Peer-review started: November 19, 2022
First decision: December 13, 2022
Revised: December 17, 2022
Accepted: February 22, 2023
Article in press: February 22, 2023
Published online: March 9, 2023
Processing time: 108 Days and 5.9 Hours
Bibliometric analysis can be used to assess the current state of the literature and publication trends on a given topic. There has not been a review of this kind on prostatic artery embolization (PAE) for benign prostatic hyperplasia (BPH). PAE is a relatively new and somewhat controversial treatment option for BPH. Given the novelty and controversy, there has been much research published on the topic recently.
To survey the current state of research on PAE for BPH by using bibliometric analysis to analyze the top 50 most highly cited articles.
A cross-sectional study was performed using the Web of Science database to identify the most cited articles published on PAE for BPH as of June 2022. Articles that did not primarily focus on PAE or BPH as an indication were eliminated. The 50 most cited articles were carried forward for analysis.
All but 6 articles were published in the last decade with contributions from 15 countries. Fifty-two percent of the studies had a C level of evidence. The majority were published in the Journal of Vascular and Interventional Radiology and Cardiovascular and Interventional Radiology. Twenty percent (n = 10) of the articles were published in urologic journals. On average, articles published in urologic journals tended to be more recent. The mean year of publication for an article in a urological journal was 2016.6 compared to 2013.9 in a non-urologic journal (P = 0.02). Seventy percent of the articles focused on clinical outcomes, while only 2% focused on practice guidelines. Self-citations accounted for 11.4 citations per article on average, corresponding to 14.7% of all citations analyzed.
The most influential papers on this topic represent a fairly recent body of work with contributions from a wide variety of countries and journals. The fact that articles in urologic journals were published significantly more recently than articles on the list in non-urologic journals may suggest that the field of urology is starting to accept PAE for a wider range of indications. Finally, while there has been much high-quality research published, more influential studies on practice guidelines and technique may be beneficial.
Core Tip: Prostatic artery embolization is a technique for treating certain patients with benign prostatic hyperplasia that although controversial is gaining traction. We utilized bibliometric review to investigate the current landscape of the literature on this topic. Based on the publication trends in the most influential papers on this topic it appears that urologists may be starting to recognize the merits of the procedure. Additionally, this procedure has an international appeal with literature being published out of a wide variety of countries in radiology and urology journals alike.
- Citation: Zoppo CT, Taros T, Harman A. Top 50 most cited articles on prostatic artery embolization for benign prostatic hyperplasia: A bibliometric review. World J Clin Urol 2023; 12(1): 1-9
- URL: https://www.wjgnet.com/2219-2816/full/v12/i1/1.htm
- DOI: https://dx.doi.org/10.5410/wjcu.v12.i1.1
Prostatic artery embolization (PAE) for the treatment of benign prostatic hyperplasia (BPH) is a relatively new, interventional radiology (IR) procedure that may serve as an alternative to traditional surgical methods in some patients. Articles on PAE for BPH began to be published in the early 2000s and since then, it has become a prominent area of IR and urologic research[1]. PAE has been shown to be an effective procedure, with success rates at 1-3 years and > 3 years post-procedure of 81.9% and 76.3% respectively[2]. Some have cited possible benefits over traditional surgical methods including shorter hospital stay, lower rates of urinary incontinence, and lower rates of retrograde ejaculation[3,4]. Nevertheless, there remains controversy surrounding the use of PAE to treat BPH by some professional societies indicating that ongoing investigation is necessary[5].
Bibliometric studies have been heralded as a way of measuring that which is inherently difficult to quantify, the quality and scope of the body of research for a specific topic[6]. They have been used to identify trends, find gaps within the evidence base, and provide guidance into new areas of study[7]. Of the many types of bibliometric reviews, citation analysis has become a popular methodology for evaluating a given subject[6,8]. Citation reviews in particular allow researchers to identify hot or controversial topics within the field, determine the nations that are leading the field, and can quantify the strength of the current evidence overall. This type of citation analysis has not previously been done on PAE for BPH.
Citation analysis was used to identify the characteristics of the current state of the literature surrounding PAE for BPH. A search was conducted for the 50 most highly cited articles within the current body of evidence. Given the controversy surrounding the subject, care was taken to identify the level of evidence present within each article.
In June 2022 the Clarivate Web of Science (WoS) database was used to identify articles that discussed PAE for BPH using the search terms: (PAE AND Prostate) OR [(Prostatic OR Prostate) AND (Embolization OR Embolisation)]. Fourth year medical students trained in bibliometric review performed the search, any discrepancies were discussed at length based on full text review. These articles were sorted by number of citations in descending order. Article titles and abstracts were used as an initial screen for inclusion, which was performed by a single author. Duplicate articles and those not focusing on PAE for BPH were excluded. The remaining articles were exported for further full text analysis.
The WoS database extracted several variables of interest pertinent to each article, including title, journal, citation count, year published and country of origin. Other variables of interest, such as level of evidence and article type, were extracted through full-text review by reviewers. Self-citation search was carried out by authors using analysis of citations within Google Scholar. Variables were extracted from the WoS database and exported to Microsoft Excel which was used to store, analyze, and visualize the data. The level of evidence was determined independently by two authors using guidelines from the Journal of Vascular and Interventional Radiology 2018 methodology update and Oxford Centre for Evidence-based Medicine[9,10]. Prior to the database search, article categories were determined to consist of clinical outcomes, technique, imaging/anatomy, translational, guidelines, and other. Each article was classified into only one category based on the consensus opinion of two authors.
A t-test was used to compare the mean year of publication between articles on the list that were published in urology journals compared to those that were not. Statistical significance was determined as P < 0.05.
