Published online Apr 18, 2025. doi: 10.5312/wjo.v16.i4.105273
Revised: March 5, 2025
Accepted: March 31, 2025
Published online: April 18, 2025
Processing time: 90 Days and 22.9 Hours
Although total hip arthroplasty (THA) is an established intervention for advanced hip disorders, not all patients achieve the anticipated functional improvements.
To investigate the impact of various preoperative factors on clinical outcomes after THA.
Data of 411 patients who underwent unilateral THA were retrospectively ana
Our results indicated that age and the WOMAC, Center for Epidemiologic Studies Depression Scale, and Central Sensitization Index (CSI) scores significantly predicted the modified Harris Hip Score outcomes, whereas age and preoperative WOMAC, EuroQol 5 dimensions, Center for Epidemiologic Studies Depression Scale, CSI, and Pain Detect Questionnaire scores were significant predictors of WOMAC outcomes. Age, WOMAC, and CSI were consistently significant factors. There were no significant differences in the operative time or blood loss across the outcome categories.
Our findings highlight the importance of preoperative assessment of central sensitization and psychological parameters. Patient-specific preoperative characteristics may play a greater role than intraoperative factors in determining recovery outcomes after THA.
Core Tip: This study reveals that preoperative factors, particularly central sensitization (Central Sensitization Index), psychological status (Center for Epidemiologic Studies Depression Scale), and functional impairment (Western Ontario and McMaster Universities Osteoarthritis Index), significantly influence recovery outcomes after total hip arthroplasty. Unlike intraoperative factors, these patient-specific characteristics strongly predicted clinical scores at six months postoperatively. Notably, age, Western Ontario and McMaster Universities Osteoarthritis Index, and Central Sensitization Index were consistent predictors across outcomes, emphasizing the importance of comprehensive preoperative evaluations. These findings underscore the critical role of addressing central sensitization and psychological health in optimizing recovery after total hip arthroplasty, offering valuable insights for personalized patient management and improved functional outcomes in advanced hip disorder interventions.
- Citation: Nishiwaki T, Ishikura H, Masuyama Y, Fujita S, Hirose R. Impact of preoperative factors on clinical outcomes after total hip arthroplasty. World J Orthop 2025; 16(4): 105273
- URL: https://www.wjgnet.com/2218-5836/full/v16/i4/105273.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i4.105273
Total hip arthroplasty (THA) is one of the most frequently performed surgical procedures in orthopedic practice because of its remarkable success in alleviating pain and restoring function in patients with advanced hip disorders[1,2]. This intervention has proven to be highly effective for conditions such as osteoarthritis and femoral head necrosis, both of which can lead to severe pain, reduced mobility, and an overall decline in quality of life[3]. With its capacity to deliver significant improvements in pain relief and functional restoration, THA has a substantial impact on patients’ daily lives, enabling them to return to a level of activity and independence that was often unimaginable prior to surgery. As life expectancy continues to rise and the demand for joint replacement grows, understanding the factors influencing THA outcomes has never been more pertinent.
Although the efficacy of THA is well-documented, postoperative outcomes can vary considerably between individuals[4,5]. Although many patients experience marked improvements, some report ongoing pain or suboptimal functional gains. These variations underscore the need to examine the preoperative factors that may influence postoperative results, as the early identification of these factors can assist in optimizing patient selection, tailoring perioperative management, and guiding postoperative rehabilitation. By identifying the modifiable risk factors, clinicians can better predict the patients who are likely to experience optimal recovery, ultimately leading to personalized and effective care[4,5].
Recently, attention has been directed toward the impact of psychological and neurological factors on THA outcomes. Central sensitization, a condition characterized by an amplified response to pain due to heightened central nervous system sensitivity, has been increasingly recognized as a significant contributor to prolonged pain and limited functional recovery after THA[6-9]. Patients with elevated central sensitization indices often report higher levels of postoperative pain and disability, suggesting that this factor may predict poorer outcomes. Neuropathic pain, measured using tools such as the Pain Detect Questionnaire (PDQ), is also of interest because of its potential adverse impact on long-term recovery[10,11]. Unlike nociceptive pain, neuropathic pain may not respond adequately to conventional analgesics, further complicating the postoperative management and rehabilitation.
