Published online Jul 15, 2022. doi: 10.5412/wjsp.v12.i1.1
Peer-review started: January 30, 2022
First decision: March 25, 2022
Revised: May 11, 2022
Accepted: June 16, 2022
Article in press: June 16, 2022
Published online: July 15, 2022
Processing time: 163 Days and 4.1 Hours
Laparoscopic colorectal surgery is still developing in the Anglophone Caribbean, having been first performed in the region in the year 2011. We report the initial outcomes using a robot camera holder to assist in laparoscopic colorectal operations.
To report our initial experience using the FreeHand® robotic camera holder (Freehand 2010 Ltd., Guildford, Surrey, United Kingdom) for laparoscopic colorectal surgery in Trinidad & Tobago.
We retrospectively collected data from all patients who underwent laparoscopic colorectal resections using the Freehand® (Freehand 2010 Ltd., Guildford, Surrey, United Kingdom) robotic camera holder between September 30, 2021 and April 30, 2022. The following data were recorded: patient demographics, robotic arm setup time, operating time, conversions to open surgery, conversions to a human camera operator, number and duration of intra-operative lens cleaning. At the termination of the operation, before operating notes were completed, the surgeons were administered a questionnaire recording information on ergonomics, user-difficulty, requirement to convert to a human camera operator and their ability to carry out effective movements to control the robot while operating.
Nine patients at a mean age of 58.9 ± 7.1 years underwent colorectal operations using the FreeHand robot: Right hemicolectomies (5), left hemicolectomy (1), sigmoid colectomies (2) and anterior resection (1). The mean robot docking time was 6.33 minutes (Median 6; Range 4-10; SD ± 1.8). The mean duration of operation was 122.33 ± 78.5 min and estimated blood loss was 113.33 ± 151.08 mL. There were no conversions to a human camera holder. The laparoscope was detached from the robot for lens cleaning/defogging an average of 2.6 ± 0.88 times per case, with cumulative mean interruption time of 4.2 ± 2.15 minutes per case. The mean duration of hospitalization was 3.2 ± 1.30 days and there were no complications recorded. When the surgeons were interviewed after operation, the surgeons reported that there were good ergonomics (100%), with no limitation on instrument movement (100%), stable image (100%) and better control of surgical field (100%).
Robot-assisted laparoscopic colorectal surgery is feasible and safe in the resource-poor Caribbean setting, once there is appropriate training.
Core Tip: This study demonstrates that robot-assisted laparoscopic colorectal surgery is feasible in the resource poor Caribbean setting, but requires appropriate user training to ensure safe introduction of the technology.
- Citation: Cawich SO, Singh Y, Naraynsingh V, Senasi R, Arulampalam T. Freehand-robot-assisted laparoscopic colorectal surgery: Initial experience in the Trinidad and Tobago. World J Surg Proced 2022; 12(1): 1-7
- URL: https://www.wjgnet.com/2219-2832/full/v12/i1/1.htm
- DOI: https://dx.doi.org/10.5412/wjsp.v12.i1.1
Cooperman et al[1] were first to report laparoscopic colectomy for neoplastic disease in 1991. After this success, multiple reports of laparoscopic colectomies appeared in the surgical literature and the technique became widely accepted as the preferred approach for colorectal resections[2-9]. The benefits of laparoscopic colectomy are supported by level I data from the Barcelona trial[2], Clinical Outcomes of Surgical Therapy trial[3], Colon Cancer Laparoscopic or Open Resection trial[4] and the Conventional vs Laparoscopic assisted Surgery in Patients with Colorectal Cancer (MRC CLASICC) trial[5]. These trials and subsequent metanalyses demonstrated laparoscopic colectomy’s superiority over open colectomy in post-operative pain, return of bowel function and hospitalization[2-9].
In the Anglophone Caribbean, Plummer et al[10] first reported a series of laparoscopic colectomies in the year 2011, approximately 20 years after the first report by Cooperman et al[1]. We report our initial experience using the FreeHand® robotic camera holder (Freehand 2010 Ltd., Guildford, Surrey, United Kingdom) for laparoscopic colorectal surgery in Trinidad & Tobago.
