Peer-review started: August 22, 2022
First decision: September 27, 2022
Revised: October 12, 2022
Accepted: November 29, 2022
Article in press: November 29, 2022
Published online: February 6, 2023
Processing time: 165 Days and 7.2 Hours
Hematidrosis is a sporadic disease, to a point where its existence is still denied up to date. It is also linked to stigmata, psychological roots, and religious beliefs, whih has strengthened clinicians' disbelief in hematidrosis.
To conduct a thorough review to classify the likelihood of hematidrosis cases.
We searched PubMed, Science Direct, Medline, and Google Scholar, as well as four different preprint databases, including Medrxiv, Research Square, SSRN, and Biorxiv. We included studies from 1996 onwards, with no limitation on language. Hematidrosis was classified as "unlikely", "likely", and "highly likely".
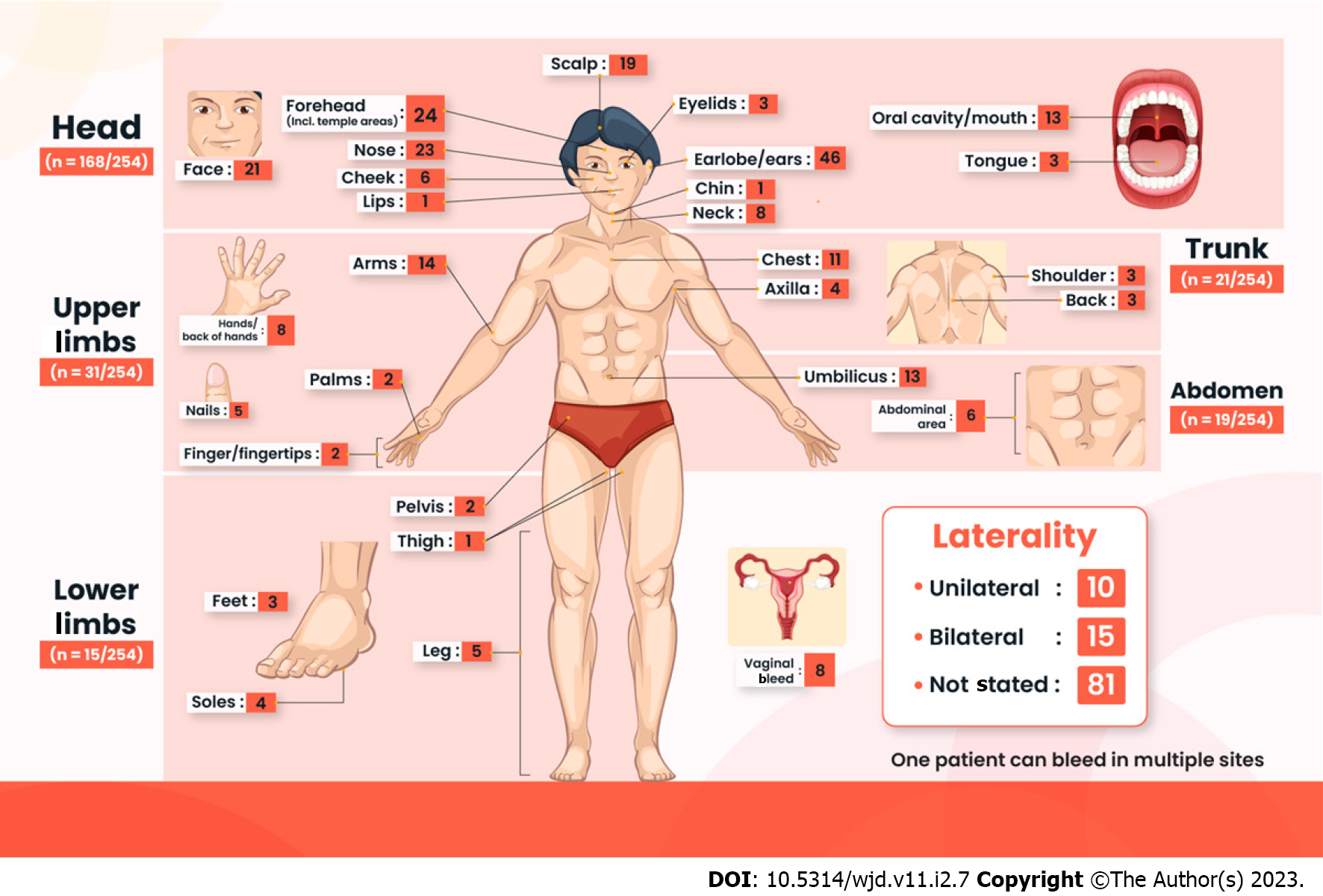
There are 74 articles with 106 hematidrosis cases. India (n = 40) and China (n = 11) report the most cases. Patients are mostly female (76.5%) with a median age of 13 years. The head region is the most common bleeding site (n = 168/254). Headaches (26.9%) and abdominal pain (16.4%) are the most common prodromes. Beta-blockers (43%) and anxiolytic (23.2%) are the most commonly prescribed pharmacotherapy. Psychotherapy (37.5%) and counseling (32.5%) are the most utilized non-pharmacotherapy measures. Only 41.1% and 19.8% of all cases reach complete resolution and are highly likely to be hematidrosis, respectively.
Although hematidrosis is rare and the pathophysiology is still largely unknown, that does not mean hematidrosis does not exist. It is important to note that the most frequent trigger factors are either anxiety, fear, or excessive stress. Clinicians need to exclude other diagnoses and search for stressors to alleviate the bleeding.
Core Tip: This is a systematic review on hematidrosis, an entity that is still mostly unknown, even to the experts. While this is not a guide to diagnose hematidrosis, this systematic review will help clinicians understand hematidrosis, the clinical pictures, the current available treatment, as well as the next steps in hematidrosis research.
- Citation: Octavius GS, Meliani F, Heriyanto RS, Yanto TA. Systematic review of hematidrosis: Time for clinicians to recognize this entity. World J Dermatol 2023; 11(2): 7-29
- URL: https://www.wjgnet.com/2218-6190/full/v11/i2/7.htm
- DOI: https://dx.doi.org/10.5314/wjd.v11.i2.7
The first case of hematidrosis dates back to the 3rd century B.C., where the first two treatizes by Aristotle contained sweat mixed with blood[1]. In the Bible, it is mentioned that these symptoms were written during Jesus Christ's sufferings in the garden of Gethsemane (Luke 22:44)[2,3]. Hematidrosis is an eccrine sweat disorder where sweat mixed with blood appear spontaneously without any visible trauma to the skin appendages. It is a diagnosis of exclusion[3]. Under International Classification of Disease 10 (ICD 10) in 2016, hematidrosis is given a diagnosis code of L74.8 under "other eccrine sweat disorders". However, this disease entity is still not widely accepted as a "true pathological disease" for various reasons[2,3].
Initially, the very existence of hematidrosis is questioned up to date. The mythical perception about hematidrosis creates a stigma where the bleeding is more related to pious beliefs than a genuine medical condition[4]. Another contributing factor is that a previous review on hematidrosis was done by Holoubek and Holoubek in 1996, encompassing 76 hematidrosis cases[5]. However, this review has been criticized for reporting the cases without laboratory confirmation[3,5]. Lastly, Favaloro & Lippi[6] mention some factors contributing to the plausible deniability of hematidrosis. Those explanations include the rarity of the disease, the possibility of Munchausen's syndrome (or Munchausen's by proxy), stress and its consequence on self-inflicted injuries, little scientific evidence that hematidrosis is an entity, and most reports are from older literature, in a foreign language, published in non-haematology journals, and there is a lack of publications in high-quality journals[6].
Several authors have attempted to conduct a literature review or systematic review on this topic[2,3,7]. However, the reviews do not present a comprehensive search, do not specify in which journals the articles were published, and more importantly, do not define what constitutes a hematidrosis. Therefore, we conduct a more thorough systematic review about hematidrosis, with a classification of the likelihood of hematidrosis cases in each journal. This review shall guide clinicians in identifying what hematidrosis is, how it presents, the necessary laboratory or radiology tests needed, as well as the treatments.
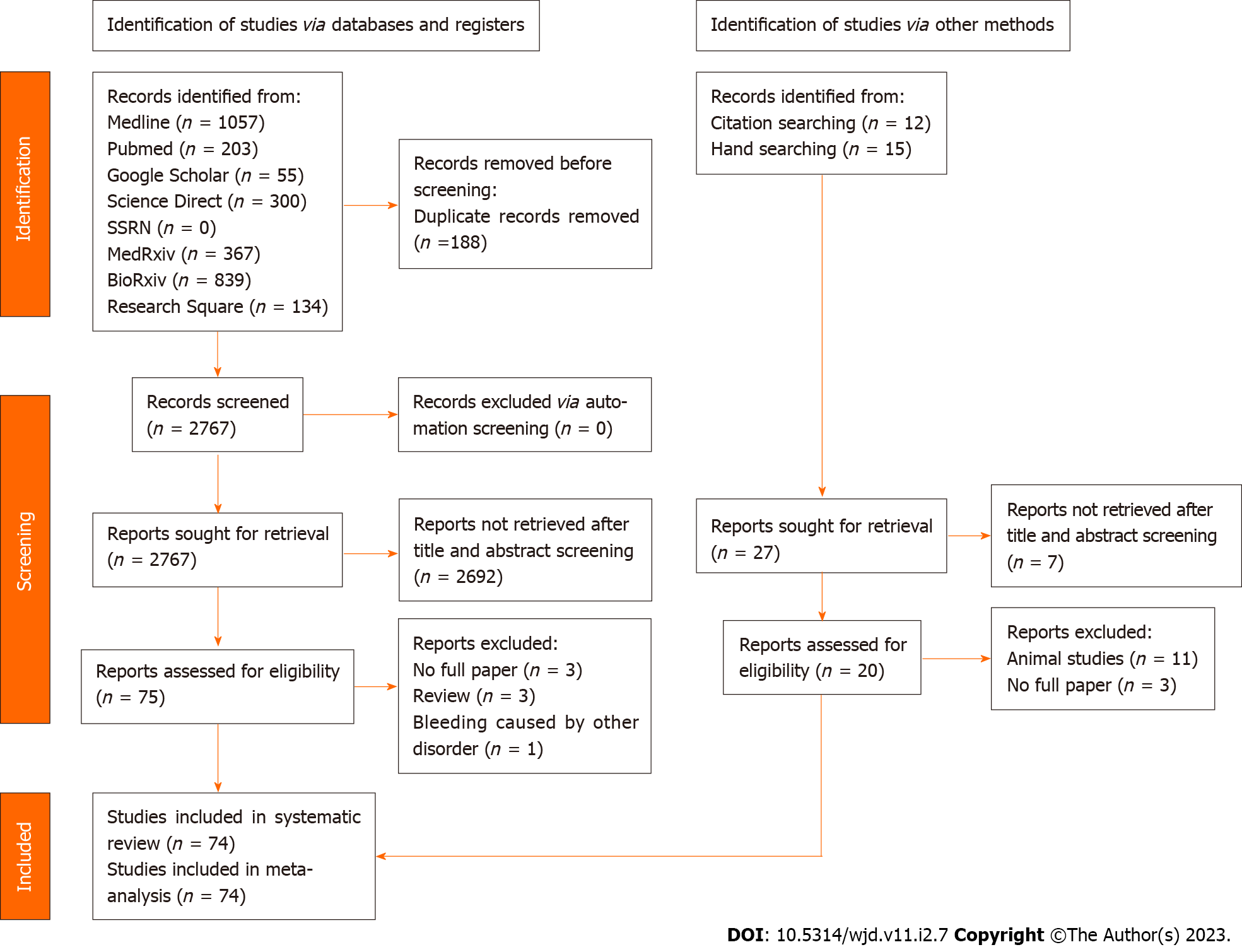
The Preferred Reporting Items for Systematic Review (PRISMA) 2020 guidance was used[8]. The protocol of this review was registered on the International Prospective Register of Systematic Reviews (PROSPERO) database with a registration number CRD42021289372.