Psychological factors, particularly depression and anxiety, are important considerations in surgical recovery[12,13]. The prevalence of depression among patients with chronic pain is high and those who experience significant psychological distress before surgery often report less satisfactory outcomes after THA. Depression and anxiety can contribute to increased perception of pain, decreased motivation for rehabilitation, and generally poorer functional outcomes. This has led to a growing consensus on the importance of including mental health assessment in preoperative evaluations[14]. Incorporating measures such as the Center for Epidemiologic Studies Depression Scale (CES-D) and EuroQol 5 dimensions (EQ5D) provides a more holistic understanding of a patient’s psychological state, which can be instrumental in planning postoperative care.
Despite a comprehensive body of literature examining individual factors, there remains a need to collectively analyze these variables to ascertain the preoperative factors that have the most predictive power for postoperative outcomes. We hypothesize that specific preoperative factors, including age, psychological distress (e.g., depression and anxiety), neuropathic pain, and central sensitization, significantly influence post-THA functional outcomes. Preoperative identification of these factors may allow for better risk stratification and personalized perioperative management to optimize recovery. This study aimed to evaluate the impact of a range of preoperative factors on clinical outcomes after THA using validated tools such as the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and modified Harris Hip Score (mHHS) as outcome measures. By focusing on these scores, which capture both pain and functional capacity, this study endeavored to provide a multidimensional perspective on recovery six months post-surgery.
The study protocol was approved by the Institutional Review Board, approval No. 2023-36 on January 15, 2024. The requirement for informed consent was waived due to the retrospective nature of this study. This study included 528 patients diagnosed with hip osteoarthritis who underwent unilateral THA at our institution between January 2020 and April 2024. Patients who required a posterior approach due to factors such as pseudarthrosis following pelvic osteotomy or residual metal implants were excluded. Additionally, cases lacking complete preoperative or postoperative data were excluded. Furthermore, two cases of periprosthetic femoral fractures that occurred during surgery or within one month postoperatively were excluded from the analysis. No cases of postoperative complications such as infection or thromboembolic events, which could have influenced rehabilitation outcomes, were observed. After these exclusions, a total of 411 hips were analyzed in this study. All surgeries were performed with the direct anterior approach using the interval between the tensor fasciae latae and sartorius muscles by the same surgeon (Toru Nishiwaki) to maintain procedural consistency. The joint capsule was incised anteriorly and preserved wherever possible.
Postoperative outcomes were assessed using the WOMAC score and mHHS. The WOMAC, a widely validated tool, assesses pain, stiffness, and functional limitations, specifically in patients with osteoarthritis, whereas the mHHS provides a comprehensive evaluation of hip functionality. In this study, WOMAC scores were evaluated by the nursing staff during preoperative and postoperative outpatient visits, and mHHS evaluations were conducted by physical therapists. The data were analyzed to determine the correlations between preoperative factors, including age; body mass index (BMI); mHHS; and WOMAC, PDQ, EQ5D, CES-D, and Central Sensitization Index (CSI) scores, and postoperative outcomes. The analysis was performed by dividing the patients into two groups: Those with a low postoperative mHHS (mHHS-low group) and those with a high postoperative mHHS (mHHS-high group). Additionally, the patients were divided into two groups based on their postoperative WOMAC scores: WOMAC-high and WOMAC-low. Statistical analyses included both univariate and multivariate techniques, allowing for a robust examination of the potential interactions between preoperative factors and their relative contributions to the outcomes. Student’s t-test was used to compare preoperative factors between the groups. Subsequently, multiple regression analysis was performed to identify significant predictors of postoperative mHHS and WOMAC scores after adjusting for potential confounders. Prior to regression analysis, a stepwise selection method was employed to identify the most significant predictors. The stepwise procedure involved both forward selection and backward elimination, with variables added or removed based on their statistical significance (P < 0.05). Additionally, the variance inflation factor was calculated to evaluate the multicollinearity among the selected variables, ensuring the stability and reliability of the regression model.