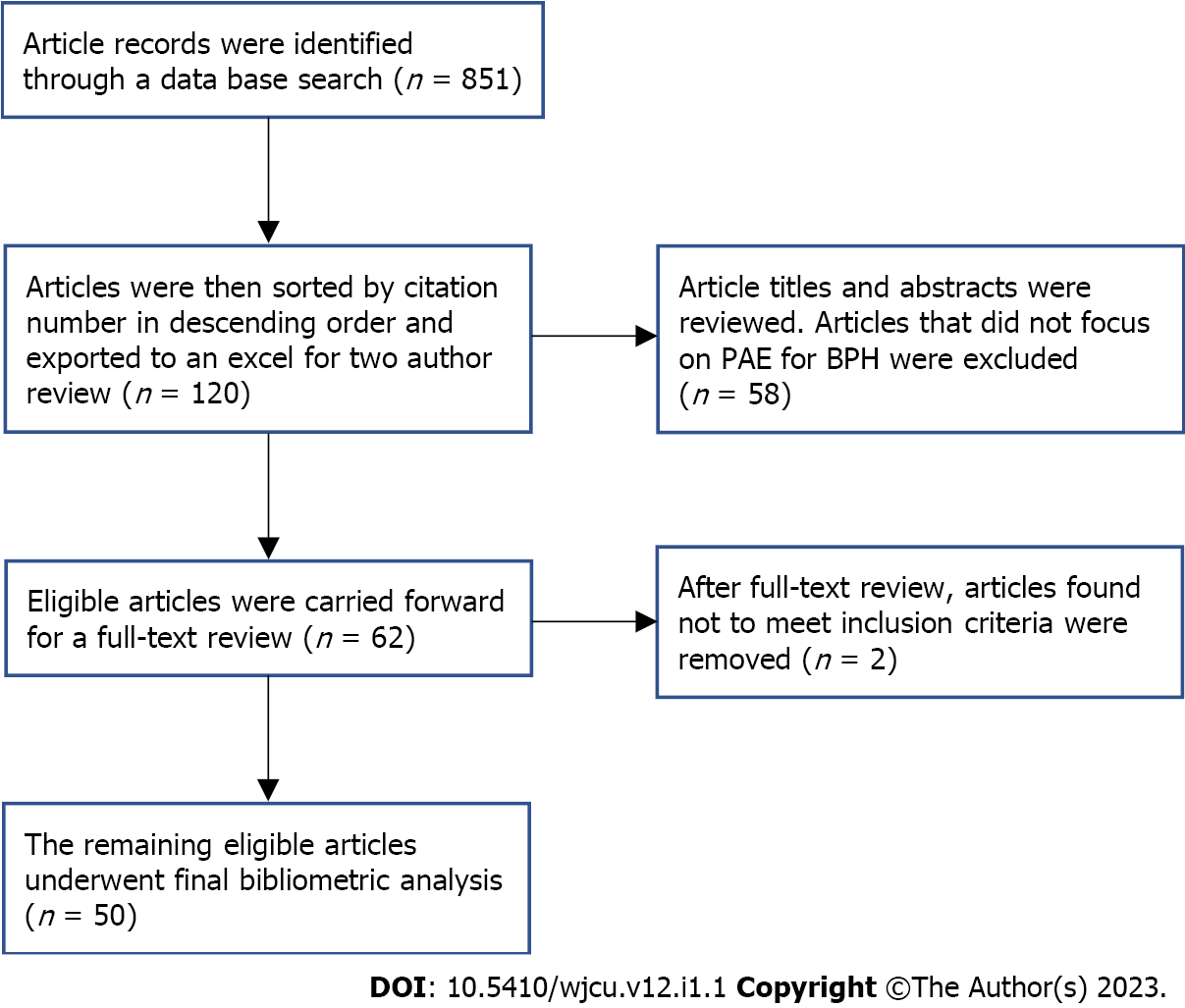
The initial search generated 851 articles. The titles and abstracts were reviewed for the first 120 articles. 58 were found not to focus on PAE specifically for BPH and were excluded from analysis leaving 62 articles that were exported for full text review. 2 additional articles were excluded after full text review, which determined that they were only tangentially related to PAE for BPH (Figure 1)[11,12]. Of the remaining articles, the 50 most cited were analyzed in this review (Supplementary Table 1).