The subjects studied were all patients diagnosed with hematidrosis without any age limitations. The diagnosis of hematidrosis is determined by the respective authors, and we classified the diagnosis as "unlikely", "likely", or "highly likely". A patient was considered to have “highly likely” hematidrosis if: (1) The bleeding episode was witnessed directly by medical professionals, (2) attempts were made to exclude other possible diagnoses, (3) skin biopsies and bleeding analysis were done and found to be normal or inconclusive, and (4) bleeding photos were included in the article; while a patient was determined to have “unlikely” hematidrosis if: (1) The bleeding episode was not witnessed by medical professionals or from family members, (2) minimal or no tests were done to exclude hematidrosis (only routine blood work was done), (3) other disorders possibly explain the bleeding, and (4) no bleeding photos were provided. Lastly, a hematidrosis case was classified as “likely” if it did not satisfy all the highly likely or unlikely criteria.
This review's inclusion criteria are any original articles published after 1996 without any restrictions in language. We restricted the year for literature search to ensure that studies that had been reviewed by Holoubek & Holoubek were not included[5]. We also included grey literature such as conference abstracts, thesis, or dissertations. The exclusion criteria of this study are reviews, opinion-based articles (letter to the editors or commentary), bleeding caused by other disorders, pure hemolacria, and animal studies. Citations from review studies were combed to ensure literature saturation. In order to guarantee that all available studies were included, we conducted citation and hand searches manually and via Research Gate.
The literature search started on December 6, 2021 and ended on the same day. We searched four different academic databases, including PubMed, Science Direct, Medline, and Google Scholar, and four different preprint databases, including Medrxiv, Research Square, SSRN, and Biorxiv. The keywords used were "hematidrosis", "hematohidrosis", and "bloody sweat". The Medical Subject Heading (MeSH) terms for each database are listed in Table 1. All records were imported into the Rayyan software, where duplicates were detected automatically and screened manually[9]. This software also allowed authors to collaborate in selecting the relevant studies. Two independent authors conducted the initial search (GSO and RSH), importing all the findings into Rayyan software. Another author (FM) cross-checked the initial searches. These three authors independently screened all available studies. Conflicts were resolved by discussion with the expert (TAY). In the case of studies with overlapping publications (abstracts later published into a full paper), we chose studies that provided more data.
| Database | Medical subject heading | Number of studies found |
| PubMed | “hematidrosis”[All Fields] OR (“haematohidrosis”[All Fields] OR “hematohidrosis”[All Fields]) OR (“bloody”[All Fields] AND (“tearings”[All Fields] OR “tears”[MeSH Terms] OR “tears”[All Fields] OR “tearing”[All Fields] OR “lacrimal apparatus diseases”[MeSH Terms] OR (“lacrimal”[All Fields] AND “apparatus”[All Fields] AND “diseases”[All Fields]) OR “lacrimal apparatus diseases”[All Fields] OR “lacerations”[MeSH Terms] OR “lacerations”[All Fields])) OR (“bloody”[All Fields] AND (“sweat”[MeSH Terms] OR “sweat”[All Fields] OR “sweating”[MeSH Terms] OR “sweating”[All Fields] OR “sweats”[All Fields] OR “sweatings”[All Fields])) OR “hemolacria”[All Fields] | 203 |
| Medline | ((hemathidrosis) OR haematohidrosis) OR bloody sweat | 1057 |
| Google Scholar | allintitle: hematidrosis OR haematohidrosis OR bloody sweat | 55 |
| Science Direct | (Hematidrosis) OR (haematohidrosis) OR (bloody sweat) | 200 |
| MedRxiv | (Hematidrosis) OR (haematohidrosis) OR (bloody sweat) | 367 |
| BioRxiv | (Hematidrosis) OR (haematohidrosis) OR (bloody sweat) | 839 |
| SSRN | (Hematidrosis) OR (haematohidrosis) OR (bloody sweat) | 0 |
| Research Square | (Hematidrosis) OR (haematohidrosis) OR (bloody sweat) | 134 |
Data extraction was carried out independently by two authors (FM and RSH), then reviewed by another author (GSO) to ensure accuracy. We extracted relevant information such as study identification (author and year of publication), study characteristics (location and article type), and patients' characteristics (number of patients, age, sex, underlying conditions, characteristics of bleeding, laboratory and radiological examinations, therapies, and outcome).
The Joanna Briggs Institute (JBI) checklist for case reports and case series were used to assess their quality, respectively[10]. Three reviewers (GSO, FM, and RSH) independently assessed the scale, and any discrepancies were sorted with the expert (TAY) until a consensus was attained. If any missing data or further data were needed, corresponding authors were contacted via an inquiry email.
To incorporate all of the data in this review, pooled descriptive tests were employed. The mean and standard deviation of data reported in median and range (or interquartile range) were calculated[11-13]. The means and standard deviations were then combined into a single value using the Cochrane method[14].
The initial search yielded 2955 articles, where 188 articles were immediately excluded as duplicates. After title and abstract screening, 2692 articles were excluded. Out of the 75 articles assessed for eligibility, three articles did not have full texts[15-17], three articles were review articles[18], one article mentioned other causes of the bleeding[19], and four articles were purely hemolacria[20-22]. These articles were then excluded, resulting in 68 articles[7,23-28]. We found another six articles through hand-searching and citation searching[29-34]. In total, there are 74 articles included in this review, with a total of 106 patients (Figure 1 and Table 1).
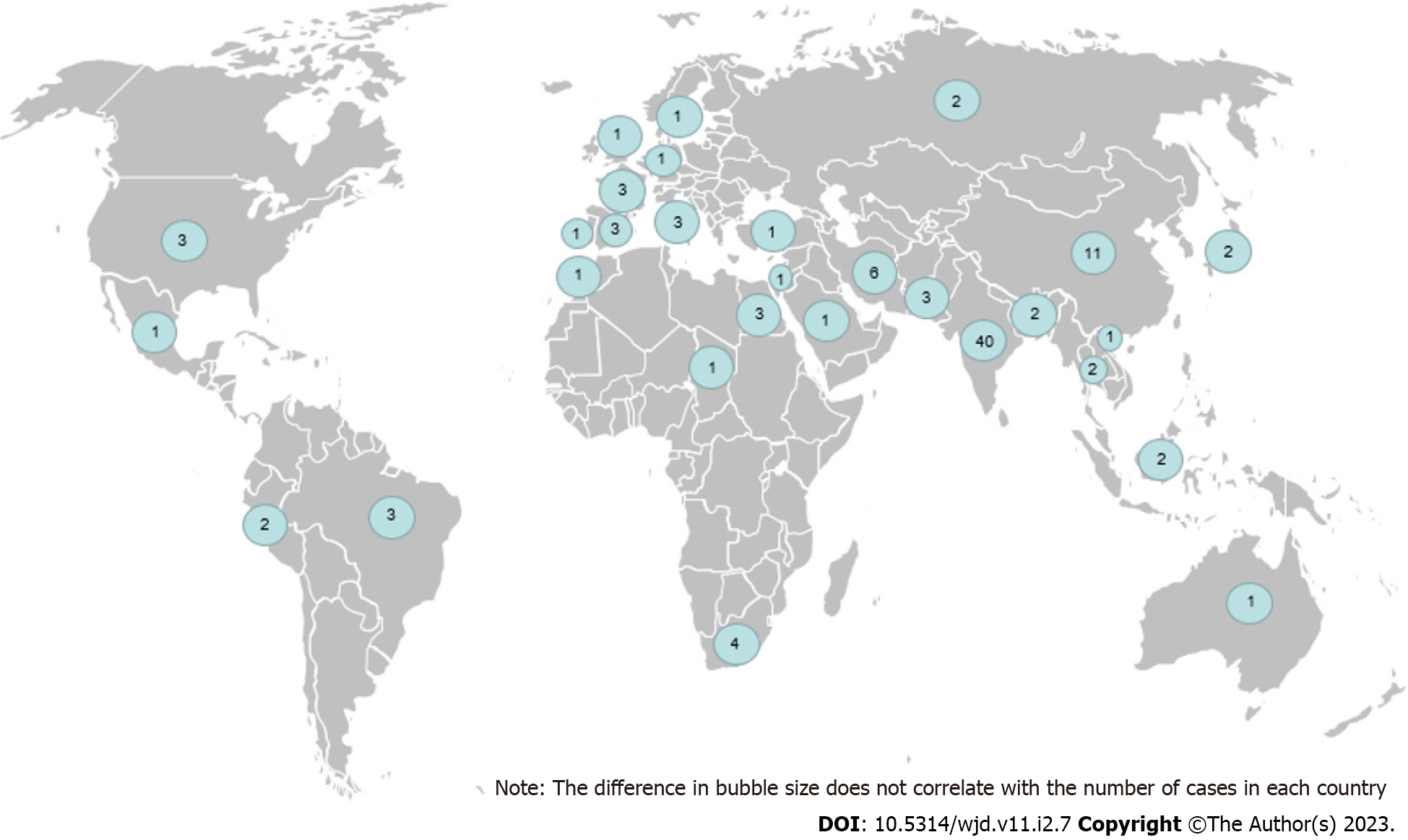
Most of the cases are heavily concentrated in Asia, particularly India (n = 40/106) and China (n = 11/106). Australia only reports one case of hematidrosis, the least among other continents (Figure 2). Patients presented with the disease as early as an hour or as late as seven years before consulting to doctors. Anxiety, stress, and fear are the most common trigger for bleeding, while psychiatric disorders are the most common comorbidities in most patients. Notably, 36 cases (34%) do not have any obvious bleeding triggers. Besides bleeding from the skin, patients may also present with hematuria, gastrointestinal (GI) bleed (hematemesis, melena, hematochezia or rectal bleed), or epistaxis. Patients may bleed as frequently as more than 35 times a day or as rare as two times in two years. Most bleeding episodes subside in a few seconds to a few minutes, although in one case, the bleeding stops after 30 min (Table 2).
