Published online May 21, 2019. doi: 10.5412/wjsp.v9.i1.1
Peer-review started: February 26, 2019
First decision: March 25, 2019
Revised: April 1, 2019
Accepted: April 26, 2019
Article in press: April 28, 2019
Published online: May 21, 2019
Processing time: 88 Days and 13.7 Hours
Despite the technological breakthroughs and discover of abdominal meshes, ventral hernia has always been challenging in therapeutic strategies by the surgeons, with high recurrence rates. The use of botulinum toxin A (BTA) for the management of ventral and incisional hernia (IH) poses an increasingly interesting practice, especially for the intimidating complex one. The preoperative administration of the toxin to the lateral abdominal muscles by use of Ultra-Sound guidance causes muscle paralysis and a reduction of intra-abdominal pressure. Thus, the hernia defect can be primarily closed without tension, if the length of the defect is up to 10 cm. In larger hernia, this method can be combined with component separation techniques or the use of a mesh. The mesh placement seems to be better by laparoscopy. The site of injection and the dosage of BTA are still under discussion amongst authors. The optimal administration is proposed by some authors to be at least 2 weeks before repair. There is also an analgesic effect of BTA to the patients that underwent hernia reconstruction. Ultimately, the role of BTA in the reconstruction of ventral hernia seems to be promising, but there is a necessity for several randomized clinical trials.
Core tip: Administration of botulinum toxin A (BTA) in the surgical repair of ventral, incisional and complex hernia is a useful method, even for large hernia defects. The toxin is intramuscularly injected under Ultra-Sound guidance, covering all layers of the lateral abdominal muscles. The neurotoxic and analgesic activity of BTA leads to tension-free hernia closure. There is an increasing use of the technique especially in laparoscopic mesh repair. However, future data analysis will demonstrate the results and the benefits of this interesting procedure.
- Citation: Farazi-Chongouki C, Filippou D. Role of botulinum toxin a in the management of complex incisional hernias. World J Surg Proced 2019; 9(1): 1-6
- URL: https://www.wjgnet.com/2219-2832/full/v9/i1/1.htm
- DOI: https://dx.doi.org/10.5412/wjsp.v9.i1.1
In the last years, there is an increasing interest concerning the possible advantages that may present in the use of botulinum toxin A (BTA) for the management of ventral hernias and especially the complex ones. BTA is usually known as Botox, although this is a brand name for the BTA produced by Allergan, and contains 100 IU of BTA. Many companies produce and distribute BTA for medical use. The most common brand names of the world market are Botox, Dysport, Neurobloc, Bocouture, Vistabel etc[1,2].
Although BTA has been used for many decades for the treatment of spastic related neurological disorders, it became popular and well known after being adopted from plastic surgeons and introduced in the “medical aesthetics industry”. Nowadays many different uses of BTA have been proposed and there is an increasing interest for this “poison”. The main indications that have been recently established include the treatment of pain syndromes, chronic low back pain, stump pain (phantom pain), arthritis, migraine, periorbital pain and persistent localized muscular pain syndromes, palmar and axillary hyperhidrosis, detrusor hyperreflexia, gastrointestinal smooth muscle and sphincter spasms[3,4].
Even though in many of these indications the results are promising, there is an ongoing active research particularly to identify and clear the exact mechanisms of BTA use. The effect of BTA has many different mechanisms and the classic knowledge of acting via its paralytic properties represents one of them. Arezzo[5] in 2002 collected and proposed various possible mechanisms including direct effects on muscle nociceptors, motor neuron and muscle spindle afferent changes, alteration of neurogenic inflammation and direct effects on pain afferents.
All these seem to be very interesting but the questions that arise is how all these are related to complex ventral hernia treatment and how they might affect or alter our existing knowledge and practice. The aim of the present editorial is to introduce to the readers this new alternative approach and define the possible physiologic and pathophysiologic mechanisms, the indications and contra-indications of the method and to present the existing techniques.
The hernias that are usually more interesting, complex and difficult to manage are the incisional hernias (IH) after laparotomy. They mostly develop, because the abdominal incision and the myofascial tissues fail to heal. Several factors have been proposed to associate with increased or decreased risk for IH incidence and several techniques have been developed to minimize the risk for postoperative hernia occurrence. However, despite the technical modifications, the high-tech instrument and meshes, the clinical studies that identified the risk factors and the best surgical techniques, the risk for IH is still high. Incidence is growing rapidly due to rising laparotomy rates in increasingly older, obese and co-morbid patients. Only in United States, 200000 IH are operated each year. It has also been estimated that 10% of all abdominal operations will be complicated with IH[6].
