INTRODUCTION
Many improvements have been made to total knee arthroplasty (TKA) since its development in the early 1970s[1]. However, despite the implementation of such innovations, as few as 43% of patients report being completely pain free following a primary TKA procedure[2]. While pain alone is seldom utilized as a criterion for revision surgery, it is estimated that 2% of all TKAs ultimately fail due to pain. When associated with other factors leading to revision, such as component wear or loosening, pain contributes to a growing number of revision procedures, increasing the monetary burden on the healthcare system, with an additional projected cost of $5.8 billion by 2015[3,4]. The reported incidence of anterior knee pain following primary TKA is 8%[5]. Several studies have been conducted to determine the cause of anterior knee pain following TKA with variable results.
Patient related factors that may contribute to increased pain following TKA include younger age, female gender, and ethnicity while modifiable non-patient related factors include prosthesis design as well as surgical error[2,6-8]. In fact, up to 41.1% of patients have been found to experience patellofemoral complications related to these modifiable elements[9,10]. Causes of patellofemoral complications include rotational errors of the femoral or tibial component, implant maltracking, patellar fracture, aseptic loosening, and polyethylene wear[5,10,11]. Addressing the prosthetic causes of TKA failure will allow improvements to be made in implant design which may result in a decreased incidence of revision surgery and a lessened economic burden for both the patient and the healthcare system. This paper aims to address several aspects of prosthetic design including femoral and patellar component features which may contribute to the development of anterior knee pain following TKA.
BIOMECHANICS AND KINEMATICS OF THE NATIVE KNEE
Identifying the biomechanical and kinematic parameters of the native knee, particularly that of the patellofemoral joint, is essential when attempting to identify prosthetic design features implicated in anterior knee pain following primary TKA. In both native and prosthetic knees, anterior knee pain has been attributed to patellar mal-alignment and mal-tracking within the femoral trochlear groove[12,13]. The primary contribution of the patella to knee biomechanics resides in its facilitation of knee extension. Through its function as a fulcrum, the patella is able to increase the moment arm of the quadriceps force increasing the muscle’s effectiveness in extending the knee[12]. The patella also plays important roles in the distribution of patellofemoral compressive forces during knee flexion as well as centralizing the multi-directional pull of the four quadriceps muscles in extension[12]. The contact area of the patella within the femoral trochlear groove is dynamic, with no contact in full extension, and contact beginning in the inferior pole of the patella with progressive increase in knee with continued knee flexion, this contact area continues to move peripherally on the patella as it goes into extreme flexion at the base of the trochlear groove[12].
The Q-angle is a measurement that aims to determine the lateral force vector acting on the patella, which is created by the combination of both the vector of the patellar tendon and the rectus[14]. It is defined as the angle between a line connecting the anterior superior iliac spine to the center of the patella and another line from the center of the patella to the tibial tubercle. This measurement describes the tendency of the quadriceps muscle to pull the patella laterally[12,15]. Higher Q-angles can increase the lateral pull by the quadriceps muscles, predisposing the knee to patellofemoral disorders such as patellar subluxation, dislocation, and increases in lateral patellofemoral contact pressure[14,15]. The Q-angle has also been demonstrated to influence active tibio-femoral kinematics through the positioning of the tibial tubercle. The extent of component rotation affects the position of the tibial tubercle and therefore the overall Q-angle[16].
ALTERATION OF KINEMATICS AFTER TKA
Anterior knee pain after TKA results primarily from excessive patello-femoral loads and abnormal patellar tracking[13,17]. Such complications can be related to the alteration of the biomechanical and kinematic parameters of the native knee, primarily factors leading to an increase in the Q-angle of the prosthetic knee. It is important to realize that the positioning of all the components of the total knee can affect the overall Q-angle and the kinematics of the patella in the trochlear groove[13]. More specifically, external rotation of the femoral component or internal rotation of the tibial component (leading to lateralization of the tibial tubercle) can result in an increase in the overall Q-angle[13]. Thus lateralizing a narrower femoral component as well as preventing excessive medial placement of the tibial component lead to reduction in the Q-angle, providing a better patellar tracking[13]. Patellofemoral loads can also be decreased by a medial pivot placement, which allows contact stress to be homogenously distributed across the patella[17]. Additionally, avoidance of overstuffing with an increased patellar height and medialization of the patellar component also prevent increases in the Q-angle[13]. Alterations in patellar kinematics can also be attributed to change in the tibiofemoral joint line with elevations leading to patellar complications including inferior edge loading and patellar impingement[18]. Therefore it is important to attempt to restore normal tibiofemoral as well as patellofemoral kinematics in order to decrease the risk of anterior knee pain following TKA[13,17].
