Published online Sep 28, 2023. doi: 10.5412/wjsp.v13.i2.7
Peer-review started: April 25, 2023
First decision: July 17, 2023
Revised: July 19, 2023
Accepted: August 8, 2023
Article in press: August 8, 2023
Published online: September 28, 2023
Processing time: 154 Days and 20.3 Hours
Simple lateral elbow dislocation (SLED) is a rare type of elbow dislocation; however, its treatment may be complicated by accompanying soft tissue or neurovascular damage. Herein, we report a rare case of SLED managed secon-darily with open reduction and soft tissue repair following failure of closed reduction.
A 67-year-old woman suffered SLED after falling on her outstretched left hand with her elbow extended. She developed pain, swelling, and movement restriction in the elbow; there were no neurovascular symptoms, except for numbness in the 4th and 5th digits. Radiologic investigation confirmed the SLED, and a closed reduction under anesthesia was performed. The follow-up radiographs at 1-wk revealed failure of reduction; accordingly, open reduction with lateral collateral ligament and common extensor origin repair were carried out. The patient regained full elbow range of motion by six weeks.
Adequate concentric reduction for SLED, conservatively or surgically, reduces complications and provides a more functional joint.
Core Tip: Despite their rarity, the results of simple lateral elbow dislocations are gratifying if they are handled well from start to finish. Treatment may be terminated with closed methods or surgery may be required. Regardless of the method of treatment, the results are good with a close follow-up.
- Citation: Albayrak M. Simple lateral elbow dislocation: A case report. World J Surg Proced 2023; 13(2): 7-13
- URL: https://www.wjgnet.com/2219-2832/full/v13/i2/7.htm
- DOI: https://dx.doi.org/10.5412/wjsp.v13.i2.7
Elbow dislocation, the second most common joint dislocation in adults[1], frequently occurs in the posterior or posterolateral direction, whereas simple lateral elbow dislocation (SLED) is a rare entity, with only a handful of reports in the literature[1-3]. Simple dislocation involves pure articular disengagement without accompanying fractures, while dislocation with a concomitant fracture is called complex dislocation[4,5].
SLEDs are usually accompanied by neurovascular involvement[6,7] or soft tissue damage[8], which may hinder closed reduction[9-11] due to interposition of muscles (such as the anconeus and brachialis) or fracture fragments (if any). In this study, we report a rare case of SLED managed by open reduction and repair of the lateral collateral ligament (LCL) and common extensor origin performed one week after a failed closed reduction.
A 67-year-old right-hand dominant woman was admitted to the emergency room with elbow pain and inability to move her elbow on January 4, 2021 with a history of falling on an outstretched left hand with her elbow extended.
She presented with a swollen left elbow and her right hand holding her left wrist with a pronated forearm. She fell down while walking and was admitted to hospital within 20 min.
There is no history since this was an emergent case.
Hypertension was her only chronic illness. There was no family history.
The patient’s body temperature was 36.2 °C, heart rate 96 bpm, respiratory rate 24 breaths/min, blood pressure 140/90 mmHg, height 162.0 cm and weight 96 kg. There was no open wound around the elbow, as seen on the first examination. There were no signs of any distal circulatory disorder or neurological deficits in the left upper extremity, except for numbness in the left 4th and 5th digits.
Complete blood count parameters were in the normal range.