| Ref. | Patient No. | Time from onset to consultation | Triggers of bleeding | Other kinds of bleeding | Comorbidities | Bleeding frequency | Bleeding duration | Other Bleeding characteristics |
| Octavius et al[70], 2021 | #1 | One month | Not mentioned | Not mentioned | Not mentioned | Three times per day | Stopped immediately | Not mentioned |
| #2 | One month | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | |
| Bhattacharya et al[42], 2013 | #1 | One month | Not mentioned | Not mentioned | Not mentioned | > 10 times per day | Not mentioned | Not mentioned |
| Manonukul et al[43], 2008 | #1 | 1.5 yr ago | Not mentioned | Not mentioned | Not mentioned | Recurrent episodes | Not mentioned | Not mentioned |
| Murota et al[45], 2020 | #1 | A few months | Excess pressure exerted while playing on the metal bar | Not mentioned | Not mentioned | Not mentioned | Not mentioned | It did not occur during sleeping |
| Das et al[89], 2020 | #1 | Two weeks | Head trauma | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned |
| #2 | One hour | Anxiety symptoms | Anxiety | |||||
| Matsuoka et al[36], 2020 | #1 | Two years | Not mentioned | Not mentioned | Dissociative disorder and self-harming | Few times per week | Not mentioned | Bloody sweat-like fluid secretion |
| Chabchoub et al[49], 2013 | #1 | 6 mau | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned |
| Shafique et al[38], 2021 | #1 | 3 mo | Not mentioned | Rectal bleed | Significant psychosocial stress due to parental separation | 3-35 times per day | Not mentioned | Occurred during sleep and wakefulness |
| Carvalho et al[35], 2008 | #1 | November 2004 | Physical exertion, increase in room temperature | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Ceased spontaneously |
| Rossio et al[32], 2014 | #1 | Not mentioned | His family was experiencing an extremely stressful time, and his mother had just passed away | Not mentioned | Not mentioned | Not mentioned | 1-2 min | No predetermined time for recurrence |
| Gayal et al[90], 2020 | #1 | Six months | Hearing voices and anxiety | Not mentioned | Schizophrenia | 1-2 or 10-15 times per day | Not mentioned | Depending on the intensity of psychotic symptoms |
| Dragan et al[91], 2017 | #1 | Not mentioned | Not mentioned | Epistaxis, hemoptysis | Tonsillectomy, benign hypertension | Not mentioned | Not mentioned | Not mentioned |
| Alsermani et al[23], 2018 | #1 | Five months | Bullying in schools | Not mentioned | Celiac disease | Twice weekly | 1-2 min | Self-limited, usually in the evening |
| Jayaraman et al[92], 2017 | #1 | Seven days | Scolding from parents due to academic performance | Not mentioned | Mixed anxiety & depressive disorders, nocturnal enuresis | 1-2 a day | 3-5 min | Appears when punished or stressed |
| Jibbawi et al[33], 2021 | #1 | Not mentioned | Emotional stress | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Appears during stress and self-limited |
| Arakkal et al[24], 2016 | #1 | 5 mau | Extreme physical exertion | Not mentioned | Not mentioned | Not mentioned | 2-3 min | Bleeding when waking up, extreme physical activities, self-limited |
| Corrà et al[93], 2020 | #1 | Five years | Stress, anxious situation, exercise | Not mentioned | The peripheral visual deficit, non-hemorrhagic chronic gastritis, severe intestinal subocclusion | Five times daily | Few minutes | Self-limited |
| Mishra[72], 2009 | #1 | Not mentioned | Minor trauma | Hematuria, gastrointestinal bleed, epistaxis | Platelet function (PF3) dysfunction | Not mentioned | Not mentioned | Not mentioned |
| Mutanabbi et al[29], 2021 | #1 | 4 mau | Stress | Hematemesis, hematuria, epistaxis | Not mentioned | 1-2 a week | 3-5 min | Ceased spontaneously, precipitated by upcoming stress & family issues |
| Soliman et al[61], 2019 | #1 | Six months | Not mentioned | Not mentioned | Hypotension, tachycardia, syncope | Not mentioned | 30 seconds | Never at sleep and self-remitting |
| Tshifularo[94], 2013 | #1 | Not mentioned | Severe mental stresses at work, study, and home | Not mentioned | Not mentioned | 2-3 a week every 3-4 mo | 15-20 min | 2-5 ml blood-stained non-clotting discharge |
| #2 | Two years | Severe stress | Four times in 2 years (2009-2010) | Not mentioned | Blood-stained sweaty discharge, not clotting and watery | |||
| #3 | Not mentioned | Stress | Two times in 2 years (2010-2011) | Not mentioned | Painless blood-stained sweat-like discharge | |||
| #4 | Not mentioned | Severe stress at school and home | 1st episode at July 2013 | Not mentioned | Not mentioned | |||
| Meyer et al[95], 2019 | #1 | Two days | Stumbled and fell on an iron toy train (trauma) | Not mentioned | Not mentioned | Almost daily | N/A | Self-limiting, episodic. Bleeding occurred from apparently healthy and undamaged skin; no superficial injuries |
| Techasatian et al[81], 2016 | #1 | April 2014 | Not mentioned | Not mentioned | Not mentioned | > 10 times | 10-30 seconds | The time of the bleeding episode was unpredictable, not related to exertion or triggers |
| Yeşilova et al[96], 2016 | #1 | 2 d | Move from cold to a warm environment, fallen out of bed (trauma) one day before | Not mentioned | Not mentioned | 20 times in 2 d | Not mentioned | Not mentioned |
| Quentric et al[97], 2019 | #1 | Not mentioned | General anxiety related to school | Epistaxis, nipple bleed | Not mentioned | 3-4 times a day | Not mentioned | Spontaneously, mostly at night |
| Mora et al[98], 2013 | #1 | 6 mo | Stress | Not mentioned | Not mentioned | Several times a day | Not mentioned | Spontaneous, self-limited, >30 episodes during hospitalization |
| Praveen et al[99], 2012 | #1 | 3 mo | Stress (She had witnessed her elder sister being kidnapped nine months ago) | Epistaxis | Not mentioned | 2-3 times every week and had two episodes on the same day on four occasions | Not mentioned | Not mentioned |
| Hansson et al[7], 2019 | #1 | Four weeks | Not mentioned | Not mentioned | Not mentioned | 20 episodes in 4 weeks | Not mentioned | Not mentioned |
| Wang et al[44], 2014 | #1 | One month | Not mentioned | Not mentioned | Not mentioned | 2-3 times a day | Not mentioned | The bleed is described as a fresh, small amount of blood |
| Jerajani et al[41], 2009 | #1 | Two months | Continuous mental stress | Not mentioned | Depressive disorder | Not mentioned | Not mentioned | Not mentioned |
| Lipsitt et al[100], 2018 | #1 | 9 mo | Extreme emotional stress, excitement, or physical exertion | Not mentioned | Depression, anxiety, PTSD, non-epileptiform seizure | Seven times a day | Not mentioned | Progressive, episodic |
| Bhagwat et al[101], 2009 | #1 | Two years | Trauma (witnessing a woman beheaded), Feeling anxious | None | Severe depression | 1-2 a day | 15-20 min | Episodic |
| Sue Tin et al[40], 2015 | #1 | Three weeks | No obvious trigger | Not mentioned | Not mentioned | 20 times a day | Not mentioned | Spontaneous, worse during warmer months |
| Pari[102], 2018 | #1 | Five days | Without any provoking factor | Not mentioned | Not mentioned | 2-3 a day | 30 min | Not mentioned |
| Patel et al[79], 2010 | #1 | Sincmaury 2007 | Not mentioned | Not mentioned | Not mentioned | Once-daily | 1 minute | Spontaenous, during school hours 9-11 am |
| Biswas et al[76], 2013 | #1 | Two years | Not mentioned | Not mentioned | An intelligent quotient (IQ) of 60-70 with a loss of insight | 1-2x daily | 10-15 min | Episodic, more frequent when waking up in the morning |
| Jafar et al[69], 2016 | #1 | Two weeks | Not mentioned | Epistaxis | Repeated faint attacks two years ago | Not mentioned | 10-20 min | It was spontaneous, unpredictable, and intermittent, with no specific patterns, and it stopped spontaneously. |
| Wang et al[103], 2010 | #1 | 3 yr | Emotional excitement | Not mentioned | Not mentioned | > 20 times during hospitalization | Not mentioned | It always occurred during the middle of the day, never when sleeping at night |
| Thigarajan[83], 2019 | #1 | Three days | Stress fr’m father's demand on academics | Not mentioned | Primary enuresis, head tonsure, and trivial head trauma in a different location to the bleed | Not mentioned | Few seconds to a few minutes | Self-limited |
| Khalid et al[82], 2013 | #1 | Five years | Emotional stress | None | None | Not mentioned | Not mentioned | Not mentioned |
| Maglie et al[104], 2017 | #1 | Three years | Not mentioned | Not mentioned | Major depressive disorder and panic disorder | Not mentioned | 1-5 min | Could occur in sleep or during physical activity & more intense bleeding occurs during emotional stress |
| Uber et al[71], 2015 | #1 | 6 yr | Not mentioned | Not mentioned | Conversion, dissociative, and generalized anxiety disorder, high peak blood pressure | Not mentioned | Few minutes | Spontaneous, sometimes occur during sleep, coincidental with high blood pressure peak |
| Salas-Alanis et al[37], 2021 | #1 | Not mentioned | Acute emotional distress | Not mentioned | Not mentioned | Numerous | 3-25 min | From 6 years old, all following emotional distress |
| Talwar et al[80], 2021 | #1 | One year | Separation from his aunt | Epistaxis, hematuria, hematochezia | Adjustment disorder | Once per week | A few minutes | It can occur during sleep |