SURGICAL TECHNIQUES WHICH REDUCE PATELLOFEMORALCOMPLICATIONS/ANTERIOR KNEE PAIN
Component mal-alignment following primary TKA
Component mal-alignment following primary TKA has a prevalence ranging between 9.4% and 11.8%[19,20]. Isolated internal rotation of the femoral component has been described as a potential source of prosthetic dysfunction, anterior knee pain, and potential early failure[21-23]. The degree of malrotation required to cause complications following TKA is not well delineated; however, surgical revisions have been successful in patients experiencing anterior knee pain and/or functional disability with ≥ 4 degrees of femoral component internal rotation[21,22].
Malrotation of the tibial prosthetic component constitutes another potential cause of a suboptimal clinical outcome following primary TKA[19,21,22]. While isolated tibial malrotation is not heavily explored in the literature, several techniques are described for quantifying the degree of component mal-rotation. One study defined the tibial component as internally mal-aligned when the rotation is of more than 18 degrees[22]. Subsequently, a strong correlation is reported between anterior or medial knee pain and isolated excessive tibial rotation[22]. When combined with femoral component internal rotation, as little as 3 degrees of mal-alignment can lead to pain and malfunction[22].
Femoral component rotation
Femoral component rotation also plays a key factor in patellar tracking and can contribute to patellofemoral complications following TKA. External rotation of the femoral component relative to the posterior femoral condyles facilitates central patellar tracking by reducing patellofemoral lateral shear forces[24-26]. External rotation of the femoral component leads to lateral positioning of the sulcus and preserves sulcus height which facilitates a more anatomic orientation of the trochlear groove[27]. This rotation also achieves a balanced flexion gap[2,5]. Therefore it is crucial for TKA systems to have instrumentation that allows for perfect external rotation of the femoral component in order to reproduce a more natural patellofemoral joint[25,27].
Patellofemoral overstuffing
Trochlear groove: Abnormal patellar tracking has been identified as a well-known cause of patellofemoral complications and anterior knee pain following TKA[24,28]. Several design features pertaining to the trochlear groove of the femoral component that directly influence the patellofemoral joint has been identified. The trochlear groove depth plays a major role in directing patellar tracking. A deepened trochlear groove better facilitates central tracking of the patella and can thus better secure the patellofemoral joint and minimize patellar instability, including lateral patellar subluxation, with increased degrees of knee flexion[25,28,29]. In addition to depth, the length of the trochlear groove can also improve overall patellar tracking by enabling a smooth transition from flexion to extension. Femoral components with a longer trochlear groove extend further proximally through the use of a longer anterior flange and allow for earlier capture of the patella in flexion, leading to a smoother articulation at earlier degrees of flexion[28,30]. Lateral tracking of the trochlear groove, facilitated by specific positioning of the femoral component, is also known to influence patellofemoral kinematics. Lateral placement of the femoral component enables earlier capture of the patella in addition to reducing patellar lateral sheer forces in early degrees of knee flexion[24,26,28]. Therefore a deeper and longer trochlear groove that tracks more laterally promotes stable and secure tracking of the patella thus producing a more natural and anatomic patellofemoral articulation[25,28,31]. In addition to improved patellar tracking, some of these design features may also facilitate a decrease in the rate of patellofemoral crepitance and patellar clunk syndrome[30]. Historically, femoral prosthesis designs did not adequately replicate the trochlear groove due in part to the lack of appropriate congruent angle. Native congruent angle is averaged to be 6 degrees with a standard deviation of 11 degrees. Data suggests that a congruent angle greater than 16 degrees was abnormal in 95% patients leading to a potential risk for malaligned result following TKA[32].
