Published online Apr 18, 2025. doi: 10.5312/wjo.v16.i4.103795
Revised: February 23, 2025
Accepted: March 6, 2025
Published online: April 18, 2025
Processing time: 137 Days and 18.8 Hours
Hook of hamate fractures occur either due to repetitive stress from gripping sports (e.g., golf, tennis, and baseball), leading to fatigue fracture, or as a result of trauma from falls or other injuries. The recommended treatment involves the excision of bone fragments to facilitate athletes’ early return to sports; excision surgery is also performed in trauma cases. However, some patients prefer nonsurgical treatment options, and conservative treatment should be considered.
To present a case series of 16 patients conservatively treated for hook of hamate fractures.
This study included 16 (11 males and 5 females; right side, 6 cases; left side, 10) patients who desired conservative treatment and could be followed-up until bone union was achieved. The average age of the patients was 49.6 (range: 24-72) years. The average time from injury to consultation was 4.3 (range: 0.2-21.4) weeks. The treatment involved 4 weeks of casting from the forearm to the metacarpophalangeal joint, followed by 8 weeks of splint fixation of the wrist. Follow-up computed tomography scans were performed every 4 weeks.
Bone union was achieved in all patients. The average duration of casting was 3.7 (range: 0-5) weeks and that of splint fixation thereafter was 8.6 (range: 0-28) weeks. The patients did not exhibit joint contractures or range of motion res
Conservative treatment with external fixation may be an option for hook of hamate fractures.
Core Tip: Hook of hamate fractures occur either due to repetitive stress in gripping sports or a traumatic occurrence. Some patients prefer nonsurgical treatment options and should consider conservative treatment. This study presented a case series of 16 patients conservatively treated for hook of hamate fractures. Bone union was achieved in all patients. Patients did not exhibit joint contractures or range of motion restrictions due to prolonged immobilization. Thus, conservative treatment with external fixation may be an option for hook of hamate fractures.
- Citation: Tanaka T, Yoshii Y. Sixteen patients regarding the conservative treatment for hook of hamate fracture. World J Orthop 2025; 16(4): 103795
- URL: https://www.wjgnet.com/2218-5836/full/v16/i4/103795.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i4.103795
A common cause of ulnar-sided wrist pain is a hook of hamate fracture, a relatively rare condition that accounts for approximately 2% of all carpal bone fractures. Its mechanism of injury often involves direct trauma (such as falling onto an outstretched hand) or repetitive stress, making this fracture more common in active individuals than in sedentary ones. The hook of hamate plays a critical role in hand function, serving as an attachment site for important structures, such as the transverse carpal ligament and flexor tendons. Because of their location, fractures of the hook can result in significant pain and functional impairment. However, diagnosing these fractures is challenging because they are often missed on standard radiographs, particularly when specialized views, such as oblique or carpal tunnel X-rays, are not used. This frequently leads to a delayed diagnosis and increases the risk of nonunion and persistent pain[1].
Generally, surgical excision is the preferred treatment for these fractures, especially in athletes seeking a quick return to activity. Surgery can relieve symptoms by removing the fractured fragment; however, it is associated with postoperative complications, such as reduced grip strength and ulnar nerve irritation[2,3]. Although surgery is often successful in resolving symptoms, it is not without risks, and not all patients, especially those who are not professional athletes, require or desire surgical intervention. In this article, we present a case series of 16 patients who were conservatively treated for hook of hamate fractures. We aimed to demonstrate that conservative management is a viable and effective option for these fractures, particularly in patients who prefer nonsurgical treatment. We discussed the clinical outcomes, including factors contributing to successful bone healing, and the conditions under which conservative treatment may be the most appropriate. Through this study, we aim to provide further support for the use of conservative treatment in managing hook of hamate fractures, offering an alternative approach to surgery for specific patients.
This study included 16 patients diagnosed with a hook of hamate fracture between January 2016 and June 2024, with a period of 8 years and 6 months. These patients opted for conservative treatment and were followed up until bone union was confirmed. The cohort included 11 males and 5 females, with 6 on the right side and 10 on the left side. The average age of the patients was 49.5 (range: 24-72) years. The average time from injury to consultation was 4.3 (range: 0.2-21.4) weeks.
