Published online Apr 18, 2025. doi: 10.5312/wjo.v16.i4.104452
Revised: March 5, 2025
Accepted: April 1, 2025
Published online: April 18, 2025
Processing time: 117 Days and 23.2 Hours
In the management of postoperative pain following total joint arthroplasty (TJA), the use of nonsteroidal anti-inflammatory drugs, including acetaminophen, plays a key role in alleviating pain. However, the comparison between intravenous and oral acetaminophen administration in patients undergoing full joint replacement surgery remains controversial.
To assess the effectiveness of intravenous and oral acetaminophen in alleviating pain and supporting rehabilitation following TJA.
PubMed, Embase and the Cochrane Library were comprehensively searched to identify cohort studies. The effects of intravenous and oral acetaminophen for managing pain and supporting rehabilitation following TJA were analysed using randomized controlled trials. PRISMA guidelines were followed. The effectiveness of the administration routes was compared based on visual analogue scale (VAS) scores at 24 and 48 h, total morphine usage within 24 h, and total duration of hospital stay.
The meta-analysis included seven studies comparing intravenous acetaminophen groups and oral acetaminophen groups. The results demonstrated that oral acetaminophen was comparable to intravenous acetaminophen with regard to VAS scores at 24 h and 48 h (P = 0.76 and 0.08, respectively). The difference in total morphine use between the two groups was not significant (P = 0.22). However, the total hospital stay duration of the intravenous acetaminophen groups was significantly reduced compared to the oral acetaminophen groups
After TJA surgery, intravenous injection of acetaminophen can shorten hospitalisation time and is suitable for rapid analgesia, Oral administration has become the preferred choice for mild cases due to its convenience and economy, providing a basis for clinical drug selection.
Core Tip: Oral acetaminophen shows similar pain management after total joint arthroplasty (TJA) which compared with intravenous acetaminophen. Intravenous acetaminophen was not found to be superior to oral acetaminophen in patients undergoing TJA in terms of visual analogue scale score at 24, 48 h, total morphine consumption. However, it can significantly reduce the length of hospital stay. Higher-quality randomized controlled trials are required for further research in the future.
- Citation: Lu B, Tian AX, Fan ZR, Zhao XW, Jin HZ, Ma JX, Ma XL. Effectiveness of oral vs intravenous acetaminophen on pain management following total joint arthroplasty: A systematic review and meta-analysis. World J Orthop 2025; 16(4): 104452
- URL: https://www.wjgnet.com/2218-5836/full/v16/i4/104452.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i4.104452
Total joint arthroplasty (TJA) provides an effective treatment for severe joint injuries caused by end-stage osteoarthritis and other diseases[1,2]. However, managing pain after TJA remains challenging, with opioids frequently being used as a common treatment option[3]. Moreover, poor postoperative rehabilitation and prolonged hospital stays are associated with inadequate pain management after TJA. Unfortunately, standardized protocols for managing pain following TJA are lacking[4]. Therefore, pain management following TJA remains controversial.
Currently, multimodal pain management is widely used to reduce postoperative pain after total joint replacement[5,6]. Given that opioid use can cause side effects like headaches and urinary retention, supportive modalities such as local anesthetic blocks, nonsteroidal anti-inflammatory drugs (NSAIDs), decadron and acetaminophen have gained importance.
Recently, acetaminophen, NSAIDs, has become commonly employed in pain management[7]. There is a difference in the comparison of pain control between intravenous and oral acetaminophen in patients undergoing TJA surgery. In their prospective, randomised, double-blind, placebo trial, O’Neal et al[8] observed no distinction between intravenous acetaminophen and oral acetaminophen in patients undergoing TJA. Stundner et al[9] reported more beneficial outcomes for oral acetaminophen compared with intravenous acetaminophen. Thus, the efficacy and safety of administering intravenous vs oral acetaminophen in patients undergoing TJA are still subjects of debate. This study aims to evaluate the efficacy and safety of intravenous and oral administration of acetaminophen in TJA through systematic review and meta-analysis.
The analysis method of this study was performed in accordance with the PRISMA standard and has been approved by the Ethics Committee of Tianjin Hospital (No. 2025 Medical Ethics Review 007).
