Published online Apr 18, 2025. doi: 10.5312/wjo.v16.i4.103388
Revised: February 21, 2025
Accepted: March 21, 2025
Published online: April 18, 2025
Processing time: 139 Days and 18.5 Hours
Non-operative spinal infections (NOSI) are caused by tuberculosis, brucella, and other specific bacteria. The etiology of the disease is insidious, the onset is slow and the diagnosis and treatment are difficult. Identifying the factors associated with spinal infection and early intervention can reduce the occurrence of the disease. At present, the research mainly focuses on the accurate diagnosis and treatment of spinal infection, and there are few studies on the prevention of spinal infection. The concept of "preventive treatment of diseases" in traditional Chinese medicine may help identify the causes and reduce the occurrence of NOSI.
To determine the association of age, bowel movements, and sleep patterns with NOSI.
Data of 69 NOSI patients and 84 healthy controls in a tertiary hospital from January 2019 to June 2024 were collected. Patients with NOSI had imaging evi
The mean age of the NOSI group and the control group was 63.55 ± 14.635 years and 59.18 ± 17.111 years, respectively, without statistical difference (P = 0.096). There was also no statistically significant difference in gender between the two groups. In the NOSI group, 45 (65.22%) were over 60 years old, and 44 (63.77%) were rural residents. Compared with the control group, the NOSI group had more patients with sleep disorder and defecation disorder, accounting for 69.57% and 68.12%, respectively, with significant statistical difference (both P < 0.001). Regression analysis showed that defecation and sleep disorders were closely related to NOSI (both P < 0.001).
Most patients with NOSI are older and have sleep disorders and abnormal defecation.
Core Tip: Non-operative spinal infection is a common clinical disease that seriously affects the stability of the spine. The etiology of the disease is insidious, the onset is slow and the diagnosis and treatment are difficult. Identifying the factors associated with spinal infection and early intervention can reduce the occurrence of the disease. We found that old age, sleep disturbances, and bowel disturbances were associated with non-surgical spinal infections. Traditional Chinese medicine emphasizes prevention more than treatment, and suggests that proper diet, moderate exercise and healthy life style can delay aging, improve sleep and intestinal abnormalities, thereby preventing spinal infections.
- Citation: Guo LL, Liu HK, Cao JF, Zhang HX, Li B, Li T, Li L. Senility, defecation disorders, sleep disorders, and non-operative spinal infections: A single-center retrospective analysis. World J Orthop 2025; 16(4): 103388
- URL: https://www.wjgnet.com/2218-5836/full/v16/i4/103388.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i4.103388
The Huang Di Nei Jing, the earliest medical classics in China, states: “The wise doctor can predict the disease before it occurs and intervene to prevent it from becoming worse; the middle-level doctors provide dialectical disease treatment, disease control and cure in time when the disease presents certain symptoms; and the low-level doctors often recognize the disease when there is a series of signs or symptoms of discomfort, and administer medicine and rescue treatment for the disease”. "Not sick, going to be sick, and already sick" are three different stages of disease development. With the continuous development of the idea of preventive treatment of disease in traditional Chinese medicine (TCM), more attention has been paid to prevention than treatment. Spinal infection is a common clinical disease that seriously affects the stability of the spine. Studies have shown that the incidence of spinal tuberculosis accounts for about 50% of patients with bone tuberculosis[1]. Spinal infection caused by brucellosis can account for more than half of the complications of brucellosis[2]. The identification of pathogenic bacteria for spinal infections is difficult, which often brings therapeutic challenges. Spinal infection is potentially fatal regardless of the cause. Severe cases can be life-threatening and mild cases can require months or even years of treatment. Therefore, it is important to explore the characteristics of spinal infection, identify possible causes, and intervene earlier to reduce its occurrence. Currently, most research on spinal infection has focused on the precise diagnosis and medical treatment, with little research into their associated causes.
In this study, we retrospectively analyzed the data of patients diagnosed with non-operative spinal infection (NOSI) in our hospital in the past 5 years. We sought to determine whether patients with NOSI were older, more likely to have sleep disorders and abnormal bowel movements, and propose suggestions and measures using the theory of "preventive treatment of diseases" in TCM.
Sixty-nine patients who were diagnosed with NOSI at our hospital from January 2019 to June 2024 were selected retrospectively for the analysis. Inclusion criteria were as follows: (1) Imaging (magnetic resonance imaging) evidence of spinal infections (including infections caused by tuberculosis, bruceopathy, and other pathogens); and (2) No history of spinal surgery in the past 1 year. Exclusion criteria were: (1) Spinal infection caused by spinal surgery; and (2) Patients whose clinical symptoms are inconsistent with imaging.
