Published online Nov 6, 2013. doi: 10.5315/wjh.v2.i4.115
Revised: August 14, 2013
Accepted: August 28, 2013
Published online: November 6, 2013
Processing time: 209 Days and 13.8 Hours
We report a case of a 59-year-old gentleman who had suffered from low back pain for several months. Abdominal sonogram showed multiple heteroechoic nodules in the bilateral liver and an enlarged pancreatic head. Abdominal computer tomography (CT) favored pancreas head tumor with liver and bone metastasis. Endoscopic retrograde cholangiopancreatography (ERCP) disclosed pancreatic duct invasion over the distal portion of the pancreatic duct with prestenotic dilatation. Liver biopsy showed undifferentiated carcinoma. As suggested by the pathologist, the nasopharyngeal area was checked by the ear, nose and throat doctor, was negative and nasopharyngeal carcinoma was excluded. Therefore, the patient was treated with Gemcitabine (1500 mg/wk), as the suggested treatment schedule, for 24 wk in opioid dependency program. Sequential abdominal CT during follow up showed the disappearance of liver metastasis and shrinkage of the pancreatic tumor. Repeated ERCP after treatment showed re-channelization of the pancreatic duct. During 11 years of follow up, 5 CT scans disclosed not only the disappearance of the hepatic tumor but also no cancer recurrence. Progressive shrinkage of pancreatic head was also noted. Therefore, we can say this malignant case was cured by monotherapy with gemcitabine.
- Citation: Yang CC, Chow WK, Peng YC, Wang RC. Gemcitabine cures metastatic hepatic carcinoma and bone metastasis. World J Hematol 2013; 2(4): 115-118
- URL: https://www.wjgnet.com/2218-6204/full/v2/i4/115.htm
- DOI: https://dx.doi.org/10.5315/wjh.v2.i4.115
