Published online Feb 18, 2026. doi: 10.5312/wjo.v17.i2.113197
Revised: September 21, 2025
Accepted: November 20, 2025
Published online: February 18, 2026
Processing time: 169 Days and 20.6 Hours
Musculoskeletal conditions are among the leading causes of disability worldwide, necessitating the development of effective, specialized treatment approaches. In response, orthopedic practice has evolved into three distinct specialties: Arthro
Core Tip: Arthroscopy, sports medicine, and regenerative orthopedics represent a triad of distinct orthopedic specialties, each defined by unique philosophies, patient profiles, and clinical expertise. Strategic, specialty-specific application - rather than forced integration - yields superior outcomes. Within the Indian healthcare landscape, the manuscript advocates for independent evolution, focused training, and supportive policy frameworks to enhance musculoskeletal care through precision techniques, functional restoration, and biologically driven healing.
- Citation: Jeyaraman M, Saketh ASPVS, Jeyaraman N, Ramasubramanian S, Nallakumarasamy A, Muthu S. Orthopedic trinity: Arthroscopy, sports medicine, and regenerative orthopedics. World J Orthop 2026; 17(2): 113197
- URL: https://www.wjgnet.com/2218-5836/full/v17/i2/113197.htm
- DOI: https://dx.doi.org/10.5312/wjo.v17.i2.113197
Musculoskeletal injuries and degenerative conditions are increasing globally, correlating with shifting demographics, aging populations, heightened sports participation, occupational changes, sedentary lifestyles, and trauma from road traffic accidents. These factors have contributed to a growing clinical and socioeconomic burden, with musculoskeletal conditions such as osteoarthritis, ligament injuries, and tendon disorders leading to significant morbidity and long-term disability[1]. According to global health estimates, low back pain and osteoarthritis rank among the top contributors to years lived with disability. In India, this burden is compounded by healthcare access disparities and high incidence of underreported injuries, particularly in peri-urban and rural populations[2,3].
Historically, orthopedic management centered around mechanical correction via open surgical interventions. While effective in many cases, these procedures often involved extensive soft tissue disruption, prolonged recovery, and higher complication rates. Over the past few decades, orthopedic care has undergone profound transformation, with three di
Each specialty has developed its own philosophical foundation, technical expertise, and clinical applications. Arthroscopy has revolutionized surgical precision through minimally invasive techniques, offering direct visualization and treatment of intra-articular pathology. Sports medicine encompasses the prevention, diagnosis, and management of musculoskeletal and sportsrelated conditions, including exercise prescription, rehabilitation, and interventional procedures such as diagnostic and therapeutic injections. Regenerative orthopedics has emerged as a biological approach, utilizing the body’s intrinsic healing mechanisms through cellular and molecular interventions[5-7].
The development of these distinct specialties is particularly relevant in the Indian context, where diverse healthcare needs require specialized approaches. Rather than viewing these as complementary components of an integrated system, recognition of their unique indications, methodologies, and outcomes allows for strategic application of the most appropriate specialty for each clinical scenario. This review explores the evolution, scope, and clinical utility of these three independent disciplines, evaluating their distinct advantages, specific applications, and future directions within the Indian orthopedic landscape. Our objective is to advocate for a specialty-specific framework that maintains the unique identity and clinical excellence of each discipline while ensuring optimal patient outcomes through appropriate specialty selection.
Arthroscopy, introduced in 1912 by Severin Nordentoft, represents the evolution of surgical intervention toward minimally invasive precision. The specialty gained clinical traction in the 1950s with Masaki Watanabe’s development of functional arthroscopes, and by the 1970s, fiber-optic systems revolutionized intra-articular visualization. This technological advancement established arthroscopy as a distinct surgical specialty focused on direct treatment of structural joint pathology[8].
The philosophical foundation of arthroscopy centers on mechanical correction through surgical intervention - the “fix what's broken” approach. Arthroscopic surgeons develop expertise in intra-articular anatomy, surgical technique, and technical precision. The specialty requires significant infrastructure investment, including specialized equipment, operating room facilities, and extensive surgical training[9,10].
In India, early adoption was limited by cost and access until the 1990s, when pioneers like Satvik N. Pai advanced training and dissemination. Today, arthroscopy allows precise treatment of meniscal tears, anterior cruciate ligament injuries, synovitis, and chondral defects through minimally invasive techniques. The specialty’s advantages include shorter recovery times, lower infection rates, and high patient satisfaction for appropriate structural lesions[11].
Innovations continue to enhance arthroscopic capabilities, including 4 kilopixels imaging systems, haptic feedback technology, and robotic assistance. However, high equipment costs and extensive skill requirements limit accessibility in resource-constrained settings. The specialty’s role remains specifically focused on structural pathology requiring surgical intervention[12,13].
Sports medicine emerged post-World War II as a distinct approach to managing injuries through functional rehabilitation rather than surgical intervention. Initially focused on military and professional athletes, the specialty has broadened to encompass comprehensive functional optimization across all populations. The philosophical foundation centers on functional restoration through rehabilitation - the “restore what’s lost” approach[14]. This specialty integrates multiple disciplines including biomechanics, exercise physiology, psychology, and rehabilitation medicine. Sports medicine practitioners develop expertise in movement analysis, exercise prescription, and performance optimization. The approach emphasizes non-operative management, functional assessment, and return-to-activity protocols[15-17].
Treatment modalities include manual therapy, proprioceptive re-education, therapeutic exercise, biomechanical analysis, and injury prevention strategies. The specialty utilizes diagnostic tools such as movement screens, strength testing, and functional assessments rather than surgical visualization. Rehabilitation protocols are evidence-based but tailored to individual functional deficits and activity goals[18].
In India, sports medicine gained momentum following the 2010 Commonwealth Games, prompting investments in athlete care infrastructure. Urban centers now house specialized sports injury clinics, though practitioner availability and insurance support remain limited. The specialty requires formal credentialing and standardized training programs to ensure consistent quality of care[19].
Regenerative orthopedics represents the newest approach to musculoskeletal care, building upon advances in tissue engineering and molecular biology. The specialty’s philosophical foundation centers on biological enhancement and healing modulation - the “heal what’s damaged” approach. Rather than mechanical correction or functional training, regenerative medicine seeks to stimulate endogenous repair mechanisms at the cellular level[20].