Data of all the hospitalized NOSI patients were collected. Patients who were repeatedly hospitalized for different diseases were counted as one patient, and the data were entered and analyzed according to the first diagnosis and treatment. Basic data were collected, sorted and analyzed in all patients, including age, sex, place of residence, sleep status and bowel movements. Patients who live in rural areas are classified as rural residents, and patients who live in urban areas are classified as urban residents. Sleep disorder was defined as sleep less than 6 hours daily, difficulty falling asleep, easy to wake up, feeling tired and inattentive after waking up; and normal sleep was defined as sleep more than 6 hours daily, and no special discomfort after waking up. Constipation is diagnosed in patients who had slow bowel movements and whose stool is dry and hard, and who need to help defecate with a cork or oral laxative. Stool more than 3 times a day with thin stool is diagnosed as diarrhea, and defecate once every 1-2 days with soft stool and easy to discharge is considered normal. Constipation and diarrhea are both considered obstacles to defecation.
In addition, 84 healthy people without spinal infection were randomly selected as the control group, and the gender, age, defecation and sleep status of the were collected.
All data were statistically analyzed using SPSS 22.0 software. Measurement data with normal distribution (such as age) were described as mean ± SD. When comparing groups, if the variance was homogeneous, the independent sample t test was used. If the variance was not uniform, the t' test was used. χ2 test was used to analyze the bicategorical variables such as sex, age, defecation and sleep. P < 0.05 was considered statistically significant.
A total of 69 patients with NOSI and 84 healthy individuals were included in the study. The average age of NOSI patients and healthy controls was 63.55 ± 14.635 and 59.18 ± 17.111, respectively, and there was no significant difference between the two groups. There were 35 men and 34 women in the NOSI group and 43 men and 41 women in the control group, and there was no statistical difference between the two groups. However, 45 of the NOSI patients were over 60 years old, accounting for 65.22%. Among the NOSI patients, 44 were rural residents, accounting for 63.77% (Table 1).
| Group | Age (year) | t value | P value | Gender | χ2 | P value | |
| Man | Female | ||||||
| Healthy (84) | 59.18 ± 17.111 | 1.677 | 0.096 | 43 | 41 | 0.003 | 0.954 |
| NOSI (69) | 63.55 ± 14.635 | 35 | 34 | ||||
Among the NOSI patients, 47 (68.12%) had abnormal defecation and 22 (31.88%) had normal defecation. Among the healthy controls, 25 (29.76%) had abnormal defecation and 59 (70.24%) had normal defecation. There was a statistical difference between the two groups (P < 0.001). Among the NOSI patients, 48 had abnormal sleep, accounting for 69.57%, and 21 had normal sleep, accounting for 30.43%. Among the healthy subjects, 25 (29.76%) had abnormal sleep and 59 (70.24%) had normal sleep. There was a statistical difference between the two groups (P < 0.001). Binary Logistics regression analysis of age, gender, defecation, sleep and NOSI showed that defecation disorders and sleep disorders were closely related to NOSI (both P < 0.001; Tables 2 and 3).
| Factors | B | S.E. | P value | Exp(B) | EXP(B) 95%CI |
| Age | 0.001 | 0.012 | 0.938 | 1.001 | 0.977-1.025 |
| Gender | -0.177 | 0.377 | 0.638 | 0.837 | 0.400-1.754 |
| defecation | 1.417 | 0.378 | < 0.001 | 4.125 | 1.965-8.659 |
| sleep | 1.515 | 0.383 | < 0.001 | 4.551 | 2.148-9.639 |
Our study showed that NOSI patients were mostly older, lived in rural areas, and had sleep disorders and defecation disorders, which may be related to the occurrence of NOSI. TCM believes that "when there is the positive qi in the body, evil qi cannot invade the body and cause diseases, whereas if evil qi accumulates, the healthy qi will be deficient". Older age, sleep disorders, and defecation disorders all can decline the body immunity through different mechanisms, resulting in "lack of healthy qi", in particular, people living in the endemic rural areas are more likely to be infected by evil qi, and eventually leading to disease occurrence.
The Huang Di Nei Jing states the effects of age on the body and disease development. With the increase of age, the body's organs are being exhausted and various functions decline. Modern research has found that as age increases, immunity declines and immune aging occurs. Immune aging can cause older people to have impaired response to infection when exposed to pathogens, and develop autoimmune diseases and chronic nonimmune diseases, including cardiovascular and neurodegenerative diseases, cancer, and epidemic diseases, such as coronavirus disease 2019; therefore, there are more age-related diseases in older people[3,4]. Reyes et al[5] summarized the contribution of viral and bacterial infections to aging and immune aging, and found that many RNA viruses (novel coronaviruses, hepatitis C virus, HIV, measles virus, dengue virus, and some influenza A viruses), DNA viruses (herpes virus Kaposi sarcoma virus, Epstein–Barr virus, hepatitis B virus, and Merkel cell polyomavirus), and bacteria are all associated with aging. There is a two-way link between infection and aging. By participating in various processes of the immune system, aging affects a variety of antibacterial functions in the host, increases the sensitivity of older people to different pathogens, induces inflammation or aggravates the original inflammatory response. In turn, bacterial infections can induce aging through a sustained inflammatory response.