Gemcitabine is a nucleoside analog with a structural similarity to cytarabine. Initially, it has a low objective response rate of around 6%-11% in chemotherapy-naive patients with pancreas cancer who are given the single agent gemcitabine (800 mg/m2 IV weekly for 3 of every 4 wk)[1].
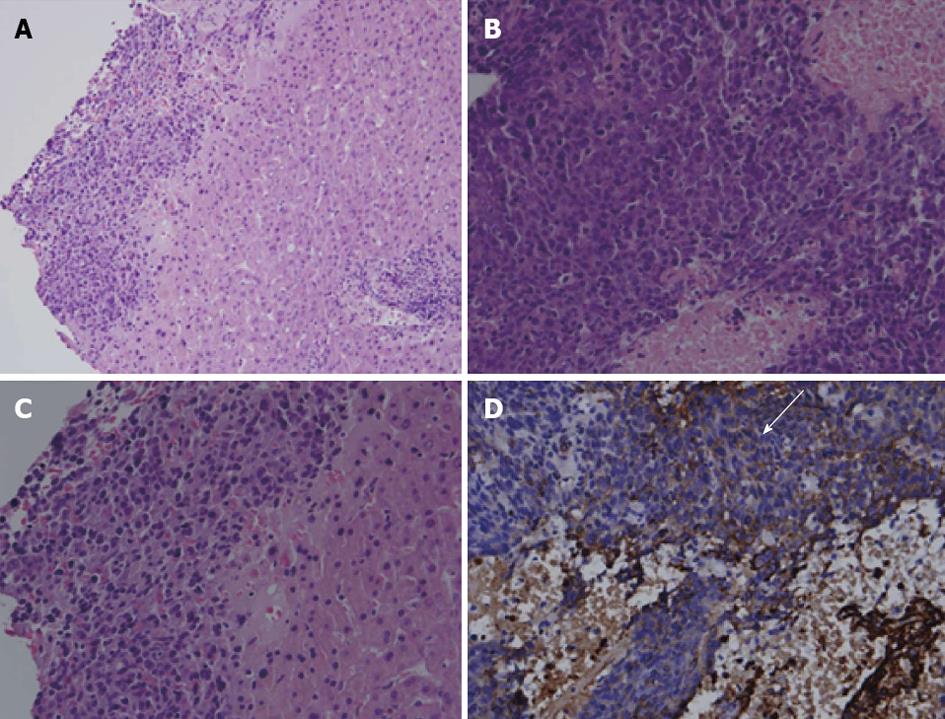
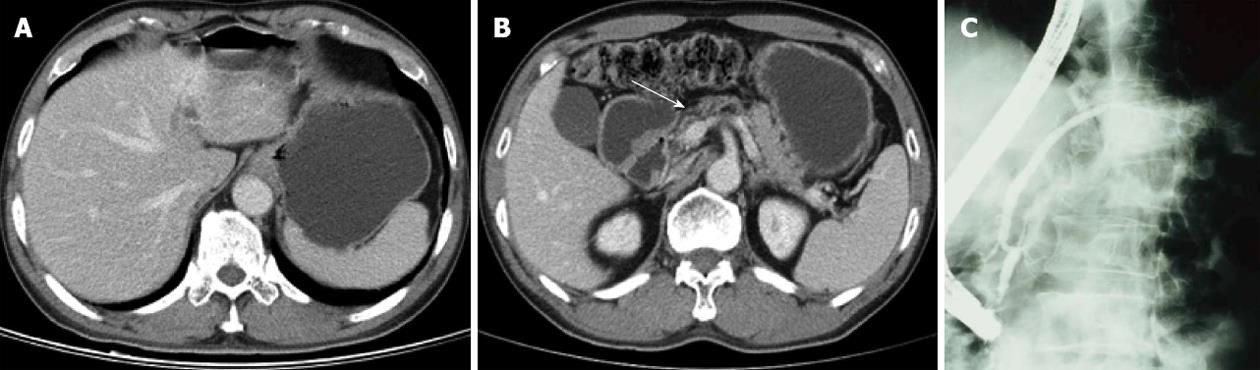
In 1999, a 59-year-old gentleman was referred from another hospital due to an unknown malignancy with liver and bone metastasis. He suffered from lower back pain and loss of body weight, about 10 kg within 3 mo. There was no familial history of malignancy. Physical examination showed pale conjunctiva, knocking pain over the lumbar spine and a mass lesion over the right sternoclavicular junction. The laboratory data showed only normocytic anemia and the hemoglobin was 10.4 mg/dL. The tumor markers, such as carcinoembryonic antigen and CA 19-9, were within normal limits. Abdominal sonogram showed many heterogeneous isoechoic tumors in bilateral lobes of the liver with enlargement of the pancreas head. Abdominal computed tomography (CT) showed suspicion of pancreas head cancer with liver and L3 metastasis (Figure 1A and B). The bone scan showed suspicion of metastasis over the right sternoclavicular area, L-spine and ischium. Liver biopsy was done. The pathologist reported undifferentiated carcinoma (Figure 2) because of the focally weakly positive result with cytokeratin AE1/AE3, a sole marker of the epithelial differential, and a nasopharyngeal check-up to rule out the possibility of nasopharyngeal carcinoma was suggested. The ear, nose and throat (ENT) doctor disclosed a smooth nasopharyngeal mucosa and biopsy showed no malignancy. Endoscopic retrograde cholangiopancreatography (ERCP) showed focal irregular stenosis, favoring tumor invasion over the pancreatic duct (Figure 1C). Clinically, pancreas cancer with liver and bone metastasis was highly likely.