DESIGN FEATURES OF THE FEMORAL COMPONENT WHICH REDUCE PATELLOFEMORAL COMPLICATIONS/ ANTERIOR KNEE PAIN
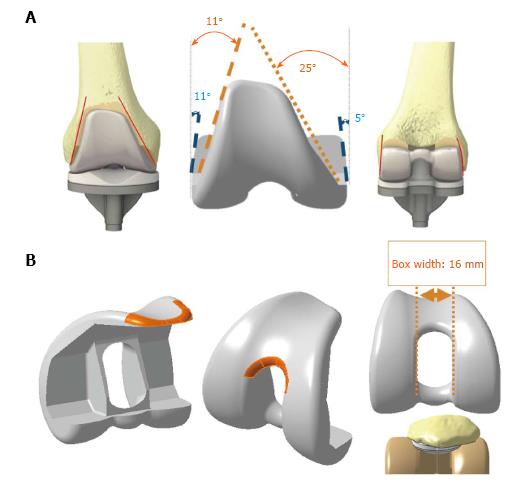
Anterior impingement (Figure
1)
Figure 1 Femoral component design showing.
A: Anterior and posterior narrowing to minimize disruption of soft tissue; B: Smoother transition radius.
Anterior impingement pain is an important potential consequence of TKA because it can cause further wear or even fracture of the post component[33,34]. It is determined by implant design, position of components in the sagittal plane, as well as the patient’s activities[33,34]. Previous studies have considered various modifications of the anterior flange of the femoral component in order to reduce anterior impingement and pain following TKA. A femoral component with a wider and thicker anterior flange can lead to stuffing of the patello-femoral joint leading to increased patellar ligament tension and thus increased patellofemoral contact forces[35]. This will eventually cause accelerated polyethylene wear and an overall higher risk of patellar complications[35]. It has been shown that a femoral component that incorporates a smoother anterior edge can decrease patellar impingement[36]. Therefore modification to the anterior flange may potentially reduce complications following TKA; however, a definitive conclusion remains unattainable, with the lack of clinical experimentation.
Gender prosthetic variations and considerations
Researchers have recently studied the morphologic variation of the native femur both within and between genders in order to identify an association between complications following primary TKA, including anterior knee pain, with mal-fitting femoral and tibial components. It has been demonstrated that women, on average, have smaller distal femurs as well as clinically significant variation in distal femur morphology compared to their male counterparts. One morphological variation in particular is a much larger aspect ratio (anterior/posterior to medial/lateral measurement) which places this patient population at a higher risk for medial/lateral femoral component overhang[35,37-41].
Different body morphologic types have a significant correlation with distal femoral morphology. Patients with short and wide morphotypes have a wider medial-to-lateral dimensions irrespective of gender, whereas patients with long and narrow morphotypes (ectomorph) have a narrower knee[39]. Therefore patients fitted with standard femoral components who possess a more ectomorph morphology may also experience, as in women, femoral component overhang, leading to potential pain and further complications following primary TKA. As a result, in an attempt to reduce complications following TKA, the prostheses-design is continuously undergoing modifications, including gender specific implants (Figure 2). Overhang of ≥ 3 mm in at least one of the predetermined zones of the femoral implant is associated with a 90% increase in the risk of patient-reported knee pain 2 years following TKA[42]. Gender specific femoral components have been demonstrated to minimize femoral overhang and thus post-surgical complications by providing a component that better matches the morphological differences of the female knee[37]. Therefore to minimize complications following TKA, surgeons must be aware of the various morphological differences in the native anatomy of the knee joint both between and within genders. By having prosthetics designed to better address this concern, medial to lateral overhang of the femoral component may be decreased leading to reduction in joint dysfunction and pain following primary TKA.
Figure 2 Femoral component design showing various sizing.
Ethnic prosthetic variations and considerations
In addition to gender, ethnicity also affects the morphologic type of both the femur and the tibia. Both male and female African Americans had increased anteroposterior height as compared to Caucasians and East Asians, while Caucasians had greater anteroposterior height as compared to East Asians[43]. There is a greater degree of curvature of the femoral condyles in Asian males and females[43]. With regards to the tibia, African American males had larger lateral anteroposterior height and smaller medial plateau anteroposterior height compared to Caucasian males, and larger mediolateral width and anteroposterior height as compared to Asian males[43]. Caucasian males and females had larger mediolateral width and anteroposterior height dimensions when compared to Asian males and females[43]. Despite known differences in the morphology of the femur and tibia among different ethnicities, prostheses are primarily made based on Caucasian morphology, which may contribute to an increase in patellofemoral complications, including anterior knee pain, following TKA in patients of different ethnicities[43].
Patellar clunk as related to the design of the femoral component
Patellar clunk syndrome is a complication that results in anterior knee pain and crepitus three to nine months following a TKA[44,45]. It is due to the formation of a fibrous nodule between the superior pole of the patellar and femoral component and the quadriceps tendon, which causes pain and displaces (clunks) with extension of the knee from approximately 30 to 45 degrees of flexion[46-48].