The first signs of weakened immunity appear after the age of 50 years, and clinical relevance increases between the ages of 70 and 100 years, along with increased morbidity and mortality from infection[6]. Older adults are more susceptible to new infections and reactivation of latent viruses[4,7,8]. Aging cells make older people more susceptible to infections, cancer and other diseases; meanwhile, older people also have a lower protective response to vaccines. These may be related to decreased B cell and T cell responses with age. B-cell aging not only leads to a decreased antibody response to new pathogens, but also leads to an increase in the prevalence of autoimmunity with age[9]. In older people, the number and function of immune cells, the ability of antibody production, and the ability of immune memory are all decreased, leading to reduced defense of the body against the external environment, infection and diseases[10]. The elderly have a variety of immune senescence such as congenital immune senescence, adaptive immune senescence, inflammatory senescence, which leads to the imbalance of inflammation and immune function in the body, making the elderly more susceptible to diseases.
Elderly people have bone senescence, which is clinically manifested as osteoporosis, microscopically as impaired self-proliferation and renewal ability of bone marrow mesenchymal stem cells, decreased function and metabolism of osteoblasts, and altered mechanical response ability of osteoclasts, leading to changes in bone microenvironment[10]. Cytokines and growth factors in the bone microenvironment participate in the local inflammatory response, resulting in bone aging and chronic inflammatory changes in bone and joint. These make the bones and joints of the elderly more susceptible to disease. Moreover, studies have shown that infection can lead to or aggravate osteoporosis[11]. In the present study, we found that NOSI patients were mostly elderly, but there was no statistical difference compared with the healthy controls, which may be related to the small sample size. Although regression analysis showed no close relationship between age and NOSI, we confirmed that there was no statistically significant difference between the two groups at baseline, and univariate analysis showed some correlation between age and NOSI. Immune imbalances and changes in bone microstructure in the elderly may increase susceptibility to NOSIs in the elderly.
Age-related body changes are also associated with changes in gut flora. Many older people's nutritional changes lead to changes in intestinal flora and immune capacity. The imbalance of intestinal flora can also promote the occurrence of low-grade inflammation. We discuss the relationship between intestinal flora and inflammation and infection later. Older people also experience normal age-related changes in sleep and circadian rhythm, with significant sleep disorders[12]. We also discuss the relationship between sleep disorders and inflammation and infection later. In this retrospective analysis, we found that 65.22% of patients aged > 60 years suffered from NOSI, and 10 (14.50%) of them were > 80 years old. It is speculated that advanced age may be closely related to the occurrence of NOSI.
Prevalence of functional constipation in adults in the United States, Canada and United Kingdm is 7.9%-8.6%[13]. A survey of Chinese people found that the prevalence of chronic constipation was positively proportional to age, at 13%–18% for those aged > 60 years and 37.3% for those aged > 80 years[14]. Clinical findings indicate that intestinal flora imbalance is closely related to functional constipation, and there are characteristic changes in intestinal flora in patients with functional constipation[15]. For example, in patients with functional constipation, the abundance of intestinal probiotics (such as Bifidobacterium and Lactobacillus) decreased, the abundance of Desulphovibrio family (whose product H2S inhibits colon movement and promotes inflammation) increased, and the abundance of Butyricogenic bacteria increased (butyric acid maintains intestinal barrier integrity, prevents bacterial endotoxins and inflammatory reactions, and reduces interference with intestinal movement). Animal experiments have found that constipation leads to intestinal flora imbalance, resulting in increased permeability of the intestinal and blood–brain barriers, damage to the integrity and function of the intestinal barrier, imbalance of T cell subsets and disturbance of cytokines, and leads to uncontrolled passage of bacterial components, bacterial metabolites and harmful substances through the intestinal barrier, causing systemic inflammation[16]. Intestinal microbiota disorders are associated with the development and severity of a growing number of diseases, such as inflammatory bowel disease, autoimmune diseases, obesity, metabolic diseases, and neurological disorders. The intestinal microbiota is involved in maintaining the integrity of the intestinal epithelial barrier, resisting exogenous pathogens, maturation of the host intestinal immune system, metabolism of foreign or
Intestinal microbes form the gut–liver and gut–lung axes as well as the gut-brain axis. The gut-liver axis refers to the effects of intestinal flora, microbial metabolites, and interactions with the immune system on different liver diseases[17]. The gut-lung axis refers to the interaction between intestinal and lung flora. When intestinal flora are destroyed, the ecological balance of the lung flora may also change accordingly, resulting in lung infection[19].
According to the concept of TCM, lung and large intestine function are physiologically related. The lungs can affect the intestines, and lung diseases can also be relieved by treating the intestines, such as coughing, which can be treated by draining the large intestine. Conversely, the intestines can affect the lungs, and intestinal diseases can also be alleviated by treating the lungs, such as diarrhea, which can be treated by supplementing Lung qi. This is consistent with a lot of modern research. Studies have found that older patients with influenza A[20] and children with sepsis[19] both have significant intestinal flora imbalance, while type 2 diabetes with intestinal flora imbalance in late pregnancy leads to an increase in neonatal lung infection rate[21]. The mechanism may be that intestinal microbes are involved in regulating intestinal immune response and endotoxin levels, as well as T cell activity and immune response of pulmonary res
The gut is not only a digestive organ, but also an immune organ with immunoregulatory function, and a second brain" affecting brain function, all dues to the presence and regulation of intestinal flora[22]. Bowel disorders directly affect the gut microbiota. Intestinal microbiome, abundance of blood metabolites and lifestyle factors differ among defecation disorders[23]. Increased permeability of the intestinal barrier may lead to the entry of bacteria and their metabolites into the blood circulation, resulting in systemic infection.