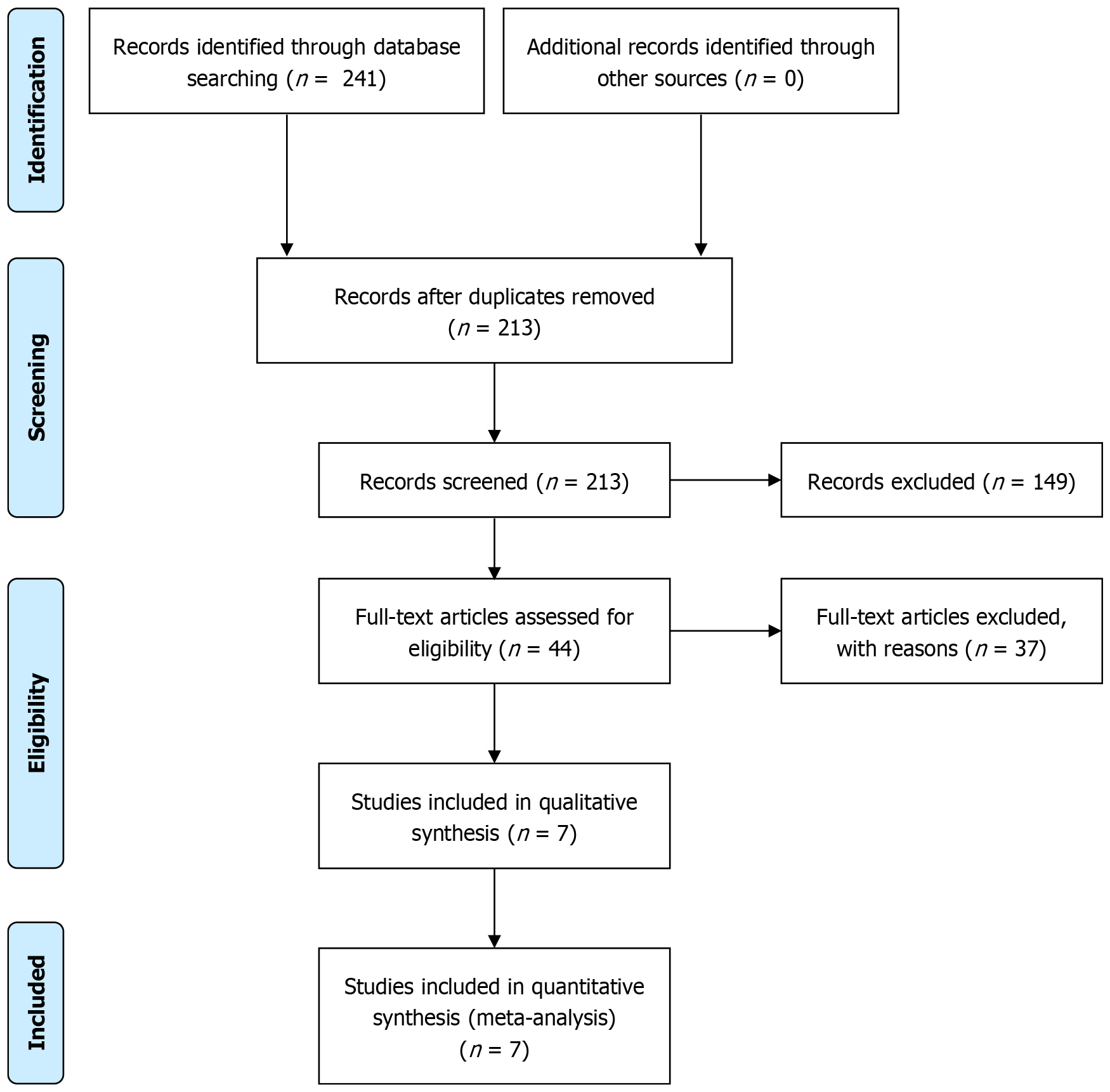
To comprehensively collect relevant literature, PubMed, Embase, and Cochrane Library were searched, with indexing up to March 2021, focusing on obtaining randomized controlled trials (RCTs), cohort studies, and controlled clinical trials. A comprehensive search was conducted with the search terms: “acetaminophen” OR “acetamidophenol” AND (“TKA” OR “THA” OR “total knee arthroplasty” OR “total hip replacement” [MeSH]). We did not impose any language restrictions to ensure coverage of the widest and most comprehensive literature resources possible. The search results are shown in Figure 1.
If a study complies with the population, intervention, control, outcome, and study design (PICOS) criteria, it is regarded as eligible for inclusion in a meta-analysis. Population: Patients planning to undergo total knee arthroplasty (TKA) or total hip arthroplasty (THA). Intervention: The patient group receiving intravenous acetaminophen for pain management after THA or TKA. Comparison: The control group received oral acetaminophen for the management of pain. Outcomes: Visual analogue scale (VAS) scores at 24 and 48 h, total morphine usage within 24 h, and total duration of hospital stay. Study design: Randomised controlled trials and retrospective studies.
The included literature in this study must meet the following criteria: (1) The research type is an acetaminophen study or case-control study; (2) The study population is all TJA patients; (3) The study population consisted of adult patients who underwent total knee replacement surgery; and (4) Literature published in the English language.
Furthermore, literature that meets the following types needs to be excluded: (1) When the same patient population has been studied multiple times and appears in multiple literature, articles with small sample sizes, earlier publication dates, or incomplete data should be excluded; (2) Research targeting special populations, such as patients with comorbidities of other serious illnesses; (3) A study that did not provide sufficient raw data to calculate drug dosage or length of hospital stay; and (4) Articles such as reviews and case reports.