For immobilization, we applied a cast extending from the proximal one-third of the forearm to the metacarpophalangeal joint. The wrist’s position during cast fixation was physiological (intrinsic plus position). Subsequently, a cock-up splint with ulnar deviation restriction was applied. During the period of splint immobilization, patients were allowed to remove the splint at times when vigorous movement of the fingers or wrist was not involved: For example, during bathing or sleeping. The average duration of cast immobilization was 3.8 (range: 0-6) weeks, followed by an average of 8.6 (range: 0-28) weeks of splint immobilization.
The causes of injury were a fall on an outstretched hand in all patients. According to the fracture classification[4], there was 1 case of type I (fracture at the tip), 1 case of type II (fracture at the central portion), and 14 cases of type III (fracture at the base). Detailed case presentations are summarized in Table 1. All 16 patients achieved bone union and were able to return to their pre-injury level of activity without any associated injuries, such as flexor tendon ruptures or nerve damage. The following are the specific case presentations. Adhering to the four principles of medical ethics (respect for autonomy, non-maleficence, beneficence, and justice), we prioritized patient dignity and provided treatment according to the described treatment protocol. No patients withdrew from the protocol. This study was conducted with approval from the Kikkoman General Hospital Ethics Committee, approval No. 2015-04.
| Case | Age | Gender | Left and right | Duration from injury | Type of fracture | Injury pattern | Cast immobilization (weeks) | Splint immobiraizaton (weeks) | VAS1 |
| Case 1 | 32 | 1 | Right | 0.2 | III | Fall down | 5 | 8.6 | 0 |
| Case 2 | 29 | 0 | Left | 4.3 | III | Fall down | 4 | 5 | 0 |