The etiology is multifactorial with the femoral component considered to be one of the contributors leading to the development of this syndrome[45,47]. Several design flaws of the femoral prosthesis have been proposed including: a sharp anterior edge at the superior aspect of the intercondylar box, a high intercondylar box ratio, an increased posterior condyle offset, and the use of smaller femoral components[45,47,48]. In addition, specific total knee systems, most notable posteriorly-stabilized TKA, have been associated with a higher incidence of patellar clunk[44,46,48].
While treatment for this syndrome is accomplished by either open or arthroscopic correction, prevention is always preferred[45]. Attempts of reducing this post-operative complication have included the following modifications to the femoral components: smoothing the transition from the notch to the anterior flange, raising the lateral flange, deepening the trochlear groove, and incorporating a more posterior intercondylar box[45-48]. To minimize the occurrence of patellar clunk syndrome, both manufactures and surgeons must continue to assess the advantages of altering the current designs of femoral components.
DESIGN FEATURES OF THE PATELLAR COMPONENT WHICH REDUCE PATELLOFEMORAL COMPLICATIONS/ANTERIOR KNEE PAIN
Since the inauguration of the dome patella, the incidence of anterior knee pain has dropped from 50% to 12%[48]. However, because patellar resurfacing has brought on its own complications, including component loosening, necrosis, and fracture, many studies have since been completed to determine the risks and benefits of employing patellar resurfacing in TKA[49,50]. One study demonstrated that while the overall rate of revision was similar, at 3.1% in resurfaced patellae and 4% in unresurfaced patellae, isolating anterior knee pain as the cause of revision garners different results: only 1% of resurfaced knees underwent revision due to anterior knee pain compared to 17% of unresurfaced knees[51]. Other studies reported similar numbers, with only 1%-5% of patients with a resurfaced patella experiencing chronic anterior knee pain compared to 10%-14% of patients with an unresurfaced patella[50,52]. However, other studies showed that there is no difference in anterior knee pain between resurfaced and unresurfaced patellae[53]. While many of the unresurfaced knees underwent secondary resurfacing due to anterior knee pain, revision surgery did not always resolve the pain[2]. Despite differing findings regarding the association of patellar resurfacing and decreased knee pain, many researchers suggest that surgeons employ at least selective resurfacing, based on factors such as patellar height and patient age[54].
Utilizing a patellar component that does not adequately match the preoperative anatomy of the knee is another mechanism potentially leading to a “stuffed” patellofemoral joint. Patellofemoral overstuffing is the result of an increase in the anteroposterior size of the patella, femur, or both, and may lead to anterior knee pain following TKA[55]. The anteroposterior size of the femur can be increased by the use of an oversized femoral component or underresection of the anterior femur[56]. The femoral component’s position in the anteroposterior plane has a crucial effect on patellofemoral biomechanics. If the size is incorrect or the component is improperly placed, the consequences could include increased patellar retinacular strain, patellar mal-tracking, or early polyethylene wear leading to premature joint failure, anterior knee pain, and decreased knee flexion[35,39,41,56-61]. The commonality of patellofemoral overstuffing is related to the design of the femoral component as well as the relatively limited availability of various component sizes[41,57,62]. An anterior buildup on the femur of 4-mm could result in as much as a 4-degree loss of passive knee flexion[41]. Therefore, it is critical that a large number of femoral component sizes be available at the time of surgery in order to prevent overstuffing of the patellofemoral joint. In addition, asymmetric patellar resurfacing can result in overstuffing. Patellar resection is performed free-hand and there are no standard guidelines or anatomic landmarks which should be used to guide the cuts, leading to an increased incidence of asymmetric resurfacing[55]. Asymmetric patellar resection can lead to bony impingement and patellar maltracking, both of which contribute to anterior knee pain post-operatively. A difference of 2 mm or greater in the thickness of the patella, as measured 15 mm from the medial and lateral edges, is considered asymmetric resection[55]. This occurs in up to 10% of procedures, and is more common in females, likely due to their smaller patellae, which makes resection technically more difficult[55]. A 15% increase in the combined anterior patellar displacement and anteroposterior femoral size is demonstrated to be associated with a significant increase in Knee Society Pain Score[57].
