses GCR oxidation, restoring GC-responsiveness in oxidant conditions. The end result is increased GC availability and GCR-α activation[47].
Overall, it seems that during critical illness GCR expression is independently regulated. This might explain the different responses seen in patients to exogenously administered steroids or endogenously secreted cortisol. Apart from GCR expression, the role of post-translational modifications, GCR complex components and the efficiency of nuclear translocation of the GCR complex should be the focus of future clinical studies.
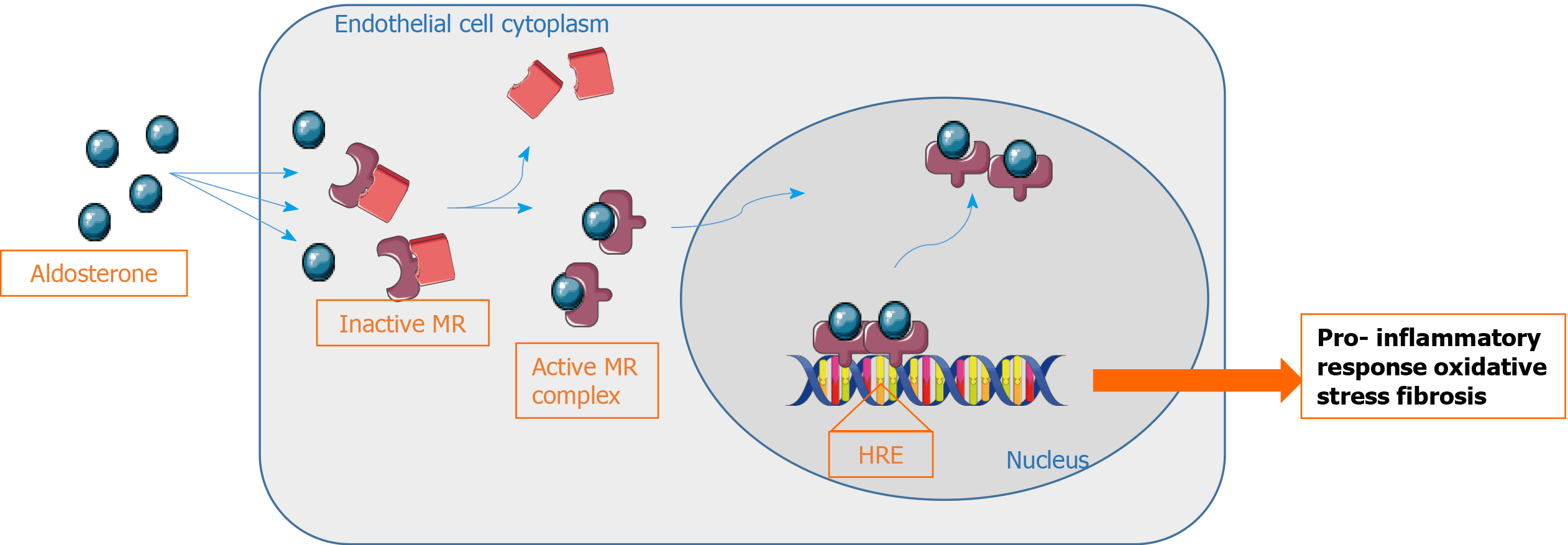
The MR is, along with the GCR, a member of the steroid receptor superfamily of hormone-dependent transcription factors. The receptors are structurally and functionally related. Similar to GCR, MR is also localized in the cytosol and translocates into the nucleus after ligand binding. In the nucleus, the ligand-receptor complex recognizes specific DNA regions and activates target gene expression[48]. While GCR is relatively ubiquitously expressed and exclusively binds GCs, the MR shows a more restricted expression pattern, and can bind both aldosterone and cortisol. MR is mostly expressed in epithelial cells of renal distal tubules, colon, sweat and salivary glands, and is implicated in sodium reabsorption, water homeostasis and potassium secretion[49]. The classical ligand for MR is aldosterone, the main mineralocorticoid steroid hormone, through activation of the renin-angiotensin system. Aldosterone is the principal regulator of salt and water balance but can also act on nonepithelial sites, contributing significantly to cardiovascular disease[50].
