Published online Feb 2, 2024. doi: 10.5412/wjsp.v14.i1.1
Peer-review started: October 12, 2023
First decision: December 11, 2023
Revised: December 23, 2023
Accepted: January 17, 2024
Article in press: January 17, 2024
Published online: February 2, 2024
Processing time: 112 Days and 21.6 Hours
The majority of published reports on foreign bodies (FBs) involve the rectum and applied a transanal retrieval. Usually, patients with FB above the rectum are subjected to laparotomy for removal. Here, we illustrate the case of a man with an FB that had migrated into the descending colon, and its successful removal via a laparoscopic approach.
A 43-year-old man, who had the habit of FB insertion into his anus to aid defe
A minimally invasive approach should be adopted to aid extraction of colorectal FB as it is effective and safe.
Core Tip: This case highlights the minimally invasive approach to foreign body removal from the rectum/distal colon, as a way forward, to avoid major laparotomy as an operative intervention.
- Citation: Che Ghazali K, Yaacob H, Mohamed Sidek AS. Combined laparoscopic and endoscopic method for foreign body removal from descending colon: A case report. World J Surg Proced 2024; 14(1): 1-7
- URL: https://www.wjgnet.com/2219-2832/full/v14/i1/1.htm
- DOI: https://dx.doi.org/10.5412/wjsp.v14.i1.1
The majority of published literature on foreign bodies (FBs) involves the rectum and transanal retrievals. However, if the FB dislodges above the rectum, the retrieval success rate drops and an operative intervention, most frequently laparotomy, may be required[1].
Herein, we describe the case of a man who presented with an anally-inserted FB that had migrated into the descending colon, and its successful removal via a laparoscopic approach. Minimally invasive approaches offer great advantages over open surgery, in terms of holistic impact on the abdominal cavity, shorter hospital stays, and earlier recovery[2].
A 43-year-old man was referred for FB in the sigmoid colon.
For the past 5 yr, the patient had experienced chronic constipation requiring straining and digitation, and resulted in a once-weekly passing motion. He also had a propensity of inserting unusual FB anally in order to dilate his anus and ease his defecation. He had no history of changed bowel habits or tenesmus, nor a family history of cancer.
Two days before hospitalisation, he had purposefully placed a shampoo bottle inside his anus to aid defecation. Unfortunately, the bottle slipped through deeper and entered the intestinal lumen. He had attempted to remove it but was unsuccessful. He stated that he sought treatment at our facility following the development of abdominal pain and subsequent personal concern about a retained FB.