All relevant literature was initially managed in EndNote, with duplicates systematically eliminated to ensure data integrity. The study was independently excluded by two researchers who reviewed the title and abstract of the article. Finally, this study performed an exclusion of information that did not satisfy the PICOS criteria. Senior reviewers will be consulted to resolve any discrepancies in the literature selection.
Two researchers extracted usable data based on a unified data extraction scheme without interfering with each other. After the extraction is completed, the two researchers cross check the data and resolve any differences through discussion or third-party arbitration. When necessary, refer to supplementary materials or cited references in the literature to obtain missing data.
This information mainly covers the basic information of the literature (author, research design, publication year), study population characteristics (sample size, patient age, gender distribution), intervention measures (dosage, frequency, course of treatment, and combination therapy of oral or injectable acetaminophen), as well as efficacy evaluation indicators (VAS scores at 24 and 48 h, opioid use within 24 h after surgery, and total hospital stay).
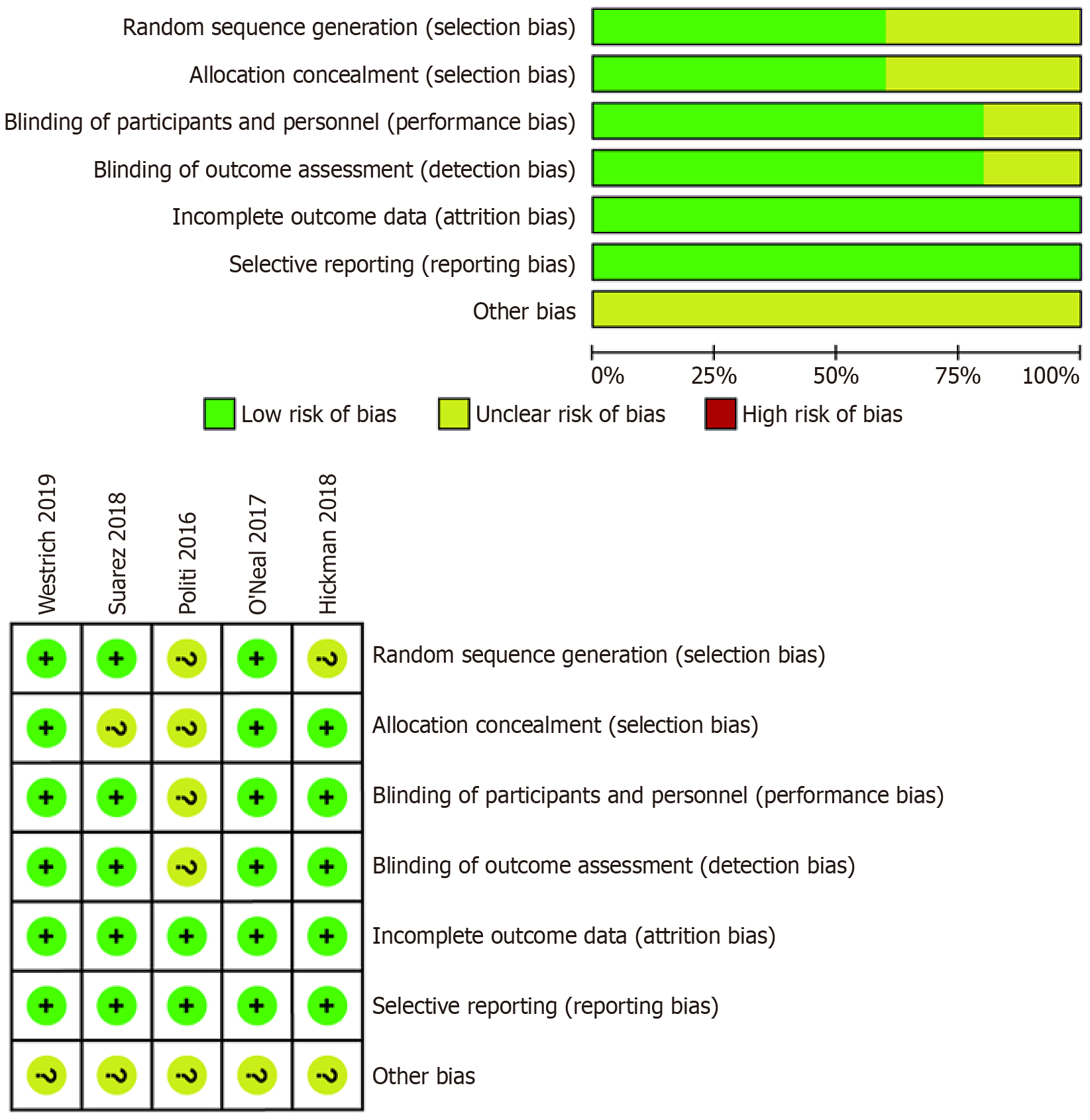
In the quality assessment process, the Cochrane risk of bias tool was used to conduct a systematic and detailed evaluation of all included RCTs. The assessment was conducted from seven dimensions: The handling of random mathematical risk factor allocation, the pathways and risk concealment after allocation, the blinding of researchers and participants, the blinding of outcome assessors, the completeness of result data, other potential biases and selective outcome reporting. Each study was evaluated as "low-risk", "high-risk", or "unclear", and in case of disagreement, a consensus was reached through a third researcher.