Hyperreninemic hypoaldosteronism may occur during critical illness and has been associated with a greater proinflammatory status, a higher degree of acute organ failure, and worse prognosis. It has been attributed to impaired adrenal response to increasing renin levels[51-53]. The recent demonstration of the reduced mortality in septic shock patients treated with adjunctive GCs combined with fludrocortisone[9], and the effectiveness of angiotensin II in treating vasodilatory shock[54] has renewed interest in the role of the MR in critical illness[55].
The MR, originally thought to be expressed only in kidneys, is now known to have a wider distribution. At the organ level, it is expressed in heart, vessels, brain, and adipose tissue[56]. MR signaling induces inflammation, oxidative stress, and fibrosis/remodeling, thereby causing tissue and organ damage, particularly in the heart and vessels[49]. Furthermore, clinical studies have reported a beneficial outcome of MR antagonism in patients with cardiovascular diseases, mainly due to the prevention of inflammatory damage[57]. At the cellular level, MR is expressed in vascular cells, adipocytes, and immune cells[58]. This inflammatory involvement of MR and aldosterone in cardiovascular diseases suggests an association with immune system changes. It has been consistently reported that aldosterone stimulation promotes proinflammatory responses[59,60]. In human leukocytes, MR expression has been shown in CD34+ hematopoietic progenitor cells, in peripheral blood T and B lymphocytes, macrophages, dendritic cells, and neutrophils[61]. In macrophages, lymphocytes and dendritic cells, MR signaling induces proinflammatory responses[62,63]. The MR antagonist, spironolactone, was shown to have anti-inflammatory effects on cultured human peripheral blood mononuclear cells isolated from healthy subjects. Furthermore, angiotensin II induced aldosterone synthesis and enhanced cytokine production through an MR-dependent mechanism in human peripheral blood mononuclear cells[64,65]. In Figure 2, MR signaling is depicted.
Both the innate and adaptive immune responses depend on the adhesion and migration of leukocytes across endothelial cells towards the inflamed site, where they protect against invading pathogens and repair damaged tissue. At the inflamed site, neutrophils undergo constitutive apoptosis to be removed from the inflammatory environment. Normally, acute inflammation rapidly resolves. However, failure to rapidly remove apoptotic neutrophils prolongs the inflammatory response. As mentioned above, endogenous GCs play a critical role in controlling inflammatory responses. Although GCs have an immunosuppressive effect on immune cells, they exert contradictory effects on neutrophils. At the inflamed sites they exert an anti-inflammatory effect by blunting neutrophil priming, whereas they increase circulating neutrophil count by delaying their apoptosis[66]. In circumstances of uncontrolled inflammation, polymorphonuclear cells can become detrimental by causing tissue injury and organ damage in critical illness[67].
Intracellular GC concentrations may vary compared to blood levels due to the action of the two 11β-HSD isozymes. 11β-HSD interconverts endogenous active cortisol and inert cortisone, which does not bind to GCR[68]. 11β-HSD2 (encoded by the HSD11B2 gene) inactivates GCs, while 11β-HSD1 (encoded by HSD11B1) regenerates active GCs from inert keto forms, and hence modulates GC-regulated functions. Moreover, 11β-HSD1 is widely expressed in tissues that express high levels of GCR, suggesting that 11β-HSD1 modulates ligand access to GCR-α[68]. The degree of expression of these two isozymes may drastically affect local GC availability within individual cells and tissues.
11β-HSD1 is widely distributed, with its expression being highest in the liver, but is also expressed in adipose tissue, vessels, brain, and immune cells. In immune cells, 11β-HSD1 is primarily expressed in macrophages and lymphocytes, especially during inflammation[56,62,69]. 11β-HSD1 activates functionally inert GC precursors (cortisone) to active GCs (cortisol) within target tissues, and amplifies local GC actions. 11β-HSD2, except being expressed in the classical aldosterone-target tissues, is also expressed in the pancreas and the reproductive system[68]. 11β-HSD2 protects the MR from illicit occupancy by cortisol by inactivating cortisol within cells.