| Chowdhury et al[105], 2019 | #1 | Two years | Migraine | Epistaxis, previous cesarean scar, menorrhagia | Migraine | Not mentioned | Not mentioned | Associated with headache, her son also had hematidrosis |
| Das et al[89], 2016 | #1 | 5 mo | Not mentioned | None | Otitis externa | Not mentioned | Not mentioned | More frequent on 06:00 A.M. |
| Hossain et al[77], 2018 | #1 | One and a half years | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned |
| #2 | Last two months | Not mentioned | Not mentioned | Repeated episodes of stiffening of limbs with associated self-muttering | Not mentioned | Not mentioned | Not mentioned | |
| #3 | Six months | Not mentioned | Not mentioned | Acute anxiety state, repeated episodes of unresponsiveness and conduct disorder | Not mentioned | Not mentioned | Not mentioned | |
| Thao et al[39], 2019 | #1 | One month | Marriage | Not mentioned | Continuous mental stress | Not mentioned | Not mentioned | Not mentioned |
| Récher[31], 2021 | #1 | Not mentioned | COVID-19 containment induced stress | Not mentioned | Not mentioned | Not mentioned | Not mentioned | A vascular pathway remains after 24 hours of bleeding |
| Omar[30], 2018 | #1 | Not mentioned | Stress | Not mentioned | Not mentioned | Occured in bouts | Not mentioned | Not mentioned |
| Tirthani et al[86], 2021 | #1 | Three months | Loss of parents | Not mentioned | Recurrent panic attacks with tachycardia | Not mentioned | 2-3 min | Not mentioned |
| Ricci et al[106], 2018 | #1 | Three months | Major stressful event from an earthquake | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned |
| Bezner et al[25], 2013 | #1 | Two years | Not mentioned | Hematuria | Heavy and irregular menstrual bleed | Up to 20 daily | Not mentioned | The bleeding episodesreportedly decreased during her menstrual period, which typically lasted for approximately ten days |
| Mahamat Abderraman et al[50], 2019 | #1 | Five years ago | Not mentioned | History of hematuria, epistaxis, | Moderate anxiety-depressive disorder, acute urine retention, seizure, genu flexum | Not mentioned | 10 min | Not mentioned |
| Rharrabti et al[51], 2016 | #1 | Not mentioned | Family abuse, parental conflicts | Vulvar bleeding | Conversion disorder. primary enuresis | Not mentioned | Not mentioned | Mostly at day, worsening during parental conflicts |
| Morillo et al[52], 2019 | #1 | Seven months | Not mentioned | Not mentioned | Bronchial asthma, previous history of abortion | Not mentioned | Not mentioned | Not mentioned |
| Kumar et al[78], 2021 | #1 | Not mentioned | Afraid, stress (during exams), anxiety | Not mentioned | High-grade anxiety | Not mentioned | Not mentioned | Spontaneous and recurrent (4-5 times in three days) |
| Camargo et al[53], 2020 | #1 | Four years | Stress and anxiety | Hematuria | Not mentioned | 2-3 times a week | Not mentioned | Sporadic occurrence |
| Shen et al[107], 2015 | #1 | Six months | Not mentioned | Not mentioned | Tonic seizures | 1x every few days | 1-2 min | Spontaneous, transient, self-limited |
| Shahriari et al[108], 2020 | #1 | Six months | Going to the toilet or feeling lonely | Not mentioned | Not mentioned | Every two weeks | Not mentioned | Not mentioned |
| #2 | Not mentioned | Not mentioned | Epistaxis | Not mentioned | Every three weeks | Not mentioned | Not mentioned | |
| #3 | Not mentioned | Fighting with her younger sister without any skin damage | Not mentioned | A history of aggression | Not mentioned | Not mentioned | Not mentioned | |
| Badry et al[27], 2020 | #1 | One month | Stress | Hematemesis | Depression | 3-5 per week | A few minutes | Not mentioned |
| Hoover et al[54], 2019 | #1 | Almost more than seven years | Illness (malaria) or distress | Hematemesis, hematochezia, hematuria | Previous history of treated malaria, human immunodeficiency virus(HIV) and hepatitis B due to blood transfusions | Not mentioned | Not mentioned | Not mentioned |
| #2 | Not mentioned | Irritability and crying | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | |
| Latorre Martinez et al[109], 2012 | #1 | One year | Stress | Not mentioned | Not mentioned | Not mentioned | A few minutes | Not mentioned |
| Kleymenova et al[47], 20201 | #1 | Not mentioned | Weather, stress | Epistaxis | Menstruation problems | Not mentioned | Not mentioned | Not mentioned |
| Rani et al[84], 2018 | #1 | Not mentioned | Autonomic dysfunction | Hematuria | Autonomic dysfunction | Not mentioned | Not mentioned | Not mentioned |
| #2 | Autonomic dysfunction | Not mentioned | Spontaneous skin breaches resembling incision | |||||
| #3 | Emotional & Psychological stressors | Not mentioned | Not mentioned | |||||
| #4 | Emotional & Psychological stressors | Not mentioned | Not mentioned | |||||
| #5 | Emotional & Psychological stressors | Not mentioned | Not mentioned | |||||
| #6 | Emotional & Psychological stressors | Not mentioned | Not mentioned | |||||
| Wang et al[110], 2021 | #1 | One year | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned |
| #2 | Four months | Not mentioned | Hematemesis | Not mentioned | Once every few days to dozens of times a day | Several minutes | Not mentioned | |
| #3 | Five months | Carsickness | Hematuria | Canker sores | Up to 60 times a day | Several minutes | Not mentioned | |
| #4 | Nine months | Anxiety or nervousness, hemolacria induced by intense light | Hematemesis, hematuria | Tonic-clonic seizures | Once every few days to dozens of times a day | Several minutes | Not mentioned | |
| #5 | Two months | Not mentioned | Not mentioned | Not mentioned | Once every few days to dozens of times a day | Several minutes | Not mentioned | |
| #6 | Four years | Military training, minor emotional stress, or even during studying | Not mentioned | Not mentioned | Once every few days to dozens of times a day | Several minutes | Not mentioned | |
| #7 | Six months | Not mentioned | Not mentioned | Not mentioned | Once every few days to dozens of times a day | Several minutes | Not mentioned | |
| Malik et al[34], 2019 | #1 | 6-8 yr | Emotional stress | History of hemolacria | Gestational hypertension (after lost to follow up) | Not mentioned | Not mentioned | Bleeding started 6-8 years ago |
| #2 | Not mentioned | Periods of rage and stress | Epistaxis | Not mentioned | Not mentioned | Not mentioned | Unprovoked, self-limited, and not triggered | |
| Shahgholi[75], 2018 | #1 | Several months | Extreme physical or emotional stress | Hematemesis | Not mentioned | Once or twice a day | 10-15 min | Sometimes occurred spontaneously during sleep, subsided as soon as it is wiped |
| #2 | Not mentioned | Upcoming exam, playing a computer game, watching fiction TV movies or when parents not satisfying his demands | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | |
| #3 | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | 5 min | Spontaneous, unpredictable, and intermittent | |
| Jagannathan et al[111], 2016 | #1 | Not mentioned | Mental stress | Epistaxis | Not mentioned | Not mentioned | Not mentioned | Not mentioned |
| #2 | Not mentioned | |||||||
| #3 | Not mentioned | |||||||
| #4 | Not mentioned | |||||||
| #5 | Not mentioned | |||||||
| #6 | Not mentioned | |||||||
| #7 | Not mentioned | |||||||
| #8 | Hematemesis | |||||||
| Agarwal et al[28], 2017 | #1 | One month | Not mentioned | Not mentioned | Not mentioned | Not mentioned | 10 seconds | Self-limited, during the day |
| Deshpande et al[112], 2014 | #1 | Since February 2013 (around more than one year ago) | Upcoming exams, fight with parents, and parents not satisfying his demands | Hemoptysis, hematuria, epistaxis, hematochezia, hematemesis | Oppositional defiant disorder | Not mentioned | Not mentioned | Not mentioned |
| Zhang et al[16], 2004 | #1 | Four months | Not mentioned | Hematemesis | A previous diagnosis of Henoch-schonlein purpura | Several times a day or once every 3-5 d | Lasts seconds | The bleeding can occur during sleep |
| Kumar et al[78], 2019 | #1 | One year ago | Suspected fear and anxiety of his lecturer | Not mentioned | Not mentioned | Three episodes per day to 20 episodes per month | Not mentioned | Not mentioned |
| #2 | Three months ago | Fearful dreams | Not mentioned | Not mentioned | > 5 episodes per day | Not mentioned | Episodes are not coinciding with dreams but occur after the event at night without any triggering factor in the day times as observed by parents at home and the hospital | |
| Karpukhina et al[48], 2020 | #1 | One month ago | Not mentioned | Epistaxis | High anxiety, neurotic behaviour, and depression | Not mentioned | A few minutes | Not mentioned |
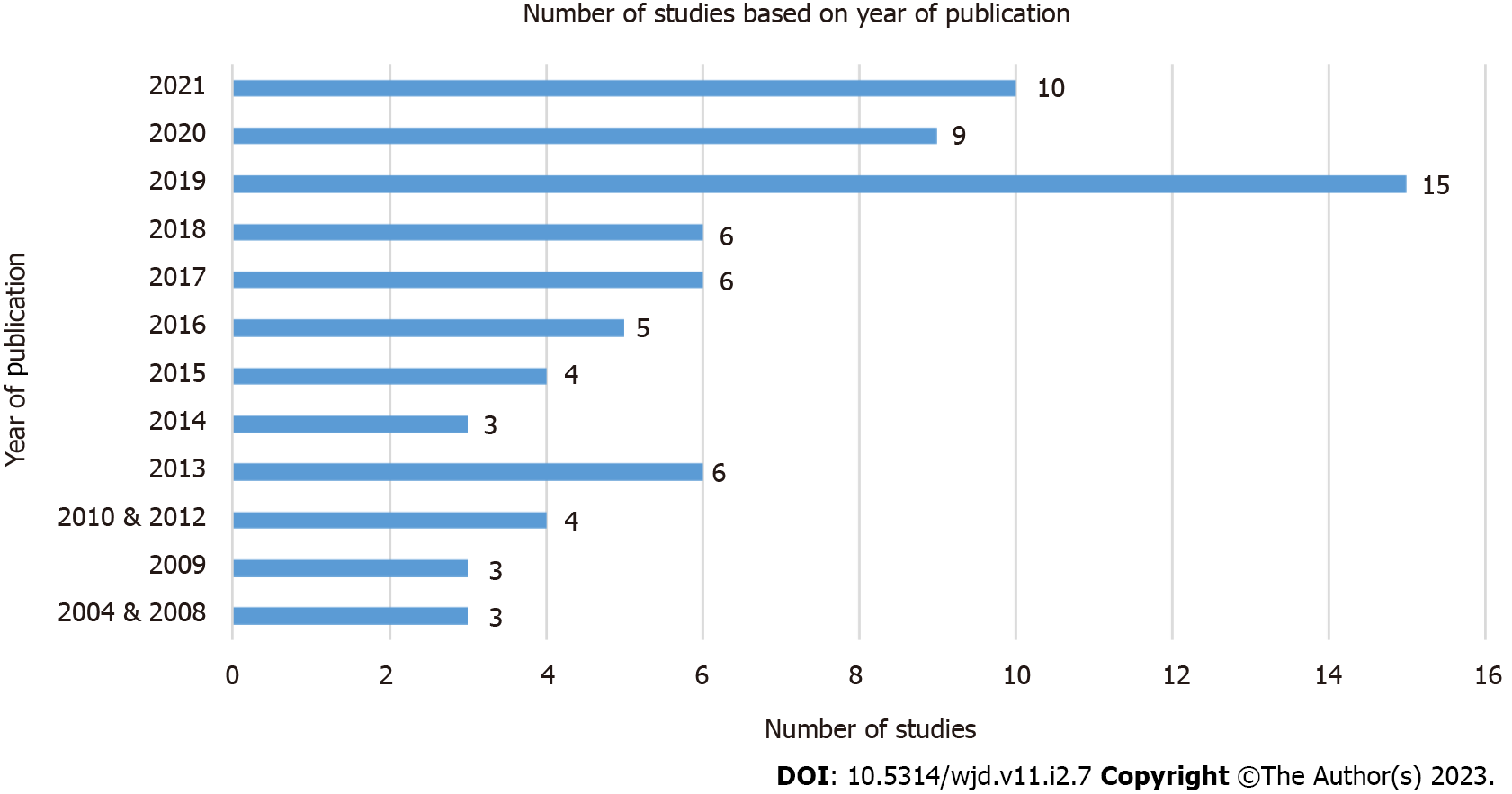
The majority of the patients are females (76.5%), with a median age of 13 (0.17-72) years old (Table 3). When patients experience prodrome(s) before the bleed, they mostly report headache (26.9%) or abdominal pain (16.4%). Most articles were published in 2019 (n = 15/74), followed by 2021 (n = 10/74) (Figure 3). When analyzed by the category of the journals, most hematidrosis cases are published in dermatology journals (25.7%), followed by internal medicine journals (23.0%) and pediatric journals (20.3%).