| Case 3 | 24 | 1 | Left | 0.2 | III | Fall down | 3 | 8 | 0 |
| Case 4 | 68 | 0 | Left | 1 | III | Fall down | 5 | 0 | 0 |
| Case 5 | 43 | 1 | Left | 3 | III | Fall down | 4 | 8 | 3 |
| Case 6 | 43 | 1 | Left | 17.1 | III | Fall down | 4 | 8 | 0 |
| Case 7 | 58 | 1 | Right | 2 | III | Fall down | 6 | 8 | 0 |
| Case 8 | 53 | 1 | Right | 0.6 | III | Fall down | 0 | 4 | 0 |
| Case 9 | 66 | 1 | Right | 0.4 | I | Falling off a bicycle | 4 | 8 | 3 |
| Case 10 | 61 | 0 | Right | 3 | III | Fall down | 4 | 8 | 0 |
| Case 11 | 72 | 0 | Left | 7 | III | Fall down | 4 | 28 | 0 |
| Case 12 | 52 | 1 | Left | 21.4 | III | Falling off a bicycle | 4 | 12 | 0 |
| Case 13 | 48 | 1 | Left | 2 | III | Falling while running | 4 | 8 | 0 |
| Case 14 | 63 | 1 | Left | 0.6 | III | Falling off a bicycle | 4 | 8 | 0 |
| Case 15 | 46 | 0 | Left | 4 | III | Falling in tennis | 3 | 8 | 0 |
| Case 16 | 35 | 1 | Right | 2 | II | Falling off a bicycle | 2 | 8 | 5 |
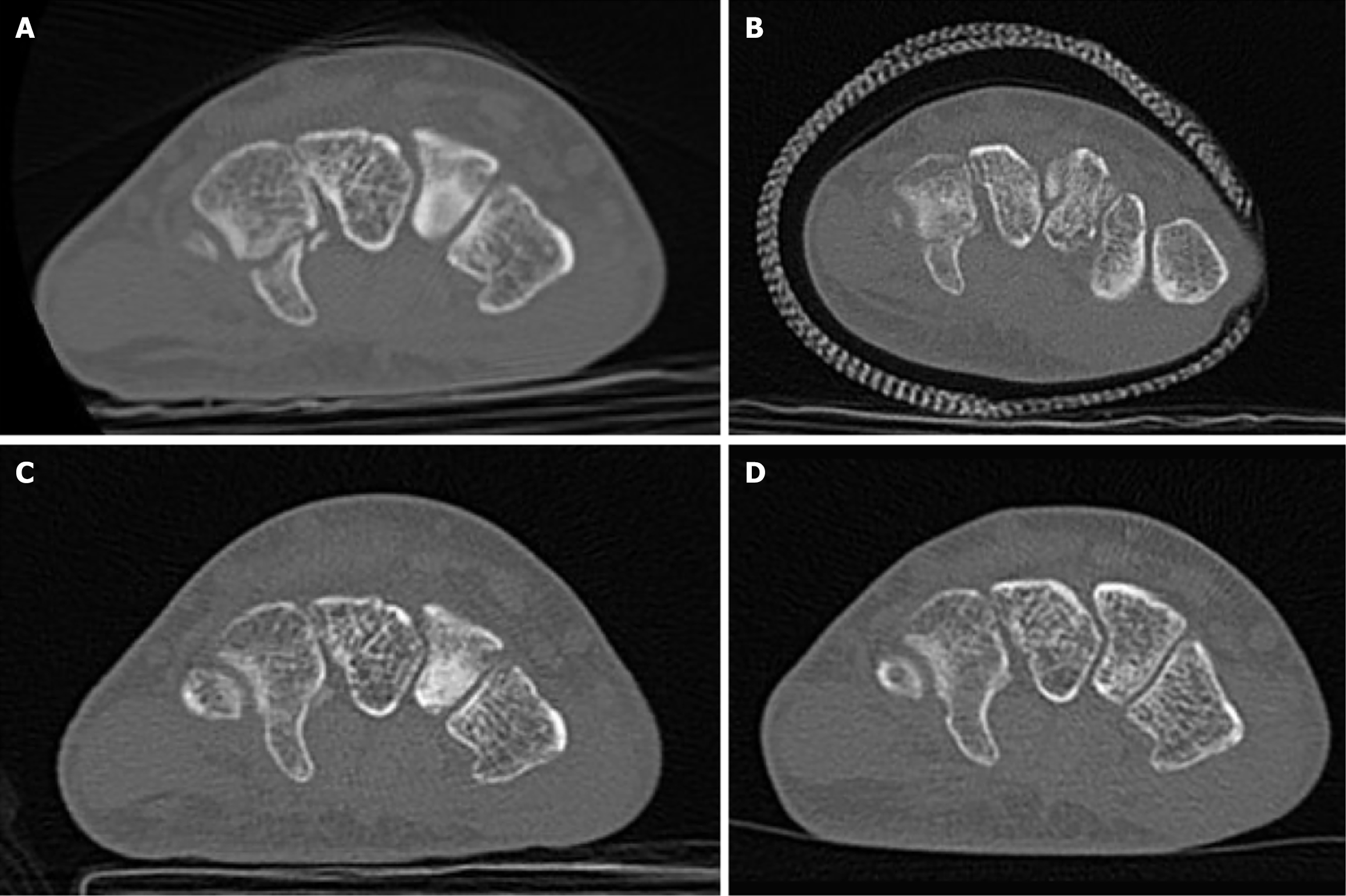
A 43-year-old man sustained a left-hand injury when he extended his arm forward during a fall (Figure 1). He initially sought treatment at a local clinic but remained undiagnosed, with pain persisting for 4 months before he sought further evaluation. He reported pain during golf swings and when putting weight on his hand. Upon clinical examination, tenderness was noted at the hook of hamate on the proximal ulnar side of the palm, and a type III hook of hamate fracture was confirmed on computed tomography (CT). The patient was treated with 4 weeks of cast immobilization and 8 weeks of splint immobilization, with instructions to avoid overexertion of the ring and little fingers. Two months after his initial clinic visit, the fracture healed, and remodeling was observed by the third month. Six months later, the patient was pain-free and had normal daily life.