Aldosterone and cortisol bind the MR and have a similar affinity for the MR. The binding of cortisol or aldosterone to the MR results in different cellular responses[55]. Under physiological conditions, plasma cortisol levels are 100 × higher than aldosterone levels, and most MRs are occupied by GCs. The 11β-HSD enzymes regulate whether cortisol or aldosterone will bind to the MR. 11β-HSD type 2 metabolizes cortisol to inactive cortisone. Cortisone is unable to bind or activate the MR, and aldosterone occupies the MR. When 11β-HSD2 is not present or not functional, the ligand binding site on the MR is occupied by cortisol.
11β-HSD2 is mainly expressed in the classical aldosterone (mineralocorticoid)-target tissues, including the distal nephron, sweat and salivary glands, and colonic epithelium. 11β-HSD1 catalyzes the regeneration of active GCs, particularly in GC-target tissues, where it amplifies GC actions. In vitro, colocalization of the two enzymes within a cell results in their reciprocal regulation to minimize simultaneous expression[68]. Figure 3 diagrammatically shows the interplay between the corticoid receptors, their ligands and the 11β-HSD isozymes.
Although the immunosuppressive and anti-inflammatory activities of GCs are well documented, the expression of 11β-HSD enzymes in immune cells, and in particular polymorphonuclear cells, is not well understood. Overall, an anti-inflammatory role for 11β-HSD1 has been proposed in leukocytes, while studies have suggested that 11β-HSD2 is not expressed in these cells[70]. In human T-lymphoblastic leukemia cells, both 11β-HSD2 expression and reciprocal regulation of 11β-HSD1 and 11β-HSD2 have been shown to be associated with GC resistance[71,72].
Data for tissue resistance to GC activity are limited in critical illness. Indirect evidence suggesting altered tissue 11β-HSD activity comes from studies that found increased plasma cortisol:cortisone ratio in critically-ill septic and trauma patients[73,74]. A recent study showed that in septic shock patients, sensitivity to GCs does not appear to be mediated by changes in the expression of the 11β-HSD2 isozyme[75]. Whether the reciprocal change in 11β-HSD1/11β-HSD2 is part of an adaptive response to inflammation or contributes to GC resistance remains to be established.
Studies on the expression of GCR, MR, 11β-HSD1 and 11β-HSD2 in critically-ill patients may allow a better understanding of homeostatic regulations of GCR and MR.
Artwork was created with the use of the Smart Servier Medical Art website.
| 1. | Drucker D, McLaughlin J. Adrenocortical dysfunction in acute medical illness. Crit Care Med. 1986;14:789-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 47] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Drucker D, Shandling M. Variable adrenocortical function in acute medical illness. Crit Care Med. 1985;13:477-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 81] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Jurney TH, Cockrell JL Jr, Lindberg JS, Lamiell JM, Wade CE. Spectrum of serum cortisol response to ACTH in ICU patients. Correlation with degree of illness and mortality. Chest. 1987;92:292-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 131] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Reincke M, Allolio B, Würth G, Winkelmann W. The hypothalamic-pituitary-adrenal axis in critical illness: response to dexamethasone and corticotropin-releasing hormone. J Clin Endocrinol Metab. 1993;77:151-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 22] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Dimopoulou I, Stamoulis K, Ilias I, Tzanela M, Lyberopoulos P, Orfanos S, Armaganidis A, Theodorakopoulou M, Tsagarakis S. A prospective study on adrenal cortex responses and outcome prediction in acute critical illness: results from a large cohort of 203 mixed ICU patients. Intensive Care Med. 2007;33:2116-2121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Vassiliadi DA, Dimopoulou I, Tzanela M, Douka E, Livaditi O, Orfanos SE, Kotanidou A, Tsagarakis S. Longitudinal assessment of adrenal function in the early and prolonged phases of critical illness in septic patients: relations to cytokine levels and outcome. J Clin Endocrinol Metab. 2014;99:4471-4480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Marik PE, Pastores SM, Annane D, Meduri GU, Sprung CL, Arlt W, Keh D, Briegel J, Beishuizen A, Dimopoulou I, Tsagarakis S, Singer M, Chrousos GP, Zaloga G, Bokhari F, Vogeser M; American College of Critical Care Medicine. Recommendations for the diagnosis and management of corticosteroid insufficiency in critically ill adult patients: consensus statements from an international task force by the American College of Critical Care Medicine. Crit Care Med. 2008;36:1937-1949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 712] [Cited by in RCA: 579] [Article Influence: 32.2] [Reference Citation Analysis (0)] |