The treatment of IH is also followed by an increased incidence for recurrence. The recurrence rate in mesh techniques is estimated 2%-36%, while in cases with simple suturing techniques the risk is much higher and ranges from 12%-54%. Although the recurrence rates may have been slightly decreased with laparoscopic techniques, there is a slight difference and the risk still high. The main reason is, that even on laparoscopic hernia treatment, there is a need of closing the defect if that is feasible. Restoration of the continuity and anatomy of the abdominal wall is important to minimize the complications and recurrence rates. Thus, all the recently developed laparoscopic techniques and modifications focus on abdominal component separation (ACST). Among the main factor that associated with IH recurrence is the extreme tension in closing the abdominal wall. The use of Mesh in IH repair is based on free-tension techniques which hopefully will decrease the recurrence rate. Several studies suggested that even though meshes can be placed by tension free techniques, if the myofascial defect remains open, the recurrence rate is still significant and associated with other factors like infections, hematomas, seromas etc[7]. Bridging has traditionally been used where there has been loss of domain of the abdominal wall or where a compartment syndrome is likely. All the above-mentioned observations suggest that mesh placement by laparoscopy is better, and even better if it can be combined with ACST to close the myofascial defect, restoring the anatomical continuity of the abdominal wall. Different methods have been described to achieve primary myofascial defect closure in patients with complex IH with domain loss and to reduce the morbidity of abdominal wall reconstruction by reducing the risk of compartment syndrome. The most popular techniques include release of fascia[8].
Some other authors suggest the progressive preoperative pneumoperitoneum but the available studies suggest increased complication rate. Tissue expanders have also been used to decrease the defect and the available results are also promising although its use presents several significant difficulties[9,10].
As mentioned above, BTA is a protein with known neurotoxic activity produced by Clostridium botulinum. The existing data suggest that BTA binds to specific glycoproteins found in the cholinergic nerve terminal, blocking the signal transmission temporarily in both motor and autonomic neurons. The paralyzing effect starts 3-4 d after the injections, reaches a maximum after 2 wk and declines gradually after 3-4 mo. Although the toxin is dangerous, application of small well calculated doses in specific points avoiding vital muscles and organs are safe[11].
The use of BTA in animal models showed that preoperative paralysis of the lateral abdominal muscles after intramuscular administration reduces the intra-abdominal pressure, allowing the closure of a hernia defect under minimized muscular tension[12].
These initial results suggested that a pharmaceutical achieved temporary preoperative paralysis of the abdominal wall muscles (with BTA) may facilitate the primary hernia defect closure without component separation (CST) need. Up to now only a few studies has been published. Searching the Medline by using the relative terms as “BTA and hernia”, “botox and hernia” etc. less than 200 published records can be found. From these the relative studies are less than 10 which suggests that research is starting now. Many things had to declare including the optimal dose, the optimal technique of injections, the exact indications that ensure the best effect, the possible adverse effects and complications etc.
First of all, we have to develop the criteria for patient selections. Who are the patients that are most likely to benefit from BTA administration? The size and the location of the hernia defect may be an important factor to patient selection. There is no evidence about that but we can presume the following anatomical facts. The mean length of the frontal abdominal musculature forms the linea alba to middle auxiliary line is about 15-18 cm. The mean myofascial length gained by BTA administration according to several studies is estimated to 3-4 cm at least from each side treated, that mean almost 6-8 cm in total. These observations suggest that myofascial defects 6-10 cm are likely to present the best results, as the initial results suggest that we can achieve the primary defect closure without CST or tension. These data are based on our primary observations and the results are only theoretical. More clinical randomized trials are required to extract reliable results[13].
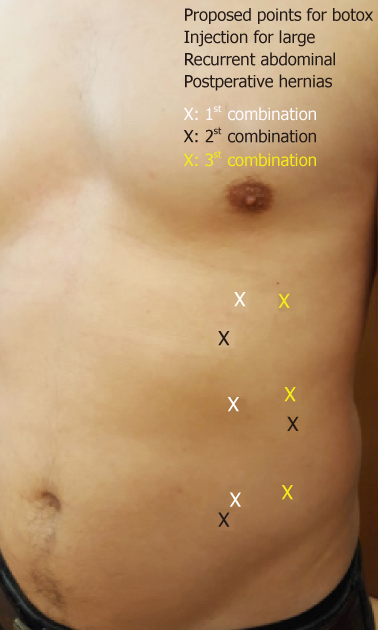
The site of BTA injection is crucial and need to be defined accurately. Four patterns of BTA injection have been proposed, by Elstner, Ibarra-Hurtado, Zielinski and Zandejas. All of them suggest that BTA injection should be performed between the middle clavicle line and the middle auxiliary line in straight line or triangles ranging from superior iliac fossa to below the lower cartilages. These techniques achieve increased length and decreased thickness of the lateral abdominal muscles, allowing the approximation of myofascial tissue and the primary closure of the hernia defect, while they result in a more anatomical appearance and better aesthetic results[14-16].