| Variables | N (%) |
| Sex (n = 102) | |
| Male | 24 (23.5) |
| Female | 78 (76.5) |
| Age in years (n = 94) (Median - range) | 13 (0.17-72) |
| Prodromes1 | |
| Headache | 18 (26.9) |
| Dizziness | 3 (4.5) |
| Abdominal pain | 11 (16.4) |
| Nausea | 4 (6.0) |
| Vomiting | 4 (6.0) |
| Tingling | 5 (7.5) |
| Photophobia | 2 (3.0) |
| Phonophobia | 2 (3.0) |
| Pain | 3 (4.5) |
| Soreness | 4 (6.0) |
| Asthenia | 3 (4.5) |
| Easily irritable | 2 (3.0) |
| Others | 6 (8.7) |
| Presence of hemolacria | 34 (32.1) |
| Types of journals | |
| Case report | 4 (5.4) |
| Dermatology | 19 (25.7) |
| Otorhinolaryngology | 4 (5.4) |
| General or internal medicine | 17 (23.0) |
| Hematology and oncology | 9 (12.2) |
| Pediatric (including pediatric hematology and oncology) | 15 (20.3) |
| Pharmacy | 1 (1.3) |
| Preprint (Research Square) | 1 (1.3) |
| Psychiatry | 3 (4.1) |
| Reproductive health | 1 (1.3) |
| Healthcare professionals witness the bleeding episodes | |
| Yes | 69 (65.1) |
| No | 25 (23.6) |
| Not explicitly mentioned | 12 (11.3) |
| Family members witness the bleeding episodes | |
| Yes | 50 (47.2) |
| No | 6 (5.6) |
| Not explicitly mentioned | 50 (47.2) |
| Provided bleeding pictures | 85 (80.2) |
| Laboratory tests done | 100 (94.3) |
| Radiologic and/or other tests done | 41 (38.7) |
| Normal results from all the diagnostic tests done | 92 (86.8) |
| Skin biopsies done | 30 (28.3) |
| Normal or non-specific | 19 (63.3) |
| Analyzed the blood from the bleeding site | 71 (67.0) |
| Doctors involved in the case1 | |
| Otolaryngologist | 25 (16.6) |
| Ophthalmologist | 6 (4) |
| Obstetrics and gynaecologist | 3 (2) |
| Psychiatrist | 29 (19.3) |
| Primary care | 4 (2.7) |
| Pediatrics | 31 (20.5) |
| Internal medicine | 19 (12.8) |
| Dermatologist | 25 (16.6) |
| Vascular surgeon | 1 (0.7) |
| Neurologist | 7 (4.8) |
| Tried to exclude other diagnoses | 90 (84.9) |
| Pharmacotherapy2 | |
| Beta-blockers | 65 (43.0) |
| Anxiolytic | 35 (23.2) |
| Antidepressants | 10 (6.6) |
| Atropine patches | 2 (1.3) |
| Drops of adrenaline with gauze | 1 (0.7) |
| Ascorbic acids | 6 (4.0) |
| Antifibrinolytic agents | 2 (1.3) |
| Antihistamine receptor blockers | 6 (4.0) |
| Hemostatics | 2 (1.3) |
| Others | 22 (14.6) |
| Psychosocial therapy2 | |
| Psychotherapy | 15 (37.5) |
| Behavioural therapy | 6 (15) |
| Relaxation technique | 6 (15) |
| Counseling | 13 (32.5) |
| Outcome (n = 90) | |
| Complete resolution | 37 (41.1) |
| Time taken for complete resolution in days (median) (n = 26) | 60 (2-730) |
| Improvement of symptoms | 37 (41.1) |
| Time taken for improvement of symptoms in days (median) (n = 19) | 28 (10-720) |
| Relapse | 8 (8.9) |
| Time taken for relapse in days (mean) (n = 6) | 60 (53.4) |
| Spontaneous resolution | 4 (4.4) |
| The patient is still under follow up | 1 (1.1) |
| Loss to follow up | 3 (3.3) |
| Possibilities of hematidrosis | |
| Highly likely | 21 (19.8) |
| Likely | 58 (54.7) |
| Unlikely | 27 (25.5) |
Out of all the body regions, the head region is the most commonly affected (n = 168/254), especially around the ears or earlobes (n = 46), forehead (n = 24), and nose (n = 23). The next most common site is in the upper limbs (n = 31/254), with the arms being the most common site of bleeding in this region (n = 14). Although most cases do not state the laterality of bleeding (n = 81), more cases are bilateral (n = 15), as compared to being unilateral bleeding (n = 10) (Figure 4).
The bleeding episodes are mostly witnessed by healthcare professionals (65.1%). In the case of family members witnessing the bleeding episode, 50 cases (47.2%) are witnessed directly, and another 50 cases (47.2%) are not explicitly mentioned. The majority of the cases provide bleeding pictures (80.2%). Laboratory tests and radiologic or other tests are done in 94.3% and 38.7% cases, respectively, resulting in a normal result in 86.8% of the cases. An analysis of the bleed is done in 67.0% of cases, generally resulting in the discovery of peripheral blood components. There are many doctors from different specialities involved in the care of hematidrosis patients, with paediatricians (20.5%), psychiatrists (19.3%), dermatologists, and otolaryngologists (both at 16.6%) being the most common specialities consulted.
Skin biopsies, the "best reference standard", is only done in 28.3% of cases, with 63.3% of them being normal or non-specific. Among skin biopsies that have been done, abnormal findings include dilation of blood vessels with extravasation of blood[35-39], possible mild squamous hyperplasia and mild dermal fibrosis[40], papillary dermal edema[41,42] with dermal melanophages[41], bloody exudate from areas that do not contain sweat glands[43,44], a low number of gross cystic disease fluid protein 15-positive eccrine sweat glands[45], loosening areas caused by the separation of collagen fibres[43], and acanthosis of the epidermis with broadening of rete pegs along with hypergranulosis and marked hyperkeratosis[42].
The most common pharmacologic therapy used is beta-blockers (43.0%), with anxiolytic the second (23.2%). Among the non-pharmacologic modality, psychotherapy (37.5%) and counseling (32.5%) are the most common therapies prescribed. Most patients experienced complete resolution (41.1%) in 60 d (2-730 d), as well as an improvement of bleeding symptoms (41.1%) in 28 d (10-720 d).
Among all the 106 cases, the majority of cases belong to the "likely" group with 58 cases (54.7%), followed by "unlikely" with 27 cases (25.5%). Only 21 cases (19.8%) are considered "highly likely" to be hematidrosis.
This systematic review contains 74 articles with 106 hematidrosis cases. We included more articles and cases compared to the other reviews and adjusting to their search timeline[2,3,7]. Hand-searching, citation searching, and including grey literature in our reviews certainly add more cases to our study. Although there has been some scepticism in including grey literature into a review, a proper systematic review shall be thorough during article searching, including finding grey literature[46]. Including the 76 cases from Holoubek and Holoubek's review[5] and our cases, there are currently 182 hematidrosis cases in the world.
Favaloro & Lippi's[6] arguments that most cases are outdated and presented in a foreign language are not valid anymore. Although some articles are written in Chinese[16,44] Russian[47,48], French[49-51], Spanish[52], and Portuguese[53], the majority of the articles are written in English language. Since the publications are mostly less than ten years old, we argue that the cases presented here are quite recent. Almost half of the articles were published in the years of 2019-2021. There is one study where the article was published in 2019, but on the website, the article is presented as if it was published in 2021. Therefore, we classify the study as published in 2019[54]. However, we believe that there is still a significant number of cases not published in a "high-quality journal" and thus may affect clinicians' perspectives on the eligibility of these cases[55]. Reflecting on the types of journal specialities, most cases are published in dermatology, pediatric, or internal medicine journals. Only 12.2% of the cases are published in a hematology journal. This point supports Favalaro & Lippi's argument about lacking publication in a high-profile hematology journal[6].
Most of the cases originate from China and India, the top two most populous countries globally. Although it seems convenient to link the connection between the majority of the cases belonging to the top two countries with the most population, the United States of America (USA) only reports three cases. Therefore, genetic, socio-cultural, race or environmental factors might play a role[56]. Lastly, publication bias may play a role in determining which cases get published[57]. Due to the rarity of the cases, many clinicians, even the most senior ones, may not encounter a hematidrosis case. Therefore, there is a lack of quality peer-reviewers who understand this case. This problem is confounded because many clinicians still doubt this disease entity[6].
The median age of patients with hematidrosis is 13 years, which is consistent with previous review findings of 9-15 years[3]. In this systematic review, 76.5% of the patients are females, while the most common trigger for hematidrosis is anxiety, fear, or mental illness. The connection between mental illnesses being more common in females[58-60] has been established and might explain the higher prevalence among these populations. In this study, the bleeding characteristics vary significantly. Some patients experienced bleeding episodes during sleep[38], while others never experienced bleeding during sleeping[45,61]. In some cases, patients usually bleed during the day or evening[23,28]. These patterns may reflect the physiological state of sympathetic nervous systems and hormonal fluctuations and their impacts on blood vessels and the pathophysiology of hematidrosis[62-64].
The head is the most common bleeding site, while headaches are the most common prodrome symptom. Spontaneous extracranial hemorrhagic phenomena may be caused by trigemino-autonomic reflex and sterile neurogenic inflammation[65]. Neural activation may also explain the prodromes of dizziness, nausea and vomiting, tingling, pain, photophobia, and phonophobia. Epistaxis is a frequent accompanying bleeding manifestation and may result from activating the trigeminovascular system and subsequent vasodilation of Kiesselbach's plexus[66]. Abdominal pain is the second most common prodrome. While certainly, the cause of abdominal pain is a multitude of etiologies, a case was reported in which bleeding from distant sites preceded by abdominal migraine[67]. Activation of selected nerves and release of neuropeptide and neurotransmitters may facilitate haemorrhage remote from the site of pain[68].
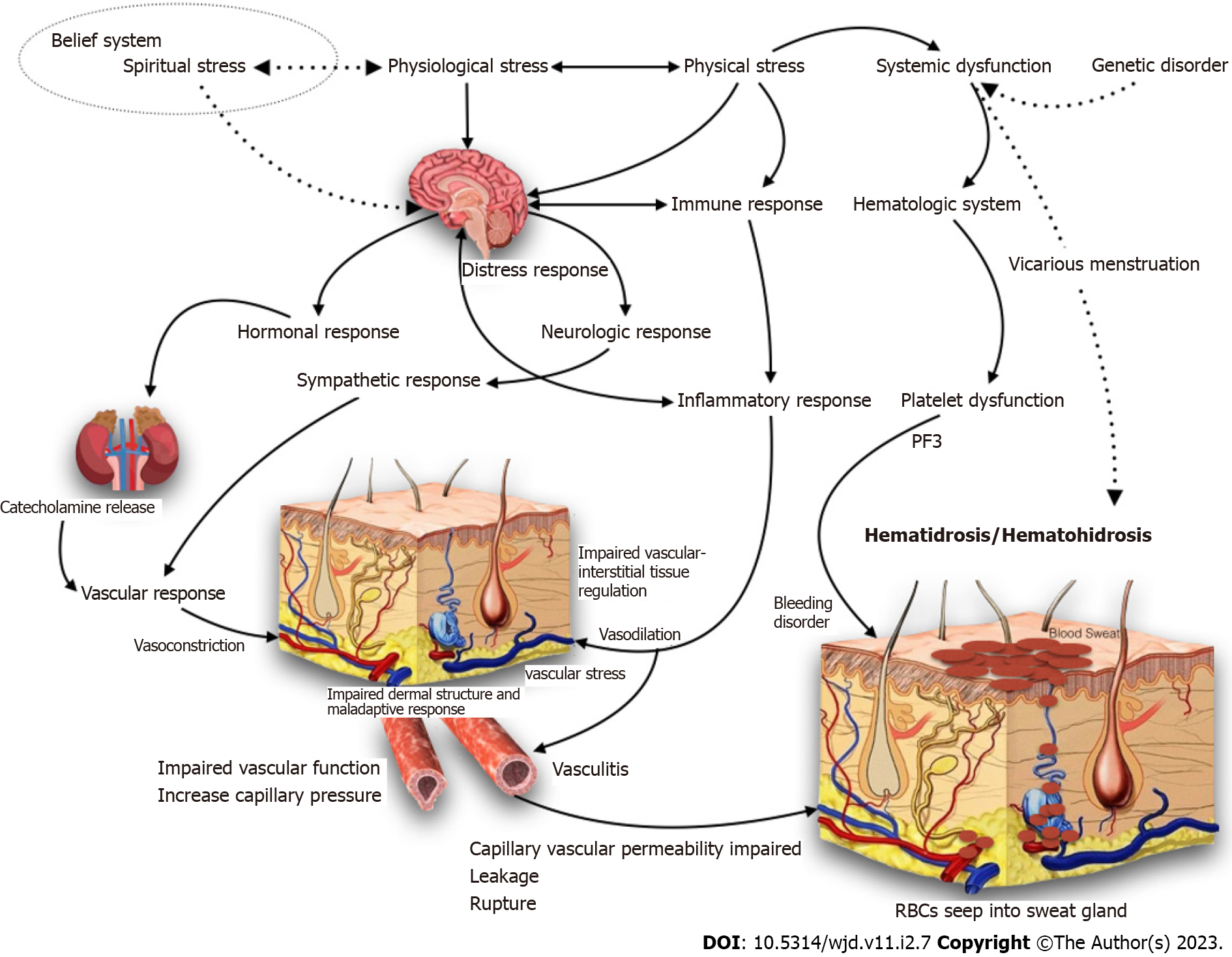
The pathophysiology of bleeding in other areas is still unknown. The blood seeps into the sweat ducts due to vasculopathies in the dermal vasculature and enhanced sympathetic activation due to acute stress and anxiety, resulting in periglandular vascular constriction and subsequent expansion[69,70]. Multiple blood veins arranged in a net-like structure surrounding the sweat glands. These vessels are thought to contract and then widen to the point of rupture when they are under much stress. The blood now travels to the sweat glands, which are pushed to the surface and manifested as blood droplets mixed with sweat[70,71]. These pathways explain why patients who suffer from anxiety, high blood pressure, or elevated sympathetic nervous system tone suffer from hematidrosis more frequently[71]. However, none of the biopsy results mention any vasculitis and this pathophysiology needs to be confirmed. The pathophysiology mentioned also does not explain the common co-occurrence of hemolacria, GI bleed, and hematuria. While there is a case of PF3 dysfunction[72], other patients do not have any hematological abnormalities after extensive workups. In the past, hematidrosis was thought to be caused by infections such as Chromobacterium prodigiosum and Micrococcus castellani[73]. One author also tested for the presence of these bacteria in their case report, although they did not find any chromogenic bacteria[38]. Figure 5 presents a complete postulated pathophysiological pathway of hematidrosis.