| 8. | Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, Rochwerg B, Rubenfeld GD, Angus DC, Annane D, Beale RJ, Bellinghan GJ, Bernard GR, Chiche JD, Coopersmith C, De Backer DP, French CJ, Fujishima S, Gerlach H, Hidalgo JL, Hollenberg SM, Jones AE, Karnad DR, Kleinpell RM, Koh Y, Lisboa TC, Machado FR, Marini JJ, Marshall JC, Mazuski JE, McIntyre LA, McLean AS, Mehta S, Moreno RP, Myburgh J, Navalesi P, Nishida O, Osborn TM, Perner A, Plunkett CM, Ranieri M, Schorr CA, Seckel MA, Seymour CW, Shieh L, Shukri KA, Simpson SQ, Singer M, Thompson BT, Townsend SR, Van der Poll T, Vincent JL, Wiersinga WJ, Zimmerman JL, Dellinger RP. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43:304-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3352] [Cited by in RCA: 4163] [Article Influence: 462.6] [Reference Citation Analysis (8)] |
| 9. | Annane D, Renault A, Brun-Buisson C, Megarbane B, Quenot JP, Siami S, Cariou A, Forceville X, Schwebel C, Martin C, Timsit JF, Misset B, Ali Benali M, Colin G, Souweine B, Asehnoune K, Mercier E, Chimot L, Charpentier C, François B, Boulain T, Petitpas F, Constantin JM, Dhonneur G, Baudin F, Combes A, Bohé J, Loriferne JF, Amathieu R, Cook F, Slama M, Leroy O, Capellier G, Dargent A, Hissem T, Maxime V, Bellissant E; CRICS-TRIGGERSEP Network. Hydrocortisone plus Fludrocortisone for Adults with Septic Shock. N Engl J Med. 2018;378:809-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 471] [Cited by in RCA: 652] [Article Influence: 81.5] [Reference Citation Analysis (0)] |
| 10. | Annane D, Sébille V, Charpentier C, Bollaert PE, François B, Korach JM, Capellier G, Cohen Y, Azoulay E, Troché G, Chaumet-Riffaud P, Bellissant E. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA. 2002;288:862-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2198] [Cited by in RCA: 1987] [Article Influence: 82.8] [Reference Citation Analysis (0)] |
| 11. | Sprung CL, Annane D, Keh D, Moreno R, Singer M, Freivogel K, Weiss YG, Benbenishty J, Kalenka A, Forst H, Laterre PF, Reinhart K, Cuthbertson BH, Payen D, Briegel J; CORTICUS Study Group. Hydrocortisone therapy for patients with septic shock. N Engl J Med. 2008;358:111-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1696] [Cited by in RCA: 1385] [Article Influence: 76.9] [Reference Citation Analysis (1)] |
| 12. | Venkatesh B, Finfer S, Cohen J, Rajbhandari D, Arabi Y, Bellomo R, Billot L, Correa M, Glass P, Harward M, Joyce C, Li Q, McArthur C, Perner A, Rhodes A, Thompson K, Webb S, Myburgh J; ADRENAL Trial Investigators and the Australian–New Zealand Intensive Care Society Clinical Trials Group. Adjunctive Glucocorticoid Therapy in Patients with Septic Shock. N Engl J Med. 2018;378:797-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 521] [Cited by in RCA: 707] [Article Influence: 88.4] [Reference Citation Analysis (0)] |
| 13. | Hollenberg SM, Weinberger C, Ong ES, Cerelli G, Oro A, Lebo R, Thompson EB, Rosenfeld MG, Evans RM. Primary structure and expression of a functional human glucocorticoid receptor cDNA. Nature. 1985;318:635-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1317] [Cited by in RCA: 1244] [Article Influence: 30.3] [Reference Citation Analysis (0)] |
| 14. | Kadmiel M, Cidlowski JA. Glucocorticoid receptor signaling in health and disease. Trends Pharmacol Sci. 2013;34:518-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 581] [Cited by in RCA: 643] [Article Influence: 49.5] [Reference Citation Analysis (0)] |
| 15. | Barnes PJ, Karin M. Nuclear factor-kappaB: a pivotal transcription factor in chronic inflammatory diseases. N Engl J Med. 1997;336:1066-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3573] [Cited by in RCA: 3603] [Article Influence: 124.2] [Reference Citation Analysis (0)] |