In this study we retrospectively collected data from hospital records of all patients who underwent laparoscopic colorectal resections using the Freehand® (Freehand 2010 Ltd., Guildford, Surrey, United Kingdom) robotic camera holder over a four-month period from September 30, 2021 to April 30, 2022. We excluded patients who were below 18 years of age, who underwent emergency operations, who had colectomies associated with other major procedures performed at the same sitting and those who did not consent to data collection.
For all patients who underwent colectomies, we recorded the following data: patient demographics, robotic arm setup time (time for draping, lens fixation and positioning), operating time, conversions to open surgery, conversions to a human camera operator, number and duration of intra-operative lens cleaning. All data were entered into an excel database and the data were analyzed using Statistical Product and Service Solutions version 20.0.
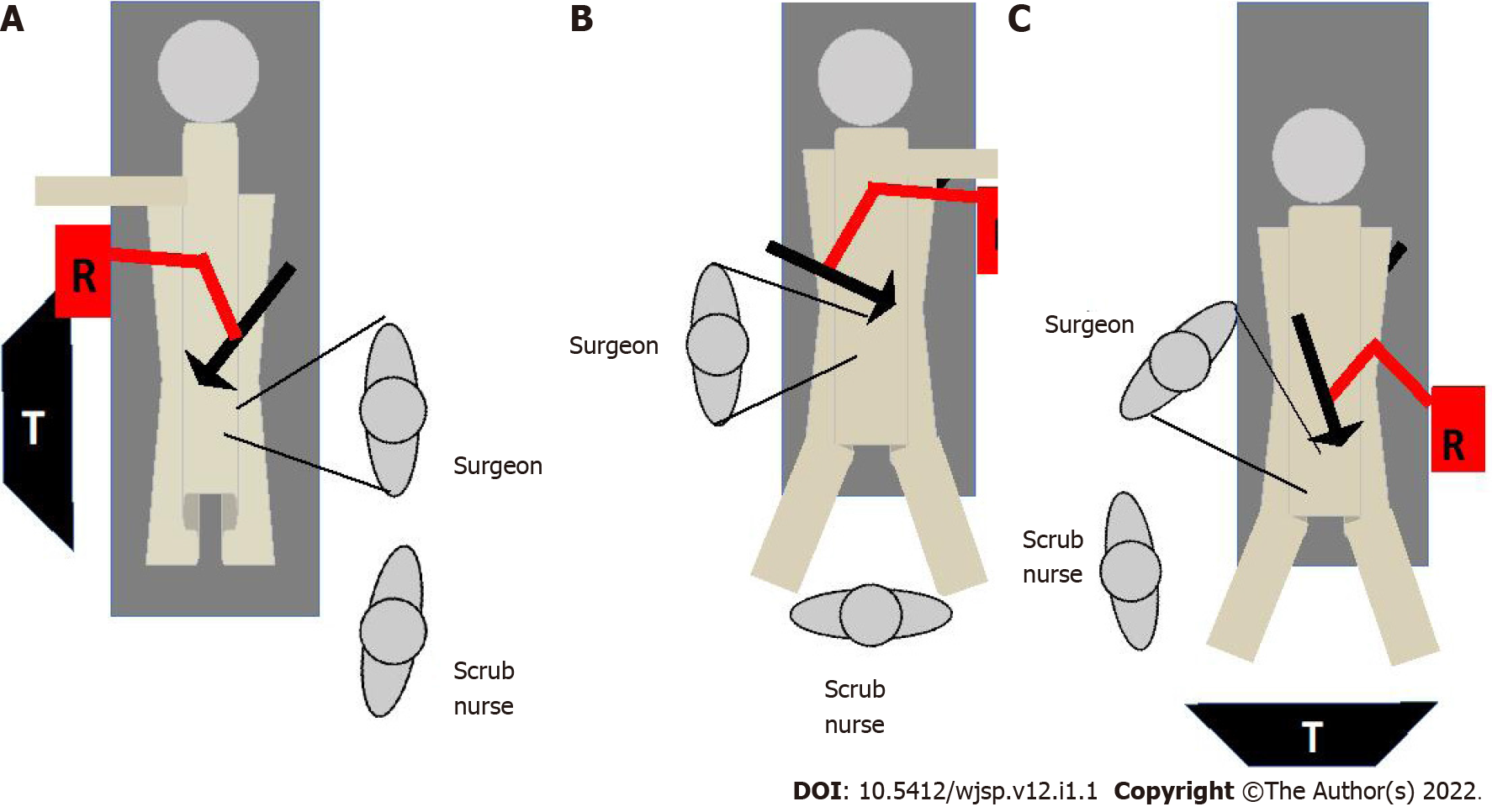
In this series, the decision on operating room setup was taken at the pre-operative time out. In all cases, a 12 mmHg pneumoperitoneum was created using Hasson’s technique via a port placed at the umbilicus. For a right hemicolectomy, the patient was placed supine and the left hand was tucked in. The laparoscopic monitors were placed on the right side of the patient and the Freehand robot was fixated to the right-side bed rail (Figure 1A). For a left hemicolectomy, the patient was placed supine and the right hand was tucked in. The laparoscopic monitors were placed on the left side of the patient and the robot was fixated to the left-side bed rail (Figure 1B). For an anterior resection, the patient was placed in reversed trendelenburg position and the both hands were tucked in. The laparoscopic monitors were placed at the patient’s feet and the Freehand robot was fixated to the left-side bed rail (Figure 1C). A three-port technique was used in these cases and the 5 mm port sites were chosen by the operating surgeon based on his ergonomics. Once ports were placed, the robot was positioned and the operation commenced.
The operations were performed using the medial-to-lateral approach. The ureters were identified and preserved prior to mesenteric vascular control. Once sufficiently mobilized the colon was transected and an anastomosis completed. The specimen was exteriorized through a site chosen by the surgeon using a wound protector. Following local fast-track protocols, all patients were offered normal diet once awake. Urethral catheters were removed and the patients mobilized on post-operative day 1. The patients were discharged once they remained well and tolerated diet.