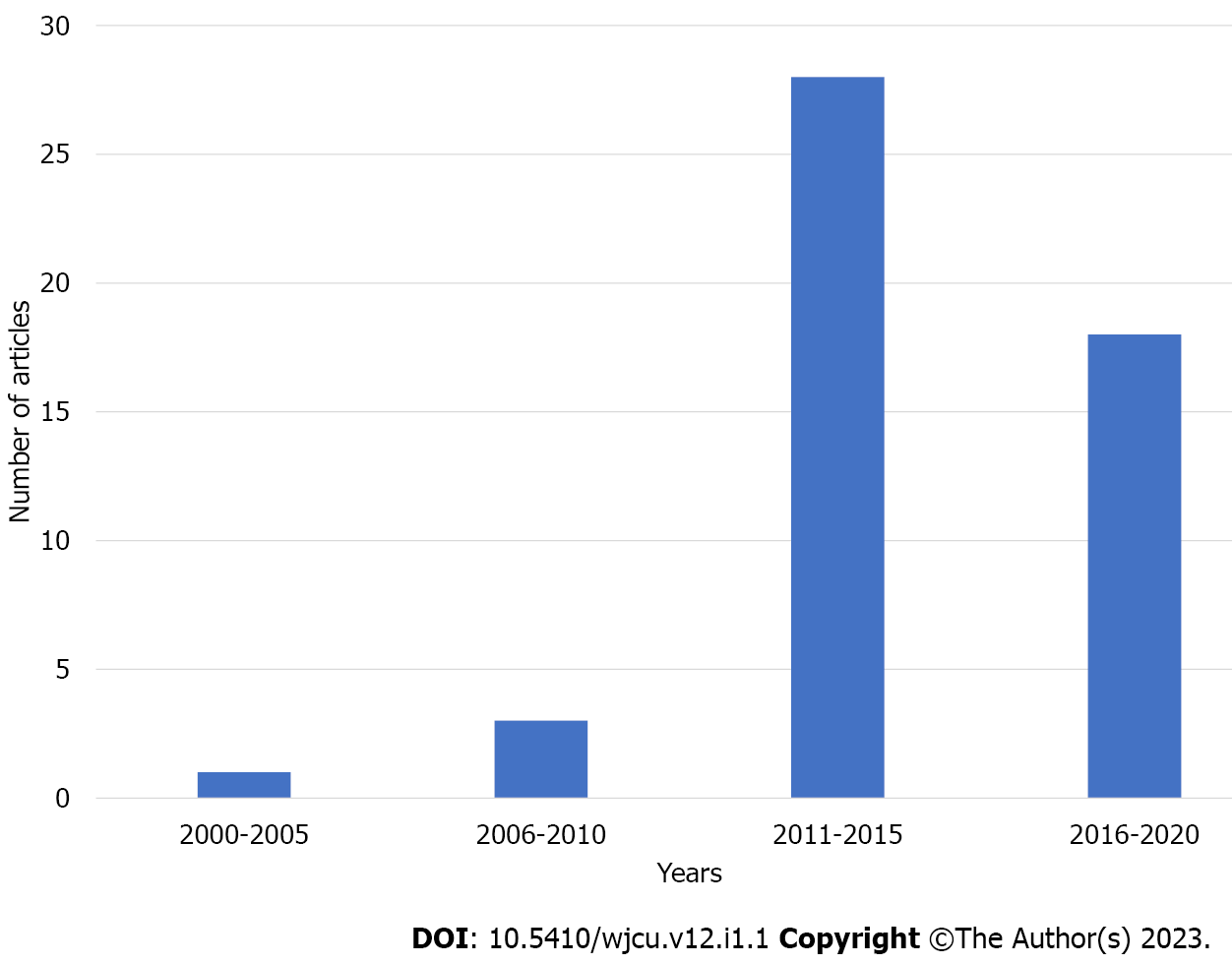
All articles were published between 2000 and 2020 with 46 published between 2011 and 2020 (Figure 2). Additionally, 9 of the top 10 articles were published during this period. The average number of citations was 77.3 with a range of 34-171 and median of 64.5. Nine articles were considered neither positive nor negative towards PAE for BPH, of the remaining 41 articles analyzed 40 (97.6%) were considered to be positive in favor of PAE for BPH.
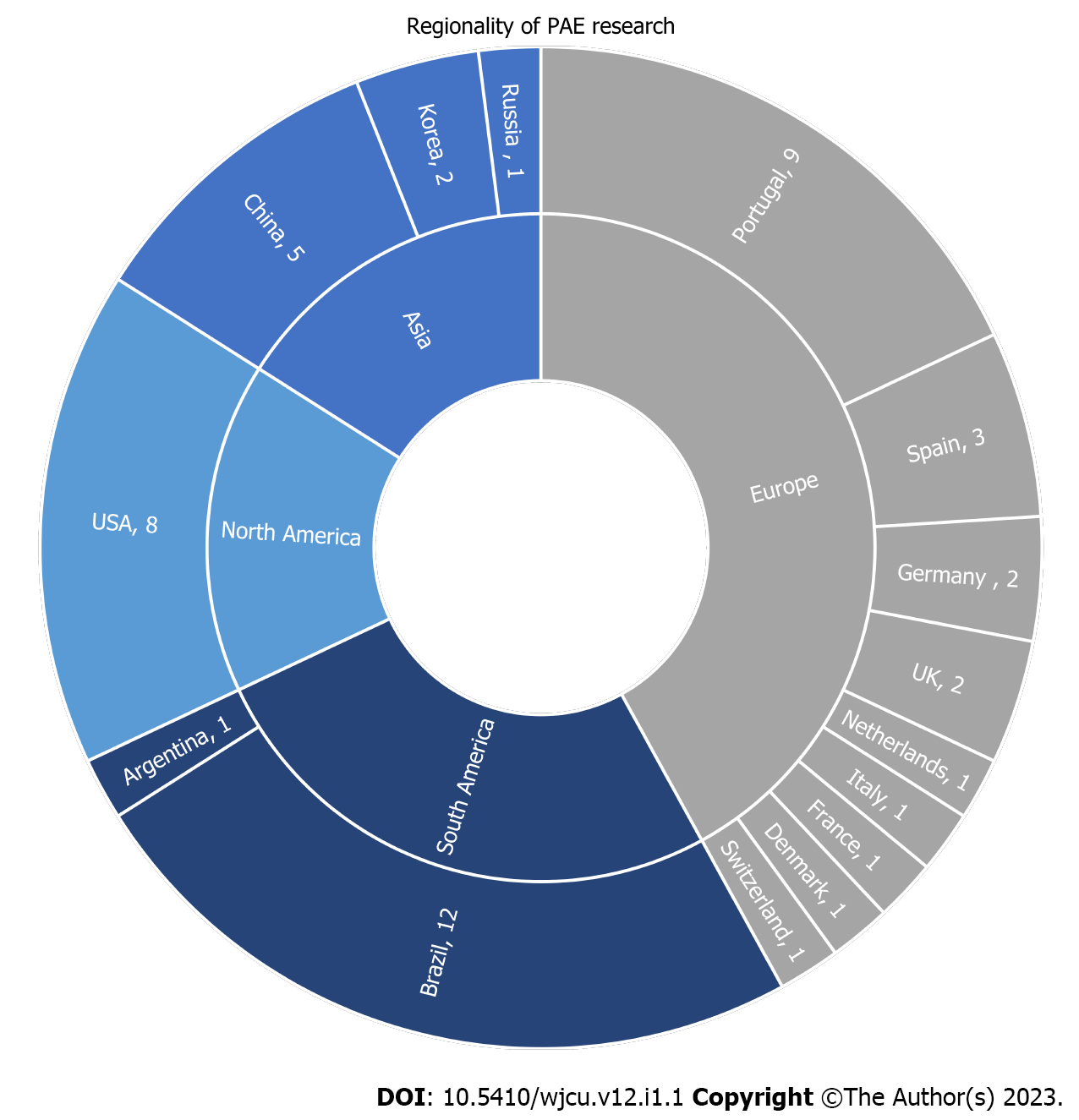
The top 50 most cited articles represent the work of researchers from 15 different countries. Brazil had the highest number of contributions (n = 12), followed by Portugal (n = 9), the United States (n = 8), and China (n = 5) (Figure 3).