| 16. | Göttlicher M, Heck S, Herrlich P. Transcriptional cross-talk, the second mode of steroid hormone receptor action. J Mol Med (Berl). 1998;76:480-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 251] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 17. | Bamberger CM, Bamberger AM, de Castro M, Chrousos GP. Glucocorticoid receptor beta, a potential endogenous inhibitor of glucocorticoid action in humans. J Clin Invest. 1995;95:2435-2441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 449] [Cited by in RCA: 441] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 18. | Kino T, Su YA, Chrousos GP. Human glucocorticoid receptor isoform beta: recent understanding of its potential implications in physiology and pathophysiology. Cell Mol Life Sci. 2009;66:3435-3448. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 145] [Cited by in RCA: 134] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 19. | Oakley RH, Sar M, Cidlowski JA. The human glucocorticoid receptor beta isoform. Expression, biochemical properties, and putative function. J Biol Chem. 1996;271:9550-9559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 394] [Cited by in RCA: 401] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 20. | Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:801-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15803] [Cited by in RCA: 18900] [Article Influence: 1890.0] [Reference Citation Analysis (4)] |
| 21. | Chrousos GP, Detera-Wadleigh SD, Karl M. Syndromes of glucocorticoid resistance. Ann Intern Med. 1993;119:1113-1124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 139] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 22. | Marques AH, Silverman MN, Sternberg EM. Glucocorticoid dysregulations and their clinical correlates. From receptors to therapeutics. Ann N Y Acad Sci. 2009;1179:1-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 116] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 23. | Bamberger CM, Schulte HM, Chrousos GP. Molecular determinants of glucocorticoid receptor function and tissue sensitivity to glucocorticoids. Endocr Rev. 1996;17:245-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 612] [Cited by in RCA: 577] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 24. | Colli LM, do Amaral FC, Torres N, de Castro M. Interindividual glucocorticoid sensitivity in young healthy subjects: the role of glucocorticoid receptor alpha and beta isoforms ratio. Horm Metab Res. 2007;39:425-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Koulouras VP, Li R, Chen L, Hedenstierna GG. Effects of inhaled carbon monoxide and glucocorticoids in porcine endotoxin sepsis. Int J Clin Exp Med. 2011;4:53-66. [PubMed] |
| 26. | Li F, Xu RB. Changes in canine leukocyte glucocorticoid receptors during endotoxin shock. Circ Shock. 1988;26:99-105. [PubMed] |
| 27. | Reichardt HM, Umland T, Bauer A, Kretz O, Schütz G. Mice with an increased glucocorticoid receptor gene dosage show enhanced resistance to stress and endotoxic shock. Mol Cell Biol. 2000;20:9009-9017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 157] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 28. | Stith RD, McCallum RE. Down regulation of hepatic glucocorticoid receptors after endotoxin treatment. Infect Immun. 1983;40:613-621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 29. | Da J, Chen L, Hedenstierna G. Nitric oxide up-regulates the glucocorticoid receptor and blunts the inflammatory reaction in porcine endotoxin sepsis. Crit Care Med. 2007;35:26-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 72] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 30. | Abraham MN, Jimenez DM, Fernandes TD, Deutschman CS. Cecal Ligation and Puncture Alters Glucocorticoid Receptor Expression. Crit Care Med. 2018;46:e797-e804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 31. | Bergquist M, Nurkkala M, Rylander C, Kristiansson E, Hedenstierna G, Lindholm C. Expression of the glucocorticoid receptor is decreased in experimental Staphylococcus aureus sepsis. J Infect. 