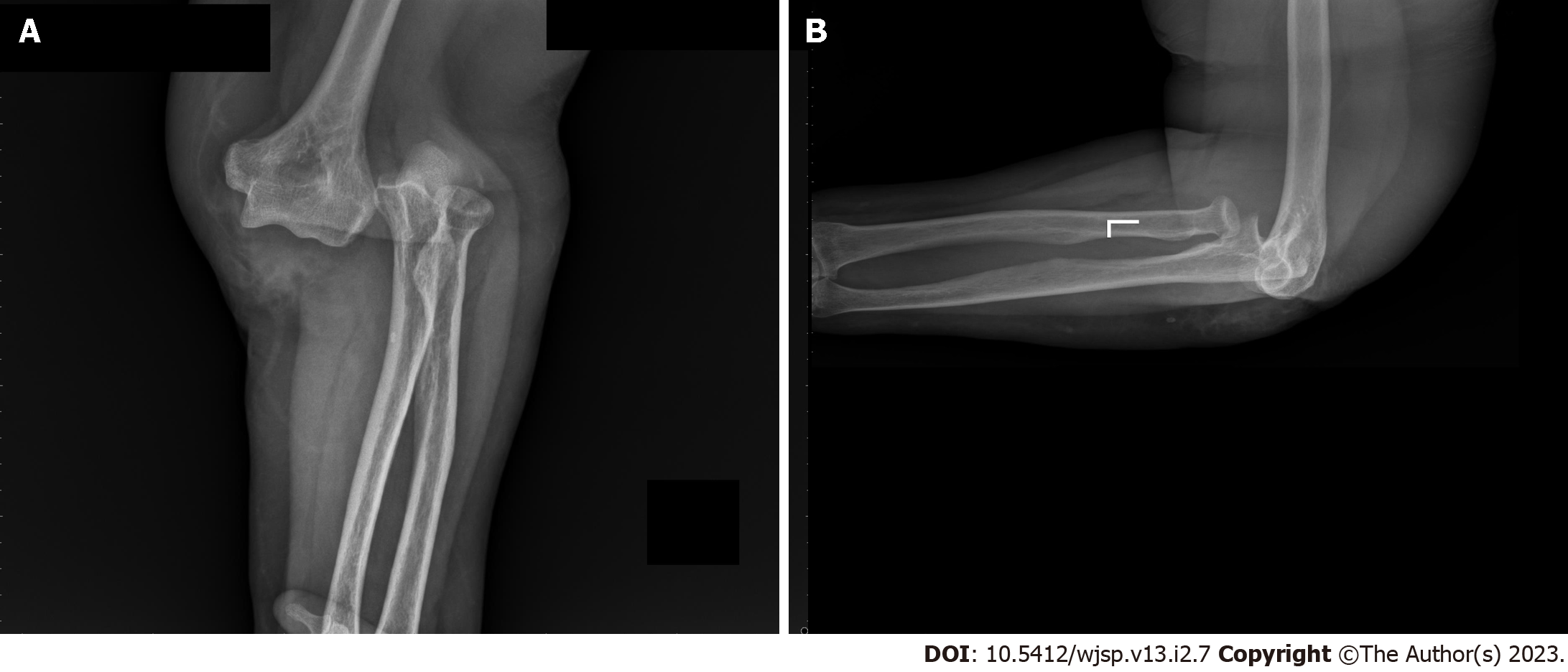
Anteroposterior and lateral radiographs of the elbow revealed lateral displacement of both the ulna and radius relative to the humerus without a fracture (Figure 1).
Left SLED.
Under sedation anesthesia in the operating room, a gentle closed reduction under fluoroscopy was performed. An assistant applied longitudinal traction to the humerus through the axilla, and the surgeon, while holding the forearm in supination, maneuvered it in the medial direction, as the assistant moved the humerus in the lateral direction. An audible click confirmed the correction of the dislocation which was also evident under fluoroscopy. After reduction, both passive flexion and extension range of motion (ROM) of the elbow were regained. The valgus stress test was normal, but the varus stress test performed at 25° elbow flexion was abnormal opening to about 20°. Next, a gravity-assisted varus stress test[12] was applied, which indicated a LCL deficiency. A concentric reduction was confirmed under fluoroscopic examination; afterward, we applied a long arm splint to immobilize the elbow in 90° flexion and neutral rotation, as LCL-deficient elbows are most unstable in supination[13,14]. When the patient woke up from anesthesia, she had no pain in her elbow, and the numbness in the fingers was also relieved. Radiographs taken after manipulation confirmed the concentric reduction (Figure 2).