At the termination of the operation, before operating notes were completed, the surgeons were administered a questionnaire to solicit their subjective impression of the Freehand system. The questionnaire sought information on ergonomics, user-difficulty, requirement to convert to a human camera operator and their ability to carry out effective movements to control the robot while operating.
Over the study period, nine patients underwent colorectal operations using the FreeHand robot (Freehand 2010 Ltd., Guildford, Surrey, United Kingdom). There were three females and six males at an average age of 58.9 years (Median 60; Range 49-70; SD ± 7.1). These patients underwent right hemicolectomies (3), extended right colectomies (2), left hemicolectomy (1), sigmoid colectomies (2) and anterior resection (1). The mean robot docking time was 6.33 min (Median 6; Range 4-10; SD ± 1.8).
Intra-operatively, there were no conversions recorded and no adverse events encountered. The mean duration of operation was 122.33 min (Median 100; Range 84-330; SD ± 78.5) and mean estimated blood loss was 113.33 mL (Median 50; Range 10-500; SD ± 151.08). Specifically related to the intra-operative handling of the robot, there were no instances of conversion to a human camera holder. The laparoscope was detached from the robot for lens cleaning/defogging an average of 2.6 times per case (Median 3; Range 1-4; SD ± 0.88), with cumulative mean interruption time of 4.2 min per case (Median 4; Range 1-8; SD ± 2.15).
Post-operation, there were no complications or deaths. The mean duration of hospitalization was 3.2 d (Median 3; Range 2-6; SD ± 1.30). Histologic assessment revealed adequate oncologic targets: 19.8 cm mean proximal margin distance (median 20, range 12-35, SD ± 7.19), 17.22 cm mean distal margin distance (median 18, range 10-20, SD ± 3.42), and 13 mean node harvest (median 12, range 10-18, SD ± 2.55). All patients were alive and disease free after a mean follow-up of 5.1 mo. However, this duration of follow-up was not sufficient to meaningfully assess overall survival or disease-free survival. Three advanced laparoscopic surgeons performed these operations. When the surgeons were interviewed after operation, the surgeons reported that there were good ergonomics (100%), with no limitation on instrument movement (100%), stable image (100%) and better control of surgical field (100%).
Generally, the Anglophone Caribbean lagged behind the developed world in terms of adopting advanced operative techniques due to a combination of resource unavailability, financial limitations and leadership deficiencies[11]. To illustrate this, consider the fact that the initial report on laparoscopic colectomies from the Caribbean[10] came 20 years after it was first reported by Cooperman et al[1].