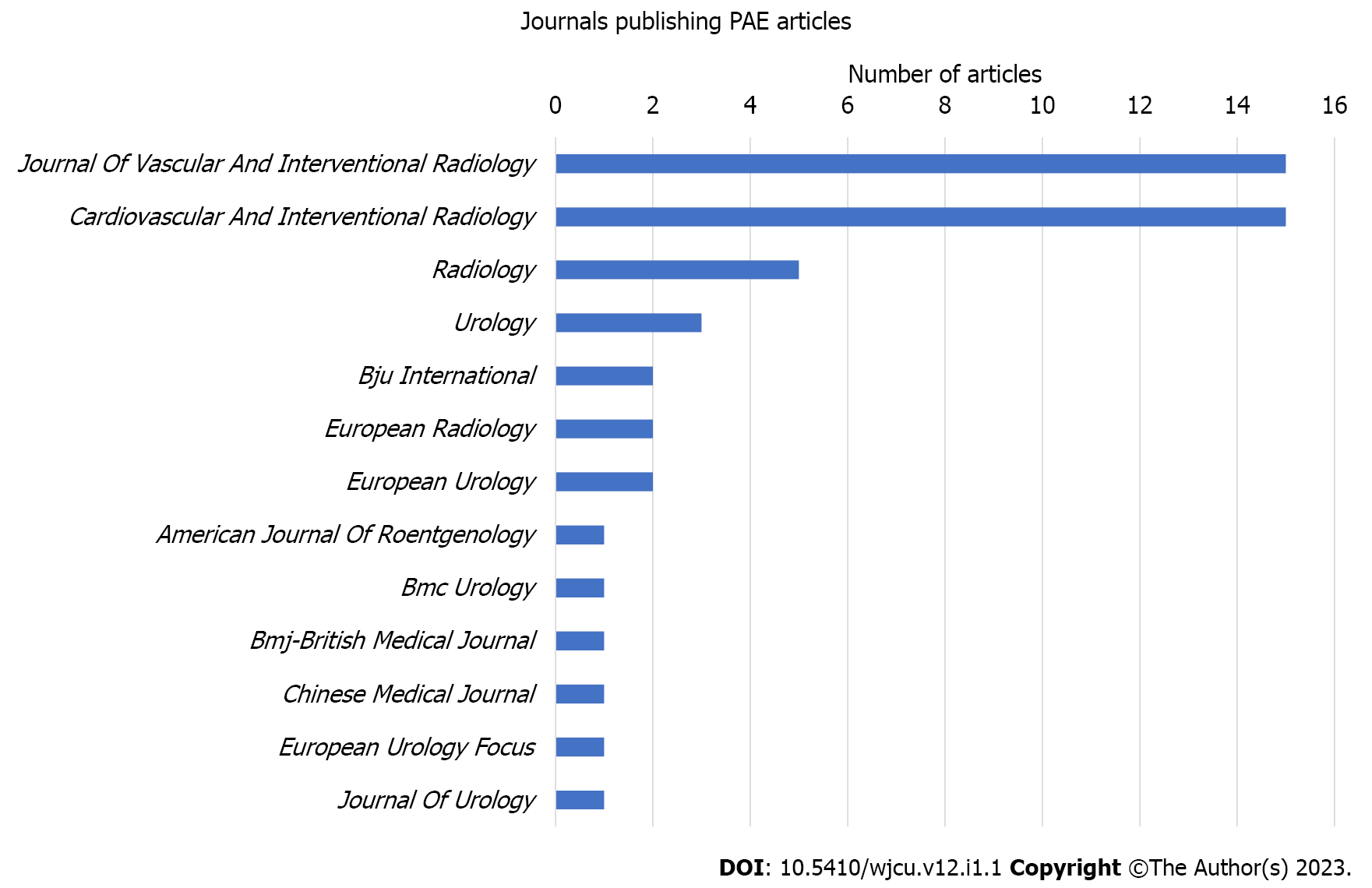
The analyzed articles were published in 13 different journals with over half published in the Journal of Vascular and Interventional Radiology (n = 15) and Cardiovascular and Interventional Radiology (n = 15). Radiology was the next most productive journal (n = 5) with all other journals having fewer than 4 contributions (Figure 4).