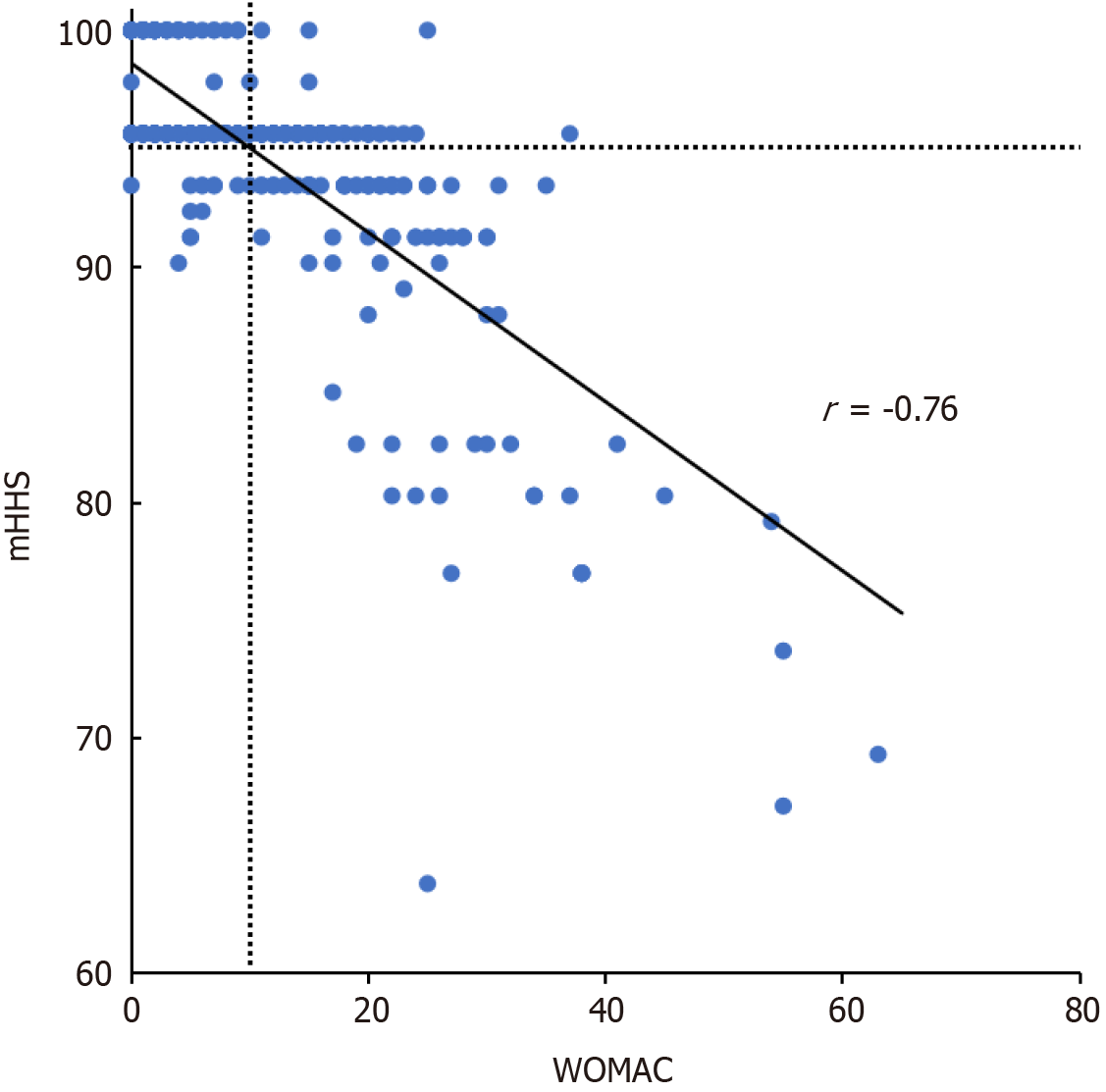
The mean postoperative WOMAC scores and mHHS were 10.8 and 94.8, respectively, showing a strong correlation between them (Figure 1). Among the WOMAC scores, 181 were above average and 230 were below average, whereas for the mHHS, 110 were above average and 301 were below average. Patients in the mHHS-low group were significantly older and had poorer preoperative mHHS and WOMAC, EQ5D, CES-D, PDQ, and CSI scores. Patients in the WOMAC-high group were significantly older and had poorer preoperative WOMAC, CES-D, PDQ, and CSI scores (Table 1). Multiple regression analysis identified age and WOMAC, CES-D, and CSI scores as significant predictors of mHHS outcomes, whereas age and preoperative WOMAC, EQ5D, CES-D, CSI, and PDQ scores were significant predictors of WOMAC outcomes. All the remaining predictors showed a variance inflation factor of < 10, indicating minimal multicollinearity (Table 2). The mean operative times were similar between the groups: 69 ± 16 minutes for both the above- and below-average WOMAC groups and 68 ± 16 minutes for the above-average and 71 ± 17 minutes for the below-average mHHS groups. Similarly, the mean blood loss did not significantly differ between the groups, indicating consistent intraoperative parameters irrespective of the postoperative score categories.
| Characteristics | Age | mHHS | WOMAC | EQ5D | CES-D | PDQ | CSI |
| mHHS-low | 70 ± 11 | 57 ± 14 | 50 ± 17 | 0.47 ± 0.16 | 17 ± 9 | 11 ± 7 | 25 ± 12 |
| mHHS-high | 66 ± 10 | 60 ± 13 | 38 ± 16 | 0.51 ± 0.17 | 13 ± 7 | 8 ± 6 | 18 ± 11 |
| P value | < 0.01b | < 0.05a | < 0.01b | < 0.05a | < 0.01b | < 0.01b | < 0.01b |
| WOMAC-high | 70 ± 10 | 58 ± 14 | 47 ± 16 | 0.48 ± 0.17 | 16 ± 8 | 11 ± 8 | 24 ± 12 |
| WOMAC-low | 65 ± 11 | 61 ± 13 | 37 ± 16 | 0.51 ± 0.17 | 12 ± 7 | 7 ± 6 | 17 ± 11 |
| P value | < 0.01b | P = 0.051 | < 0.01b | P = 0.161 | < 0.01b | < 0.01b | < 0.01b |