The patient’s past medical history was irrelevant.
The patient had no significant personal or family history.
The patient’s abdomen was soft on palpation, and there was no peritonism. A vague lump could be felt above the left iliac fossa region. On digital rectal examination, we were unable to feel the FB.
All within normal range.
Plain abdominal radiograph revealed a bottle-shaped FB, positioned in the left iliac fossa region, correlating with the clinical history and examination findings (Figure 1). No free air was noted.
Retained FB in descending colon.
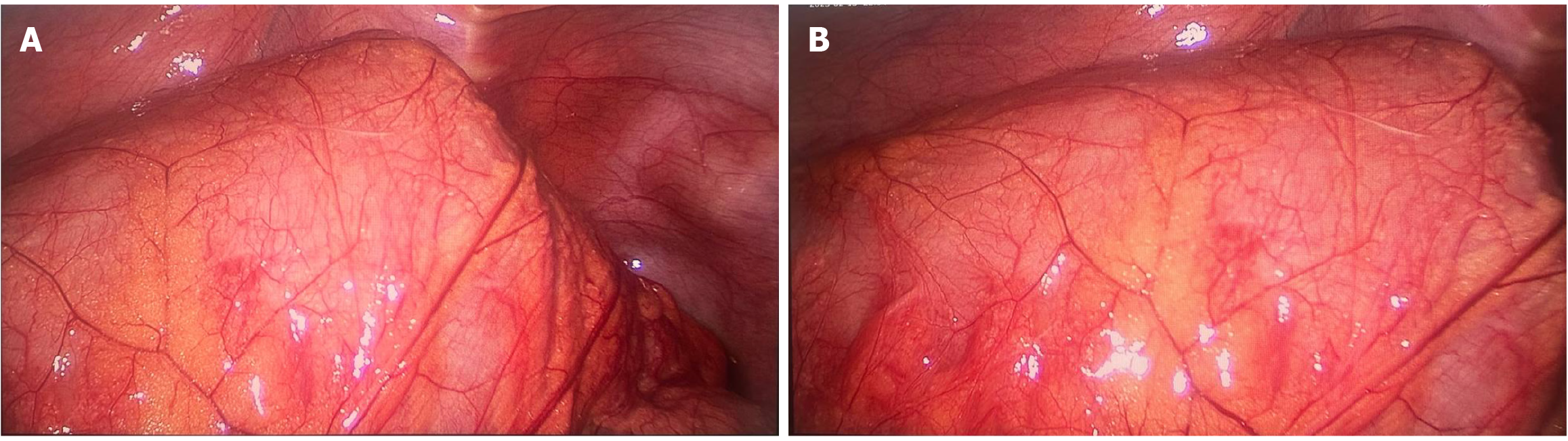
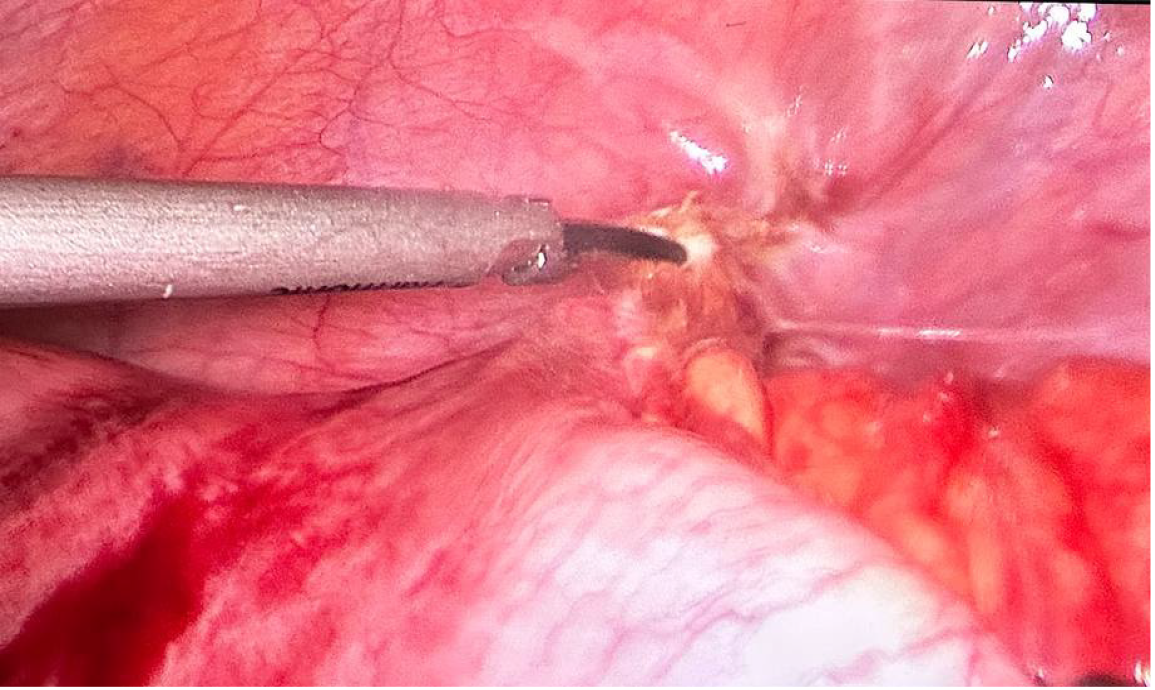
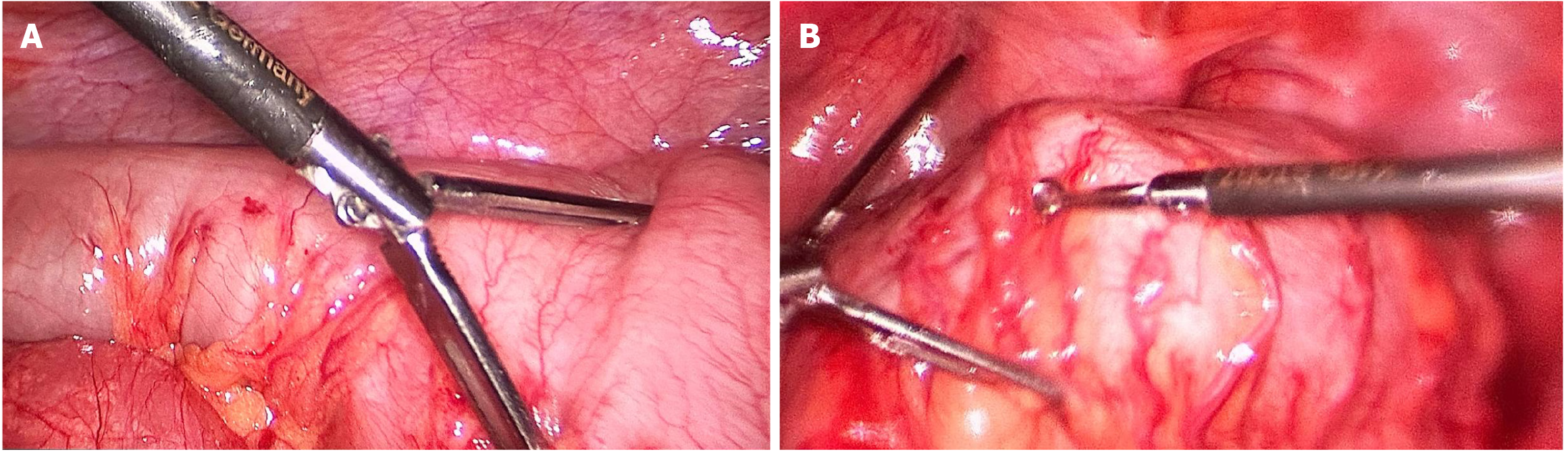
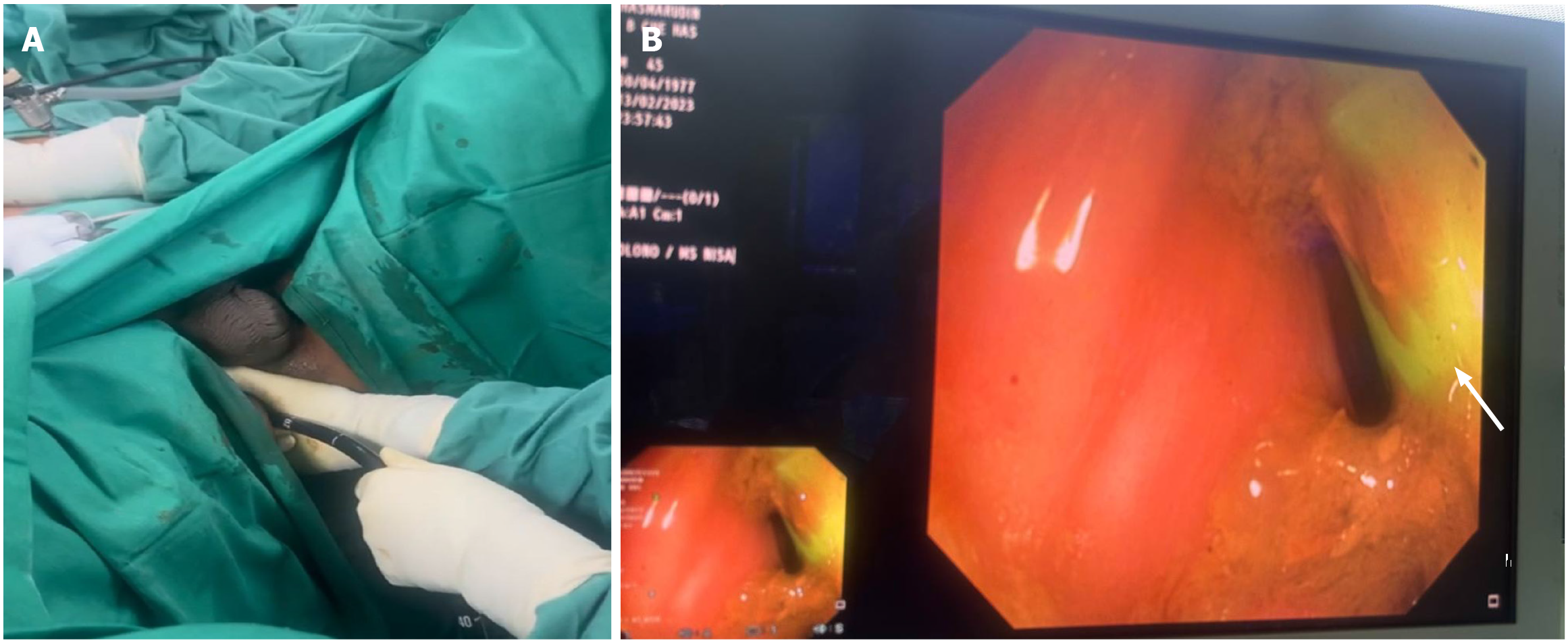
The patient consented to examination under anaesthesia, including laparoscopic assessment. The laparoscopic-assisted procedure itself involved a 12-mm infraumbilical camera port and another two 5-mm working ports placed at the right iliac fossa and left lumbar under direct vision. During the laparoscopy, a bulging FB was noted at the descending colon. The bowel wall appeared normal (Figure 2). There was