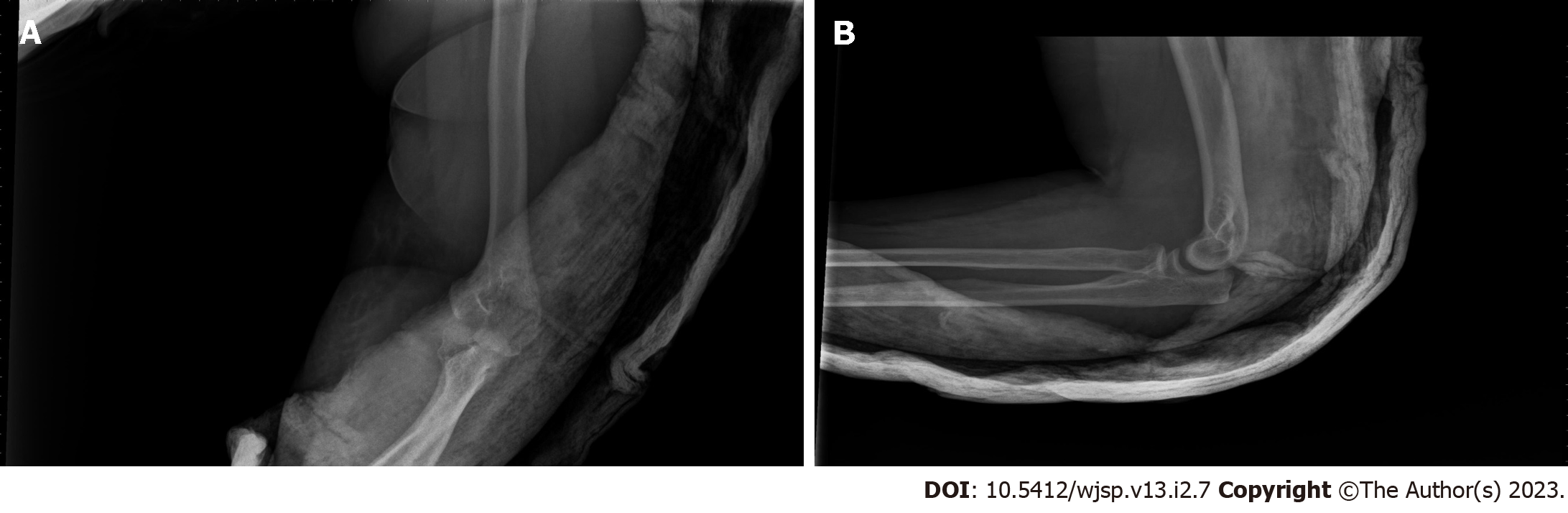
At the one-week follow-up, although the patient remained pain-free, the follow-up radiographs revealed a loss of reduction (Figure 3).
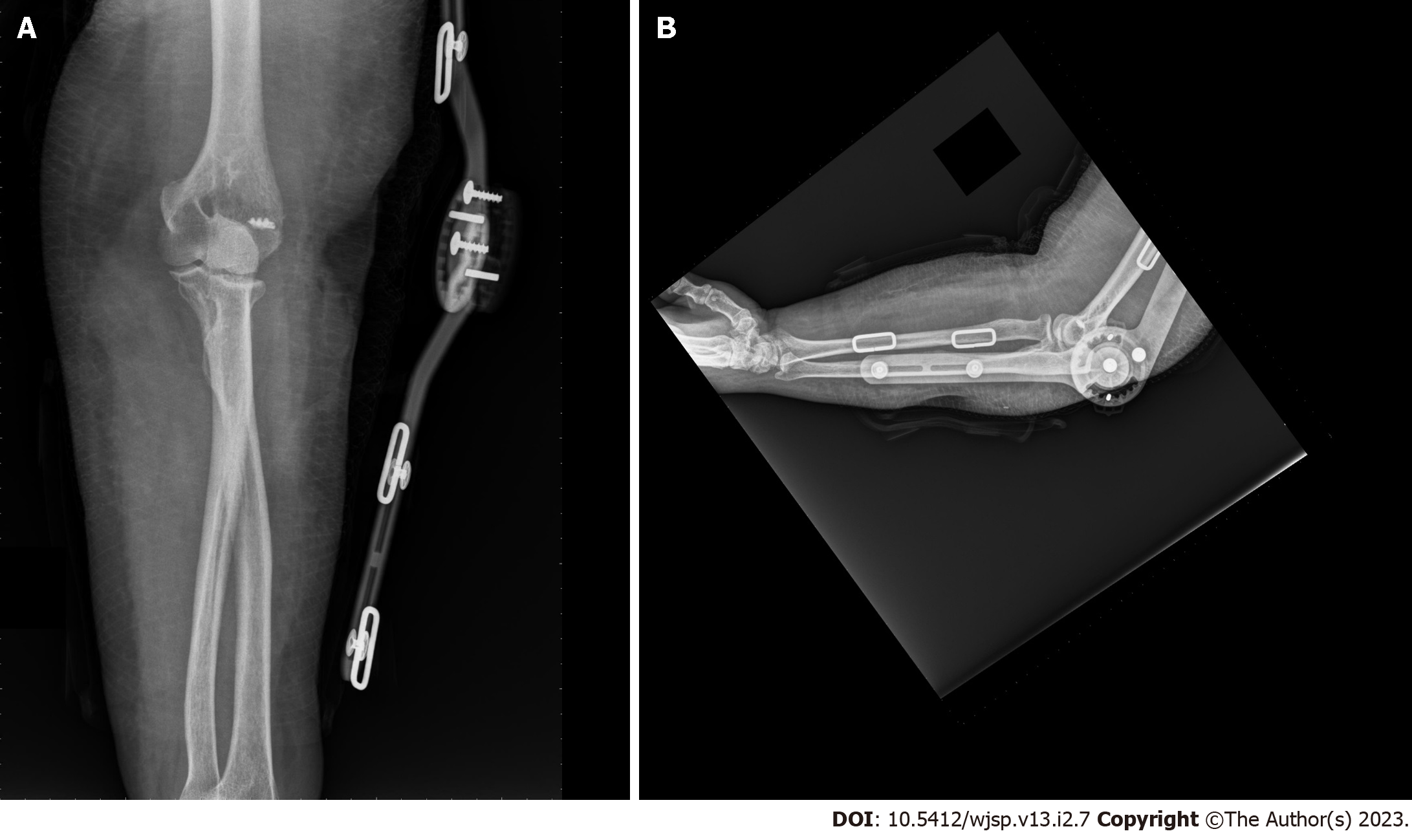
Accordingly, a decision was made for open reduction and LCL repair using the Kocher approach. During surgery, the disrupted LCL and joint capsule were exposed just after dissecting the fascia underlying the subcutaneous tissue. The LCL complex was repaired with a suture anchor (DePuy Mitek; Johnson and Johnson, Raynham, MA, United States), and the torn common extensor origin was sutured using non-absorbable sutures (2-0 Ethibond Excel, Ethicon; Johnson and Johnson, Raynham, MA, United States). Elbow joint stability, both in flexion and extension, was evaluated using fluoroscopy. As full ROM of the elbow was achieved, and there was no subluxation or articular incongruity fluoroscopically, the surgery was terminated. No additional intervention was planned for the medial side, and the elbow was immobilized at 90° flexion and neutral rotation in a splint for 5 d.
A hinged elbow brace was subsequently applied to allow active joint movement (12th day after the injury) (Figure 4).
The ROM was controlled by increasing the flexion and extension angles daily after the fifth day of brace application. Full ROM of the elbow was achieved by the end of three weeks post-injury, and the brace was removed.
The patient was followed up for two years, during which she remained symptom free. Figure 5 shows the radiographs at the two-year follow-up; the joint retained concentric reduction with minimal heterotopic ossification along the radiohumeral joint without compromising the ROM for supination and pronation. The patient reported no problems carrying heavy objects or getting up from a chair by pushing bilaterally.