2013;67:574-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 32. | Goodwin JE, Feng Y, Velazquez H, Sessa WC. Endothelial glucocorticoid receptor is required for protection against sepsis. Proc Natl Acad Sci USA. 2013;110:306-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 119] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 33. | Kamiyama K, Matsuda N, Yamamoto S, Takano K, Takano Y, Yamazaki H, Kageyama S, Yokoo H, Nagata T, Hatakeyama N, Tsukada K, Hattori Y. Modulation of glucocorticoid receptor expression, inflammation, and cell apoptosis in septic guinea pig lungs using methylprednisolone. Am J Physiol Lung Cell Mol Physiol. 2008;295:L998-L1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 34. | Ledderose C, Möhnle P, Limbeck E, Schütz S, Weis F, Rink J, Briegel J, Kreth S. Corticosteroid resistance in sepsis is influenced by microRNA-124--induced downregulation of glucocorticoid receptor-α. Crit Care Med. 2012;40:2745-2753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 108] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 35. | Guerrero J, Gatica HA, Rodríguez M, Estay R, Goecke IA. Septic serum induces glucocorticoid resistance and modifies the expression of glucocorticoid isoforms receptors: a prospective cohort study and in vitro experimental assay. Crit Care. 2013;17:R107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 36. | Molijn GJ, Koper JW, van Uffelen CJ, de Jong FH, Brinkmann AO, Bruining HA, Lamberts SW. Temperature-induced down-regulation of the glucocorticoid receptor in peripheral blood mononuclear leucocyte in patients with sepsis or septic shock. Clin Endocrinol (Oxf). 1995;43:197-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 63] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 37. | Dekelbab BH, Witchel SF, DeFranco DB. TNF-alpha and glucocorticoid receptor interaction in L6 muscle cells: a cooperative downregulation of myosin heavy chain. Steroids. 2007;72:705-712. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 38. | Bergquist M, Lindholm C, Strinnholm M, Hedenstierna G, Rylander C. Impairment of neutrophilic glucocorticoid receptor function in patients treated with steroids for septic shock. Intensive Care Med Exp. 2015;3:59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 39. | Sigal GA, Maria DA, Katayama ML, Wajchenberg BL, Brentani MM. Glucocorticoid receptors in mononuclear cells of patients with sepsis. Scand J Infect Dis. 1993;25:245-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 40. | Vardas K, Ilia S, Sertedaki A, Charmandari E, Briassouli E, Goukos D, Apostolou K, Psarra K, Botoula E, Tsagarakis S, Magira E, Routsi C, Stratakis CA, Nanas S, Briassoulis G. Increased glucocorticoid receptor expression in sepsis is related to heat shock proteins, cytokines, and cortisol and is associated with increased mortality. Intensive Care Med Exp. 2017;5:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 41. | Siebig S, Meinel A, Rogler G, Klebl E, Wrede CE, Gelbmann C, Froh S, Rockmann F, Bruennler T, Schoelmerich J, Langgartner J. Decreased cytosolic glucocorticoid receptor levels in critically ill patients. Anaesth Intensive Care. 2010;38:133-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 42. | Vassiliou AG, Floros G, Jahaj E, Stamogiannos G, Gennimata S, Vassiliadi DA, Tsagarakis S, Tzanela M, Ilias I, Orfanos SE, Kotanidou A, Dimopoulou I. Decreased glucocorticoid receptor expression during critical illness. Eur J Clin Invest. 2019;49:e13073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 43. | Vassiliou AG, Stamogiannos G, Jahaj E, Botoula E, Floros G, Vassiliadi DA, Ilias I, Tsagarakis S, Tzanela M, Orfanos SE, Kotanidou A, Dimopoulou I. Longitudinal evaluation of glucocorticoid receptor alpha/beta expression and signalling, adrenocortical function and cytokines in critically ill steroid-free patients. Mol Cell Endocrinol. 2020;501:110656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 44. | RECOVERY Collaborative Group. Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, Staplin N, Brightling C, Ustianowski A, Elmahi E, Prudon B, Green C, Felton T, Chadwick D, Rege K, Fegan C, Chappell LC, Faust SN, Jaki T, Jeffery K, Montgomery A, Rowan K, Juszczak E, Baillie JK, Haynes R, Landray MJ. Dexamethasone in Hospitalized Patients with Covid-19. N Engl J Med. 2021;384:693-704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6762] [Cited by in RCA: 7590] [Article Influence: 1518.0] [Reference Citation Analysis (7)] |