The methodological quality of non-RCTs was evaluated using the Non Randomized Study Methodology Index (MINORS) scale. Covering 12 items, including clarity of research objectives, data collection methods, applicability of outcome measures, blinding implementation, follow-up time and sample size justification, each study was evaluated by two independent evaluators. Based on their performance in various criteria, each item scored 0-2 to obtain the total score. During the quality assessment process, any disagreements between evaluators are resolved through discussion and consensus.
Use RevMan 5.3 for data processing (https://revman.cochrane.org/info). For continuous variables such as VAS score, total opioid consumption, and total duration of hospital stay, standardised mean difference (SMD) was used to compare the differences between groups and provide the accuracy range of SMD estimates using a 95% confidence interval (95%CI). The count data were combined using relative odds ratio (OR) and its 95%CI as effect measures. Cochrane's Q-test and I2 statistic were employed to evaluate the heterogeneity among the included studies. If there is substantial heterogeneity (P ≤ 0.10 or I2 ≥ 50%), such as 24-hour drug dosage, a random effects model is used; If there is no heterogeneity or heterogeneity is low (P > 0.10 and I2 < 50%), such as VAS scores at 24 and 48 h, a fixed effects model is used.
EndNote software was used to delete 28 duplicate studies. Based on the titles and abstracts, 149 studies unrelated to the research topic were excluded. Subsequently, after reading the full text, 37 studies were not included in the criteria and were further excluded. Finally, seven studies that met the inclusion criteria were included in the meta-analysis[8,10-15]. The specific screening process and research selection details can be found in the PRISMA flowchart (Figure 1)[16].
Table 1 lists the key details of seven studies involving 192515 cases. All studies assessed the efficacy and safety of intravenous and oral acetaminophen in alleviating postoperative pain following TJA. All seven included studies were conducted between 2016 and 2020, with five RCTs and two non-RCTs. Six studies assessed 24-hour VAS scores, and two studies presented 48-hour VAS scores. Six articles evaluated the total consumption of morphine within 24 h. The duration of hospital stay was reported by five studies.
| Studies | Cases | Mean age (year) | Female gender (%) | Type | Anesthesia | Surgical approach | Intervention group | Control group | Follow-up |
| Barrington et al[15], 2019 | 56475/134216 | 66/67 | 61.4/63.3 | Retrospective study | Unclear | TKA | 1000 mg of intravenous acetaminophen | 1000 mg of oral acetaminophen | Unclear |
| O'Neal et al[8], 2017 | 57/58 | 68/67 | 44/55 | RCT | Spinal anesthesia | TKA | 1000 mg of intravenous acetaminophen | 1000 mg of oral acetaminophen | 1 month |
| Suarez et al[11], 2018 | 52/52 | 66.6/67.3 | 28/26 | RCT | Spinal anesthesia | TKA | 4000 mg of intravenous acetaminophen | 4000 mg of oral acetaminophen | 6 weeks |
| Hickman et al[10], 2018 | 245/241 | 67/67 | 57.1/61.4 | RCT | General or spinal anesthesia | TKA | 1000 mg of intravenous acetaminophen | 2500 mg of oral acetaminophen | 8 weeks |
| Yu et al[12], 2020 | 318/527 | 66/65 | 70/73 | Retrospective study | Spinal anesthesia | TKA | 1000 mg of intravenous acetaminophen | 1000 mg of oral acetaminophen | Unclear |
| Politi et al[13], 2017 | 63/57 | 66/69 | 45/40 | RCT | General anesthesia | THA and TKA | 1000 mg of intravenous acetaminophen | 1000 mg of oral acetaminophen | 2 months |
| Westrich et al[14], 2019 | 77/77 | 63/65 | 64/55 | RCT | Spinal anesthesia | THA | 1000 mg of intravenous acetaminophen | 1000 mg of oral acetaminophen | Unclear |
The quality assessment chart of the RCT is shown in Figure 2. Random sequence generation was not addressed in two articles[10,13]. Four items were unclear in one study. One study did not describe allocation concealment in detail[11]. All other categories showed a low risk of bias. Two high-quality non-RCTs were evaluated using the MINORS database. Additional information is provided in Table 2.