Similarly, the first report of robotic colectomy was published by Weber et al[12] in March, 2001. They reported two cases in which they used the DaVinci robotic platform (Intuitive Surgical Inc, Sunnyvale, California, United States) to perform a sigmoid colectomy for diverticulitis and a right hemicolectomy for diverticulitis. In the next few years, several reports of robotic colectomies began to appear in the surgical literature for benign and malignant disease[13,14]. However, robotic surgery remained dormant in the Anglophone Caribbean[15]. To the best of our knowledge, there has been no report of colorectal resections using the DaVinci or any other full robotic platform from the Caribbean. The first step toward robotics in the Caribbean was a FreeHand robot-assisted laparoscopic right hemicolectomy performed on November 29, 2021. To illustrate our point once more, this was two decades after robotic hemicolectomy was first described by Weber et al[12].
In the report by Weber et al[12] the DaVinci robot (Intuitive Surgical Inc, Sunnyvale, California, United States) was utilized. However, there are no da Vinci platforms in any nation in the Anglophone Caribbean. It is a resource-poor region with some of the poorest nations in the Western hemisphere. The cases in this report were performed by advanced laparoscopic surgeons with the assistance of the FreeHand robot (Freehand 2010 Ltd., Guildford, Surrey, United Kingdom). This was a single robotic arm that controlled the laparoscope and was under the direct control of the surgeon via an infrared communicator. The resource poor nations in the Caribbean could not afford more advanced robotic platforms that are available on the commercial market, but we found this system to be a good intermediary that brought advantages over conventional laparoscopy while balancing cost.
In our small series, these operations were performed by advanced laparoscopic surgeons who were already facile with laparoscopic colectomies. Therefore, it was not surprising that the mean operating time was comparable to those in published reports on laparoscopic colectomies from the Caribbean[10,11,16] that ranged from 150 min[10] to 175 min[16], as well as reports from international literature[17-20]. Similarly, our other outcomes were comparable to those in reports on laparoscopic colectomies from the region, where the median length of hospitalization ranged from 4[11] to 5[10] days, overall morbidity from 10%[10] to 35.3%[16] and no reported mortality[10,11,16].
Ballantyne et al[21] wrote during their early experience with robotic colectomies in 2001 that the DaVinci system overcame the pitfalls of conventional laparoscopy that included: an unstable video camera platform, limited motion (degrees of freedom) of straight laparoscopic instruments, two-dimensional imaging and poor surgeon ergonomics. Ballantyne et al[21] also wrote that “inexperienced or bored camera-holders move the camera frequently and rotate it away from the horizon.” We agree with Ballantyne et al[21] and we found that the surgeon being in full control of the visual field was a distinct advantage of the FreeHand robot. The operators also unanimously found the stability of the vision advantageous. In our cases, the robot was assigned a conventional 30-degree laparoscope with a single lens. Therefore, unlike the advanced multi-lens cameras in advanced robotic systems that allow depth perception, the FreeHand robot could not overcome the two-dimensional views that is a recognized limitation of conventional laparoscopy.
Surgeon ergonomics has been one criticism of the FreeHand platform. More sophisticated robotic systems such as the DaVinci platform would allow intra-corporeal articulation with specialized instruments, but the Freehand robot had only one arm to operate the camera. Therefore, conventional laparoscopic instruments had to be used in these cases. The straight, long instruments would still be limited in their motion by the fixation enforced by the abdominal wall trocars[21]. Providing more degrees of freedom of movement would require a more sophisticated robot with additional operating arms, but the point was already made that these come at a significant increase in cost. On the other hand, all surgeons in our series unanimously reported that the robotic arm was not intrusive and did not negatively impact surgeon ergonomics, although it did not improve ergonomics either.
We have shown that the use of the FreeHand robot for laparoscopic colorectal resections is feasible, provides some advantages over conventional laparoscopy and has similar short-term outcomes to conventional laparoscopy. From this study, we cannot comment on the long-term outcomes, although we expect it to be similar conventional laparoscopy. It has already been proven and accepted from randomized controlled trials[2-7] and large metanalyses[7,8,22] that conventional laparoscopic colorectal resections have equivalent oncologic outcomes to open surgery.