| 45. | Mao Y, Xu B, Guan W, Xu D, Li F, Ren R, Zhu X, Gao Y, Jiang L. The Adrenal Cortex, an Underestimated Site of SARS-CoV-2 Infection. Front Endocrinol (Lausanne). 2020;11:593179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 62] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 46. | Patak P, Willenberg HS, Bornstein SR. Vitamin C is an important cofactor for both adrenal cortex and adrenal medulla. Endocr Res. 2004;30:871-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 66] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 47. | Meduri GU. New rationale for glucocorticoid treatment in septic shock. J Chemother. 1999;11:541-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 48. | Funder JW. Glucocorticoid and mineralocorticoid receptors: biology and clinical relevance. Annu Rev Med. 1997;48:231-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 227] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 49. | Gomez-Sanchez E, Gomez-Sanchez CE. The multifaceted mineralocorticoid receptor. Compr Physiol. 2014;4:965-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 224] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 50. | Funder JW. Aldosterone and Mineralocorticoid Receptors-Physiology and Pathophysiology. Int J Mol Sci. 2017;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 109] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 51. | du Cheyron D, Bouchet B, Cauquelin B, Guillotin D, Ramakers M, Daubin C, Ballet JJ, Charbonneau P. Hyperreninemic hypoaldosteronism syndrome, plasma concentrations of interleukin-6 and outcome in critically ill patients with liver cirrhosis. Intensive Care Med. 2008;34:116-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 52. | du Cheyron D, Lesage A, Daubin C, Ramakers M, Charbonneau P. Hyperreninemic hypoaldosteronism: a possible etiological factor of septic shock-induced acute renal failure. Intensive Care Med. 2003;29:1703-1709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 58] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 53. | Muto S, Fujisawa G, Natsume T, Asano Y, Yaginuma T, Hosoda S, Saito T. Hyponatremia and hyperreninemic hypoaldosteronism in a critically ill patient: combination of insensitivity to angiotensin II and tubular unresponsiveness to mineralocorticoid. Clin Nephrol. 1990;34:208-213. [PubMed] |
| 54. | Khanna A, Ostermann M, Bellomo R. Angiotensin II for the Treatment of Vasodilatory Shock. N Engl J Med. 2017;377:2604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 55. | Nethathe GD, Cohen J, Lipman J, Anderson R, Feldman C. Mineralocorticoid Dysfunction during Critical Illness: A Review of the Evidence. Anesthesiology. 2020;133:439-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (8)] |
| 56. | Cole TJ, Young MJ. 30 YEARS OF THE MINERALOCORTICOID RECEPTOR: Mineralocorticoid receptor null mice: informing cell-type-specific roles. J Endocrinol. 2017;234:T83-T92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 57. | Rossignol P, Ménard J, Fay R, Gustafsson F, Pitt B, Zannad F. Eplerenone survival benefits in heart failure patients post-myocardial infarction are independent from its diuretic and potassium-sparing effects. Insights from an EPHESUS (Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study) substudy. J Am Coll Cardiol. 2011;58:1958-1966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 105] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 58. | Gilbert KC, Brown NJ. Aldosterone and inflammation. Curr Opin Endocrinol Diabetes Obes. 2010;17:199-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 123] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 59. | Herrada AA, Campino C, Amador CA, Michea LF, Fardella CE, Kalergis AM. Aldosterone as a modulator of immunity: implications in the organ damage. J Hypertens. 2011;29:1684-1692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 60. | Muñoz-Durango N, Barake MF, Letelier NA, Campino C, Fardella CE, Kalergis AM. Immune system alterations by aldosterone during hypertension: from clinical observations to genomic and non-genomic mechanisms leading to vascular damage. Curr Mol Med. 2013;13:1035-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 61. | Grafte-Faure S, Leveque C, Vasse M, Soria C, Norris V, Vannier JP. Effects of glucocorticoids and mineralocorticoids on proliferation and maturation of human peripheral blood stem cells. Am J Hematol. 