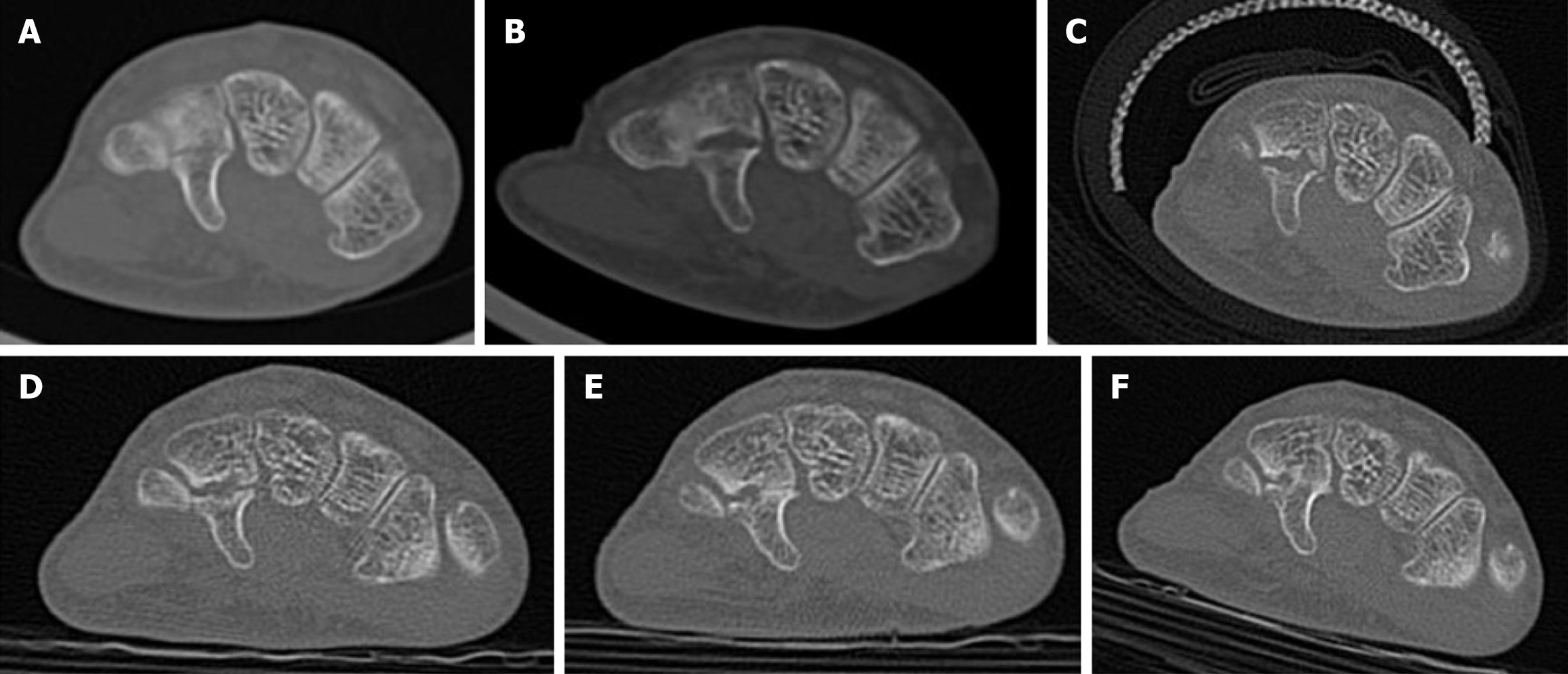
A 72-year-old woman sustained an injury from a fall while running and was treated with 6 weeks of cast immobilization at another hospital (Figure 2). However, owing to the development of nonunion, the patient was referred to our clinic. CT revealed separation at the fracture site. Considering that 7 weeks had passed since the injury, conservative treatment was selected. The patient underwent 4 weeks of cast immobilization, during which early bone bridging was observed, indicating callus formation. Splint immobilization was continued while the patient was under observation. During the splint period, no restrictions were placed on the patient’s participation in running or marathons. Full bone union was achieved 7 months after the injury. After the splint was removed, the patients were instructed to perform range-of-motion exercises using the opposite wrist as a reference. No restrictions in range-of-motion were observed. Given the patient's age, osteoporosis must be considered; however, this patient is highly active, completing full marathons in approximately 4 hours. They engage in daily training and have declined osteoporosis screening.
The hook of hamate protrudes prominently into the palmar region, forming Guyon’s canal on its ulnar side, together with the pisiform and pisohamate ligaments, through which the motor and sensory branches of the ulnar nerve pass. On the radial side, the transverse carpal ligament is attached to the tip of the hook of hamate, forming a part of the carpal tunnel. Muscles and ligaments that directly attach to the hook of hamate include the flexor digiti minimi brevis, opponens digiti minimi, and pisohamate ligament. Although the flexor digitorum profundus tendon does not directly attach to the hook of hamate, it wraps around the radial side of the hook during wrist ulnar deviation and little finger flexion, allowing the hook of hamate to function like a pulley[2,5].