We acknowledge that these colorectal operations were performed by experienced surgeons who were already facile with laparoscopic colectomies and beyond the learning curves. Therefore, this does introduce some bias in outcomes, but it was equally important to show that this technique was feasible in this setting.
We also acknowledge that the sample size is small. This is a low resource nation with a population of 1.3 million persons so few persons qualified for use of the robotic arm during the study period.
We have shown that robot assisted colorectal surgery is feasible and safe in the resource-poor Caribbean setting.
Laparoscopic colorectal surgery is still developing in the Anglophone Caribbean and there has been no report of robot assisted colorectal surgery in the region. This paper reports our initial experience with advanced colorectal surgery using the Freehand robot.
Robot-assisted colorectal surgery using the FreeHand® robotic camera holder (Freehand 2010 Ltd., Guildford, Surrey, United Kingdom) was introduced to the Caribbean in 2021. We report our initial experience with this technology.
This paper reports the initial experience with the FreeHand(R) robotic camera holder to complete colorectal operations in a resource-poor setting.
A retrospective study was performed, collecting data from all consecutive patients who underwent colorectal operations using the FreeHand robot from September 20201 to April 2022. The data collected included: demographics, docking time, operating time, conversions, number and duration of intra-operative lens cleaning. All operating surgeons completed a survey that sought information on robot use.
There were 9 patients in this study who underwent: Right hemicolectomies (5), left hemicolectomy (1), sigmoid colectomies (2) and anterior resection (1). These operations were completed with a mean robot docking time of 6.33 min, mean duration of surgery of 122.33 min and mean estimated blood loss of 113.33 mL. The laparoscope was detached from the robot an average of 2.6 times per case, with cumulative mean interruption time of 4.2 min per case. The mean duration of hospitalization was 3.2 d and there were no complications recorded. Surgeons reported that there were good ergonomics, with no limitation on instrument movement, stable image and better control of surgical field.
Robot-assisted laparoscopic colorectal surgery is feasible and safe in the resource-poor Caribbean setting, once there is appropriate training.
Future research should incorporate large numbers of patients and a comparison of outcomes between robot-assisted and laparoscopic cases.
| 1. | Cooperman AM, Katz V, Zimmon D, Botero G. Laparoscopic colon resection: a case report. J Laparoendosc Surg. 1991;1:221-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 77] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Lacy AM, Garcia-Valdecasas JC, Delgado S. Laparoscopic-assisted colectomy vs open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359:2224e9. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1901] [Cited by in RCA: 1829] [Article Influence: 76.2] [Reference Citation Analysis (0)] |
| 3. | Clinical Outcomes of Surgical Therapy Study Group, Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, Stryker SJ, Beart RW Jr, Hellinger M, Flanagan R Jr, Peters W, Ota D. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2050-2059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2606] [Cited by in RCA: 2540] [Article Influence: 115.5] [Reference Citation Analysis (0)] |
| 4. | Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M, Lacy AM; COlon cancer Laparoscopic or Open Resection Study Group (COLOR). Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6:477-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1691] [Cited by in RCA: 1709] [Article Influence: 81.4] [Reference Citation Analysis (0)] |
| 5. | Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM; MRC CLASICC trial group. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718-1726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2360] [Cited by in RCA: 2325] [Article Influence: 110.7] [Reference Citation Analysis (0)] |
| 6. | Weeks JC, Nelson H, Gelber S, Sargent D, Schroeder G; Clinical Outcomes of Surgical Therapy (COST) Study Group. Short-term quality-of-life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: a randomized trial. JAMA. 2002;287:321-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 547] [Cited by in RCA: 543] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 7. | Janson M, Lindholm E, Anderberg B, Haglind E. Randomized trial of health-related quality of life after open and laparoscopic surgery for colon cancer. Surg Endosc. 2007;21:747-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 79] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 8. | Jackson TD, Kaplan GG, Arena G, Page JH, Rogers SO Jr. Laparoscopic versus open resection for colorectal cancer: a metaanalysis of oncologic outcomes. J Am Coll Surg. 2007;204:439-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 105] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 9. | Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, Heath RM, Brown JM; UK MRC CLASICC Trial Group. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol. 2007;25:3061-3068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1108] [Cited by in RCA: 1121] [Article Influence: 59.0] [Reference Citation Analysis (0)] |