| Quality assessment for non-RCT | Barrington | Yu |
| A clearly stated aim | 2 | 2 |
| Inclusion of consecutive patients | 2 | 2 |
| Prospective of data collection | 2 | 2 |
| Endpoints appropriate to the aim of the study | 2 | 2 |
| Unbiased assessment of the study endpoint | 1 | 1 |
| A follow-up period appropriate to the aims of study | 1 | 1 |
| Less than 5% loss to follow-up | 0 | 0 |
| Prospective calculation of the sample size | 2 | 2 |
| An adequate control group | 2 | 2 |
| Contemporary groups | 2 | 2 |
| Baseline equivalence of groups | 2 | 2 |
| Adequate statistical analyses | 2 | 2 |
| Total score | 20 | 20 |
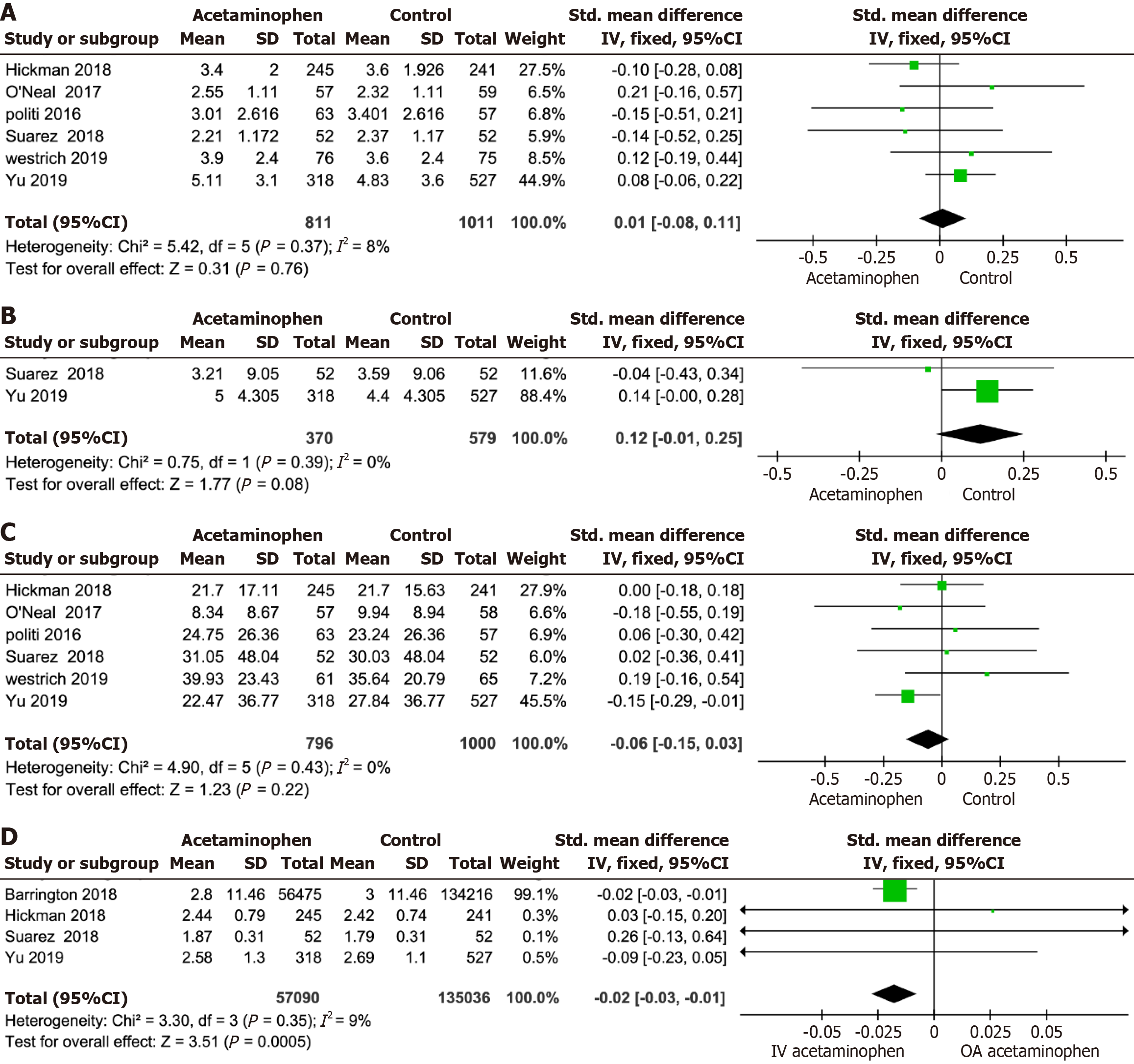
VAS score at 24 h: The summary data from six studies[8,10-14] reported VAS scores at 24 h. Compared to oral acetaminophen, there was no significant correlation between intravenous acetaminophen and a reduction in VAS scores (SMD = 0.01, 95%CI: -0.08 to 0.11, P = 0.76; Figure 3A. Due to the lack of observed statistical heterogeneity (χ2 = 5.42, df = 5, I² = 8%, P = 0.37), a fixed effects model was adopted.