DESIGN CONSIDERATIONS AIMED AT RESTORING NORMAL TIBIOFEMORAL KINEMATICS IN POSTERIOR SUBSITUTING/STABAZLING TKA
The post-cam mechanism is often seen in posterior stabilized knee prostheses in order to mimic the posterior cruciate ligament (PCL), minimize tibial posterior displacement, and increase posterior femoral translation[63-65]. Distal placement of the femoral cam as well as a larger femoral posterior radius can increase the amount of posterior femoral movement; however, excessive anterior or posterior cam placement can cause femoral rollback impingement or excessive rollback, respectively[64]. Femoral condyle rollback is seen in normal knee kinematics during knee flexion but may be decreased in TKA[26] (Figure 3). It was found that up to 30% of different TKA designs rotate the opposite direction in axial rotation, which effect patellar kinematics and place a larger lateral vector on the patella in flexion[66]. Axial rotation patterns in knees after TKA are similar to those in normal knees, but the amount of rotation is less than in normal knees and is more variable due to prosthesis design and ligament abilities[66]. Constrained post-cam mechanisms are more susceptible to post wear or fracture, which can ultimately cause instability, impingement, pain and locking[63]. Constrained designs can be affected by local geometry, high contact loads, small contact areas, and abnormal extensor mechanism tracking[26]. These factors can influence whether patients develop patellofemoral complications such as anterior knee pain, patellar subluxation, abnormal polyethylene damage, and loosening[26]. Surface geometry may in fact be a stronger factor than the actual post-cam design when determining kinematic improvement[67]. Patellar tendon angle abnormalities can cause abnormal muscle loads and joint contact forces, whereas patellofemoral joint abnormalities can increase the patellar tendon angle[67].
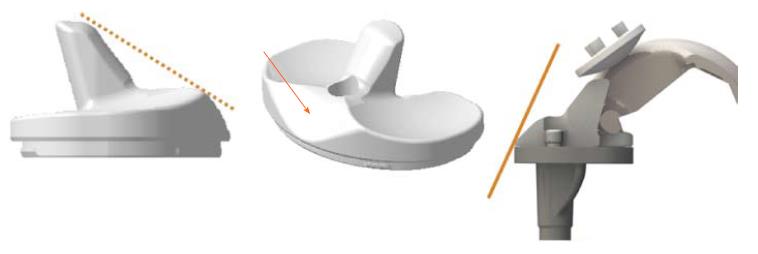
Figure 3 Femoral rollback and medial pivot.
FUTURE DIRECTIONS OF TKA DESIGN TO REDUCE PATTELOFEMORAL COMPLICATIONS/ANTERIOR KNEE PAIN FOLLOWING TKA
Design features of the polyethylene insert as it pertains to post-operative complications following primary TKA is an area that has not been well studied. However it is as important to identify and furthermore include the design of the polyethylene insert in an attempt to minimize anterior knee pain following TKA. The anterior edge of the polyethylene (PE) insert is a potential source of patellar tendon pain and tendonitis as the tendon is forced to glide against the sharp PE edge. Thus designing the PE insert to include a smooth anterior edge might decrease patellar tendon irritation (Figure 4). Furthermore, in PCL-substituting designs, anterior impingement has been related to tibial damage[33]. It has been demonstrated that a tibial post polyethylene insert can also cause anterior impingement through knee hyperextension when the post has been worn out[37]. Impingement of the patellar button from the polyethylene post is another potential source of complication in PCL-substituting TKA systems. Inserts which incorporate a posterior angulation to the polyethylene post can improve overall TKA kinematics by minimizing patellar button impingement.
Figure 4 Polyethylene component showing an inclination of 55° and anterior cut-out to avoid conflicts with extensor mechanism.
CONCLUSION
Anterior knee pain continues to be problematic following primary TKA procedures, oftentimes leading to prosthesis failure and revision surgery. While certain non-modifiable patient factors may lead to persistent post-operative pain, there are many modifiable elements including those related to the prosthesis and to surgical technique that also contribute. In particular, rotation and sizing of the tibial and femoral components, trochlear groove size and rotation, and patellar resurfacing have been associated with anterior knee pain post-TKA. These elements alternate knee biomechanics, either directly or through their effects on the Q-angle, which may result in excessive patello-femoral loads and abnormal patellar tracking. With specific contributors to post-surgical anterior knee pain being identified, further research should investigate improvements in both prostheses and surgical technique which would allow more accurate mimicking of native knee biomechanics, potentially leading to a decrease in anterior knee pain following primary TKA and a resultant decrease in revision procedures.
P- Reviewer: Drosos GI, Rothschild BM S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/