Published online Aug 20, 2013. doi: 10.5321/wjs.v2.i3.48
Revised: March 27, 2013
Accepted: April 10, 2013
Published online: August 20, 2013
Processing time: 112 Days and 9.9 Hours
AIM: To show the efficacy of reconstruction and rehabilitation of large acquired maxillofacial defects due to tumor resections and firearm injuries.
METHODS: The study group comprised of 16 patients (10 men and 6 women) who were operated on because of their maxillofacial defects under local and general anesthesia between June 2007 and June 2011. Prosthetic treatment with the aid of dental implants was performed for all of the patients. Eight patients received an implant supported fixed prosthesis; six patients received implant supported overdentures and two patients received both. Patients were followed up postoperatively for 1 to 4 years. Implant success and survival rates were recorded. Panoramic radiographs were taken preoperatively, immediately after surgery, immediately after loading and at every recall session. Peri-implant and prosthetic complications were recorded. Subjects were asked to grade their oral health satisfaction after treatment according to 100 mm visual analog scale (VAS) and the oral health related quality of life of the patients was measured with the short-form Oral Health Impact Profile.
RESULTS: Five implants (3 in the mandible, 2 in the maxilla) in five patients were lost, while the other 53 survived, which brings an overall survival rate of 91.37% on the implant basis, but 68.75% on patient basis. All the failed implants were lost before abutment connection and were therefore regarded as early failures. For all failed implants, new implants were placed after a 2 mo period and the planning was maintained. The mean marginal bone loss (MBL) was 1.4 mm on the mesial side and 1.6 mm on the distal side of the implants. Five of the implants showed MBL > 2 mm (mean MBL = 2.3 mm) but less than 1/2 of the implant bodies and therefore were regarded as not successful but surviving implants. The VAS General Comfort mean score was 85.07, the VAS Speech mean score was 75.25 and the VAS Esthetics mean score was 82.74. No patient reported low scores (score lower than 50) of satisfaction in any of the evaluated factors. The mean of OHIP-14 scores was 5.5.
CONCLUSION: Although further follow up and larger case numbers will give more information about the success of dental implants as a treatment modality in maxillofacial defects patients, the actual results are encouraging and can be recommended for similar cases.
Core tip: Dental implant treatment is efficient in the reconstruction and rehabilitation of large acquired maxillofacial defects due to tumor resections and firearm injuries. Although further follow up and larger case numbers will give more information about the success of dental implants as a treatment modality in patients with maxillofacial defects, the actual results are encouraging and can be recommended for similar cases.
- Citation: Atalay B, Bilhan H, Geckili O, Bilmenoglu C, Meric U. Clinical evaluation of implants in patients with maxillofacial defects. World J Stomatol 2013; 2(3): 48-55
- URL: https://www.wjgnet.com/2218-6263/full/v2/i3/48.htm
- DOI: https://dx.doi.org/10.5321/wjs.v2.i3.48
Maxillofacial defects are initiated either by trauma or tumor resection. In both cases, the function and esthetics of the patients are impaired and a prosthetic rehabilitation is essential. Since removable prosthetic appliances function on soft tissues and the denture bearing areas are supposed to be composed of keratinized mucosa, defect cases create a challenge. Most of the acquired defects are surgically covered with thin mucosa which is not able to support denture bases. In this manner, dental implant treatment is a valuable aid to support the dentures, leaving the non-keratinized mucosa unloaded[1]. The use of dental implants in patients after trauma due to oral surgical resections, deformities, accidents or firearm injuries can give patients better function and self confidence by the achievement of retention and stability[1,2].
The structural and functional rehabilitation of maxillofacial defects, after oral tumor resection, maxillofacial trauma such as firearm injuries, avascular bone necrosis or large bone cysts, requires prosthetic reconstruction in most of the related patients. Local oral conditions, general health, as well as psychological, social and economic aspects, determine the final treatment outcome of the prosthetic rehabilitation[3]. The prosthodontic treatment in these patients creates a challenge due to several factors, such as bone volume deficiency, low quality of bone, altered anatomy, xerostomia, missing attached gingiva and associated fragile mucosa[4,5].