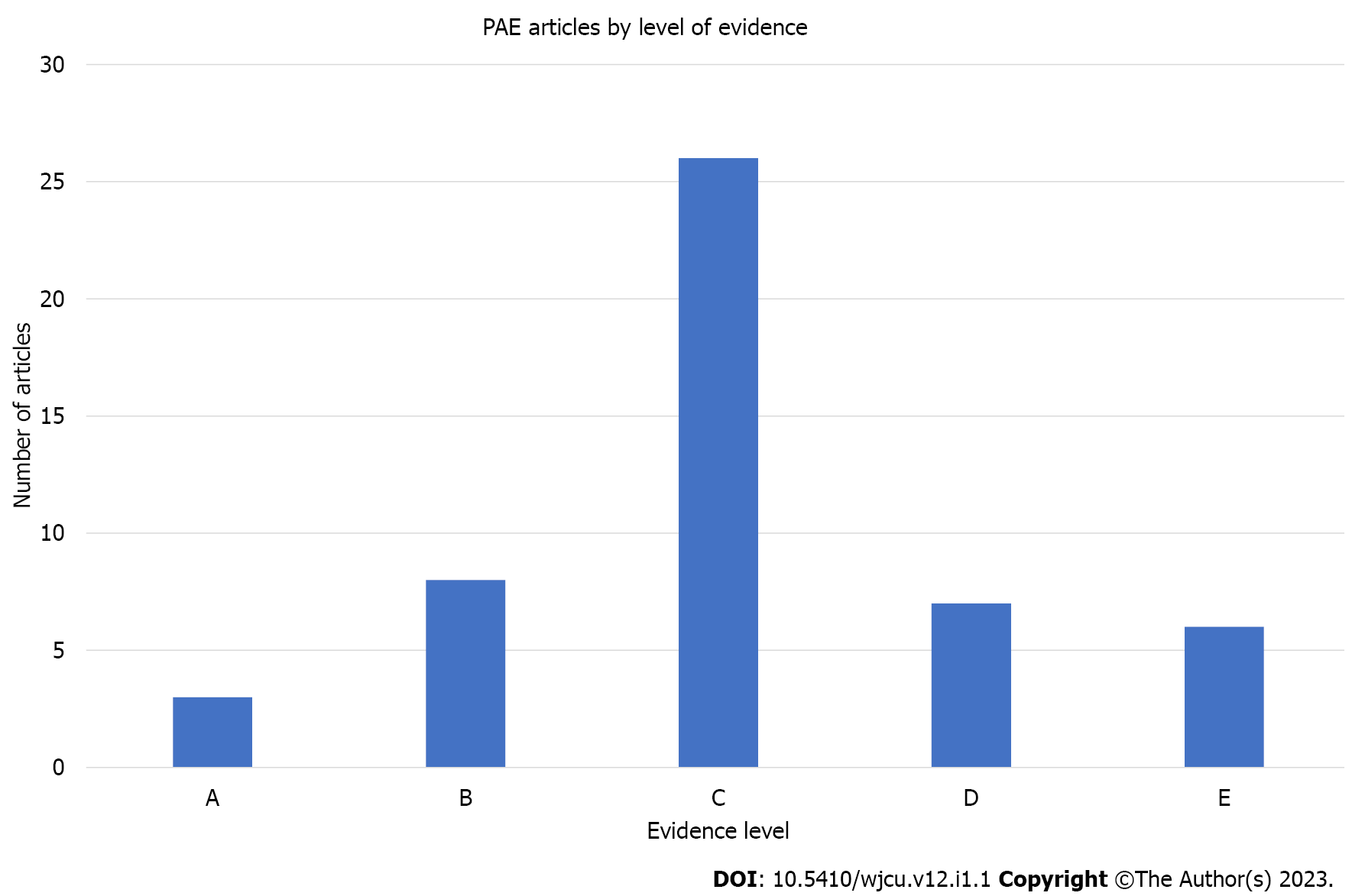
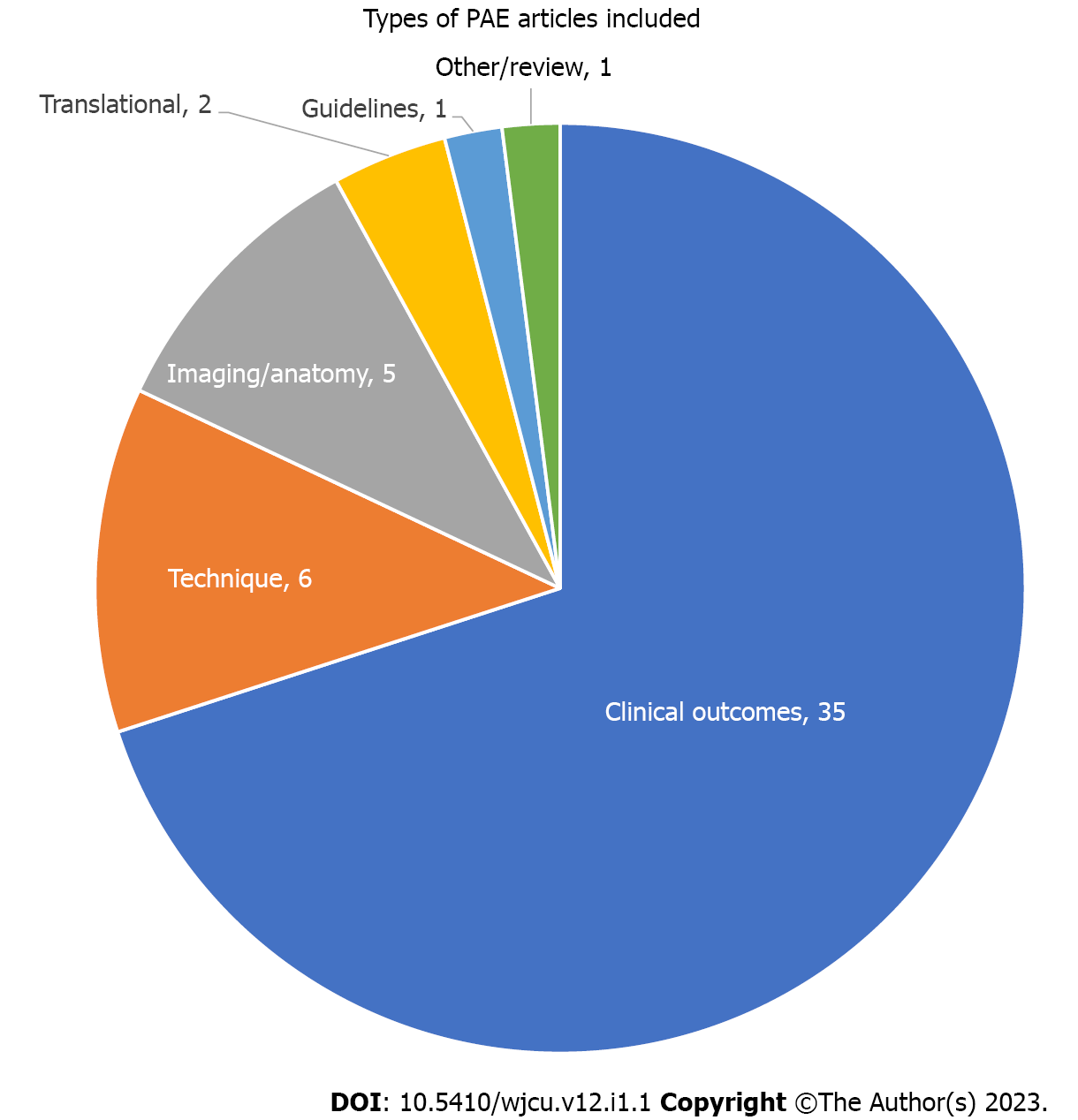
The most common level of evidence was C (n = 26), followed by B (n = 8), D (n = 7), E (n = 6), and A (n = 3) (Figure 5). The majority of articles were classified as clinical outcomes (n = 35), followed by technique (n = 6), imaging/anatomy (n = 5), translational (n = 2), guidelines (n = 1), and basic science (n = 1) (Figure 6).
Twenty percent (n = 10) of the articles were published in urologic journals. On average, articles published in urologic journals tended to be more recent. The mean year of publication for an article in a urological journal was 2016.6 compared to 2013.9 in a non-urologic journal (P = 0.02).
Self-citations accounted for 14.7% of all citations, or an average of 11.4 self-citations per article, for the top 50 most cited articles. Seventy-two percent of the articles analyzed had greater than 10% of their citations coming from the authors of the article themselves. Two articles had no self-citations.
The most cited studies of PAE for BPH were published out of a variety of countries, with Brazil, Portugal, the United States, and China being particularly well represented. Some of the first research on PAE was conducted in China, so it is unsurprising that the number one cited paper was published by a research group based there. Additionally, much of the early research by Wang is represented at various positions in the list, including at the 21st, 33rd, and 36th spots.
Though articles on the topic were first published in the early 2000s, many of the most highly cited articles have been published in the last decade. This illustrates both continued high-quality research and the growing popularity of the procedure based on a track record of safety and efficacy. Many of these recent articles focus on clinical outcomes. This is not surprising given surgical therapies such as TURP have long been accepted as reliable options for the treatment of BPH refractory to medical management. Surgical management has well demonstrated benefits and clearly outlined risks, therefore much work had to be done to demonstrate the noninferiority of PAE as it became more commonplace. The Society of Interventional Radiology, along with other professional societies have continued to support this kind of research, urging for larger trials with longer follow-up periods to compare PAE to established surgical therapies[13].