The specialty utilizes biological therapies including platelet-rich plasma (PRP), bone marrow aspirate concentrate (BMAC), and biomaterial scaffolds. PRP delivers concentrated growth factors (platelet-derived growth factor, transforming growth factor-β) to promote healing in tendinopathies and mild osteoarthritis[21]. BMAC provides mesenchymal stem cells and cytokines for managing osteochondral lesions and early osteoarthritis[22]. Biomaterial scaffolds aid in structural support and cell migration[23].
Practitioners require expertise in cell biology, molecular medicine, and laboratory techniques. The specialty demands understanding of inflammatory cascades, tissue regeneration, and cellular responses. Treatment protocols focus on biological optimization rather than mechanical or functional intervention.
In India, PRP has gained widespread adoption due to its relative simplicity and cost-effectiveness, while BMAC remains restricted to advanced centers. However, concerns about unregulated stem cell use highlight the need for stricter regulatory oversight and standardized protocols. The specialty’s success depends heavily on proper patient selection, biological preparation, and understanding of healing mechanisms[24,25].
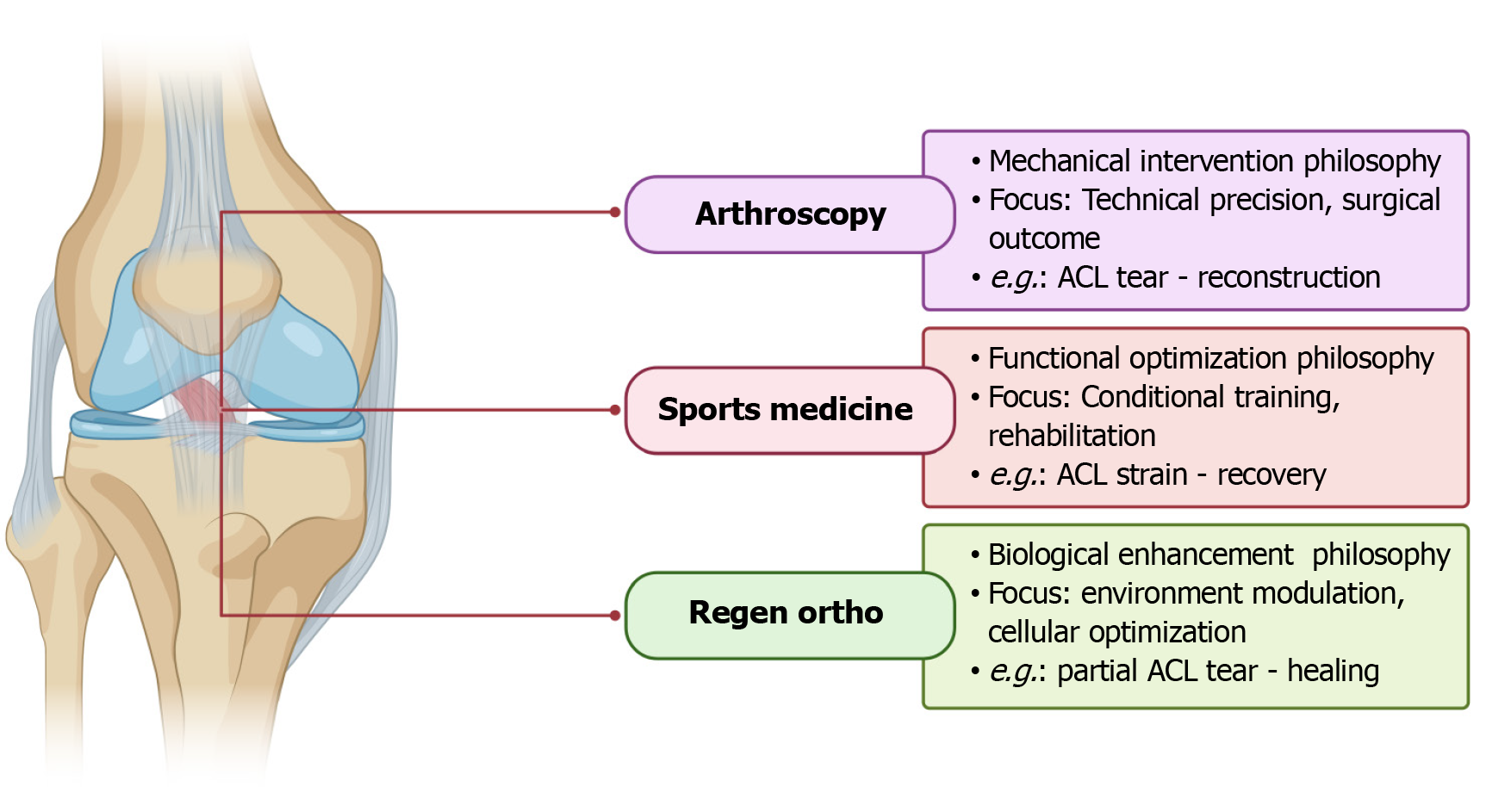
The three specialties operate from fundamentally different philosophical foundations that shape their approach to patient care. Arthroscopy embodies a pure mechanical intervention philosophy - identifying structural problems and correcting them through surgical means. This approach assumes that anatomical restoration leads to functional improvement, focusing on technical precision and surgical outcomes[26].
Sports medicine operates from a functional optimization philosophy, addressing movement dysfunction and performance limitations through rehabilitation. This approach emphasizes the body’s adaptive capacity and seeks to restore function through training and conditioning, regardless of underlying structural variations[27].
Regenerative orthopedics follows a biological enhancement philosophy - modulating healing processes at the cellular level to promote tissue repair. This approach recognizes that many musculoskeletal conditions result from failed healing responses and seeks to optimize the biological environment for recovery[28].
These philosophical differences create distinct treatment paradigms that are not interchangeable. Each specialty views the same pathology through different lenses and applies entirely different treatment strategies based on their unique theoretical frameworks as shown in Figure 1.