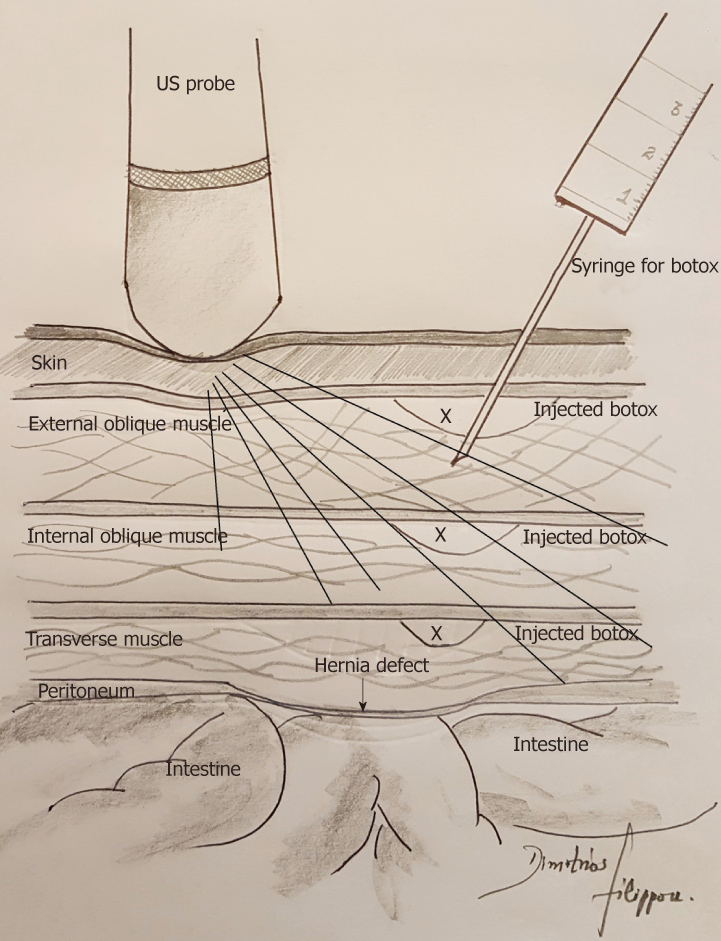
The dose of BTA is still something that should be defined in future controlled studies. The existing studies present significant differences concerning the dilution, the dose, the number of the treatments required and the time that BTA should be injected. Although several authors suggest that large doses of BTA (e.g., up to 400 IU of Botox) may be safe, we suggest that a more conservative protocol should be applied. We propose that 2 wk prior to the operation an injection of 100 IU Botox or 500IU Dysport should be applied in 3 points to each side (IU equally divided). The injection should be performed under Ultra-Sound guidance to avoid complications and to ensure that all the related muscles were treated[14].
Another very interesting parameter that has been studied by Zendejas et al[17] is the analgesic effect of BTA. Patients who treated preoperatively with BTA under Ultra-Sound guidance required significantly less analgesics postoperatively (Figure 1). The BTA injected into the transversus abdominis and internal and external oblique muscles at three sites bilaterally and the U Ultra-Sound guidance required to ensure the accuracy of the injection and to avoid complications (Figure 2).
Soltanizadeh et al[18] evaluated the literature by searching in PubMed and Embase electronic databases in 2016, regarding BTA as an adjunct to abdominal wall reconstruction for IH. This evaluation included six cohort studies with a total of 133 patients, and no randomized or case-control studies were found. Their eligibility criteria were population, intervention, comparison and outcomes. As for the latter, the primary outcome was the rate of primary fascial closure and the secondary outcomes were safety and long-term results. They suggest that preoperative administration of BTA increases muscle length and the optimal administration is at least 2 wk before repair.
BTA effect lasts for 3-4 mo facilitating the healing process postoperatively. The decreased tension of the abdominal muscles decreases significantly the risk for myofascial tissues tear, or mesh transposition secondary to increased muscle forces.