Maxillofacial defects caused by different reasons represent a challenging problem with regard to restoring optimal oral function and esthetics. These kinds of wounds exhibit a spectrum of complexity and mostly include extensive soft tissue trauma complicated by burns, foreign bodies, fractures and/or tissue loss. Since the clinician often faces situations with a remarkable tissue loss, dental implants are crucial to secure retention of the prosthetic appliances. Meanwhile, it is well known that dental implants enhance patient satisfaction and quality of life[6], provide improved retention and stability and enhanced chewing function and have the potential to preserve substantial bone[7-9].
The aim of this study was to report the treatment outcome of patients up to 4 years after reconstruction of oral and maxillofacial defects with a dental implant supported prosthesis and focus on prosthetic aspects, implant survival/success, patient satisfaction and quality of life.
Fifty-eight implants placed in 16 patients with maxillofacial defects caused either by trauma, such as firearm injuries or accidents, or tumor resections of oral cancers at a university clinic between June 2007 and June 2011 were included in the present study. Informed written consent with regard to treatment and measurement procedures was given by all patients and approval from the university ethics commission was duly obtained. All the implants came from one manufacturer (Straumann®, Basel, Switzerland) and were placed by the same oral and maxillofacial surgeon.
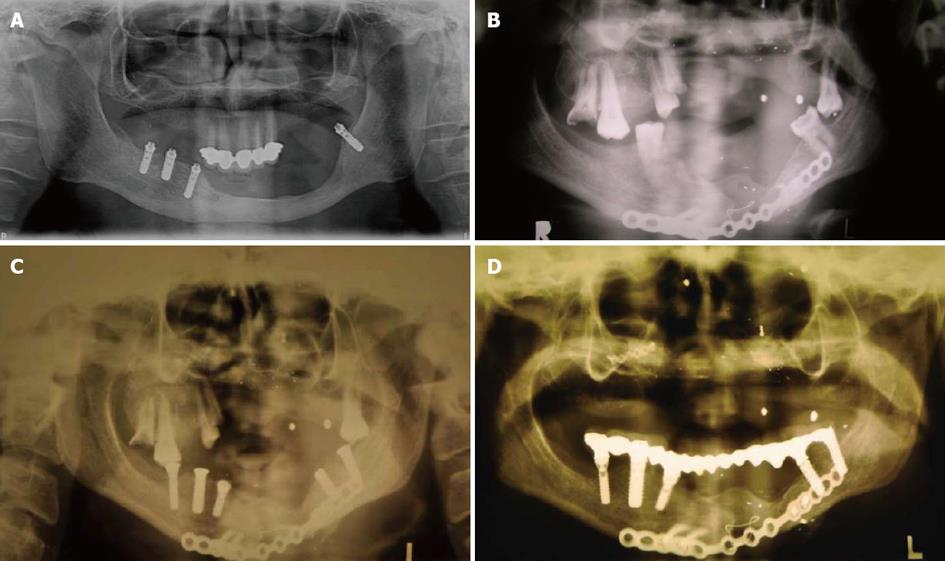
All the patients suffered from alterations of the oral cavity (Table 1). Seven out of 16 patients (6 male, 1 female) had limitations in jaw opening (microstomia). The alterations were due to firearm injuries (3 patients: 2 male, 1 female) or ablative tumor surgery (13 patients: 8 male, 5 female) (Figures 1A-C). The details of the patients are presented in Table 1. For the patients with firearm injuries (n = 3; Figure 2A and B), the implant treatments were performed 1 year after reconstructive surgeries for the patients with firearm injuries and 2 years after the radiotherapy and/or chemotherapy for the patients who had undergone ablative tumor surgeries.
| Patients (n) | 16 |
| Implants (n) | 58 |
| Patient age (mean, yr) | 39 |
| Patient gender | 10 female, 6 male |
| Type of injury | firearm injuries (3 patients; 2 male, 1 female) or ablative tumor surgery (13 patients; 8 male, 5 female) |
| Insertion time of the implants | 1 year after reconstructive surgeries for firearm injuries (n = 3) 2 years later for the patients who have undergone ablative tumor surgery (n = 13) |
| Loading time of the implants | 3 mo after insertion for lower jaw and 6 mo after insertion for upper jaw for every patient |
| Location of implants | 41 in the mandible, 17 in the maxilla |
| Type of prosthesis | 8 patients received fixed prosthesis, 6 patients received overdentures, 2 patients received both |
Surgery was performed as recommended by the manufacturer, using a one-stage surgical protocol in 10 patients (Figure 1D) and a two-stage surgical protocol in 6 patients. In all of the patients, large bony reconstructions were carried out by using free monocortico-cancellous iliac bone grafts or vascularized tissue flaps.