Each specialty serves fundamentally different patient populations with specific characteristics and needs. Arthroscopy primarily treats patients with acute structural injuries, failed conservative management, or mechanical symptoms requiring surgical intervention. Ideal candidates include young athletes with ligament ruptures, patients with locked joints, or individuals with definitive structural lesions on imaging[29].
Sports medicine serves performance athletes, patients with chronic pain, and individuals requiring injury prevention strategies. The specialty focuses on patients with functional deficits, movement dysfunction, or those seeking per
Regenerative orthopedics targets patients with early degenerative disease, chronic tendinopathies, or those seeking biological healing enhancement. The specialty serves patients with intact joint architecture but symptomatic impairment, individuals who are poor surgical candidates, or those preferring non-operative interventions[31].
These patient populations have different expectations, treatment timelines, and outcome measures. Surgical patients expect definitive correction of structural problems, rehabilitation patients focus on functional improvement, and regenerative patients seek biological healing and symptom modification[32].
Each specialty demands distinct technical skills and knowledge bases that require specialized training. Arthroscopic surgeons must master surgical techniques, intra-articular anatomy, and technical precision. Training involves extensive surgical apprenticeship, procedural quotas, and competency-based assessment. The learning curve is steep and requires significant investment in equipment and infrastructure[33].
Sports medicine practitioners require expertise in biomechanics, exercise physiology, and movement analysis. Training emphasizes functional assessment, exercise prescription, and rehabilitation protocols. The specialty demands understanding of human performance, injury mechanisms, and return-to-activity principles[30,34].
Regenerative medicine specialists need expertise in cell biology, molecular medicine, and laboratory techniques. Training focuses on biological preparation methods, cellular mechanisms, and tissue engineering principles. The specialty requires understanding of inflammatory cascades, growth factors, and regenerative processes[35].
These expertise requirements are not transferable between specialties. A skilled arthroscopic surgeon cannot automatically perform effective sports rehabilitation, just as a sports medicine practitioner cannot safely perform arthroscopic procedures. Each specialty requires dedicated training and ongoing education within its specific domain (Table 1). This comparative analysis demonstrates that while all three specialties address musculoskeletal conditions, they do so through entirely different approaches, requiring distinct expertise and serving different patient populations.
| Parameter | Arthroscopy | Sports medicine | Regenerative orthopedics |
| Core approach[14] | Surgical, mechanical correction | Conservative, functional optimization | Biological repair and modulation |
| Primary setting[14] | Operating room | Clinic/rehabilitation center | Outpatient or laboratory |
| Training background[10] | Surgical fellowship | Rehabilitation medicine | Molecular biology |
| Intervention tools[22] | Arthroscope, surgical instruments | Exercise equipment, assessment tools | PRP, BMAC, scaffolds |
| Common indications[22] | Meniscal tear, ACL rupture | Chronic pain, movement dysfunction | Early OA, partial tendon tears |
| Success metrics[10] | Structural repair | Functional scores | Biological markers |
| Invasiveness[14] | Minimally invasive | Non-invasive | Minimally invasive |
| Time to benefit[14] | Immediate | Gradual | Delayed |
| Failure management[22] | Revision surgery | Modified protocols | Alternative biologics |
| Cost considerations[14] | High equipment and OR costs | Moderate, ongoing therapy | High processing and materials |
| Evidence strength[22] | Strong for structural lesions | Moderate to strong | Emerging, variable |
| Accessibility (India)[34] | Limited to urban centers | Variable, developing | Growing, unregulated |
Optimal musculoskeletal care requires strategic selection of the most appropriate specialty based on specific clinical criteria. Rather than attempting to integrate multiple approaches, clinicians should follow clear decision trees that direct patients to the specialty best suited for their particular condition and circumstances[36].
Patients with structural damage who are suitable surgical candidates benefit most from arthroscopic intervention. These individuals present with imaging-confirmed structural lesions such as meniscal tears, ligament ruptures, or loose bodies, often accompanied by mechanical symptoms including locking, catching, or instability. The ideal arthroscopic candidate has failed conservative management, demonstrates surgical fitness with appropriate consent, and maintains realistic expectations for structural correction outcomes[37,38].
Patients with functional deficits but intact structural anatomy are optimal candidates for sports medicine approaches. These individuals typically show normal or minimal structural findings on imaging but experience functional limitations affecting daily activities or performance. They demonstrate movement dysfunction or biomechanical abnormalities, possess motivation for active rehabilitation participation, and maintain realistic expectations for functional improvement through conservative management[38,39].
Patients with degenerative processes who retain biological healing potential may benefit from regenerative medicine approaches[40]. These individuals present with early-stage degenerative disease or chronic tendinopathies, often with contraindications to surgery or patient preference for non-operative care. Successful regenerative candidates maintain realistic expectations for biological healing and possess adequate financial resources for treatments that may not be covered by insurance[41].
These cases demonstrate the distinct applications of each specialty, where the chosen approach directly addresses the underlying pathophysiology through specialty-specific mechanisms.
A 38-year-old construction worker sustained a knee injury during a fall. Clinical examination revealed mechanical symptoms with knee locking and the inability to fully extend. Magnetic resonance imaging confirmed a bucket-handle meniscal tear with displaced fragment. The patient was otherwise healthy with normal function prior to injury.
Arthroscopic management: The patient underwent arthroscopic partial meniscectomy with removal of the displaced fragment. The procedure was performed under regional anesthesia with same-day discharge. Post-operative care included wound management, early range of motion, and gradual return to activities. The patient returned to full work duties at 4 weeks with complete resolution of mechanical symptoms.
Outcome: Excellent structural correction with restoration of normal knee mechanics. The surgical approach directly addressed the mechanical problem without need for additional interventions[42].
A 45-year-old recreational runner presented with chronic ankle instability following multiple sprains over 2 years. Clinical examination revealed functional instability with negative anterior drawer test and normal imaging studies. The patient demonstrated poor proprioception and weakness in ankle stabilizing muscles.
Sports medicine management: The patient underwent comprehensive functional assessment including balance testing, strength evaluation, and movement analysis. Treatment included proprioceptive training, ankle strengthening exercises, and running technique modification. A 12-week progressive program addressed neuromuscular control and movement patterns.