Elbow dislocations are more commonly seen in men than in women. They are also more common in the adult age group than in the younger age group. Overall prognosis is better in the younger age group (< 35 years old)[4]. Despite elbow dislocation being a common musculoskeletal injury, SLEDs are rare and seldom managed by closed reduction[1]. Predominantly, only case reports are available for this injury. Even in a systematic review of 342 cases of complete elbow dislocations, only three lateral dislocations were reported[1].
Schnetzke et al[15] revealed that in cases of simple elbow dislocations, a diverse range of ligamentous and muscular soft tissue injuries are observed. A subset of patients exhibit prominent injury patterns with a notable emphasis on the medial aspect. These significant findings provide robust evidence for the existence of a valgus mechanism, characterized by the initiation and propagation of a medial force from the medial to anterior regions. Our patient also injured a valgus mechanism.
Ulnar nerve involvement is a common complication with lateral elbow dislocation[10], as reported in our patient; thus, a detailed neurologic examination was necessary at the time of admission. Hopefully, as in our patient, neurological involvement resolves rapidly and spontaneously once nerve compression is relieved by joint reduction. Radiological investigation is necessary, starting with conventional roentgenography, whereas computed tomography is mandatory if there is an accompanying fracture[5]. In our patient, there was no evidence of a fracture, so we did not perform computed tomography.
There are two treatment options for SLEDs-conservative or surgical. The existing case reports for simple lateral dislocations state that conservative treatment comprising closed reduction and functional treatment with a pressure bandage[1] or splinting[2,7,9-11], followed by early movement, is satisfactory. Moreover, certain closed reduction maneuvers have been specifically designed for lateral elbow dislocations[9-11]. Since our patient also had a simple dislocation, we proceeded with a closed reduction first.
However, a number of studies have described the use of open reduction for lateral elbow dislocations[3-6,8]. Muscle or fracture fragment interposition is often cited as the reason for failure of the closed reduction; however, in our patient, there was no muscle or soft tissue interposing the joint space. We were able to approach the bone just under subcutaneous tissue in the open reduction due to a large defect in the LCL and the joint capsule. Therefore, repair of the lateral complex in elbow dislocation is essential[4]. Micic et al[16] and Hobgood et al[17] checked elbow joint stability in extension under fluoroscopy after repairing the LCL complex and the common extensor origin, and reported that if the elbow is stable in extension, there is no need to repair medial structures. Similarly, in our patient, the elbow joint was stable in extension after repairing the LCL and common extensor origin, so we decided not to touch the medial side.
According to the publication by de Klerk et al[18], surgical intervention may offer a more advantageous result in comparison to non-operative treatment. However, it is not possible to definitively conclude this based solely on the findings of the aforementioned study. It is recommended that future investigations prioritize the comparison between these approaches and additionally determine specific subsets of patients with uncomplicated elbow dislocation who would derive benefits from surgical intervention.
The complications of simple elbow dislocations include loss of motion due to contracture, pain, and heterotopic ossification[4], residual instability is also a major concern[4]. In our case, none of the aforementioned complications were observed with closed reduction; however, when the radiographs revealed a loss of joint congruency at the end of the one-week observation period, open reduction was inevitable.
If the elbow remains unstable after reduction, primary ligament repair begets sufficient stability to allow early movement, which prevents contractures formation[4]. We also opted for ligament repair along with open reduction, which allowed early ROM exercises, and the patient was protected from developing contractures.