It is likely that strong research in the field has been important for the adoption of PAE as an established therapy by practice groups and specialty societies. Additionally, with increasing interest and access to scientific literature, this research is also important in informing patients who may be interested in a variety of treatment options for BPH. As the efficacy and safety of PAE continues to be demonstrated, the proportion of patients who self-refer for the procedure may also be growing[14]. Despite this body of research, PAE is not a universally recognized alternative to existing therapies in appropriate patients[12,15]. Though outcomes research will likely remain a popular article subject, over time it is possible that more of the influential research in the field will shift to updating practice guidelines and improving techniques.
Despite strong resistance early on, our findings suggest that the field of urology may be starting to accept PAE for a wider range of indications. This is supported by the fact that articles in urologic journals were published significantly more recently than articles on the list in non-urologic journals. Still, official urologic guidelines such as those published by the American Urologic Association still do not support PAE for BPH[12]. Continued publication of high impact research on this topic may indicate slowly changing opinions on these specific indications in the field.
The majority of the top articles had a “C” level of evidence, which was somewhat expected given the novelty of the field. Performing a randomized controlled trial (RCT) that meets the criteria for an “A” level of evidence is challenging in any field, however some of these barriers are more apparent when investigating PAE. Given that PAE is a relatively new treatment option, patient volume can be a concern when attempting to construct large scale RCTs. The case volume at some centers is growing, which will likely enable larger scale RCTs as well as cohorts for retrospective analysis[14].
Though high quality RCTs are considered the gold standard, not all clinical questions lend themselves to this type of analysis, and the value of other well-designed studies should not be discounted. The utility of observational studies in complementing randomized trial findings is clearly demonstrated by the United Kingdom ROPE study, which showed PAE could be a cost-effective surgery alternative in certain healthcare systems[3]. The ease of performing these large-scale studies will only improve with increased procedure volume. Increased recognition by patients and specialty societies will also aid in opening the door for more high-level research.