Outcome: Significant improvement in functional stability and return to recreational running without recurrent sprains. The rehabilitation approach addressed the functional deficits without surgical intervention.
A 52-year-old office worker presented with bilateral knee pain and morning stiffness consistent with early osteoarthritis. Radiographs revealed Kellgren-Lawrence grade 2 changes with joint space narrowing. The patient preferred non-surgical management and maintains good functional capacity.
Regenerative medicine management: The patient received a series of three intra-articular PRP injections administered at 4-week intervals. Each injection was prepared using standardized protocol with platelet concentration monitoring. The patient continued normal activities with activity modification during treatment.
Outcome: Moderate improvement in pain and stiffness with functional improvement maintained at 6-month follow-up. The biological approach addressed the degenerative process without surgical intervention.
Arthroscopic training requires extensive surgical apprenticeship following orthopedic surgery residency. Fellowship programs typically span 12 months with structured curriculum focused on technical skills development. Trainees must master arthroscopic anatomy and spatial orientation, develop proficiency in portal placement and instrumentation, and acquire expertise in visualization techniques and camera navigation. The training emphasizes surgical technique refinement and complication management across various joint systems.
Procedural requirements include minimum case volumes for knee, shoulder, hip, and ankle procedures, with competency-based assessment and skill verification throughout the training period. Trainees must demonstrate proficiency in surgical outcome tracking and quality metrics, while completing a research project that contributes to the specialty’s evidence base. The training demands access to modern arthroscopic equipment and dedicated operating room facilities, with experienced surgical mentors providing high-volume case exposure essential for skill development[33].
Sports medicine training emphasizes functional assessment and rehabilitation expertise through comprehensive educational programs. Training pathways focus on developing core competencies in movement analysis and biomechanical assessment, requiring practitioners to understand exercise physiology and training principles. The curriculum emphasizes injury prevention and risk factor modification, while developing expertise in return-to-activity protocols and performance optimization strategies across diverse populations[30].
Clinical training encompasses functional assessment techniques and rehabilitation protocol development, with emphasis on injectable procedures and point-of-care ultrasound applications[16]. Trainees must develop skills in interdisciplinary team collaboration and outcome measurement techniques. Certification requirements include formal fellowship training or equivalent experience, with competency examination and skill verification processes. The specialty demands continuing education requirements and professional society membership to maintain current knowledge and clinical standards.
Regenerative medicine training focuses on biological principles and laboratory techniques essential for cellular therapy applications. The scientific foundation requires comprehensive understanding of cell biology and tissue engineering, with emphasis on growth factor biology and signaling pathways. Trainees must master inflammatory cascade and healing mechanisms, while developing expertise in biomaterial science and scaffold design[23]. The curriculum includes regulatory requirements and quality control procedures essential for safe clinical practice.
Clinical applications training covers patient selection and indication algorithms, with emphasis on biological preparation techniques and injection procedures using image guidance. Trainees must develop competency in outcome assessment and tracking methodologies, while understanding adverse event management protocols. Laboratory training encompasses cell culture techniques and biological product preparation, with emphasis on quality control and standardization procedures[41]. The program includes research methodology and clinical trials training, ensuring practitioners understand regulatory compliance requirements for this rapidly evolving field.
Each specialty requires dedicated training infrastructure and experienced mentors within that specific domain. Cross-training between specialties is not sufficient for competency development.
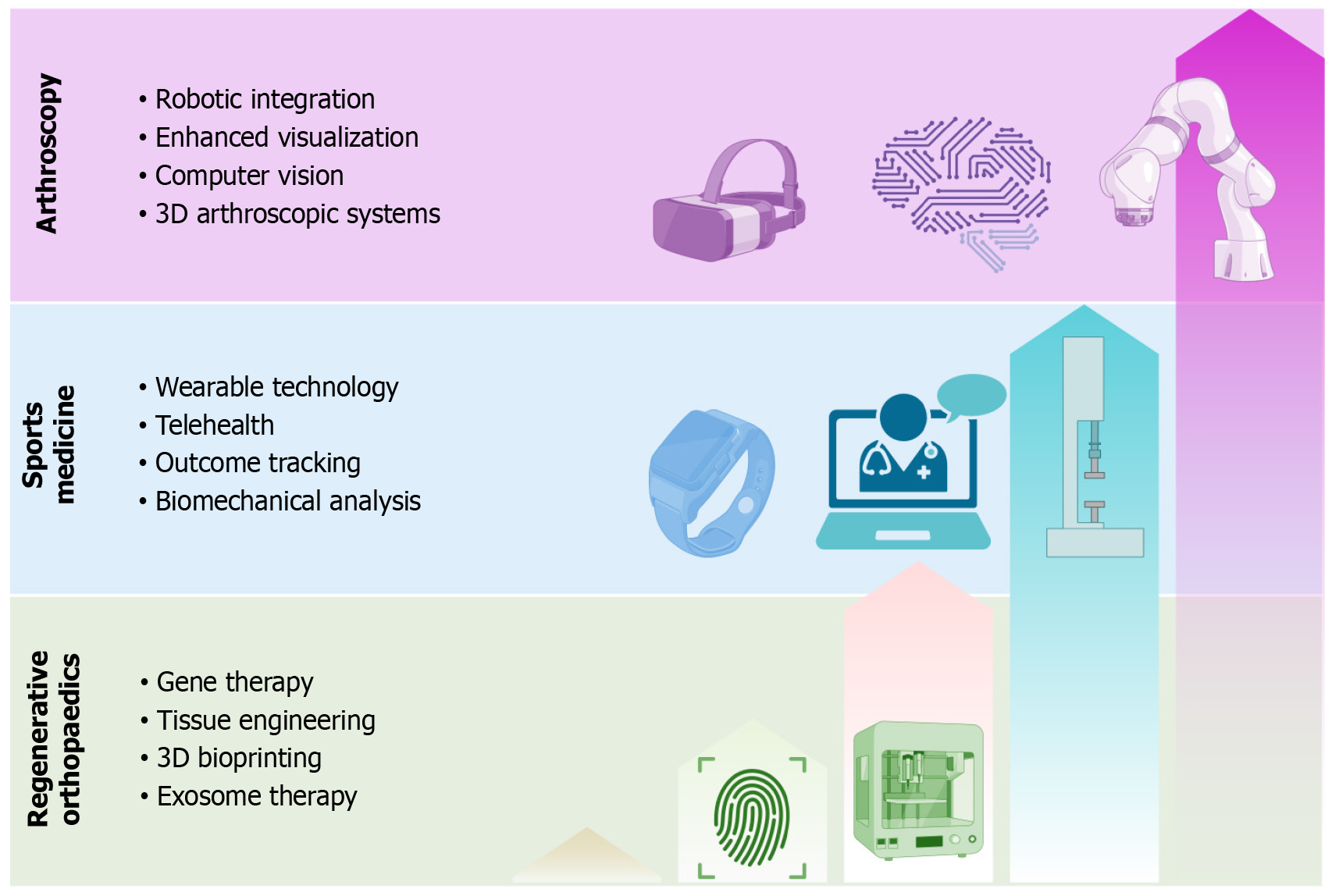
The future of arthroscopic surgery lies in technological enhancement of surgical precision and outcomes through multiple innovative approaches. Robotic surgery integration represents a significant advancement, incorporating haptic feedback systems for enhanced tactile sensation and robotic-assisted instrumentation for improved precision. These systems include automated suturing and knot-tying capabilities, along with real-time surgical navigation and guidance systems that enhance surgical accuracy and reduce procedural complications.