Prosthetic treatment of the defect patients was performed by 2 prosthodontists with 10 years of clinical experience. After implant surgery, 3 mo for the lower jaw and 6 mo for the upper jaw, osseointegration was waited for and then 8 patients received an implant supported fixed prosthesis (Figures 1E and 2A); six received implant supported overdentures (Figure 1B) and 2 received both (Table 1). The chosen prosthetic superstructures of the patients are presented in Table 1.
All participants received digital (Morita Veraview IC5®, J Morita MFG Corp, Kyoto, Japan) or analog panoramic radiographs (Planmeca®, Proline XC, Helsinki, Finland) using the imaging equipment before the surgery for treatment planning, immediately after and every year after loading of the implants for the evaluation of marginal bone levels of the implants.
Recalls were routinely performed 12, 24, 36 and 48 mo after loading. At each recall session, a clinical examination was performed by the same examiner. Implant success and survival rates were determined based on the following criteria: implants fulfilling all of the following criteria were regarded as successful[10]: no pain or tenderness upon function; 0 mobility (checked by manual manipulation); < 2 mm radiographic bone loss from initial surgery; no exudate history.
Implants with at least one of the following criteria but with no mobility (checked by manual manipulation) were regarded as surviving but not successful[10]: may have sensitivity on function; radiographic bone loss > 2 mm but less than 1/2 of implant body; may have exudate history.
Panoramic radiographs were taken preoperatively (Figure 2B), immediately after surgery (Figure 2C), immediately after loading (Figure 2D) and at every recall session. In cases of insufficient quality, intraoral radiographs were taken as well. Mesial and distal marginal bone levels of all implants were determined at baseline and recall evaluations. The analog panoramic radiographs were scanned and digitized (Epson 1680 Pro®, Seiko Epson Cooperation, Nagano, Japan). Measurements were obtained from images of successive radiographs, which were analyzed at X20 magnification with the use of a software program (CorelDraw 11.0®, Corel Corp and Coral Ltd, Ottawa, Canada).
The known diameter of the implant at the collar region according to the manufacturer’s dimensions of the respective implants was used as a reference point [11]. The distance from the supracrestal widest part of the implant to the crestal bone level was measured on the magnified images. To account for variability, the implant dimension (width) was measured and compared with the documentation dimensions; ratios were calculated to adjust for distortion. Bone levels were determined by applying a distortion coefficient (true bone height is equal to true implant width multiplied by bone height as measured on the radiograph, which is then divided by the implant diameter measured on the radiograph). The actual bone level measurement was performed independently by 2 examiners (a prosthodontist and an oral and maxillofacial surgeon) who were calibrated before the study.
The average from the 2 examiner calculations was used as the marginal bone level value. The level at which the marginal bone seemed to be attached was assessed by visual evaluation at the distal and mesial surfaces of all implants.
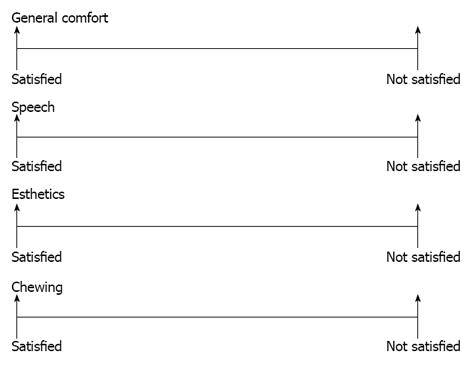
Subjects were asked to grade their oral health satisfaction after treatment on a 0-100 mm visual analog scale (VAS) for 4 separate factors: general comfort, speech, esthetics and chewing (Figure 3). The scales were anchored by the extremes of potential responses (e.g., completely satisfied-completely dissatisfied: the higher the score, the more satisfied the subject).