| Total | 67 ± 11 | 59 ± 14 | 41 ± 17 | 0.50 ± 0.17 | 14 ± 8 | 9 ± 7 | 20 ± 12 |
Our findings demonstrate that age, central sensitization, neuropathic pain, and psychological distress significantly predict post-THA functional outcomes. Notably, higher preoperative WOMAC and CSI scores were strongly associated with worse postoperative outcomes, underscoring the importance of addressing these factors preoperatively. Our findings corroborate the established value of both WOMAC scores and mHHS in assessing the clinical outcomes of THA. These scoring systems complement each other, with the WOMAC scores emphasizing pain, stiffness, and function, whereas the mHHS offers a broader evaluation of hip function. Various preoperative factors have been identified as potential predictors of THA outcomes. These include demographic factors such as age and BMI[15], as well as clinical variables, including preoperative pain levels, functional impairment, and comorbidities.
Notably, age emerged as a significant predictor of THA outcomes, which is consistent with previous study findings showing that older patients often experience slower recovery and diminished improvement in functional outcomes. These findings suggest the need for age-adjusted rehabilitation programs tailored to specific challenges faced by older patients. BMI plays a role, as higher values have been associated with a greater risk of complications and reduced functional recovery[15]. However, our study found that BMI was not a significant contributing factor. Preoperative functional impairment, as reflected by the WOMAC score and mHHS, also significantly impacted postoperative recovery[16]. The greater the preoperative disability, the worse the postoperative outcomes. Therefore, setting realistic expectations for patients with varying levels of preoperative functional impairment and conducting thorough preoperative assessments are crucial.