| 10. | Plummer JM, Mitchell DI, Arthurs M, Leake PA, Deans-Minott J, Cawich SO, Martin A. Laparoscopic colectomy for colonic neoplasms in a developing country. Int J Surg. 2011;9:382-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Cawich SO, Pooran S, Amow B, Ali E, Mohammed F, Mencia M, Ramsewak S, Hariharan S, Naraynsingh V. Impact of a medical university on laparoscopic surgery in a service-oriented public hospital in the Caribbean. Risk Manag Healthc Policy. 2016;9:253-260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Weber PA, Merola S, Wasielewski A, Ballantyne GH. Telerobotic-assisted laparoscopic right and sigmoid colectomies for benign disease. Dis Colon Rectum. 2002;45:1689-94; discussion 1695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 308] [Cited by in RCA: 336] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 13. | D'Annibale A, Morpurgo E, Fiscon V, Trevisan P, Sovernigo G, Orsini C, Guidolin D. Robotic and laparoscopic surgery for treatment of colorectal diseases. Dis Colon Rectum. 2004;47:2162-2168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 254] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 14. | Braumann C, Jacobi CA, Menenakos C, Borchert U, Rueckert JC, Mueller JM. Computer-assisted laparoscopic colon resection with the Da Vinci system: our first experiences. Dis Colon Rectum. 2005;48:1820-1827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 1.8] [Reference Citation Analysis (4)] |
| 15. | Cawich SO, Arulampalam T, Senasi R, Naraynsingh V. Robot-Assisted Minimally Invasive Surgery: First Report from the Caribbean. Cureus. 2021;13:e18739. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Leake PA, Pitzul K, Roberts PO, Plummer JM. Comparative analysis of open and laparoscopic colectomy for malignancy in a developing country. World J Gastrointest Surg. 2013;5:294-299. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Trastulli S, Coratti A, Guarino S, Piagnerelli R, Annecchiarico M, Coratti F, Di Marino M, Ricci F, Desiderio J, Cirocchi R, Parisi A. Robotic right colectomy with intracorporeal anastomosis compared with laparoscopic right colectomy with extracorporeal and intracorporeal anastomosis: a retrospective multicentre study. Surg Endosc. 2015;29:1512-1521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 110] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 18. | Morpurgo E, Contardo T, Molaro R, Zerbinati A, Orsini C, D'Annibale A. Robotic-assisted intracorporeal anastomosis versus extracorporeal anastomosis in laparoscopic right hemicolectomy for cancer: a case control study. J Laparoendosc Adv Surg Tech A. 2013;23:414-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 97] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 19. | Petrucciani N, Sirimarco D, Nigri GR, Magistri P, La Torre M, Aurello P, D'Angelo F, Ramacciato G. Robotic right colectomy: A worthwhile procedure? J Minim Access Surg. 2015;11:22-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 20. | Lujan HJ, Plasencia G, Rivera BX, Molano A, Fagenson A, Jane LA, Holguin D. Advantages of Robotic Right Colectomy With Intracorporeal Anastomosis. Surg Laparosc Endosc Percutan Tech. 2018;28:36-41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 54] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 21. | Ballantyne GH, Merola P, Weber A, Wasielewski A. Robotic solutions to the pitfalls of laparoscopic colectomy. Osp Ital Chir. 2001;7:405-412. [RCA] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 44] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Bonjer HJ, Hop WC, Nelson H, Sargent DJ, Lacy AM, Castells A, Guillou PJ, Thorpe H, Brown J, Delgado S, Kuhrij E, Haglind E, Påhlman L; Transatlantic Laparoscopically Assisted vs Open Colectomy Trials Study Group. Laparoscopically assisted vs open colectomy for colon cancer: a meta-analysis. Arch Surg. 2007;142:298-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 397] [Cited by in RCA: 390] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Trinidad and Tobago
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Badessi G, Italy; Lei Y, China A-Editor: Zhu JQ, China S-Editor: Liu JH L-Editor: A P-Editor: Liu JH