Published online Jul 18, 2025. doi: 10.5312/wjo.v16.i7.107698
Revised: May 4, 2025
Accepted: June 13, 2025
Published online: July 18, 2025
Processing time: 111 Days and 19.7 Hours
Uniportal full-endoscopy (UFE) technique has been continuously developed and applied for treating lumbar spinal stenosis. However, achieving effective decom
To contrast the clinical outcomes between biportal and UFE techniques for trea
This study retrospectively examined 100 patients diagnosed with lumbar spinal stenosis and bilateral symptoms. Among them, 52 cases were part of group A (BFE technique group), and 48 cases belonged to group B (UFE technique group). The visual analogue scale (VAS), Oswestry Disability Index (ODI), and modified Macnab criteria were used to evaluate the clinical outcomes.
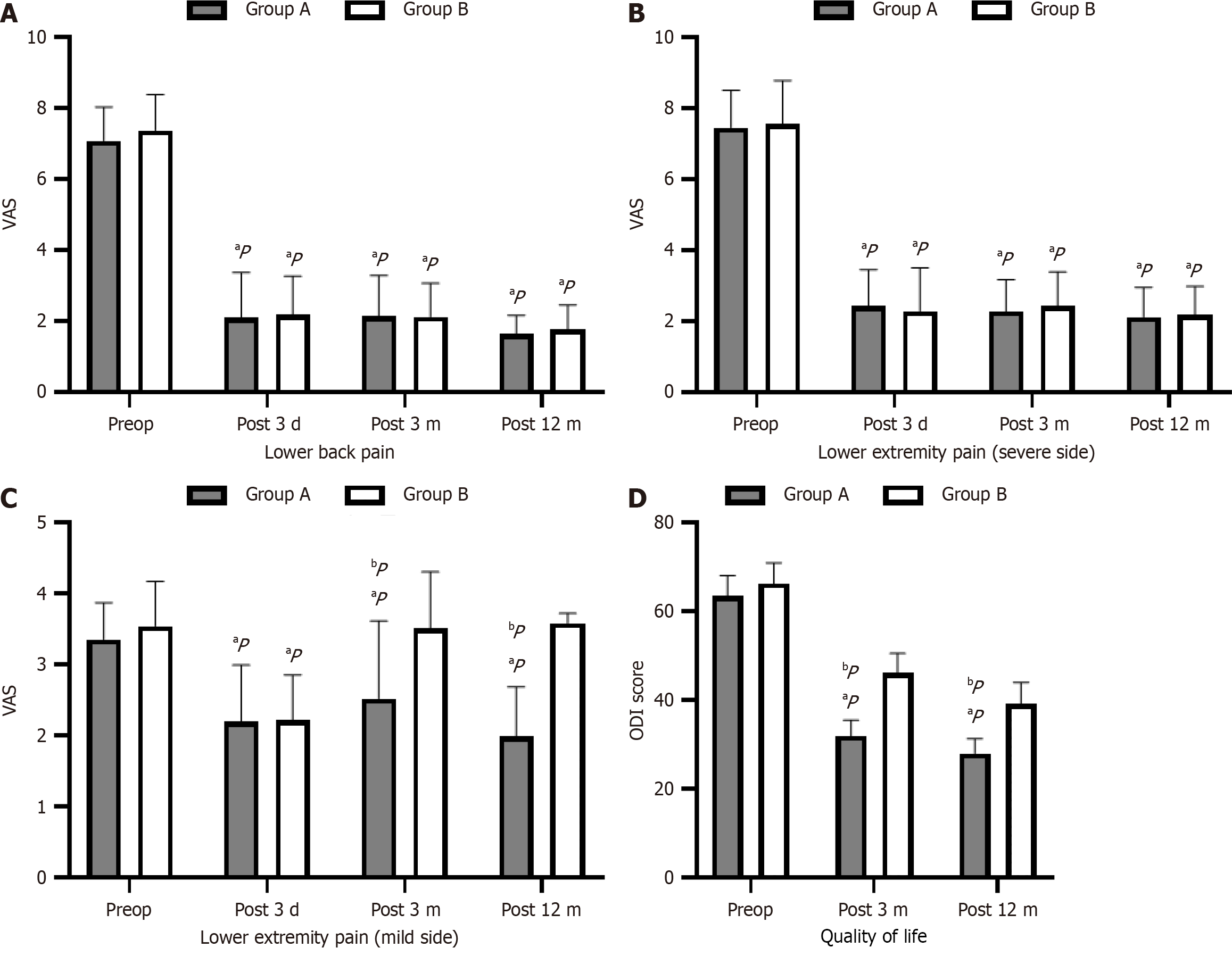
Group A had significantly shorter operation time than group B. Both groups experienced substantial relief in lower back and lower extremity pain on the severe side at postoperative 3 days, 3 months, and 12 months. Group A had notably lower VAS scores for mild side lower extremity pain at postoperative 3 months and 12 months compared to group B. Group A's ODI scores were significantly lower at postoperative 3 months and 12 months, whereas group B's scores did not significantly differ from preoperative values. Group A's ODI scores were significantly lower than group B's at postoperative 3 months and 12 months. Group A had a significantly higher excellent and good response rate (94.23%) compared to group B (81.25%) at postoperative 12 months based on the modified Macnab scale outcomes.