1999;62:65-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 62. | Bene NC, Alcaide P, Wortis HH, Jaffe IZ. Mineralocorticoid receptors in immune cells: emerging role in cardiovascular disease. Steroids. 2014;91:38-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 86] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 63. | van der Heijden CDCC, Deinum J, Joosten LAB, Netea MG, Riksen NP. The mineralocorticoid receptor as a modulator of innate immunity and atherosclerosis. Cardiovasc Res. 2018;114:944-953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 56] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 64. | Miura R, Nakamura K, Miura D, Miura A, Hisamatsu K, Kajiya M, Hashimoto K, Nagase S, Morita H, Fukushima Kusano K, Emori T, Ishihara K, Ohe T. Aldosterone synthesis and cytokine production in human peripheral blood mononuclear cells. J Pharmacol Sci. 2006;102:288-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 65. | Miura R, Nakamura K, Miura D, Miura A, Hisamatsu K, Kajiya M, Nagase S, Morita H, Fukushima Kusano K, Ohe T, Ishihara K. Anti-inflammatory effect of spironolactone on human peripheral blood mononuclear cells. J Pharmacol Sci. 2006;101:256-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 66. | Ronchetti S, Ricci E, Migliorati G, Gentili M, Riccardi C. How Glucocorticoids Affect the Neutrophil Life. Int J Mol Sci. 2018;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 164] [Article Influence: 20.5] [Reference Citation Analysis (2)] |
| 67. | McDonald B. Neutrophils in critical illness. Cell Tissue Res. 2018;371:607-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 68. | Chapman KE, Coutinho AE, Zhang Z, Kipari T, Savill JS, Seckl JR. Changing glucocorticoid action: 11β-hydroxysteroid dehydrogenase type 1 in acute and chronic inflammation. J Steroid Biochem Mol Biol. 2013;137:82-92. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 91] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 69. | Zhang Z, Coutinho AE, Man TY, Kipari TMJ, Hadoke PWF, Salter DM, Seckl JR, Chapman KE. Macrophage 11β-HSD-1 deficiency promotes inflammatory angiogenesis. J Endocrinol. 2017;234:291-299. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 70. | Gilmour JS, Coutinho AE, Cailhier JF, Man TY, Clay M, Thomas G, Harris HJ, Mullins JJ, Seckl JR, Savill JS, Chapman KE. Local amplification of glucocorticoids by 11 beta-hydroxysteroid dehydrogenase type 1 promotes macrophage phagocytosis of apoptotic leukocytes. J Immunol. 2006;176:7605-7611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 111] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 71. | Agnew EJ, Ivy JR, Stock SJ, Chapman KE. Glucocorticoids, antenatal corticosteroid therapy and fetal heart maturation. J Mol Endocrinol. 2018;61:R61-R73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 72. | Sai S, Nakagawa Y, Yamaguchi R, Suzuki M, Sakaguchi K, Okada S, Seckl JR, Ohzeki T, Chapman KE. Expression of 11beta-hydroxysteroid dehydrogenase 2 contributes to glucocorticoid resistance in lymphoblastic leukemia cells. Leuk Res. 2011;35:1644-1648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 73. | Cohen J, Smith ML, Deans RV, Pretorius CJ, Ungerer JP, Tan T, Jones M, Venkatesh B. Serial changes in plasma total cortisol, plasma free cortisol, and tissue cortisol activity in patients with septic shock: an observational study. Shock. 2012;37:28-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 74. | Venkatesh B, Cohen J, Hickman I, Nisbet J, Thomas P, Ward G, Hall J, Prins J. Evidence of altered cortisol metabolism in critically ill patients: a prospective study. Intensive Care Med. 2007;33:1746-1753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 75. | Cohen J, Pretorius CJ, Ungerer JP, Cardinal J, Blumenthal A, Presneill J, Gatica-Andrades M, Jarrett P, Lassig-Smith M, Stuart J, Dunlop R, Starr T, Venkatesh B. Glucocorticoid Sensitivity Is Highly Variable in Critically Ill Patients With Septic Shock and Is Associated With Disease Severity. Crit Care Med. 2016;44:1034-1041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Critical care medicine
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lal A S-Editor: Liu M L-Editor: Filipodia P-Editor: Wang LL