VAS score at 48 h: Two studies provided VAS score data at 48 h[11,12], which showed no significant difference between the intravenous and oral acetaminophen groups (SMD = 0.12, 95%CI: -0.01 to 0.25, P = 0.08; Figure 3B Due to slight heterogeneity between studies, a fixed effects model was adopted (χ2 = 0.75, df = 1, I² = 0%, P = 0.39).
Total morphine usage at 24 h: Six studies among those included reported the total morphine usage at 24 h after TJA. There was no significant difference in the total morphine usage at 24 h between the intravenous injection group and the oral acetaminophen group (SMD = -0.06, 95%CI: -0.15 to 0.03, P = 0.22; Figure 3C Due to the statistical heterogeneity of the indicator data, a random effects model was adopted (χ2 = 4.9, df = 5, I² = 0%, P = 0.43).
Total duration of hospital stay: The total duration of hospital stay was evaluated by five studies among those included[8,10-12,15]. Compared with the oral acetaminophen group, intravenous acetaminophen injection showed significant differences in shortening hospitalisation time (SMD = -0.02, 95%CI: -0.03, -0.01, P = 0.0005; Figure 3D Since there was no significant heterogeneity between the studies, a fixed effects model was adopted (χ2 = 3.30, df = 3, I² = 9%, P = 0.35).
This study comprehensively evaluated the efficacy and role of intravenous and oral acetaminophen in pain control after TJA. Effective pain management is crucial for promoting the recovery of TJA patients after surgery. It not only helps to alleviate postoperative pain and shorten hospital stays but also reduces the occurrence of postoperative complications and medical expenses, thereby reducing the overall burden on patients. Existing studies and clinical data[9,17] have shown that intravenous injection of acetaminophen has significant and safe analgesic effects after TJA surgery. However, intravenous administration of acetaminophen is more expensive than oral acetaminophen (33.05 dollars vs 0.05 dollars)[13]. Although several studies have investigated oral administration as an alternative to intravenous administration in TJA, its comparative effectiveness remains controversial. This study conducted keyword analysis and selected seven relevant studies, including five RCTs and two non-RCTs. After data analysis, the results showed that oral acetaminophen had the same effect as intravenous acetaminophen on VAS scores data at 24 and 48 h, total morphine usage, and postoperative nausea. Therefore, oral administration should be considered as an inexpensive alternative to pain relief after TJA.
VAS score is a key indicator in this study, and comprehensive data show that intravenous injection and oral administration of acetaminophen have comparable effects in pain management after TJA surgery. Recent studies[12] have shown that although intravenous injection of acetaminophen can significantly improve pain relief within 2 h after surgery as a complementary treatment to various pain management strategies, there is no significant difference between intravenous injection of acetaminophen and other pain management methods within 24 and 48 h after surgery. Meanwhile, Politi et al[13] demonstrated that intravenous acetaminophen was more effective than oral acetaminophen during the first interval (0-4 h postoperatively). These results provide strong evidence for selecting appropriate analgesic regimens in clinical practice, suggesting that oral acetaminophen as a low-cost alternative treatment has similar effects as intravenous injection.
One of the important evaluation indicators for postoperative analgesic effect is the usage of morphine drugs. Despite the use of various analgesic measures to alleviate postoperative pain, the effectiveness of these methods is still limited in many cases. To further control pain, additional use of opioid drugs is usually required. However, the use of morphine drugs also brings some side effects, including discomfort such as nausea, dizziness, and other discomfort reactions, and prolonged use may also increase the risk of drug dependence[18,19]. Currently, intravenous acetaminophen is used to increase pain control. Sinatra et al[20] reported significantly lower total morphine usage in patients administered intravenous acetaminophen group compared with the placebo group. As an alternative to intravenous acetaminophen, oral acetaminophen has the same effect in terms of opioid side effects and opioid consumption[14]. This article indicates that patients who receive intravenous and oral acetaminophen after TJA use similar amounts of opioid drugs. This discovery may be related to the pharmacokinetic properties of acetaminophen. Whether taken orally or injected, acetaminophen exhibits high bioavailability and effectively inhibits prostaglandin synthesis, targeting both peripheral and central pathways. Therefore, the impact of the administration route on dosage may be relatively small.