Enhanced visualization technologies continue to revolutionize arthroscopic procedures through 4 kilopixels and 8 kilopixels ultra-high-definition imaging systems that provide unprecedented detail of intra-articular structures. Augmented reality overlay with anatomical mapping allows surgeons to visualize structures beyond direct vision, while fluorescence imaging for tissue viability assessment helps determine optimal treatment strategies. Three-dimensional arthroscopic systems provide depth perception that enhances surgical precision and reduces learning curve requirements[26].
Artificial intelligence applications are transforming arthroscopic practice through computer vision systems for anatomical recognition and predictive analytics for surgical outcomes. These technologies include automated lesion detection and classification systems, along with surgical skill assessment and training platforms that enhance educational effectiveness and ensure consistent competency development across training programs[33].
Sports medicine advancement focuses on digital health technologies and performance optimization through comprehensive technological integration. Wearable technology integration enables real-time biomechanical analysis during activity, providing continuous monitoring of movement patterns and injury risk prediction algorithms. These systems deliver performance optimization feedback that allows athletes and patients to modify activities in real-time, reducing injury risk and enhancing performance outcomes[18].
Telehealth and remote monitoring capabilities have revolutionized sports medicine practice through virtual rehabilitation platforms that extend clinical care beyond traditional boundaries. Remote exercise prescription and monitoring systems enable practitioners to guide rehabilitation programs from distance, while digital coaching and feedback systems provide continuous support throughout recovery. Outcome tracking and progress assessment tools ensure that patients receive appropriate modifications to their treatment programs based on objective data[36].
Advanced biomechanical analysis technologies provide unprecedented insight into movement dysfunction and performance limitations. Markerless motion capture systems eliminate the need for cumbersome sensor placement while providing detailed movement analysis. Force plate integration and analysis reveal ground reaction forces and weight distribution patterns, while muscle activation patterns and timing assessments identify neuromuscular dysfunction[15]. Movement quality assessment tools provide objective measures of functional improvement throughout the rehabilitation process.
Regenerative medicine advancement centers on enhanced biological therapies that expand treatment capabilities beyond current limitations. Gene therapy applications represent the next frontier, incorporating targeted gene delivery systems for tissue repair and growth factor gene expression enhancement. Anti-inflammatory gene therapy approaches address chronic inflammatory conditions at their source, while personalized genetic medicine approaches tailor treatments to individual genetic profiles and healing capabilities.
Tissue engineering advancement continues to revolutionize regenerative capabilities through three-dimensions bioprinting of tissue constructs that can replace damaged structures[20]. Scaffold-free tissue engineering eliminates foreign material complications while promoting natural tissue regeneration. Organoid development for drug testing accelerates therapeutic development, while personalized tissue replacement options provide patient-specific solutions for complex defects.
Advanced cell therapies expand beyond traditional approaches through induced pluripotent stem cell applications that overcome ethical and availability limitations. Exosome therapy for tissue repair harnesses cellular communication mechanisms to promote healing without direct cell transplantation[43]. Cell-free approaches to regeneration reduce complications associated with cellular therapies, while combination biological therapies optimize multiple healing pathways simultaneously for enhanced therapeutic outcomes[28]. Each specialty’s technological advancement follows distinct pathways aligned with their core principles and clinical applications. The advancements in these three fields are highlighted in Figure 2.
Arthroscopic surgery requires comprehensive regulatory oversight focusing on surgical safety and quality through multiple regulatory mechanisms. Facility standards must address operating room equipment specifications and sterile processing requirements, while ensuring adequate infection control measures and emergency response capabilities. Quality assurance programs provide ongoing monitoring of surgical outcomes and safety metrics, ensuring consistent standards across all arthroscopic facilities[12].
Surgeon credentialing encompasses board certification requirements and continuing medical education mandates that ensure practitioners maintain current knowledge and skills. Peer review and outcome monitoring systems provide ongoing assessment of surgical performance, while competency maintenance standards ensure that arthroscopic surgeons continue to meet professional requirements throughout their careers. Quality metrics focus on surgical site infection rates, reoperation rates and indications, patient satisfaction scores, and functional outcome measures that provide objective assessment of surgical success.
Sports medicine requires standardized credentialing and scope of practice definition through comprehensive regulatory frameworks. Professional certification must be established through national certification boards that provide stan
Clinic standards address equipment and facility requirements necessary for safe and effective sports medicine practice, while ensuring adequate staff training and certification. Safety protocols and emergency procedures must be established and regularly updated, with appropriate insurance and liability coverage protecting both practitioners and patients. Quality assurance encompasses outcome tracking and reporting systems, patient safety monitoring protocols, professional development requirements, and peer review processes that ensure consistent quality across all sports medicine practices[30].