For the determination of quality of life of the patients, all subjects were asked to complete the Turkish version of the short-form Oral Health Impact Profile (OHIP-14), which has previously been determined to be valid and reliable[12]. Subjects rated each of the 14 items on a 5-point Likert scale from 0 = “never” to 4 = “very often”. Items were added up to yield the total score. Achievable OHIP-14 score ranged from 0-56, with lower scores representing higher oral health-related quality of life[13].
Five implants (3 in the mandible, 2 in the maxilla) in five patients were lost, while the other 53 survived, which brings an overall survival rate of 91.37% on the implant basis and 68.75% on a patient basis. Out of the 53 surviving implants, 48 were regarded as successful according to the criteria proposed by Misch et al[10] and thus the success rate was calculated as 82.75%. All the failed implants were lost before abutment connection and therefore regarded as early failures [14]. For all failed implants, new implants were placed after a 2 mo period and the planning was maintained.
The mean marginal bone loss (MBL) was 1.4 mm on the mesial side and 1.6 mm on the distal side of the implants. 5 of the implants showed MBL > 2 mm (mean MBL = 2.3 mm) but less than 1/2 of implant bodies and were therefore regarded as not successful but surviving implants.
The MBL on the distal and mesial aspects of the implants up to 48 mo following loading did not exceed 2 mm on average.
In two cases using fixed-detachable (hybrid type) restorations, excessive soft tissue under the prosthesis were observed at the 12 month recall appointment. For treatment, the hybrid dentures were unscrewed and removed and the large hyperplasic tissues were surgically excised. In order not to cause further trauma, the borders of the denture bases were adequately shortened in these areas and a week after surgical intervention, hybrid dentures were screwed to the abutments and tightened with the appropriate torque wrenches.
During the observation period of up to 48 mo, the following prosthetic complications occurred: 1 fracture of a mandibular hybrid denture; 1 fracture of an abutment screw of a locator abutment; 1 fracture of the male part of a ball abutment; the requirement of rebasing in two overdentures (1 in the maxilla, 1 in the mandible); chipping of the veneering of a hybrid denture; and the requirement of substitution of the retention mechanism of 2 overdentures after an average service period of 21 mo (9-28 mo).
All prosthetic complications were eliminated and repaired; the fractured mandibular hybrid denture was redone on a new impression and model. Two overdentures were relined and the two fractured abutments were replaced. The chipped part of the hybrid denture was repaired and the retention mechanisms of the overdentures were replaced.
Patient satisfaction scores were as follows: VAS General Comfort mean score = 85.07 out of 100; VAS Speech mean score = 75.25 out of 100; VAS Esthetics mean score = 82.74 out of 100. No patient reported low scores (score lower than 50) of satisfaction in any of the evaluated factors. The mean of OHIP-14 scores was 5.5. The OHIP-14 total and the 7 domain scores of the patients are presented in Table 2.
| OHIP total | 5.5 (range 0-56) |
| Functional limitation | 0.31(range 0-8) |
| Physical pain | 1.56 (range 0-8) |
| Psychological discomfort | 1.37 (range 0-8) |
| Physical disability | 1.06 (range 0-8) |
| Psychological disability | 0.56 (range 0-8) |
| Social disability | 0.18 (range 0-8) |
| Handicap | 0.25 (range 0-8) |
Implant-supported prostheses for maxillofacial defect patients have become a reliable treatment modality[1,2]. It may be expected that in this kind of patients, implant failures increase since the conditions are tougher compared to conventionally placed and loaded dental implants. Often the implants are facing situations such as altered anatomy, xerostomia, missing attached gingiva around the implant neck or inconvenient bone[15-17]. It should be pointed out that maintenance of daily hygiene is very important for these patients, especially for patients suffering from xerostomia. With the absence or presence of small amounts of saliva, the oral cavity becomes more prone to oral infections; thus, the risk of implant failures may rise. As shown in one of our cases, the long edentulous span, which cannot be covered by a denture base because of grafted skin covering the reconstruction, had to be restored with a hybrid denture supported by a few implants (Figure 1C-E). Additionally, missing attached gingiva is known to be a disadvantageous condition for peri-implant health. In the present clinical study, the implant survival rate and success was lower compared to implants in conventional sites. In spite of a higher implant failure rate, this treatment gradually became a well-accepted option in the therapeutic spectrum of oral and maxillofacial deformities[18,19]. In spite of the improper implant positions in several cases, a success rate of 82.75% was obtained. Due to the need of malpositioning of the implants in the remaining tissue support, it