Published online Jan 16, 2026. doi: 10.5412/wjsp.v16.i1.115792
Revised: November 23, 2025
Accepted: December 12, 2025
Published online: January 16, 2026
Processing time: 78 Days and 5.5 Hours
Aortic stenosis (AS) often coexists with carotid artery stenosis. However, clear guidelines for the optimal treatment strategy and sequencing of interventions in patients with both conditions are lacking.
A 79-year-old man with a history of hypertension presented with right-sided pa
Treatment strategy should be individualized, balancing perioperative risks and benefits in patients with severe AS and carotid artery stenosis.
Core Tip: Aortic stenosis (AS) often coexists with carotid artery stenosis. The treatment strategy for patients with coexisting severe AS and carotid artery stenosis should be individualized, weighing the perioperative risks and benefits of each planned intervention.
- Citation: Okada Y, Oishi R, Kimura S, Egi M. Anesthetic and procedural strategy for coexisting severe aortic stenosis and carotid artery stenosis: A case report. World J Surg Proced 2026; 16(1): 115792
- URL: https://www.wjgnet.com/2219-2832/full/v16/i1/115792.htm
- DOI: https://dx.doi.org/10.5412/wjsp.v16.i1.115792
Aortic stenosis (AS) is the most common valvular disease in adults[1,2]. Transcatheter aortic valve implantation (TAVI) has recently emerged as a less invasive alternative to surgical aortic valve replacement (SAVR). As candidacy for intervention expands to a broader population of patients with AS[3], the presence of comorbidities plays a critical role in decision-making and perioperative management.
Carotid atherosclerosis and stenosis frequently coexist with severe AS[4]. Given that stroke is a major complication of both SAVR and TAVI, prior intervention for carotid stenosis may be beneficial. However, carotid revascularization can lead to life-threatening hemodynamic collapse in patients with AS. Although various professional societies have published guidelines for managing AS[5,6] and carotid stenosis[7] independently, no consensus exists regarding the optimal treatment strategy or sequencing of interventions for patients with both conditions.
This report presents the preoperative assessment, multidisciplinary decision-making process, and anesthetic management of a patient with concurrent severe AS and carotid artery stenosis.
A 79-year-old male with a body mass index of 26 kg/m2 presented with paralysis of the right upper and lower limbs.
Numbness in the right upper and lower limbs appeared two weeks prior, and 12 days after the initial symptom onset, the numbness in the right upper limb worsened, accompanied by dysarthria and speech disturbance. He had no history of chest pain or syncope and was classified as New York Heart Association class I for heart failure.
The patient had a history of hypertension, treated with amlodipine.
There was no personal or family history suggestive of anesthesia-related complications.
On presentation, his blood pressure was 128/64 mmHg, heart rate 68 bpm, and peripheral oxygen saturation 95% on room air. Although the patient was alert, he exhibited non-fluent speech and numbness in the affected limbs.
Blood test results, including complete blood count, serum biochemistry, and coagulation parameters, were within the normal range. The plasma B-type natriuretic peptide level was 22.6 pg/mL.
Chest radiography revealed cardiomegaly with a cardiothoracic ratio of 63%. Electrocardiography (ECG) showed an incomplete right bundle branch block without evidence of left ventricular hypertrophy.