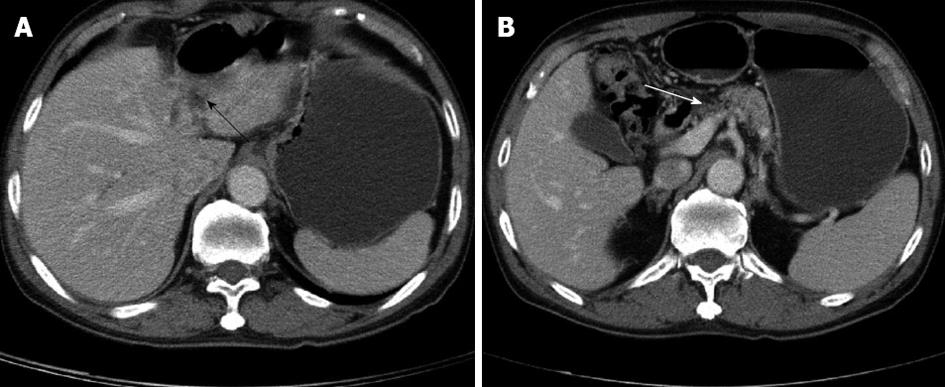
The patient was treated with monotherapy of gemcitabine 1500 mg/wk in GI-OPD. The dose was 1000 mg/m2 body surface area and medication was infused in 30 min. The patient received gemcitabine every week for the first 7 wk and then rested for 1 wk. Thereafter, he received treatment weekly for 3 wk and then rested for 1 wk. In total, the patient received 19 doses within 24 wk. Throughout, the patient tolerated the treatment well and blood transfusion was not necessary. Repeat CT scan showed disappearance of the liver mass (Figure 3A) and shrinkage of the pancreatic head (Figure 3B). Repeat ERCP showed re-channelization of the pancreatic duct (Figure 3C). The mass over the right sternoclavicular joint became softer and smaller gradually. Lumbago improved gradually during gemcitabine therapy and finally vanished after the treatment course. In the following 11 years, 5 CT scans showed progressive shrinkage of the left lobe of the liver (Figure 4A) and pancreatic head (Figure 4B). No cancer recurrence was noted. Also, repeat CA19-9 was normal. In 2010, 11 years after treatment, the patient had senile dementia but was still cancer free. Therefore, we can say this patient was cured by gemcitabine.
Undifferentiated carcinoma with multiple metastasis is common, about 20%-25%, in cancer of an unknown primary site[2]. In our case, NPC was excluded by biopsy on grossly normal mucosa of the nasopharyngeal area. In clinics, the mid or lower third portion of thoracic esophageal carcinoma with intra abdominal metastasis is also common, with an incidence of around 15.0%-17.4%[3,4]. However, the gastroscope was negative too. The positive reaction with immunohistochemistry stain of AE1/AE3 was specific for carcinoma but carcinoma with pancreatic duct metastasis is very rare. Image studies of CT and ERCP, together with liver biopsy, resulted in the diagnosis of pancreas adenocarcinoma with multiple metastases.
In 1997, the study of Burris et al[5] showed that the clinical benefit and survival of gemcitabine (1000 mg/m2 weekly for 7 wk followed by 1 wk of rest, then weekly for three out of every 4 wk) was approved for first-line therapy of metastatic pancreatic cancer. However, there was no evidence to show that gemcitabine has the ability to cure advanced pancreas adenocarcinoma, even in cases with multiple organ metastases. But in our case, the liver mass disappeared and atrophy of left lobe of liver was noted in the following abdominal CT after treatment with gemcitabine. The repeated ERCP also showed the re-channelization of the irregular stenotic pancreatic duct. There was no cancer recurrence during the eleven years of follow-up. It was amazing that gemcitabine could cure metastatic liver carcinoma.
| 1. | Carmichael J, Fink U, Russell RC, Spittle MF, Harris AL, Spiessi G, Blatter J. Phase II study of gemcitabine in patients with advanced pancreatic cancer. Br J Cancer. 1996;73:101-105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 246] [Cited by in RCA: 257] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 2. | Greco FA, Hainsworth JD. Introduction: unknown primary cancer. Semin Oncol. 2009;36:6-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Chen G, Wang Z, Liu XY, Zhang MY, Liu FY. Abdominal lymph node metastasis in patients with mid thoracic esophageal squamous cell carcinoma. World J Surg. 2009;33:278-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Seto Y, Fukuda T, Yamada K, Matsubara T, Hiki N, Fukunaga T, Oyama S, Yamaguchi T, Nakajima T, Kato Y. Celiac lymph nodes: distant or regional for thoracic esophageal carcinoma? Dis Esophagus. 2008;21:704-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Burris HA, Moore MJ, Andersen J, Green MR, Rothenberg ML, Modiano MR, Cripps MC, Portenoy RK, Storniolo AM, Tarassoff P. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J Clin Oncol. 1997;15:2403-2413. [PubMed] |
P- Reviewer: Rory K S- Editor: Zhai HH L- Editor: Roemmele A E- Editor: Liu XM