Sleep plays an important role in regulating adaptive and innate immune responses. There is evidence that sleep disorders lead to downregulation of adaptive immunity, manifested by impaired response to infectious challenges, and upregulation of innate immune responses, manifested by increased cellular and genomic markers of inflammation[24]. The survey shows that nearly 25% of the population in the United States suffers from insomnia, and the prevalence of insomnia among older people in China ranges from 12% to 20%[25]. Sleep disturbances weaken adaptive immunity; therefore, the vaccine response and antiviral immune response are weakened, and the susceptibility to infectious diseases is increased. Sleep disorders are associated with inflammatory diseases such as rheumatoid arthritis and heart failure by increasing C-reactive protein, interleukin (IL)-6, IL-1β and tumor necrosis factor, reducing the activity of natural killer cells, and triggering immune responses. Habitual sleep duration decreased (< 5 h) or prolonged (> 9 h) is associated with an increased risk of pneumonia, and shorter sleep duration and fragmented sleep are associated with the common cold[24,25]. Ruel et al[26] found that insomnia before chemotherapy may increase the risk of immunity decline and infection due to chemotherapy during cancer treatment.
The pathogenesis of insomnia includes abnormalities of neurotransmitters, brain structure and endocrine system involved in sleep-wake regulation, activation of immune system and regulation of inflammatory response[27]. Long-term insomnia can lead to increased levels of inflammatory cytokines and reactive oxygen species in the blood[28], resulting in immune function changes in patients, and an increase in the incidence of various infections and tumors. Chronic insomnia by affecting T lymphocytes (CD3, CD4, CD8 cells), and natural killer cells (CD56) resulted in increased clinical infection and a variety of system infection compared with the normal population, especially the incidence of respiratory system infection and oral ulcer[29]. Long-term insomnia in the elderly can increase the risk of metabolic diseases such as osteoporosis[30]. Insomnia may trigger osteoporosis by affecting the immune system (immune cells and inflammatory factors), oxidative stress, increased sympathetic nerve activity, and decreased growth hormone levels[31,32]. Similar to aging that causes bone senescence and chronic inflammatory changes in bone and joint, insomnia affects multiple systems and causes changes in bone microenvironment, resulting in multiple bone and joint diseases. In the present study, we found that sleep disorders are closely related to NOSI, and immune imbalance and changes in bone microstructure in patients with sleep disorders may increase the susceptibility of this population to NOSI.
Wang et al[33]found that there was a two-way relationship between sleep and intestinal flora. They found that the three kinds of intestinal flora (class Negativicutes, order Selenomonadales, genus Rikenellaceae RC9 gut group) were significantly positively related with insomnia, and one type of gut microbiota (Lactococcus) was significantly negatively associated with insomnia. And Rikenellaceae RC9 intestinal group and insomnia are mutually causal. It is speculated that the microbial-gut-brain axis also plays a role in the course of spinal infection.
In this study, the place of residence of the patients was also recorded, and there were more rural than urban patients. However, no control study was conducted, and it was not clear whether the place of residence was related to spinal infection. People living in rural areas are more likely to come into contact with animals such as cattle, sheep, pigs and chickens, as well as water, soil and crops contaminated with feces. In areas with animal husbandry, surface water is easily polluted by untreated human and animal feces[34] resulting in serious water pollution in rural areas, and the number of intestinal infectious diseases caused by water pollution in rural areas is much higher than that in urban areas[35]. Zhu et al[36] monitored the contamination of roundworm eggs in the soil of 22 sites of 1090 households for 5 years, and found that the total detection rate of roundworm eggs in the soil was 30.73%, among which the detection rate of roundworm eggs in the soil of vegetable gardens, around toilets, yards and kitchens all exceeded 10%. These significantly increase the risk of infectious diseases in rural populations. A foreign survey of cyclospora in 732 people found that living in thatched huts, drinking untreated water, not having toilets, contact with fecal contaminated soil, and contact with poultry were the main causes of infection[37]. This is basically consistent with the domestic research results. Water, soil and crops contaminated by feces contain various parasites or their oocysts[37] and viruses and bacteria[38], which can cause infection. Animals are a common source of zoonotic bacteria[23]. Contact with animals carrying zoonotic bacteria can increase the risk of human infection, which may lead to temporary residence of bacteria in the body, and gradually cause local or even systemic infection under the stimulation of specific factors in the body. Cattle, sheep, pigs, etc. are the most common livestock in rural areas, and are also the most susceptible to Brucella infection. People are generally susceptible to Brucella, which can be transmitted through contact with infected livestock through damaged skin and mucous membranes, consumption of infected dairy products and meat, and mosquito bites[39]. In addition, with the adaptation of pathogenic microorganisms to the ecological environment, it will increase the mode of transmission of pathogens and increase the risk of zoonosis[40].