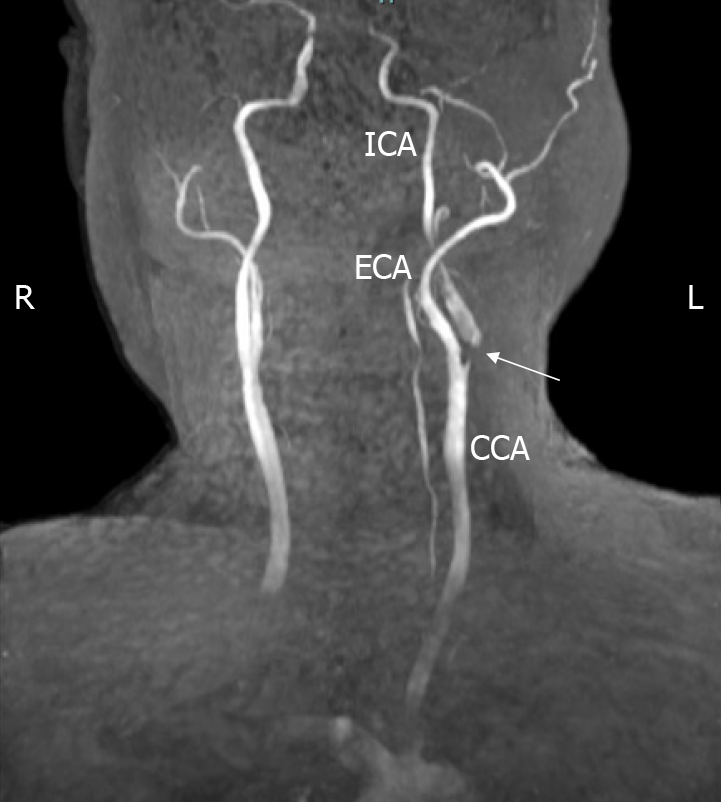
Magnetic resonance imaging revealed multiple infarctions in the left temporal, parietal, occipital, and frontal lobes, along with severe stenosis extending from the left common carotid artery (CCA) to the bifurcation of the internal carotid artery (ICA) (Figure 1). Carotid ultrasonography confirmed significant stenosis extending from the bifurcation of the left CCA to the proximal ICA, with a peak systolic flow velocity of 3.8 m/s. The degree of stenosis in the left CCA was estimated at 70% using the North American Symptomatic Carotid Endarterectomy Trial method and 90% by the area method.
Carotid endarterectomy (CEA) or carotid artery stenting (CAS) was considered for the patient. However, preoperative transthoracic echocardiography revealed severe AS, with an aortic valve cross-sectional area of 0.8 cm2, peak transvalvular velocity of 4.2 m/s, and peak/mean pressure gradients of 72/45 mmHg. The left ventricular ejection fraction (EF) was preserved at 81%, with no evidence of hypertrophy. Computed tomography showed minimal aortic arch calcification. Risk stratification for cardiac surgery yielded a Society of Thoracic Surgeons morbidity/mortality risk score of 30.1% and a EuroSCORE II of 3.59%.
A multidisciplinary conference was convened to determine the optimal treatment sequence, and the perspectives of each specialty were explicitly discussed. From the neurosurgical standpoint, prioritizing hemodynamic stability was essential. The team emphasized that CEA carries a substantial risk of perioperative circulatory collapse due to intraoperative carotid sinus stimulation, postoperative blood pressure reduction aimed at preventing hyperperfusion syndrome, and the presence of concomitant coronary artery disease. Given that the carotid stenosis was non-urgent, the neurosurgical team advocated performing TAVI first to minimize these risks. The cardiology team acknowledged that the patient did not meet the absolute indications for TAVI; however, they agreed that TAVI could be justified, if needed, to reduce the perioperative hemodynamic burden imposed by CEA. From an anesthesiological perspective, the team concurred with the neurosurgical assessment regarding the high risk of circulatory instability during CEA and emphasized the importance of minimizing the risk of perioperative stroke during TAVI, by selecting an anesthetic strategy capable of responding flexibly to potential hemodynamic or neurological changes. Based on these multidisciplinary considerations, the team agreed to proceed with transfemoral TAVI under general anesthesia (GA) as the initial intervention and defer CEA to a later date.
The final diagnosis was concomitant asymptomatic severe AS, scattered cerebral infarctions in the left hemisphere, and left ICA stenosis.