Central sensitization and neuropathic pain were identified as important predictors of outcomes, as measured by the PDQ and CSI scores. Central sensitization, with its characteristic heightened pain sensitivity, is increasingly being recognized as a contributor to chronic pain and poor outcomes in THA[17,18]. Patients with higher levels of central sensitization may benefit from preoperative interventions aimed at mitigating this risk, such as pharmacological or cognitive-behavioral therapy[18]. Psychological factors, particularly depression and anxiety, negatively affect postoperative recovery. This finding aligns with that of previous research demonstrating that patients with psychological comorbidities often report higher pain levels and greater functional limitations post-THA[19,20]. Consequently, preoperative psychological assessments should be standard practice because addressing mental health conditions prior to surgery could facilitate better postoperative outcomes.
Among the preoperative factors examined, multiple regression analysis identified age and the WOMAC, CES-D, CSI, EQ5D, and PDQ scores as explanatory variables after excluding multicollinearity and confounding variables. Notably, age and the WOMAC and CSI scores were the common significant factors. Interestingly, our findings showed no significant differences in operative time or blood loss across the groups, suggesting that the variability in outcomes was more strongly influenced by preoperative characteristics than by intraoperative factors. This underscores the importance of personalized perioperative strategies that address specific preoperative physical and psychological needs.
Although this study offers valuable insights, it has some limitations. This study exclusively focused on THA performed using direct anterior approach by a single surgeon, which limits the generalizability of our findings to other surgical approaches such as the posterior or lateral approaches. While it offers advantages such as muscle preservation and faster early recovery, it also presents challenges, including a steep learning curve and potential complications such as femoral fractures or nerve injuries. The lack of comparison with other approaches may limit the applicability of our findings to broader THA populations. Additionally, reliance on self-reported measures, such as the WOMAC and mHHS, may introduce subjective biases. Finally, this study did not analyze the potential impact of medical comorbidities, such as diabetes and cardiovascular diseases, and postoperative complications, including infection and deep vein thrombosis. Future multicenter studies that consider various surgical approaches, objective measures, comorbidities, and complications will contribute to a comprehensive understanding of THA outcomes.
In conclusion, this study underscores the importance of preoperative assessment in optimizing THA outcomes. By elucidating the preoperative factors that significantly influence postoperative recovery, this study aimed to contribute to the ongoing development of evidence-based protocols for THA. By incorporating evaluations of neuropathic pain, central sensitization, and mental health into routine preoperative protocols, our findings may assist clinicians in better predicting which patients are at greater risk of suboptimal outcomes, thereby optimizing surgical planning and ultimately improving the quality of care provided to individuals undergoing this life-changing procedure.