Cutaneous manifestation of Munchausen syndrome or other factitious bleeding related to stigmata usually presents in areas within reach of the arms of the patients (legs, arms, anterior part of the body, and face). These episodes always occur alone and is never witnessed by family members or general practitioners[74]. Therefore, when 34.9% and 52.8% of cases are not witnessed or explicitly mentioned to be witnessed by healthcare professionals and family members, respectively, the diagnosis of hematidrosis becomes weaker. It is important to note that family members as a witness have a lower strength of proof compared to being directly witnessed by healthcare professionals such as doctors, nurses, or residents. Munchausen syndrome cases by proxy where the parents smear their blood to their children to mimic hematidrosis[18].
Analysis of the exudate is done to ensure that the reddish or pinkish liquid contains blood components[75]. Some authors add benzidine test[32,41,53,76-82], hemochromogen test[39], chloride test[83], or blood group matching[84] in order to ensure that the blood is likely from the patient. However, as stated above, even though the presence of blood is confirmed via observation of red blood cells and other peripheral blood components under the microscope, the blood does not necessarily belong to the patient, even when matched by their blood group. Therefore, we propose that a skin biopsy needs further studies to be the "gold standard" to exclude other skin pathologies before safely confirming that a patient has hematidrosis[43]. However, a biopsy needs to be taken immediately during or after bleeding episodes. When the biopsy is taken any later, the results may be insignificant or even normal[43]. This means that patients need to be admitted just for the biopsy procedures. Clinicians need to weigh the unnecessary risks of hospitalization and added fear and stress against the need for a confirmatory procedure that may add little value to the diagnosis.
The wide involvement of specialists indicates that clinicians are initially perplexed by this condition. Multicollaboration among specialists is needed to exclude other causes of bleeding before diagnosing a patient with hematidrosis. The majority of the cases presented in this review tried to exclude other diagnoses before jumping into diagnosing hematidrosis. The full differential diagnosis of hematidrosis is presented in Table 4.
| Hematologic disorders (Bezner et al[25], 2013; Peretz et al[68], 2016) |
| Acquired disorder of hemostatic mechanism |
| A hereditary disorder of hemostatic mechanism |
| Infection (Jirka, 1968; Peretz et al[68], 2016) |
| Chromobacterium prodigiosum |
| Micrococcus castellani |
| Disorders of vascular integrity (Bezner et al[25], 2013; Peretz et al[68], 2016) |
| Vasculitis |
| Amyloidosis |
| Connective tissue disorders |
| Gynecologic disorders (Bezner et al[25], 2013) |
| Ectopic endometriosis |
| Pathologic processes causing an acute increase in intracranial pressure |
| Cerebral venous thrombosis |
| Subarachnoid hemorrhage |
| Valsalva maneuver |
| Drugs (Girolami et al[74], 2014; Peretz et al[68], 2016) |
| Antiplatelets such as non-steroidal anti-inflammatory drugs |
| Anticoagulants |
| Glucocorticoids |
| Antidepressants (e.g. selective serotonin reuptake inhibitors) |
| Antiepiletics (e.g. topiramate) |
| Antibiotics |
| Chemotherapeutic agents |
| Intoxication with lysergic acid diethylamide (LSD) |
| Herbal supplement (e.g. Gingko Biloba) |
| Trauma (Meyer et al[95], 2019; Peretz et al[68], 2016; Rani et al[84], 2018; Yeşilova et al[96], 2017; Zhang et al[16], 2004) |
| Sleep disorders (parasomnia) (Peretz et al[68], 2016) |
| Psychiatric disorders (Bezner et al[25], 2013; Karpukhina et al[48], 2020; Peretz et al[68], 2016) |
| Factitious disorder/factitious disorder by proxy |
| Psychogenic purpura |
| "Artistic bleeding" |
| Religious stigmata or culture-bound phenomenon (Bezner et al[25], 2013; Girolami et al[74], 2014) |
| Sweat gland disorders (e.g. chromhidrosis) (Jerajani et al[41], 2009) |
The most effective treatment seems to be a combination of pharmacologic and non-pharmacologic therapies. Beta-blockers and anxiolytics are the most commonly used pharmacotherapies in concordance with the postulated pathophysiology. However, other therapeutic modalities such as tap-water iontophoresis[45], inosine[44], aluminium chloride hexahydrate[85], and oxybutynin[86] are also used with mixed results. The wide range of therapies indicates that the optimal route, timing, and dosage of therapy is still largely unknown. For example, while atropine transdermal patches may be an effective treatment, certain bleeding locations such as the eyes or vaginal bleeding will exclude this treatment modality[40,76]. When a patient has underlying anxiety or fear, a psychiatrist should be consulted to give appropriate psychosocial therapy[87]. Only 41.1% of patients are fully resolved from bleeding episodes. This emphasizes that the current treatment is still not effective in managing hematidrosis. Clinicians are encouraged to educate and communicate about the aetiology and nature of the disease, emphasizing that this is not a stigma or a "shame" to suffer from hematidrosis. Underlying psychiatric disorders need to be addressed as well.
Shahgholi et al[75] also attempt at establishing hematidrosis diagnostic criteria. We agree on health professionals witnessing the bleeding episode to exclude psychiatric causes. However, Shahgholi et al[75] mentioned blood analysis as one of their criteria. We opt for skin biopsies as they are the "gold standard" for diagnosis, however more confirmatory studies need to be done before skin biopsies can be considered the “gold standard” for hematidrosis. Blood analysis can be plagued by some issues mentioned above. The last criteria by Shahgholi et al[75] are summarised in our criteria as the authors tried to exclude other possible diagnoses. This is imperative as hematidrosis is currently a diagnosis of exclusion. However, to be categorized as "highly likely" as hematidrosis, we also encouraged authors to include the bleeding pictures in the publication. This criterion is usually unable to be met by abstract or poster publications[84]. Our criteria serve only as guidance to consider hematidrosis as a plausible diagnosis and not as a confirmatory guideline.
Our review has some limitations. We could not confirm the true nature of hematidrosis in each case due to limited presentations in some of the articles. Therefore, we judged each case with the best available information. None of the contacted authors replied. Secondly, we could only postulate some associations, theories, and hypotheses between each finding without any causal confirmation. A cohort study with a standardized protocol will help determine the nature, progression, and treatment of hematidrosis. The exclusion of three articles without access to the full article is another limitation. However, those three articles are from China screened from their abstracts, they are unlikely to alter our review's findings significantly. Lastly, we do not include pure hemolacria cases in our review because pure hemolacria has its own sets of causes[88]. Therefore, including pure hemolacria in this review will cause heterogeneity.
Despite the limitations, our review is the most up-to-date with the most comprehensive literature search compared to other reviews[7,16,23-25,27-39,40-45,47,48,49-54,61,69-72,75-78,79-84,86,89-112]. Including articles in any language, combined with grey literature, citation searching, and hand searching, ensured that all available articles were included. We present clinical, diagnostic, and other socio-demographic findings that will help clinicians identify hematidrosis.
The future direction in diagnosing hematidrosis is currently evolving. Manonukul et al[43] performed electron microscopy and immunoperoxidase studies with normal results on both. Salas-Alanis et al[37] performed a genetic analysis and found that 91.5% of the variants are missense variants. The pathogenic variants were found in genes related to the extracellular matrix. These examinations will help us better understand the pathophysiology of hematidrosis.
Hematidrosis is a rare disorder with an increasing number of cases. This disease is more common in Asia and young females with underlying anxiety, fear, stress, or depression. The head region is the most common bleeding site, and some patients may experience prodromal symptoms such as headache and abdominal pain. An important note to take is that hematidrosis might be accompanied by other kinds of bleeding episodes such as hemolacria, GI bleeding, and epistaxis. The diagnosis is primarily on exclusion after ensuring that all the other diagnostic tests are normal. The most common treatment modality is a combination of pharmacologic (beta-blockers and anxiolytics) and non-pharmacologic (psychotherapy and counselling).
Although hematidrosis is rare and the pathophysiology is still largely unknown, that does not mean hematidrosis does not exist. It can bring severe panic towards parents or family members who care for these patients. Communication about the disease entity is imperative. A statement by Chambers perfectly surmmarized the rarity of hematidrosis "And as a rule, too, the more common the ailment, the more useful it is for you to hear about it"[113].
Hematidrosis is a largely unknown entity, even to professional doctors.
In order to bridge the underlying knowledge deficit about hematidrosis, an updated systematic review is conducted.
We aim to conduct a systematic review of hematidrosis and identify the clinical characteristics, laboratory findings, as well as treatments given so far.
We conducted a systematic search on eight different databases with no restrictions on the timeline using the English language.
There are 74 articles with 106 hematidrosis cases with India and China contributing the most cases. Patients are mostly females aged around 13 years. Bleeding occur most in the head region while beta-blockers and anxiolytics are the most frequent treatment given.
Hematidrosis exists, and it is up to clinical researchers to further dissect this entity so that physicians can give better treatment in the future.