The BFE technique offers multiple benefits, including reduced trauma and quicker recovery as a minimally invasive surgery, and enhanced decompression efficiency over the UFE technique when treating lumbar spinal stenosis with bilateral symptoms.
Core Tip: The clinical efficacy of the uniportal full-endoscopy (UFE) technique in decompressing lumbar spinal stenosis is technically difficult and uncertain. Therefore, to overcome these limitations, we previously proposed the biportal full-endoscopy technique, which combines the advantages of both UFE and unilateral biportal endoscopy. The following is a retrospective comparison of clinical outcomes of biportal and UFE methods in the treatment of lumbar spinal stenosis with bilateral symptoms. According to the results, the biportal method has some benefits over the uniportal method such as less trauma during surgery, faster recovery time, and improved decompression efficiency of the affected regions.
- Citation: Guo S, Hang RN, Zhu K, Wu CQ, Yan MJ, Li XH, Liu YB, Fu Q. Comparison of clinical outcomes between biportal and uniportal full-endoscopy techniques in lumbar spinal stenosis with bilateral symptoms. World J Orthop 2025; 16(7): 107698
- URL: https://www.wjgnet.com/2218-5836/full/v16/i7/107698.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i7.107698
Lumbar spinal stenosis is on the rise due to the aging population, manifesting as neurogenic claudication in one or both lower limbs[1,2]. The primary factors contributing to spinal canal stenosis include ligamentum flavum hypertrophy, calcification, articular process hyperplasia, and disc herniation[3,4]. Traditional posterior laminectomy and fusion surgery has emerged as a viable approach for managing lumbar spinal stenosis[5]. Nevertheless, several issues have been high
Uniportal full-endoscopy (UFE) technique has been continuously developed and applied to remove the protruding nucleus pulposus and decompress nerve roots while ensuring spine stability[8]. However, the decompression outcome of bilateral lateral recess using the UFE technique remains technically demanding and uncertain[9]. In a retrospective study, Komp et al[9] treated 72 patients with bilateral lateral recess stenosis using the UFE technique to perform unilateral laminectomy for bilateral decompression (ULBD). They found that 70.8% of patients experienced significant symptom relief on the ipsilateral (surgical) side, while improvement on the contralateral side was less pronounced during the two-year follow-up[10]. Additionally, the UFE technique also exhibits notable limitations, such as a steep learning curve and restricted indications. In recent years, the unilateral biportal endoscopy (UBE) technique has gained wide acceptance in treating lumbar spinal stenosis[11-13]. Plasma radiofrequency is utilized to treat soft tissue under UBE technique, resulting in improved treatment efficiency. Additionally, standard surgical instruments can be employed to enhance decompression efficiency[14,15]. However, UBE technique employs an arthroscope as a monitoring endoscope. The observation channel is separated from the operating channel, preventing instrument access to or from the observation channel. Consequently, the observation field of view and the operating window are not coaxial, increasing the difficulty of hand-eye coordination[16]. Moreover, because UBE technique cannot utilize endoscopic instruments and radiofrequency to control intraspinal bleeding, when such bleeding occurs, the high plasma radiofrequency energy adds challenge to precise point-to-point operations, thereby prolonging bleeding time and increasing the risk of nerve damage to some extent.
Drawing on extensive clinical experience with both surgical techniques mentioned, the author's research team has proposed the biportal full-endoscopy (BFE) technique to integrate their respective advantages. The team aims to further enhance operational efficiency and safety by using both conventional and endoscopic instruments. Therefore, we conducted this retrospective clinical study to compare and analyze the clinical outcomes of the easily mastered BFE technique and the UFE technique in treating lumbar spinal stenosis with bilateral symptoms.