Hook of hamate fractures have several characteristics. First, they are rare, accounting for only approximately 2% of all carpal bone fractures. Their injury mechanisms often include stress fractures caused by repetitive forces during sports, such as golf, baseball, and racket sports[6]. These fractures can also occur because of direct trauma, such as falling onto an outstretched hand[7]. One characteristic of hook of hamate fractures is the difficulty in achieving bone union. Blood supply to the hook of hamate is provided by one vessel from the radial side, nourishing the radial side of the base, and two smaller vessels from the medial side, nourishing the medial base and tip[8,9]. Although vascular issues have been considered, there are no reports of avascular necrosis, suggesting that muscle and ligament forces are more likely to affect healing than vascular factors[7]. Second, hook of hamate fractures are classified into three types based on their anatomical locations: Type I, distal tip; type II, middle part; and type III, base of the hook. Type III fractures account for 75% of all hook of hamate fractures, and it is more difficult to achieve bone union in type II fractures[4]. However, in our study, bone union was achieved across all fracture types. Finally, diagnosing hook of hamate fractures can be difficult. Oblique and carpal tunnel radiographs are necessary, but fracture lines are often obscured by overlapping carpal bones[10]. CT or magnetic resonance imaging is useful for definitive diagnosis[1,10]. In this study, we used CT for both the diagnosis and follow-up of bone healing.
Surgical excision of the fracture fragment is frequently performed[8], and open reduction and internal fixation is also an option[11,12]. However, postoperative complications have been reported in 25%-59% of cases, with some residual symptoms. Sheridan et al[6] performed excision surgery on 145 professional baseball players, reporting postoperative ulnar nerve numbness in 2 patients, pain at the surgical site in 6 patients, and heterotopic ossification in 1 patient. Additionally, a decrease in grip strength of 11%-15% following excision of the hook of hamate has been noted[2,3,13]. Although not without risk, excision remains the first-line treatment for athletes seeking a quick return to sports[4]. The average time from surgery to return to exercise or daily life was 12.3[11], 12.66 ± 11.58 weeks (15 case reports and 93 patients, range: 3 weeks to 1 year)[14], similar to the 12.6 weeks of immobilization in our cases of combined cast and splinting.
The high risk of nonunion associated with conservative treatment, causes of nonunion include poor blood supply to the hook of hamate[8,15], repetitive stress on the small fracture area[8], and delayed diagnosis[1]. The reported rates of nonunion are 6/25 (24%)[16], 5/6 (83%)[15,16], and 3/3 (100%)[8], with many of these cases requiring excision after 6 weeks of immobilization failed to achieve bone union. Early diagnosis and timely surgical intervention are often recommended[17], which is understandable. In our study, 4 of 16 (25%) patients presented > 6 weeks after injury, and although the healing process was slower, all patients eventually achieved full bone union. Whalen et al[17] reported that all six cases of acute fractures treated conservatively healed after an average immobilization period of 11 weeks, and one of two delayed cases achieved bone union after 28 weeks.