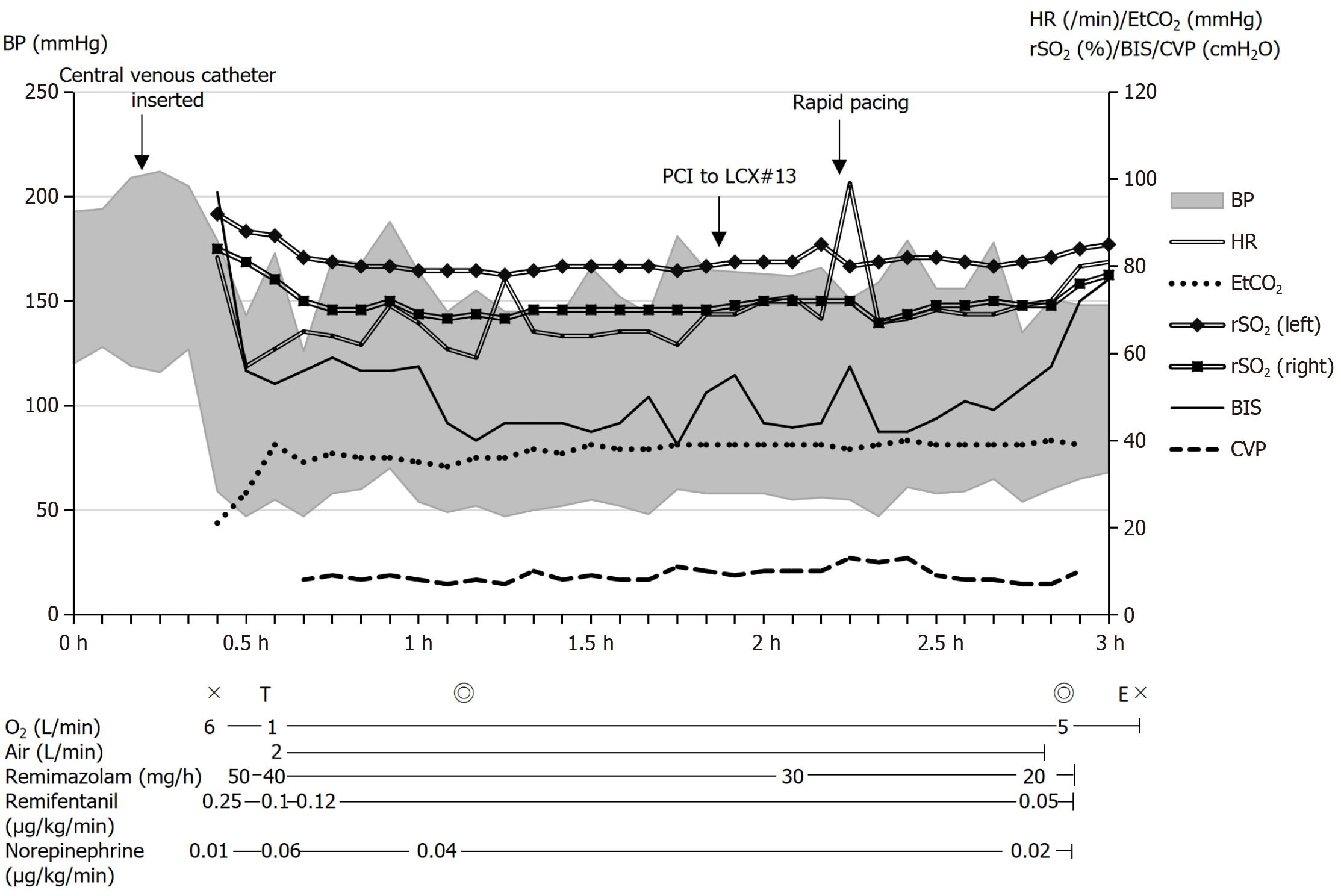
Upon arrival in the operating room, arterial and central venous lines were secured. GA was induced with remimazolam (5 mg), remifentanil (0.25 μg/kg/minute), and rocuronium (50 mg), followed by an endotracheal intubation. Processed regional cerebral oxygen saturation (rSO2) and electroencephalography (EEG) were continuously monitored using INVOS® (Medtronic, Dublin, Ireland) and BIS® (Medtronic, Dublin, Ireland), respectively, in addition to standard monitoring modalities, including 5-lead ECG, pulse oximetry, capnography, and neuromuscular blockade monitoring. A transesophageal echocardiography probe was inserted to assess the cardiac function and detect potential intraoperative complications. Anesthesia was maintained with continuous infusions of remimazolam and remifentanil, titrated to achieve a target bispectral index value of 40-60, and appropriate EEG patterns. Norepinephrine (0.02-0.06 µg/kg/minute) was administered to maintain hemodynamic stability (Figure 2).