Patients who underwent the BFE technique and UFE technique for lumbar spinal stenosis with bilateral symptoms at Shanghai General Hospital between January 2022 and March 2023 were retrospectively analyzed. Magnetic resonance imaging (MRI) was performed prior to surgery in all cases to confirm lumbar spinal stenosis. The inclusion criteria included: (1) Patients experiencing lower back pain along with bilateral intermittent claudication symptoms; (2) Indivi
Spine endoscopy and Elliquence radiofrequency systems were purchased from SPINEDOS (Munich, Germany). The COBLATION radiofrequency system was sourced from Smith+Nephew (London, United Kingdom), and the orthopedic C-arm fluoroscope was bought from Siemens (Munich, Germany).
In this study, we selected the Oswestry Disability Index (ODI) as the primary outcome, which is consistent with its widespread use in previous spinal surgery research. Many prior studies on low back pain have calculated the minimum clinically important difference for the ODI[17-20]. Therefore, we used the ODI as the primary outcome measure to estimate the sample size in this study. We set the 12-month postoperative ODI as the primary endpoint. Based on prior research and clinical experience, we expected a mean 12-month postoperative ODI of 30% in group A (SD = 15%) and 40% in group B (SD = 15%). Using a two-sided test with a significance level of α = 0.05 and power of 0.8, and accounting for a 15% loss to follow-up, the required sample size was calculated to be 43 patients per group using NCSS PASS software. In practice, we retrospectively included 52 cases in group A and 48 cases in group B.
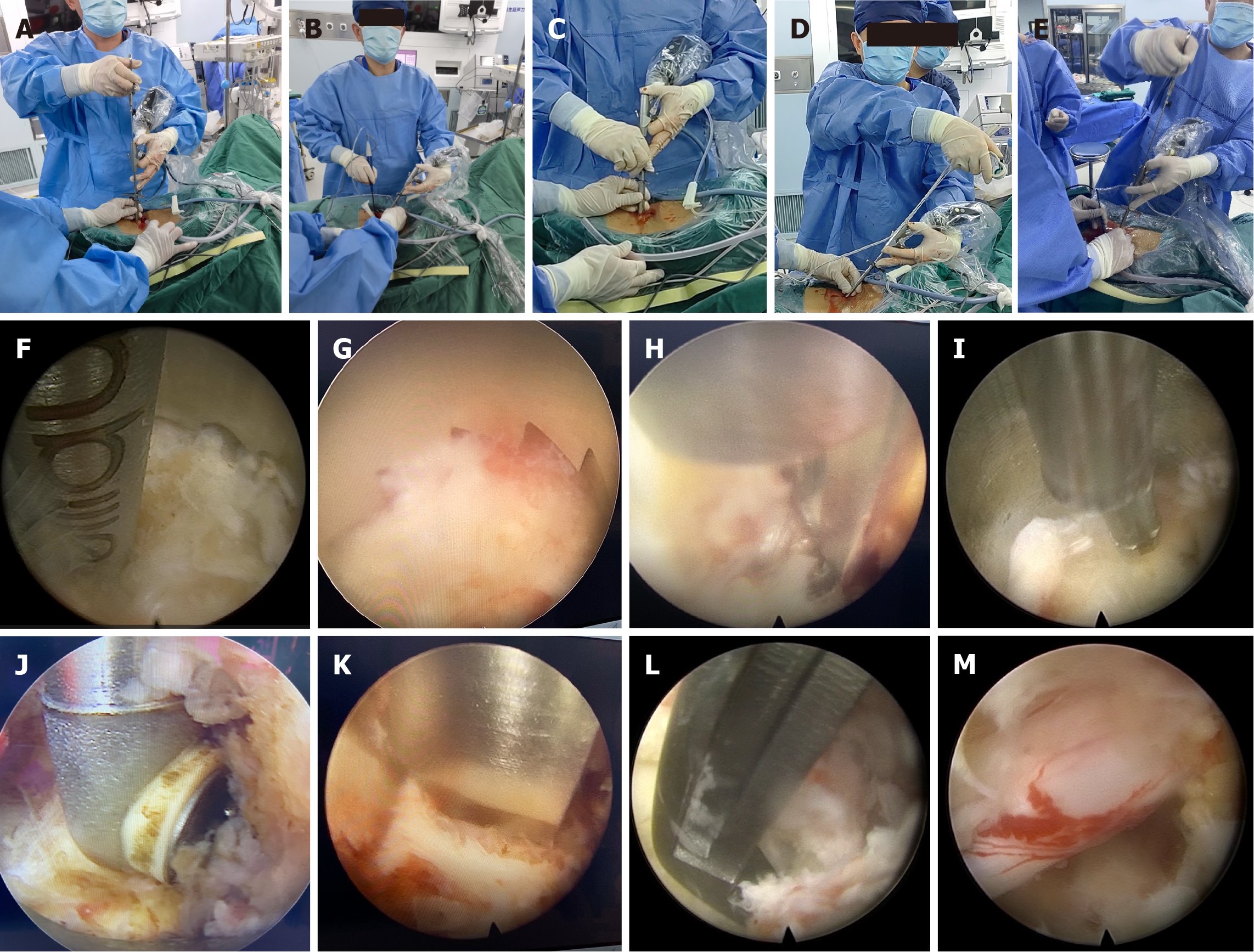
BFE group (group A): The patient lay prone on the all-carbon Allen spinal operation bed, and the lesion segment to be treated was determined by C-arm fluoroscopy. Two 7 mm-length of skin incisions were performed at the upper and lower margins of the interlaminar space. The two incisions are about 1 cm apart from the midline and the upper and lower incisions are about 1.5 cm apart. The serial dilators and strippers were inserted to separate the soft tissue of the lamina, and adjust the position and angle of bilateral channels to complete the "meeting". A 30-degree spinal endoscope was inserted into the observation channel, both COBLATION and Elliquence radiofrequency were used alternately in the working channel to clean the soft tissue that attached on the lamina. Subsequently, laminotomy was carried out employing a 3.5-mm endoscopic high-speed grinding drill, endoscopic punches, and the regular trephine and Kerrison punch. The lateral boundary of decompression extended to the medial side of the ipsilateral superior articular process, while the proximal and distal boundaries were marked by the endpoints of ligamentum flavum. After the ligamentum flavum was resected using a basket punch, endoscopic punch, and Kerrison punch, the ipsilateral nerve root was exposed. Subsequently, the working channel was adjusted across the base of the spinous process to remove the medial side of the contralateral superior articular process and ligamentum flavum, thus revealing the contralateral nerve root. Following sufficient nerve decompression, a drainage tube was inserted. The BFE technique has the following four operating modes: (1) Full UBE mode (dual channels); (2) Full uniportal endoscopic mode (single channel); (3) Observation channel and working channel interchanged mode; and (4) Dual working channel mode, namely, the spinal endoscopic channel can be used as both an observation endoscopy and an operation channel to achieve simultaneous dual-channel operation (Figure 1).
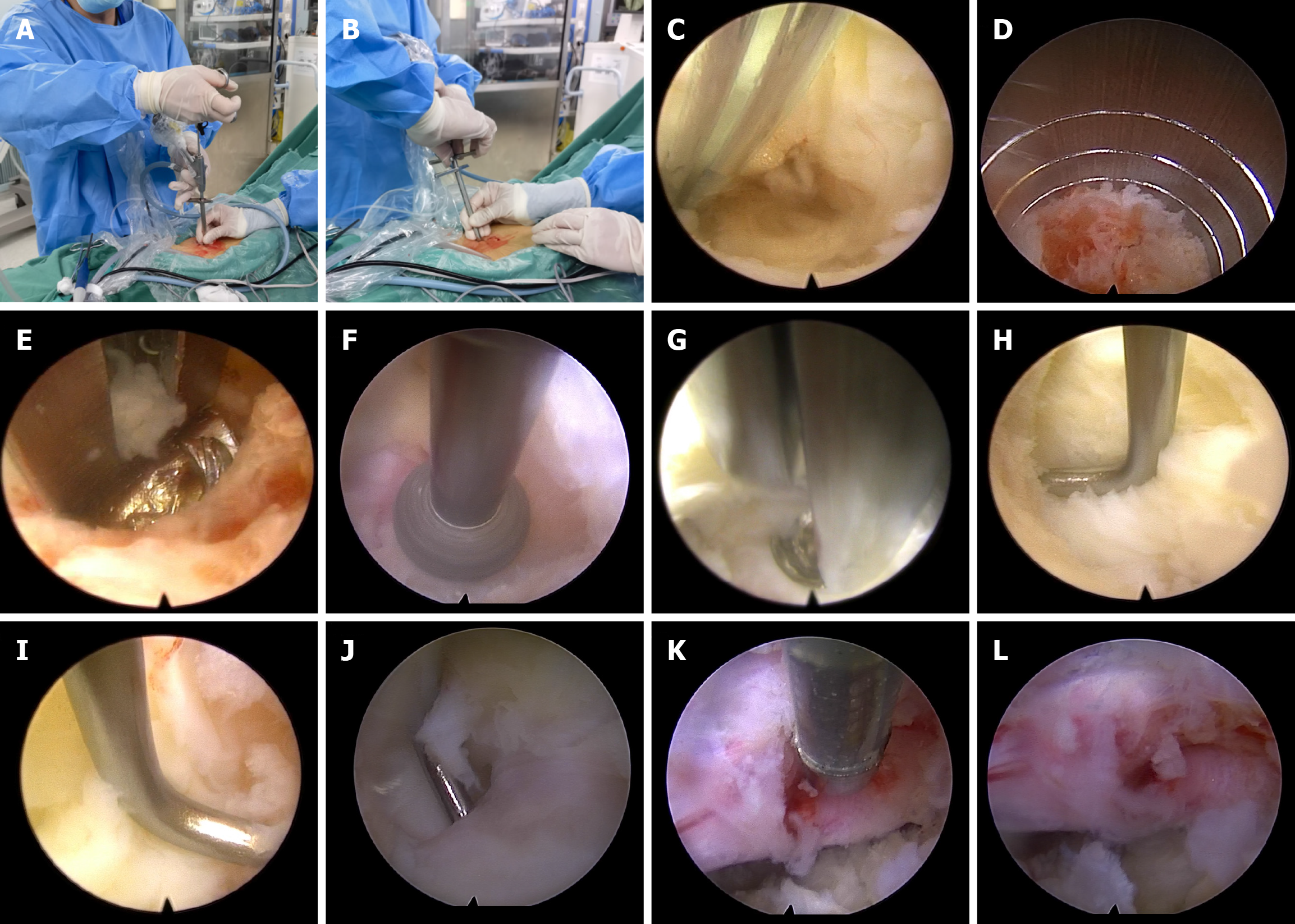
UFE group (group B): The patient was positioned prone on the Allen spinal operation bed, and the location of the lesion segment was determined using C-arm fluoroscopy. An incision measuring 10 mm in length was carefully made 1.5 cm from the midline. Serial dilators and strippers were then inserted to separate the soft tissue of the lamina, creating a working channel. A 30-degree spinal endoscope was inserted, and Elliquence radiofrequency was used through the working channel to remove soft tissue, exposing the lamina and part of the facet joint. Subsequently, laminotomy was performed using a 3.5-mm endoscopic high-speed grinding drill and endoscopic punches (Figure 2).
The day after surgery, patients were directed to perform rehabilitation exercises, and were primarily recommended to rest in bed for four weeks post-surgery. They were also advised to utilize a brace when not in bed. Concurrently, patients were counseled to refrain from engaging in vigorous activities, bending, and bearing weight in the immediate term.
(1) Characteristics of patients; (2) Operation time, hospital stay; (3) Visual analogue scale (VAS) scores for lumbar and lower extremity radiation pain before treatment and at the 3rd day, 3 months and 12 months after surgery; (4) ODI before surgery, and at the 3rd day, 3 months and 12 months after surgery; (5) Excellent and good rate of modified Macnab in both groups at 12 months after surgery; and (6) Complications.
As this retrospective study included a relatively small number of patients, we made sure to have complete follow-up for all participants to maintain the accuracy of the analysis. As a result, there were no missing data in this study.
Statistical Package for the Social Sciences 20.0 software was utilized for statistical analysis. The measurement data were expressed as mean ± SD. The t test was employed to compare all parameters between groups. The χ² test was used to compare rates between groups. P < 0.05 was considered statistically significant.
All patients successfully completed the surgery and follow-up with an average time of 16.00 months ± 1.50 months. According to the above criteria, a total of 100 patients with bilateral symptoms of lumbar spinal stenosis were included in this study, consisting of 27 men and 25 women belonging to group A, and 24 men and 24 women in group B. Group A was found to have more than 92% of stenosis at L4-5 and L5-S1 segments, while 4 cases involved L3-4 segment. The same was true for group B as its distribution of stenosis segments was similar to that of group A. The average body mass index (BMI) in both groups was more than 25. There was no significant difference in age, gender, BMI, underlying disease, smoking status, marital status surgical segment and Schizas grade between the two groups (P > 0.05) (Table 1).
| Group A | Group B | ||||
| Gender | Male | Female | Male | Female | |
| 27 | 25 | 24 | 24 | ||
| Age (years) | 53.50 ± 15.20 | 52.80 ± 13.65 | |||
| Body mass index (kg/m²) | 25.6 ± 6.26 | 27.53 ± 5.89 | |||
| Hypertension | Yes | No | Yes | No | |
| 24 | 28 | 22 | 26 | ||
| Diabetes | Yes | No | Yes | No | |
| 13 | 39 | 12 | 36 | ||
| Smoking status | Yes | No | Yes | No | |
| 21 | 31 | 20 | 28 | ||
| Marital status | Married | Unmarried | Married | Unmarried | |
| 50 | 2 | 47 | 1 | ||
| Surgical segment | L3-4 | 4 | 3 | ||
| L4-5 | 24 | 22 | |||
| L5-S1 | 24 | 23 | |||
| Schizas grade | A | 0 | 0 | ||
| B | 2 | 1 | |||
| C | 31 | 30 | |||
| D | 19 | 17 | |||
The operation time in group A (90.80 minutes ± 7.25 minutes) was significantly shorter than that in group B (110.30 minutes ± 6.25 minutes) (P < 0.05). Although the average hospital stay for group A (4.25 days ± 0.65 days) was slightly longer than that for group B (3.98 days ± 1.05 days), statistical analysis revealed no significant difference between the two groups (P > 0.05).
The lower back pain and lower extremity pain on the severe side were notably alleviated at postoperative 3 days, 3 months, and 12 months in both groups. In group A, the VAS score for lower extremity pain on the mild side exhibited a significant decrease at postoperative 3 days, 3 months, and 12 months compared to the preoperative level. In group B, the VAS score for lower extremity pain on the mild side saw a significant decrease only at postoperative 3 days. However, in group B, the VAS scores for lower extremity pain on the mild side at postoperative 3 months and 12 months did not display a significant reduction compared to the preoperative scores. Comparing the two groups, no substantial difference was observed in the VAS scores for postoperative lower back pain and lower extremity pain on the severe side. Notably, the VAS scores for lower extremity pain on the mild side were significantly lower in group A than in group B at post
The ODI scores for both groups were notably lower at postoperative day 3 compared to preoperative levels. Additionally, for group A, the ODI scores at postoperative 3 months and 12 months were significantly reduced compared to preope
The results of modified Macnab score showed that the excellent and good rate of group A (94.23%) was significantly higher than that of group B (81.25%) at postoperative 12 months.
In group A, complications included incidental durotomy (n = 1) and epidural hematoma (n = 2), while in group B, there were incidental durotomy (n = 2) and epidural hematoma (n = 1). All cases of complications were effectively managed with conservative treatment.
In this study, we propose a novel spinal endoscopy approach, namely BFE technique, which combines the benefits of the UFE technique and the UBE technique for treating lumbar spinal stenosis. We aim to compare the clinical outcomes of this approach with those of UFE. The spinal endoscopy was not only used as the monitoring endoscope but also as the operation channel in BFE technique, and a conventional surgical instrument operation channel was also constructed to achieve uniportal endoscopic operation and hands-free operation[21]. Compared with UFE, BFE approach has two working channels, and the surgery can be performed in the two channels to avoid interference between instruments. Additionally, both the observation channel and the working channel can be moved and tilted freely, thereby greatly increasing surgical flexibility is greatly increased to explore all directions of the spinal canal and achieve comprehensive decompression of the spinal canal. Additionally, all kinds of open and endoscopic instruments can be used in the operation by BFE approach to improve the efficiency of intraoperative procedures like laminectomy and separation of ligamentum flavum. In comparison to UBE technique, BFE approach employs spinal endoscopy as a monitoring channel to enable precise coaxial operation. This approach enhances accuracy and minimizes tissue damage resulting from repeated instrument insertions and withdrawals. Furthermore, BFE approach surpasses the UBE technique in achieving intraoperative hemostasis. Unlike the UBE technique, which relies on COBLATION radiofrequency for hemostasis with its broad planar working interface and substantial tissue contact area, the BFE approach ensures accurate hemostasis. This mitigates the risk of nerve injury during hemostasis within the spinal canal.
The BFE approach employs the translaminar approach, allowing for either unilateral laminectomy or ULBD of the spinal canal. Utilizing this technique, ULBD is performed to minimize damage to the posterior complex of muscles, ligaments, and laminae. With this approach, the spinal endoscope is angled to pass the root of the spinous process, reaching the ventral side of the opposite laminae. This enables resection of the contralateral ligamentum flavum to expose the dural sac and the dorsal side of the contralateral nerve root. Consequently, the VAS scores at 3 months and 12 months post-surgery for the mildly symptomatic side in group A exhibited substantial improvement compared to pre-surgery scores.
The UFE technique, compared to the spinal BFE technique, presents limitations in surgical visualization, increased challenge in instrument manipulation under the endoscope, and restricted angles of instrument use. These drawbacks reduce the efficacy of contralateral bony structure removal, making decompression of the contralateral nerve root challenging. Furthermore, the use of a single hemostasis device in the UFE technique results in an extended operating lever arm and more constrained angles for hemostasis, making it more challenging to accomplish sufficient decom
Despite the numerous advantages of the BFE approach, such as its effectiveness in nerve decompression, improved surgical efficiency, and reduced risk, the increased soft tissue damage associated with this technique stems from the necessity to resect more soft tissue in order to achieve a broader field of view. Consequently, this study observed a greater extent of soft tissue swelling in the BFE group compared to the UFE group, a finding akin to the results reported by Choi et al[24] in their research on the UBE technique. Choi et al[24] conducted a comparative analysis of lumbar MRI changes and inflammatory markers during the postoperative follow-up of UBE, lateral foraminal approach, and posterior interlaminar approach endoscopy techniques. Their findings revealed that the UBE technique induced more trauma than the lateral foraminal and interlaminar approaches, leading to more conspicuous postoperative MRI soft tissue swelling[24]. To mitigate the risk of intraspinal hematoma after decompression, the routine placement of drainage tubes is recommended in the BFE group. This is because the BFE technique requires a broader extent of laminectomy and ligamentum flavum dissociation, leading to more extensive nerve decompression. While the introduction of drainage tubes prolongs bed rest, this necessitates a slightly longer hospital stay in the BFE group.
The limitations of this study are outlined as follows: (1) The study primarily encompassed single-level cases of bilateral lumbar spinal stenosis, omitting cases with multi-level involvement; (2) This research constitutes a clinical retrospective study with a relatively limited case count, lacking extensive large-scale, randomized, multicenter investigations. More
While the UFE technique has become popular in treating lumbar disc herniation, its deployment in lumbar spinal stenosis has been relatively limited. This has been primarily attributed to technical difficulties, inefficiency in decompression, and a high learning curve. Based on clinical experience, we introduced BFE technique to counter these shortcomings. By incorporating a secondary working canal, BFE enhances operating efficiency as well as providing more complete decompression. It also provides enhanced intraoperative bleeding control. BFE further preserves tissue integrity and allows for faster recovery as a minimally invasive procedure. Collectively, these benefits imply that BFE would be a safe, effective, and viable alternative to UFE in managing bilateral lumbar spinal stenosis.
| 1. | Fatoye F, Gebrye T, Odeyemi I. Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatol Int. 2019;39:619-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 222] [Article Influence: 31.7] [Reference Citation Analysis (0)] |
| 2. | Hsieh AH, Yoon ST. Update on the pathophysiology of degenerative disc disease and new developments in treatment strategies. Open Access J Sports Med. 2010;1:191-199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Lai MKL, Cheung PWH, Cheung JPY. A systematic review of developmental lumbar spinal stenosis. Eur Spine J. 2020;29:2173-2187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 4. | Hao J, Cheng J, Xue H, Zhang F. Clinical comparison of unilateral biportal endoscopic discectomy with percutaneous endoscopic lumbar discectomy for single l4/5-level lumbar disk herniation. Pain Pract. 2022;22:191-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 5. | Katz JN, Zimmerman ZE, Mass H, Makhni MC. Diagnosis and Management of Lumbar Spinal Stenosis: A Review. JAMA. 2022;327:1688-1699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 294] [Article Influence: 73.5] [Reference Citation Analysis (0)] |
| 6. | Khalifeh JM, Massie LW, Dibble CF, Dorward IG, Macki M, Khandpur U, Alshohatee K, Jain D, Chang V, Ray WZ. Decompression of Lumbar Central Spinal Canal Stenosis Following Minimally Invasive Transforaminal Lumbar Interbody Fusion. Clin Spine Surg. 2021;34:E439-E449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Heemskerk JL, Oluwadara Akinduro O, Clifton W, Quiñones-Hinojosa A, Abode-Iyamah KO. Long-term clinical outcome of minimally invasive versus open single-level transforaminal lumbar interbody fusion for degenerative lumbar diseases: a meta-analysis. Spine J. 2021;21:2049-2065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 77] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 8. | Gadjradj PS, Harhangi BS, Amelink J, van Susante J, Kamper S, van Tulder M, Peul WC, Vleggeert-Lankamp C, Rubinstein SM. Percutaneous Transforaminal Endoscopic Discectomy Versus Open Microdiscectomy for Lumbar Disc Herniation: A Systematic Review and Meta-analysis. Spine (Phila Pa 1976). 2021;46:538-549. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 107] [Article Influence: 21.4] [Reference Citation Analysis (10)] |
| 9. | Komp M, Hahn P, Merk H, Godolias G, Ruetten S. Bilateral operation of lumbar degenerative central spinal stenosis in full-endoscopic interlaminar technique with unilateral approach: prospective 2-year results of 74 patients. J Spinal Disord Tech. 2011;24:281-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 83] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 10. | Akar E, Toprak F, Öğrenci A. The relationship between bone canal diameter and facet tropism in cases of lumbar spinal stenosis. J Neurosci Rural Pract. 2022;13:641-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Park DK, Weng C, Zakko P, Choi DJ. Unilateral Biportal Endoscopy for Lumbar Spinal Stenosis and Lumbar Disc Herniation. JBJS Essent Surg Tech. 2023;13:e22.00020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 25] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 12. | Xu J, Wang D, Liu J, Zhu C, Bao J, Gao W, Zhang W, Pan H. Learning Curve and Complications of Unilateral Biportal Endoscopy: Cumulative Sum and Risk-Adjusted Cumulative Sum Analysis. Neurospine. 2022;19:792-804. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 81] [Reference Citation Analysis (0)] |
| 13. | Pao JL, Lin SM, Chen WC, Chang CH. Unilateral biportal endoscopic decompression for degenerative lumbar canal stenosis. J Spine Surg. 2020;6:438-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 80] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 14. | Hua W, Liao Z, Chen C, Feng X, Ke W, Wang B, Li S, Wang K, Zeng X, Wu X, Zhang Y, Yang C. Clinical Outcomes of Uniportal and Biportal Lumbar Endoscopic Unilateral Laminotomy for Bilateral Decompression in Patients with Lumbar Spinal Stenosis: A Retrospective Pair-Matched Case-Control Study. World Neurosurg. 2022;161:e134-e145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 40] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 15. | Wei WB, Dang SJ, Liu HZ, Duan DP, Wei L. Unilateral Biportal Endoscopic Discectomy versus Percutaneous Endoscopic Interlaminar Discectomy for Lumbar Disc Herniation. J Pain Res. 2024;17:1737-1744. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 16. | Li YS, Chen CM, Hsu CJ, Yao ZK. Complications of Unilateral Biportal Endoscopic Lumbar Discectomy: A Systematic Review. World Neurosurg. 2022;168:359-368.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 17. | Ma C, Wu S, Xiao L, Xue Y. Responsiveness of the Chinese version of the Oswestry disability index in patients with chronic low back pain. Eur Spine J. 2011;20:475-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 42] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Parker SL, Adogwa O, Paul AR, Anderson WN, Aaronson O, Cheng JS, McGirt MJ. Utility of minimum clinically important difference in assessing pain, disability, and health state after transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Neurosurg Spine. 2011;14:598-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 297] [Article Influence: 19.8] [Reference Citation Analysis (1)] |
| 19. | Cleland JA, Whitman JM, Houser JL, Wainner RS, Childs JD. Psychometric properties of selected tests in patients with lumbar spinal stenosis. Spine J. 2012;12:921-931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 85] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 20. | Monticone M, Baiardi P, Vanti C, Ferrari S, Pillastrini P, Mugnai R, Foti C. Responsiveness of the Oswestry Disability Index and the Roland Morris Disability Questionnaire in Italian subjects with sub-acute and chronic low back pain. Eur Spine J. 2012;21:122-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 115] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 21. | Fujita N. Lumbar Spinal Canal Stenosis from the Perspective of Locomotive Syndrome and Metabolic Syndrome: A Narrative Review. Spine Surg Relat Res. 2021;5:61-67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Hu Y, Fu H, Yang D, Xu W. Clinical efficacy and imaging outcomes of unilateral biportal endoscopy with unilateral laminotomy for bilateral decompression in the treatment of severe lumbar spinal stenosis. Front Surg. 2022;9:1061566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 23. | Giordan E, Liu Y, Suvithayasiri S, Russo S, Lee C, Hasan GA, Jin-Sung K. Endoscopic Treatment of Thoracolumbar Spondylodiscitis: A Systematic Review and Meta-Analysis. World Neurosurg. 2024;189:296-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Choi KC, Shim HK, Hwang JS, Shin SH, Lee DC, Jung HH, Park HA, Park CK. Comparison of Surgical Invasiveness Between Microdiscectomy and 3 Different Endoscopic Discectomy Techniques for Lumbar Disc Herniation. World Neurosurg. 2018;116:e750-e758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 109] [Article Influence: 13.6] [Reference Citation Analysis (0)] |