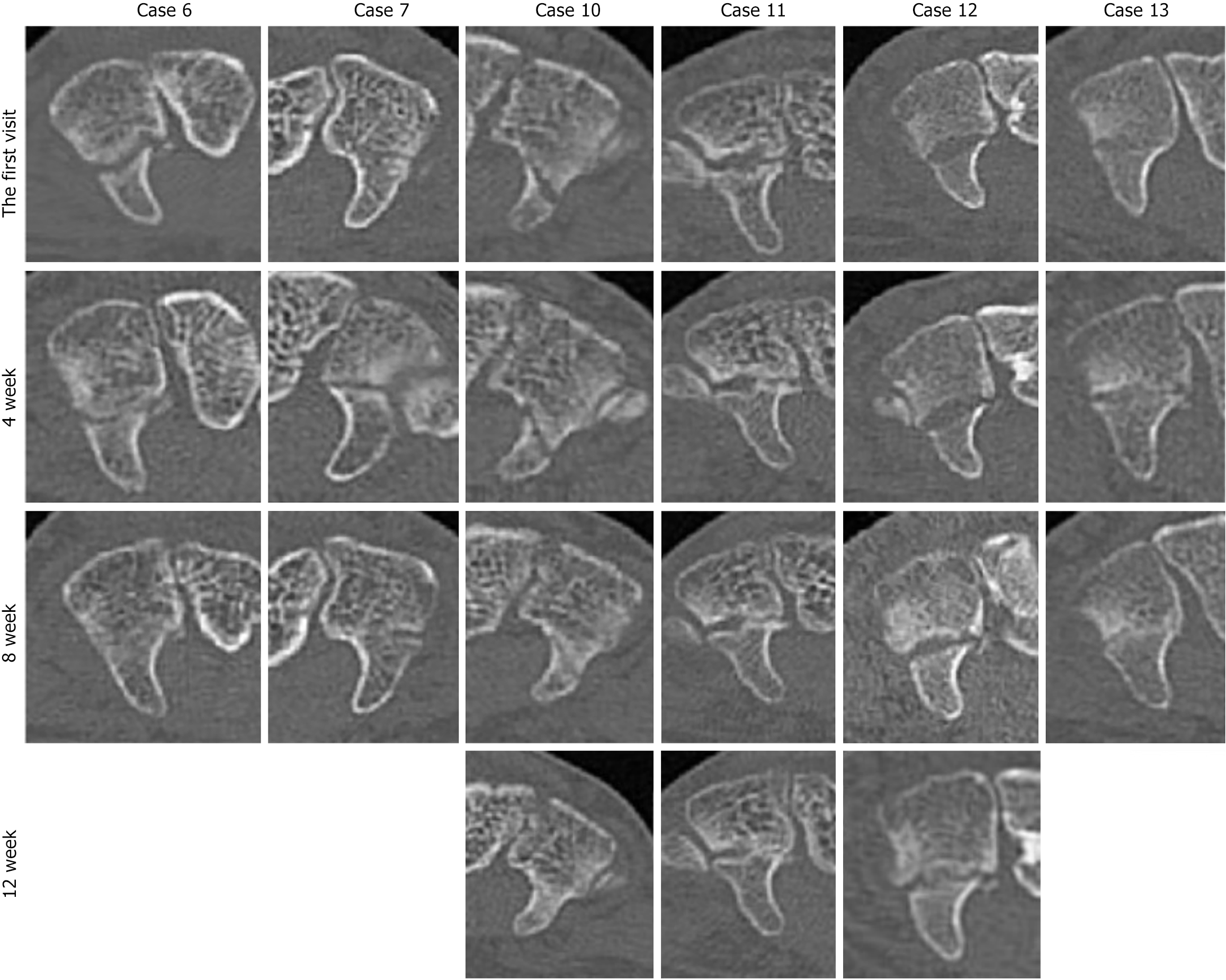
In previous reports, the conservative treatment period for fractures of the hook of the hamate is described as 6 weeks. Based on our investigation, we suggest that extending the immobilization period is more beneficial. Figure 3 tracks the bone-healing progress of our current cases using CT imaging. In cases with prolonged healing, such as cases 10, 11, and 12, gaps between bone fragments remained at 8 weeks. However, compared to those at 4 weeks, the gaps had narrowed and the volume of regenerated trabecular bone had increased. By 12 weeks, nearly complete union was observed. Similar to that for the hook of the hamate, the bone-healing patterns of the scaphoid, one of the carpal bones, have been studied using quantitative CT[18]. Scaphoid fractures are known for their prolonged healing time and high rates of nonunion. The healing of long bone fractures typically emphasizes the periosteal healing on the cortical bone side. However, in the case of the scaphoid, healing progresses from the trabecular bone side toward the cortical bone side[19], with an increase in trabecular bone volume at 12 weeks and completion by 26 weeks. Therefore, we recommend extending the observation period to 8 weeks or more.
The difference between scaphoid fractures and hook of hamate fractures lies in the dynamic impact on the fracture during wrist movement. Compared to the hook of hamate, the scaphoid has greater range of motion. In this study, the 16 patients had a splint applied from the 5th week, which included ulnar deviation restriction, thereby reducing the influence of the flexor tendons on the fracture site.
Furthermore, the reasons for our favorable results include the use of CT for follow-up observations and the implementation of wrist immobilization whenever possible. For the first 4 weeks, patients were subjected to rigid cast immobilization, followed by the use of a removable splint after the 5th week, while being advised to avoid activities that applied force on the ulnar side. After 5 weeks, no excessive restrictions on wrist immobilization were imposed. Consequently, even after 12 weeks, there was almost no observed limitation in the range of motion (Figure 4). Following splint removal, the patients performed range-of-motion exercises using the opposite wrist as a reference. The splint was designed to restrict ulnar flexion. Its application and removal were at the discretion of the patients, but they were advised to keep the splint on as much as possible. As a result, it is possible to achieve a range of motion in the wrist without significant side-to-side differences at an early stage. The limitations of this study include the small sample size. Additionally, in cases of sports injuries resulting from repetitive external forces, even if healing is achieved, there may be a high risk of recurrence, which could make such injuries unsuitable for treatment.