| 1. | Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370:1508-1519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1477] [Cited by in RCA: 1912] [Article Influence: 100.6] [Reference Citation Analysis (0)] |
| 2. | Blom AW, Donovan RL, Beswick AD, Whitehouse MR, Kunutsor SK. Common elective orthopaedic procedures and their clinical effectiveness: umbrella review of level 1 evidence. BMJ. 2021;374:n1511. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 101] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 3. | Ng CY, Ballantyne JA, Brenkel IJ. Quality of life and functional outcome after primary total hip replacement. A five-year follow-up. J Bone Joint Surg Br. 2007;89:868-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 114] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 4. | Anakwe RE, Jenkins PJ, Moran M. Predicting dissatisfaction after total hip arthroplasty: a study of 850 patients. J Arthroplasty. 2011;26:209-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 262] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 5. | Slaven EJ. Prediction of functional outcome at six months following total hip arthroplasty. Phys Ther. 2012;92:1386-1394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 6. | Hattori T, Shimo K, Niwa Y, Tokiwa Y, Matsubara T. Association of Chronic Pain with Radiologic Severity and Central Sensitization in Hip Osteoarthritis Patients. J Pain Res. 2021;14:1153-1160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 7. | Willett MJ, Siebertz M, Petzke F, Erlenwein J, Rushton A, Soldini E, Barbero M, Falla D. The Extent of Pain Is Associated With Signs of Central Sensitization in Patients With Hip Osteoarthritis. Pain Pract. 2020;20:277-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 8. | Ohashi Y, Fukushima K, Inoue G, Uchida K, Koyama T, Tsuchiya M, Uchiyama K, Takahira N, Takaso M. Central sensitization inventory scores correlate with pain at rest in patients with hip osteoarthritis: a retrospective study. BMC Musculoskelet Disord. 2020;21:595. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Wylde V, Sayers A, Lenguerrand E, Gooberman-Hill R, Pyke M, Beswick AD, Dieppe P, Blom AW. Preoperative widespread pain sensitization and chronic pain after hip and knee replacement: a cohort analysis. Pain. 2015;156:47-54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 123] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 10. | Blikman T, Rienstra W, van Raay JJAM, Dijkstra B, Bulstra SK, Stevens M, van den Akker-Scheek I. Neuropathic-like symptoms and the association with joint-specific function and quality of life in patients with hip and knee osteoarthritis. PLoS One. 2018;13:e0199165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 11. | Yamabe Y, Hasegawa M, Kobayashi G, Tone S, Naito Y, Sudo A. Neuropathic pain in patients with osteoarthritis of the hip before and after total hip arthroplasty. PLoS One. 2024;19:e0301352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 12. | Wilson L, Bekeris J, Fiasconaro M, Liu J, Poeran J, Kim DH, Gonzalez Della Valle A, Memtsoudis SG. Risk factors for new-onset depression or anxiety following total joint arthroplasty: the role of chronic opioid use. Reg Anesth Pain Med. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Hassett AL, Marshall E, Bailey AM, Moser S, Clauw DJ, Hooten WM, Urquhart A, Brummett CM. Changes in Anxiety and Depression Are Mediated by Changes in Pain Severity in Patients Undergoing Lower-Extremity Total Joint Arthroplasty. Reg Anesth Pain Med. 2018;43:14-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 53] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 14. | Nishiwaki T, Ishikura H, Yamamoto T. Pain characteristics in patients with hip osteoarthritis. J Joint Surg Res. 2024;2:168-172. [DOI] [Full Text] |
| 15. | Zhang B, Rao S, Mekkawy KL, Rahman R, Sarfraz A, Hollifield L, Runge N, Oni JK. Risk factors for pain after total hip arthroplasty: a systematic review. Arthroplasty. 2023;5:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 28] [Reference Citation Analysis (1)] |
| 16. | Quintana JM, Escobar A, Aguirre U, Lafuente I, Arenaza JC. Predictors of health-related quality-of-life change after total hip arthroplasty. Clin Orthop Relat Res. 2009;467:2886-2894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 118] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 17. | Yu H, Huang T, Lu WW, Tong L, Chen D. Osteoarthritis Pain. Int J Mol Sci. 2022;23:4642. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 94] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 18. | Imagama T, Okazaki T, Matsuki Y, Kaneoka T, Kawakami T, Yamazaki K, Sakai T. Negative correlation between central sensitization and forgotten joint score-12 after total hip arthroplasty. J Orthop Surg Res. 2023;18:691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 19. | O'Connor JP, Holden P, Gagnier JJ. Systematic review: preoperative psychological factors and total hip arthroplasty outcomes. J Orthop Surg Res. 2022;17:457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 32] [Reference Citation Analysis (0)] |
| 20. | Volcheck MM, Graham SM, Fleming KC, Mohabbat AB, Luedtke CA. Central sensitization, chronic pain, and other symptoms: Better understanding, better management. Cleve Clin J Med. 2023;90:245-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 88] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/