could be expected that the survival and success rate of these implants would be impaired. There are studies reporting that implants had comparable success rates when they are placed angled or malpositioned[20]. The implant success and survival rates in the present study showed similarities to the studies illustrating the successful use of osseointegrated implants in the reconstruction of traumatic craniomaxillofacial injuries and in the rehabilitation of oral function in head and neck cancer patients[5,21-23]. However, the present study showed a higher rate of implant failure, peri-implant soft tissue complications and marginal bone loss than studies showing the implant data of patients without maxillofacial defects[6,8,11-14]. On the basis of clinical observations, bone loss ranging between 1 and 2.6 mm has been reported to occur around the margin of successfully osseointegrated dental implants[24,25]. In spite of a lack of consensus, the values generally accepted as a reasonable guideline for bone loss since the late 1980s is 1.5 mm for the first year after loading the implants and 0.2 mm of additional loss for each following year[10,26].
Regarding this guideline, the marginal bone loss rate reported here in the present study could be accepted as successful in spite of unfavorable conditions. On the other hand, it should be noted that the marginal bone loss rate presented in more recent studies lies much lower. The minimization of crestal bone loss was explained by surface roughness, evaluated as one of the key factors[27]. Nevertheless, the patients’ clear judgment in favor of dental implant supported prosthetic rehabilitation in this study, which encourages this treatment modality. In the present study, a high level of patient satisfaction and quality of life were achieved (Table 2). The obtained VAS and quality of life scores in this pilot study show similarities to the study of Schoen et al[21] which investigated the patient satisfaction and quality of life outcome of implant treatment in head and neck cancer patients[1]. Additionally, our results are comparable to other studies concerning treatment with dental implants[6,8,28-30].
In the present study, the patients were not asked to complete the VAS and OHIP-14 questionnaires before the treatment; thus, it was not possible to compare the pre and post treatment scores, which may be regarded as a limitation. All the patients were unable to function with the pre-treatment oral conditions; therefore, the authors did not consider it necessary and moral to constrain the patients in completing the questionnaires before treatment. Additionally, in the opinion of the authors, the OHIP-14 questionnaire is very hard to comprehend and could cause misleading results in these patients. The form could be modified for patients with maxillofacial defects just like the previously made modification for edentulous patients as OHIP-EDENT[31].
Early management of injured patients must focus on the basics of resuscitation. The secondary target in the treatment of these cases, however, should focus on tissue preservation, abstaining from unnecessary tissue resection, because the placement of dental implants can be problematic from time to time. The attention paid at the early stage of intervention can have an important impact on the quality of life of patients.
As a general approach at the dental school, the implant treatment has to be postponed for a certain period if a major resection and reconstruction has been performed. If radiotherapy and/or chemotherapy is administered, the patient has to wait at least 2 years for the implantation, as suggested previously[5]. The prosthetic complications recorded in the present study were slightly over the average of prosthetic patients treated in the related university clinic. Although complications, such as requirement of rebasing, chipping of veneering material and substitution of retention mechanism, are routinely encountered and well documented in the literature[32], the fracture of a hybrid denture, a locator abutment or of the male part of a ball attachment is not common. The misalignment or strategically disadvantageous numbers and positions of implants may be a factor that explains higher rates of complications in the present patient group.
Oral rehabilitation becomes even more complicated with the presence of microstomia[33], which can be encountered in this kind of patients. Microstomic patients experience considerable limitation in jaw opening and overall jaw mobility. This limitation in the oral opening makes gaining access to the oral cavity difficult, depending on the severity of microstomia. Therefore, traditional approaches for dental restoration should be modified to accommodate microstomia. Various treatment approaches have been proposed for microstomic patients, with or without endosseous implants. Reduced mouth opening may prevent instruments from safely entering the mouth for insertion of the implants. This is a critical factor in determining whether implant treatment can be provided and in deciding the number of inserts needed and the best places for insertion[34].