Regenerative medicine requires strict regulatory control due to biological product complexity and potential safety concerns. Product regulation encompasses biological product classification and approval processes, manufacturing standards and quality control requirements, batch testing and traceability systems, and adverse event reporting mechanisms. These regulations ensure that biological products meet safety and efficacy standards before clinical use.
Clinical practice standards address informed consent requirements that ensure patients understand treatment risks and benefits, patient selection criteria that identify appropriate candidates, treatment protocols and standardization that ensure consistent care delivery, and outcome monitoring and follow-up requirements that track long-term results. Research oversight includes clinical trial design and approval processes, ethics review and patient protection measures, data collection and analysis standards, and publication and dissemination requirements that ensure scientific integrity in regenerative medicine research[41].
In India the three emerging disciplines, namely, arthroscopy, sports medicine, and regenerative medicine, show distinct patterns in availability, infrastructure needs, and economic implications. Arthroscopy services remain centered in metropolitan and corporate hospitals. Trained surgeons are increasing in number but their reach is confined largely to tier-1 cities. Sports medicine is in its infancy. Formal training programs are sparse and credentialing varies by institution. Rehabilitation services often fall outside standard insurance schemes. Regenerative medicine has seen rapid expansion but regulatory clarity and quality assurance lag behind. Costs for all three specialties pose barriers to widespread adoption. Insurance programs cover arthroscopy for established indications. Sports medicine and regenerative treatments require new policy frameworks to address uncertain long-term outcomes.
Infrastructure demands differ sharply. Arthroscopy centers need dedicated theatres, high-definition imaging suites and specialized post-operative rehabilitation units. Sports medicine clinics depend on functional assessment tools, biomechanical labs and multidisciplinary teams. Regenerative medicine facilities must incorporate clean rooms, controlled-environment laboratories and stringent quality-control processes. Integration into the health system must align each specialty with appropriate levels of care. Complex arthroscopic procedures fit tertiary hospitals. Sports injury management suits secondary-level facilities. Regenerative therapies demand specialized centers that combine clinical practice with ongoing research (Table 2).
| Specialty | Availability[34] | Infrastructure requirements[24] | Economic model[25] | Insurance coverage[37] | System integration[17] |
| Arthroscopy | Urban and corporate hospitals; scarce in smaller cities | Dedicated ORs; HD imaging; surgical teams; post-op rehab | High initial cost; predictable outcomes | Established for approved procedures | Tertiary care for complex surgeries |
| Sports medicine | Major sports academies; few formal training sites | Functional assessment tools; movement analysis; exercise therapy facilities | Moderate cost; long-term gains | Limited; requires policy development | Secondary care for injury management |
| Regenerative medicine | Growing presence; inconsistent standards | Laboratory prep; clean rooms; storage/handling; R&D infrastructure | Variable cost; outcome uncertainty | Minimal; pending robust efficacy evidence | Specialized research-clinical centers |
Arthroscopic surgery faces significant technical limitations that affect its accessibility and effectiveness. The steep learning curve and extensive skill requirements create barriers for surgeon training and competency development. Equipment cost and maintenance complexity limit facility capabilities, while the procedure’s limited applicability to degenerative conditions restricts its therapeutic scope. Complication risks and revision surgery rates remain concerns that affect patient outcomes and healthcare costs.
Access and equity issues compound these technical challenges, creating disparities in arthroscopic care availability. Urban-rural disparities in facility and surgeon availability limit access for patients in underserved areas. High-cost barriers prevent many patients from receiving arthroscopic treatment, while limited insurance coverage for some procedures creates financial obstacles. Surgeon distribution and training capacity limitations affect the specialty’s ability to meet growing demand for arthroscopic services.
Sports medicine faces significant professional development challenges that limit its growth and effectiveness. The lack of standardized training programs creates inconsistency in practitioner preparation and competency levels. Unclear scope of practice definitions lead to confusion about professional boundaries and capabilities. Limited career advancement pathways discourage practitioners from entering the field, while insufficient research and evidence base weakens the specialty’s scientific foundation.
Healthcare system integration challenges further complicate sports medicine development. Poor integration with medical education limits awareness and understanding of the specialty’s capabilities. Limited recognition by healthcare policy makers affects funding and resource allocation. Inadequate funding for rehabilitation services restricts treatment options and accessibility. The lack of interdisciplinary collaboration reduces the effectiveness of care delivery and limits the specialty’s impact on patient outcomes.
Regenerative medicine faces significant scientific and clinical challenges that affect its credibility and effectiveness. The limited high-quality evidence base creates uncertainty about treatment efficacy and optimal protocols. Variability in preparation and delivery methods leads to inconsistent outcomes and difficulty in comparing results across studies. Unclear mechanisms of action complicate treatment selection and protocol development, while heterogeneous patient responses make outcome prediction challenging.
Regulatory and ethical challenges compound these scientific limitations and affect patient safety. Inadequate regulatory oversight allows unproven treatments to be offered without appropriate safety monitoring. Unproven claims and marketing issues mislead patients about treatment effectiveness and safety. Patient safety concerns arise from inadequate adverse event reporting systems, while ethical concerns about unregulated practices threaten the specialty’s credibility and patient trust.
Each specialty requires targeted development approaches that address their unique challenges and opportunities. Arthroscopy advancement focuses on expanding training programs to tier-2 cities, developing cost-effective equipment and techniques, establishing outcome registries and quality metrics, and creating sustainable financing models that improve accessibility while maintaining quality standards[33].
Sports medicine growth emphasizes establishing formal training and certification programs, developing evidence-based practice guidelines, creating integrated care delivery models, and expanding insurance coverage for rehabilitation services. These initiatives address the specialty’s need for professional recognition and systematic development.
Regenerative medicine maturation requires implementing comprehensive regulatory frameworks, establishing standardized protocols and quality control measures, developing robust clinical trial infrastructure, and creating ethical guidelines and patient protection mechanisms. These measures address the specialty’s need for scientific validation and safety assurance.
Effective development of these three specialties requires comprehensive policy initiatives that recognize their distinct needs and characteristics. Education and training policies should establish separate, specialized training institutes for each field, create distinct certification pathways and credentialing systems, develop specialty-specific research programs, and implement continuing education requirements that maintain current knowledge within each discipline.