A balloon-expandable valve (SAPIEN 3 Ultra®, Edwards Lifesciences, Irvine, United States) was selected over a self-expanding device to minimize cerebral hypoperfusion by shortening the duration of rapid pacing during deployment. The valve was successfully deployed under rapid pacing at 180 bpm. No significant changes in rSO2 or EEG were observed during the deployment. The procedure lasted for 105 minutes, with minimal blood loss. The patient received 1150 mL of Ringer’s solution, and the total urine output was 740 mL. Following smooth emergence from anesthesia without any neurological abnormalities, the patient was extubated in the operating room and transferred to the high-care unit as planned.
No TAVI-related complications or exacerbations of pre-existing neurological symptoms were observed. CEA was subsequently performed under GA without any incident 4 months later, and the patient was discharged on postoperative day 9. At both 6-month and 1-year follow-up, no new neurological abnormalities were found.
Current guidelines recommend SAVR or TAVI in both symptomatic and asymptomatic patients, depending on the severity of AS, life expectancy, and surgical risk[5,6]. Considering the presence of asymptomatic severe AS with preserved left ventricular EF, and advanced age, TAVI was considered a reasonable treatment option in this case. Extracranial carotid artery stenosis is a significant cause of stroke and mortality[8]. In patients with a recent transient ischemic attack or non-disabling ischemic stroke and ipsilateral moderate-to-severe stenosis, CEA is recommended to reduce the risk of recurrent stroke[7]. Our patient presented with moderate-to-severe left CCA stenosis and had recently experienced a stroke, warranting carotid intervention.
Although established guidelines exist for the independent management of AS[5,6] and carotid stenosis[7], evidence-based recommendations for patients with coexisting AS and carotid artery stenosis remain limited. AS has been associated with a high incidence of cardiovascular complications in patients undergoing non-cardiac surgery[9-11]. Although large-scale data on perioperative outcomes of CEA in patients with severe AS are lacking, hemodynamic depression, characterized by hypotension and bradycardia due to autonomic stimulation of the carotid sinus, is a well-documented complication of carotid surgery[12]. Hyperperfusion syndrome is another serious complication of CEA, necessitating strict blood pressure control[13]. In patients with severe AS, perioperative hypotension, whether un
Stroke is a potential complication of aortic valve replacement, resulting from catheter manipulation of a heavily calcified aortic valve or embolization of atheromatous plaques[15,16]. Additionally, rapid pacing and perioperative hypotension during valve deployment may result in cerebral hypoperfusion[17]. However, the association between carotid artery stenosis and stroke in patients undergoing TAVI remains controversial[4,18-20], and recent reports have suggested that unilateral carotid artery stenosis does not increase the risk of periprocedural stroke[21,22].
Several case reports have proposed different strategies for patients requiring both TAVI and carotid revascularization. Moraca et al[16] reported 16 patients who underwent concomitant interventions with CEA, followed by TAVI on the same day. Ravindra et al[23] described five patients who successfully underwent CAS before TAVI (median interval: 30 days), one of whom experienced worsening heart failure during stenting. In contrast, Gennari et al[24] and Rossi et al[25] presented cases treated with TAVI first, followed by transcarotid artery revascularization shortly thereafter. Shintoku et al[26] reported a case managed with a staged approach involving angioplasty, followed by TAVI 2 weeks later, and CAS 1 week after that[26]. No perioperative cerebrovascular events or fatal circulatory collapse were observed in these studies[16,23-26].
In our case, although the patient had a recent stroke and moderate-to-severe CCA stenosis, his neurological condition remained stable under medical management, allowing the CEA to be deferred for several months. Conversely, severe AS presented a significant obstacle to maintaining strict blood pressure control during CEA and increased the risk of circulatory collapse. After weighting the potential risks of performing CEA in the setting of concomitant AS and coronary disease, the multidisciplinary conference determined to perform TAVI prior to carotid revascularization.