In the present study, 3 patients had a limited intraoral access, requiring modification of the approach. Also, there might be problems with the precision of dental laboratory work because of the inaccurate impressions which were hardly made with the modification methods[33]. Therefore, the precision of fit of the dental frameworks were very limited (Figure 2D). The strains due to the misfit of the denture can be a reason for the failures and prosthetic complications. In cases of firearm injuries, the severity of the defect resulting from facial firearm injuries varies according to the caliber of the weapon used, the distance from which the patient is shot and the part of the body involved[35]. Close range, high velocity firearm wounds can result in devastating functional and esthetic consequences. Maxillofacial traumas are mostly encountered in males (78%) and at a higher rate between the ages of 20-39 years. There are many reasons for maxillofacial trauma, such as fighting (48.2%), falling (26.2%), car accidents (4.2%) and firearm injury (1.2%)[36,37]. The epidemiology of facial fractures varies in type, severity and cause, depending on the population studied[38]. The differences between populations in the causes of maxillofacial fractures may be the result of risk factors and cultural differences between countries but are more likely to be influenced by the injury severity[39].
In situations with insufficient bone volume, invasive surgical procedures such as maxillary sinus floor elevation or the zygomatic implant placement[19], procedures mainly accomplished by maxillofacial surgeons, can be an alternative. However, individuals of the related patient group could appeal against additional complex surgical interventions after the long and griping procedures they have endured.
Meanwhile, it is a well known fact that the first year is critical for implant failure and for the largest portion of marginal bone loss around dental implants[34]. The results of an investigation showed that practically all implant losses occurred during the first 2 years, whereupon a steady state seemed to follow for up to 5 years after loading[40].
Despite disadvantageous loading conditions and poor bone quality and quantity, all the presented cases showed a stable situation around the implants after a period of 12-48 mo of loading time. Although further follow up and larger case numbers will give more information about the success of dental implants as a treatment modality in maxillofacial defect patients, the actual results are encouraging and can be recommended for similar cases. Even although the success and survival rate is slightly lower than conventionally loaded implants due to tougher conditions, dental implants seem to be a valuable aid in the maintenance of comfortable rehabilitation of maxillofacial defect patients.
In patients with maxillofacial defects, implant failures may increase, since the conditions are harder compared to conventionally placed dental implants. Often the implants are facing situations such as altered anatomy, xerostomia, missing attached gingiva around the implant neck or inconvenient bone.
The treatment outcome of patients with maxillofacial defects up to 4 years after dental implant supported prosthesis should be investigated and prosthetic aspects, implant survival/success, patient satisfaction and quality of life of these patients should be demonstrated. In this study, the authors show that dental implants seem to be a valuable aid in the maintenance of comfortable rehabilitation of maxillofacial defect patients.
Studies of patients with maxillofacial defects are mostly case reports. This is one of the first studies to report the outcome of dental implant treatment in these patients.
The actual results are encouraging and dental implant treatment can be recommended for similar cases.
The authors examined the prosthetic and peri-implant complications, patient satisfaction, marginal bone loss and success and survival of implants in patients with maxillofacial defects. The obtained positive results will be a valuable guide for clinicians facing the same difficulties in patients.