The highest cited paper of the group, “Benign Prostatic Hyperplasia: Prostatic Arterial Embolization vs Transurethral Resection of the Prostate-A Prospective, Randomized, and Controlled Clinical Trial” by Gao et al[16] garnered 171 citations and was one of a handful to earn an “A” level of evidence. This paper was the culmination of several smaller studies by Gao et al[16] and the rest of his China-based team, some of which represent the earliest PAE related research found[1]. This is a high quality, well designed RCT that came at a time when there were few prospective randomized studies within the literature. Despite its relatively small sample size, it was a critical early study in affirming the efficacy of PAE for BPH, even when compared to the gold standard operative management. It also was among the first to outline a specific methodology for performing PAE, which others continue to build on. As the first RCT on the subject, its position at the top of the list is not surprising.
“Embolization of prostatic arteries as treatment of moderate to severe lower urinary symptoms (LUTS) secondary to benign hyperplasia: results of short- and mid-term follow up” by Pisco et al[17] was cited 155 times, the second most cited article of those evaluated. This early, large, and well-designed prospective study demonstrated the safety and efficacy of PAE in treating moderate and severe, medically refractory BPH. Having been published in 2013, this study came at a time when there were few nonsurgical options for these patients. Contributing to the popularity of this article is the framework the study established, one that other authors such as Carnevale et al[4] would use in later prospective randomized trials.
With 134 citations, the third most highly cited article on this list is 2015’s “Transurethral Resection of the Prostate (TURP) Versus original and PErFecTED Prostate Artery Embolization (PAE) Due to Benign Prostatic Hyperplasia (BPH): Preliminary Results of a Single Center, Prospective, Urodynamic-Controlled Analysis” by Carnevale et al[4]. Only the second RCT published on PAE, it sought to expand upon the works published by Gao et al[16] and Pisco et al[17]. This study utilized urodynamic evaluation to assess patient’s bladder dysfunction, something previous studies had not evaluated, likely due to the invasiveness of the testing. The use of these established metrics for evaluating participants was important in producing a more quantitative comparison between PAE and TURP. Additionally, this study included a third arm allowing for the evaluation of two different methods for PAE, something not done before. The study’s findings supported earlier works by other authors and laid the foundation for future PAE research.
At first glance, the self-citation rate of 14.7% may seem unreasonably high, leading to questions of the validity of the research of PAE for BPH. This is explained, however, by the status of many of these papers as landmark studies within the PAE literature. In this setting, the high self-citation rate corresponds to the continued work of many prolific authors, whose citing of themselves is quite reasonable as they are often the innovators who created and published on many of the popular techniques employed today.
The goal of the bibliometric review is to analyze the most influential articles in a given field. Despite contributing to the literature on this topic, the analysis does have some limitations. Citations were the only measure used within this study to rank articles. Although considered a good measure, citations do not consider all dimensions of influence an article may have. This measure is also biased towards older articles which have had more opportunity to be cited. Newer, potentially more influential articles may not have been included due to inadequate time to accrue citations. Citation counts for each article were generated by WoS which does not count citations from every journal. Finally, citations in certain types of publications such as books, patents, conference proceedings, and dissertations, among others, are not counted. As a result, the full influence of some publications may not be fully reflected by the analysis.
The most influential research articles on PAE come from a variety of countries and represent a fairly recent body of work with all but 6 published in the last decade. The majority of these highly cited works were published in either JVIR or CVIR, though 20% of the articles were published in urologic journals. Both of these fields will likely remain important sources of influential research on this topic. Though PAE is more widely accepted today, some still feel there is insufficient evidence to support it for BPH. The sustained resistance illustrates the continued need for large, high-quality studies to corroborate previously published findings, outline improved techniques, and develop impactful and up-to-date practice guidelines to ensure optimal patient outcomes.
Prostate artery embolization (PAE) for benign prostatic hyperplasia (BPH) is a new technique hardly past its infancy. Past studies have evaluated the utility, indications, efficacy and basic science of the procedure. Although there have been some systematic studies, a bibliometric review has not been conducted prior to this study.
This bibliometric review will analyze the 50 most cited articles with regards to PAE for BPH. This will show the strengths and weaknesses of the current body of literature, where said literature is being produced, and will attempt to quantify the growing acceptance of this procedure by the field of urology.
By performing a bibliometric review, it is hoped that avenues for future expansion of the literature are elucidated. This will allow future researchers to better pursue novel and helpful research, rather than studies similar to those that have already been conducted and are well-respected.
The bibliometric review, while popular in many fields, has not seen the same level of acceptance in the fields of interventional radiology or urology. As described previously, PAE for BPH is relatively cutting-edge and the literature on the subject is not yet well-established. Therefore, it is unsurprising that this study represents the first bibliometric analysis of PAE for BPH.
The top 50 articles on PAE for BPH were all written within the last two decades, with a heavy bias towards the last decade. Although only 20% of these articles were published in urology journals, those that were published within these journals were significantly newer than their non-urologically published counterparts. The C level of evidence was the most common level represented. Future research should include higher evidence level studies (comparative randomized control trials and meta-analyses) and may be more likely to be accepted into urology journals.
The methodology of applying a bibliometric review to PAE for BPH is a completely novel endeavor. This theory proposes the idea that the literature for PAE for BPH is young but growing. Additionally, our results suggest that PAE for BPH is steadily gaining greater acceptance within the field of urology.