Anesthetic management also required careful consideration. TAVI can be performed under either GA with en
We encountered a patient requiring intervention for both severe AS and carotid stenosis, where treating one condition in the presence of the other poses potential complications. Given the lack of clear recommendations or clinical guidelines for managing these coexisting conditions, individualized, multidisciplinary treatment planning is essential.
| 1. | Iung B, Baron G, Butchart EG, Delahaye F, Gohlke-Bärwolf C, Levang OW, Tornos P, Vanoverschelde JL, Vermeer F, Boersma E, Ravaud P, Vahanian A. A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J. 2003;24:1231-1243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2255] [Cited by in RCA: 2301] [Article Influence: 100.0] [Reference Citation Analysis (0)] |
| 2. | Danielsen R, Aspelund T, Harris TB, Gudnason V. The prevalence of aortic stenosis in the elderly in Iceland and predictions for the coming decades: the AGES-Reykjavík study. Int J Cardiol. 2014;176:916-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 124] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 3. | Thourani VH, Gunter RL, Neravetla S, Block P, Guyton RA, Kilgo P, Lerakis S, Devireddy C, Leshnower B, Mavromatis K, Stewart J, Simone A, Keegan P, Nguyen TC, Merlino J, Babaliaros V. Use of transaortic, transapical, and transcarotid transcatheter aortic valve replacement in inoperable patients. Ann Thorac Surg. 2013;96:1349-1357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 4. | Steinvil A, Leshem-Rubinow E, Abramowitz Y, Shacham Y, Arbel Y, Banai S, Bornstein NM, Finkelstein A, Halkin A. Prevalence and predictors of carotid artery stenosis in patients with severe aortic stenosis undergoing transcatheter aortic valve implantation. Catheter Cardiovasc Interv. 2014;84:1007-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, Jneid H, Krieger EV, Mack M, McLeod C, O'Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A, Toly C. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;143:e35-e71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 303] [Cited by in RCA: 697] [Article Influence: 139.4] [Reference Citation Analysis (0)] |
| 6. | Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, Capodanno D, Conradi L, De Bonis M, De Paulis R, Delgado V, Freemantle N, Gilard M, Haugaa KH, Jeppsson A, Jüni P, Pierard L, Prendergast BD, Sádaba JR, Tribouilloy C, Wojakowski W; ESC/EACTS Scientific Document Group. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2022;43:561-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 501] [Cited by in RCA: 3852] [Article Influence: 770.4] [Reference Citation Analysis (0)] |
| 7. | Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, Kamel H, Kernan WN, Kittner SJ, Leira EC, Lennon O, Meschia JF, Nguyen TN, Pollak PM, Santangeli P, Sharrief AZ, Smith SC Jr, Turan TN, Williams LS. 2021 Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline From the American Heart Association/American Stroke Association. Stroke. 2021;52:e364-e467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 519] [Cited by in RCA: 1969] [Article Influence: 393.8] [Reference Citation Analysis (0)] |
| 8. | Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O'Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation. 2018;137:e67-e492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4163] [Cited by in RCA: 4940] [Article Influence: 617.5] [Reference Citation Analysis (1)] |
| 9. | Kwok CS, Bagur R, Rashid M, Lavi R, Cibelli M, de Belder MA, Moat N, Hildick-Smith D, Ludman P, Mamas MA. Aortic stenosis and non-cardiac surgery: A systematic review and meta-analysis. Int J Cardiol. 2017;240:145-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Tashiro T, Pislaru SV, Blustin JM, Nkomo VT, Abel MD, Scott CG, Pellikka PA. Perioperative risk of major non-cardiac surgery in patients with severe aortic stenosis: a reappraisal in contemporary practice. Eur Heart J. 2014;35:2372-2381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 99] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 11. | Zahid M, Sonel AF, Saba S, Good CB. Perioperative risk of noncardiac surgery associated with aortic stenosis. Am J Cardiol. 2005;96:436-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 45] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Bogniotti LAC, Teivelis MP, Cardozo FAM, Caramelli B, Wolosker N, Puech-Leão P, De Luccia N, Calderaro D. Hemodynamic depression after carotid surgery: Incidence, risk factors and outcomes. Clinics (Sao Paulo). 2022;77:100090. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 13. | Moulakakis KG, Mylonas SN, Sfyroeras GS, Andrikopoulos V. Hyperperfusion syndrome after carotid revascularization. J Vasc Surg. 2009;49:1060-1068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 173] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 14. | Agarwal S, Rajamanickam A, Bajaj NS, Griffin BP, Catacutan T, Svensson LG, Anabtawi AG, Tuzcu EM, Kapadia SR. Impact of aortic stenosis on postoperative outcomes after noncardiac surgeries. Circ Cardiovasc Qual Outcomes. 2013;6:193-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 101] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 15. | Eggebrecht H, Schmermund A, Voigtländer T, Kahlert P, Erbel R, Mehta RH. Risk of stroke after transcatheter aortic valve implantation (TAVI): a meta-analysis of 10,037 published patients. EuroIntervention. 2012;8:129-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 319] [Cited by in RCA: 290] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 16. | Moraca RJ, Shah AA, Bailey SH, Benckart D, Lasorda D, Khalil R, Chess B, McGregor W, Halbreiner MS. Combined carotid endarterectomy and transcatheter aortic valve replacement: Technique and outcomes. J Card Surg. 2018;33:265-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Kleiman NS, Maini BJ, Reardon MJ, Conte J, Katz S, Rajagopal V, Kauten J, Hartman A, McKay R, Hagberg R, Huang J, Popma J; CoreValve Investigators. Neurological Events Following Transcatheter Aortic Valve Replacement and Their Predictors: A Report From the CoreValve Trials. Circ Cardiovasc Interv. 2016;9:e003551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 78] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 18. | Chakraborty S, Faisaluddin M, Ashish K, Amgai B, Bandyopadhyay D, Patel N, Hajra A, Aggarwal G, Ghosh RK, Kalra A. In-hospital clinical outcomes of transcatheter aortic valve replacement in patients with concomitant carotid artery stenosis: Insights from the national inpatient sample. Int J Cardiol Heart Vasc. 2020;31:100621. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 19. | Kochar A, Li Z, Harrison JK, Hughes GC, Thourani VH, Mack MJ, Matsouaka RA, Cohen DJ, Peterson ED, Jones WS, Vemulapalli S. Stroke and Cardiovascular Outcomes in Patients With Carotid Disease Undergoing Transcatheter Aortic Valve Replacement. Circ Cardiovasc Interv. 2018;11:e006322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 20. | Caetano L da Silva, Gibicoski TB, Rodriguez F, Scabello I, da Silva Neto EP, Iplinski B. Impact of carotid artery stenosis on outcomes of transcatheter aortic valve replacement: A systematic review and meta-analysis. Int J Cardiol. 2024;399:131670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 21. | Lepidi S, Squizzato F, Fovino LN, D'Oria M, Badawy MR, Fraccaro C, Antonello M, Tarantini G. Prevalence and Prognostic Impact of Carotid Artery Disease in Patients Undergoing Transcatheter Aortic Valve Implantation. Ann Vasc Surg. 2022;84:61-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 22. | Oestreicher S, Vella A, Muller O, Kirsch M, Eeckhout E, Fournier S, Monney P, Roux O, Roguelov C, Zhang P, Abraham P, Ferlay C, Antiochos P, Lu H. Neurovascular Outcomes in Relation With Carotid Artery Stenosis in Patients Undergoing Transcatheter Aortic Valve Implantation. J Invasive Cardiol. 2023;35:E136-E142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 23. | Ravindra VM, Mazur MD, Kumpati GS, Park MS, Patel AN, Tandar A, Welt FG, Bull D, Couldwell WT, Taussky P. Carotid Artery Stenosis in the Setting of Transcatheter Aortic Valve Replacement: Clinical and Technical Considerations of Carotid Stenting. World Neurosurg. 2016;86:194-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Gennari M, Trabattoni P, Bartorelli AL, Agrifoglio M. A Short Report on Single Stage Transcatheter Aortic Valve Replacement and Carotid Stenting. Thorac Cardiovasc Surg Rep. 2017;6:e37-e39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Rossi PJ, Wood JC, Jim J. Concomitant transcarotid artery revascularization and transcatheter aortic valve replacement. J Vasc Surg Cases Innov Tech. 2020;6:205-208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 26. | Shintoku R, Hayakawa M, Hoshi T, Okune S, Hiramine T, Takahashi T, Hosoo H, Ito Y, Marushima A, Ishikawa E, Matsumaru Y. Carotid artery stenosis concomitant with severe aortic stenosis treated by combination of staged angioplasty and transcatheter aortic valve implantation: A case report. Surg Neurol Int. 2022;13:469. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/