| 1. | Esser E, Wagner W. Dental implants following radical oral cancer surgery and adjuvant radiotherapy. Int J Oral Maxillofac Implants. 1997;12:552-557. [PubMed] |
| 2. | Cheng AC, Wee AG, Shiu-Yin C, Tat-Keung L. Prosthodontic management of limited oral access after ablative tumor surgery: a clinical report. J Prosthet Dent. 2000;84:269-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Schliephake H, Jamil MU. Prospective evaluation of quality of life after oncologic surgery for oral cancer. Int J Oral Maxillofac Surg. 2002;31:427-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 111] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 4. | Eckert SE, Desjardins RP, Keller EE, Tolman DE. Endosseous implants in an irradiated tissue bed. J Prosthet Dent. 1996;76:45-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 46] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Visch LL, van Waas MA, Schmitz PI, Levendag PC. A clinical evaluation of implants in irradiated oral cancer patients. J Dent Res. 2002;81:856-859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 108] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 6. | Geckili O, Bilhan H, Bilgin T. Impact of mandibular two-implant retained overdentures on life quality in a group of elderly Turkish edentulous patients. Arch Gerontol Geriatr. 2011;53:233-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Rad AS, Siadat H, Monzavi A, Mangoli AA. Full mouth rehabilitation of a hypohidrotic ectodermal dysplasia patient with dental implants: a clinical report. J Prosthodont. 2007;16:209-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Bakke M, Holm B, Gotfredsen K. Masticatory function and patient satisfaction with implant-supported mandibular overdentures: a prospective 5-year study. Int J Prosthodont. 2002;15:575-581. [PubMed] |
| 9. | Doundoulakis JH, Eckert SE, Lindquist CC, Jeffcoat MK. The implant-supported overdenture as an alternative to the complete mandibular denture. J Am Dent Assoc. 2003;134:1455-1458. [PubMed] |
| 10. | Misch CE, Perel ML, Wang HL, Sammartino G, Galindo-Moreno P, Trisi P, Steigmann M, Rebaudi A, Palti A, Pikos MA. Implant success, survival, and failure: the International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant Dent. 2008;17:5-15. [PubMed] |
| 11. | Geckili O, Bilhan H, Mumcu E, Bilgin T. Three-year radiologic follow-up of marginal bone loss around titanium dioxide grit-blasted dental implants with and without fluoride treatment. Int J Oral Maxillofac Implants. 2011;26:319-324. [PubMed] |
| 12. | Mumcu G, Inanc N, Ergun T, Ikiz K, Gunes M, Islek U, Yavuz S, Sur H, Atalay T, Direskeneli H. Oral health related quality of life is affected by disease activity in Behçet’s disease. Oral Dis. 2006;12:145-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 100] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 13. | Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1351] [Cited by in RCA: 1658] [Article Influence: 57.2] [Reference Citation Analysis (0)] |
| 14. | Esposito M, Hirsch JM, Lekholm U, Thomsen P. Biological factors contributing to failures of osseointegrated oral implants. (I). Success criteria and epidemiology. Eur J Oral Sci. 1998;106:527-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 787] [Cited by in RCA: 772] [Article Influence: 27.6] [Reference Citation Analysis (0)] |
| 15. | Aghabeigi B, Bousdras VA. Rehabilitation of severe maxillary atrophy with zygomatic implants. Clinical report of four cases. Br Dent J. 2007;202:669-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Widmark G, Andersson B, Andrup B, Carlsson GE, Ivanoff CJ, Lindvall AM. Rehabilitation of patients with severely resorbed maxillae by means of implants with or without bone grafts. A 1-year follow-up study. Int J Oral Maxillofac Implants. 1998;13:474-482. [PubMed] |
| 17. | Duyck J, Van Oosterwyck H, Vander Sloten J, De Cooman M, Puers R, Naert I. In vivo forces on oral implants supporting a mandibular overdenture: the influence of attachment system. Clin Oral Investig. 1999;3:201-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Tang JA, Rieger JM, Wolfaardt JF. A review of functional outcomes related to prosthetic treatment after maxillary and mandibular reconstruction in patients with head and neck cancer. Int J Prosthodont. 2008;21:337-354. [PubMed] |