congenital adhesion at the descending-sigmoid junction and the lateral abdominal wall, causing angulation; hence, adhesiolysis was performed to straighten the axis (Figure 3). We then applied a laparoscopic bowel grasper and Babcock forceps to assist in milking down the FB from the sigmoid colon to the rectum (Figure 4). A surgeon manipulated the bowel with the traction and counter-traction method, until it reached the rectum (Figure 5).
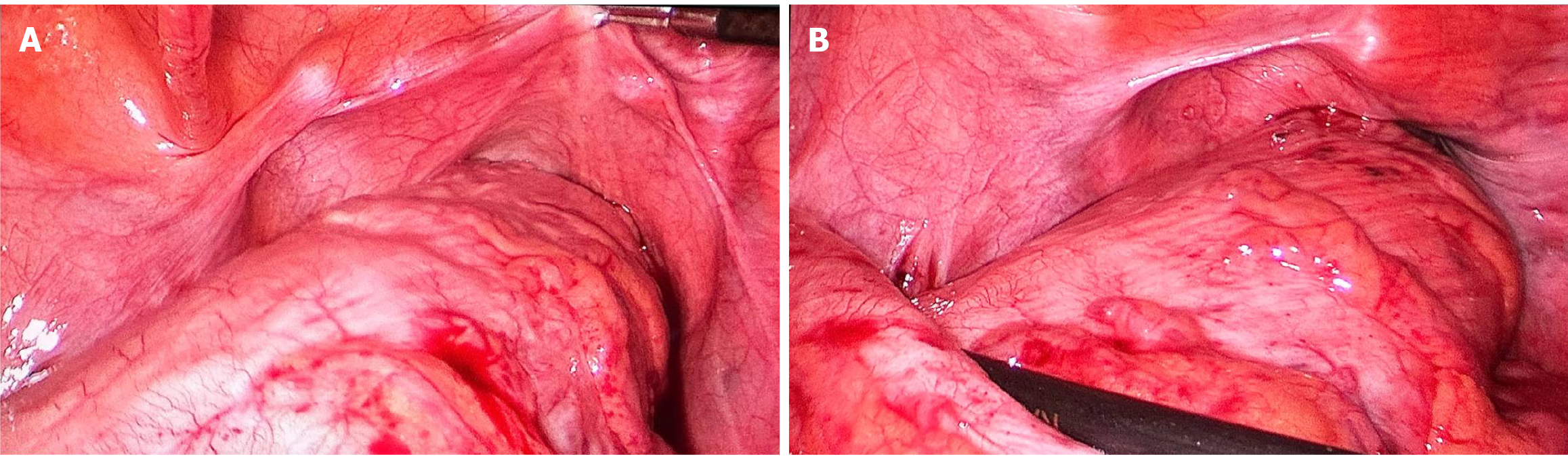
No proper bowel preparation was made. We only performed a gentle on-table rectal wash-out, to clean the rectum. Following that, we performed a sigmoidoscopy, to visualize the colonic mucosa and the FB in the rectum. The rectal mucosa was not inflamed nor oedematous (Figure 6). To facilitate the extraction, the bimanual manipulation technique was applied. Gentle suprapubic pressure was applied by a second surgeon and via a transanal approach to retrieve the bottle. Meanwhile, the first surgeon pushed the FB toward the anus via laparoscopy until it reached the second surgeon’s hand in the anus (Figure 7). Once the bottom of the bottle could be felt, it was grasped by the second surgeon’s fingers and fully pulled out. A 14 cm × 4 cm green-coloured plastic shampoo bottle was removed successfully (Figure 8).