Regardless of the severity of the trauma, a closed reduction maneuver while monitoring neurovascular status can efficiently manage SLED. However, in the case of failure of closed reduction, open reduction with additional soft tissue repair may be required to ensure the maintenance of joint congruity. Adequate concentric reduction with conservative or surgical methods allows early resumption of ROM, reduces complications, and provides a more functional joint.
| 1. | de Haan J, Schep NW, Tuinebreijer WE, Patka P, den Hartog D. Simple elbow dislocations: a systematic review of the literature. Arch Orthop Trauma Surg. 2010;130:241-249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 2. | Latifi M, Aziz S, Alaoui A, Essadki B, Fikry T. [Lateral dislocation of the elbow: pathophysiological and therapeutic analysis]. Rev Chir Orthop Reparatrice Appar Mot. 2003;89:453-456. [PubMed] |
| 3. | Olasinde AA, Iryivuze O, Sikakluya FK. Open postero-lateral dislocation of the left elbow secondary to assault: A case report. Int J Surg Case Rep. 2022;101:107798. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 4. | Heo YM, Yi JW, Lee JB, Lee DH, Park WK, Kim SJ. Unstable Simple Elbow Dislocation Treated with the Repair of Lateral Collateral Ligament Complex. Clin Orthop Surg. 2015;7:241-247. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Ando A, Hagiwara Y, Koide M, Yamashiro M, Matsuda M, Itoi E. Lateral dislocation of the elbow with concomitant lateral epicondyle fracture: A case report and review of the literature. J Orthop Sci. 2019;24:563-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (1)] |
| 6. | Kim JY, Choi GJ. Lateral Elbow Dislocation of a Patient with Elbow Flexion Contracture and a Traumatic Brain Lesion. J Hand Surg Asian Pac Vol. 2021;26:451-454. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Zaraa M, Saied W, Bouchoucha S, Ben Ghachem M. [Purely lateral elbow dislocation in a child, case report and literature review]. Chir Main. 2012;31:38-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Chhaparwal M, Aroojis A, Divekar M, Kulkarni S, Vaidya SV. Irreducible lateral dislocation of the elbow. J Postgrad Med. 1997;43:19-20. [PubMed] |
| 9. | Watanabe K, Fukuzawa T, Mitsui K. Successful Closed Reduction of a Lateral Elbow Dislocation. Case Rep Orthop. 2016;2016:5934281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Khan SK, Chopra R, Chakravarty D. Successful closed manipulation of a pure lateral traumatic dislocation of the elbow joint using a modified Stimson's technique: a case report. J Med Case Rep. 2008;2:170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Gokcen B, Ozyurek S, Atik A, Sivrioglu AK, Kaya E, Keklikci K. Successful Closed Manipulation of Simple Lateral Dislocation of the Elbow Joint: A Case Report. Oman Med J. 2013;28:e062. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Pollock JW, Brownhill J, Ferreira L, McDonald CP, Johnson J, King G. The effect of anteromedial facet fractures of the coronoid and lateral collateral ligament injury on elbow stability and kinematics. J Bone Joint Surg Am. 2009;91:1448-1458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 131] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 13. | Bryce CD, Armstrong AD. Anatomy and biomechanics of the elbow. Orthop Clin North Am. 2008;39:141-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 108] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 14. | Safran MR, Baillargeon D. Soft-tissue stabilizers of the elbow. J Shoulder Elbow Surg. 2005;14:179S-185S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 96] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 15. | Schnetzke M, Ellwein A, Maier D, Wagner FC, Grützner PA, Guehring T. Injury patterns following simple elbow dislocation: radiological analysis implies existence of a pure valgus dislocation mechanism. Arch Orthop Trauma Surg. 2021;141:1649-1657. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 16. | Micic I, Kim SY, Park IH, Kim PT, Jeon IH. Surgical management of unstable elbow dislocation without intra-articular fracture. Int Orthop. 2009;33:1141-1147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 38] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Hobgood ER, Khan SO, Field LD. Acute dislocations of the adult elbow. Hand Clin. 2008;24:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 38] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | de Klerk HH, Eygendaal D, van den Bekerom MPJ. We still do not know which patients with a(n) (almost) simple elbow dislocation need an operative treatment. Eur J Trauma Emerg Surg. 2021;47:875-876. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dreyfuss D, Israel S-Editor: Fan JR L-Editor: Webster JR P-Editor: Chen YX