| 19. | Schoen PJ, Reintsema H, Raghoebar GM, Vissink A, Roodenburg JL. The use of implant retained mandibular prostheses in the oral rehabilitation of head and neck cancer patients. A review and rationale for treatment planning. Oral Oncol. 2004;40:862-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 67] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 20. | Bilhan H. An alternative method to treat a case with severe maxillary atrophy by the use of angled implants instead of complicated augmentation procedures: a case report. J Oral Implantol. 2008;34:47-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Schoen PJ, Raghoebar GM, Bouma J, Reintsema H, Vissink A, Sterk W, Roodenburg JL. Rehabilitation of oral function in head and neck cancer patients after radiotherapy with implant-retained dentures: effects of hyperbaric oxygen therapy. Oral Oncol. 2007;43:379-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 105] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 22. | McGhee MA, Stern SJ, Callan D, Shewmake K, Smith T. Osseointegrated implants in the head and neck cancer patient. Head Neck. 1997;19:659-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 23. | Roumanas ED, Markowitz BL, Lorant JA, Calcaterra TC, Jones NF, Beumer J. Reconstructed mandibular defects: fibula free flaps and osseointegrated implants. Plast Reconstr Surg. 1997;99:356-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 87] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 24. | Lekholm U, Gunne J, Henry P, Higuchi K, Lindén U, Bergström C, van Steenberghe D. Survival of the Brånemark implant in partially edentulous jaws: a 10-year prospective multicenter study. Int J Oral Maxillofac Implants. 1999;14:639-645. [PubMed] |
| 25. | Weber HP, Crohin CC, Fiorellini JP. A 5-year prospective clinical and radiographic study of non-submerged dental implants. Clin Oral Implants Res. 2000;11:144-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 80] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 26. | Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11-25. [PubMed] |
| 27. | Wiskott HW, Belser UC. Lack of integration of smooth titanium surfaces: a working hypothesis based on strains generated in the surrounding bone. Clin Oral Implants Res. 1999;10:429-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 136] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 28. | Pavel K, Seydlova M, Dostalova T, Zdenek V, Chleborad K, Jana Z, Feberova J, Radek H. Dental implants and improvement of oral health-related quality of life. Community Dent Oral Epidemiol. 2012;40 Suppl 1:65-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 29. | Borges Tde F, Mendes FA, de Oliveira TR, Gomes VL, do Prado CJ, das Neves FD. Mandibular overdentures with immediate loading: satisfaction and quality of life. Int J Prosthodont. 2011;24:534-539. [PubMed] |
| 30. | Geckili O, Bilhan H, Mumcu E. Clinical and radiographic evaluation of three-implant-retained mandibular overdentures: a 3-year retrospective study. Quintessence Int. 2011;42:721-728. [PubMed] |
| 31. | Allen F, Locker D. A modified short version of the oral health impact profile for assessing health-related quality of life in edentulous adults. Int J Prosthodont. 2002;15:446-450. [PubMed] |
| 32. | Bilhan H, Geckili O, Mumcu E, Bilmenoglu C. Maintenance requirements associated with mandibular implant overdentures: clinical results after first year of service. J Oral Implantol. 2011;37:697-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 33. | Geckili O, Cilingir A, Bilgin T. Impression procedures and construction of a sectional denture for a patient with microstomia: a clinical report. J Prosthet Dent. 2006;96:387-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 34. | Garnett MJ, Nohl FS, Barclay SC. Management of patients with reduced oral aperture and mandibular hypomobility (trismus) and implications for operative dentistry. Br Dent J. 2008;204:125-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 35. | Lucena JS, Romero C. Retrograde transthoracic venous bullet embolism. Report of a case following a single gunshot with multiple wounds in the left arm and chest. Forensic Sci Int. 2002;125:269-272. [PubMed] |
| 36. | Wulkan M, Parreira JG, Botter DA. [Epidemiology of facial trauma]. Rev Assoc Med Bras. 2005;51:290-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 37. | Yuksel F, Celikoz B, Ergun O, Peker F, Açikel C, Ebrinc S. Management of maxillofacial problems in self-inflicted rifle wounds. Ann Plast Surg. 2004;53:111-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 38. | Haug RH, Prather J, Indresano AT. An epidemiologic survey of facial fractures and concomitant injuries. J Oral Maxillofac Surg. 1990;48:926-932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 282] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 39. | Gassner R, Tuli T, Hächl O, Rudisch A, Ulmer H. Cranio-maxillofacial trauma: a 10 year review of 9,543 cases with 21,067 injuries. J Craniomaxillofac Surg. 2003;31:51-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 496] [Cited by in RCA: 490] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 40. | Widmark G, Andersson B, Carlsson GE, Lindvall AM, Ivanoff CJ. Rehabilitation of patients with severely resorbed maxillae by means of implants with or without bone grafts: a 3- to 5-year follow-up clinical report. Int J Oral Maxillofac Implants. 2001;16:73-79. [PubMed] |
P- Reviewers Enkling N, Mishra AK, Patil P S- Editor Gou SX L- Editor Roemmele A E- Editor Lu YJ