The total duration of hospital stay is related to many factors, among which physiological status, age, and body mass index play important roles[21]. However, studies have shown that different routes of administration may have varying effects on the total duration of hospital stay. Hansen et al[22] demonstrated in a study involving 22828 hysterectomy cases that intravenous acetaminophen reduced hospital stay by 0.8 days and lowered hospitalisation costs by 2449 dollars compared to the oral acetaminophen group. Another study further supports this conclusion, Subramaniam et al[23] found that intravenous injection of acetaminophen combined with propofol and dexmedetomidine in the intensive care unit (ICU) of elderly patients after cardiac surgery marked decreased the occurrence of postoperative delirium and shortened ICU stay. These results indicate that intravenous injection of acetaminophen can effectively shorten hospital stay and accelerate postoperative recovery after hysterectomy and cardiac surgery. However, it is still unclear whether TJA surgery has the same effect. The results of this article indicate a statistically significant reduction in total hospital stay for the intravenous acetaminophen group compared to the oral group. Patients who received acetaminophen injections had shorter hospital stays, indicating that injection administration may have significant advantages in optimising postoperative recovery and shortening hospital stay after total joint replacement surgery. This result may be related to the rapid onset of injection administration and higher blood drug concentration, thereby reducing the patient’s need for additional analgesic drugs and shortening hospitalisation time. However, shortening hospitalization time may also be influenced by other factors such as the patient's baseline health condition, the type of surgery, and the quality of postoperative care[24], and should be carefully considered in clinical practice.
Although oral and intravenous acetaminophen shows comparable efficacy in pain management and dosage requirements, the advantage of intravenous administration in reducing hospital stays may enhance its appeal in specific clinical scenarios. For postoperative patients or those who require rapid pain relief, intravenous administration may be more appropriate. However, oral administration remains the preferred choice for many patients due to its convenience and lower cost. Future studies should investigate how different administration routes affect long-term patient outcomes, as well as the optimal administration strategies in different clinical contexts.
There are some limitations to this article: (1) The study only includes seven studies, with a relatively small sample size; The availability of more research will enhance our statistical analysis capabilities; (2) Due to the fact that meta-analysis only includes English language research, there may be publication bias; (3) The existing research lacks sufficient long-term follow-up; it is urgent to conduct long-term follow-up research; and (4) Among TJA postoperative recovery criteria, complications, such as nausea, are also important parameters; these findings require verification in a larger number of RCTs.
The efficacies of main management after TJA were similar between oral and intravenous acetaminophen. Intravenous acetaminophen was not superior to oral acetaminophen regarding VAS scores at 24 and 48 h and total morphine usage. However, intravenous acetaminophen significantly reduced the length of the hospital stay. These findings underscore the need for higher-quality RCTs.
The authors would like to thank Prof. Ma for his valuable suggestions and Dr. Tian for her assistance with data analysis.
| 1. | Wang Z, Levin JE, Amen TB, Arzani A, Manzi JE, Lane JM. Total Joint Arthroplasty and Osteoporosis: Looking Beyond the Joint to Bone Health. J Arthroplasty. 2022;37:1719-1725.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 2. | Patel KM, Mears SC, Barnes CL, Stambough JB, Stronach BM. Sepsis and Total Joint Arthroplasty. Orthop Clin North Am. 2022;53:13-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 3. | Zhang XL, Cheng T, Zeng BF; Chinese Medical Association; Chinese Orthopaedic Association. Experts' consensus on minimally invasive surgery for total joint arthroplasty. Orthop Surg. 2011;3:147-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Paredes AC, Pinto JM, Almeida A, Pinto PR. Predictive value of quantitative sensory testing for acute and chronic postsurgical pain after total joint arthroplasty: a systematic review. Pain. 2022;163:e385-e400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Karam JA, Schwenk ES, Parvizi J. An Update on Multimodal Pain Management After Total Joint Arthroplasty. J Bone Joint Surg Am. 2021;103:1652-1662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 50] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 6. | Hansen CW, Carlino EK, Saunee LA, Dasa V, Bhandutia AK. Modern Perioperative Pain Management Strategies to Minimize Opioids after Total Knee Arthroplasty. Orthop Clin North Am. 2023;54:359-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 7. | Lavand'homme PM, Kehlet H, Rawal N, Joshi GP; PROSPECT Working Group of the European Society of Regional Anaesthesia and Pain Therapy (ESRA). Pain management after total knee arthroplasty: PROcedure SPEcific Postoperative Pain ManagemenT recommendations. Eur J Anaesthesiol. 2022;39:743-757. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 164] [Article Influence: 41.0] [Reference Citation Analysis (0)] |