Healthcare system integration policies must recognize each specialty as a distinct medical discipline with unique capabilities and limitations. Development of separate insurance coverage categories ensures appropriate reimbursement for specialty-specific services. Creating specialty-specific quality metrics allows for meaningful performance assessment, while establishing independent regulatory pathways ensures appropriate oversight for each field’s unique requirements.
Research and development policies should fund specialty-specific research initiatives that address each field’s particular challenges and opportunities. Establishing outcome registries for each field enables evidence-based practice development. Creating evidence-based practice guidelines ensures consistent, high-quality care delivery, while establishing innovation centers for each specialty promotes technological advancement and clinical improvement within their respective domains[44,45].
Arthroscopy, sports medicine, and regenerative orthopedics represent three distinct and equally valuable approaches to musculoskeletal care that should be recognized as independent specialties rather than integrated components. Each field has developed unique philosophical foundations, technical expertise, and clinical applications that serve different patient populations with specific needs and expectations. Arthroscopy provides surgical precision for structural pathology through minimally invasive techniques, Sports Medicine offers functional optimization through evidence-based rehabilitation, and regenerative medicine delivers biological healing through cellular intervention. These approaches require distinct training pathways, specialized infrastructure, and independent regulatory frameworks to maintain their effectiveness and safety. The future success of orthopedic care depends on strategic application of the most appropriate spe
| 1. | Blyth FM, Briggs AM, Schneider CH, Hoy DG, March LM. The Global Burden of Musculoskeletal Pain-Where to From Here? Am J Public Health. 2019;109:35-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 302] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 2. | GBD 2021 Other Musculoskeletal Disorders Collaborators. Global, regional, and national burden of other musculoskeletal disorders, 1990-2020, and projections to 2050: a systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023;5:e670-e682. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 124] [Cited by in RCA: 206] [Article Influence: 68.7] [Reference Citation Analysis (0)] |
| 3. | GBD 2021 Low Back Pain Collaborators. Global, regional, and national burden of low back pain, 1990-2020, its attributable risk factors, and projections to 2050: a systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023;5:e316-e329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 567] [Cited by in RCA: 889] [Article Influence: 296.3] [Reference Citation Analysis (0)] |
| 4. | Liang W, Zhou C, Bai J, Zhang H, Jiang B, Wang J, Fu L, Long H, Huang X, Zhao J, Zhu H. Current advancements in therapeutic approaches in orthopedic surgery: a review of recent trends. Front Bioeng Biotechnol. 2024;12:1328997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 27] [Reference Citation Analysis (0)] |
| 5. | Tao Y, Lv X. Research hotspots and trends on sports medicine of athletes: A scientometric analysis from 2003 to 2023. Medicine (Baltimore). 2023;102:e35254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Treuting R. Minimally invasive orthopedic surgery: arthroscopy. Ochsner J. 2000;2:158-163. [PubMed] |
| 7. | Ibrahim A, Gupton M, Schroeder F. Regenerative Medicine in Orthopedic Surgery: Expanding Our Toolbox. Cureus. 2024;16:e68487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 8. | Solheim E, Grøntvedt T, Mølster A, Uppheim G, Gay C, Dimmen S. Milestones in the early history of arthroscopy. J Orthop Rep. 2022;1:100060. [DOI] [Full Text] |
| 9. | Jackson RW. Arthroscopy: the catalyst for minimally invasive surgery. An R Acad Nac Med (Madr). 2004;121:257-260. [PubMed] |
| 10. | Kim SJ, Kim HJ. High portal: Practical philosophy for positioning portals in knee arthroscopy. Arthroscopy. 2001;17:333-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Rajan DV, Keyi MA, Challumuri N, Sahanand SK. History of arthroscopy in India: Origins and evolution. J Arthrosc Surg Sports Med. 2020;1:5-10. [DOI] [Full Text] |
| 12. | Pai SN. Arthroscopy in India Through the Medicolegal Lens: A Comprehensive Review. Indian J Orthop. 2023;57:1984-1992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Riad A, Hadid M, Elomri A, Al-Ansari A, Rejeb MA, Qaraqe M, Dakua SP, Jaber AR, Al-Ansari A, Aboumarzouk OM, El Omri A. Advancements and challenges in robotic surgery: A holistic examination of operational dynamics and future directions. Surg Pract Sci. 2025;22:100294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 14. | Rehan H, Geetha Kumari D, Zameer A, Sambreen Z. The History of Sports Medicine. J Sports Med Ther. 2025;10:025-026. [DOI] [Full Text] |
| 15. | Elliott B. Biomechanics: an integral part of sport science and sport medicine. J Sci Med Sport. 1999;2:299-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Pate RR, Durstine JL. Exercise physiology and its role in clinical sports medicine. South Med J. 2004;97:881-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Ahern DK, Lohr BA. Psychosocial factors in sports injury rehabilitation. Clin Sports Med. 1997;16:755-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Hübscher M, Zech A, Pfeifer K, Hänsel F, Vogt L, Banzer W. Neuromuscular training for sports injury prevention: a systematic review. Med Sci Sports Exerc. 2010;42:413-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 282] [Cited by in RCA: 230] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 19. | Henehan MJ, Cappellari AM, Stromwall AE, Donaldson NG. Sports medicine training and practice opportunities for emergency physicians. J Emerg Med. 2013;45:619-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Ivkovic A, Marijanovic I, Hudetz D, Porter RM, Pecina M, Evans CH. Regenerative medicine and tissue engineering in orthopaedic surgery. Front Biosci (Elite Ed). 2011;3:923-944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 21. | Louis ML, Magalon J, Jouve E, Bornet CE, Mattei JC, Chagnaud C, Rochwerger A, Veran J, Sabatier F. Growth Factors Levels Determine Efficacy of Platelets Rich Plasma Injection in Knee Osteoarthritis: A Randomized Double Blind Noninferiority Trial Compared With Viscosupplementation. Arthroscopy. 2018;34:1530-1540.