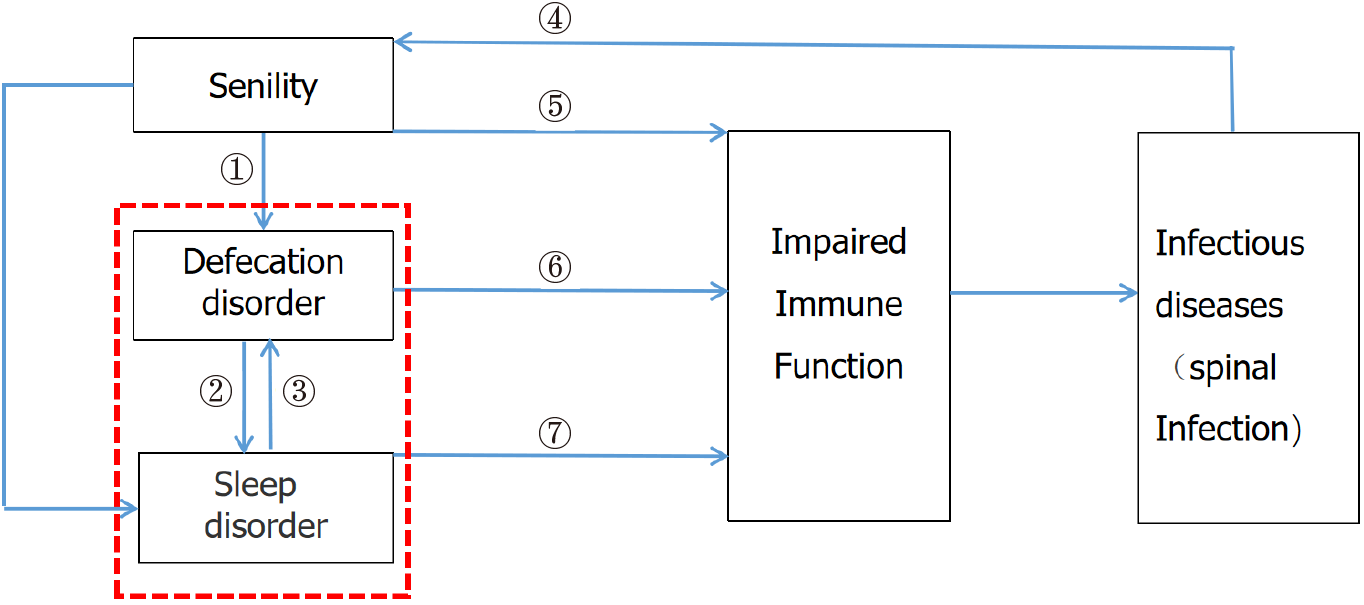
Old age, sleep disorders and defecation disorders are interrelated and interact with each other (Figure 1). They can all affect innate and adaptive immunity, resulting in reduced immunity. When the body is exposed to zoonotic bacteria, infection will occur. These factors may be closely related to the occurrence of NOSI.
The concept of preventive treatment of disease in TCM has the ideological connotation of preventing diseases before they occur, taking measures in advance to avoid disease aggravation, and preventing relapse after the diseases occur. It corresponds to the tertiary prevention of Western medicine, in which primary prevention is particularly important. If we take corresponding measures against pathogenic factors or risk factors at this time, we can directly avoid the occurrence and development of the diseases[41]. The thought of preventive treatment of disease in TCM aims at improving people's health awareness and advocating a healthy lifestyle in the new era. It pays attention to "conforming to the unity of nature and man", "nourishing healthy qi in the body", "regulating the spirit and behavior", and "cultivating the character and virtue"[42]. These are in line with the World Health Organization's "pivot forward" strategy. Compared with the Western medicine theory of disease prevention and treatment, Professor Zhang Bo-Li believes that “the medicine that makes people not get sick is good medicine”. The idea of "preventive treatment of disease" and health care advocated by TCM represents a more positive preventive medicine idea[43]. The healthy life style advocated by this idea is similar to a new medical science in modern times - lifestyle medicine. Lifestyle medicine is a new interdisciplinary discipline involving medicine, nutrition, exercise science, epidemiology, psychology and other fields, which plays a bridging role between promoting public health and clinical treatment. It focuses more on individual behavior and lifestyle adjustments, emphasizing the role of daily life[44]. The Lifestyle Medicine Global Alliance identifies six key elements of lifestyle medicine, including whole food or plant-based eating patterns, physical activity, restorative sleep, stress management, avoidance of dangerous substances, and positive social relationships[45]. The connotation of lifestyle medicine has already been reflected in the thought of preventive treatment of disease in Huang Di Nei Jing. For example, it pays attention to diet adjustment, emphasizing that "grains are nourishing, five fruits are helping, five animals are benefiting, and five vegetables are supplementing". It emphasizes the importance of exercise, pointing out that "sitting for a long time hurts the flesh, lying for a long time hurts the qi", and "exercise removes all diseases and prolongs life". It also emphasizes mental and psychological peace, pointing out that "all diseases are born from qi", and people should be in a state of calm and nihilism so that natural qi can act normally, thus preventing diseases. It emphasizes that people should have adequate sleep in accordance with nature; and maintain a good lifestyle.