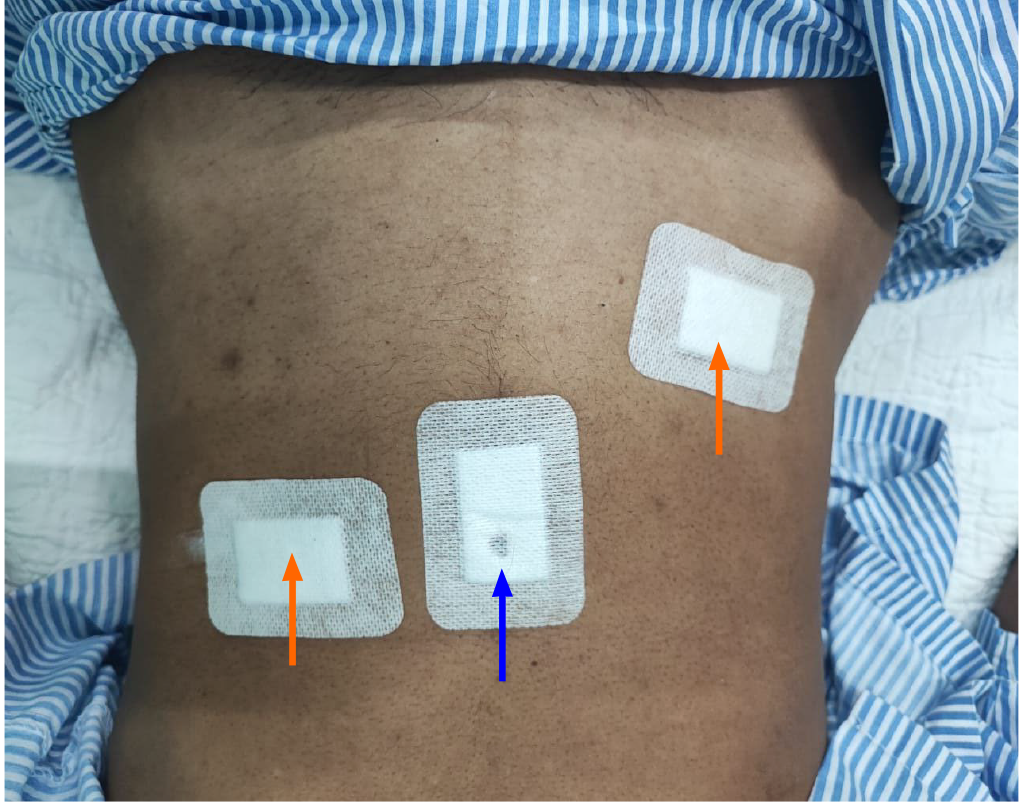
Figure 9 shows the port placement wound postoperatively.
The patient was monitored for 2 d postoperatively and subsequently discharged to home. Prior to discharge, he was referred to the psychiatric unit to elicit any diagnosis on psychiatric illness underlying this abnormal habit. Based on the psychiatric assessment, his behaviour was mainly attributed to his constipation, and a plan was made to follow-up with manometry and biofeedback.
Despite being underreported, colorectal FBs occur frequently[1]. Usually, a patient suffering from colorectal FB will present late after the lodging episode, when they fail attempt(s) to remove it; this is typically due to embarrassment and a perception of taboo[1]. The reasons for colorectal FB insertion are varied and include underlying psychiatric illness, self-administration to alleviate a symptom of anorectal disease, for sexual gratification or autoeroticism, from a criminal assault, for drug trafficking, or as a relatively mundane medical manoeuvre (e.g., thermometer or enema insertion)[3-5]. Objects recorded in case reports are toys, bottles, light bulbs, glasses, fruits, and vegetables[6,7].