More controlled skin biopsies and genetic studies with prospective follow-up or case-control studies may be needed to elucidate further and deepen our understanding of the pathophysiology and treatment of this disease.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dermatology
Country/Territory of origin: Indonesia
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shalaby MN, Egypt; Sofou EI, Greece S-Editor: Liu JH L-Editor: Ma JY P-Editor: Liu JH
| 1. | Stolberg M. Sweat: learned concepts and popular perceptions, 1500-1800. In: Horstmanshoff M, King H, Zittel C, editors. Blood, sweat and tears: The changing concepts of physiology from antiquity into early modern Europe. Leiden-Boston: Brill; 2012; 503-522. |
| 2. | Duffin J. Sweating blood: history and review. CMAJ. 2017;189:E1315-E1317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 3. | Kluger N. Hematidrosis (bloody sweat): a review of the recent literature (1996-2016). Acta Dermatovenerol Alp Pannonica Adriat. 2018;27:85-90. [PubMed] |
| 4. | Bonamonte D, Vestita M, Filoni A, Giudice G, Angelini G. Religious stigmata as malingering artifact: Report of a case and review of the literature. Medicine (Baltimore). 2016;95:e5354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Holoubek JE, Holoubek AB. Blood, sweat and fear. "A classification of hematidrosis". J Med. 1996;27:115-133. [PubMed] |
| 6. | Favaloro EJ, Lippi G. Commentary: Controversies in Thrombosis and Hemostasis Part 1-Hematidrosis: "Blood, Sweat and Fears" or A "Pigment of Fertile Imaginations? Semin Thromb Hemost. 2018;44:296-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 7. | Hansson K, Johansson EK, Albåge M, Ballardini N. Paediatric haematohidrosis: an overview of a rare but clinically distinct condition. Acta Paediatr. 2019;108:1023-1027. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2603] [Cited by in RCA: 5526] [Article Influence: 1105.2] [Reference Citation Analysis (33)] |
| 9. | Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Systematic Reviews. 2016;5: 210. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5711] [Cited by in RCA: 14136] [Article Influence: 1413.6] [Reference Citation Analysis (1)] |
| 10. | Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, Currie M, Lisy K, Qureshi R, Mattis P, Mu P. Chapter 7: Systematic reviews of etiology and risk. In: Aromataris E, Munn Z (Editors). Joanna Briggs Institute Reviewer's Manual. JBI Manual for Evidence Synthesis. 2022;. [DOI] [Full Text] |
| 11. | Shi J, Luo D, Weng H, Zeng XT, Lin L, Chu H, Tong T. Optimally estimating the sample standard deviation from the five-number summary. Res Synth Methods. 2020;11:641-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 345] [Article Influence: 57.5] [Reference Citation Analysis (0)] |
| 12. | Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018;27:1785-1805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2418] [Cited by in RCA: 2734] [Article Influence: 341.8] [Reference Citation Analysis (0)] |
| 13. | Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3433] [Cited by in RCA: 7931] [Article Influence: 660.9] [Reference Citation Analysis (0)] |
| 14. | Higgins JPT, Li T, Deeks JJ, (editors). Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions. 2nd Edition. Chichester (UK): John Wiley & Sons; 2019. p. 143-176 Available from: https://training.cochrane.org/handbook/current/chapter-06. |
| 15. | Chengrong X, Fan G, Yingling C. [A case of hemohidrosis]. Chinese Journal of Dermatology. 2010;43:79-81. |
| 16. | Zhang FK, Zheng YL, Liu JH, Chen HS, Liu SH, Xu MQ, Nie N, Hao YS. [Clinical and laboratory study of a case of hematidrosis]. Zhonghua Xue Ye Xue Za Zhi. 2004;25:147-150. [PubMed] |
| 17. | Wei L, Guoqiang Z, Yixia W, Guang Z, Rusong M. A case of hematohidrosis in children. Chinese Journal of Dermatology. 2006;39:113. |
| 18. | Saha B. Intriguing hemorrhages: a review of last seven decades (1951-2021). IJRMS. 2021;9:2520-2534. [DOI] [Full Text] |
| 19. | Naqvi S, Asadullah Khan R, Rupareliya C, Hanif R, Ali Z, Farooq F. Bleeding Diathesis or Fabrication: Munchausen Syndrome. Cureus. 2017;9:e1339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (1)] |
| 20. | Wiese MF. Bloody tears, and more! Br J Ophthalmol. 2003;87:1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Wieser S. Bloody tears. Emerg Med J. 2012;29:286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Barakova L, Reid J. Haemolacria Associated with Severe Attacks of Migraine with Visual Aura and Hypertension. Journal of Clinical Studies and Medical Case Reports. 7:102-104. [DOI] [Full Text] |
| 23. | Alsermani M, Alzahrani H, El Fakih R. Hematidrosis: A Fascinating Phenomenon-Case Study and Overview of the Literature. Semin Thromb Hemost. 2018;44:293-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Arakkal G, Poojari S, Netha G, Kumar B. Hematohidrosis: A rare case of a female child who sweat blood. IJPD. 2017;18:327-329. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Bezner SK, Buchanan GR. Bleeding from the eyes and through intact skin: physiologic, structural, spiritual, or faked? Am J Hematol. 2013;88:713-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Varalakshmi B, Doshi VV, Sivalingam D, Nambi S. The story of a girl with weeping blood: Childhood depression with a rare presentation. Indian J Psychiatry. 2015;57:88-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Badry M, Elbadry M, Ragab A-R, Ahmed M. Hematohidrosis: Reports and update of clinically mysterious phenomenon. Indian Journal of Otology. 2020;26:99-102. [DOI] [Full Text] |
| 28. | Agarwal S, Rani S. Hematidrosis: a hematology challenge. HTIJ. 2017;4:130-131. [DOI] [Full Text] |
| 29. | Mutanabbi M, Ali A, Akhter S, Mosleh T, Morshed J. Haematohidrosis: A Rare Case Report of A 12 year Old Girl with Unexplained & Puzzling Spontaneous Multiple Site Bleeding. Bangladesh Journal of Child Health. 2021;45:45-47. [DOI] [Full Text] |
| 30. | Omar S. Hematohidrosis, the Annoying Rare Condition, Case Report. Experiments in Rhinology & Otolaryngology. 2018;1:83-84. [DOI] [Full Text] |
| 31. | Récher C. Hematidrosis as a manifestation of COVID-19 containment-induced stress. EJHaem. 2021;2:25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (33)] |
| 32. | Rossio I, Gonçalves A. Haematidrosis: The Rare Phenomenon of Sweating Blood. Eur J Case Rep Intern Med. 2014:1-3. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 33. | Jibbawi A, Dirani F, Hassam I. An Extremely Rare Case Report of Hematiderosis in Lebanon ISSN Print : 2709-3522 | ISSN Online : 2709-3530 Frequency : Bi-Monthly Language : English An Extremely Rare Case Report of Hematiderosis in Lebanon I NTRODUCTION : 2021; 0–3. [DOI] [Full Text] |
| 34. | Malik KZ, Abdullah A, Maka TA. Hematohidrosis-A Rare Knocker At Otolaryngologist's Door. Pakistan Armed Forces Medical Journal. 2019;69:730-732. |
| 35. | Carvalho AC, Machado-Pinto J, Nogueira GC, Almeida LM, Nunes MB. Hematidrosis: a case report and review of the literature. Int J Dermatol. 2008;47:1058-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 36. | Matsuoka R, Tanaka M. Hematidrosis in a Japanese girl: Treatment with propranolol and psychotherapy. Pediatr Int. 2020;62:1001-1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 37. | Salas-Alanis JC, Salas-Garza M, Goldust MM, Fajardo-Ramirez OR. Haematidrosis and haemolacria in a young adult. Clin Exp Dermatol. 2021;46:394-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (33)] |
| 38. | Shafique DA, Hickman AW, Thorne A, Elwood HR, Zlotoff BJ. Pediatric hematidrosis - A case report and review of the literature and pathogenesis. Pediatr Dermatol. 2021;38:994-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (33)] |
| 39. | Thao NM, Lam THT, Doanh LH, Linh TT, Khang TH. A Vietnamese Case of Hematohidrosis. Madridge J Case Rep Stud. 2019;3:148-150. [DOI] [Full Text] |
| 40. | Sue Tin A, Cohn A. Blood sweat and tears - tackling the stigma of stigmata. J Paediatr Child Health. 2015;51:1134-1136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 41. | Jerajani HR, Jaju B, Phiske MM, Lade N. Hematohidrosis - a rare clinical phenomenon. Indian J Dermatol. 2009;54:290-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 42. | Bhattacharya S, Das MK, Sarkar S, De A. Hematidrosis. Indian Pediatr. 2013;50:703-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 43. | Manonukul J, Wisuthsarewong W, Chantorn R, Vongirad A, Omeapinyan P. Hematidrosis: a pathologic process or stigmata. A case report with comprehensive histopathologic and immunoperoxidase studies. Am J Dermatopathol. 2008;30:135-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 44] [Article Influence: 2.4] [Reference Citation Analysis (1)] |
| 44. | Wang LJ, An CX, Li YM, Cao CQ. [A case report of childhood hematidrosis]. Zhongguo Dang Dai Er Ke Za Zhi. 2014;16:214-215. [PubMed] |
| 45. | Murota H, Kotobuki Y, Yamaga K, Yoshioka Y. Female child with hematidrosis of the palm: Case report and published work review. J Dermatol. 2020;47:166-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 46. | Saleh AA, Ratajeski MA, Bertolet M. Grey Literature Searching for Health Sciences Systematic Reviews: A Prospective Study of Time Spent and Resources Utilized. Evid Based Libr Inf Pract. 2014;9:28-50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 47. | Kleymenova M, Khashchenko E, Kiseleva I, Uvarova E. Hemolacria and hematohydrosis: literature review and description of rare clinical cases in adolescent girls. Reproduktivnoe zdorov’e detey i podrostkov [Pediatric and Adolescent Reproductive Health]. 2020; 16: 102-16.. [DOI] [Full Text] |
| 48. | Karpukhina VN, Rudneva NS, Drachyov SN. Hematidrosis or artistic dermatitis? Medical Alphabet. 2020;6:34-35. [DOI] [Full Text] |
| 49. | Chabchoub RBA, Safi F, Trabelsi L, Maalej B, Gargouri L, Turki F, Amouri M, Halima NB, Turki, H, Mahfoud A. L’he´matidrose: a` propos d’un cas pe´diatrique. Archives de Pe´diatrie. 2013; 20: 559-566. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 50. | Mahamat Abderraman G, Djidita Hagre Y, Mahamat Hissein A, Boudalia A, Sauvage J, Ibrahim H, Glenn R, Brahim N, Achta AF, Tara F, Charfadine S, Aboubacar A, Haddoum F. Haematidrosis responding favorably to propranolol. Press Medicale. 2019;48:324-326. |
| 51. | Rharrabti S, Khattala K, Belahsen M, Aalouane R. [Hematidrosis and hemolacrea associated with conversion disorder. About a pediatric case]. Presse Med. 2016;45:712-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 52. | Morillo Z, Ureña Correa W, Guzmán D, Ortiz Y. A propósito de un caso: “la niña que suda sangre: un raro caso de hematohidrosis”. Ciencia y Salud. 2019;3:65-69. [DOI] [Full Text] |
| 53. | Camargo KdCFd, Rezende LV, Galisteu BL, Muniz DN, Gatica JL, Ribeiro TS, Kinoshita JN. Hematidrose: Doença Rara Relatada em Paciente Pediátrico. Press Medicale. 2020;1-10. |
| 54. | Hoover A, Fustino N, Sparks AO, Rokes C. Sweating Blood: A Case Series of 2 Siblings With Hematohidrosis. J Pediatr Hematol Oncol. 2021;43:70-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (33)] |