In conclusion we can assume that the possible advantages of the BTA in the treatment of complex IH have raised the interest of the researchers. The paralyzing effect of BTA in the muscles may facilitate the primary closure without tension of large hernia defects, may decrease the need for opioid analgesics postoperatively and may also facilitate the postoperative healing process by eliminating the muscle forces. All these possible advantages are supported by the existing data, but it is for sure that large randomized prospective clinical trials are required to certify the current initial results.
| 1. | Cheng CM, Chen JS, Patel RP. Unlabeled uses of botulinum toxins: a review, part 1. Am J Health Syst Pharm. 2006;63:145-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 43] [Article Influence: 2.2] [Reference Citation Analysis (1)] |
| 2. | Cheng CM, Chen JS, Patel RP. Unlabeled uses of botulinum toxins: a review, part 2. Am J Health Syst Pharm. 2006;63:225-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Layeeque R, Hochberg J, Siegel E, Kunkel K, Kepple J, Henry-Tillman RS, Dunlap M, Seibert J, Klimberg VS. Botulinum toxin infiltration for pain control after mastectomy and expander reconstruction. Ann Surg. 2004;240:608-13; discussion 613-4. [PubMed] |
| 4. | Smith HS, Audette J, Royal MA. Botulinum toxin in pain management of soft tissue syndromes. Clin J Pain. 2002;18:S147-S154. [PubMed] |
| 5. | Arezzo JC. Possible mechanisms for the effects of botulinum toxin on pain. Clin J Pain. 2002;18:S125-S132. [PubMed] |
| 6. | Mudge M, Hughes LE. Incisional hernia: a 10 year prospective study of incidence and attitudes. Br J Surg. 1985;72:70-71. [PubMed] |
| 7. | Brown RH, Subramanian A, Hwang CS, Chang S, Awad SS. Comparison of infectious complications with synthetic mesh in ventral hernia repair. Am J Surg. 2013;205:182-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Ramirez OM, Ruas E, Dellon AL. "Components separation" method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg. 1990;86:519-526. [PubMed] |
| 9. | Terrosu G, Cracco S, Intini S, Biasio F, Brizzolari Parodi PC. Multimodality approach to a big defect of the abdominal wall. Chirurgia. 2012;407–412. |
| 10. | Mcadory RS, Cobb WS, Carbonell AM. Progressive preoperative pneumoperitoneum for hernias with loss of domain. Am Surg. 2009;75:504-508; discussion 508-509. [PubMed] |
| 11. | Dressler D. Clinical applications of botulinum toxin. Curr Opin Microbiol. 2012;15:325-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 126] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 12. | Cakmak M, Caglayan F, Somuncu S, Leventoglu A, Ulusoy S, Akman H, Kaya M. Effect of paralysis of the abdominal wall muscles by botulinum A toxin to intraabdominal pressure: an experimental study. J Pediatr Surg. 2006;41:821-825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 46] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Lien SC, Hu Y, Wollstein A, Franz MG, Patel SP, Kuzon WM, Urbanchek MG. Contraction of abdominal wall muscles influences size and occurrence of incisional hernia. Surgery. 2015;158:278-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (1)] |
| 14. | Weissler JM, Lanni MA, Tecce MG, Carney MJ, Shubinets V, Fischer JP. Chemical component separation: a systematic review and meta-analysis of botulinum toxin for management of ventral hernia. J Plast Surg Hand Surg. 2017;51:366-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (1)] |
| 15. | Elstner KE, Read JW, Rodriguez-Acevedo O, Ho-Shon K, Magnussen J, Ibrahim N. Preoperative progressive pneumoperitoneum complementing chemical component relaxation in complex ventral hernia repair. Surg Endosc. 2017;31:1914-1922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 16. | Smoot D, Zielinski M, Jenkins D, Schiller H. Botox A injection for pain after laparoscopic ventral hernia: a case report. Pain Med. 2011;12:1121-1123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (1)] |
| 17. | Zendejas B, Khasawneh MA, Srvantstyan B, Jenkins DH, Schiller HJ, Zielinski MD. Outcomes of chemical component paralysis using botulinum toxin for incisional hernia repairs. World J Surg. 2013;37:2830-2837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 69] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 18. | Soltanizadeh S, Helgstrand F, Jorgensen LN. Botulinum Toxin A as an Adjunct to Abdominal Wall Reconstruction for Incisional Hernia. Plast Reconstr Surg Glob Open. 2017;5:e1358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Invited Manuscript
Specialty type: Surgery
Country of origin: Greece
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fekaj E, Rolle U S-Editor: Cui LJ L-Editor: A E-Editor: Xing YX