Eftaiha et al[5] simplified the classification of retained FB by dividing them into low-lying or high-lying, which then dictates the clinical approach for removal. For low-lying FB, the mass can be palpated in the rectal ampulla; for high-lying FB, the mass is proximal to the rectosigmoid junction. FBs retained in the rectum can usually be managed with a transanal removal at bedside; sometimes, the case may require appropriate anaesthesia[8]. If the FB becomes dislodged cranially, operative intervention is usually required[6,8], and in the presence of peritonism, emergency laparotomy is necessitated[1,3,7]. In the case of a stable patient with no need for urgent surgery, sedation and attempt at bedside extraction should be performed[5,8].
A retrospective study by Coskun et al[6] evaluated 15 patients with FB in rectum who were treated in Izmir, Turkey over a 10-yr period. The rectal FBs were removed transanally under general anaesthesia from 12 of the patients, while the remaining 3 required laparotomy. Kim et al[2] performed a retrospective study of 14 Korean patients with retained FBs, from January 2006 to December 2018. Among these patients, 2 had removal of the FB in the emergency department, 12 underwent general anaesthesia for anal sphincter relaxation, and 5 had FB retrieved transanally. The remaining 7 patients had laparotomy, with 2 needing colonic milking only, 4 requiring colotomy and repair, and 1 necessitating Hartman’s procedure due to faecal peritonitis.
In our patient, who presented with a retained FB after 3 d, the possibility of a successful transanal extraction was minimal. In some circumstances, choosing the best treatment approach can be difficult. Knowing that the FB was a shampoo bottle, and it is quite large, hence endoscopic retrieval alone may not be adequate since we know that endoscopic equipment to retrieve specimen is small for example the Roth Net retrieval device. Hence, the patient was therefore subjected to laparoscopic assessment as well. Many advantages of laparoscopy surgery in the treatment of FB removal. It allows assessment of intraperitoneum, in this case we can assess large bowel condition with just a keyhole wound. In our case, combination approach was suitable because firstly, this is because the FB was trapped higher up, at the descending colon area. Secondly, we speculated the affected bowel was probably inflamed, thickened, and oedema
In most cases, close observation is adequate as postextraction management. However, some authors have suggested sigmoidoscopy assessment to evaluate mucosal laceration, bleeding, or perforation[1,6,7]. Follow-up, in general, is suggested for assessing long-term complications, such as incontinence, stenosis, or fistula[1,3,6].
In conclusion, the colorectal surgeon should be familiar with various extraction methods. A minimally invasive approach should be the way forward, as it has also been shown to be safe in aiding extraction of colorectal FB. Another approach that can be explored is the hand-assisted laparoscopic (otherwise known as HAL) technique.
| 1. | Cologne KG, Ault GT. Rectal foreign bodies: what is the current standard? Clin Colon Rectal Surg. 2012;25:214-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 67] [Article Influence: 5.2] [Reference Citation Analysis (1)] |
| 2. | Kim JH, Um E, Jung SM, Shin YC, Jung SW, Kim JI, Heo TG, Lee MS, Jun H, Choi PW. The Management of Retained Rectal Foreign Body. Ann Coloproctol. 2020;36:335-343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Mani H, Waits R. Retained Colorectal Foreign Body: A Case Report. Int J Clin Med Imaging. 2018;5:07. [DOI] [Full Text] |
| 4. | Koornstra JJ, Weersma RK. Management of rectal foreign bodies: description of a new technique and clinical practice guidelines. World J Gastroenterol. 2008;14:4403-4406. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 52] [Cited by in RCA: 55] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Eftaiha M, Hambrick E, Abcarian H. Principles of Management of Colorectal Foreign Bodies. Arch Surg. 1977;112:691-695. [RCA] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 46] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Coskun A, Erkan N, Yakan S, Yıldirim M, Cengiz F. Management of rectal foreign bodies. World J Emerg Surg. 2013;8:11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 63] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 7. | Lake JP, Essani R, Petrone P, Kaiser AM, Asensio J, Beart RW Jr. Management of retained colorectal foreign bodies: predictors of operative intervention. Dis Colon Rectum. 2004;47:1694-1698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 104] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 8. | Rispoli G, Esposito C, Monachese TD, Armellino M. Removal of a foreign body from the distal colon using a combined laparoscopic and endoanal approach: report of a case. Dis Colon Rectum. 2000;43:1632-1634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Malaysia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Wu W, China S-Editor: Gao CC L-Editor: A P-Editor: Zhao YQ