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 96] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 22. | Waterman BR, Burns TC, McCriskin B, Kilcoyne K, Cameron KL, Owens BD. Outcomes after bankart repair in a military population: predictors for surgical revision and long-term disability. Arthroscopy. 2014;30:172-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 23. | Jafari M, Paknejad Z, Rad MR, Motamedian SR, Eghbal MJ, Nadjmi N, Khojasteh A. Polymeric scaffolds in tissue engineering: a literature review. J Biomed Mater Res B Appl Biomater. 2017;105:431-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 183] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 24. | Ferozkhan S, Sivakumar AP, Elumalai SB, Jeyaraman N, Jeyaraman M. Core Decompression with Bone Marrow Aspirate Concentrate Implantation in Osteonecrosis of the Femoral Head with a Minimum of 2-year Follow-up - A Pilot Study. J Orthop Case Rep. 2024;14:192-199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 25. | Marei HE. Stem cell therapy: a revolutionary cure or a pandora's box. Stem Cell Res Ther. 2025;16:255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 26. | Huri G, Popescu IA, Rinaldi VG, Marcheggiani Muccioli GM. The Evolution of Arthroscopic Shoulder Surgery: Current Trends and Future Perspectives. J Clin Med. 2025;14:2405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 27. | McCrory P. What is sports and exercise medicine? Br J Sports Med. 2006;40:955-957. [PubMed] |
| 28. | Das S, Thakur A, Datta A, Sahoo A, Bandyopadhyay S, Sah AK. Advances in Regenerative Medicine for Orthopedic Injuries: A Comprehensive Review. Cureus. 2025;17:e79860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 29. | Smeets A, Ghafelzadeh Ahwaz F, Bogaerts S, Berger P, Peers K. Comparison of immediate versus optional delayed surgical repair for treatment of acute anterior cruciate ligament injury through a parallel, multicentric, pragmatic randomized controlled trial - IODA trial. BMC Sports Sci Med Rehabil. 2024;16:22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 30. | Frank RM, Bradsell H, Thompson SR. What's New in Sports Medicine. J Bone Joint Surg Am. 2021;103:653-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 31. | Murray IR, Safran MR, Laprade RF. Biologics in orthopaedics. Bone Joint 360. 2018;7:2-8. [DOI] [Full Text] |
| 32. | Peck E, Ely E. Successful treatment of de Quervain tenosynovitis with ultrasound-guided percutaneous needle tenotomy and platelet-rich plasma injection: a case presentation. PM R. 2013;5:438-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 33. | Rashed S, Ahrens PM, Maruthainar N, Garlick N, Saeed MZ. The Role of Arthroscopic Simulation in Teaching Surgical Skills: A Systematic Review of the Literature. JBJS Rev. 2018;6:e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 34. | Kumar R. Building a healthy nation: A white paper on Olympic sports and the Indian education system. J Family Med Prim Care. 2024;13:2805-2818. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 35. | Park S, Rahaman KA, Kim YC, Jeon H, Han HS. Fostering tissue engineering and regenerative medicine to treat musculoskeletal disorders in bone and muscle. Bioact Mater. 2024;40:345-365. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 23] [Reference Citation Analysis (0)] |
| 36. | Yung KK, Ardern CL, Serpiello FR, Robertson S. A Framework for Clinicians to Improve the Decision-Making Process in Return to Sport. Sports Med Open. 2022;8:52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 37. | Siemieniuk RAC, Harris IA, Agoritsas T, Poolman RW, Brignardello-Petersen R, Van de Velde S, Buchbinder R, Englund M, Lytvyn L, Quinlan C, Helsingen L, Knutsen G, Olsen NR, Macdonald H, Hailey L, Wilson HM, Lydiatt A, Kristiansen A. Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. BMJ. 2017;357:j1982. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 143] [Cited by in RCA: 155] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 38. | Beaufils P, Becker R, Kopf S, Englund M, Verdonk R, Ollivier M, Seil R. Surgical management of degenerative meniscus lesions: the 2016 ESSKA meniscus consensus. Knee Surg Sports Traumatol Arthrosc. 2017;25:335-346. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 148] [Cited by in RCA: 198] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 39. | Dingenen B, Gokeler A. Optimization of the Return-to-Sport Paradigm After Anterior Cruciate Ligament Reconstruction: A Critical Step Back to Move Forward. Sports Med. 2017;47:1487-1500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 211] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 40. | Liu M, Ding J, Peng Y, Fang J, Zhao M, Zhang W, Chen H, Zhang J, Peng H, Wang Q. Platelet-rich plasma-contained drug delivery systems to treat orthopedic injuries. Int J Pharm X. 2025;10:100372. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 41. | Chahla J, Cinque ME, Piuzzi NS, Mannava S, Geeslin AG, Murray IR, Dornan GJ, Muschler GF, LaPrade RF. A Call for Standardization in Platelet-Rich Plasma Preparation Protocols and Composition Reporting: A Systematic Review of the Clinical Orthopaedic Literature. J Bone Joint Surg Am. 2017;99:1769-1779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 301] [Cited by in RCA: 413] [Article Influence: 45.9] [Reference Citation Analysis (0)] |
| 42. | Koukoulias NE, Kyparlis D, Koumis P, Lola D, Papastergiou SG. Locked bucket-handle tears of both medial and lateral menisci with simultaneous anterior cruciate and medial collateral ligaments injury. BMJ Case Rep. 2011;2011:bcr0320114046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 43. | Muthu S, Bapat A, Jain R, Jeyaraman N, Jeyaraman M. Exosomal therapy-a new frontier in regenerative medicine. Stem Cell Investig. 2021;8:7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 109] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 44. | Tay CT, Joham AE, Teede HJ. Key standards and principles for developing evidence-based clinical guidelines: balancing health professional, patient, funder, and government needs. Fertil Steril. 2025;123:561-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 45. | Connor L, Dean J, McNett M, Tydings DM, Shrout A, Gorsuch PF, Hole A, Moore L, Brown R, Melnyk BM, Gallagher-Ford L. Evidence-based practice improves patient outcomes and healthcare system return on investment: Findings from a scoping review. Worldviews Evid Based Nurs. 2023;20:6-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 168] [Article Influence: 56.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/