| 55. | Kratz JE, Strasser C. Researcher perspectives on publication and peer review of data. PLoS One. 2015;10:e0117619. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 56. | Bamshad M. Genetic influences on health: does race matter? JAMA. 2005;294:937-946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 101] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 57. | Joober R, Schmitz N, Annable L, Boksa P. Publication bias: what are the challenges and can they be overcome? J Psychiatry Neurosci. 2012;37:149-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 219] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 58. | Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry. 2017;4:146-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 596] [Cited by in RCA: 1011] [Article Influence: 112.3] [Reference Citation Analysis (0)] |
| 59. | Li SH, Graham BM. Why are women so vulnerable to anxiety, trauma-related and stress-related disorders? Lancet Psychiatry. 2017;4:73-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 389] [Article Influence: 43.2] [Reference Citation Analysis (0)] |
| 60. | Otten D, Tibubos AN, Schomerus G, Brähler E, Binder H, Kruse J, Ladwig KH, Wild PS, Grabe HJ, Beutel ME. Similarities and Differences of Mental Health in Women and Men: A Systematic Review of Findings in Three Large German Cohorts. Front Public Health. 2021;9:553071. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 100] [Article Influence: 20.0] [Reference Citation Analysis (33)] |
| 61. | Soliman M, Mowafy K, Soliman R. Synchronous genital and facial hematohidrosis in adult female: first case report from Egypt. EJMCR. 2019;3:28-32. [DOI] [Full Text] |
| 62. | Dodt C, Breckling U, Derad I, Fehm HL, Born J. Plasma epinephrine and norepinephrine concentrations of healthy humans associated with nighttime sleep and morning arousal. Hypertension. 1997;30:71-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 168] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 63. | Muller JE, Tofler GH, Verrier RL. Sympathetic activity as the cause of the morning increase in cardiac events. A likely culprit, but the evidence remains circumstantial. Circulation. 1995;91:2508-2509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 64. | Maus TL, McLaren JW, Shepard JW Jr, Brubaker RF. The effects of sleep on circulating catecholamines and aqueous flow in human subjects. Exp Eye Res. 1996;62:351-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 65. | Drummond PD. Mechanisms of autonomic disturbance in the face during and between attacks of cluster headache. Cephalalgia. 2006;26:633-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 42] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 66. | Jarjour IT, Jarjour LK. Migraine and recurrent epistaxis in children. Pediatr Neurol. 2005;33:94-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 67. | Kakisaka Y, Uematsu M, Wang ZI, Haginoya K. Abdominal migraine reviewed from both central and peripheral aspects. World J Exp Med. 2012;2:75-77. [PubMed] [DOI] [Full Text] |
| 68. | Peretz AM, Woldeamanuel YW, Rapoport AM, Cowan RP. Spontaneous extracranial hemorrhagic phenomena in primary headache disorders: A systematic review of published cases. Cephalalgia. 2016;36:1257-1267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 69. | Jafar A, Ahmad A. Child Who Presented with Facial Hematohidrosis Compared with Published Cases. Case Rep Dermatol Med. 2016;2016:5095781. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 70. | Octavius GS, Koleta T, Garniasih D, Yanto TA. Hematidrosis and Hemolacria: Report of Two Cases From Indonesia. Iranian Journal of Blood and Cancer. 2021;13:98-101. |
| 71. | Uber M, Robl R, Abagge KT, Carvalho VO, Ehlke PP, Antoniuk SA, Werner B. Hematohidrosis: insights in the pathophysiology. Int J Dermatol. 2015;54:e542-e543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 72. | Mishra KL. Bloody tears and hematohidrosis in a patient of PF3 dysfunction: a case report. Cases J. 2009;2:9029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 73. | Jirka M. Hemingway's sweating waiter. The Lancet. 1968;291:1429. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 74. | Girolami A, Bertozzi I, Tasinato V, Sambado L, Treleani M. Bleeding manifestations apparently unrelated to coagulation or other organic disorders: A tentative classification and diagnostic clues. Hematology. 2014;19:293-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 75. | Shahgholi E. A case series of hematohidrosis: A puzzling medical phenomenon. Turk J Pediatr. 2018;60:757-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 76. | Biswas S, Surana T, De A, Nag F. A curious case of sweating blood. Indian J Dermatol. 2013;58:478-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 77. | Hossain A, Nath S, Ghosh S, Hannan MHS, Pathak, Arnab, Mukherjee S, Dhar T. Hematohidrosis: Case Reports. Indian Journal of Psychiatry: Medknow Publications & Media Pvt Ltd; 2018; S124-S68. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5830862/. |
| 78. | Kumar S, Bhoi K, Yelme G. Hematohidrosis: A Rare and Mysterious Case. Asian Journal of Case Reports in Medicine and Health. 2021;5:10-13. |
| 79. | Patel RM, Mahajan S. Hematohidrosis: A rare clinical entity. Indian Dermatol Online J. 2010;1:30-32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 80. | Talwar M, Chidambaram AC, Mekala S, Parameswaran N, Delhikumar CG. Haematohidrosis in a 12-year-old boy: blood, sweat and tears. Paediatr Int Child Health. 2021;41:300-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (33)] |
| 81. | Techasatian L, Waraasawapati S, Jetsrisuparb C, Jetsrisuparb A. Hematidrosis: a report with histological and biochemical documents. Int J Dermatol. 2016;55:916-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 82. | Khalid SR, Maqbool S, Raza N, Mukhtar T, Ikram A, Qureshi S. Ghost spell or hematohidrosis. J Coll Physicians Surg Pak. 2013;23:293-294. [PubMed] |
| 83. | Thigarajan KRT. The vanishing ghastly bleeds - hematohidrosis. University Journal of Medicine and Medical Specialities. 2019;5:1-2. |
| 84. | Rani S, Sandhya V, Varshini B, Vishnuvardhan, Agarwal S. Hematidrosis-Case Series From A Tertiary Care Center. Pediatric Hematology Oncology Journal. 2018;. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 85. | Patel NA. Pediatric COVID-19: Systematic review of the literature. Am J Otolaryngol. 2020;41:102573. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 152] [Cited by in RCA: 153] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 86. | Tirthani K, Sardana K, Mathachan SR. Hematohidrosis of the mid-face and hands treated with oral oxybutynin. Pediatr Dermatol. 2021;38:962-963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (32)] |
| 87. | Shamoon ZA, Lappan S, Blow AJ. Managing Anxiety: A Therapist Common Factor. Contemporary Family Therapy. 2017;39:43-53. [RCA] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 88. | Ho VH, Wilson MW, Linder JS, Fleming JC, Haik BG. Bloody tears of unknown cause: case series and review of the literature. Ophthalmic Plast Reconstr Surg. 2004;20:442-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 89. | Das D, Kumari P, Poddar A, Laha T. Bleeding to Life: A Case Series of Hematohidrosis and Hemolacria. Indian J Pediatr. 2020;87:84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 90. | Gayal TD, Devi MG. A rare case of hematohidrosis in a patient with paranoid schizophrenia. IJRMS. 2020;8:3085-3087. [DOI] [Full Text] |
| 91. | Dragan J, Parrish RC. A 13-Year Old Female With Hemolacria and Hemoptysis. IJCMPR. 2017;3:2584-2586. [DOI] [Full Text] |
| 92. | Jayaraman AR, Kannan P, Jayanthini V. An Interesting Case Report of Hematohidrosis. Indian J Psychol Med. 2017;39:83-85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 93. | Corrà A, Quintarelli L, Caproni M. Bleeding from the oral cavity: a new case of hematohidrosis. Int J Dermatol. 2020;59:e421-e422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 94. | Tshifularo M. Blood otorrhea: blood stained sweaty ear discharges: hematohidrosis; four case series (2001-2013). Am J Otolaryngol. 2014;35:271-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 95. | Meyer J, Spacil K, Stehr M, Hinrichs W, Haller S, Schäfer FM. Hematidrosis After Head Injury - A Case Report. Klin Padiatr. 2019;231:326-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 96. | Yeşilova Y, Turan E, Aksoy M. Hematidrosis on the forehead following trauma: a case report. Int J Dermatol. 2017;56:212-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 97. | Quentric PV, Sauvêtre G. Unusual bleeding. Eur J Intern Med. 2019;68:e1-e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 98. | Mora E, Lucas J. Hematidrosis: blood sweat. Blood. 2013;121:1493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 99. | Praveen BK, Vincent J. Hematidrosis and hemolacria: a case report. Indian J Pediatr. 2012;79:109-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 100. | American Society of Pediatric Hematology/Oncology (ASPHO), David L. Lawrence Convention Center, Pittsburgh, PA, May 2-5, 2018. Pediatr Blood Cancer. 2018;65 Suppl 1:e27057. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 101. | Bhagwat PV, Tophakhane RS, Rathod RM, Shashikumar BM, Naidu V. Hematohidrosis. Indian J Dermatol Venereol Leprol. 2009;75:317-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 102. | Pari T. Hematohidrosis - A Rare Case. Indian Dermatol Online J. 2019;10:334-335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 103. | Wang Z, Yu Z, Su J, Cao L, Zhao X, Bai X, Zhan S, Wu T, Jin L, Zhou P, Ruan C. A case of hematidrosis successfully treated with propranolol. Am J Clin Dermatol. 2010;11:440-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 104. | Maglie R, Caproni M. A case of blood sweating: hematohidrosis syndrome. CMAJ. 2017;189:E1314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 105. | Chowdhury A, Islam M, Rahman H, Jannat M, Rahman M. Haematohidrosis with Headache-A Rare Phenomenon of Sweating Blood: A Case Report. Bangladesh Med Res Counc Bull. 2019;45:205-207. [DOI] [Full Text] |
| 106. | Ricci F, Oranges T, Novembre E, Della Bona ML, la Marca G, de Martino M, Filippi L. Haematohidrosis treated with propranolol: a case report. Arch Dis Child. 2019;104:171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 107. | Shen H, Wang Z, Wu T, Wang J, Ren C, Chen H, Yu Z, Don W. Haematidrosis associated with epilepsy in a girl successfully treated with oxcarbazepine: case report. J Int Med Res. 2015;43:263-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 108. | Shahriari M, Bazrafshan A, Karimi M, Shakibazad N. Case series of bloody sweating; a scary event for families. Acta Haematologica Polonica. 2020;51:258-260. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (31)] |
| 109. | Latorre Martinez N, Betlloch Mas I, Monteagudo Paz AF, Lucas Boronat J. Recurrent bleeding in an 18-year-old girl. Arch Dermatol. 2012;148:960-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 110. | Wang Z, Yin J, Yu Z, Han Y, Cao L, Kong D, Gu C, Bai X, Zhang X. Hematidrosis: Pathophysiology and Therapeutic Strategy. Research Square 2021, Preprint, Available from: https://doi.org/10.21203/rs.3.rs-256984/v1. |
| 111. | Jagannathan VV, Rajasekar M, Mathivanan S, Mehta MP. Spontaneous ear nose throat bleed: hematohidrosis an unknown entity series of eight cases. Int J of Otolaryngology and Head & Neck Surgery. 2016;2:164-167. |
| 112. | Deshpande M, Indla V, Kumar V, Reddy IR. Child who presented with hematohidrosis (sweating blood) with oppositional defiant disorder. Indian J Psychiatry. 2014;56:289-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |