Published online Apr 18, 2025. doi: 10.5312/wjo.v16.i4.106862
Revised: March 23, 2025
Accepted: April 11, 2025
Published online: April 18, 2025
Processing time: 39 Days and 6.4 Hours
In intertrochanteric fractures, the positive medial cortex support reduction is considered to provide a non-anatomical buttress that helps in controlled collapse.
To analyze the concept of medial cortical reduction (MCR) and its clinical and radiological association in geriatric intertrochanteric femur fractures.
Geriatric patients who presented with AO/OTA 31A1 and 31A2 femur fractures and treated with proximal femoral nailing between July 2021 and June 2023 were include in this prospective cohort study. Based on the degree of MCR, they were divided into positive, neutral, or negative MCR groups. The demographic base
47 patients (Male: Famale 35:12) with mean age of 65.8 ± 4.2 years were included in this study. Twenty-two cases had neutral support, nine had negative support, and sixteen had positive support in the medial cortex post-operatively. Baseline characteristics of the three groups were comparable. No significant differences were found in the femur neck length and femur neck-shaft angle changes post-surgery between the groups. The modified HHS was not found to be significant between the groups (P = 0.883) as that of the time to full weight bearing (P = 0.789).
The type of reduction achieved based on medial cortical alignment does not affect the femur neck length shortening or varus collapse. Future randomized controlled trials are needed to validate the findings noted in the study.
Core Tip: In this prospective cohort study, 47 geriatric patients with AO/OTA 31A1 and 31A2 femur fractures treated with proximal femoral nailing were analyzed based on medial cortical reduction (MCR). They were divided into positive, neutral, or negative MCR groups. The study found no significant differences in femur neck length shortening, neck-shaft angle changes, modified Harris Hip Scores, or time to full weight-bearing among the groups. MCR alignment does not affect femur neck length or varus collapse. Future randomized trials are needed to validate these findings.
- Citation: Mounisamy P, Suresh H, Chandrashekar S, D U, Jeyaraman N, Jeyaraman M, Muthu S. Medial cortical reduction does not influence outcomes in geriatric intertrochanteric femur fractures treated with proximal femoral nail. World J Orthop 2025; 16(4): 106862
- URL: https://www.wjgnet.com/2218-5836/full/v16/i4/106862.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i4.106862
With the unprecedented aging of the global population, hip fractures have become a significant health concern, impacting over 4.5 million individuals each year—a figure anticipated to escalate substantially over the next four decades[1-3]. Among these, trochanteric hip fractures constitute about 50% and are increasingly prevalent among the elderly[4-7]. Surgical intervention is crucial for promoting early mobilization and rehabilitation, yet the reoperation rate remains high in cases of trochanteric hip fractures, ranging from 10.0% to 18.1%[8-12]. This has led to a persistent interest and ad
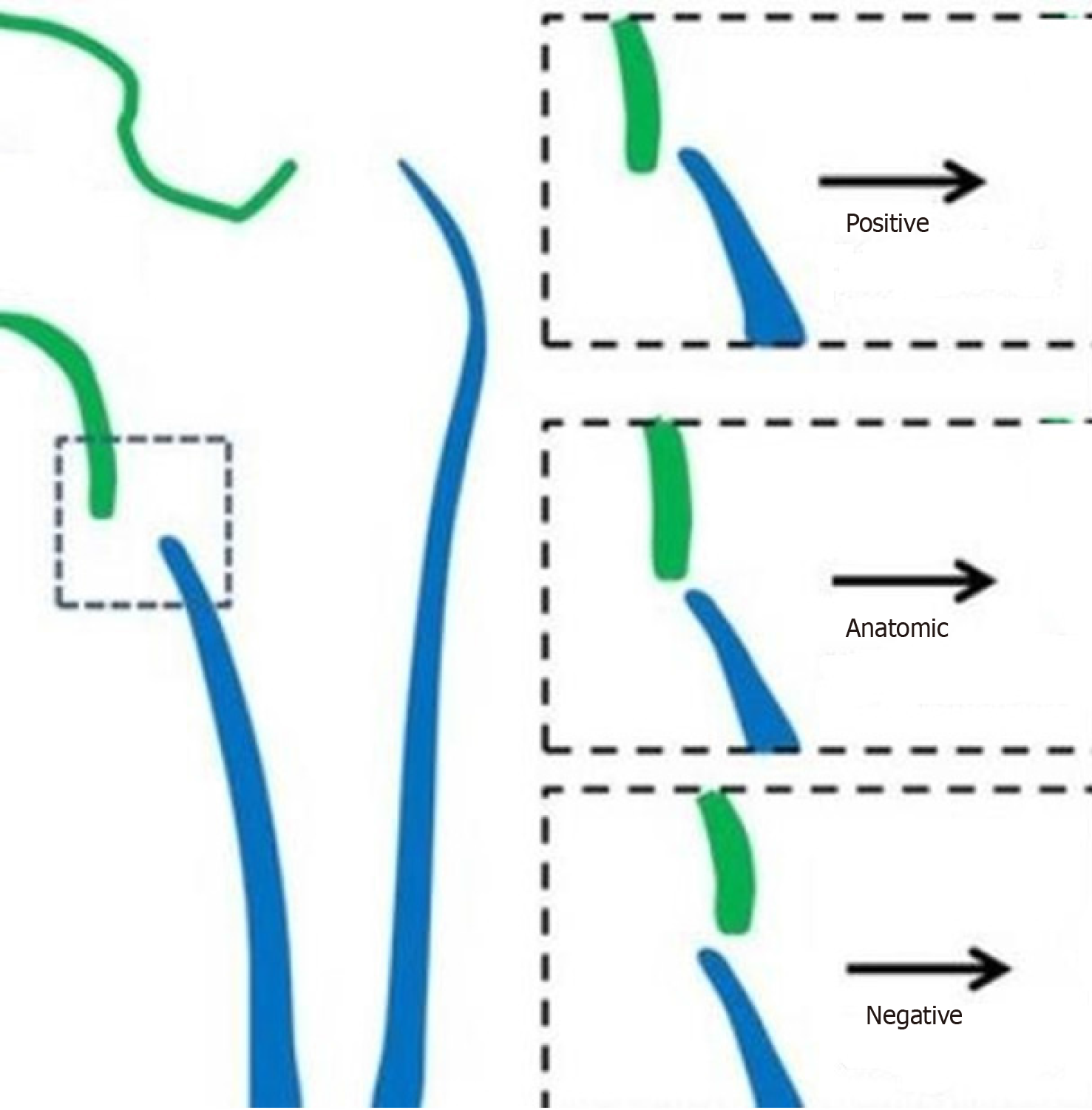
One such technique, Medial Cortical Reduction (MCR, Figure 1), introduced in 2015, has sparked considerable debate. While it is broadly accepted that positive MCR offers greater mechanical stability compared to negative or neutral MCR (Figure 1), there is still ongoing discussion regarding whether positive MCR is the optimal approach for treating these trochanteric fractures[13-17]. Conflicting evidences are noted on the ideal reduction to be maintained to achieve favorable clinical and radiological outcomes. This study aims to analyze the concept of fracture reduction in the medial cortex and its clinical and radiological association in geriatric intertrochanteric femur fractures.
After obtaining institute ethics committee clearance (JIP/IEC-OS/125/2022 dated 01.10.2023), the geriatric patients of age > 60 years who presented with AO/OTA 31A1 and 31A2 femur fractures and treated with proximal femoral nailing (PFN) between July 2021 and June 2023 were included in this prospective cohort study. We excluded patients who did not give consent to participate in the study.
After initial evaluation subjects were taken up for surgery for PFN fixation. The average time between an injury and an operation was between two and seven days. Under general or spinal anaesthesia, all procedures were carried out with the subjects in the supine position on a fracture table. On the medial border of the greater trochanter's tip, a nail entry site was made. The medullary canal's proximal portion—no more than two centimeters—was reamed.
After the nail was inserted, the proximal lag screw was inserted in the desired position, inferiorly through the calcar and centrally in lateral view. PFN-rotation (PFNA2) and PFN were both utilized depending upon the availability, and affordability of the patients in consideration. The two proximal screws of PFN are an anti-rotation screw and a lag screw. The single helical screw on PFNA2 is intended to provide additional anchoring by preserving bone material and compacting the cancellous bone surrounding it as it is being inserted. It is considered that the helical blade also offers compression and rotational stability.
For PFNA-2, the helical blade was placed in the middle of the femoral head both on anteroposterior (AP) and lateral view. While for the PFN nail, the lag screw was placed inferiorly in the lower one third of the head on AP view and in the middle on lateral view. The derotation screw was inserted superior to the neck screw. Distal locking was performed with one locking bolt in static mode. Isometric quadriceps workouts were started by the subjects on the first postoperative day. Toe touch weight bearing as tolerated was allowed on first post-operative day in cases with good reduction and stable fixation. Physical therapists were included in the rehabilitation protocol. Following surgery, routine anterior-posterior hip AP radiographs were taken with both legs positioned 15 degrees internally rotated. With the contralateral hip flexed and abducted, lateral radiographs were obtained.
Subjects were divided based on the proximal fragment’s medial cortex relative to the femur shaft’s medial cortex in AP view as follows: (1) Positive medial cortex support: The proximal fragments medial cortex is located a little bit (one cortex thickness) superior and medial to the femur shaft’s medial cortex; (2) Neutral position: The proximal fragments medial cortex and the femur shaft’s medial cortex are reduced anatomically; and (3) Negative medial cortex support: The proximal fragments medial cortex is displaced lateral to the femur shaft’s medial cortex.
After division of subjects into one of the three reduction groups, they were followed up at timely intervals-6 weeks, 3 months and 6 months. The following radiological parameters such as femoral neck-shaft angle, length of the femoral neck were calculated at specified time intervals-initial post-operative, at 6 weeks, at 3 months and at 6 months. Further, functional recovery scores such as modified Harris Hip Score (HHS) and time to full weight bearing were also analyzed post surgery.
Data was analyzed using version SPSS 26.0, IBM Corp., Chicago, Illinois, United States. The continuous variables like age, neck-shaft angle, and femur neck length were summarized as mean with standard deviation or median with interquartile range. The categorical variables such as gender and comorbidities were expressed as frequency or proportion. The continuous variable between the groups were compared using one way analysis of variance/Kruskal-Wallis test and post-hoc test were done. The categorical variable between the groups were analyzed using Chi-square/Fischer’s Exact test.
We included 47 patients (Male: Famale 35:12) between 61-70 years in this study. Twenty-two cases had neutral support, nine had negative support, and sixteen had positive support. Baseline characteristics of the three groups were comparable as shown in Table 1. With respect to fracture type distribution, AO 31A1 was noted in 12 patients of which 5/12 were fixed in positive and 7/12 were fixed in neutral and none in negative. Of the 35 patients of AO 31A2 type, 11/35 were fixed in positive and 15/35 were fixed in neutral and 9/35 in negative. In this study, neutral medial cortical support reduction (22/47) was the commonest type of reduction achieved post operatively followed by positive (16/47) and negative (9/47).
| Characteristics | Positive MCR (n = 16) | Neutral MCR (n = 22) | Negative MCR (n = 9) | P value |
| Age (years) | 64.3 ± 3.2 | 67.7 ± 4.2 | 65.4 ± 3.6 | 0.876 |
| Male/Female | 10/6 | 17/5 | 8/1 | 0.432 |
| Fracture type | ||||
| 31A1 | 5 (31.2) | 7 (31.8) | 0 (0.0) | 0.032 |
| 31A2 | 11 (68.7) | 15 (68.1) | 9 (100) | |
| ASA types | ||||
| I | 4 (25.0) | 7 (31.8) | 3 (33.3) | 0.543 |
| II | 12 (75.0) | 15 (68.1) | 6 (66.6) | |
| Diabetes mellitus | 7 (43.7) | 9 (40.9) | 5 (55.5) | 0.761 |
| Ischemic heart disease | 4 (25.0) | 5 (22.7) | 3 (33.3) | 0.876 |
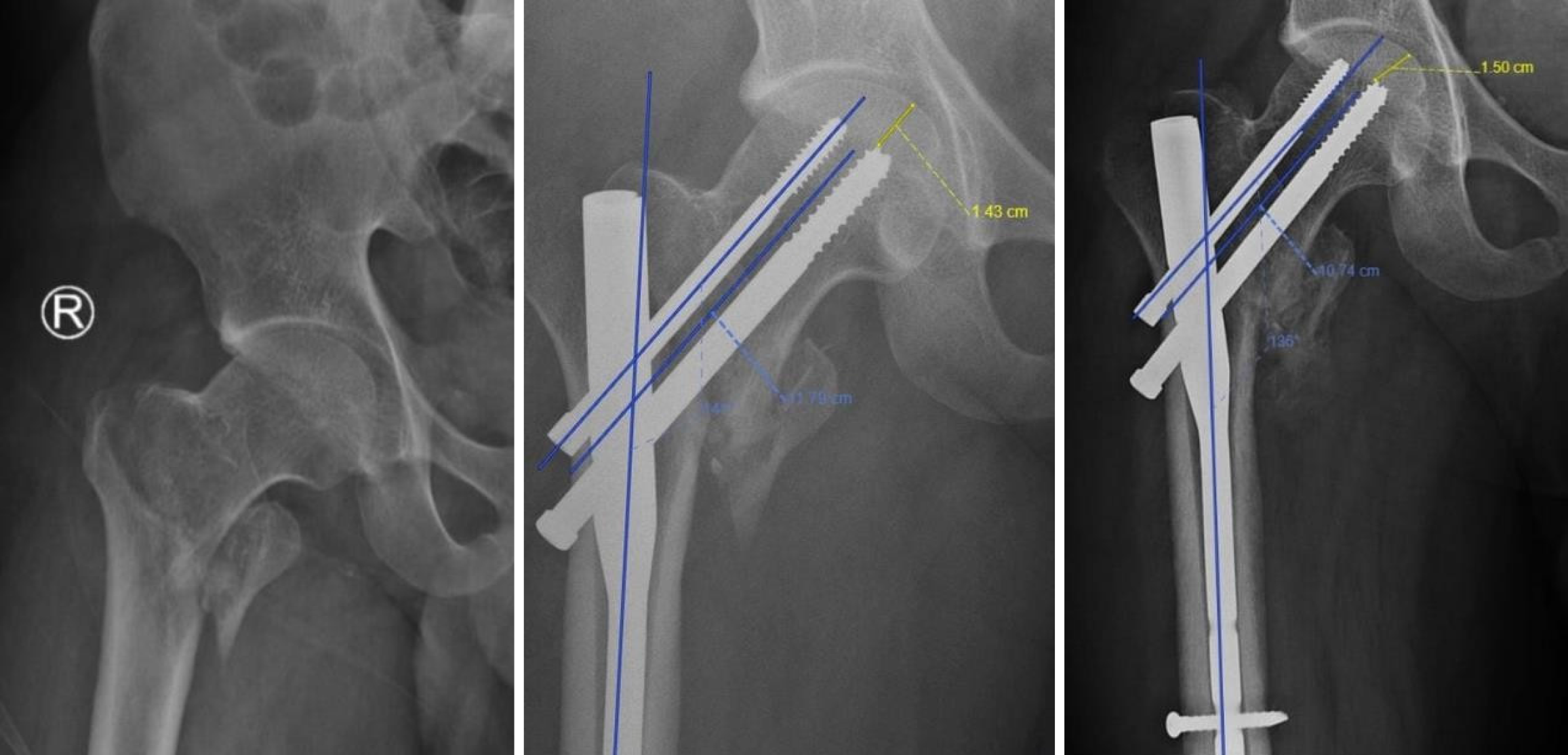
The average decrease in femur neck length and femur shaft angle/varus collapse over 6 months are given in Table 2. The neck length and varus collapse noted were 69 mm/8.3degree, 95 mm/8.44degree, 85 mm/7.87 degree in positive, neutral and negative groups respectively and the difference was not found to be significant among the three groups as shown in Table 2. The modified HHS among the three groups were not found to be significant between the groups (P = 0.883) as that of the time to full weight bearing (P = 0.789). An illustrative case of unstable intertrochanteric femur fracture with positive medial cortical alignment is Figure 2.
| Outcomes | Positive MCR (n = 16) | Neutral MCR (n = 22) | Negative MCR (n = 9) | P value |
| Femur neck length (cm) | ||||
| Initial post op | 9.08 ± 1.2 | 8.93 ± 0.9 | 8.8 ± 1.1 | 0.765 |
| 6 weeks post op | 8.62 ± 1.1 | 8.46 ± 1.5 | 8.23 ± 1.2 | 0.865 |
| 3 months post op | 8.42 ± 0.9 | 8.22 ± 1.3 | 8.05 ± 0.9 | 0.893 |
| 6 months post op | 8.39 ± 1.2 | 7.98 ± 1.1 | 7.95 ± 1.3 | 0.792 |
| 6months, initial post op (mm) | 7.9 ± 1.1 | 9.5 ± 0.8 | 8.5 ± 0.9 | 0.118 |
| Femur shaft angle (degrees) | ||||
| Initial post op | 141.38 ± 9.8 | 139.50 ± 7.3 | 138.00 ± 11.2 | 0.545 |
| 6 weeks post op | 137.00 ± 7.2 | 135.30 ± 9.2 | 134.11 ± 9.7 | 0.754 |
| 3 months post op | 134.87 ± 9.4 | 132.78 ± 8.6 | 131.89 ± 10.4 | 0.634 |
| 6 months post op | 133.08 ± 10.2 | 131.06 ± 11.2 | 130.13 ± 9.8 | 0.549 |
| 6months, initial post op | 8.37 ± 0.7 | 8.42 ± 0.8 | 7.87 ± 0.9 | 0.312 |
| Clinical outcomes | ||||
| Timeto full weight bearing (weeks) | 4.63 ± 1.2 | 4.77 ± 1.4 | 4.56 ± 1.3 | 0.786 |
| Modified Harris Hip score | 70.44 ± 11.4 | 67.55 ± 9.7 | 67.89 ± 10.2 | 0.883 |
Mechanical stability, a key determinant in fracture healing, is significantly influenced by reduction quality, fragment geometry, and implant placement[18-21]. Kaufer’s five variables elucidate the intricate interplay between bone quality, fracture reduction, and fixation technique[22]. Our findings resonate with Kaufer's work, demonstrating that stable fracture reduction enhances cortical contact between proximal and distal fragments, effectively resisting varus and posterior displacement forces and contributing to the overall strength of the fracture-implant assembly without any variability in the reduction pattern.
In addressing the reduction of unstable pertrochanteric fractures, particularly AO/OTA type A2 fractures, loss of posteromedial cortical support, commonly due to displacement of the lesser trochanter fragment, poses significant challenges[13,23,24]. However, the intact anteromedial cortex often compensates, providing sufficient support for the head-neck fragment post-reduction[25,26]. This finding aligns with the reduction criteria modified by Baumgartner, which prioritize Garden alignments and anteromedial contact for achieving acceptable reductions in unstable fractures without any preponderance on the grade of reduction (positive/neutral/negative)[27,28].
Furthermore, our study challenges Gotfried's non-anatomical reduction technique[29] and Chang et al’s positive anteromedial cortical support reduction theory[13]. These methodologies advocate for creating a positive buttress and ensuring secondary stability, crucial for preventing future reduction deterioration. The concept of medial cortical support, as posited by Chang et al[13], does not seem to correlate with the clinical and radiological results as noted in our study. Our study offers a promising direction for future biomechanical research towards other factors that might contribute to the fracture stability to correlate with clinical and radiological outcomes.
With respect to fracture type distribution, AO 2.3 was the predominant type (19/47). Among the 12 subjects with simple fractures (AO 31A1) 5/12 were fixed in positive and 7/12 were fixed in neutral and none in negative. Remaining 35 subjects with more unstable fracture types AO 31A2, 11/35 were fixed in positive, 15/35 in neutral and 9/35 in negative. These findings could be explained by the reduction achieved intraoperatively as among those with simpler fracture types, it was easier to obtain an anatomical reduction. In this study, neutral medial cortical support reduction (22/47) was the commonest type of reduction achieved post operatively followed by positive (16/47) and negative (9/47). Similar results were obtained in the study conducted by Chang et al[13], positive, neutral and negative were 89/127, 26/127 and 12/127 respectively.
In PFN surgeries, routine reduction maneuvers including traction and internal rotation were used. The goal was anatomic reduction though it was difficult in certain cases because of the fracture pattern. Positive MCR (16/47) was more commonly observed than negative (9/47). This may be attributed to the wedge open effect, wherein as the proximal femur nail passes to the femur shaft from the medial part of greater trochanter, it moves the shaft laterally.
Our results seem to go against (Kaufer's work) the notion that cortical contact reduces varus collapse. The current study did not find a significant correlation between the type of MCR and the radiological parameters, specifically femur neck length shortening and varus collapse, despite the fact that positive medial cortex support reduction can theoretically provide a non-anatomical buttress and further aid in controlled collapse. The femur neck length and femur shaft angle seemed to decrease over time in a similar trend among all three groups and the decrease was not found to be significant as shown in Table 2. A possible explanation for this observation was that reduction quality and fixation quality are more critical to the stability of fracture fixation than the type of reduction with respect to MCR alone.
The femur neck length shortening, varus collapse, and functional result were significantly correlated with the quality of reduction attained as determined by the Baumgaertner score and fixation stability as defined by the tip apex and tip calcar distances. A similar result was noted in the study by Mallya et al[30], where the stability of fixation correlated with the varus collapse and functional outcomes rather than the medical cortical reduction.
It is important to distinguish between the term reduction quality and reduction type. With respect to the type of reduction based on MCR, post operatively patients were divided into positive, neutral or negative MCR group with respect to the medial cortices of the proximal fragment and the femoral shafts medial cortex. Whereas the quality of reduction was evaluated using the reduction criteria published by Baumgaertner et al[31]. If the displacement on the AP and lateral X-ray was less than 4 mm, the reduction satisfied the displacement requirement. If there was less than 20 degrees of angulation on the lateral X-ray and the neck shaft angle in the AP view was either normal or slightly valgus (130-150°), the angulation criteria were satisfied. A reduction was rated as good if it satisfied both requirements, acceptable if it satisfied just one, and poor if it satisfied neither.
As the reduction quality in terms of alignment in both coronal and sagittal planes, and fixation quality were good and comparable in all three groups, the collapse of the intertrochanteric fracture region was similar, irrespective of the type of MCR obtained. Subjects on average resumed full weight bearing walking by 4 to 5 weeks in all three groups. Association between modified HHS among the three groups was not found to be significant. A possible explanation for the similar functional outcomes in the three groups might be attributed to the comparable decrease in femur neck length and femur shaft angles in the three groups. With the varus collapse and decrease in femur neck length, the effective abductor lever arm length reduced, and this caused a decrease in strength of the abductors and a lurch while walking. Adequate rehabilitation in terms of hip abductor strengthening exercises play an important part of rehabilitation protocol and collaboration between geriatric specialists and physiotherapists were crucial for effective patient care[32-37].
Our study has limitations to acknowledge. First, the sample size of the geriatric population included in the study is small that might affect the generalizability of the results obtained from the study. Second, factors such as bone mineral density was not estimated between the groups analyzed which might have affected the outcomes measured. However, other variables such as age, sex, comorbidities were comparable across the study groups. Future research should focus on validating these findings through prospective clinical trials of increased sample size and biomechanical analyses to establish comprehensive guidelines for the management of unstable per-trochanteric fractures in the elderly.
Based on the findings of this study, we conclude that the type of reduction achieved with respect to the medical cortical alignment does not affect the femur neck length shortening, the varus collapse or the function a outcome and that the fracture reduction quality as assessed by Baumgaertner reduction criteria the and stability of fixation as assessed by the tip-apex-distance are more important factors in predicting the same. Future randomized controlled trials are needed to validate the findings of the study.
| 1. | Harris E, Clement N, MacLullich A, Farrow L. The impact of an ageing population on future increases in hip fracture burden. Bone Joint J. 2024;106-B:62-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 36] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 2. | Makaram NS, Hall AJ, Clement ND, MacLullich AJ, Simpson AHRW. Lessons learned from hip fracture registries - From the Scottish perspective to global practice. Injury. 2023;54 Suppl 5:110935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Dong Y, Zhang Y, Song K, Kang H, Ye D, Li F. What was the Epidemiology and Global Burden of Disease of Hip Fractures From 1990 to 2019? Results From and Additional Analysis of the Global Burden of Disease Study 2019. Clin Orthop Relat Res. 2023;481:1209-1220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 108] [Article Influence: 36.0] [Reference Citation Analysis (0)] |
| 4. | Hadjimichael AC. Hip fractures in the elderly without osteoporosis. J Frailty Sarcopenia Falls. 2018;3:8-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | George J, Sharma V, Farooque K, Mittal S, Trikha V, Malhotra R. Injury Mechanisms of Hip Fractures in India. Hip Pelvis. 2021;33:62-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Lim SK, Choi K, Heo NH, Kim Y, Lim JY. Characteristics of fragility hip fracture-related falls in the older adults: A systematic review. J Nutr Health Aging. 2024;28:100357. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 16] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 7. | Azevedo DC, Hoff LS, Kowalski SC, de Andrade CAF, Trevisani VFM, de Melo AKG. Risk factors for osteoporotic hip fracture among community-dwelling older adults: a real-world evidence study. Adv Rheumatol. 2024;64:8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 8. | Fischer H, Maleitzke T, Eder C, Ahmad S, Stöckle U, Braun KF. Management of proximal femur fractures in the elderly: current concepts and treatment options. Eur J Med Res. 2021;26:86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 117] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 9. | Mao W, Chang SM, Zhang YQ, Li Y, Du SC, Hu SJ, Yang A, Zhou KH. Positive medial cortical support versus anatomical reduction for trochanteric hip fractures: Finite element analysis and biomechanical testing. Comput Methods Programs Biomed. 2023;234:107502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 10. | Agarwal N, Feng T, Maclullich A, Duckworth A, Clement N. Early mobilisation after hip fracture surgery is associated with improved patient outcomes: A systematic review and meta-analysis. Musculoskeletal Care. 2024;22:e1863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 30] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 11. | Aprisunadi, Nursalam N, Mustikasari M, Ifadah E, Hapsari ED. Effect of Early Mobilization on Hip and Lower Extremity Postoperative: A Literature Review. SAGE Open Nurs. 2023;9:23779608231167825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 39] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 12. | Tang W, Wang Y, He Y, Liu B, Yuan R, Zhou Y, Huang H. Effect of early rehabilitation on hospital stay and postoperative complications in elderly hip fracture patients: a prospective cohort study. J Orthop Surg Res. 2025;20:84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 13. | Chang SM, Zhang YQ, Ma Z, Li Q, Dargel J, Eysel P. Fracture reduction with positive medial cortical support: a key element in stability reconstruction for the unstable pertrochanteric hip fractures. Arch Orthop Trauma Surg. 2015;135:811-818. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 204] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 14. | Ling L, Qu Z, Zhou K. Effect of Fracture Reduction with Different Medial Cortical Support on Stability After Cephalomedullary Nail Fixation of Unstable Pertrochanteric Fractures: A Biomechanical Analysis. Indian J Orthop. 2022;56:34-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 15. | Xie W, Shi L, Zhang C, Cui X, Chen X, Xie T, Zhang S, Chen H, Rui Y. Anteromedial cortical support reduction of intertrochanteric fractures-A review. Injury. 2024;55:111926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Huang X, Zuo Q, Zhou H, Lv T, Liu J. The use of intramedullary reduction techniques in the treatment of irreducible intertrochanteric femoral fractures with negative medial cortical support. Front Surg. 2024;11:1391718. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Li X, Zhao C, Sun G, Liu P, Tang J, Yang F, Wang X. Accurate reduction of medial arch fracture fragments in intertrochanteric fractures: A novel technical note. Front Surg. 2023;10:1140250. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Wähnert D, Greiner J, Brianza S, Kaltschmidt C, Vordemvenne T, Kaltschmidt B. Strategies to Improve Bone Healing: Innovative Surgical Implants Meet Nano-/Micro-Topography of Bone Scaffolds. Biomedicines. 2021;9:746. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 19. | Ghiasi MS, Chen J, Vaziri A, Rodriguez EK, Nazarian A. Bone fracture healing in mechanobiological modeling: A review of principles and methods. Bone Rep. 2017;6:87-100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 254] [Cited by in RCA: 289] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 20. | Mehl J, Farahani SK, Brauer E, Klaus-Bergmann A, Thiele T, Ellinghaus A, Bartels-Klein E, Koch K, Schmidt-Bleek K, Petersen A, Gerhardt H, Vogel V, Duda GN. External Mechanical Stability Regulates Hematoma Vascularization in Bone Healing Rather than Endothelial YAP/TAZ Mechanotransduction. Adv Sci (Weinh). 2024;11:e2307050. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 21. | Ma Q, Miri Z, Haugen HJ, Moghanian A, Loca D. Significance of mechanical loading in bone fracture healing, bone regeneration, and vascularization. J Tissue Eng. 2023;14:20417314231172573. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 89] [Article Influence: 29.7] [Reference Citation Analysis (0)] |
| 22. | Kaufer H. Mechanics of the treatment of hip injuries. Clin Orthop Relat Res. 1980;146:53-61. [PubMed] |
| 23. | Sharma G, kumar G N K, Yadav S, Lakhotia D, Singh R, Gamanagatti S, Sharma V. Pertrochanteric fractures (AO/OTA 31-A1 and A2) not amenable to closed reduction: causes of irreducibility. Injury. 2014;45:1950-1957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Ren H, Ao R, Wu L, Jian Z, Jiang X, Yu B. Effect of lesser trochanter posteromedial wall defect on the stability of femoral intertrochanteric fracture using 3D simulation. J Orthop Surg Res. 2020;15:242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 25. | Chang SM, Zhang YQ, Du SC, Ma Z, Hu SJ, Yao XZ, Xiong WF. Anteromedial cortical support reduction in unstable pertrochanteric fractures: a comparison of intra-operative fluoroscopy and post-operative three dimensional computerised tomography reconstruction. Int Orthop. 2018;42:183-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 26. | Chen SY, Chang SM, Tuladhar R, Wei Z, Xiong WF, Hu SJ, Du SC. A new fluoroscopic view for evaluation of anteromedial cortex reduction quality during cephalomedullary nailing for intertrochanteric femur fractures: the 30° oblique tangential projection. BMC Musculoskelet Disord. 2020;21:719. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 27. | Mao W, Ni H, Li L, He Y, Chen X, Tang H, Dong Y. Comparison of Baumgaertner and Chang reduction quality criteria for the assessment of trochanteric fractures. Bone Joint Res. 2019;8:502-508. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 52] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 28. | Rasheed MA, Amin MS, Chaudhry MN, Nadeem F, Mushtaq Khan A, Fatima A, Noor I. Role of Anteromedial Cortical Support for Unstable Intertrochanteric Fractures Being Treated With Cephalomedullary Nails. Cureus. 2024;16:e58303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 29. | Gotfried Y, Kovalenko S, Fuchs D. Nonanatomical reduction of displaced subcapital femoral fractures (Gotfried reduction). J Orthop Trauma. 2013;27:e254-e259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 30. | Mallya S, Kamath SU, Madegowda A, Krishnamurthy SL, Jain MK, Holla R. Comparison of radiological and functional outcome of unstable intertrochanteric femur fractures treated using PFN and PFNA-2 in patients with osteoporosis. Eur J Orthop Surg Traumatol. 2019;29:1035-1042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 31. | Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77:1058-1064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 865] [Cited by in RCA: 914] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 32. | Orthogeriatrics: The Management of Older Patients with Fragility Fractures [Internet]. Cham (CH): Springer, 2021 . [PubMed] |
| 33. | Binder EF, Brown M, Sinacore DR, Steger-May K, Yarasheski KE, Schechtman KB. Effects of extended outpatient rehabilitation after hip fracture: a randomized controlled trial. JAMA. 2004;292:837-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 264] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 34. | Lalwani SS, Jain DS, Phansopkar PA, Lakkadsha TM, Saifee SS. Physiotherapy Rehabilitation to Recuperate a Patient From an Intertrochanteric Fracture: A Case Report. Cureus. 2022;14:e27660. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 35. | Lee KJ, Um SH, Kim YH. Postoperative Rehabilitation after Hip Fracture: A Literature Review. Hip Pelvis. 2020;32:125-131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 36. | Phang JK, Lim ZY, Yee WQ, Tan CYF, Kwan YH, Low LL. Post-surgery interventions for hip fracture: a systematic review of randomized controlled trials. BMC Musculoskelet Disord. 2023;24:417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 37. | McDonough CM, Harris-Hayes M, Kristensen MT, Overgaard JA, Herring TB, Kenny AM, Mangione KK. Physical Therapy Management of Older Adults With Hip Fracture. J Orthop Sports Phys Ther. 2021;51:CPG1-CPG81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 142] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/