Conservative treatment can be considered an option for hook of hamate fractures.
| 1. | Bishop AT, Beckenbaugh RD. Fracture of the hamate hook. J Hand Surg Am. 1988;13:135-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 120] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 2. | Watson HK, Rogers WD. Nonunion of the hook of the hamate: an argument for bone grafting the nonunion. J Hand Surg Am. 1989;14:486-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 46] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Demirkan F, Calandruccio JH, Diangelo D. Biomechanical evaluation of flexor tendon function after hamate hook excision. J Hand Surg Am. 2003;28:138-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 43] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Xiong G, Dai L, Zheng W, Sun Y, Tian G. Clinical classification and treatment strategy of hamate hook fracture. J Huazhong Univ Sci Technolog Med Sci. 2010;30:762-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Davis DL. Hook of the Hamate: The Spectrum of Often Missed Pathologic Findings. AJR Am J Roentgenol. 2017;209:1110-1118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Sheridan J, Sheridan D, Sheridan D. Hook of Hamate Fractures in Major and Minor League Baseball Players. J Hand Surg Am. 2021;46:653-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Failla JM. Hook of hamate vascularity: vulnerability to osteonecrosis and nonunion. J Hand Surg Am. 1993;18:1075-1079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 47] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Stark HH, Chao EK, Zemel NP, Rickard TA, Ashworth CR. Fracture of the hook of the hamate. J Bone Joint Surg Am. 1989;71:1202-1207. [PubMed] |
| 9. | Gelberman RH, Gross MS. The vascularity of the wrist. Identification of arterial patterns at risk. Clin Orthop Relat Res. 1986;40-49. [PubMed] |
| 10. | Kato H, Nakamura R, Horii E, Nakao E, Yajima H. Diagnostic imaging for fracture of the hook of the hamate. Hand Surg. 2000;5:19-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Jie F, Hui Z, Dawei Z, Weiya Q. Treatment of the hook of hamate fracture with robot navigation: A note on technique. Acta Orthop Traumatol Turc. 2022;56:296-299. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 12. | Ceccarelli R, Dumontier C, Camuzard O. Minimally Invasive Fixation With a Volar Approach Using a Cannulated Compression Screw for Acute Hook of Hamate Fractures. J Hand Surg Am. 2019;44:993.e1-993.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Kuptniratsaikul V, Luangjarmekorn P, Kerr S, Vinitpairot C, Kitidumrongsook P. Grip strength after hamate hook excision and reconstruction surgery: A biomechanical cadaveric study. J Biomech. 2022;141:111221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 14. | Kim H, Kwon B, Kim J, Nam K. Isolated hook of hamate fracture in sports that require a strong grip comprehensive literature review. Medicine (Baltimore). 2018;97:e13275. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Egawa M, Asai T. Fracture of the hook of the hamate: report of six cases and the suitability of computerized tomography. J Hand Surg Am. 1983;8:393-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 51] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Scheufler O, Andresen R, Radmer S, Erdmann D, Exner K, Germann G. Hook of hamate fractures: critical evaluation of different therapeutic procedures. Plast Reconstr Surg. 2005;115:488-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 52] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 17. | Whalen JL, Bishop AT, Linscheid RL. Nonoperative treatment of acute hamate hook fractures. J Hand Surg Am. 1992;17:507-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 52] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Bevers MSAM, Daniels AM, van Rietbergen B, Geusens PPMM, van Kuijk SMJ, Sassen S, Kaarsemaker S, Hannemann PFW, Poeze M, Janzing HMJ, van den Bergh JP, Wyers CE. Assessment of the healing of conservatively-treated scaphoid fractures using HR-pQCT. Bone. 2021;153:116161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Sandberg OH, Aspenberg P. Inter-trabecular bone formation: a specific mechanism for healing of cancellous bone. Acta Orthop. 2016;87:459-465. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 53] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/