| 8. | O'Neal JB, Freiberg AA, Yelle MD, Jiang Y, Zhang C, Gu Y, Kong X, Jian W, O'Neal WT, Wang J. Intravenous vs Oral Acetaminophen as an Adjunct to Multimodal Analgesia After Total Knee Arthroplasty: A Prospective, Randomized, Double-Blind Clinical Trial. J Arthroplasty. 2017;32:3029-3033. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 55] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 9. | Stundner O, Poeran J, Ladenhauf HN, Berger MM, Levy SB, Zubizarreta N, Mazumdar M, Bekeris J, Liu J, Galatz LM, Moucha CS, Memtsoudis S. Effectiveness of intravenous acetaminophen for postoperative pain management in hip and knee arthroplasties: a population-based study. Reg Anesth Pain Med. 2019;44:565-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 10. | Hickman SR, Mathieson KM, Bradford LM, Garman CD, Gregg RW, Lukens DW. Randomized trial of oral versus intravenous acetaminophen for postoperative pain control. Am J Health Syst Pharm. 2018;75:367-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 11. | Suarez JC, Al-Mansoori AA, Kanwar S, Semien GA, Villa JM, McNamara CA, Patel PD. Effectiveness of Novel Adjuncts in Pain Management Following Total Knee Arthroplasty: A Randomized Clinical Trial. J Arthroplasty. 2018;33:S136-S141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Yu S, Eftekhary N, Wiznia D, Schwarzkopf R, Long WJ, Bosco JA, Iorio R. Evolution of an Opioid Sparse Pain Management Program for Total Knee Arthroplasty With the Addition of Intravenous Acetaminophen. J Arthroplasty. 2020;35:89-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 13. | Politi JR, Davis RL 2nd, Matrka AK. Randomized Prospective Trial Comparing the Use of Intravenous versus Oral Acetaminophen in Total Joint Arthroplasty. J Arthroplasty. 2017;32:1125-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 71] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 14. | Westrich GH, Birch GA, Muskat AR, Padgett DE, Goytizolo EA, Bostrom MP, Mayman DJ, Lin Y, YaDeau JT. Intravenous vs Oral Acetaminophen as a Component of Multimodal Analgesia After Total Hip Arthroplasty: A Randomized, Blinded Trial. J Arthroplasty. 2019;34:S215-S220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 15. | Barrington JW, Hansen RN, Lovelace B, Böing EA, Chughtai M, Newman JM, Pham AT, Khlopas A, Sodhi N, Sultan AA, Mont MA. Impact of Intravenous Acetaminophen on Lengths of Stay and Discharge Status after Total Knee Arthroplasty. J Knee Surg. 2019;32:111-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Grassini S. Virtual Reality Assisted Non-Pharmacological Treatments in Chronic Pain Management: A Systematic Review and Quantitative Meta-Analysis. Int J Environ Res Public Health. 2022;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 46] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 17. | Murata-Ooiwa M, Tsukada S, Wakui M. Intravenous Acetaminophen in Multimodal Pain Management for Patients Undergoing Total Knee Arthroplasty: A Randomized, Double-Blind, Placebo-Controlled Trial. J Arthroplasty. 2017;32:3024-3028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 18. | Zi-Yun X, Ruo-Lin Z, Yue-Wei X, Tao B. Efficacy and Safety of Oral Acetaminophen for Premature Infants With Patent Ductus Arteriosus: A Meta-Analysis. Front Pharmacol. 2021;12:696417. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 19. | Myler CS, Chapman MR, Eden BD, Lehman EB, Karamchandani K. Oral versus intravenous acetaminophen for perioperative pain management in adult patients undergoing non-cardiac surgery: A quantile segmented regression analysis. J Clin Anesth. 2023;90:111220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 20. | Sinatra RS, Jahr JS, Reynolds LW, Viscusi ER, Groudine SB, Payen-Champenois C. Efficacy and safety of single and repeated administration of 1 gram intravenous acetaminophen injection (paracetamol) for pain management after major orthopedic surgery. Anesthesiology. 2005;102:822-831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 308] [Cited by in RCA: 288] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 21. | Shadman KA, Edmonson MB, Coller RJ, Sklansky DJ, Nacht CL, Zhao Q, Kelly MM. US Hospital Stays in Children and Adolescents With Acetaminophen Poisoning. Hosp Pediatr. 2022;12:e60-e67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 22. | Hansen RN, Pham AT, Boing EA, Lovelace B, Wan GJ, Urman RD. Reduced length of stay and hospitalization costs among inpatient hysterectomy patients with postoperative pain management including IV versus oral acetaminophen. PLoS One. 2018;13:e0203746. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Subramaniam B, Shankar P, Shaefi S, Mueller A, O'Gara B, Banner-Goodspeed V, Gallagher J, Gasangwa D, Patxot M, Packiasabapathy S, Mathur P, Eikermann M, Talmor D, Marcantonio ER. Effect of Intravenous Acetaminophen vs Placebo Combined With Propofol or Dexmedetomidine on Postoperative Delirium Among Older Patients Following Cardiac Surgery: The DEXACET Randomized Clinical Trial. JAMA. 2019;321:686-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 240] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 24. | Skura BW, Goubeaux C, Passias BJ, Schuette HB, Melaragno AJ, Glazier MT, Faherty M, Burgette W. Increased length of stay following total joint arthroplasty based on insurance type. Arch Orthop Trauma Surg. 2023;143:2273-2281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/