Future research should be directed towards high evidence level studies. This will steadily increase the evidence level seen by future bibliometric reviews as would be expected in a young but rapidly expanding field.
| 1. | Lawler P, Miao W, Williams P. From the editor's desk: frontiers in medicine: the McGill Journal of Medicine celebrates ten years, and insights into interventional medicine. Mcgill J Med. 2007;10:71-72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Pisco JM, Bilhim T, Pinheiro LC, Fernandes L, Pereira J, Costa NV, Duarte M, Oliveira AG. Medium- and Long-Term Outcome of Prostate Artery Embolization for Patients with Benign Prostatic Hyperplasia: Results in 630 Patients. J Vasc Interv Radiol. 2016;27:1115-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 189] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 3. | Ray AF, Powell J, Speakman MJ, Longford NT, DasGupta R, Bryant T, Modi S, Dyer J, Harris M, Carolan-Rees G, Hacking N. Efficacy and safety of prostate artery embolization for benign prostatic hyperplasia: an observational study and propensity-matched comparison with transurethral resection of the prostate (the UK-ROPE study). BJU Int. 2018;122:270-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 160] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 4. | Carnevale FC, Iscaife A, Yoshinaga EM, Moreira AM, Antunes AA, Srougi M. Transurethral Resection of the Prostate (TURP) Versus Original and PErFecTED Prostate Artery Embolization (PAE) Due to Benign Prostatic Hyperplasia (BPH): Preliminary Results of a Single Center, Prospective, Urodynamic-Controlled Analysis. Cardiovasc Intervent Radiol. 2016;39:44-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 200] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 5. | Lerner LB, McVary KT, Barry MJ, Bixler BR, Dahm P, Das AK, Gandhi MC, Kaplan SA, Kohler TS, Martin L, Parsons JK, Roehrborn CG, Stoffel JT, Welliver C, Wilt TJ. Management of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia: AUA GUIDELINE PART II-Surgical Evaluation and Treatment. J Urol. 2021;206:818-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 196] [Article Influence: 39.2] [Reference Citation Analysis (0)] |
| 6. | Wallin JA. Bibliometric methods: pitfalls and possibilities. Basic Clin Pharmacol Toxicol. 2005;97:261-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 274] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 7. | Zupic I, Čater T. Bibliometric Methods in Management and Organization. Organ Res Methods. 2015;18. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1309] [Cited by in RCA: 1374] [Article Influence: 114.5] [Reference Citation Analysis (0)] |
| 8. | Donthu N, Kumar S, Mukherjee D, Pandey N, Lim WM. How to conduct a bibliometric analysis: An overview and guidelines. J Bus Res. 2021;133. [DOI] [Full Text] |
| 9. | Tam AL, Findeiss L, Dake MD, Collins JD, Liu RW, Haskal ZJ, Vedantham S, Sedory SE, Marx MV. Standards 2.0: Methodology Update. J Vasc Interv Radiol. 2018;29:1347-1349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | OCEBM Levels of Evidence Working Group. The Oxford 2011 Levels of Evidence. Oxford Centre for Evidence-Based Medicine. [cited 11 July 2022]. Available from: https://www.cebm.net/index.aspx?o=5653. |
| 11. | Nickel JC, Aaron L, Barkin J, Elterman D, Nachabé M, Zorn KC. Canadian Urological Association guideline on male lower urinary tract symptoms/benign prostatic hyperplasia (MLUTS/BPH): 2018 update. Can Urol Assoc J. 2018;12:303-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 12. | Parsons JK, Dahm P, Köhler TS, Lerner LB, Wilt TJ. Surgical Management of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia: AUA Guideline Amendment 2020. J Urol. 2020;204:799-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 113] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 13. | McWilliams JP, Bilhim TA, Carnevale FC, Bhatia S, Isaacson AJ, Bagla S, Sapoval MR, Golzarian J, Salem R, McClure TD, Kava BR, Spies JB, Sabharwal T, McCafferty I, Tam AL. Society of Interventional Radiology Multisociety Consensus Position Statement on Prostatic Artery Embolization for Treatment of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia: From the Society of Interventional Radiology, the Cardiovascular and Interventional Radiological Society of Europe, Société Française de Radiologie, and the British Society of Interventional Radiology: Endorsed by the Asia Pacific Society of Cardiovascular and Interventional Radiology, Canadian Association for Interventional Radiology, Chinese College of Interventionalists, Interventional Radiology Society of Australasia, Japanese Society of Interventional Radiology, and Korean Society of Interventional Radiology. J Vasc Interv Radiol. 2019;30:627-637.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 85] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 14. | Sharma H, Maron SZ, Rastinehad AR, Fischman AM. Prostate artery embolization: increasing self-referrals and awareness of treatment options. CVIR Endovasc. 2021;4:64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 15. |
Lerner LB, McVary KT, Barry MJ, et al Management of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia: AUA GUIDELINE PART II-Surgical Evaluation and Treatment.
|
| 16. | Gao YA, Huang Y, Zhang R, Yang YD, Zhang Q, Hou M, Wang Y. Benign prostatic hyperplasia: prostatic arterial embolization versus transurethral resection of the prostate--a prospective, randomized, and controlled clinical trial. Radiology. 2014;270:920-928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 225] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 17. | Pisco JM, Rio Tinto H, Campos Pinheiro L, Bilhim T, Duarte M, Fernandes L, Pereira J, Oliveira AG. Embolisation of prostatic arteries as treatment of moderate to severe lower urinary symptoms (LUTS) secondary to benign hyperplasia: results of short- and mid-term follow-up. Eur Radiol. 2013;23:2561-2572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 148] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Society of Interventional Radiology, No. 00155853; American Roentgen Ray Society, No. 776734; American College of Radiology, No. ACR-053445865.
Specialty type: Urology and nephrology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Gadelkareem RA, Egypt; He G, China S-Editor: Chen YL L-Editor: A P-Editor: Chen YL