Studies have shown that old age, malnutrition, obesity, long-term smoking, high-risk occupations, hypoalbuminemia, immunocompromised and other comorbidities and long-term specific medications are associated with spinal infections[46,47].
Older people need to reduce the risk of NOSI in the following ways. (1) Maintaining a reasonable diet, maintaining normal intestinal flora, and ensuring normal bowel habits and frequency; (2) Having sufficient sleep and maintaining the normal circadian rhythm of sleep; (3) Having appropriate physical activity to increase the immunity of middle-aged and older people; and (4) Keeping a peaceful mind.
This is a preliminary study with a small sample size, and a correlation study with a large sample size is needed in the future. Due to its retrospective nature, this study did not conduct immune-related laboratory index analysis, which is also the direction of further exploration in the future. In this paper, the incidence of combined diseases was counted initially, but no correlation analysis was made. A large randomized controlled trial is needed in the future studies. Further research is also possible to reduce lumbar susceptibility by studying better posture to reduce compression in the lumbar spine.
NOSI is a common clinical disease that seriously affects the stability of the spine. We found that older age, sleep disturbances, and bowel movement disturbances were associated with NOSI. Older age, sleep disorders, and intestinal disorders may be related to NOSI through immune aging, bone aging, intestinal flora disorders, chronic low-grade inflammation and other mechanisms. TCM emphasizes prevention more than treatment, and suggests that proper diet, moderate exercise and healthy life style can delay aging, improve sleep and intestinal abnormalities, thereby preventing spinal infections.
| 1. | Kumar V, Neradi D, Sherry B, Gaurav A, Dhatt SS. Tuberculosis of the spine and drug resistance: a review article. Neurosurg Rev. 2022;45:217-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 2. | Wang W, Fan Z, Zhen J. MRI radiomics-based evaluation of tuberculous and brucella spondylitis. J Int Med Res. 2023;51:3000605231195156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 3. | Calder PC, Ortega EF, Meydani SN, Adkins Y, Stephensen CB, Thompson B, Zwickey H. Nutrition, Immunosenescence, and Infectious Disease: An Overview of the Scientific Evidence on Micronutrients and on Modulation of the Gut Microbiota. Adv Nutr. 2022;13:S1-S26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 70] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 4. | Liu Z, Liang Q, Ren Y, Guo C, Ge X, Wang L, Cheng Q, Luo P, Zhang Y, Han X. Immunosenescence: molecular mechanisms and diseases. Signal Transduct Target Ther. 2023;8:200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 296] [Cited by in RCA: 550] [Article Influence: 183.3] [Reference Citation Analysis (3)] |
| 5. | Reyes A, Ortiz G, Duarte LF, Fernández C, Hernández-Armengol R, Palacios PA, Prado Y, Andrade CA, Rodriguez-Guilarte L, Kalergis AM, Simon F, Carreño LJ, Riedel CA, Cáceres M, González PA. Contribution of viral and bacterial infections to senescence and immunosenescence. Front Cell Infect Microbiol. 2023;13:1229098. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 6. | Zhang H, Weyand CM, Goronzy JJ. Hallmarks of the aging T-cell system. FEBS J. 2021;288:7123-7142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 111] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 7. | Goronzy JJ, Weyand CM. Mechanisms underlying T cell ageing. Nat Rev Immunol. 2019;19:573-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 355] [Article Influence: 50.7] [Reference Citation Analysis (0)] |
| 8. | De Maeyer RPH, Chambers ES. The impact of ageing on monocytes and macrophages. Immunol Lett. 2021;230:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 187] [Article Influence: 31.2] [Reference Citation Analysis (0)] |
| 9. | Teissier T, Boulanger E, Cox LS. Interconnections between Inflammageing and Immunosenescence during Ageing. Cells. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 179] [Article Influence: 44.8] [Reference Citation Analysis (0)] |
| 10. | Wang JX, Dong ZH, Huang ZS, Li SY, Yang G. [Interaction between immune microenvironment and bone aging and treatment strategies]. Zhongguo Zuzhi Gongcheng Yanjiu. 2025;1-11. |
| 11. | Zou X, Ma Z, Liu X, Zhang K, Qiu C, Liang R, Weng D, Xie L, Cao X, Wu Y, Wen L. Risk factors and prognostic value of osteoporosis in hospitalized patients with bronchiectasis. BMC Pulm Med. 2023;23:55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 12. | Cohen ZL, Eigenberger PM, Sharkey KM, Conroy ML, Wilkins KM. Insomnia and Other Sleep Disorders in Older Adults. Psychiatr Clin North Am. 2022;45:717-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 39] [Reference Citation Analysis (0)] |
| 13. | Palsson OS, Whitehead W, Törnblom H, Sperber AD, Simren M. Prevalence of Rome IV Functional Bowel Disorders Among Adults in the United States, Canada, and the United Kingdom. Gastroenterology. 2020;158:1262-1273.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 310] [Article Influence: 51.7] [Reference Citation Analysis (0)] |
| 14. | Chu H, Zhong L, Li H, Zhang X, Zhang J, Hou X. Epidemiology characteristics of constipation for general population, pediatric population, and elderly population in china. Gastroenterol Res Pract. 2014;2014:532734. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 88] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 15. | Li Y, Zhang XH, Wang ZK. Microbiota treatment of functional constipation: Current status and future prospects. World J Hepatol. 2024;16:776-783. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 16. | Lin X, Liu Y, Ma L, Ma X, Shen L, Ma X, Chen Z, Chen H, Li D, Su Z, Chen X. Constipation induced gut microbiota dysbiosis exacerbates experimental autoimmune encephalomyelitis in C57BL/6 mice. J Transl Med. 2021;19:317. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 53] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 17. | Di Vincenzo F, Del Gaudio A, Petito V, Lopetuso LR, Scaldaferri F. Gut microbiota, intestinal permeability, and systemic inflammation: a narrative review. Intern Emerg Med. 2024;19:275-293. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 624] [Article Influence: 312.0] [Reference Citation Analysis (0)] |
| 18. | Wang Z, Wang Z, Lu T, Chen W, Yan W, Yuan K, Shi L, Liu X, Zhou X, Shi J, Vitiello MV, Han Y, Lu L. The microbiota-gut-brain axis in sleep disorders. Sleep Med Rev. 2022;65:101691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 190] [Reference Citation Analysis (0)] |
| 19. | Wang LY, Li XL, Wang HF, Li SY. [Discussion on Correlation Between Intestinal Microbes and Respiratory Diseases]. Zhonghua Zhongyiyao Xuekan. 2019;37:1859-1861. [DOI] [Full Text] |
| 20. | Maimetiturson A, Kai L, Abduweili K. [Relationship between intestinal flora imbalance and Pneumococcus infection in elderly patients with severe pneumonia caused by influenza A virus]. Zhongguo Weishengtaixue Zazhi. 2024;36:688-693. [DOI] [Full Text] |
| 21. | Lyv ZY, Wang LJ, Xu MX, Bai XF, Cao LJ. [Association between the structure of intestinal flora and inflammatory response in children with sepsis: a prospective cohort study]. Zhongguo Dang Dai Er Ke Za Zhi. 2024;26:567-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 22. | Cryan JF, O'Riordan KJ, Cowan CSM, Sandhu KV, Bastiaanssen TFS, Boehme M, Codagnone MG, Cussotto S, Fulling C, Golubeva AV, Guzzetta KE, Jaggar M, Long-Smith CM, Lyte JM, Martin JA, Molinero-Perez A, Moloney G, Morelli E, Morillas E, O'Connor R, Cruz-Pereira JS, Peterson VL, Rea K, Ritz NL, Sherwin E, Spichak S, Teichman EM, van de Wouw M, Ventura-Silva AP, Wallace-Fitzsimons SE, Hyland N, Clarke G, Dinan TG. The Microbiota-Gut-Brain Axis. Physiol Rev. 2019;99:1877-2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1156] [Cited by in RCA: 3212] [Article Influence: 458.9] [Reference Citation Analysis (2)] |
| 23. | Johnson-Martínez JP, Diener C, Levine AE, Wilmanski T, Suskind DL, Ralevski A, Hadlock J, Magis AT, Hood L, Rappaport N, Gibbons SM. Aberrant bowel movement frequencies coincide with increased microbe-derived blood metabolites associated with reduced organ function. Cell Rep Med. 2024;5:101646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 24. | Irwin MR. Why sleep is important for health: a psychoneuroimmunology perspective. Annu Rev Psychol. 2015;66:143-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 482] [Cited by in RCA: 797] [Article Influence: 66.4] [Reference Citation Analysis (0)] |
| 25. | Irwin MR, Straub RH, Smith MT. Heat of the night: sleep disturbance activates inflammatory mechanisms and induces pain in rheumatoid arthritis. Nat Rev Rheumatol. 2023;19:545-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 38] [Reference Citation Analysis (0)] |
| 26. | Ruel S, Ivers H, Savard MH, Gouin JP, Lemieux J, Provencher L, Caplette-Gingras A, Bastien C, Morin CM, Couture F, Savard J. Insomnia, immunity, and infections in cancer patients: Results from a longitudinal study. Health Psychol. 2020;39:358-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 27. | Qian JH, Gao XY, Qi SW, Li YB, Li YJ, Li W. [Effects of Needling Back-Shu Points on Levels of STAT3, Th17/Treg Balance, and Related Inflammatory Factors in Hypothalamus of Insomnia Model Rats]. Zhenjiu Linchuang Zazhi. 2024;40:72-78. [DOI] [Full Text] |
| 28. | Aghelan Z, Karima S, Khazaie H, Abtahi SH, Farokhi AR, Rostampour M, Bahrehmand F, Khodarahmi R. Interleukin-1α and tumor necrosis factor α as an inducer for reactive-oxygen-species-mediated NOD-like receptor protein 1/NOD-like receptor protein 3 inflammasome activation in mononuclear blood cells from individuals with chronic insomnia disorder. Eur J Neurol. 2022;29:3647-3657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 29. | Savard J, Laroche L, Simard S, Ivers H, Morin CM. Chronic insomnia and immune functioning. Psychosom Med. 2003;65:211-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 124] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 30. | Liu HZ, Fu XM, Li XJ, Wang YH, Hu XD, Xu HJ, Wang AN, Lyu ZH, Dong S, Pei Y. [A Mendelian randomization study on the relationship between insomnia and osteoporosis]. Zhonghua Nei Ke Za Zhi. 2024;63:776-780. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 31. | Wright CJ, Milosavljevic S, Pocivavsek A. The stress of losing sleep: Sex-specific neurobiological outcomes. Neurobiol Stress. 2023;24:100543. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 30] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 32. | Lucassen EA, de Mutsert R, le Cessie S, Appelman-Dijkstra NM, Rosendaal FR, van Heemst D, den Heijer M, Biermasz NR; NEO study group. Poor sleep quality and later sleep timing are risk factors for osteopenia and sarcopenia in middle-aged men and women: The NEO study. PLoS One. 2017;12:e0176685. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 82] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 33. | Wang Q, Gao T, Zhang W, Liu D, Li X, Chen F, Mei J. Causal relationship between the gut microbiota and insomnia: a two-sample Mendelian randomization study. Front Cell Infect Microbiol. 2024;14:1279218. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 34. | Akhter S, Bhat MA, Ahmed S, Siddiqui WA. Antibiotic residue contamination in the aquatic environment, sources and associated potential health risks. Environ Geochem Health. 2024;46:387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 31] [Reference Citation Analysis (0)] |
| 35. | Wang Q, Zhao YC, Qu WD, Chen XD, He ZA, Tao L, Wu CY, E XL, Zhang L, Zhang SZ, Li QH, Cao ZJ. [Investigation of Drinking Water Contamination Incidents in China during 1996-2006]. Huangjingyujiankang Zazhi. 2010;27:328-331. |
| 36. | Zhu HH, Zhou CH, Zang W, Zhang XQ, Chen YD. [Monitoring and SWOT analysis of Ascaris eggs pollution in soil of rural China]. Zhongguo Xuexichongbing Fangzhi Zazhi. 2014;26:274-278. [DOI] [Full Text] |
| 37. | Chacin-Bonilla L, Sanchez Y, Cardenas R. Factors associated with Cyclospora infection in a Venezuelan community: extreme poverty and soil transmission relate to cyclosporiasis. Trans R Soc Trop Med Hyg. 2023;117:83-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 38. | Ferreira FDG, Carlon P, Fongaro G, Magri ME. Recycling composted human feces as biofertilizer for crop production: Assessment of soil and lettuce plant tissue contamination by Escherichia coli and human adenovirus. Sci Total Environ. 2024;928:172375. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 39. | Shin IS, Roh SG, Gill BC, Kim YS, Hwang KW. Assessment of brucellosis-causing pathogens with an emphasis on the prevalence of Brucella melitensis in the Republic of Korea: insights from a decade of pathogen surveillance (2014-2023), a retrospective study. Osong Public Health Res Perspect. 2024;15:489-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 40. | Green AG, Vargas R, Marin MG, Freschi L, Xie J, Farhat MR. Analysis of Genome-Wide Mutational Dependence in Naturally Evolving Mycobacterium tuberculosis Populations. Mol Biol Evol. 2023;40:msad131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 41. | Sartori P, Egloff C, Hcini N, Vauloup Fellous C, Périllaud-Dubois C, Picone O, Pomar L. Primary, Secondary, and Tertiary Prevention of Congenital Cytomegalovirus Infection. Viruses. 2023;15:819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 42. | Hao YD, Zhang XH, Zhang Y, Wang XC. [Exploration of the thought of preventive treatment of disease in traditional Chinese medicine and its modern application]. Changchun Zhongyiyaodaxue Xuebao. 2024;40:600-603. [DOI] [Full Text] |
| 43. | Zhang BL. [For the future: the world needs Traditional Chinese Medicine]. Yijia Zhengming. 2016;7:1-4. [DOI] [Full Text] |
| 44. | Phillips EM, Frates EP, Park DJ. Lifestyle Medicine. Phys Med Rehabil Clin N Am. 2020;31:515-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 45. | Guthrie GE. What Is Lifestyle Medicine? Am J Lifestyle Med. 2018;12:363-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 46. | Galetta MS, Kepler CK, Divi SN, Russo GS, Segar AH, Boody BS, Bronson WH, Rihn JA, Goyal DKC, Fang T, Schroeder GD, Vaccaro AR. Consensus on Wound Care of SSI in Spine Surgery. Clin Spine Surg. 2020;33:E206-E212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 47. | Chen M, Baumann AN, Fraiman ET, Cheng CW, Furey CG. Long-term survivability of surgical and nonsurgical management of spinal epidural abscess. Spine J. 2024;24:748-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/